Abstract
The purpose of this study is to compare the clinicopathological characteristics and outcomes of esophageal foreign body (FB) ingestion in adults between weekdays and holidays. This is a retrospective study including 1058 patients with esophageal FB ingestion from 2012 to 2016. Patient characteristics, the types and locations of FB, and clinical outcomes were compared between patients on weekdays and holidays. Furthermore, independent risk factors of complication on weekdays and holidays respectively were evaluated. The locations of FB, underlying diseases, and complications significantly differed between weekdays and holidays groups, while no difference was found in the types of FB. Patients got higher percentage of erosion complication on holidays than that on weekdays (60.8% vs 47.6%, P < .0001). Multivariate logistic regression analysis revealed that jujube shell was a significant predictor of complication on weekdays (P < .001). However, complication was significantly associated with nonfood bolus FB ingestion on holidays (P < .001). Our data suggest that there were different clinicopathological characteristics of FB ingestion between weekdays and holidays, and more patients got complications on holidays. On holidays, a latex protector hood or an overtube should be applied to patients who swallowed nonfood bolus in order to reduce esophageal mucosal damage.
Keywords: complication, esophageal, foreign body, holidays, weekdays
1. Introduction
As a common clinical problem, foreign body (FB) ingestion sometimes presents as endoscopic emergencies,[1] although the majority of ingested foreign bodies pass spontaneously without complications.[2–4] Actually, esophageal FB ingestion has a wide spectrum of clinical manifestations from minor disease that can resolve spontaneously to severe fatal diseases. About 10% to 20% of patients’ FB ingestion will require nonoperative intervention, and less than 1% of patients will require a surgical procedure.[5] Most FB ingestion occurs without identifiable contributing factors in adults, but some may be due to psychiatric disorders, mental retardation, alcohol consumption, or an edentulous state.[6] Intentionally ingested FB commonly require endoscopic treatment (63–76%) and surgery (12–16%).[7,8] An estimated 1500 people in the United States die annually from foreign bodies in the upper-gastrointestinal (GI) tract.[9] Crucially, esophageal foreign bodies should be removed within 24 hours because delayed treatment decreases the likelihood of successful removal and increases the risk of complications including risk of perforation.[10,11] Since the first report in 1972 describing the removal of FB with a flexible endoscope by McKechnie,[12] esophagogastroduodenoscopy has been a widespread and rapidly developed therapeutic technique, which has recently become the first therapeutic modality for the esophageal FB ingestion.[13] Simple radiology would be used before esophagogastroduodenoscopy in most institutions, as it allows the examination of both the pharynx and upper esophagus in patients complaining with only a “neck” FB sensation.[14] Most of foreign bodies in adults are caused by the impaction of bone components in food.[15–17] At present, the percentage of bone-type foreign bodies has been shown higher in eastern countries than in western countries.[18] Dietary customs vary depending on the region of origin, culture, and religious beliefs. Eating practices are not only a part of the habituated lives of people but also linked to cultural identity, which makes food imbued with social and cultural meaning.[19,20] Dietary change has been shown to alter the management of heart failure in older Chinese people.[21] According to Chinese dietary custom, people are happy to enjoy a hearty dinner during holidays, which may affect the occurrence of esophageal FB, but none has ever investigated the influence of dietary change on esophageal FB ingestion. In this study, we compared the type and location of foreign bodies and clinical outcomes on weekdays and holidays, and further evaluated the predictors of complication on weekdays and holidays, respectively.
2. Materials and methods
2.1. Study population selection
A retrospective study was conducted on adult patients with suspected FB ingestion in the esophagus who visited the emergency department or outpatient clinic or during hospitalization in Nanjing Drum Tower Hospital from January 2012 to January 2016. A total of 1058 patients were enrolled in this study. First, a physical examination would evaluate the patient's general condition and assess signs of any complications. Second, radiographic study of the neck, chest, and abdomen was taken to assess the presence, location, size, configuration, and number of ingested objects. Computed tomography scan was performed in selected cases in which a complication is suspected. After perforation, peritonitis or small-bowel obstruction were excluded, esophagogastroduodenoscopy would be taken to not only confirm the diagnosis but also rule out FB ingestion. A flow diagram of the strategy for inclusion in this study is shown in Fig. 1, and some typical images were presented in Fig. 2. This study had been approved by ethics committee of The Affiliated Drum Tower Hospital of Nanjing University Medical School. There is no need to obtain informed consent from patients because this is a retrospective study and all data were collected and analyzed anonymously.
Figure 1.
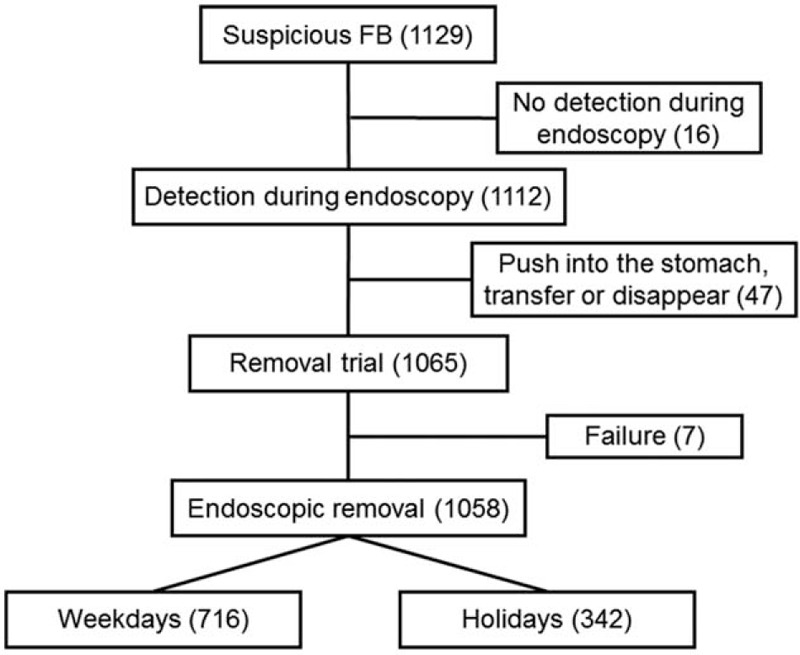
Entries and outcomes of all patients. A retrospective study was conducted on adult patients (age 15–95 years old) with suspected FB ingestion who visited the emergency department or outpatient clinic or during hospitalization in Nanjing Drum Tower Hospital from January 2012 to January 2016. During the study period, 1129 patients with suspected FB ingestion were admitted to our hospital. A total of 1058 patients who met the criteria were enrolled in the study. FB = foreign body.
Figure 2.

Illustrations of esophageal foreign bodies. (A) A denture with hook was ingested by a male patient aged 45 years on a weekday. (B) A jujube shell was ingested by a female patient aged 72 years on s holiday. (C) A bone FB was ingested by a male patient aged 52 years on a holiday. FB = foreign body.
2.2. Methods
The following clinical data were collected: demographic data, including gender, age, and date of endoscopy (date was divided into weekdays and holidays depending on the adjustment of statutory holidays in China); type of foreign bodies, including fish bone, other animal bone, jujube shell, food bolus, plastic item, metal item, and denture; location of foreign bodies, including upper esophagus (22 cm away from the upper incisor teeth), mid-esophagus (22–30 cm away from the upper incisor teeth), and lower esophagus (30 cm from the terminal of mid-esophagus to esophagogastric junction), anastomosis (postesophagus resection); underlying diseases, including associated upper GI diseases composed of esophagitis, postesophagus resection, esophageal cancer, esophageal stenosis, hiatal hernias and achalasia, and unassociated upper GI diseases composed of esophageal diverticulum, esophageal varices, and inflammation, polyps or ulcer located on cardia, stomach, and duodenum; and complications after FB removal, including erosion, perforation, ulceration, and infection, in which erosion refers to relatively mild mucosal damage with slightly bleeding.
2.3. Statistical analysis
Comparisons of continuous variables were conducted by Student t test. Categorical variables were compared using Pearson χ2 test or Fisher exact test. Multivariate logistic regression analyses were used to detect independent risk factors predicting the development of complications on weekdays. P values < .05 were considered statistically significant. Analyses were performed using SPSS software, version 22.0 (SPSS Inc., Chicago, IL).
3. Results
3.1. Characteristics and outcomes of patients on weekdays and holidays
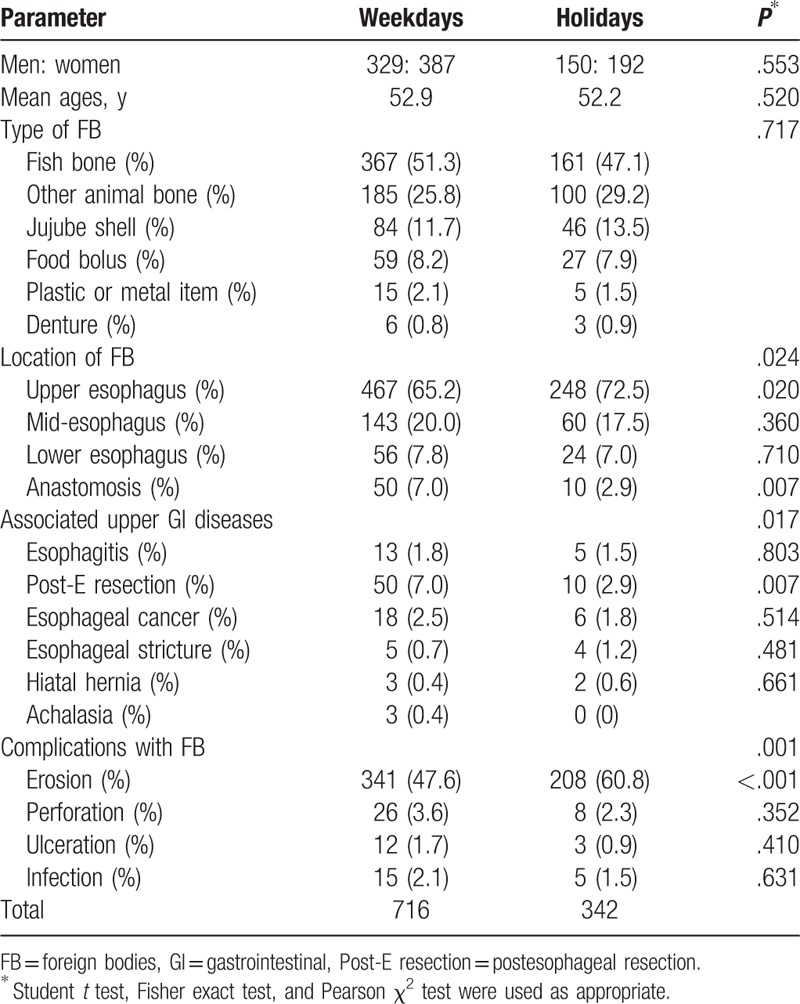
From January 2012 to January 2016, 1058 cases (716 patients on weekdays and 342 patients on holidays) occurred in 721 days including 493 weekdays and 228 holidays. Endoscopic removal was successful in 99.3% (1058/1065) of the patients, and the remaining 0.7% (7/1065) required surgery. Among the 7 patients, 3 patients were found on weekdays and 4 patients were found on holidays. The mean age was 52.9 ± 16.5 years for patients on weekdays, and 52.2 ± 16.6 years for patients on holidays. On both weekdays and holidays, the percentage of females was higher than that of males (54.1% vs 45.9% and 56.1% vs 43.9%, respectively), but age and gender distribution were not significantly different between weekdays and holidays (age: P = .553; gender: P = .520). Fish bones (51.3% on weekdays and 47.1% on holidays) and other animal bones (25.8% on weekdays and 29.2% on holidays) were the most common FB, and the proportion of jujube shell (11.7% on weekdays and 13.5% on holidays) and food bolus (8.2% on weekdays and 7.9% on holidays) ingestion is relatively low on weekdays and holidays. The types of FB were similarly distributed between weekdays and holidays groups (P = .717). The locations of FB ingestion found in esophagus were significantly different between weekdays and holidays groups (P = .024). Foreign bodies located at anastomosis were significantly more common on weekdays (7.0%) than holidays (2.9%) (P < .01), but the location of upper esophagus was more common on holidays (72.5%) than weekdays (65.2%) (P < .05) (Table 1). One hundred nineteen patients had associated upper GI diseases, including esophagitis, postesophagus resection, esophageal cancer, esophageal stricture, and so on. More patients had associated upper GI diseases on weekdays (12.8%) than holidays (7.9%) (P < .05), especially postesophagus resection (weekdays vs holidays: 7.0% vs 2.9%) (P < .01) (Table 1). Four hundred forty patients had none complications with the management of endoscopy. As the most common complication, erosion was noted in 549 cases and significantly more common on holidays (60.8%) than weekdays (47.6%) (P < .001). Distribution of the proportion of serious complications, including perforation, ulceration, and infection, was similar in the 2 groups (Table 1).
Table 1.
Characteristics and outcomes of patients in weekdays and holidays.
3.2. Risk factors predicting the development of complication
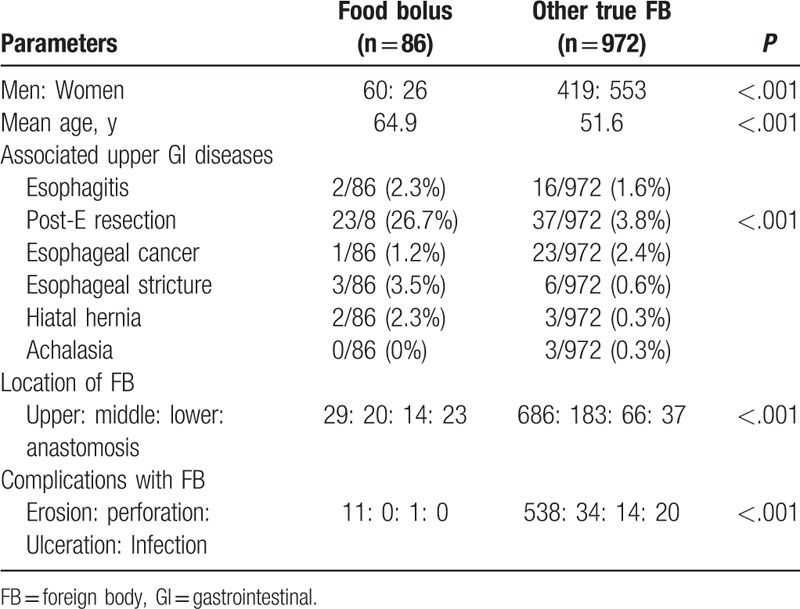
Age was not the risk factor for complications on weekdays, as well as on holidays. Type was the only risk factor related with complications of esophageal FB ingestion on holidays. Type and location of FB and associated upper GI disease were all related with complication with ingestion of FB on weekdays. However, type was the only significant risk factor of complications by multivariate logistic regression analyses on weekdays (P < .001). Patients with food bolus ingestion were less likely to get complications both on weekdays (11.9% vs 88.1%, P < .001) and holidays (18.5% vs 81.5%, P < .001). However, patients with jujube shell ingestion were likelier to get complications on weekdays (70.2% vs 29.8%, P < .01) (Tables 2 and 3). A total of 130 patients were found with esophageal jujube shell impaction. Different from nonjujube shell, patients with jujube shell impaction had higher proportion of female (76.2% vs 51.7%, P < .001), older age (58 vs 51.9, P < .001), lower proportion of postesophagus resection (1.5% vs 6.3%, P < .05), higher proportion of upper esophagus (86.2% vs 64.9%, P < .001), and more common complications (72.3% vs 56.5%, P < .01) (Table 4). There was a total of 86 patients with ingestion of food bolus and 972 patients with ingestion of nonfood bolus. Patients with ingestion of food bolus had higher proportion of male sex (69.8% vs 43.1%, P < .001) and older age (64.9 vs 51.6, P < .01) than those with ingestion of nonfood bolus. Postesophagus resection (29.0% vs. 5.4%, P < .01) and anastomosis (26.7% vs. 3.8%, P < .001) were more common in patients with ingestion of food bolus, but lower proportion of complication was found in these patients (14.0% vs 62.3%, P < .01) (Table 5).
Table 2.
Risk factors for complications with foreign bodies removal on weekdays.
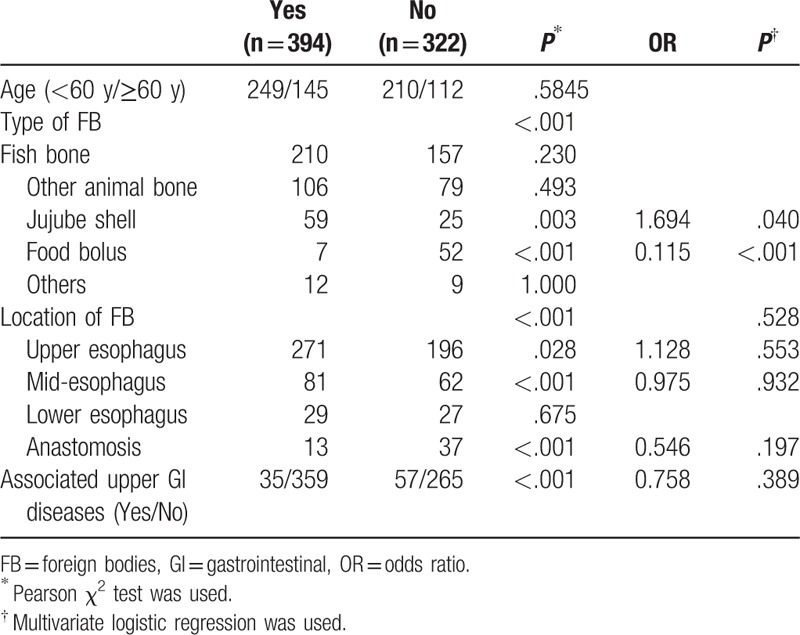
Table 3.
Risk factors for complications with foreign bodies removal on holidays.
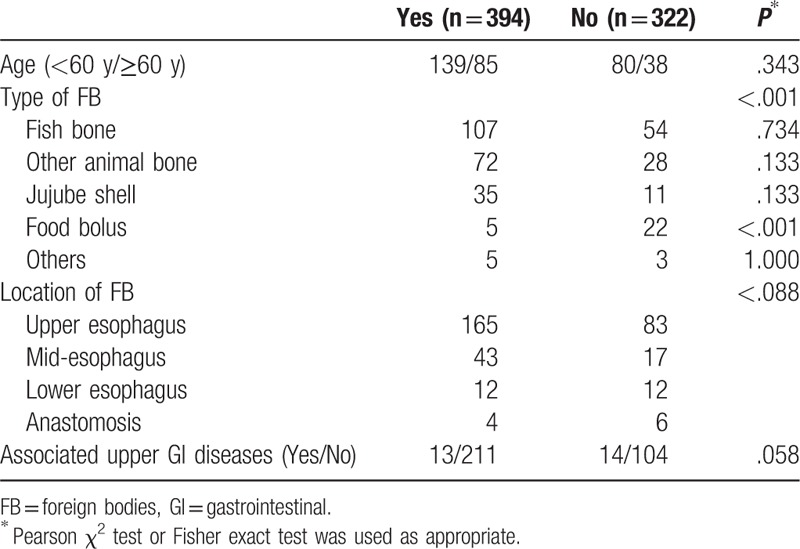
Table 4.
Comparisons of patients with esophageal jujube shell impaction or other foreign bodies.
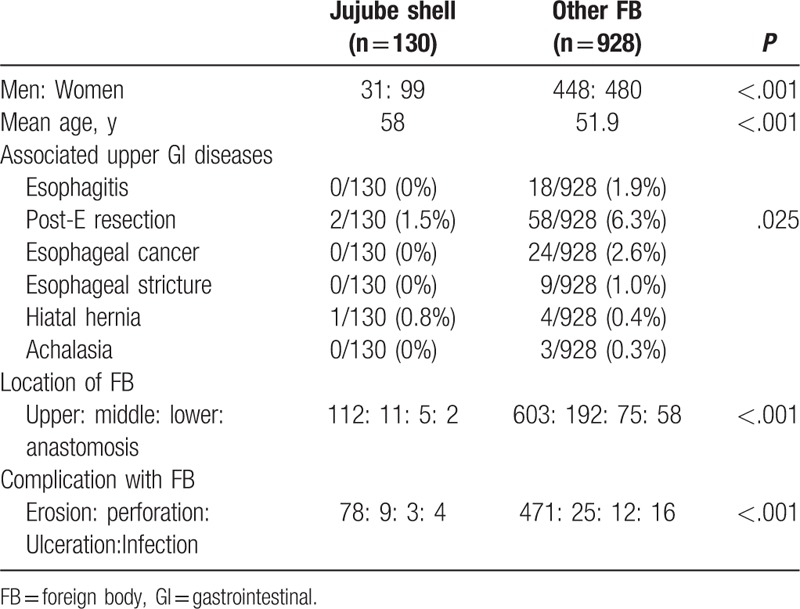
Table 5.
Comparisons of patients with esophageal food bolus impaction or other true foreign bodies.
4. Discussion
Foreign body ingestion is a commonly encountered problem in the endoscopic department around the world.[22] American Society for Gastrointestinal Endoscopy has suggested that only 10% to 20% of foreign bodies may need to be removed endoscopically, but most patients in China were treated endoscopically due to high percentage of bone-type foreign bodies and low cost of endoscopic procedures.[14,23,24] The differences of foreign bodied ingested between Chinese and Western populations may result from the difference of dietary customs, but few studies have focused on this factor. On the basis of the difference of eating habits between weekdays and holidays in China, we investigated the characteristics of FB ingestion and clinical outcomes between weekdays and holidays. Our study suggested that more patients had associated upper GI diseases on weekdays than those on holidays, especially postesophagus resection. It is noted that patients with food bolus impaction have a significant higher percentage of postesophagus resection than those with other FB ingested. This was the potential cause of FB impaction, which would pass through the GI tract in healthy people. It is recommended that patients with postesophagus resection chew slowly to avoid the food bolus blocked in the esophagus, especially on weekdays. Foreign bodies located at anastomosis were more common on weekdays than on holidays, but foreign bodies located at upper esophagus were more common on holidays than on weekdays. Sites of trapped foreign bodies may be related to 3 factors: anatomical, pathological, and the nature of FB. This, in turn, determined the tools to be used in removal: lodged foreign bodies or food impaction were grasped by forceps while in the stomach, it was easy to use the snare or to open and close the basket.[25,26]
In our study, we observed that complications of erosion were significantly more common on holidays than on weekdays. It is noted that type of FB was the only risk factor related with complications on holidays. Previous study showed that patients with esophageal food bolus impaction had significant fewer complications and higher proportions of esophageal cancer, which is consistent with our result.[27] Patients with impaction of food bolus had lower complications than those with ingestion of nonfood bolus, probably due to that food bolus is different from bone and jujube shell, which have sharp edge. In addition, we found that the type of jujube shell and nonfood bolus was, respectively, committed to complications on weekdays and holidays. In particular, patients with jujube shell ingested were more likely to be female, old, and get complications. Since the first report in 1972 on the endoscopic removal of a FB, flexible endoscopy has been the first choice for esophageal food bolus impaction with high success rate and less complications.[24] Endoscopic removal is characterized by technical facility, excellent visualization, simultaneous diagnosis of other diseases, and a low rate of morbidity.[28] European Society of Gastrointestinal Endoscopy suggests treatment of food bolus impaction in the esophagus by gently pushing the bolus into the stomach. If this procedure is not successful, retrieval should be considered and a repeat endoscopy should be carried out after extraction of foreign bodies in all patients to detect any underlying disease.[29] Nevertheless, in clinical endoscopic practice, if the risk of esophageal perforation and bleeding is high, as in those cases with sharpened or pointed foreign bodies deeply fixed into the wall, it is better to avoid any endoscopic attempts and to resort to surgery.[30] According to our study, the older women were suggested to change their eating habits or eat non-nuclear jujube. At the same time, a latex protector hood or an overtube especially should be taken for patients with ingestion of nonfood bolus in order to protect the esophageal mucosa during procedure on holidays.
In our center, the endoscopic procedure was performed in most of the patients within 24 hours, because the foreign bodies had not passed through the upper-GI tract. Some studies have shown that long duration from ingestion to endoscopy and mucosal injury were risk factors of complications of endoscopic FB removal.[31] On the contrary, Huang et al[32] have shown that longer wait times are not associated with mucosal injury or postoperative complication. Given the study participants consisted of children, which was different from other researches, more data need to be collected to support this view. However, our investigation was limited by obtaining accurate waiting time from ingestion to endoscopy. Limitations also include the absence of diameter size of ingested foreign bodied, which was identified as a risk factor predicting conversion to surgery due to inability to remove the FB endoscopically.[33] In addition, duration of endoscopic performance may influence treatment outcome, although no study has shown evidence to support this.[34]
5. Conclusion
Our study provides reference for endoscopic treatment of esophageal foreign bodies ingestion between weekdays and holidays. We suggest that patients with postoperative esophagus chew slowly to avoid the food bolus blocked in the esophagus, especially on weekdays. On holidays, a latex protector hood or an overtube should be applied to patients who swallowed nonfood bolus in order to reduce esophageal mucosal damage.
Footnotes
Abbreviations: FB = foreign body, GI = gastrointestinal, Post-E resection = postesophageal resection.
Both QZ and RJ contributed equally to this work.
Authorship: QZ, RJ, WR, and LW contributed to study conception and design; QZ, WR, and LW contributed to the acquisition of data; QZ, XF, YX, FL, and CP contributed to the analysis and interpretation of data; QZ, RJ, XZ, GX, WR, and LW contributed to the drafting or revising.
Funding/support: This study was supported by Medical Science and Technology Development Foundation of Nanjing Department of Health, No. 201402032.
The authors declare that there were no conflicts of interest in this work.
References
- [1].Ginsberg GG. Management of ingested foreign objects and food bolus impactions. Gastrointest Endosc 1995;41:33–8. [DOI] [PubMed] [Google Scholar]
- [2].Chauvin A, Viala J, Marteau P, et al. Management and endoscopic techniques for digestive foreign body and food bolus impaction. Dig Liver Dis 2013;45:529–42. [DOI] [PubMed] [Google Scholar]
- [3].Pfau PR. Removal and management of esophageal foreign bodies. Tech Gastrointest Endosc 2014;16:32–9. [Google Scholar]
- [4].Birk M, Bauerfeind P, Deprez PH, et al. Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2016;48:489–96. [DOI] [PubMed] [Google Scholar]
- [5].Eisen GM, Baron TH, Dominitz JA, et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc 2002;55:802–6. [DOI] [PubMed] [Google Scholar]
- [6].Ambe P, Weber SA, Schauer M, et al. Swallowed foreign bodies in adults. Dtsch Arztebl Int 2012;109:869–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Palta R, Sahota A, Bemarki A, et al. Foreign-body ingestion: characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest Endosc 2009;69(3 Pt 1):426–33. [DOI] [PubMed] [Google Scholar]
- [8].Weiland ST, Schurr MJ. Conservative management of ingested foreign bodies. J Gastrointest Surg 2002;6:496–500. [DOI] [PubMed] [Google Scholar]
- [9].Schwartz GF, Polsky HS. Ingested foreign bodies of the gastrointestinal tract. Am Surg 1976;42:236–8. [PubMed] [Google Scholar]
- [10].Loh KS, Tan LK, Smith JD, et al. Complications of foreign bodies in the esophagus. Otolaryngol Head Neck Surg 2000;123:613–6. [DOI] [PubMed] [Google Scholar]
- [11].Park JH, Park CH, Park JH, et al. Review of 209 cases of foreign bodies in the upper gastrointestinal tract and clinical factors for successful endoscopic removal. Korean J Gastroenterol 2004;43:226–33. [PubMed] [Google Scholar]
- [12].McKechnie JC. Gastroscopic removal of a phytobezoar. Gastroenterology 1972;62:1047–51. [PubMed] [Google Scholar]
- [13].Geraci G, Sciume C, Carlo G Di, et al. Retrospective analysis of management of ingested foreign bodies and food impactions in emergency endoscopic setting in adults. BMC Emerg Med 2016;16:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Mosca S, Manes G, Martino R, et al. Endoscopic management of foreign bodies in the upper gastrointestinal tract: report on a series of 414 adult patients. Endoscopy 2001;33:692–6. [DOI] [PubMed] [Google Scholar]
- [15].Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc 1995;41:39–51. [DOI] [PubMed] [Google Scholar]
- [16].Kim HU. Oroesophageal fish bone foreign body. Clin Endosc 2016;49:318–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Lai ATY, Chow TL, Lee DTY, et al. Risk factors predicting the development of complications after foreign body ingestion. Br J Surg 2003;90:1531–5. [DOI] [PubMed] [Google Scholar]
- [18].Reddy VM, Bennett W, Burrows SA, et al. Recurrence of food bolus impaction of the oesophagus: a retrospective observational study. Int J Surg 2011;9:464–6. [DOI] [PubMed] [Google Scholar]
- [19].Chesla CA, Chun KM, Kwan CML. Cultural and family challenges to managing type 2 diabetes in immigrant Chinese Americans. Diabetes Care 2009;32:1812–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Clark L, Vincent D, Zimmer L, et al. Cultural values and political economic contexts of diabetes among low-income Mexican Americans. J Transcult Nurs 2009;20:382–94. [DOI] [PubMed] [Google Scholar]
- [21].Rong X, Peng Y, Yu H, et al. Cultural factors influencing dietary and fluid restriction behavior: perceptions of older Chinese patients with heart failure. J Clin Nurs 2017;26:717–26. [DOI] [PubMed] [Google Scholar]
- [22].Sugawa C, Ono H, Taleb M, et al. Endoscopic management of foreign bodies in the upper gastrointestinal tract: a review. World J Gastrointest Endosc 2014;6:475–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Li Z-S, Sun Z-X, Zou D-W, et al. Endoscopic management of foreign bodies in the upper-GI tract: experience with 1088 cases in China. Gastrointest Endosc 2006;64:485–92. [DOI] [PubMed] [Google Scholar]
- [24].Longstreth GF, Longstreth KJ, Yao JF. Esophageal food impaction: epidemiology and therapy. A retrospective, observational study. Gastrointest Endosc 2001;53:193–8. [DOI] [PubMed] [Google Scholar]
- [25].Emara MH, Darwiesh EM, Refaey MM, et al. Endoscopic removal of foreign bodies from the upper gastrointestinal tract: 5-year experience. Clin Exp Gastroenterol 2014;7:249–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Chen T, Wu H-F, Shi Q, et al. Endoscopic management of impacted esophageal foreign bodies. Dis esophagus 2013;26:799–806. [DOI] [PubMed] [Google Scholar]
- [27].Wu W, Chiu C, Kuo C, et al. Endoscopic management of suspected esophageal foreign body in adults. Dis Esophagus 2011;24:131–7. [DOI] [PubMed] [Google Scholar]
- [28].Emara MH, Darwiesh EM, Refaey MM, Galal SM. Endoscopic removal of foreign bodies from the upper gastrointestinal tract: 5-year experience. Clin Exp Gastroenterol 2014;7:249–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Narra S, Al-Kawas FH. The importance of preparation and innovation in the endoscopic management of esophageal foreign bodies. Gastroenterol Hepatol (N Y)V 6 2010;795–7. [PMC free article] [PubMed] [Google Scholar]
- [30].Bekkerman M, Sachdev AH, Andrade J, et al. Endoscopic management of foreign bodies in the gastrointestinal tract: a review of the literature. Gastroenterol Res Pract 2016;2016:8520767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Park Y-K, Kim K-O, Yang J-H, et al. Factors associated with development of complications after endoscopic foreign body removal. Saudi J Gastroenterol 2013;19:230–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Huang ZJ, Guffey D, Minard CG, et al. Outcomes variability in non-emergent esophageal foreign body removal: is daytime removal better? Int J Pediatr Otorhinolaryngol 2015;79:1630–3. [DOI] [PubMed] [Google Scholar]
- [33].Bonjoch A, Echeverria P, Perez-Alvarez N, et al. Prospective study to assess progression of renal markers after interruption of tenofovir due to nephrotoxicity. Biomed Res Int 2016;2016:4380845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Hong KH, Kim YJ, Kim JH, et al. Risk factors for complications associated with upper gastrointestinal foreign bodies. World J Gastroenterol 2015;21:8125–31. [DOI] [PMC free article] [PubMed] [Google Scholar]


