Abstract
The aims of present study were to evaluate the prevalence, risk factors, and prognostic significance of masked hypertension in diabetic patients. Using a cross-sectional design, 266 patients with documented type 2 diabetes mellitus and clinic blood pressure (BP) <140/90 mm Hg without antihypertension treatment were enrolled; 24-hour ambulatory BP monitoring was applied to evaluate mean 24-hour systolic/diastolic BP. Demographics, medical histories, and medications usage were obtained using questionnaire. Fasting venous blood was drawn for biochemical analysis. Approximately 26.5% of participants were diagnosed as masked hypertension with mean 24-hour systolic BP >130 mm Hg and/or mean 24-hour diastolic BP >80 mm Hg. Compared with those without masked hypertension, other than significantly higher mean 24-hour systolic/diastolic BP, patients with masked hypertension were more elderly, had higher serum glycated hemoglobin (HbA1c) and C-reactive protein (CRP) levels and higher prevalence of coronary heart disease (CHD). Multivariate regression analysis showed that aging, increased HbA1c and CRP levels, and prevalent CHD were independently associated with masked hypertension. Logistic regression analysis revealed that after adjusted for traditional risk factors including age, male sex, smoking status, low-density lipoprotein-cholesterol, CRP, clinic systolic BP, and HbA1c, masked hypertension remained independently associated with prevalent cardiovascular disease (CVD), with odds ratio of 1.31 and 95% confidence interval of 1.11 to 1.85. In summary, in diabetic patients, concurrent masked hypertension increases the odds of having CVD. Future randomized controlled trials are warranted to investigate whether screening and managing masked hypertension could reduce cardiovascular events in diabetic patients.
Keywords: cardiovascular diseases, diabetes mellitus, mask hypertension
1. Introduction
Hypertension is a major public health problem around the world owing to its causal relationship to a variety of cardiovascular and renal diseases.[1–3] Epidemiological studies indicate that a substantial number of patients are masked hypertension that is defined as clinic blood pressure (BP) <140/90 mm Hg, whereas mean 24-hour ambulatory BP (ABP) >130 and/or 80 mm Hg.[4–6] In recent years, results from observational studies reveal that individuals with masked hypertension have a higher cardiovascular disease (CVD) risk compared with those with normotension,[6,7] suggesting that it may be beneficial to screen and manage individuals with masked hypertension.
Diabetes mellitus (DM) is another major risk factor for cardiovascular and renal diseases.[8,9] Interestingly and importantly, prior epidemiological studies indicate that patients with DM have increased risk of developing incident hypertension than those without DM,[10,11] and the underlying mechanisms may be at least partially related to increased sympathetic nerve activity in diabetic patients, which is also a potential mechanism of masked hypertension.[12] Taken together, one may speculate that the prevalence of masked hypertension may be higher in patients with DM versus those without DM. Nevertheless, the prevalence and potential risk factors of masked hypertension in patients with DM is less well studied. In addition, whether diabetic patients with masked hypertension have higher prevalence of CVD than their diabetic counterparts without masked hypertension is also unknown. Therefore, in our present study, we used a cross-sectional design to evaluate the prevalence, risk factors, and prognostic significance of masked hypertension in patients with DM.
2. Methods
2.1. Studied design and participants enrollment
This was a cross-sectional study, and the present study was approved by the Clinical Research Ethic Committee of the Shenzhen Sun Yat-sen Cardiovascular Hospital. Participants were enrolled after informed consent was obtained and all participants were treated based on the Declaration of Helsinki. Included criteria were 2-folds: 45 to 75 years old and had documented type 2 DM. Excluded criteria were as follows: documented hypertension, treating with antihypertensive medications or clinic BP >40 and/or 90 mm Hg at screening, had myocardial infarction, ischemic stroke or congestive heart failure in the past 12 months, or with estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2.[13]
2.2. Clinic and ambulatory blood pressure measurements
Clinic BP measurements were conducted in accordance to the JNC7 guideline recommendation[14] and participants sat quietly for 5 minutes and nondominant arm was selected and placed at the heart level. Three consecutive BP readings were obtained with 1-minute interval of each reading, and the last 2 readings were averaged and defined as clinic BP (HEM7200, Omron Healthcare, Tokyo, Japan). ABP measurements were performed by 24-hour ABP monitoring (The Spacelabs 90217, Spacelabs Inc, Redmond, WA) and BP reading was measured in each 20 minutes during daytime and each 30 minutes during nighttime. Participants were asked to record the time when they went to sleep that was used to defined daytime and nighttime periods. Masked hypertension was defined as clinic systolic and diastolic BP <140/90 mm Hg, whereas mean 24-hour systolic BP >130 mm Hg and/or mean 24-hour diastolic BP >80 mm Hg.
2.3. Clinical and biochemical data collection
Structured questionnaire including information about participants’ demographics, medical histories, and current medications usage was provided to each participant. In brief, CVD including coronary heart disease (CHD), ischemic stroke, and peripheral artery disease were diagnosed based on clinical symptoms and imaging evidence including coronary angiography, computed tomography with contrast, and peripheral vascular ultrasound as appropriate. Biochemical parameters including serum levels of fasting plasma glucose (FPG), glycated hemoglobin A1c (HbA1c), lipid profiles, creatinine (Cr), and C-reactive protein (CRP) were measured using fasting venous blood.
2.4. Statistical analysis
Continuous variables were expressed as mean ± SD and categorical variables were expressed as number and frequency of cases. Between-group differences were evaluated by the independent Student t test or the χ2 analysis as appropriate. Univariate and multivariate regression analysis were used to evaluate potential risk factors of masked hypertension. In the logistic regression analysis, age, male sex, smoking status, low-density lipoprotein-cholesterol (LDL-C), CRP, clinic SBP, and HbA1c were entered in stepwise models for adjustment of the association between masked hypertension and prevalence of CVD in diabetic participants. Statistical analysis was conducted in SPSS 23.0 (IBM, Armonk, NY).
3. Results
3.1. General characteristics
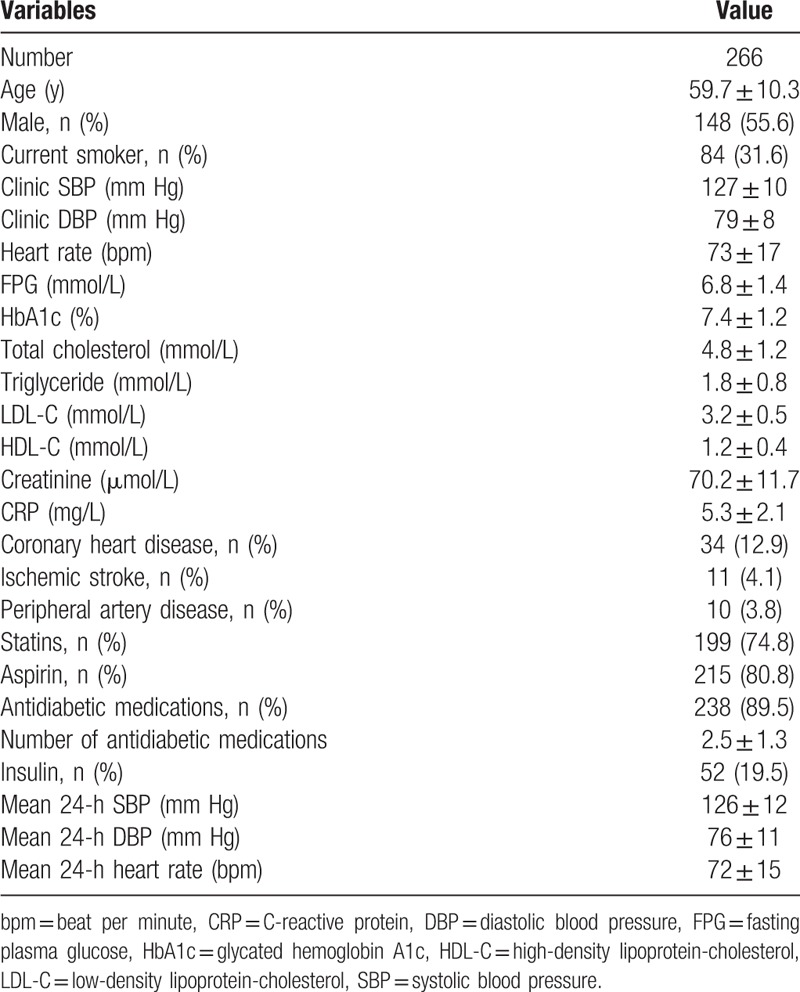
From January of 2016 to March of 2017, a total of 266 participants were enrolled. General characteristics of participants were presented in Table 1. The mean age was 59.7 ± 10.3 years old and male participants accounted for 55.6%. The mean clinic systolic and diastolic BP were 127 ± 10 and 79 ± 8 mm Hg, respectively. The mean 24-hour systolic and diastolic BP were 126 ± 12 and 76 ± 11 mm Hg, respectively. Regarding the prevalence of CVD, 12.9%, 4.1%, and 3.8% of participants had coronary artery disease, ischemic stroke, and peripheral artery disease, respectively. The mean number of antidiabetic medication was 2.5 ± 1.3 and 19.5% were prescribed insulin.
Table 1.
General characteristics of participants.
3.2. Prevalence of masked hypertension
Among enrolled participants, the prevalence of masked hypertension was approximately 26.5%. Compared with those without masked hypertension, participants with masked hypertension had significantly higher mean 24-hour systolic BP (135 ± 7 vs 122 ± 6 mm Hg), diastolic BP (87 ± 9 vs 72 ± 7 mm Hg), and mean heart rate, whereas no significant between-group differences in clinic BP were observed (Table 2).
Table 2.
Comparisons between masked hypertension and no masked hypertension groups.
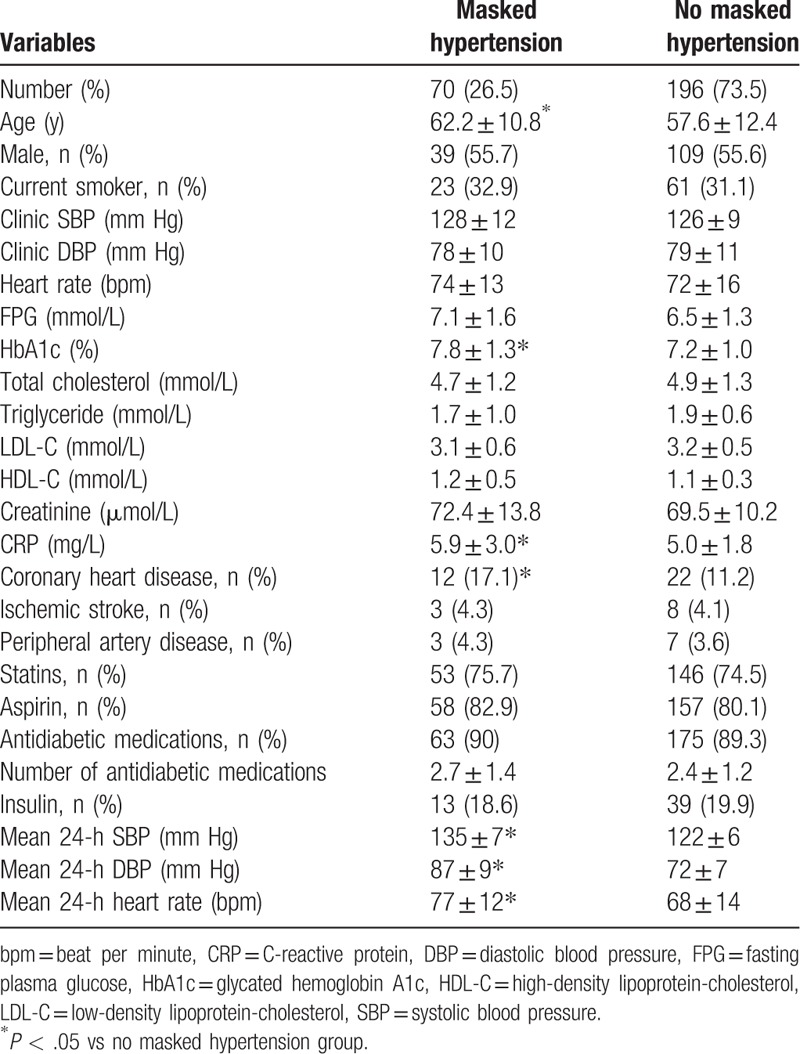
In addition, participants in the masked hypertension group were more elderly, had higher serum HbA1c and CRP levels, and had higher prevalence of CHD compared with those without masked hypertension. No significant between-group differences in other risk factors and comorbidities were observed.
3.3. Risk factors of masked hypertension
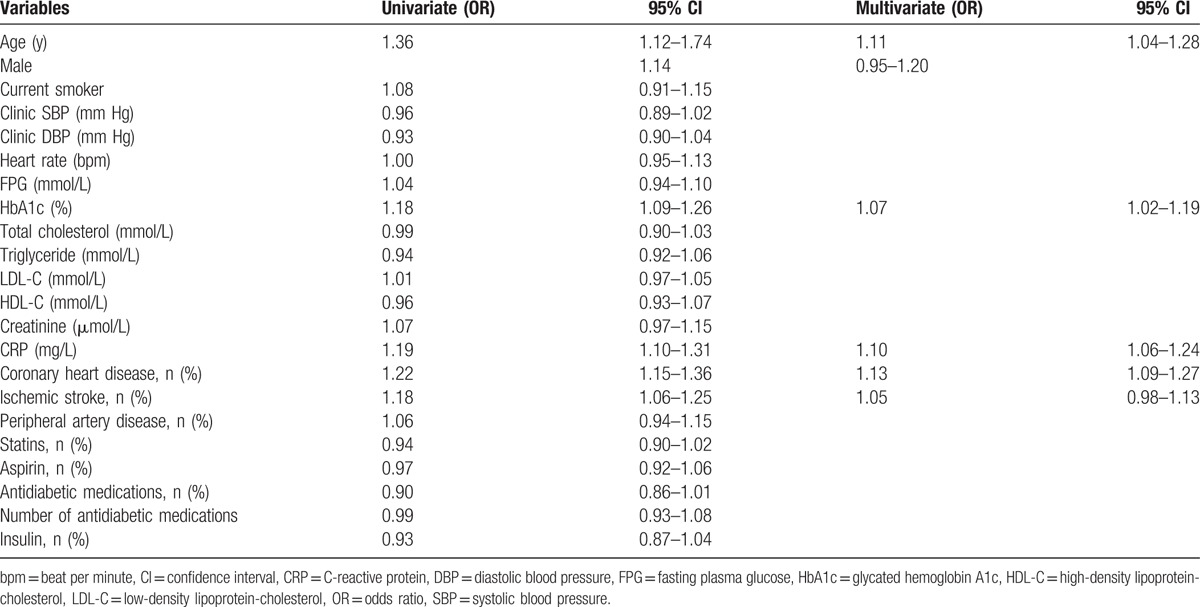
Univariate and multivariate regression analyses were used to evaluate the potential risk factors of masked hypertension, and as presented in Table 3, in the univariate regression analysis, aging, increased serum HbA1c and CRP levels, prevalent CHD, and ischemic stroke were all significantly associated with masked hypertension. Nonetheless, in the multivariate regression analysis, the odds ratios of these above risk factors were attenuated but still statistically significant except ischemic stroke.
Table 3.
Risk factors of masked hypertension.
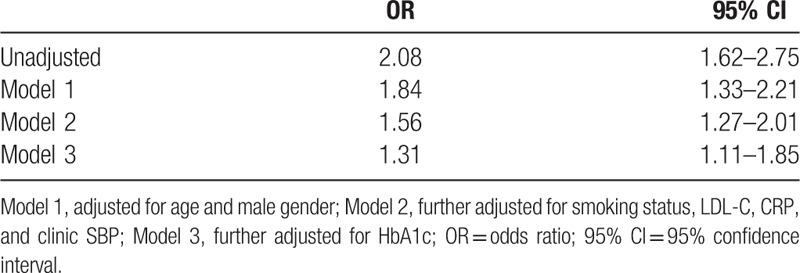
3.4. Association of masked hypertension and prevalent CVD
The association of masked hypertension and prevalent CVD including CHD, ischemic stroke, and peripheral artery disease were evaluated using logistic regression analysis. As presented in Table 4, in adjusted model, masked hypertension was associated with approximately 2-fold higher odds of prevalent CVD. In a stepwise adjusted model, after adjusted for age, male sex, smoking status, LDL-C, CRP, clinic SBP, and HbA1c, masked hypertension remained significantly associated with prevalent CVD in diabetic patients, with odds ratio of 1.31 and 95% confidence interval of 1.11 to 1.85.
Table 4.
Associations of masked hypertension and prevalent CVD.
4. Discussion
To our best knowledge, our present study is the first few studies to investigate the prevalence, risk factors, and prognostic significance of masked hypertension in patients with diabetes. The principal findings of present study include the following: first, the prevalence of masked hypertension in diabetic patients of present study was 26.5%; second, associated independent risk factors of masked hypertension included aging, increased serum HbA1c and CRP levels, and prevalent CHD; third, masked hypertension was associated with approximately 31% higher odds of having prevalent CVD in diabetic patients even adjusted for other risk factors.
Notably, hypertension and DM are 2 major independent risk factors of CVD. In addition, prior epidemiological studies show that diabetic patients have increased risk of developing hypertension compared with those without diabetes,[11] and diabetic patients with hypertension also have increased risk of developing cardiovascular and renal diseases compared with their counterparts without hypertension.[10] Therefore, it is clinically relevant to screen and manage hypertension in patients with diabetes. Masked hypertension is an important phenotype of hypertension. Masked hypertension is featured by normal clinic BP level, whereas BP out of clinic office is elevated. Numerous studies also have shown that masked hypertension is associated with increased cardiovascular events.[6,7] In our present study, we observed that in diabetic patients with normal clinic BP level, using 24-hour ABPM identified approximately 26.5% of masked hypertensive patients. Importantly, as presented in Table 2, these patients had higher cardiovascular risk profiles compared with those without masked hypertension, suggesting that in diabetic patients with normal clinic BP level, evaluating their 24-hour ambulatory BP level may be beneficial for identifying those high-risk patients.
Our present study showed that aging, increased serum CRP and HbA1c level, and prevalent CHD were independently associated with masked hypertension. Notably, aging [15–17] and DM [18,19] are commonly associated with autonomic nerve disorder that in turn led to BP fluctuation, especially under stress and having daily physical activity. Therefore, it is possible that increased age and HbA1c level were independently associated with masked hypertension. Interestingly, increased serum CRP level was also independently associated with masked hypertension. We were unsure about the underlying mechanism. However, one might speculate that increased serum CRP level might be associated with endothelial dysfunction,[20] which in turn caused vascular diastolic function impairment and BP elevation. In addition, prevalent CHD might also reflect the existing endothelial dysfunction and decreased organ perfusion, which in turn also led to BP elevation. Owing to the weakness of clinic BP in terms of limited BP measurement, one may speculate that using 24-hour ABPM to capture out of clinic's BP in diabetic patients should be beneficial to identify masked hypertensive patients.
We further evaluated whether prevalent masked hypertension would increase risk of having prevalent CVD in diabetic patients. Importantly, we observed that even adjusted for traditional risk factors of CVD, masked hypertension still significantly associated with prevalent CVD, with 31% higher odds, suggesting that screening masked hypertension in diabetic patients may be beneficial to better stratify CVD risk. Owing to the independent risk of BP elevation for CVD, one may speculate that using antihypertensive medications to normalize 24-hour ambulatory BP level in diabetic patients would be beneficial to reduce cardiovascular risk.
There are some limitations of our present study deserved to be addressed. First, this was a cross-sectional study that could not allow us to draw causal relationship between risk factors and masked hypertension. In addition, the associations of masked hypertension and prevalent CVD were also compromised by undetected and unmeasured biases. Second, the present study should not be generalized to other population groups. Third, since the prevalence of CVD in present study was relatively small, the findings of present study should not be extrapolated to other populations group with much higher prevalent CVD. Nevertheless, of the first few studies the present study was to evaluate the prevalence, risk factors, and prognostic significance of masked hypertension in diabetic patients, and findings from present study could provide novel and deep insights into the relationship between masked hypertension and diabetes.
5. Conclusions
Our present study observes that the prevalence of masked hypertension in diabetic patients is now low, and masked hypertension is independently associated with aging, increased serum HbA1c and CRP levels, and prevalent CHD. In diabetic patients, concurrent masked hypertension increases the odds of having CVD. Future randomized controlled trials are warranted to investigate whether screening and managing masked hypertension could reduce cardiovascular events in diabetic patients.
Acknowledgment
We thank Huan Wang, PhD, for assisting us in performing statistical analysis of our paper.
Footnotes
Abbreviations: ABPM = ambulatory blood pressure monitoring, BP = blood pressure, CHD = coronary heart disease, CI = confidence interval, Cr = creatinine, CRP = C-reactive protein, CVD = cardiovascular diseases, DBP = diastolic blood pressure, DM = diabetes mellitus, eGFR = estimated glomerular filtration rate, FPG = fasting plasma glucose, HbA1c = glycated hemoglobin, LDL-C = low-density lipoprotein-cholesterol, OR = odds ratio, SBP = systolic blood pressure.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013;31:1281–357. [DOI] [PubMed] [Google Scholar]
- [2].Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet 2016;387:435–43. [DOI] [PubMed] [Google Scholar]
- [3].Brunström M, Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta-analyses. BMJ 2016;352:i717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Melgarejo JD, Maestre GE, Thijs L, et al. Prevalence, treatment, and control rates of conventional and ambulatory hypertension across 10 populations in 3 continents. Hypertension 2017;70:50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Morris JH, Bisognano JD. Masked hypertension: finding trouble under the disguise. Circ Cardiovasc Qual Outcomes 2017;10: pii: e003945. [DOI] [PubMed] [Google Scholar]
- [6].Gijón-Conde T, Graciani A, López-García E, et al. Short-term variability and nocturnal decline in ambulatory blood pressure in normotension, white-coat hypertension, masked hypertension and sustained hypertension: a population-based study of older individuals in Spain. Hypertens Res 2017;40:613–9. [DOI] [PubMed] [Google Scholar]
- [7].Anstey DE, Booth JN, Abdalla M, et al. Predicted atherosclerotic cardiovascular disease risk and masked hypertension among blacks in the Jackson heart study. Circ Cardiovasc Qual Outcomes 2017;10: pii: e003421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kissela BM, Khoury J, Kleindorfer D, et al. Epidemiology of ischemic stroke in patients with diabetes: the greater Cincinnati/Northern Kentucky Stroke Study. Diabetes Care 2005;28:355–9. [DOI] [PubMed] [Google Scholar]
- [9].Astrup AS, Nielsen FS, Rossing P, et al. Predictors of mortality in patients with type 2 diabetes with or without diabetic nephropathy: a follow-up study. J Hypertens 2007;25:2479–85. [DOI] [PubMed] [Google Scholar]
- [10].Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 2000;321:412–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Hypertension in Diabetes Study (HDS): II. Increased risk of cardiovascular complications in hypertensive type 2 diabetic patients. J Hypertens. 1993;11:319–325. [DOI] [PubMed] [Google Scholar]
- [12].Muñoz-Durango N, Fuentes CA, Castillo AE, et al. Role of the renin-angiotensin-aldosterone system beyond blood pressure regulation: molecular and cellular mechanisms involved in end-organ damage during arterial hypertension. Int J Mol Sci 2016;17: pii: E797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002;39(2 Suppl. 1):S1–266. [PubMed] [Google Scholar]
- [14].Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–72. [DOI] [PubMed] [Google Scholar]
- [15].Maselli M, Giantin V, Franchin A, et al. Detection of blood pressure increments in active elderly individuals: the role of ambulatory blood pressure monitoring. Nutr Metab Cardiovasc Dis 2014;24:914–20. [DOI] [PubMed] [Google Scholar]
- [16].Satoh M, Asayama K, Kikuya M, et al. Long-term stroke risk due to partial white-coat or masked hypertension based on home and ambulatory blood pressure measurements: the Ohasama study. Hypertension 2016;67:48–55. [DOI] [PubMed] [Google Scholar]
- [17].Conen D, Aeschbacher S, Thijs L, et al. Age-specific differences between conventional and ambulatory daytime blood pressure values. Hypertension 2014 2014;64:1073–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Kushiro T, Kario K, Saito I, et al. Increased cardiovascular risk of treated white coat and masked hypertension in patients with diabetes and chronic kidney disease: the HONEST study. Hypertens Res 2017;40:87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Nakano S, Konishi K, Furuya K, et al. A prognostic role of mean 24-h pulse pressure level for cardiovascular events in type 2 diabetic subjects under 60 years of age. Diabetes Care 2005;28:95–100. [DOI] [PubMed] [Google Scholar]
- [20].von SBJ, Reinhard H, Hansen TW, et al. Markers of inflammation and endothelial dysfunction are associated with incident cardiovascular disease, all-cause mortality, and progression of coronary calcification in type 2 diabetic patients with microalbuminuria. J Diabetes Complications 2016;30:248–55. [DOI] [PubMed] [Google Scholar]


