Over the past 30 years there has been a controversy about the optimal diet composition for weight loss and maintenance. Some have defended the more conventional low-fat high-carbohydrate diet (Astrup et al., 2000), whereas others point at a restriction in carbohydrates as being more effective. Multiple variations of popular diets exist from ketogenic very-low carbohydrate diets (Astrup et al., 2004), to diets pointing more at a slight increase in protein, and lowering the glycemic index of the carbohydrates as the most effective strategy (Larsen et al., 2010). Numerous randomized controlled trials (RTC) have compared the various diets for the treatment of overweight and obesity based on the assumption that one diet fits all without being able to provide strong evidence for one or the other. And even meta-analyses comparing the different diet options have been unable to identity a clear winner.
In this issue of EBioMedicine, Wan et al. compared three different diets in a RCT conducted in a Chinese population of overweight individuals (BMI < 28 kg/m2) without traits of the metabolic syndrome: a LF-HC diet (fat 20%, carbohydrate 66% energy), a MF-MC diet (fat 30%, carbohydrate 56%), and the a HF-LC diet (fat 40%, carbohydrate 46%) (Wan et al., 2017).
About 300 individuals were randomized into the three treatment arms, and after 6 months 245 (79.8%) were retained in the study. Reduction in body weight was significantly greater in LF-HC throughout the intervention, and after 6 months weight loss was 0.5 kg greater than in the MF-MC, and 0.7 kg greater than in the HF-LC group. Effects on cardio-metabolic risk factors were somewhat similar across the three diets. Wan et al. should be congratulated with an excellent trial conducted with state of the art methodology, and this trial is one of the few larger one conducted in an Asian population and lasting for 6 months.
So how should the superiority of the low-fat carbohydrate diet in this population be viewed? Well, a recent discovery has shown that the effectiveness of these diets depends on the glucose metabolism of the overweight and obese participants (Hjorth et al., 2017). Briefly, normoglycemic individuals lost most weight on a low-fat high carbohydrate diet, whereas pre-diabetic individuals are much more susceptible to lose weight on a diet with more focus on quality of the carbohydrate content, i.e. lower glycemic index, more fiber and wholegrain (Hjorth et al., 2017). Notably, these effects are quite pronounced even under ad libitum conditions i.e. without putting any limit on the caloric intake (Fig. 1). For the overweight and obese diabetics a reduction in carbohydrate amount is pivotal, and for this group a relatively higher amount of fat and protein in the diet is beneficial for weight control and glycemic status (Snorgaard et al., 2017). With these studies it is obvious that one diet does not fit all, and a personalized dietary approach is warranted.
Fig. 1.
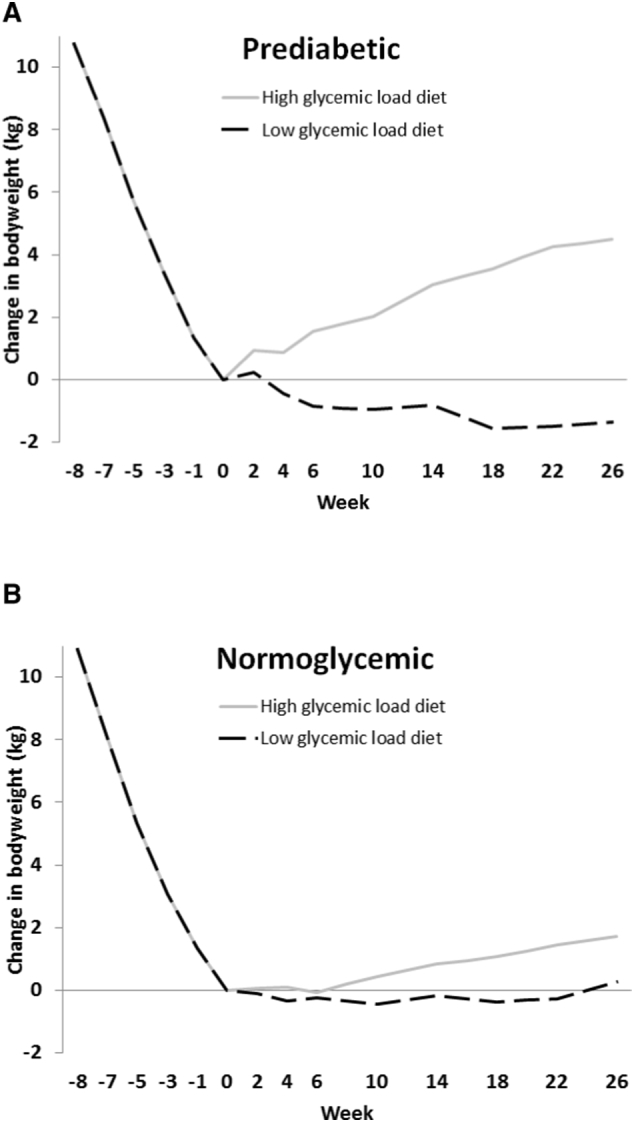
Changes in bodyweight among participants during an initial 8-week low calorie diet followed by a 26 weeks weight maintenance diet high or low in glycemic load. (A) Participants with prediabetes. (B) Normoglycemic participants. Based on data from reference Hjorth et al. (2017).
Participants in the study by Wan et al. had a mean age of 23 years, mean BMI of 21.8 kg/m2 and mean fasting glucose of 4.1 mmol/L. Therefore, the population must be characterized as a healthy, insulin sensitive group that actually could have been predicted to have a better responsiveness on the low-fat high-carbohydrate diet. It would be interesting to extend the studies to pre-diabetic and diabetic Asian obese to examine if the findings in a predominantly Caucasian population also are valid for Asians.
Disclosure
AA and MFH are co-inventors on an international patent application (PCT/US17/35537) on the use of biomarkers for prediction of weight loss responses based on fasting plasma glucose and insulin.
References
- Astrup A., Grunwald G.K., Melanson E.L., Saris W.H.M., Hill J.O. The role of low-fat diets in body weight control: a meta-analysis of ad libitum intervention studies. Int. J. Obes. 2000;24:1545–1552. doi: 10.1038/sj.ijo.0801453. [DOI] [PubMed] [Google Scholar]
- Astrup A., Larsen T.M., Harper A. Atkins and other low-carbohydrate diets: hoax or an effective tool for weight loss? Lancet. 2004;364:897–899. doi: 10.1016/S0140-6736(04)16986-9. [DOI] [PubMed] [Google Scholar]
- Hjorth M.F., Ritz C., Blaak E.E., Saris W.H.M., Langin D., Poulsen S.K. Pre-treatment fasting plasma glucose and insulin modify dietary weight loss success: results from three randomized clinical trials. Am. J. Clin. Nutr. 2017 doi: 10.3945/ajcn.117.155200. (In press) [DOI] [PubMed] [Google Scholar]
- Larsen T.M., Dalskov S., van Baak M., Jebb S., Papadaki A., Pfeiffer A.F.H., Martinez J.A., Handjieva-Darlenska T., Kunešová M., Pihlsgård M., Stender S., Holst C., Saris W.H.M., Astrup A. For the diet, obesity, and genes (Diogenes) project. Diets with high or low protein content and glycemic index for weight-loss maintenance. N. Engl. J. Med. 2010;362:2102–2113. doi: 10.1056/NEJMoa1007137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snorgaard O., Poulsen G.M., Andersen H.K., Astrup A. Systematic review and meta-analysis of dietary carbohydrate restriction in patients with type 2 diabetes. BMJ Open Diabetes Res. Care. 2017 Feb 23;5(1):e000354. doi: 10.1136/bmjdrc-2016-000354. (eCollection 2017) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan Yi. Effects of macronutrient distribution on weight and related cardiometabolic profile in healthy non-obese chinese: a 6-month, randomized controlled-feeding trial. EBioMedicine. 2017 doi: 10.1016/j.ebiom.2017.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]


