Abstract
Background and Purpose: A case series review of chronic pelvic osteomyelitis treated with combined medical and surgical treatment by a multidisciplinary team.
Methods: All patients treated with surgical excision of pelvic osteomyelitis at our tertiary referral centre between 2002 and 2014 were included. All received combined care from a clinical microbiologist, an orthopaedic surgeon and a plastic surgeon. The rate of recurrent infection, wound healing problems and post-operative mortality was determined in all. Treatment failure was defined as reoperation involving further bone debridement, a requirement for the use of long-term suppressive antibiotics or sinus recurrence.
Results: Sixty-one adults (mean age 50.2 years, range 16.8-80.6) underwent surgery. According to the Cierny-Mader classification of osteomyelitis there were 19 type II, 35 type III and 7 type IV cases. The ischium was the most common site of infection. Osteomyelitis was usually the result of contiguous focus infection associated with decubitus ulcers, predominantly in patients with spinal or cerebral disorders. Most patients with positive microbiology had polymicrobial infection (52.5%). Thirty patients required soft tissue reconstruction with muscle or myocutaneous flaps.
Twelve deaths occurred a mean of 2.8 years following surgery (range 7 days-7.4 years). Excluding these deaths the mean follow-up was 4.6 years (range 1.5-12.2 years). Recurrent infection occurred in seven (11.5%) a mean of 1.5 years post-operatively (92 days - 5.3 years). After further treatment 58 cases (95.1%) were infection free at final follow-up.
Interpretation: Patients in this series have many comorbidities and risk factors for poor surgical outcome. Nevertheless, the multidisciplinary approach allows successful treatment in the majority of cases.
Keywords: Chronic osteomyelitis, pelvis, pressure ulcer, infection, surgical debridement.
Introduction
Chronic osteomyelitis is a debilitating condition which may require prolonged periods of multidisciplinary treatment to effect cure or control symptoms. In the presence of dead bone, infection cannot be successfully eradicated with antibiotics alone due to causative organisms' ability to establish a biofilm. In this glycocalyx matrix, bacteria with altered phenotype become tolerant of antimicrobials and relatively resistant to attack by the host immune system 1.
Chronic osteomyelitis of the pelvic bones is uncommon in adults but it is a very debilitating condition. Treatment of osteomyelitis affecting the pelvic bones is challenging due to the anatomic constraints of the pelvis and the high degree of comorbidity in affected patients. Several distinct aetiologies affect different groups of patients 2.
Pressure ulceration overlying the sacrum, ilium and ischium may develop osteomyelitis in the underlying bone. Spinal injury is a risk factor for pressure ulcers, with up to a third of patients affected 3, 4. These patients typically have multiple comorbidities which complicate surgical recovery 3-5.
Contiguous focus infection can also arise from intra-abdominal or pelvic sources. Osteomyelitis may occur secondary to inflammatory bowel disease 6. Instrumentation of the abdominal cavity (including urethral or suprapubic catheterisation) 7, gynaecological, colorectal or urological surgery 8-10 may be complicated by osteomyelitis. Uro-gynaecological reconstructive surgery with bone anchors has an osteomyelitis risk in the order of 0.1-2% 11, 12. Osteomyelitis may develop in areas of osteoradionecrosis following pelvic radiotherapy 13-15.
Open fracture or instrumentation of the pelvic bones may introduce infection 16, 17. Osteomyelitis may also arise from contiguous spread of septic arthritis of the native hip or sacroiliac joints, pubic symphysis, or arthroplasty infection.
Although pubic symphysis infection may occur through contiguous focus infection following abdominal surgery, it may also occur in healthy adults such as in athletes and post-partum women 12, 18. Pubic bone infection may therefore be misdiagnosed as osteitis pubis, a non-infectious condition, that tends to affect a similar demographic of young, relatively healthy individuals. Diagnosis is often delayed because osteomyelitis is not initially considered as a potential differential in those with pelvic pain and no obvious external sinus or fistula.
In adults, haematogenous osteomyelitis is unusual, and often associated with comorbid illness. It rarely affects the pelvic bones 2, 19.
In the absence of extensive osteomyelitis many patients who develop decubitus ulcers may potentially respond well to non-surgical therapy 20-24. Debridement and soft tissue flap reconstruction in selected patients, with careful attention to pre-operative optimisation and post-operative rehabilitation, can be effective and aid long-term resolution of decubitus ulcers 25. However, post-operative morbidity and ulcer recurrence is particularly high in patients with underlying osteomyelitis 26. Once there is extension to the underlying bone, with more than just cortical involvement, it is unlikely that cure will be achieved without surgery (see figure 1).
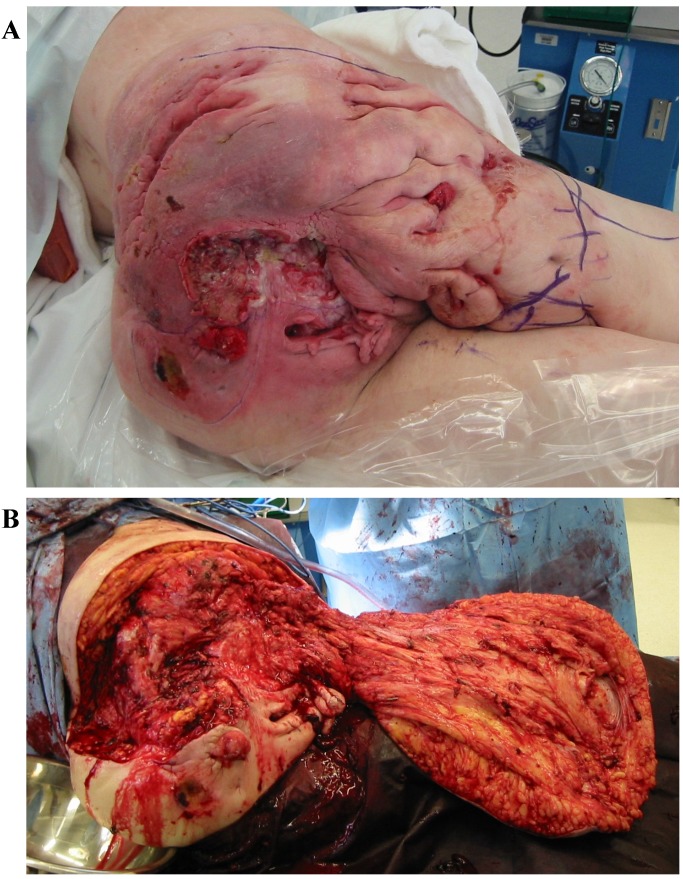
Figure 1.
Extensive osteomyelitis in a paraplegic patient with sinus drainage from the ischium, trochanteric region and sacrum.
The aims of the surgical approach to pelvic osteomyelitis are to achieve resection of all necrotic and infected tissue, to obtain clean deep tissue samples for microbiological diagnosis, to eliminate dead space and to provide well-perfused tissue cover of the pelvic bones. Avoidance of faecal and urinary soiling of the wound is critical. Reconstruction must provide a residual pelvic structure that enables comfortable sitting with good pressure distribution.
The extent and location of osteomyelitis, the condition of local soft tissues and the patient's overall health, dictate the surgical approach. In patients with a small focus of disease, limited bone debridement and direct soft tissue closure may suffice. Conversely in patients with extensive disease affecting multiple pelvic bones, with overlying decubitus ulcers that are resistant to treatment, or in those where ulceration is complicated by squamous cell carcinoma, hemipelvectomy or hemicorporectomy may be required (see figure 2). The pelvic girdle and lower limbs provide a good source of tissue grafts in these cases 5, 27-30. The 30-day mortality in patients undergoing hemicorporectomy is up to 20%, but survival for more than 20 years post-operatively has been reported 29.
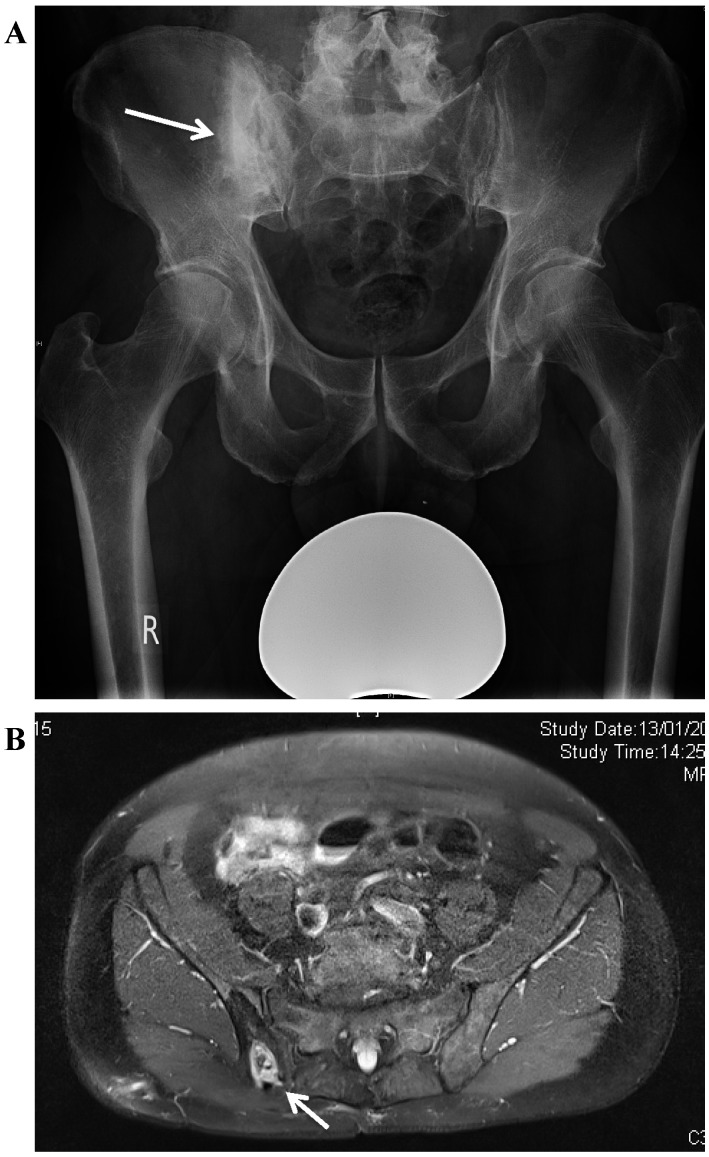
Figure 2.
A. This patient had Crohn's Disease with multiple fistulae extending from the bowel to the pelvis and right hip joint. The right sacro-iliac joint was exposed. B. The pelvic osteomyelitis was treated by radical excision including the right hemipelvis, the right hip and lower limb. The anterior thigh muscles were preserved on the healthy femoral vessels. C. The defect was directly closed using the thigh musculocutaneous flap.
Broad-spectrum empirical antibiotic treatment is often used due to the range of infecting organisms found, and frequent polymicrobial infection 27, 28. Treatment is then tailored to the organisms isolated from tissue samples. Following surgical debridement, the ideal duration of antibiotic therapy is not clear; long-term resolution may be achieved, after surgery, with short courses 25.
We describe the treatment and outcome of 61 consecutive adult patients who underwent surgical management of their pelvic osteomyelitis. To our knowledge this is the largest reported case series undergoing surgical management for confirmed chronic osteomyelitis.
Materials and Methods
Our study gained Institutional Governance Review Board approval from the Orthopaedic Governance Board at Nuffield Orthopaedic Centre. All patients who presented for surgical treatment of osteomyelitis affecting the bones of the pelvic ring between 2002 and 2014 were included. Each patient was assessed by a multidisciplinary team comprising an orthopaedic surgeon, a plastic surgeon and an infectious disease physician in a specialist unit. This assessment was supported by the input of specialist nurses, physiotherapists, occupational therapists and musculoskeletal radiologists.
A key aspect of care was the optimisation of patients before surgery. This treatment was focused on reducing comorbidities, improving nutrition, encouraging smoking cessation and drug rehabilitation, as well as optimization of the patient's psychological state. In some cases, surgery was delayed for several months to allow these issues to be addressed.
Inclusion criteria
All patients were judged to have chronic osteomyelitis, defined as having symptoms for a minimum of six months as well as clinical and radiological features accompanied by at least one of the following: positive intraoperative microbiological culture, a histology supportive of chronic osteomyelitis or the presence of a sinus, abscess or intra-operative purulence at the time of surgery.
Patients were defined as having positive cultures if two or more samples yielded the same species of organism, indistinguishable by routine laboratory identification and antimicrobial sensitivity pattern. Patients were described as having mixed microbial infection if they had positive cultures (as above) for two or more species of organism.
Data collection
Information regarding pre-operative health, peri-operative care and outpatient follow-up was obtained from notes and electronic patient records; comorbidities were recorded from hospital admission and discharge documentation. Staging of chronic osteomyelitis was classified from radiological imaging according to the Cierny-Mader staging system 31 and confirmed intra-operatively. Microbiological and histological data was obtained from the laboratory electronic database.
Patient clinical outcomes were determined by two independent reviewers, who were not involved in the treatment of patients.
Surgical management
All surgery was performed in a single stage procedure. To maximise the accuracy of causative organism identification through intra-operative sampling, all antibiotics were stopped pre operatively for a minimum of two weeks. Multiple intraoperative sterile site samples were taken for microbiological analysis (usually five) and at least one sample for histological analysis, usually including bone and periosteum. These were collected using a previously described protocol 32. Samples were not routinely cultured for mycobacteria unless clinically indicated. After sampling, broad spectrum intravenous antibiotics were given and continued until the specimen results were obtained.
A radical excision of all involved bone and soft tissue was performed back to healthy bleeding surfaces. Any bony prominences were removed to prevent later skin compromise. The area was washed with 0.05% Aqueous Chlorhexidine and the defect primarily closed, either directly or with local muscle or myocutaneous flaps.
After surgery, great care was taken to avoid pressure over the areas of surgical resection and reconstruction. Patients were nursed off the affected area for up to six weeks. Adequate pressure relieving surfaces for sitting and lying were provided, and education about position changes was undertaken, especially in patients with paraparesis 26. Multi-disciplinary care was vital in achieving wound healing without complications for these patients.
Outcome measures
Treatment failure was defined as: (a) recurrent infection with positive cultures from further radiologically guided aspiration or biopsy at the original site of infection, (b) further surgery performed at the same site for infection, (c) the use of long-term suppressive antibiotics for uncontrolled infection, or (d) recurrence of sinus formation. Secondary outcomes included the rate of wound complications in the post-operative period and the incidence of further pressure ulceration.
Statistics
Data were collected using an Excel spreadsheet (Microsoft, Redmond, Washington) and analysed using SPSS v20 (SPSS Inc. Chicago, Illinois). All data were considered to be non-parametric. Associations between categorical variables were made using Fisher's exact test on account of low cell frequencies. A p-value of < 0.05 was considered statistically significant.
Results
Case mix
61 patients with chronic osteomyelitis of the ilium, ischium, pubis or sacrum, were managed operatively between April 2002 and 2014.
32 men and 29 women were treated, with a mean age of 50.2 years (range 16.8-80.6 years).
41/61 cases in this series (67.2%) had osteomyelitis associated with pressure ulcers. 39 of these were affected by central nervous system injury or pathology causing paraparesis or tetraparesis as follows: 17 patients had traumatic spinal injury; 10 patients had spina bifida; seven patients had multiple sclerosis; three had undergone previous spinal tumour excision and two had other neurologic pathologies. Of the other two remaining cases with pressure ulcers, both developed these following a period of immobility caused by ill health; the first following surgery and radiotherapy for anal carcinoma and the second following recovery from a chest infection.
8/61 cases had osteomyelitis associated with or contiguous to intra-abdominal or pelvic organ infection; three patients had a psoas abscess, one had Crohn's disease, one had infection following cholecystectomy, and three had surgery and radiotherapy for cancer (one cervical cancer and two prostatic cancer; both had radical prostatectomy and pelvic radiotherapy, with one suffering radiation necrosis of the bowel).
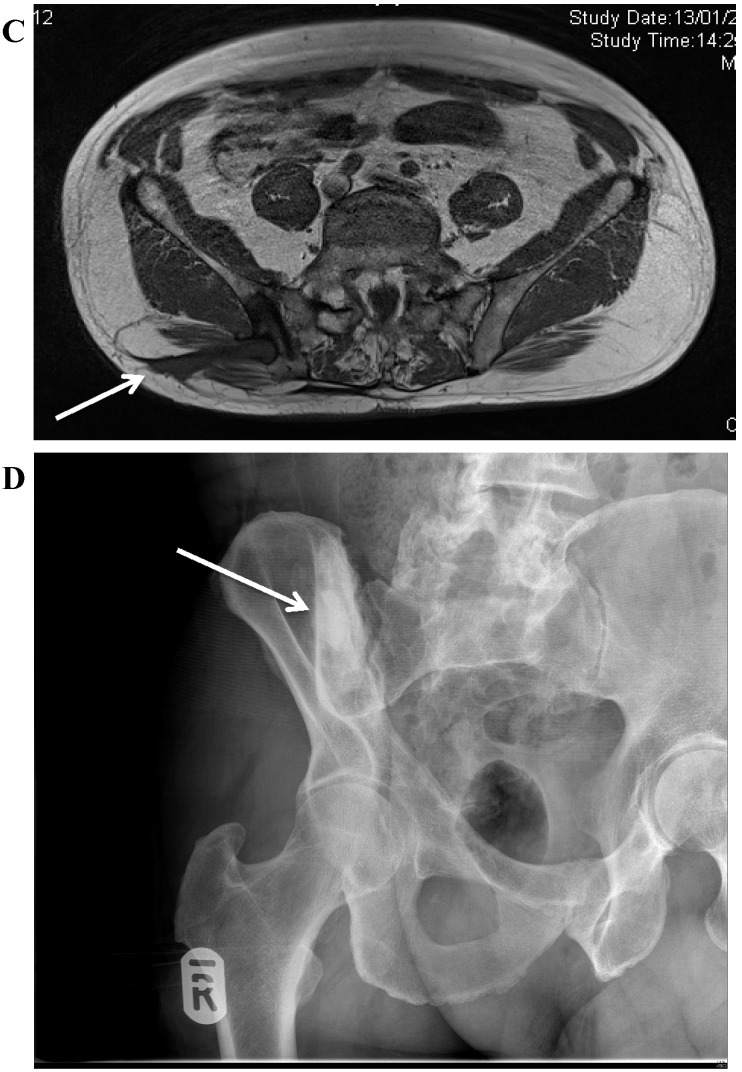
6/61 patients had infection associated with previous bone or joint surgery as follows; three patients had iliac crest bone graft donor site infection (see figure 3), two had pelvic infections following total hip replacement, and one had an infection after pelvic osteotomy for Perthes' disease.
Figure 3.
A. Osteomyelitis of the right posterior ilium after a bone graft harvest for a spinal fusion. There is a central cavity with surrounding increased bone density (involucrum). B. MRI showing the bone destruction in the ilium, with a central area of dead bone. C. MRI demonstrating the bone involvement and sinus formation to the skin of the lateral buttock. D. Postoperative radiograph showing the area of resection. The bone defect has been filled with a bioabsorbable antibiotic carrier with Gentamicin (Cerament G, Bonesupport AB, Sweden).
3/61 cases developed infection following a pelvic fracture; two patients had associated visceral injuries that caused fracture infection and the other developed a psoas abscess associated with the fracture.
3/61 patients had evidence of haematogenous infection. One patient with myelodysplasia had a previous abdominal aortic aneurysm repair complicated by bacteraemia and haematogenous infection of the ilium, another suffered sepsis following a hallux valgus correction and the third developed sepsis associated with an undiagnosed skin condition thought to be Hidradenitis Suppurativa.
Many patients had systemic disease and other factors predisposing to poor recovery. The median number of comorbidities was 2.4 per patient (range 0-6). The distribution of comorbidities is shown in Table 1.
Table 1.
Risk factors for pelvic osteomyelitis
| Significant systemic disease | Number of patients affected | |
|---|---|---|
| Previous myocardial infarction | 5 | |
| Respiratory disease | 8 | |
| Inflammatory bowel disease or bowel injury | 10 | |
| Liver disease (alcoholic cirrhosis, chronic hepatitis C) | 2 | |
| Renal disease (CKD 3-5) | 4 | |
| Malignancy | 9 | |
| Diabetes mellitus | 9 | |
| Previous arterial or venous thrombosis | 5 | |
| Central nervous system disease or injury | 40 | |
| Factors predisposing to poor wound healing | ||
| Malnutrition | 10 | |
| Obesity | 3 | |
| Smoking | 12 | |
| Use of steroids or immunosuppressants | 7 | |
| Peripheral vascular disease | 2 | |
| Pelvic radiotherapy | 4 | |
| Factors predisposing to recurrent pressure ulcers | ||
| Para- or tetra-paresis | 40 | |
| Psychiatric comorbidities | ||
| Substance misuse | 3 | |
| Depression (moderate or severe) | 3 | |
Surgical management
According to the Cierny-Mader classification; 19 patients had stage II osteomyelitis, 35 patients had stage III osteomyelitis, and seven patients had stage IV osteomyelitis.
The most common site of osteomyelitis was the ischium in 32 (52.5%) of the cases. A breakdown of the locations within the pelvic bones of the osteomyelitis resected at operation is described in Table 2.
Table 2.
Bone or joint excised or resected
| Site of bone resection | Number of patients | |
|---|---|---|
| Ischium | 32 | |
| Ilium | 9 | |
| Pubis | 2 | |
| Sacrum/coccyx | 2 | |
| Sacro-iliac joint | 3 | |
| Periacetabular | 4 | |
| Hemipelvis (SI joint to pubic symphysis) | 1 | |
| Mixed sites | 8 | |
| Sacroiliac Joint and sacrum | 2 | |
| Sacroiliac Joint and Ilium | 1 | |
| Pubis and Ischium | 2 | |
| Ischium and periacetabular region | 2 | |
| Ilium and periacetabular region | 1 | |
Thirty patients had soft tissue reconstruction with local muscle or myocutaneous flaps; in 15/30 we used gluteal muscle flaps, in 11/30 we used the hamstring muscles, in 2/30 we used quadriceps and in 2/30 the gracilis muscle.
Local antibiotic carriers were used in 16 cases; 10/16 had biodegradeable antibiotic carriers and 6/16 had gentamicin containing polymethylmethacrylate beads.
Microbiology results
The distribution of cultured organisms is shown in Table 3. Twenty-one patients had a single organism isolated and eight patients had no significant microbiological isolates, but had either positive histology or intraoperative pus. Thirty-two patients (52.5%) had mixed cultures with an average of 3.1 different organisms isolated in each case. The breakdown of these polymicrobial infections can be seen in Table 4.
Table 3.
Breakdown of organisms cultured
| Organism | Total | Pressure Ulcer | Intra-abdominal or pelvic organ infection | Previous bone or joint surgery | Fracture | Haematogenous |
|---|---|---|---|---|---|---|
| Total | 61 | 41 | 8 | 6 | 3 | 3 |
| Polymicrobial | 32 (52.5%) | 26 | 3 | 1 | 1 | 1 |
| No Growth | 8 (13.1%) | 2 | 3 | 2 | 1 | |
| Monomicrobial | 21 (34.4%) | |||||
| Staphylococci | 10 (16.4%) | |||||
| MSSA | 5 of 10 (8.2%) | 3 | 1 | 1 | ||
| CoNS | 3 of 10 (4.9%) | 1 | 1 | 1 | ||
| MRSA | 2 of 10 (3.3%) | 1 | 1 | |||
| Streptococci | 2 (3.3%) | 2 | ||||
| Diphtheroids | 2 (3.3%) | 2 | ||||
| Enterobacteriaceae | 4 (6.6%) | |||||
| Proteus spp | 3 of 4 (4.9%) | 3 | ||||
| Klebsiella spp | 1 of 4 (1.6%) | 1 | ||||
| Pseudomonas spp | 1 (1.6%) | 1 | ||||
| Anaerobes | 2 (1.6%) | 2 | ||||
MSSA- Methicillin Sensitive Staphylococcus aureus, CoNS = Coagulase negative Staphylococci, MRSA= Methicillin Resistant Staphylococcus aureus
Table 4.
Breakdown of the organisms cultured in the 32 cases with polymicrobial infection
| Organism | Number of polymicrobial cases with cultured organism |
|---|---|
| MSSA | 10 |
| CoNS | 18 |
| MRSA | 4 |
| Streptococci | 22 |
| Streptococcus milleri | 7 of 22 |
| Enterococci | 5 |
| Diphtheroids | 11 |
| Enterobacteriaceae | 16 |
| Escherichia coli | 7 of 16 |
| Proteus spp | 3 of 16 |
| Klebsiella spp | 1 of 16 |
| Other Enterobacteriaceae | 5 of 16 |
| Anaerobes | 7 |
| Pseudomonas spp | 2 |
| Propionibacterium spp | 2 |
| HACEK group | 1 |
| Candida spp. | 1 |
MSSA- Methicillin Sensitive Staphylococcus aureus, CoNS = Coagulase negative Staphylococci, MRSA= Methicillin Resistant Staphylococcus aureus
The mean total duration of post-operative antimicrobial therapy given in those that survived the first 90 days following surgery was 8.8 weeks (range 2-26 weeks).
Of the 53 cases with positive microbiology cultures, six (11.3%) had MRSA monomicrobial or polymicrobial infection. A further six (11.3%) had monomicrobial or polymicrobial infection involving Gram negative organisms with extended-spectrum beta-lactamases (ESBL) or an AmpC beta-lactamase. There were no patients who had vancomycin-resistant Enterococci.
Follow-up
There were 12 deaths occurring at a mean of 2.8 years following surgery (range 7 days-7.4 years). Excluding these deaths the mean follow up was 4.6 years (range 1.5-12.2 years). There were no intraoperative deaths. One patient died within seven days of initial operation, from a cerebrovascular event. There were no other post-operative deaths within the first 90 days. In two of the patients who died, squamous cell carcinoma associated with long standing sinus tracts was discovered on intraoperative histology (see Figure 4). The other deaths were not related to the osteomyelitis, the surgery or the antimicrobial therapy.
Figure 4.
Patient with a longstanding pressure ulcer over the left ischium. At operation, this was found to have developed a squamous carcinoma.
Infection recurrence
There were seven cases with recurrence occurring at a mean of 1.5 years post index procedure (range 92 days to 5.3 years). Table 5 shows a breakdown of these cases. 6/7 patients required a further osteomyelitis excision procedure for their infection recurrence and one individual required long-term suppression with antibiotics. There was no association between the use of a flap for reconstruction and patient outcome (p=0.25).
Table 5.
Breakdown of the details of the infection recurrence group
| Case | Site | Aetiology | C-M Stage | Initial Surgery | Days to recurrence | Initial Microbiology | Recurrent microbiology | Presentation of recurrence | Subsequent intervention | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Ilium | Residual infection after Girdlestone excision arthroplasty | III A | Partial iliectomy | 92 | No growth | No growth | Recurrent sinus | Restarted antibiotics for 6 months | Well at final follow up |
| 2 | Ilium | T6 traumatic paraplegia with bilateral pelvic & femoral head osteomyelitis | III BL | Right Hemipelvectomy and excision of proximal femur | 193 | Enterococcus, E. coli & Proteus mirabilis | Enterococci | Recurrent ulceration | Excision bilateral ischial pressure sores and cover with bilateral posterior thigh flaps. Defunctioning stoma to aid perineal wound healing | Well at final follow up |
| 3 | Ischium | Perineal sinus and purulent anal discharge Prostate cancer treated with radical cystoproctectomy, ileal conduit. Lat dorsi reconstruction and radiotherapy |
III BL | Partial excision of ischium and pubic ramus | 209 | Streptococcus milleri & CoNS |
E.coli, CoNS, Pseudomonas
(resistant to ciprofloxacin) |
Discharge from pubic symphysis region and scrotal swelling | Excision of osteomyelitis from right and left ischium, drainage of pelvic abscess in left hemipelvis, bilateral local gracilis flap | Well at final follow up |
| 4 | Ischium | Paraplegia following spinal desmoid tumour excision with pressure sore Diabetes |
II BLS | Partial ischiectomy and posterior thigh fasciocutaneous flap | 301 | Corynebacterium spp & Staphylococcus lugdenesis | No growth | Sinus developed in labia majora. MRI showed communication with ischium | Ischiectomy and hamstring advancement | Well at final follow up |
| 5 | Ischium | T10 traumatic paraplegia with sacral and ischial pressure sores | II BLS | 539 | No growth | No growth | Developed bilateral pressure sores | Required staged excision of the proximal femur bilaterally with local muscle flap | No recurrence at operative site but has developed infection in L5 fusion instrumentation. Now requiring removal of instrumentation | |
| 6 | Hemipelvectomy | Spina bifida with sacral and ischial pressure ulcers Urostomy |
IV BLS | Hemipelvectomy | 575 | Diphtheroids | Not available | Recurrent sinus over right hip. Large inflammatory mass over iliac remnant. Not excised due to technical challenge of reoperation | Treated with long-term antimicrobial course. Had soft tissue excision of sinus 2 years after index procedure and did well thereafter | Died of Hodgkin's lymphoma |
| 7 | Ischium | Traumatic paraplegia with pressure sore Ankylosing Spondylitis and Crohn's disease |
II BLS | Partial ischiectomy | 1917 | CoNS, Coliforms & Enterococci | No growth | Recurrent sinus | Ischiectomy and glut max rotational flap | Well at final follow up |
5/7 patients who had recurrence were affected by decubitus ulcers. However, having sensory loss was not shown to increase the risk of recurrence compared to those with intact neurology. There was also no statistically significant increased risk of recurrence in those with either polymicrobial infection (p=1.00) or no growth (p=0.23) from sterile site cultures at index procedure.
After further treatment 58 of the 61 cases (95.1%) were infection free at final follow. Taking into account the 12 deaths during follow up the mean follow up was 4.25 years (range 7 days - 12.2 years).
Secondary outcome measures
Excluding the seven cases who had osteomyelitis recurrence there were a further eight patients who had wound healing problems. In 3/8 the wound breakdown healed with conservative management, in 1/8 cases there was evidence of cellulitis of the wound that settled within the first 10 days after surgery. In the remaining 4/8 the wound dehiscence required further surgery. In two the wound was resutured and in another a flap was required. The last case requiring surgery for wound breakdown was subsequently shown to have a squamous cell carcinoma on histology. This was treated with a hemipelvectomy but unfortunately metastatic disease developed, with involvement of distant lymph nodes. This lady received palliative radiotherapy and subsequently died 2.9 years after index procedure.
One case in this series developed a residual collection at the operation site that was due to a seroma. This was treated conservatively and eventually resolved over several months with no evidence of recurrent infection.
Three additional patients experienced general complications of treatment - one patient developed post-operative bacteraemic sepsis, one developed pneumonia, and the other developed line-related infection associated with a PICC used to administer intravenous antibiotics at home. All made a full recovery.
Twelve cases subsequently developed pressure sores at different sites to their index operation. Of these 12 cases, eight underwent further surgery and four were treated non-operatively.
Discussion
Previous cohort studies of patients with pelvic osteomyelitis have been small, or focused on the outcome after one type of surgical procedure 27-29. We report 61 consecutive patients treated for osteomyelitis of the pelvic bones and sacrum in a tertiary referral centre.
In our cohort, three patients (5.9%) had haematogenous osteomyelitis of the pelvis. One of these patients was affected as a complication of haemodialysis, similar to a previously-described case 19. All patients with haematogenous osteomyelitis in this group had successful treatment; this may suggest that haematogenous pelvic osteomyelitis has a better prognosis than that associated with decubitus ulcers or other contiguous foci. What is surprising in this cohort is that aetiology of the osteomyelitis (e.g. haematogenous versus contiguous focus) did not seem to predict the type of microbiology that was encountered.
Pelvic osteomyelitis is commonly polymicrobial; in our cohort we applied a strict definition of positive diagnosis of osteomyelitis on microbiological culture, and it is likely that the definition of 'positive culture' used in the analysis underestimates the diversity of organisms causing infection in each patient. There were on average 3.1 different organisms cultured in each of the polymicrobial group. Furthermore 12 of the 61 cases (19.7%) had cultures that included multi-drug resistant organisms, such as MRSA, ESBL or AmpC producing Enterobacteriaceae. This underlines the importance of involving infection specialists early in these complex cases.
In our cohort, the majority of patients required limited bony resection; only one patient was treated with hemipelvectomy initially. Another patient went on to undergo hemipelvectomy following failed initial resection for squamous cell carcinoma. Both these cases died during follow up. Other studies have found significant post-operative morbidity and mortality following hemipelvectomy 5,27. Limited bony resection was successful even in the majority of patients with persistent decubitus ulcers, supporting its use as a first-line surgical strategy in patients with anatomically limited disease.
Pelvic osteomyelitis is a relatively rare disease and the relatively small cohort of patients in this study limited our ability to perform statistical analysis for the sub-groups. Consequently it has not been possible perform risk factor analysis for failure. We also accept that this group contains a heterogeneous group of aetiologies leading to pelvic osteomyelitis. Patients with pressure ulceration are not the same as those with osteomyelitis secondary to pelvic fracture, haematogenous spread or those who develop osteomyelitis related to a pelvic organ infection. Although there are unique issues related to the various locations of infection and aetiologies encountered, once osteomyelitis becomes established many of the management principles for treating bone infection are common to all cases. The large variation in aetiologies encountered in pelvic osteomyelitis and the associated comorbidities does underline the importance of extensive multi-disciplinary working.
While the outcomes in this complex group of patients is encouraging, our experience demonstrates the complex nature of the condition. Treatment requires careful planning of surgery and postoperative care before treatment begins. These patients consume an enormous amount of nursing care and rehabilitation from therapists in the months after surgery.
Two patients in the cohort developed squamous cell carcinoma associated with chronic ulceration. This is a complication that must be recognised in patients who have long-standing ulcers 3. It has been reported that the average time from ulceration to malignant change may be up to 30 years and that high-grade carcinomas will usually present with metastases 33. It is possible that earlier diagnosis or treatment could have reduced the risk of metastasis and improved the life expectancy of these patients 34.
We describe a cohort where resection of pelvic osteomyelitis in patients with significant comorbidity achieved infection resolution in a high proportion of patients, with less than 2% perioperative mortality. We advocate a multi-disciplinary approach to assessment, with meticulous pre-operative preparation, surgery and post-operative care.
Acknowledgments
The authors would like to thank Dr Bernadette Young for her assistance with the microbiology analysis.
Author contributions
McNally M Atkins B and Stubbs D contributed to study conception and design; Dudareva M, Ferguson J, Riley N contributed to data acquisition, data analysis and interpretation, Dudareva M and Ferguson J contributed to writing of article; McNally M, Atkins B, Riley N, Stubbs D contributed to editing, reviewing and final approval of article.
Institutional Review Board Statement
This study was part of our hospitals normal service evaluation process and did not require formal ethical approval.
Informed consent statement
Informed consent was gained for the use of all imaging and medical illustrations used in this article.
References
- 1.McNally M, Nagarajah K. Osteomyelitis. Orthop Trauma. 2010;24(6):416–29. [Google Scholar]
- 2.Waldvogel FA, Medoff G, Swartz MN. Osteomyelitis: A review of clinical features, therapeutic considerations and unusual aspects. N Engl J Med. 1970;282(4):198–206. doi: 10.1056/NEJM197001222820406. [DOI] [PubMed] [Google Scholar]
- 3.Grey JE, Harding KG, Enoch S. Pressure ulcers. British Medical Journal. 2006;7539:472–5. doi: 10.1136/bmj.332.7539.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fuhrer MJ, Garber SL, Rintala DH, Clearman R, Hart KA. Pressure ulcers in community-resident persons with spinal cord injury: Prevalence and risk factors. Archives of Physical Medicine and Rehabilitation. 1993;74(11):1172–7. [PubMed] [Google Scholar]
- 5.Chan JWH, Virgo KS, Johnson FE. Hemipelvectomy for severe decubitus ulcers in patients with previous spinal cord injury. The American Journal of Surgery. 2003;185(1):69–73. doi: 10.1016/s0002-9610(02)01123-6. [DOI] [PubMed] [Google Scholar]
- 6.Chandler JT, Riddle CD. Osteomyelitis associated with Crohn's disease: A case report and literature review. Orthopedics. 1989;12(2):285–8. doi: 10.3928/0147-7447-19890201-12. [DOI] [PubMed] [Google Scholar]
- 7.Stern JA, Clemens JQ. Osteomyelitis of the pubis: A complication of a chronic indwelling catheter. Urology. 2003;61(2):462. doi: 10.1016/s0090-4295(02)02140-4. [DOI] [PubMed] [Google Scholar]
- 8.Collins SA, Tulikangas PK, LaSala CA, Lind LR. Complex sacral abscess 8 years after abdominal sacral colpopexy. Obstetrics & Gynecology. 2011;118(Part 2):451–4. doi: 10.1097/AOG.0b013e3182234e7c. [DOI] [PubMed] [Google Scholar]
- 9.Taylor WE, Wolff BG, Pemberton JH, Yaszemski MJ. Sacral osteomyelitis after ileal pouch-anal anastomosis: Report of four cases. Diseases of the Colon & Rectum. 2006;49(6):913–8. doi: 10.1007/s10350-006-0524-3. [DOI] [PubMed] [Google Scholar]
- 10.Andonian S, Rabah DM, Aprikian AG. Pseudomonas aeruginosa sacroiliitis and osteomyelitis of pelvic bones after radical prostatectomy. Urology. 2002;60(4):698. doi: 10.1016/s0090-4295(02)01862-9. [DOI] [PubMed] [Google Scholar]
- 11.Frederick RW, Carey JM, Leach GE. Osseous complications after transvaginal bone anchor fixation in female pelvic reconstructive surgery: Report from single largest prospective series and literature review. Urology. 2004;64(4):669–74. doi: 10.1016/j.urology.2004.04.051. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg RP, Tchetgen MB, Sand PK, Koduri S, Rackley R, Appell R, Culligan PJ. Incidence of pubic osteomyelitis after bladder neck suspension using bone anchors. Urology. 2004;63(4):704–8. doi: 10.1016/j.urology.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 13.Minassian AM, Atkins BL, Mansour R, Byren I, Stubbs D, Ramsden A. et al. Chronic osteomyelitis of the pubic bones following radiotherapy for urological malignancy. Journal of Clinical Urology. 2017;10(3):213–9. [Google Scholar]
- 14.Moore DC, Keegan KA, Resnick MJ, Eisenberg R, Holt GE, Cookson MS. A 57-year-old man with a history of prostatectomy and pelvic irradiation presents with recurrent urinary tract infections, hematuria, and pelvic pain. Urology. 2013;81(2):221–5. doi: 10.1016/j.urology.2012.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Micha JP, Goldstein BH, Rettenmaier MA, Caillouette JT, Fee MJ, Brown JV. Pelvic radiation necrosis and osteomyelitis following chemoradiation for advanced stage vulvar and cervical carcinoma. Gynecologic Oncology. 2006;101(2):349–52. doi: 10.1016/j.ygyno.2005.12.007. [DOI] [PubMed] [Google Scholar]
- 16.Brenneman FD, Katyal D, Boulanger BR, Tile M, Redelmeier DA. Long-term outcomes in open pelvic fractures. Journal of Trauma and Acute Care Surgery. 1997;42(5):773–7. doi: 10.1097/00005373-199705000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Stewart MC, Little RE, Highland TR. Osteomyelitis of the ilium secondary to external pelvic fixation. Journal of Trauma and Acute Care Surgery. 1986;26(3):284–6. doi: 10.1097/00005373-198603000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Ross JJ, Hu LT. Septic arthritis of the pubic symphysis: Review of 100 cases. Medicine. 2003;82(5):340–5. doi: 10.1097/01.md.0000091180.93122.1c. [DOI] [PubMed] [Google Scholar]
- 19.Patzkowski JC, Hurst FP, Neff RT, Abbott KC. Hemipelvic osteomyelitis in a hemodialysis patient associated with methicillin-resistant staphylococcus aureus bacteremia. International Journal of Nephrology and Renovascular Disease. 2008;1:1–4. doi: 10.2147/ijnrd.s3917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thornhill-Joynes M, Gonzales F, Stewart CA, Kanel GC, Lee GC, Capen DA. et al. Osteomyelitis associated with pressure ulcers. Arch Phys Med Rehabil. 1986;67(5):314–8. [PubMed] [Google Scholar]
- 21.Lewis VL, Bailey MH, Pulawski G, Kind G, Bashioum MD, Hendrix RW. The diagnosis of osteomyelitis in patients with pressure sores. Plastic and Reconstructive Surgery. 1988;81:229–32. doi: 10.1097/00006534-198802000-00016. [DOI] [PubMed] [Google Scholar]
- 22.Türk EE, Tsokos M, Delling G. Autopsy-based assessment of extent and type of osteomyelitis in advanced-grade sacral decubitus ulcers: A histopathologic study. Archives of Pathology & Laboratory Medicine. 2003;127(12):1599–602. doi: 10.5858/2003-127-1599-AAOEAT. [DOI] [PubMed] [Google Scholar]
- 23.Reddy M. Pressure ulcers. BMJ Clin Evid. 2011;2011:1901. [PMC free article] [PubMed] [Google Scholar]
- 24.McInnes E, Jammali-Blasi A, Bell-Syer SE, Dumville JC, Cullum N. Support surfaces for pressure ulcer prevention. Cochrane Database Syst Rev; 2011. p. 4. DOI: 10.1002/14651858.CD001735.pub4. [DOI] [PubMed] [Google Scholar]
- 25.Mathes SJ, Feng LJ, Hunt TK. Coverage of the infected wound. Annals of Surgery. 1983;198(4):420–8. doi: 10.1097/00000658-198310000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tchanque-Fossuo CN, Kuzon Jr WM. An evidence-based approach to pressure sores. Plastic and Reconstructive Surgery. 2011;127(2):932–9. doi: 10.1097/PRS.0b013e3182046a02. [DOI] [PubMed] [Google Scholar]
- 27.Ziran BH, Smith WR, Rao N. Hemipelvic amputations for recalcitrant pelvic osteomyelitis. Injury. 2008;39(4):411–8. doi: 10.1016/j.injury.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 28.Ramaesh R, Gaston MS, Simpson AH. Chronic osteomyelitis of the pelvis. Acta Orthop Belg. 2013;79:280–6. [PubMed] [Google Scholar]
- 29.Janis JE, Ahmad J, Lemmon JA, Barnett Jr CC, Morrill KC, McClelland RN. A 25-year experience with hemicorporectomy for terminal pelvic osteomyelitis. Plastic and Reconstructive Surgery. 2009;124(4):1165–76. doi: 10.1097/PRS.0b013e3181b61169. [DOI] [PubMed] [Google Scholar]
- 30.Peterson R, Sardi A. Hemicorporectomy for chronic pressure ulcer carcinoma: 7 years of follow-up. The American Surgeon. 2004;70(6):507–11. [PubMed] [Google Scholar]
- 31.Cierny G, Mader JT, Penninck JJ. The classic: A clinical staging system for adult osteomyelitis. Clin Orthop Relat Res. 2003;414:7–24. doi: 10.1097/01.blo.0000088564.81746.62. [DOI] [PubMed] [Google Scholar]
- 32.Sheehy SH, Atkins BA, Bejon P, Byren I, Wyllie D, Athanasou NA. et al. The microbiology of chronic osteomyelitis: Prevalence of resistance to common empirical anti-microbial regimens. Journal of Infection. 2010;60(5):338–43. doi: 10.1016/j.jinf.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 33.Esther RJ, Lamps L, Schwartz HS. Marjolin ulcers: Secondary carcinomas in chronic wounds. Journal of the Southern Orthopaedic Association. 1998;8(3):181–7. [PubMed] [Google Scholar]
- 34.Lack W, McKinley T. Marjolin's ulcer: Incidental diagnosis of squamous cell carcinoma on hemipelvectomy for recalcitrant pelvic osteomyelitis. The Iowa Orthopaedic Journal. 2010;30:174–6. [PMC free article] [PubMed] [Google Scholar]