Abstract
M2-like polarized tumor-associated macrophages (TAMs) play a pivotal role in promoting cancer cell growth, invasion, metastasis and angiogenesis. The identification of M2-like TAMs during tumor progression is an attractive approach for cancer therapy. In this study, we investigated the relevance of macrophage polarization and the antitumor effect of gefitinib in Lewis Lung cancer (LLC) in vitro and in vivo. Gefitinib at a concentration below 2.5 μmol/L did not cause significant growth inhibition on LLC and RAW 264.7 cell lines and bone marrow-derived macrophage (BMDMs). However, a small concentration of gefitinib (0.62 μmol/L) significantly inhibited IL-13-induced M2-like polarization of macrophages, evidenced by the decreased expression of the M2 surface markers CD206 and CD163, down-regulation of specific M2-marker genes (Mrc1, Ym1, Fizz1, Arg1, IL-10 and CCL2) as well as inhibition of M2-like macrophage-mediated invasion and migration of LLC cells. In RAW 264.7 cells, gefitinib inhibits IL-13-induced phosphorylation of STAT6, which was a crucial signaling pathway in macrophage M2-like polarization. In LLC mice metastasis model, oral administration of gefitinib (75 mg·kg−1·d−1, for 21 d) significantly reduced the number of lung metastasis nodules, down-regulated the expression of M2 marker genes and the percentages CD206+ and CD68+ macrophages in tumor tissues. These results demonstrated that gefitinib effectively inhibits M2-like polarization both in vitro and in vivo, revealing a novel potential mechanism for the chemopreventative effect of gefitinib.
Keywords: gefitinib, Lewis Lung cancer, tumor-associated macrophages, M2-like polarization, STAT6 signaling
Introduction
Macrophages are a fundamental component of innate immunity and exert a crucial role in inflammation and the body's defense system by acting as the first line of resistance against microorganisms. The recruitment of monocytes and their differentiation into macrophages in tumor tissues shows significant diversity and plasticity1,2,3. Previously, developed hypotheses have proposed that tumor-associated macrophages (TAMs) participate in the antitumor responses of the body, but many recent clinical and experimental studies have demonstrated that in most cases, TAMs increase tumor progression to malignancy4,5,6. Several clinical studies have shown a correlation between the high influx of TAMs into the tumor with poor clinical outcomes in breast, prostate, ovarian, hepatocellular, and cervical cancers7,8. Because plasticity and heterogeneity are the main features of macrophages in the tumor microenvironment, upon different stimuli, TAMs have either a tumor-preventing or tumor-promoting role that depends on the polarization status of the macrophages. Macrophages are primarily differentiated into two distinct phenotypes. Both classically activated M1 and alternatively activated M2 have been observed in tumors9. In nonmalignant tumors, the majority of TAMs are classically activated M1-like macrophages that are activated by interferon-γ (IFN-γ) or lipopolysaccharide (LPS), which promote the production of pro-inflammatory cytokines, lead to antigen presentation and promote tumor lysis. In contrast, M2-like macrophages stimulated in the presence of Th2 cytokines, such as interleukin-4 (IL-4) or interleukin-13 (IL-13), activate the signal transducer and activator of transcription-6 (STAT6) signaling pathway, which is indispensable for macrophage M2-like polarization. Moreover, STAT6 regulates the expression of macrophage M2-like associated specific genes such as arginase-1 (Arg1), mannose receptor C type-1 (Mrc1), Retnla (Fizz1), and chil3 (Ym1)10,11. In established tumors, TAMs have an anti-inflammatory function and are similar to M2-like polarized macrophages, which enhance angiogenesis, tissue remodeling and suppress antitumor immune responses12,13. Thus, M2-like polarized TAMs are considered a promising target for adjuvant anticancer therapies. However, the extremely complicated association between TAMs and cancer cells has not yet been clearly elucidated. Most importantly, whether TAMs can increase tumor progression remains a subject of controversy14. Thus, the multifaceted role of TAMs in tumor progression highlights the importance of developing novel therapeutic strategies by targeting these macrophages.
Gefitinib, an EGFR tyrosine kinase inhibitor (TKI), is a small molecule and has been approved to treat patients suffering from non-small cell lung cancer (NSCLC) metastasis15,16. Gefitinib is also being used in clinical trials for certain types of cancers, including esophageal, breast, and lung cancers. Data from in vitro studies have shown that, in addition to reducing proliferation in transformed cells, gefitinib promotes cell cycle arrest, apoptosis, and antiangiogenic activity17. However, published studies that focused on the inhibition of cell proliferation and the induction of cell apoptosis are not able to exclusively explain the mechanism underlying the beneficial effect of gefitinib against TAMs M2-like polarized macrophages related cancer.
Our study demonstrates the relevance of macrophage polarization and the antitumor effect of gefitinib. In the current study, we showed that gefitinib at 0.62 μmol/L efficiently skewed macrophages away from the M2-like polarization induced by IL-13 in vitro. Furthermore, we demonstrated that the STAT6 signaling pathway participated in the inhibition of M2-like polarization by gefitinib. Importantly, the in vivo effect of gefitinib was linked to the decreased number of M2-like macrophages in the tumor region of Lewis lung cancer (LLC) metastasis. Altogether, our study showed for the first time that gefitinib can inhibit TAMs M2-like polarization, which may contribute to reduced cancer incidence and cancer-related mortality.
Materials and methods
Materials, antibodies, and reagents
Gefitinib was obtained from Selleck Chemicals (China). It was dissolved in dimethylsulfoxide (DMSO) for the in vitro study. IL-13 was purchased from PeproTech (Rocky Hill, NJ, USA). M-CSF (mouse recombinant) and antibody against STAT6 were purchased from Cell Signaling Technology (Beverly, MA, USA). p-STAT6 (phospho-Y641) and Ym1 antibodies were purchased from Abcam (Cambridge, UK). Antibodies against Mrc1, Arg1, Fizz1 and actin were purchased from Santa Cruz Biotechnology (CA, USA). For flow cytometry analysis, antibodies including PE-conjugated anti-mouse CD163, CD206 and F4/80 were purchased from Biolegend (San Diego, CA, USA). For immunofluorescence, primary antibodies including FITC-conjugated anti-mouse CD206 and CD68 were purchased from Biolegend, Bioscience, and Sigma, respectively, while anti-rat and anti-goat secondary antibodies were purchased from Life Technologies (Thermo Fisher Scientific).
Cell culture and differentiation
LLC and RAW 264.7 cells were obtained from the Cell Bank of Chinese Academy of Sciences (Shanghai, China). RAW 264.7 and LLC cells were cultured and maintained in Dulbecco's modified Eagle's medium (DMEM) enriched with 10% FBS and 100 units/mL of penicillin-streptomycin in a 5% CO2 humidified incubator at 37 °C.
LLC mice metastasis model
The C57BL/6 (6–8 weeks old) mice used in this study were purchased from the National Rodent Laboratory Animal Resource (Shanghai, China). All animal protocols were approved by the Animal Research Committee at Zhejiang University, and all treatments were administered according to the Guidelines of the Institutional Animal Use and Care Committee.
For the LLCs intravenous model, mice were chosen randomly and divided into four groups (10 mice in each) based on the difference in macrophages co-inoculated with LLC cells. Lung cancer metastasis in mice was generated by intravenous tail vein injection with 1×106 LLCs cells in 0.2 mL DMEM or 1×106 RAW 264.7 cells in 0.2 mL DMEM. After tumor-cell injection, gefitinib was given orally at 75 mg/kg. All animals were euthanized at d 21 after the injection of tumor cells.
Immunofluorescence
To analyze the expression of M2-like macrophages, tumor tissues were immediately frozen in OCT compound. For the evaluation of tumor vessel normalization, tumor tissues were fixed in 4% PFA for 1 h, dehydrated overnight at 4 °C and then frozen in OCT compound. Then, all tissues were cut at a thickness of 8 μm. For immunofluorescence, the following primary antibodies were used: goat anti-CD206 (1:200) and rat anti-CD68 (1:500). Then, the approximate secondary fluorescent antibodies conjugated with Alexa Fluor 488 or 594 were incubated. For the analysis of M2-like macrophages, FITC-conjugated anti-rat CD163 antibody (1:1000) and FITC-conjugated anti-goat CD206 (1:1000) were incubated for 4 h at room temperature. Then, nuclei were visualized by DAPI staining for 5 min. Slides were then dehydrated, mounted and cover slipped. For morphometric evaluation, at least five optical fields per tumor section were randomly chosen and analyzed by an Olympus IX81-FV1000 confocal laser-scanning microscope. For all studies, 5–10 optical fields (20× or 40× magnification) per tumor section were randomly chosen and analyzed.
Bone marrow-derived macrophage isolation and differentiation
Bone marrow-derived macrophage (BMDMs) isolation was performed as previously described, with minor modifications18. Six-week-old C57BL/6 mice were euthanized, soaked in 75% ethanol, and the femurs were dissected using scissors. The bones were flushed with a syringe filled with DMEM to extrude the bone marrow into a small petri dish. Then, bone marrow cells were cultured in DMEM containing 10% FBS and 50 ng/mL macrophage colony-stimulating factor (M-CSF) for three days to allow differentiation to macrophages.
Cell survival assay
For the analysis of cell proliferation, cells were incubated at a density of (2–5)×103 cells per well in 96-well plates. Cells were allowed to adhere overnight and were then exposed to serial concentrations of gefitinib for 72 h. Cells were harvested after 72 h in culture and fixed by 10% TCA for 1 h at 4 °C. After fixing, media was removed, cells were washed, and they were then subsequently stained by sulforhodamine B (SRB). Following dye incorporation, fluorescence was measured at 492 nm to reflect cell density with the Multiskan Microplate Spectrophotometer (Thermo Scientific, Wilmington, DE, USA). The inhibitory rate of cell proliferation for each well was calculated.
Flow cytometry
The presence of M2-like macrophage-specific cell surface markers was detected by using flow cytometry. RAW 264.7 or BMDM cells were seeded in 6 well plates and treated with IL-13 (10 ng/mL) with or without gefitinib; after 72 h, cells were collected with a scraper and blocked with 3% BSA for 1 h. Then, cells were suspended in PBS and incubated with PE-conjugated anti-mouse CD206 (1:100), CD163 (1:100) (Biolegend) or FITC-conjugated anti-mouse F4/80 (1:200) (eBioscience) antibody for 1 h at 4 °C according to the manufacturers' instructions. Finally, 1×104 viable cells for each sample were analyzed using a BD FACSCalibur cytometer (Becton Dickinson, San Jose, CA, USA).
Quantitative RT-PCR assay
The total RNA extracted from RAW 264.7 and BMDMs using the Easy Pure RNA Kit (Transgen Biotech Co, Ltd) was used to synthesize single-stranded cDNA. The sequences of the forward and reverse primers used for RT-PCR are listed in Table 1.
Table 1. Primers used for quantitative real time-PCR analysis.
| Genes | Primer sequence (5′ → 3′) |
|---|---|
| Mrc1 | Forward primer: AGGGACCTGGATGGATGACA |
| Reverse primer: TGTACCGCACCCTCCATCTA | |
| Arg1 | Forward primer: AACACGGCAGTGGCTTTAAC |
| Reverse primer: GTCAGTCCCTGGCTTATGGTT | |
| Chil3 (Ym1) | Forward primer: CATGAGCAAGACTTGCGTGAC |
| Reverse primer: GGTCCAAACTTCCATCCTCCA | |
| Retnla (Fizz1) | Forward primer: CCCTGCTGGGATGACTGCTA |
| Reverse primer: TGCAAGTATCTCCACTCTGGATCT | |
| IL-10 | Forward primer: CCTGGATCTGTATCACCGAAGC |
| Reverse primer: CTCCGACCACTCTGCCTTGTTA | |
| CCL2 | Forward primer: GAGAGCAACACAGGTTGGGA |
| Reverse primer: GGAAGGACTGGGGCTTTTGT | |
| Actin | Forward primer: GGTCATCACTATTGGCAACG |
| Reverse primer: ACGGATGTCAACGTCACACT |
The reaction of real-time PCR mixtures containing SYBR Green was composed according to the manufacturer's protocol. The real-time quantitative PCR analysis was performed with Bio-Rad SYBR Premix (Bio-Rad, Hercules, CA, USA). The expression of the relative mRNA levels of target genes was normalized to β-actin mRNA.
Conditioned medium preparation
The conditioned medium for macrophage polarization was obtained by seeding the cells in DMEM medium enriched with 10% FBS and 10 ng/mL IL-13 with or without gefitinib for 72 h. Then, culture medium of different polarized RAW 264.7 cells was replaced by fresh FBS-free medium for 24 h. The supernatant medium was collected as macrophage conditioned medium (CM). The CM was then centrifuged at 3000 revolutions per minute for 10 min to separate out the debris and then stored at -80 °C.
Wound-healing assay
RAW 264.7 and LLC cells were seeded in 24-well plates in DMEM medium enriched with 10% FBS and cultured until 70% to 80% confluence. The cells were then wounded with a straight scratch of approximately 0.4 to 0.5 mm in width made with a sterile pipette tip. The culture medium was then immediately replaced with fresh conditioned medium and cells were then incubated in CM for 24 h. Digitized images were captured to evaluate the migration of cells across the artificial wound with optical fields (10× magnification) that were randomly chosen and analyzed by using a Leica DMI 4000B (Buffalo Grove, USA) with Leica Application Suite software.
Transwell assay
A Transwell Boyden Chamber with 6.5-mm diameter polycarbonate filters and 8-μm pore size (Costar, Bethesda, MD, USA) was used to perform the migration assay. LLC or RAW 264.7 cells were seeded at a density of 1×104 (in 200 μL CM) per well in the upper chamber. A volume of 0.6 mL CM was placed into the lower chambers and allowed to incubate at 37 °C for 24 h. RAW 264.7 or LLC cells were incubated in the upper chamber for 24 h. In the upper chamber, non-migrated cells were then removed using cotton buds dipped in PBS and discarded. The migrant cells were fixed with 90% ethanol for at least 30 min. The migrated cells on the bottom chamber were stained with 0.1% crystal violet. The stained cells were photographed with a Leica DMI 4000B (Buffalo Grove, USA) in which five optical fields (10× magnification) per well were randomly chosen and quantitatively analyzed by using ImageJ software.
Western blot analysis
Cells were seeded in 6-well plates at a density of 1×105 cells per well for 24 h. After treatment with gefitinib for the indicated times, the macrophages were collected. Then, cellular and nuclear extracts were prepared and analyzed as previously described19.
Statistical analysis
Results are presented as the mean value±standard deviations (SD). The significance of the differences between the values of the groups was calculated with a two-tailed unpaired Student's t-test. Differences were considered significant if the P value was less than 0.05.
Results
Effect of gefitinib on cell proliferation
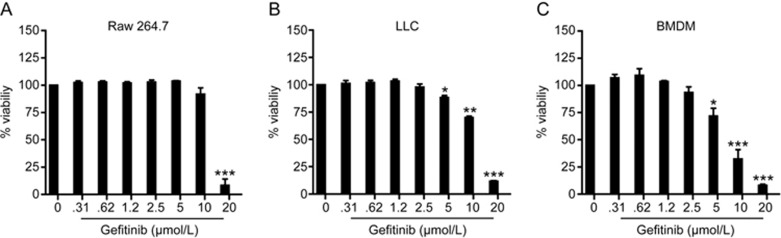
We assessed the proliferative and inhibitory effect of gefitinib on RAW 264.7, LLC and BMDM cells that were incubated in 96-well plates and maintained in DMEM containing 10% FBS overnight. Then, cells were exposed to serial concentrations of gefitinib from 0.31 to 20 μmol/L for 72 h. The cell proliferation and inhibitory activities were measured using SRB assays. The results are depicted in Figure 1. Gefitinib treatment did not cause significant growth inhibition below a 2.5 μmol/L concentration in all three cell lines.
Figure 1.
The effect of gefitinib on cell proliferation. (A) RAW 264.7, (B) LLC, and (C) BMDM cells were seeded in 96-well plates in DMEM+10% FBS. The cells were incubated overnight at 37 °C. Cells exposed to serial concentrations of gefitinib (0.31–20 μmol/L) for 72 h. The cell proliferation and inhibitory activities of gefitinib were assessed by SRB assays. Each assay was performed independently in triplicate. The error bars represent the standard deviation (±SD). *P<0.05; **P<0.01; ***P<0.001.
Gefitinib efficiently inhibits IL-13-induced M2-like polarization of macrophages
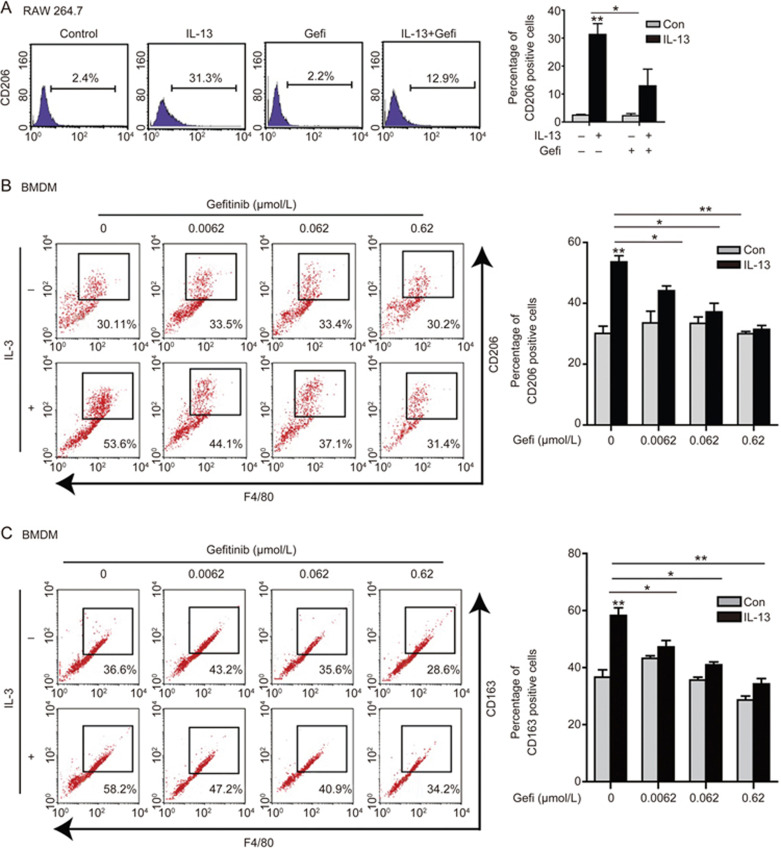
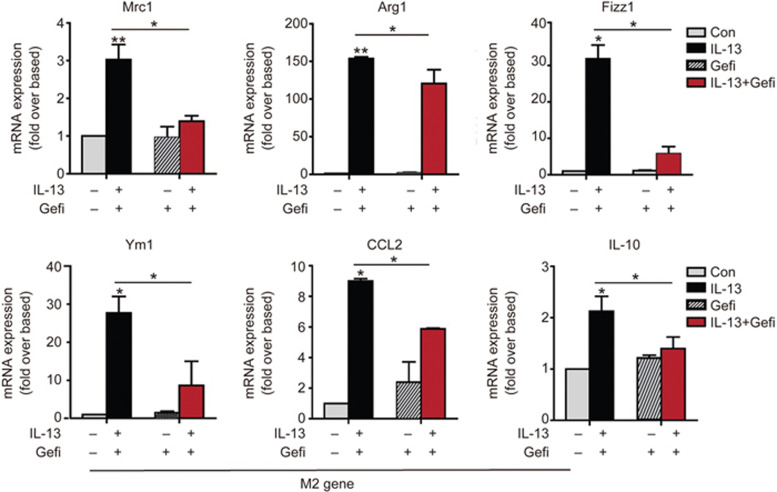
The alternate activation of M2-like polarization contributes to the poor progression of tumors20. CD206 and CD163 are M2-like macrophage surface markers in mice and humans. The expression of CD206 and CD163 is high in TAMs21. We assessed whether gefitinib could affect the M2-like polarization of macrophages. Consequently, we first analyzed the effect of gefitinib on the IL-13-induced M2-like polarization of macrophages in vitro. Significant up-regulation of surface marker CD206 expression was observed when RAW 264.7 cells were treated with 10 ng/mL IL-13 for 72 h. The surface marker expression of CD206 was greatly reduced by gefitinib at 0.62 μmol/L (Figure 2A). Similarly, IL-13 induced the surface marker expression of CD206 and CD163 in BMDMs. The expression of CD206 and CD163 was reduced in a gefitinib concentration-dependent manner (Figure 2B and 2C). To confirm the impact of gefitinib on M2-like polarization, the transcriptional changes of specific M2 marker genes were assessed by quantitative real-time PCR. The mRNA levels of M2 marker, Mrc1, Ym1, Fizz1, Arg1, IL-10 and CCL2 were all markedly decreased upon treatment with gefitinib at 0.62 μmol/L compared to the IL-13-treated group (Figure 3). Macrophages release various types of cytokines depending on the type of external stimuli and play a significant role in tumors22,23. The chemokine CCL2 has a crucial role in the regulation of the infiltration and migration of monocytes and influences macrophage M2-like polarization24. Our data demonstrated that gefitinib significantly inhibits the mRNA levels of IL-13-induced CCL2. Therefore, these results clearly suggest that gefitinib inhibited the macrophage M2-like polarization induced by IL-13.
Figure 2.
Gefitinib efficiently inhibits the M2-like polarization of macrophages induced by IL-13. (A) RAW 264.7 cells were treated with IL-13 (10 ng/mL) with or without gefitinib (0.62 μmol/L) for 72 h. The expression of the cell surface M2 marker CD206+ was analyzed by FACS analysis. (B and C) Bone marrow-derived macrophages (BMDMs) were treated with IL-13 (10 ng/mL) with or without different concentrations of gefitinib for 72 h. The percentages of F4/80+, CD206+ and CD163+ macrophages were analyzed by FACS analysis. The results are presented as the mean±SEM of triplicate determination. *P<0.05; **P<0.01.
Figure 3.
Gefitinib inhibits the expression of specific M2-marker genes. Quantitative real-time PCR was performed to assess the mRNA levels of M2-marker genes. BMDMs were exposed to IL-13 (10 ng/mL) and treated with or without gefitinib (0.62 μmol/L) for 24 h. The results are presented as the mean±SEM of triplicate determination. *P<0.05; **P<0.01.
The IL-13-induced STAT6 signaling pathway participates in gefitinib-mediated inhibition of M2-like polarization
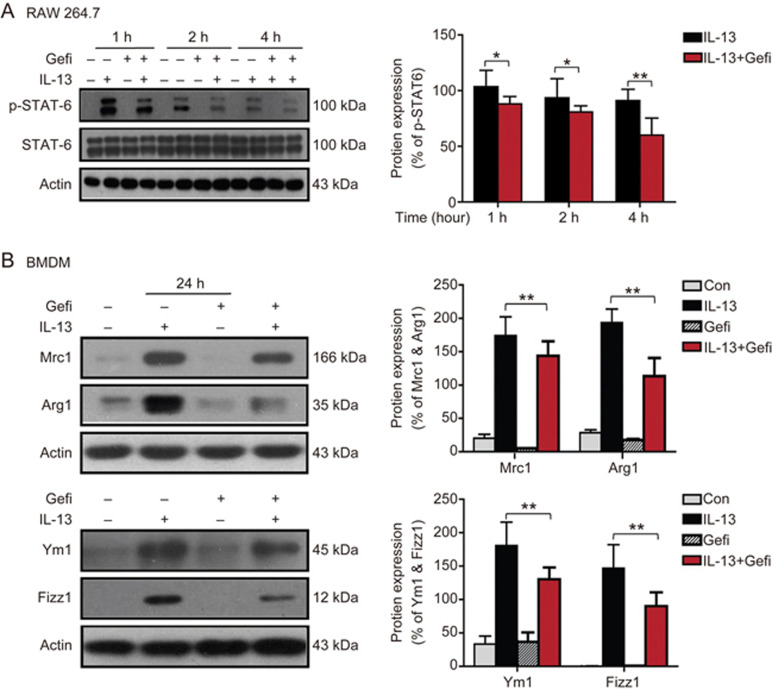
Next, we investigated the molecular mechanisms by which gefitinib inhibited macrophage M2-like polarization. The classical signaling pathway for IL-4/IL-13-induced tumor-associated macrophages involves the phosphorylation of STAT6, which plays a significant role in M2-like polarization25. Additionally, the expression of M2 genes such as Mrc1 and Arg1 has been described to be STAT6-dependent26,27. In general, STAT6 is rapidly activated upon cytokine receptor binding. Consistent with this idea, IL-13-induced STAT6 played an important role in M2-like polarization. We analyzed the phosphorylated level of STAT6 during the polarization process. RAW 264.7 cells were treated IL-13 with or without gefitinib for the indicated time. IL-13 significantly increased the p-STAT6 level while co-treatment with gefitinib dramatically reduced its expression over time, suggesting that IL-13-induced STAT6 might be contributing to the gefitinib-mediated inhibition of M2-like polarization of TAMs (Figure 4A). In addition to quantitative PCR, we further determined the protein levels of Arg1, Mrc1, Ym1 and Fizz1 via Western blot. As shown in Figure 4B, gefitinib decreased the IL-13-induced expression of Mrc1, Arg1, Ym1, and Fizz1. Taken together, these in vitro results suggest that gefitinib significantly inhibited the IL-13-induced M2-like polarization of macrophages through the STAT6-dependent signaling pathway.
Figure 4.
STAT6 signaling pathway involvement in gefitinib-mediated inhibition of M2-like polarization of macrophages. (A) RAW 264.7 cells were treated with IL-13 (10 ng/mL) with or without gefitinib for the indicated times. Western blots of STAT6 and activated p-STAT6 in cell lysates. (B) Western blot was performed to measure the protein level of Mrc1, Arg1, Ym1, and Fizz1. BMDMs were stimulated with IL-13 (10 ng/mL) and treated with or without gefitinib for 24 h. Actin was used as a loading control. The results are presented as the mean±SEM of triplicate determinations. *P<0.05; **P<0.01.
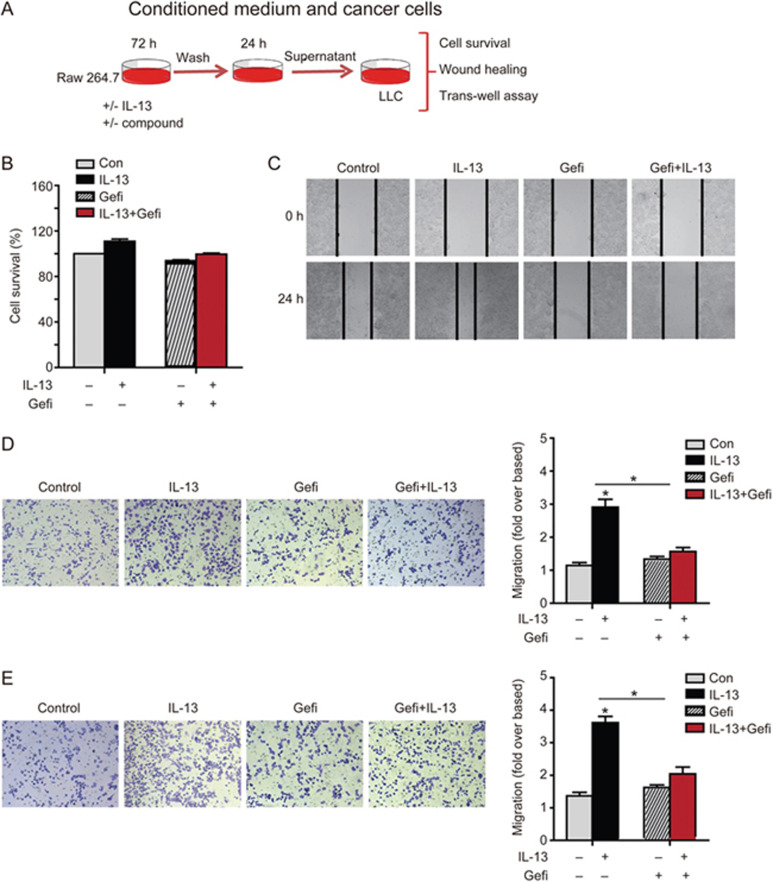
Gefitinib abrogates M2-like macrophage promoted invasion and migration of LLCs in vitro
Increasing evidence suggests that M2-like macrophages have the capacity to promote angiogenesis and cancer metastasis28,29. We investigated the effect of gefitinib on the functional macrophage tumor cell interaction. Macrophage cells were treated with IL-13 with or without gefitinib for 72 h, and then, the culture medium was replaced with fresh FBS-free medium for 24 h. Then, the supernatant medium was collected as macrophage conditioned medium (CM). To eliminate the impact of conditioned medium on tumor cell survival, LLCs cells were treated with a conditioned medium for 24 h and cell proliferation was analyzed by SRB assay. Surprisingly, no significant difference was observed in all four groups (Figure 5B). We further analyzed the effect of gefitinib on the angiogenesis-promoting ability of macrophages by evaluating the migrating ability of LLCs in different CMs using the wound-healing assay. We found that IL-13-treated macrophage CM significantly promoted the migration of cells by 24 h, whereas combination treated CM of IL-13 and gefitinib did not show this effect, nor did the CM from gefitinib treated-macrophages (Figure 5C). We evaluated the migrating ability of LLC and RAW 264.7 cells in different CMs using the Transwell assay; IL-13-treated macrophage CM promoted LLC and RAW 264.7 migration, which was abrogated by gefitinib (Figure 5D and 5E).
Figure 5.
Gefitinib inhibits M2-like macrophage-promoted invasion and migration in vitro. (A) Schematic representation of the experimental approach used in vitro as described in the Methods section. BMDMs were treated with IL-13 (10 ng/mL) with or without gefitinib (0.62 μmol/L) for 72 h and the culture medium was replaced with fresh serum-free medium. After 24 h, the supernatant medium was collected as macrophage-conditioned medium (CM). (B) LLCs were cultured with CM for 24 h. Cell survival was determined by SRB assay. (C) For the wound healing assay, LLCs cells were seeded in 24-well plates in DMEM medium with 10% FBS, cells were then wounded with a straight scratch using a pipette tip and treated with CMs for 24 h. (D and E) The cells were seeded in the upper chamber and CM was placed into the lower chambers and allowed to incubate at 37 °C for 24 h. The migrated cells on the bottom chamber were stained with 0.1% crystal violet. Then, the effect of different CMs on RAW 264.7 and LLCs migration was evaluated by Transwell assay. The results are presented as the mean±SEM of triplicate determinations. *P<0.05.
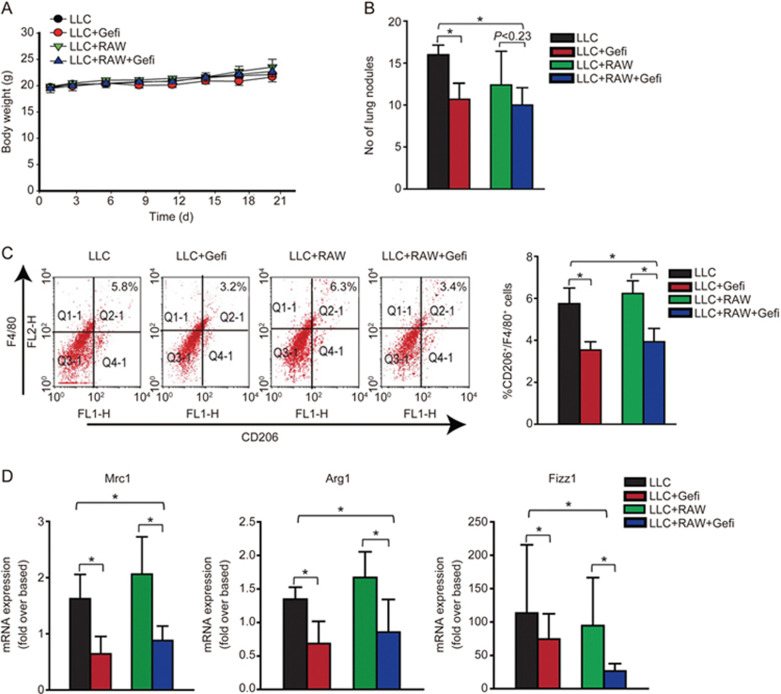
Gefitinib prevents LLC formation in vivo by targeting macrophages
To validate our in vitro results, we then analyzed whether gefitinib had an in vivo effect on lung cancer growth in addition to whether it inhibits the occurrence of TAMs M2-like macrophages. Using the LLCs intravenous model, mice were randomly chosen and divided into four groups based on the difference in macrophages co-inoculated with LLC cells. Mice with LLC tumors were euthanized at d 21 after the injection of tumor cells. The average body weight of mice was not affected (Figure 6A). The number of lung metastasis nodules was potentially reduced in the gefitinib treatment group compared to the untreated control group (Figure 6B). We then investigated whether gefitinib altered TAMs polarization in tumor tissue. The expression of the M2 surface marker CD206 in tumor tissue was analyzed by FACS. The percentage of CD206 was greatly reduced in the gefitinib-treated group compared to the untreated control group (Figure 6C). Next, we examined the expression of specific M2 TAM marker genes in tumor tissue. Quantitative real-time PCR was performed to assess the mRNA levels of M2-like macrophages. The mRNA expression of Mrc1, Arg1, and Fizz1 were significantly decreased in gefitinib-treated groups.
Figure 6.
Gefitinib prevents Lewis lung cancer formation in vivo by targeting macrophages. C57BL/6 mice were injected intravenously and were treated with gefitinib (75 mg/kg). After 21 d, animals were euthanized and the lungs were analyzed. (A) The average body weight of each group is expressed as the mean±SD (n=6). (B) Quantitative analysis of lung metastasis nodules (n=6). (C) The percentage of M2 surface markers F4/80+ CD206+ was analyzed by FACS analysis. (D) Quantitative real-time PCR was performed to assess the mRNA levels of the M2-marker genes Mrc1, Arg1, and Fizz1. The results are presented as the mean±SEM *P<0.05.
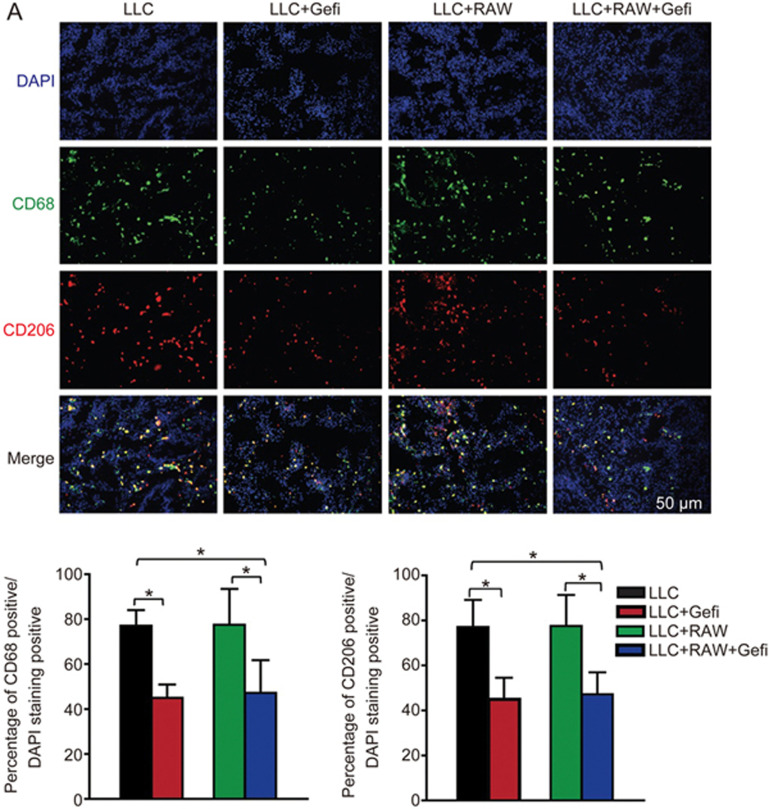
Macrophages are the most important and prominent component of leukocytes that infiltrate tumor-bearing mice and humans with different types of cancers7. Considering the effects of gefitinib on metastasis, we assume that gefitinib may inhibit lung metastasis by acting on macrophages. Furthermore, we investigated the gefitinib-mediated effect on altered TAMs polarization in tumor tissue. Immunohistochemistry analysis showed that, compared to untreated controls, gefitinib-mediated inhibition markedly decreased the percentage of CD206+ and CD68+ macrophages in tumor tissue (Figure 7). These observations suggest that M2-like polarized macrophages play a significant role in the regulation of tumorigenesis in lung cancer. Nevertheless, gefitinib antagonizes the tumorigenesis induced by M2-like polarized macrophages.
Figure 7.
Gefitinib decreases the M2 polarization of TAMs. (A) The lung sections from a different group were double stained with the macrophage marker CD68 and the M2-marker CD206. The percentage of CD68+ and CD206+ cells was calculated as a ratio of green cells to DAPI blue cells. Random non-overlapping fields from sections of each group were examined. The results are presented as the mean±SEM. *P<0.05.
Discussion
Many studies have revealed that M2-like polarized TAMs contribute in angiogenesis, cancer progression, and metastasis in various types of cancer including pancreatic cancer, liver cancer, ovarian cancer, and NSCLC. In recent studies, it was reported that gefitinib inhibits angiogenesis, chemotactic migration, metastasis-related proteins and matrix metalloproteinases-2 and -9 (MMP-2 and -9)30 . The antitumor and anti-migration activity of gefitinib in NSCLC is conferred by the suppression of the expression of DOCK1, Akt activity, and the phosphorylation of vimentin31. Brouxhon et al reported that gefitinib inhibits soluble E-cadherin (sEcad) induced proliferation, migration and invasion in skin squamous cell carcinomas (SCCs)32. However, the mechanism of action by which gefitinib inhibits angiogenesis, invasion and cancer metastasis requires further investigation. In this study, we demonstrated that gefitinib efficiently suppressed TAMs M2 macrophages and LLCs metastasis in vivo. Consequently, our study suggests that gefitinib may act as a regulator of the tumor microenvironment in metastatic sites by affecting macrophage biology and provides new mechanistic insight into the antitumor function of gefitinib.
TAMs in the tumor microenvironment act as the most abundant immune cell types expressing pro-inflammatory cytokines, including IL-4, IL-13, and CCL2, which stimulate angiogenesis, tumor progression, and metastasis by suppressing immune responses7,33. It is well documented that in the tumor microenvironment TAMs are programmed and polarized into M2-like macrophages34. Our results highlight the relevance between macrophages and the anti-metastasis effect of gefitinib and suggest that the anti-metastasis effect of gefitinib may be due to inhibited accumulation of M2-like macrophages in LLCs.
The tumor microenvironment is composed of tumor cells, stromal cells, and their secreted inflammatory factors such as IL-13. Several studies have reported the effect of gefitinib on the biological functions of macrophages. Lin et al reported that gefitinib inhibits the secretion of soluble factors from activated macrophages that can promote EMT via the down-regulation of E-cadherin and β-catenin at the adherent junctions between hepatocellular carcinoma cells14. Gefitinib inhibits the EGFR which significantly decreases NF-κB pathway signaling and cytokine production35. Using the IL-13-induced M2-polarization model, we found that gefitinib inhibits IL-13-induced expression of M2 surface markers such as CD163 and CD206, as well as decreases the mRNA levels of M2 genes including Mrc1, Fizz1, Arg1, Ym1, and IL-10.
IL-4/IL-13-induced STAT6 signaling activates the genes responsible for M2-like polarization that play an important role in several human diseases36,37. Aberrant activation of STAT6 may also be involved in the development of various diseases38. The activation and differentiation of macrophages remains a subject of intense investigation39. In the present study, we showed for the first time that gefitinib could skew macrophages away from M2-like polarization in vivo and in vitro and suppress lung metastasis in LLCs cells. Furthermore, we demonstrated in vitro that gefitinib markedly decreased the IL-13-induced STAT6 signaling pathway and the expression of Mrc1 and Arg1, Ym1, and Fizz1, indicating that gefitinib acts as a potent inhibitor of M2-like macrophages.
Recently, various studies showed that conditioned medium from tumor cells can mimic the tumor microenvironment and induce the formation of tumor promoting M2-like macrophages with features similar to macrophages isolated from malignant tumors40,41. IL-4/IL-13 expression is a well-known phenotype of M2-like TAMs that promotes proliferation and angiogenesis9,42. However, consistent with previous studies, our data showed that conditioned medium from IL-13-activated macrophages promotes the migration of LLCs and RAW 264.7 cells and that co-treatment with gefitinib eliminated this IL-13-activated tumor-promoting effect. It has been observed that gefitinib does not directly affect the migration of LLCs or RAW 264.7 cells. These results indicated that IL-13-activated M2-like polarization was abrogated by gefitinib.
In summary, we reported that gefitinib inhibits the M2-like polarization of macrophages both in vitro and in vivo, which contributes to the inhibition of tumor metastasis. Our findings link TAMs with the anti-tumorigenic effect of gefitinib, specifically via the STAT6 signaling pathway, which represents a promising approach to modulate the LLCs environment and provides further support for the clinical application of gefitinib. Overall, these results suggest that gefitinib may target cancer cells under certain circumstances by inhibiting the M2-like polarization of macrophages. These observations highlight a novel effect of gefitinib and provide new insight to treat lung cancer by inhibiting M2 polarization.
Author contribution
Muhammad TARIQ, Jie-qiong ZHANG, and Gui-kai LIANG performed the majority of the experiments; Ling DING and Muhammad TARIQ participated in research design and performed data analysis; Ling DING, Bo YANG, and Qiao-jun HE participated in research design and wrote the manuscript.
Acknowledgments
We also acknowledge Zhejiang University for providing a scholarship for PhD studies to Mr Muhammad TARIQ.
References
- Ding L, Liang G, Yao Z, Zhang J, Liu R, Chen H, et al. Metformin prevents cancer metastasis by inhibiting M2-like polarization of tumor associated macrophages. Oncotarget 2015; 6: 36441–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sica A, Mantovani A. Macrophage plasticity and polarization: in vivo veritas. J Clin Invest 2012; 122: 787–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W, Wang J, Dong SF, Liu CH, Italiani P, Sun SH, et al. Immunomodulatory activity of andrographolide on macrophage activation and specific antibody response. Acta Pharmacol Sin 2010; 31: 191–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Y, Ping YF, Zhang X, Bian XW. Hostile takeover: glioma stem cells recruit TAMs to support tumor progression. Cell Stem Cell 2015; 16: 219–20. [DOI] [PubMed] [Google Scholar]
- Fan QM, Jing YY, Yu GF, Kou XR, Ye F, Gao L, et al. Tumor-associated macrophages promote cancer stem cell-like properties via transforming growth factor-beta1-induced epithelial–mesenchymal transition in hepatocellular carcinoma. Cancer Lett 2014; 352: 160–8. [DOI] [PubMed] [Google Scholar]
- Germano G, Frapolli R, Belgiovine C, Anselmo A, Pesce S, Liguori M, et al. Role of macrophage targeting in the antitumor activity of trabectedin. Cancer Cell 2013; 23: 249–62. [DOI] [PubMed] [Google Scholar]
- Qian BZ, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell 2010; 141: 39–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weagel E, Smith C, Liu PG, Robison R, O'Neill K. Macrophage polarization and its role in cancer. J Clin Cell Immunol 2015. doi: 10.4172/2155-9899.1000338.
- Dong R, Gong Y, Meng W, Yuan M, Zhu H, Ying M, et al. The involvement of M2 macrophage polarization inhibition in fenretinide-mediated chemopreventive effects on colon cancer. Cancer Lett 2017; 388: 43–53. [DOI] [PubMed] [Google Scholar]
- Jiménez-Garcia L, Herránz S, Luque A, Hortelano S. Critical role of p38 MAPK in IL-4-induced alternative activation of peritoneal macrophages. Eur J Immunol 2015; 45: 273–86. [DOI] [PubMed] [Google Scholar]
- Tugal D, Liao X, Jain MK. Transcriptional control of macrophage polarization. Arterioscler Thromb Vasc Biol 2013; 33: 1135–44. [DOI] [PubMed] [Google Scholar]
- Zhu L, Yang T, Li L, Sun L, Hou Y, Hu X, et al. TSC1 controls macrophage polarization to prevent inflammatory disease. Nat Commun 2014; 5: 4696. [DOI] [PubMed] [Google Scholar]
- Paulson JC. Innate immune response triggers lupus-like autoimmune disease. Cell 2007; 130: 589–91. [DOI] [PubMed] [Google Scholar]
- Lin CY, Lin CJ, Chen KH, Wu JC, Huang SH, Wang SM. Macrophage activation increases the invasive properties of hepatoma cells by destabilization of the adherens junction. FEBS Lett 2006; 580: 3042–50. [DOI] [PubMed] [Google Scholar]
- Normanno N, Maiello MR, De Luca A. Epidermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKIs): Simple drugs with a complex mechanism of action? J Cell Physiol 2003; 194: 13–9. [DOI] [PubMed] [Google Scholar]
- Zhang SR, Zhu LC, Jiang YP, Zhang J, Xu RJ, Xu YS, et al. Efficacy of afatinib, an irreversible ErbB family blocker, in the treatment of intracerebral metastases of non-small cell lung cancer in mice. Acta Pharmacol Sin 2017; 38: 233–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranson M, Wardell S. Gefitinib, a novel, orally administered agent for the treatment of cancer. J Clin Pharm Ther 2004; 29: 95–103. [DOI] [PubMed] [Google Scholar]
- Marim FM, Silveira TN. Lima DS Jr, Zamboni DS. A method for generation of bone marrow-derived macrophages from cryopreserved mouse bone marrow cells. PLoS One 2010; 5: e15263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding L, Ma W, Littmann T, Camp R, Shen J. The P2Y2 nucleotide receptor mediates tissue factor expression in human coronary artery endothelial cells. J Biol Chem 2011; 286: 27027–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mantovani A, Sozzani S, Locati M, Allavena P, Sica A. Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol 2002; 23: 549–55. [DOI] [PubMed] [Google Scholar]
- Rőszer T. Understanding the mysterious M2 macrophage through activation markers and effector mechanisms. Mediators Inflamm 2015; 2015: 816460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi HJ, Choi HJ, Chung TW, Ha KT. Luteolin inhibits recruitment of monocytes and migration of Lewis lung carcinoma cells by suppressing chemokine (C–C motif) ligand 2 expression in tumor-associated macrophage. Biochem Biophys Res Commun 2016; 470: 101–6. [DOI] [PubMed] [Google Scholar]
- Wang C, Yu X, Cao Q, Wang Y, Zheng G, Tan TK, et al. Characterization of murine macrophages from bone marrow, spleen and peritoneum. BMC Immunol 2013; 14: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chanmee T, Ontong P, Konno K, Itano N. Tumor-associated macrophages as major players in the tumor microenvironment. Cancers 2014; 6: 1670–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez FO, Helming L, Gordon S. Alternative activation of macrophages: an immunologic functional perspective. Annu Rev Immunol 2009; 27: 451–83. [DOI] [PubMed] [Google Scholar]
- Pauleau AL, Rutschman R, Lang R, Pernis A, Watowich SS, Murray PJ. Enhancer-mediated control of macrophage-specific arginase I expression. J Immunol 2004; 172: 7565–73. [DOI] [PubMed] [Google Scholar]
- Gensel JC, Zhang B. Macrophage activation and its role in repair and pathology after spinal cord injury. Brain Res 2015; 1619: 1–11. [DOI] [PubMed] [Google Scholar]
- Murdoch C, Muthana M, Coffelt SB, Lewis CE. The role of myeloid cells in the promotion of tumour angiogenesis. Nat Rev Cancer 2008; 8: 618–31. [DOI] [PubMed] [Google Scholar]
- Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature 2008; 454: 436–44. [DOI] [PubMed] [Google Scholar]
- Song J, Zhu J, Zhao Q, Tian B. Gefitinib causes growth arrest and inhibition of metastasis in human chondrosarcoma cells. J BUON 2015; 20: 894–901. [PubMed] [Google Scholar]
- Pan Y, Li X, Duan J, Yuan L, Fan S, Fan J, et al. Enoxaparin sensitizes human non-small-cell lung carcinomas to gefitinib by inhibiting DOCK1 expression, vimentin phosphorylation, and Akt activation. Mol Pharmacol 2015; 87: 378–90. [DOI] [PubMed] [Google Scholar]
- Brouxhon SM, Kyrkanides S, Teng X, Athar M, Ghazizadeh S, Simon M, et al. Soluble E-cadherin: a critical oncogene modulating receptor tyrosine kinases, MAPK and PI3K/Akt/mTOR signaling. Oncogene 2014; 33: 225–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai F, Liu L, Che G, Yu N, Pu Q, Zhang S, et al. The number and microlocalization of tumor-associated immune cells are associated with patient's survival time in non-small cell lung cancer. BMC Cancer 2010; 10: 220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruffell B, Affara NI, Coussens LM. Differential macrophage programming in the tumor microenvironment. Trends Immunol 2012; 33: 119–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardbower DM, Singh K, Asim M, Verriere TG, Olivares-Villagómez D, Barry DP, et al. EGFR regulates macrophage activation and function in bacterial infection. J Clin Inves 2016; 126: 3296–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David M, Ford D, Bertoglio J, Maizel AL, Pierre J. Induction of the IL-13 receptor α2-chain by IL-4 and IL-13 in human keratinocytes: involvement of STAT6, ERK and p38 MAPK pathways. Oncogene 2001; 20: 6660–8. [DOI] [PubMed] [Google Scholar]
- Yang M, Hogan SP, Henry PJ, Matthaei KI, McKenzie AN, Young IG, et al. Interleukin-13 mediates airways hyperreactivity through the IL-4 receptor-alpha chain and STAT-6 independently of IL-5 and eotaxin. Am J Respir Cell Mol Biol 2001; 25: 522–30. [DOI] [PubMed] [Google Scholar]
- Stütz AM, Pickart LA, Trifilieff A, Baumruker T, Prieschl-Strassmayr E, Woisetschläger M. The Th2 cell cytokines IL-4 and IL-13 regulate found in inflammatory zone 1/resistin-like molecule α gene expression by a STAT6 and CCAAT/enhancer-binding protein-dependent mechanism. J Immunol 2003; 170: 1789–96. [DOI] [PubMed] [Google Scholar]
- Jia X, Yu F, Wang J, Iwanowycz S, Saaoud F, Wang Y, et al. Emodin suppresses pulmonary metastasis of breast cancer accompanied with decreased macrophage recruitment and M2 polarization in the lungs. Breast Cancer Res Treat 2014; 148: 291–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu F, Jia X, Du F, Wang J, Wang Y, Ai W, et al. miR-155-deficient bone marrow promotes tumor metastasis. Mol Cancer Res 2013; 11: 923–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Chen K, Wang C, Gong W, Yoshimura T, Liu M, et al. Cell surface receptor FPR2 promotes antitumor host defense by limiting M2 polarization of macrophages. Cancer Res 2013; 73: 550–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jetten N, Verbruggen S, Gijbels MJ, Post MJ, De Winther MP, Donners MM. Anti-inflammatory M2, but not pro-inflammatory M1 macrophages promote angiogenesis in vivo. Angiogenesis 2014; 17: 109–18. [DOI] [PubMed] [Google Scholar]