Abstract
Sensorimotor timing deficits are considered central to ADHD. However, the tasks establishing timing impairments often involve interconnected processes, including low-level sensorimotor timing and higher-level executive processes such as attention. Thus the source of timing deficits in ADHD remains unclear. Low-level sensorimotor timing can be isolated from higher-level processes in a finger-tapping task that examines the motor response to unexpected shifts of metronome onsets. In this study, adults with ADHD and ADHD-like symptoms (n=25) and controls (n=26) performed two finger-tapping tasks. The first assessed tapping variability in a standard tapping task (metronome-paced and unpaced). In the other task, participants tapped along with a metronome that contained unexpected shifts (± 15, 50 ms); the timing adjustment on the tap following the shift captures pre-attentive sensorimotor timing (i.e. phase correction) and thus should be free of potential higher order confounds (e.g., attention). In the standard tapping task, as expected, the ADHD group had higher timing variability in both paced and unpaced tapping. However, in the pre-attentive task, performance did not differ between the ADHD and control groups. Together, results suggest that low-level sensorimotor timing and phase correction are largely preserved in ADHD and that some timing impairments observed in ADHD may stem from higher-level factors (such as sustained attention).
Keywords: Attention Deficit/Hyperactivity Disorder, timing, finger tapping, phase correction
1. Introduction
Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurobehavioral disorder characterized by hyperactivity, inattention, and impulsivity. While ADHD is most commonly associated with impaired cognitive and executive function, the disorder is also associated with timing abnormalities (for reviews see Noreika et al. 2013; Toplak et al. 2006). Impaired timing performance in ADHD has been observed in tasks of sensory timing (Smith et al. 2002; Toplak et al., 2003), motor timing (Valera et al. 2010; Zelaznik et al. 2012), and timing of sensorimotor integration (Ben-Pazi et al. 2006; Rubia et al. 2003). As such, timing deficits have been proposed to be central to ADHD (Castellanos and Tannock 2002; Rommelse et al. 2008).
Timing tasks typically require other cognitive processes such as sustained attention and working memory. For example, duration discrimination requires working memory. Supporting this, duration-discrimination performance is predicted by working-memory scores (Toplak et al. 2003, 2005). Working-memory scores also predict performance on finger-tapping tasks with complex (Bailey and Penhune 2010; Grahn and Schuit 2012) and isochronous rhythms (Jacoby et al., 2016). Similarly, isochronous finger tapping requires sustained attention—transient lapses of attention, as in periods of mind-wandering, are associated with more variable timing in synchronized tapping (Seli et al. 2013). Impairments in working memory, executive function, and sustained attention are well established in ADHD (Franklin et al. 2014; Willcutt et al. 2005). As such, the question remains as to whether increased timing variability in ADHD stems from purely time-related processes or from other attention, cognitive, and executive functions (Allman and Meck 2012; Toplak et al. 2006).
The influence of executive function on timing impairments in ADHD has been addressed by partialling out factors such as working memory and IQ from timing performance (Noreika et al. 2013; Rubia et al. 1999; Smith et al. 2002). When controlling for such global measures, timing deficits for ADHD groups appear to survive, suggesting that at least some timing deficit is independent of executive function (Noreika et al. 2013). Although controlling for global measures like IQ or working memory is an important step, it might not control for transient lapses in attention that would impair timing performance. Ideally, time-related processing could be assessed in a task that does not depend on attention or working memory.
Experimental paradigms have been established that separate timing from attention. Pre-attentive sensory timing can be assessed with EEG in the mismatch negativity (MMN) paradigm (Hove et al. 2014; Näätänen et al. 2007; Picton et al. 2000). In previous work, the MMN elicited by timing deviations was similar for children with attention deficit/ADHD and controls (Gomes et al. 2013; Huutunen et al. 2007; Huutunen-Scott et al. 2008) suggesting that deficits in perceptual timing might not be due to impaired sensory timing (Gomes et al. 2013; Noreika et al. 2013). In the sensorimotor domain, pre-attentive timing can be assessed in a finger-tapping task that examines the timing adjustment of a finger tap after an unexpected metronome perturbation. We used this task here to examine pre-attentive sensorimotor timing.
Synchronizing movements with a beat requires rapid adjustment of movement timing when deviations from synchrony occur. This adjustment is called phase correction and has been studied extensively in the timing literature (e.g., Jacoby et al. 2015; Madison and Merker 2004; Mates 1994; Pressing 1998; Repp 2000, 2001, 2005; Semjen et al. 1998). A common way to examine phase correction is the phase-perturbation paradigm, wherein participants synchronize their finger taps with a metronome that contains unexpected timing perturbations. An unexpected delay or advance creates an asynchrony between metronome and tap, which leads to timing adjustments on the following tap (Repp, 2001, 2005). The response to timing perturbations is called the Phase-Correction Response (PCR).
Phase correction generally occurs without awareness and is pre-attentive. For example, phase correction is similarly effective for metronome perturbations that are above and below the detection threshold (Repp 2001, 2005). For small undetectable perturbations, phase correction occurs even when participants attempt to suppress their phase correction, thus indicating that awareness and intention are not required for phase correction (Repp 2002). Repp and Keller (2004) manipulated attention by having participants perform concurrent mental arithmetic while tapping with a tempo changing metronome. The dual-task condition did not impair phase correction. Thus, the phase-correction tasks provide a method of assessing sensorimotor timing without confounding higher-level processes such as attention. To our knowledge, such a pre-attentive timing task has not been assessed in ADHD, but could help isolate and identify the source of reported timing deficits in ADHD.
In this study, adults diagnosed with ADHD or exhibiting ADHD-like symptoms (as identified with a validated ADHD symptom checklist) and controls performed two tasks. One task was a standard synchronization-continuation tapping task: participants tapped in synchrony with an isochronous metronome – the metronome then stopped and they continued tapping at that same rate unpaced. This task assessed participants’ ability to synchronize with a pacing stimulus and maintain a constant movement rhythm (involving both low-level sensorimotor timing and higher-level processes such as attention (Repp 2005; Seli et al. 2013)). The isochronous tapping task included a range of tempi (250, 500, 1000, 1500 ms inter-onset intervals (IOI)). Different time scales are mediated by partially distinct brain networks [e.g., subsecond timing is more reliant on cerebellar regions, and suprasecond timing is more reliant on prefrontal regions (Ivry 1996; Weiner et al. 2010)], and thus could potentially implicate either cerebellar or frontal neural regions previously implicated in ADHD (Hove et al. 2015; Kucyi et al. 2015; Valera et al. 2007, 2010). The other task was a phase-perturbation task in which participants tapped in synchrony with a metronome that contained occasional phase shifts (± 15, 50 ms) to create timing errors. If timing deficits in ADHD are associated with an impairment in sensorimotor timing independent of attention, we would expect to see impairments in phase correction in the ADHD group. Otherwise, intact phase correction in the ADHD group would suggest that higher-level processes contribute to the observed timing abnormalities. In sum, these experiments aimed to isolate pre-attentive sensorimotor timing from higher-level processes, and provide insights into the source and meaning of timing deficits in ADHD.
2. Material and Methods
2.1 Participants
Participants were 51 young adults who volunteered in exchange for course credit or monetary compensation. The ADHD group consisted of 25 participants (17 female, 8 male; mean age = 20.3 ± 1.0) and the non-ADHD control group consisted of 26 participants (20 female; 6 male; mean age = 20.6 ± 1.5). Participants were recruited from and participated at two public universities in Massachusetts: the University of Massachusetts-Amherst (“Site 1”) and Fitchburg State University (“Site 2”).
At Site 1, participants in the ADHD group (N = 17; 12 female, 5 male; mean age 20.2 ± 0.9) were classified as having ADHD symptoms based on the Adult ADHD Self-Report Scale (ASRS; Kessler et al. 2005). This approach has been used in previous studies (Kurdziel et al. 2015). The ASRS is a common symptom checklist that includes eighteen questions consistent with DSM-IV criteria for ADHD with response options ranging from Never (=0) to Very Often (=4). The ASRS is a valid and reliable scale for evaluating ADHD symptoms (Adler et al. 2006). The participants with ADHD or ADHD-like symptoms were identified in an online prescreening of students enrolled in psychology courses who completed questionnaires in exchange for course credit. Respondents with high symptom scores on the ASRS and who did not report other exclusion criteria (i.e., any history of neurological disease or injury or a past or current diagnosis of depression or anxiety disorder) were invited to participate. Those who enrolled in the study completed the ASRS again in the laboratory, and these scores were used to determine ADHD symptomology at the time of the experiment (ASRS total score M = 52.1; SE = 2.3). Ten of 17 participants in the ADHD group had a previous ADHD diagnosis. Fifteen non-ADHD controls (12 female, 3 male; mean age 20.7 ± 1.5) were recruited from the same participant pool and student community. The control group underwent the same experimental protocol including completing the ASRS (ASRS total M = 20.2; SE = 2.4). One additional control participant was excluded due to diagnostic uncertainty.
At Site 2, participants were recruited from Psychology classes and fliers on campus. After potential participants contacted study staff, they were asked in a prescreening email if they had a previous diagnosis of ADHD and whether they met any of the exclusion criteria. Participants in the ADHD group (N = 8; 5 female, 3 male; mean age 20.5 ± 1.2) all had a previous diagnosis of ADHD. Participants in the control group (N = 11; 8 female, 3 male; mean age = 20.5 ± 1.6) did not have a previous diagnosis. Both groups underwent the same experimental protocol including taking the ASRS at the lab (ASRS total scores: ADHD group M = 25.6; SE = 3.0; control group M = 20.1; SE = 1.8).
All participants performed the same experimental tasks. Exclusion criteria were the same for all participants (i.e., any history of neurological disease or injury, or a past or current diagnosis of depression or anxiety disorder). Participants taking psychostimulants for their ADHD symptoms were asked to refrain from taking their medication in the morning before their experiment. The study was approved by Institutional Review Boards at the University of Massachusetts-Amherst and Fitchburg State University. Participants provided written informed consent prior to participating.
2.2 Materials and Procedure
Participants performed two finger-tapping tasks: an isochronous synchronization-continuation task and a phase-correction task. Participants performed the experiment in a quiet room. Auditory sequences consisted of 40-ms long digital piano tones with a fundamental frequency of 440 Hz. Tones were presented over circumaural headphones. Participants tapped their right index finger on a Roland SPD-6 drum machine. Sequences were presented and taps were recorded using programs written in MAX/MSP (Version 6; Cycling 74). Participants initiated each trial by pressing the spacebar. The experimenter was seated out of the participant’s visual field. At Site 1, task order was fixed: participants first completed the isochronous task followed by the phase-perturbation task. At Site 2, task order was counter-balanced; analyses revealed that task order had no effect on any performance measures, thus there were no “practice” effects (p-values ranged from .2 to .8).
2.2.1 Isochronous finger tapping
Participants tapped in synchrony with an isochronous metronome presented for 40 cycles. Participants were instructed to continue tapping unpaced at the same rate for the equivalent of 40 more cycles at which time a higher-pitched tone signaled the end of the trial. The metronome was presented at one of four tempi: 250, 500, 1000, 1500 ms inter-onset interval (IOI). The order of tempi was randomized. Three trials were presented at each tempo, for 12 total trials (approximately 960 taps per participant).
2.2.2 Phase-perturbation tapping
In the phase-perturbation portion, participants tapped along with a 500 ms IOI metronome that contained occasional timing shifts. Phase-perturbation magnitudes were -50 ms, -15 ms, +15 ms, and +50 ms, where negative values denote an earlier-than-expected onset, and positive values denote a delayed onset. The small 15-ms perturbations should be subliminal and below the detection threshold, whereas the large 50-ms perturbations should be noticeable and above the detection threshold (Repp 2000). Each perturbation magnitude was presented twice per trial. Phase perturbations were presented in random order and were separated by 4–7 fixed IOI tones (resulting in approximately 56 total taps per trial). Participants completed 25 phase-perturbation trials (50 total perturbations for each perturbation magnitude).
Following the tapping tasks, participants filled out the ASRS and other questionnaires. The entire experimental session lasted approximately 1 hour.
2.3 Data Analysis
2.3.1 Isochronous tapping
Tap onsets were recorded from the drum machine. The inter-tap intervals (ITI) were calculated by subtracting each tap time from the following tap time. Taps at the beginning of each trial prior to the second metronome onset were not analyzed. Outlier ITIs stemming from doubled or missing taps were filtered out if they were shorter than 50% or longer than 175% of that trial’s target tempo. We calculated the mean and standard deviation of ITIs and the coefficient of variation (SD of ITI/ mean ITI). The coefficient of variation was the main measure of timing variability.
2.3.2 Phase-correction response (PCR)
The response to a metronome perturbation, the PCR, indexes the response to timing error (Hove, Balasubramaniam and Keller 2014; Repp 2005; Repp 2008). The PCR was calculated by subtracting the baseline metronome tempo (500 ms) from the inter-tap interval (ITI) immediately following a metronome perturbation. For example, if the ITI following a +50 ms (late) perturbation was 535, the PCR would be 35, indicating that the participant lengthened their tap by 35 ms in response to the perturbation. PCRs greater than 100 ms were filtered out. To help ensure that participants were synchronized with the metronome at the time of the shift, we only included PCRs if the tap at the shift was within 100 ms of the metronome.
For each participant, the average PCR for each magnitude was regressed onto the perturbation magnitude. The slope of this regression line gives an estimate of the error correction parameter, α (Repp 2005), and captures how much of the introduced error was corrected on the following tap (e.g., at α = .70, 70% of the introduced error is corrected on the following tap). We examined the PCR for each perturbation magnitude and the overall error-correction parameter α.
One participant (ADHD, Site 2) incorrectly performed the phase-perturbation task by tapping at twice the metronome rate, and was excluded from the phase-perturbation analyses.
2.3.3 Data reduction and statistical analysis
Participants’ scores of timing variability and phase correction were defined as an outlier if it was less than the first or greater than the third quartile by more than 1.5 * interquartile range (Tukey 1977). Eighteen of the 663 total cells (2.7%) were identified as outliers with high values (8 in the ADHD group and 10 in the control group). These extreme values were winsorized and were replaced with the next highest value for that condition, group, and site (Barnett and Lewis 1994). Tapping data at each tempo were approximately normally distributed for ADHD and control groups and Sites 1 and 2, as assessed by visual inspection of the Normal Q-Q plots. Greenhouse-Geisser corrections were applied when assumptions of sphericity were not met. Significance levels were set to p < .05. Statistical analyses were performed using SPSS 21.
In isochronous tapping, the mean inter-tap intervals and coefficients of variation for synchronization and continuation tapping were assessed in separate ANOVAs with the within-subjects factor Tempo (250, 500, 1000, 1500 ms IOI) and the between-subjects factors Site (Site 1, Site 2) and Group (ADHD, Control). The four tempi were compared in post-hoc t-tests (uncorrected). Additionally, group differences were assessed in separate two-way ANOVAs with factors Group and Site for each tempo.
For phase-perturbation tapping, PCRs were compared in an ANOVA with the within-subjects factor Perturbation Size (-50, -15, +15, +50 ms) and the between-subjects factors Site (Site 1, Site 2) and Group (ADHD, Control). The phase-correction parameter α was compared in a two-way ANOVA with factors Site and Group.
ADHD symptomatology (as measured by ASRS total symptom score) was analyzed in an ANOVA with factors Site (Site 1, Site 2) and Group (ADHD, Control); and we ran Pearson correlations between ADHD symptomology and measures of tapping variability and phase correction.
3. Results
3.1 Isochronous Tapping
3.1.1 Isochronous tapping tempo
The mean ITIs aligned well with the target tempo for both synchronization and continuation phases for the ADHD and control groups (Table 1). Mean ITIs did not differ significantly between ADHD and control groups in synchronization, F(1,47)=2.90, p = .10, or in continuation, F(1,47)=0.51, p = .48. There were no differences between sites, ps > .7. Continuation tapping displayed a fair amount of tempo dispersion especially at slow tempi as indicated by high standard errors of the mean. Therefore, we controlled for tempo by using the coefficient of variation as our index of tapping variability.
Table 1.
Mean inter-tap interval in milliseconds (± standard error of the mean) at each tempo for synchronization and continuation tapping for ADHD and control groups. Both groups tapped at the correct tempo and there were no between-group differences in mean inter-tap intervals.
| Group | 250 ms tempo | 500 ms tempo | 1000 ms tempo | 1500 ms tempo | |
|---|---|---|---|---|---|
| Synchronization | ADHD | 248.4 (1.45) | 493.8 (1.01) | 994.0 (1.83) | 1492.5 (3.16) |
| Control | 251.0 (1.34) | 497.3 (0.94) | 996.1 (1.70) | 1493.2 (2.93) | |
| Continuation | ADHD | 243.8 (2.48) | 494.2 (3.88) | 1038.3 (10.86) | 1518.1 (19.37) |
| Control | 251.7 (2.30) | 495.0 (3.60) | 1008.8 (10.05) | 1511.7 (17.94) |
3.1.2 Isochronous tapping variability
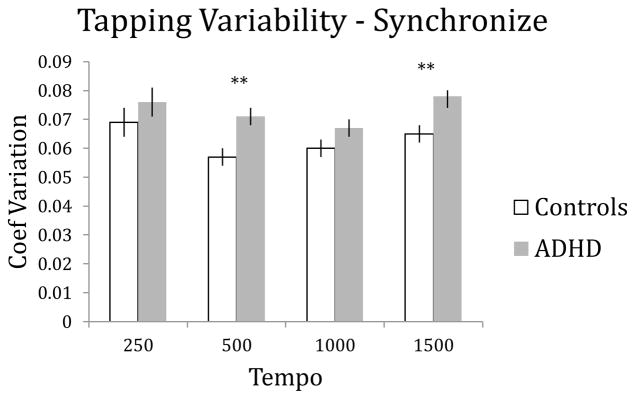
In the synchronization phase, the coefficient of variation was significantly higher for the ADHD group than the control group, as indicated by a main effect of group, F(1,47)=7.01, p = .011, ηp2 = .130. There was a main effect of Site, with lower variability at Site 1, F(1,47)=20.57, p < .001, ηp2 = .304, but importantly Site had no significant interactions (ps > .7), indicating that differences between ADHD and control groups were similar across sites. The coefficient of variation differed between tempi, as indicated by a main effect of tempo, F(2.07, 97.29)=4.66, p =.011, ηp2 = .090 – higher variability occurred at the 250 ms and 1500 ms tempi, post-hoc t-tests (uncorrected) ps < .05 (Figure 1). No interactions were significant.
Figure 1.
Tapping variability in the synchronization phase (with metronome). Error bars represent standard error, and significant differences at each tempo are denoted by **p < .01.
Separate ANOVAs at each tempo revealed that the ADHD group had significantly higher synchronized tapping variability at the 500 ms (F(1,47)=7.80, p=.008) and 1500 ms tempi (F(1,47)=7.59, p=.008), but not at the 250 ms tempo (p=.31) or 1000 ms tempo (p=.13).
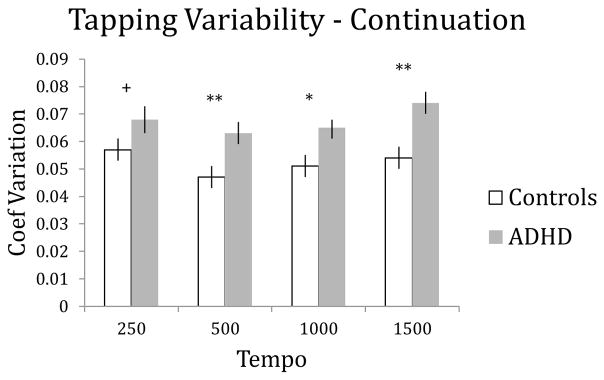
In the unpaced continuation phase, the coefficient of variation was significantly higher for the ADHD group than the control group, as indicated by a main effect of group, F(1,47)=10.37, p = .002, ηp2 = .181. There was no significant main effect of Site, F(1,47)=3.08, p = .086, and no significant interactions, again indicating that ADHD/control group differences were similar across Sites. The coefficient of variation differed between tempi, as indicated by a main effect of tempo, F(3, 141)=4.00, p =.009, ηp2 = .078 – highest variability occurred at the 250 ms and 1500 ms tempi, post-hoc t-tests (uncorrected) ps < .05 (Figure 2).
Figure 2.
Tapping variability in the unpaced continuation phase. Error bars represent standard error, and differences at each tempo are denoted by +p<.10, *p< .05, and **p < .01.
Separate ANOVAs at each tempo revealed that the ADHD group had significantly higher unpaced tapping variability at the 500 ms tempo (F(1,47)=9.76, p=.003), the 1000 ms tempo, (F(1,47)=5.47, p=.024), and the 1500 ms tempo (F(1,47)=10.44, p=.003), but did not attain significance at the 250 ms tempo (p=.095).
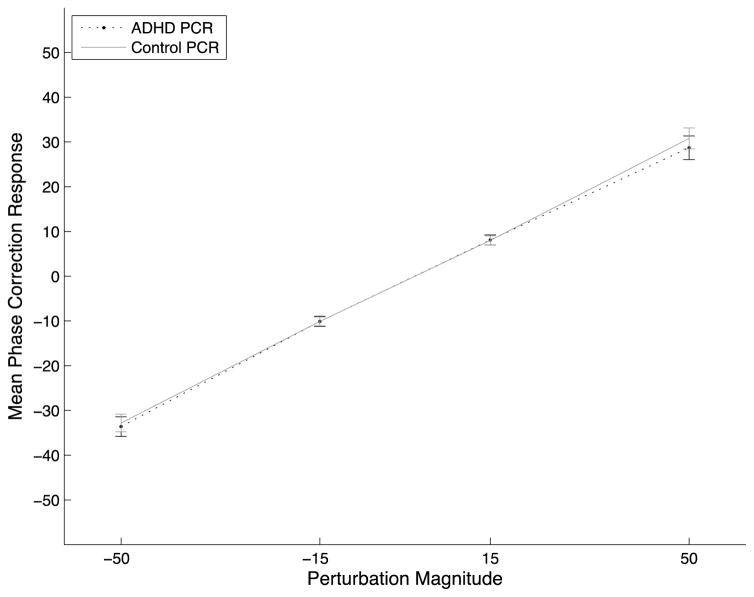
3.2 Phase-Correction Response
The phase-correction response following a perturbation did not differ between ADHD and control groups (Figure 3). The ANOVA revealed no main effect of Group on the phase-correction response at the various perturbation magnitudes, F(1,46)=1.22, p = .28, ηp2 = .026. There was no significant effect of Site (p > .7), nor any interactions (ps > .7). The phase-correction parameter α was nearly identical for both groups [αADHD = .634, αControl = .630; F(1,46)=.007, p = .94. There was no effect of Site or interaction (ps > .8)].
Figure 3.
The mean phase-correction response for each perturbation magnitude is displayed for the four perturbation magnitudes (±15, ±50 ms) for the ADHD and control groups. Error bars depict the standard error of the mean.
3.3 ADHD Sub-Group Analyses
The ADHD group contained participants with a previous ADHD diagnosis (n=18 total; 10 from Site 1, 8 from Site 2), and those without a previous diagnosis (n=7; all from Site 1). Including participants without a previous diagnosis (who were recruited based on high symptom scores) did not dilute the sample or mask results. In support of this, we re-ran all analyses excluding the ADHD participants without a previous diagnosis. The analyses comparing the ADHD participants with a diagnosis (n=18) to the control participants (n=26) yielded qualitatively unchanged effects: the ADHD group was impaired in isochronous tapping (ps < .01), but not in phase-correction (ps > .3).
Additionally, we directly compared ADHD participants from Site 1 with and without a previous diagnosis. Site 1 participants in the ADHD group with a diagnosis of ADHD (n=10) performed similarly to those without a previous diagnosis (n=7). In separate ANOVAs on tapping variability with the between-subjects factor ADHD subgroup (ADHD with diagnosis, ADHD without diagnosis), no significant difference was observed between subgroups during synchronization, F(1,15)=1.96, p = .18, or continuation tapping, F(1,15)=0.76, p = .40 (See Appendix Table A-1). For phase correction, independent samples t-tests revealed no differences between these subgroups for the overall phase correction alpha (p=.47) or for phase correction at any perturbation magnitude (ps > .3) (See Appendix Table A-2).
3.4 ADHD Symptoms and Timing
Finally, we compared ADHD symptomatology scores from the ASRS between groups in an ANOVA and examined potential relations between symptomatology scores and tapping performance with Pearson correlations.
The ANOVA revealed significantly higher ASRS scores for the ADHD group than the control group as expected, F(1,47) = 54.53, p < .001, ηp2 = .54. Additionally, a main effect of Site showed significantly higher ASRS scores at Site 1, F(1,47) = 27.51, p < .001, ηp2 = .37; and a significant interaction between Group and Site, F(1,47) = 27.06, p < .001, ηp2 = .36, indicated that the difference between ADHD and control scores was more pronounced at Site 1. These Site effects likely reflect the recruitment of subjects at Site 1 based on their high ASRS scores.
Due to the differences in ASRS scores between Sites, we ran separate correlations between ASRS scores and tapping performance for each site and group. Significant correlations only occurred in the Site 1 ADHD group: the total ASRS score correlated significantly with the coefficient of variation at the 250 ms tempo for synchronization (r(15) = .559, p = .020) and continuation (r(15) = .547, p = .023) and at the 1500 ms tempo for synchronization (r(15) = .488, p = .047) and continuation (r(15) = .700, p = .002). All other relationships between ASRS scores and tapping variability and phase-correction were not significant.
4. Discussion
We examined timing performance of adults with ADHD and controls in an isochronous tapping task and in a phase-perturbation task that assesses pre-attentive timing. This design allowed us to examine factors that contribute to increased intrasubject variability in ADHD. Despite higher tapping variability in the ADHD group in the isochronous tapping task, the phase-correction response was nearly identical for the two groups. Since the phase-correction task is pre-attentive and isolates sensorimotor timing from higher-level processes such as attention (e.g., Repp 2002, 2005; Repp & Keller 2004), our results indicate that low-level sensorimotor timing was largely intact in the ADHD group. Thus, the increased variability on timing tasks in ADHD might stem more from well-established deficits in attention rather than timing per se.
4.1 Isochronous tapping variability
Relative to controls, the ADHD group displayed higher timing variability during synchronized tapping consistent with numerous other reports examining tapping variability in ADHD (Noreika et al. 2013; Toplak et al. 2006). We also observed significant timing impairments in the ADHD group for unpaced tapping, consistent with earlier work (e.g., Valera et al. 2010; Zelaznik et al. 2012).
In the isochronous tapping task, we examined a range of sub- and supra-second tempi. Results showed that the ADHD group had higher timing variability than controls (significant or numerical trends) across all tempi (and no Group x Tempo interactions). This relative symmetry across tempi suggests that some time-invariant process contributes to the ADHD group’s observed timing variability. However participants might subdivide slow tempi and future work could discourage subdividing through dual tasks (Gilden & Marusich, 2009).
Within the ADHD group at Site 1, ADHD symptomatology correlated with tapping variability at the extreme tempi – greater ADHD symptom severity was associated with more variable tapping at the fastest (250 ms IOI) and slowest (1500 ms IOI) tempi. These extreme tempi also yielded the most variable tapping, and were most difficult as they approach the rates where stable synchronization is not possible (Repp 2005). Thus in one group, the most challenging conditions yielded worse performance in the participants with more severe symptoms.
4.2 Phase correction and pre-attentive timing
The PCR has been studied extensively in healthy controls (Hove, Balasubramaniam & Keller, 2014; Repp et al. 2001, 2004, 2005; Thaut et al. 1998), but not in individuals with ADHD. Here the ADHD group’s overall PCR (α = .634) was nearly identical to the control group’s (α = .630), and was similar to that reported in other studies (e.g., α ~ .6 at a 500 ms tempo in Repp 2008). The PCR was similar between groups for both large detectable (± 50 ms) and small subliminal perturbations (± 15 ms). Successful phase correction for small perturbations indicates that awareness and conscious strategies did not contribute to performance (Repp, 2002; Repp & Keller, 2004). Moreover, only taps that were quasi-synchronized with the metronome at the time of the perturbation (within 100ms) were analyzed, so measures of phase correction were unlikely influenced by potentially more frequent attentional lapses or greater baseline variability in the ADHD group. The current results show that pre-attentive sensorimotor timing is largely intact in this sample of adults with ADHD and ADHD-like symptoms.
The current results in pre-attentive sensorimotor timing parallel previous EEG work on pre-attentive sensory timing. Timing deviations elicited similar MMN in children with attention deficit/ADHD and controls, suggesting that ADHD deficits in duration discrimination might stem from compromised executive function or usage of temporal information, rather than impaired sensory timing (Gomes et al., 2013; Huutunen-Scott et al., 2008). Our data suggest that non-timing related processes may account for ADHD timing abnormalities in the sensorimotor domain as well.
Since timing deficits in ADHD are commonly reported in sensory, motor, and sensorimotor integration tasks, but do not readily emerge in pre-attentive timing tasks, increased timing variability might not stem from timing per se. ADHD participants exhibit greater variability in nearly all experimental tasks, so it is difficult to separate variability on timing tasks from general performance variability (Toplak et al. 2006). For example, greater reaction-time variability commonly observed in ADHD groups (Kofler et al. 2013) might stem not from systematically more variable responses across all trials, but rather from attention lapses (Hervey et al. 2006; cf. Schmiedek et al. 2007). Such attention lapses are linked to ADHD symptomatology (Franklin et al. 2014) and can impair performance on timing tasks (Seli et al. 2013). Whether impaired timing performance in ADHD can be pinpointed to attention lapses remains to be determined.
A number of potential limitations should be mentioned. Data collection took place at two sites and used slightly different recruitment strategies. At Site 1, the ADHD sample was identified from the ASRS questionnaire, whereas at Site 2, the ADHD sample consisted of interested parties with a previous ADHD diagnosis. This likely led to the higher ASRS symptom scores in the ADHD group at Site 1. The Site 1 participants also had slightly lower tapping variability during the synchronization phase, but it is unclear why. Importantly however, Site did not interact with Group on any measure of tapping performance. This indicates that the group effects (ADHD vs. Control) were stable across sites. We believe the positives of collecting data from the two sites (i.e., increased generalizability, a larger sample, and evidence against order effects) outweighs any potential negatives that might arise from possible differences between samples (e.g., in recruitment, school culture, or experimenter effects). Additionally in the Site 1 ADHD sample, only ten of seventeen reported a previous ADHD diagnosis. Notably, however, tapping performance was very similar for previously diagnosed and undiagnosed participants in the ADHD group. Nonetheless, it is possible that some participants in our ADHD group would not meet the full diagnostic criteria for ADHD, and comorbidities may exist in both the ADHD and control groups. Effects of the PCR could be hard to detect if the ADHD sample is diluted. However, the near identical PCR values between the control group and the ADHD group (both the full ADHD sample, and only those with a previous ADHD diagnosis), as well as between the ADHD subgroups suggests that the null effect here accurately captures non-impaired preattentive timing in ADHD.
Future studies that isolate various subprocesses are needed to identify the exact source of increased timing variability in ADHD. Other experimental methodologies, such as neuromodulation, manipulating distractibility and motivation, or assessing attention lapses via thought-probes, could help dissociate higher cognitive processes from timing processes and would improve our understanding of timing performance in ADHD. Timing abnormalities and cognitive and attentional impairments are reported in other neurological and developmental disorders, including Parkinson’s disease, schizophrenia, and autism (Allman & Meck, 2012;Hove & Keller, 2015). Similar methodologies could help identify the source of poor timing performance. A more complete understanding of these disorders will ultimately help inform treatment strategies.
Acknowledgments
We thank Laura Kurdziel for help recruiting participants and Heather Malone and Samantha Shorrock for help collecting data. This work was supported by grants from the National Institute of Health T32 MH16259 (to MJH) and R01 HD067744-01A1 (to EMV).
APPENDIX
Table A-1.
Coefficient of Variation (± standard error of the mean) for synchronization and continuation tapping for the Site 1 ADHD subgroups: those with a previous diagnosis (n=10) and those without a previous diagnosis (n=7).
| Group | 250 ms tempo | 500 ms tempo | 1000 ms tempo | 1500 ms tempo | |
|---|---|---|---|---|---|
| Synchronization | Diagnosed ADHD (n=10) | 0.073 (.007) | 0.068 (.006) | 0.055 (.004) | 0.074 (.006) |
| ‘ADHD-like’ (n=7) | 0.057 (.008) | 0.059 (.007) | 0.053 (.004) | 0.063 (.007) | |
| Continuation | Diagnosed ADHD (n=10) | 0.069 (.007) | 0.061 (.008) | 0.054 (.005) | 0.069 (.006) |
| ‘ADHD-like’ (n=7) | 0.056 (.009) | 0.057 (.010) | 0.055 (.006) | 0.055 (.007) |
Table A-2.
The mean phase-correction parameter alpha and the Phase-Correction Response (PCR) for each perturbation magnitude for the Site 1 ADHD subgroups. Standard error is presented in parentheses.
| Group | Phase correction alpha | PCR −50 ms perturbation | PCR −15 ms perturbation | PCR +15 ms perturbation | PCR +50 ms perturbation |
|---|---|---|---|---|---|
| Diagnosed ADHD (n=10) | 0.611 (.055) | -33.9 (2.7) | -11.4 (1.9) | 9.2 (1.7) | 30.0 (4.1) |
| ‘ADHD-like’ (n=7) | 0.669 (.053) | -37.7 (2.0) | -9.7 (2.4) | 7.8 (2.0) | 26.5 (4.8) |
References
- Adler LA, Spencer T, Faraone SV. Validity of pilot adult ADHD Self-Report Scale (ASRS) to rate adult ADHD symptoms. Ann of Clin Psychiatry. 2006;18:145–148. doi: 10.1080/10401230600801077. [DOI] [PubMed] [Google Scholar]
- Allman MJ, Meck WH. Pathophysiological distortions in time perception and timed performance. Brain. 2012;135(3):656–677. doi: 10.1093/brain/awr210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey JA, Penhune VB. Rhythm synchronization performance and auditory working memory in early-and late-trained musicians. Exp Brain Res. 2010;204(1):91–101. doi: 10.1007/s00221-010-2299-y. [DOI] [PubMed] [Google Scholar]
- Barnett V, Lewis T. Outliers in statistical data. 3. NY: Wiley; 1994. [Google Scholar]
- Ben-Pazi H, Shalev RS, Gross-Tsur V, Bergman H. Age and medication effects on rhythmic responses in ADHD: Possible oscillatory mechanisms? Neuropsychologia. 2006;44:412–416. doi: 10.1016/j.neuropsychologia.2005.05.022. [DOI] [PubMed] [Google Scholar]
- Castellanos FX, Tannock R. Neuroscience of attention-deficit/hyperactivity disorder: The search for endophenotypes. Nature Rev Neurosci. 2002;3(8):617–628. doi: 10.1038/nrn896. [DOI] [PubMed] [Google Scholar]
- Franklin MS, Mrazek MD, Anderson CL, Johnston C, Smallwood J, Kingstone A, Schooler JW. Tracking distraction the relationship between mind-wandering, meta-awareness, and ADHD symptomatology. J Atten Disord. 2014 doi: 10.1177/1087054714543494. 1087054714543494. [DOI] [PubMed] [Google Scholar]
- Gomes H, Duff M, Flores A, Halperin JM. Automatic processing of duration in children with attention-deficit/hyperactivity disorder. J Int Neuropyschol Soc. 2013;19:686–694. doi: 10.1017/S1355617713000258. [DOI] [PubMed] [Google Scholar]
- Grahn JA, Schuit D. Individual differences in rhythmic ability: Behavioral and neuroimaging investigations. PsychoMcol. 2012;22(2):105. [Google Scholar]
- Hervey AS, Epstein JN, Curry JF, Tonev S, Arnold LE, Conners CK, Hinshaw SP, Swanson JM, Hechtman L. Reaction time distribution analysis of neuropsychological performance in an ADHD sample. Child Neuropsychol. 2006;12:125–140. doi: 10.1080/09297040500499081. [DOI] [PubMed] [Google Scholar]
- Hove MJ, Balasubramaniam R, Keller PE. The time course of phase correction: A kinematic investigation of motor adjustment to timing perturbations during sensorimotor synchronization. J Exp Psychol Hum Percept Perform. 2014;40:2243–2251. doi: 10.1037/a0037826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hove MJ, Keller PE. Impaired movement timing in neurological disorders: rehabilitation and treatment strategies. Ann N Y Acad Sci. 2015;1337(1):111–117. doi: 10.1111/nyas.12615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hove MJ, Marie C, Bruce IC, Trainor LJ. Superior time perception for lower musical pitch explains why bass-ranged instruments lay down musical rhythms. Proc Natl Acad Sci U S A. 2014;111(28):10383–10388. doi: 10.1073/pnas.1402039111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hove MJ, Zeffiro TA, Biederman J, Li Z, Schmahmann J, Valera EM. Postural sway and regional cerebellar volume in adults with attention-deficit/hyperactivity disorder. NeuroImage: Clinical. 2015;8:422–428. doi: 10.1016/j.nicl.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huttunen T, Halonen A, Kaartinen J, Lyytinen H. Does mismatch negativity show differences in reading-disabled children compared to normal children and children with attention deficit? Dev Neuropsychol. 2007;31(3):453–470. doi: 10.1080/87565640701229656. [DOI] [PubMed] [Google Scholar]
- Huttunen-Scott T, Kaartinen J, Tolvanen A, Lyytinen H. Mismatch negativity (MMN) elicited by duration deviations in children with reading disorder, attention deficit or both. Int J Psychophysiol. 2008;69(1):69–77. doi: 10.1016/j.ijpsycho.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Ivry RB. The representation of temporal information in perception and motor control. Curr Opin Neurobiol. 1996;6(6):851–857. doi: 10.1016/s0959-4388(96)80037-7. [DOI] [PubMed] [Google Scholar]
- Jacoby N, Tishby N, Repp BH, Ahissar M, Keller PE. Parameter estimation of linear sensorimotor synchronization models: Phase correction, period correction, and ensemble coordination. Timing and Time Perception. 2015;3:52–87. [Google Scholar]
- Jacoby N, Tishby N, Jakoby H, Ahissar M. Individual differences and reading skills: another PATH needed?. 14th Biennial International Conference on Music Perception and Cognition (ICMPC); San Francisco, CA. 2016. Jul, Retrieved from http://www.icmpc.org/icmpc14/files/ICMPC14_Proceedings.pdf. [Google Scholar]
- Kessler RC, Adler L, Ames M, Demler O, Faraone S, Hiripi E, Howes MJ, Jin R, Secnik K, Spencer T, Ustun TB, Walters EE. The World Health Organization Adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol Med. 2005;35:245–256. doi: 10.1017/s0033291704002892. [DOI] [PubMed] [Google Scholar]
- Kofler MJ, Rapport MD, Sarver DE, Raiker JS, Orban SA, Friedman LM, Kolomeyer EG. Reaction time variability in ADHD: A meta-analytic review of 319 studies. Clin Psychol Rev. 2013;33:795–811. doi: 10.1016/j.cpr.2013.06.001. [DOI] [PubMed] [Google Scholar]
- Kucyi A, Hove MJ, Biederman J, Van Dijk KR, Valera EM. Disrupted functional connectivity of cerebellar default network areas in attention-deficit/hyperactivity disorder. Hum Brain Mapp. 2015;36(9):3373–3386. doi: 10.1002/hbm.22850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurdziel LBF, Dempsey K, Zahara M, Valera EM, Spencer RMC. Impaired visuomotor adaptation in adults with ADHD. Exp Brain Res. 2015;233:1145–1153. doi: 10.1007/s00221-014-4190-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madison G, Merker B. Human sensorimotor tracking of continuous subliminal deviations from isochrony. Neurosci Lett. 2004;370:69–73. doi: 10.1016/j.neulet.2004.07.094. [DOI] [PubMed] [Google Scholar]
- Mates J. A model of synchronization of motor acts to a stimulus sequence: I. Timing and error corrections. Biol Cybern. 1994;70:463–473. doi: 10.1007/BF00203239. [DOI] [PubMed] [Google Scholar]
- Näätänen R, Paavilainen P, Rinne T, Alho K. The mismatch negativity (MMN) in basic research of central auditory processing: A review. Clin Neurophysiol. 2007;118(12):2544–2590. doi: 10.1016/j.clinph.2007.04.026. [DOI] [PubMed] [Google Scholar]
- Noreika V, Falter CM, Rubia K. Timing deficits in attention-deficit/hyperactivity disorder (ADHD): Evidence from neurocognitive and neuroimaging studies. Neuropsychologia. 2013;51(2):235–266. doi: 10.1016/j.neuropsychologia.2012.09.036. [DOI] [PubMed] [Google Scholar]
- Picton TW, Alain C, Otten L, Ritter W, Achim A. Mismatch negativity: Different water in the same river. Audiol Neurootol. 2000;5(3–4):111–139. doi: 10.1159/000013875. [DOI] [PubMed] [Google Scholar]
- Pressing J. Error correction processes in temporal pattern production. J Math Psychol. 1998;42:63–101. doi: 10.1006/jmps.1997.1194. [DOI] [PubMed] [Google Scholar]
- Repp BH. Compensation for subliminal timing perturbations in perceptual-motor synchronization. Psychol Res. 2000;63(2):106–128. doi: 10.1007/pl00008170. [DOI] [PubMed] [Google Scholar]
- Repp BH. Phase correction, phase resetting, and phase shifts after subliminal timing perturbations in sensorimotor synchronization. J Exp Psychol Hum Percept Perform. 2001;27:600–621. [PubMed] [Google Scholar]
- Repp BH. Automaticity and voluntary control of phase correction following event onset shifts in sensorimotor synchronization. J Exp Psychol Hum Percept Perform. 2002;28(2):410–430. [PubMed] [Google Scholar]
- Repp BH. Sensorimotor synchronization: A review of the tapping literature. Psychon Bull Rev. 2005;12(6):969–992. doi: 10.3758/bf03206433. [DOI] [PubMed] [Google Scholar]
- Repp BH. Perfect phase correction in synchronization with slow auditory sequences. J Motor Behav. 2008;40:363–367. doi: 10.3200/JMBR.40.5.363-367. [DOI] [PubMed] [Google Scholar]
- Repp BH, Keller PE. Adaptation to tempo changes in sensorimotor synchronization: Effects of intention, attention, and awareness. Q J Exp Psychol-A. 2004;57(3):499–521. doi: 10.1080/02724980343000369. [DOI] [PubMed] [Google Scholar]
- Rommelse NN, Altink ME, Oosterlaan J, Beem L, Buschgens CJ, Buitelaar J, Sergeant JA. Speed, variability, and timing of motor output in ADHD: Which measures are useful for endophenotypic research? Behav Genet. 2008;38(2):121–132. doi: 10.1007/s10519-007-9186-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubia K, Taylor A, Taylor E, Sergeant JA. Synchronization, anticipation and consistency of motor timing in dimensionally defined children with attention deficit hyperactivity disorder. Percept Motor Skill. 1999;89:1237–125. doi: 10.2466/pms.1999.89.3f.1237. [DOI] [PubMed] [Google Scholar]
- Rubia K, Noorloos J, Smith A, Gunning B, Sergeant J. Motor timing deficits in community and clinical boys with hyperactive behavior: The effect of methylphenidate on motor timing. J Abnorm Child Psych. 2003;31:301–313. doi: 10.1023/a:1023233630774. [DOI] [PubMed] [Google Scholar]
- Schmiedek F, Oberauer K, Wilhelm O, Süb HM, Wittmann WW. Individual differences in components of reaction time distributions and their relations to working memory and intelligence. J Exp Psychol Gen. 2007;136:414–429. doi: 10.1037/0096-3445.136.3.414. [DOI] [PubMed] [Google Scholar]
- Seli P, Cheyne JA, Smilek D. Wandering minds and wavering rhythms: Linking mind wandering and behavioral variability. J Exp Psychol Human. 2013;39(1):1–5. doi: 10.1037/a0030954. [DOI] [PubMed] [Google Scholar]
- Semjen A, Vorberg D, Schulze HH. Getting synchronized with the metronome: Comparisons between phase and period correction. Psychol Res. 1998;61:44–55. [Google Scholar]
- Smith A, Taylor E, Warner-Rogers J, Newman S, Rubia K. Evidence of a pure time perception deficit in children with ADHD. J Child Psychol Psychiatry. 2002;43:529–542. doi: 10.1111/1469-7610.00043. [DOI] [PubMed] [Google Scholar]
- Thaut MH, Miller RA, Schauer LM. Multiple synchronization strategies in rhythmic sensorimotor tasks: Phase vs. period correction. Biol Cybern. 1998;79:241–250. doi: 10.1007/s004220050474. [DOI] [PubMed] [Google Scholar]
- Toplak ME, Rucklidge JJ, Hetherington R, John SCF, Tannock R. Time perception deficits in attention-deficit/hyperactivity disorder and comorbid reading difficulties in child and adolescent samples. J Child Psychol Psychiatry. 2003;44:888–903. doi: 10.1111/1469-7610.00173. [DOI] [PubMed] [Google Scholar]
- Toplak ME, Tannock R. Time perception: Modality and duration effects in attention-deficit/hyperactivity disorder (ADHD) J Abnorm Child Psychol. 2005;33(5):639–654. doi: 10.1007/s10802-005-6743-6. [DOI] [PubMed] [Google Scholar]
- Toplak ME, Dockstader C, Tannock R. Temporal information processing in ADHD: Findings to date and new methods. J Neurosci Methods. 2006;151(1):15–29. doi: 10.1016/j.jneumeth.2005.09.018. [DOI] [PubMed] [Google Scholar]
- Tukey J. Exploratory Data Analysis. Reading, MA: Addison-Wesley; 1977. [Google Scholar]
- Valera EM, Faraone SV, Murray K, Seidman LJ. Meta-analysis of structural imaging findings in attention-deficit/hyperactivity disorder. Biol Psychiatry. 2007;61:1361–1369. doi: 10.1016/j.biopsych.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Valera EM, Spencer RM, Zeffiro TA, Makris N, Spencer TJ, Faraone SV, Biederman J, Seidman LJ. Neural substrates of impaired sensorimotor timing in adult attention-deficit/hyperactivity disorder. Biol Psychiatry. 2010;68(4):359–367. doi: 10.1016/j.biopsych.2010.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiener M, Turkeltaub P, Coslett HB. The image of time: A voxel-wise meta analysis. Neuroimage. 2010;49(2):1728–1740. doi: 10.1016/j.neuroimage.2009.09.064. [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biol Psychiatry. 2005;57:1336–1346. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]
- Zelaznik HN, Vaughn AJ, Green JT, Smith AL, Hoza B, Linnea K. Motor timing deficits in children with attention-deficit/hyperactivity disorder. Hum Movement Sci. 2012;31(1):255–265. doi: 10.1016/j.humov.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]