Abstract
Background and Aims:
Optimization of patient's head and neck position for the best laryngeal view is the most important step before laryngoscopy and intubation. The objective of this prospective crossover study was to determine the differences, if any, between the gold standard sniffing position (SP) and the further head elevation (HE) (neck flexion) with regard to the incidence of difficult laryngoscopy, intubation difficulty, and variables of the I ntubation Difficulty Scale (IDS) in adult patients undergoing elective surgery under general anesthesia.
Material and Methods:
In the “SP” the neck must be flexed on the chest by elevating the head with a cushion under the occiput and extending the head at the atlanto-occipital joint. Our study was carried out to evaluate the glottic view in SP compared to further HE by 1.5 inches during direct laryngoscopy in elective surgeries. Patients were randomly assigned to either Group A (“SP” during first laryngoscopy and “HE” during second laryngoscopy) or vice versa in Group B. The effect of patient position on ease of intubation was assessed using a quantitative scale - The intubation difficulty scale (IDS).
Results:
There were significant differences with regard to glottic visualization (P = 0.00), number of operators (P = 0.001), laryngeal pressure (P = 0.00), and lifting force (P = 0.00) required for intubation and IDS (P = 0.00), thus favoring further HE position.
Conclusion:
We conclude that the HE position is superior to standard SP with regard to ease of intubation as assessed by IDS.
Keywords: Head elevation (neck flexion) position, intubation difficulty scale, sniffing position
Introduction
Proper positioning of the head and neck is important for optimizing the laryngeal view during direct laryngoscopy.[1] Routine laryngoscopy is performed in “Sniffing position (SP)” (neck will be flexed [flexion of 35°] on the chest with a cushion under the occiput and extending [extension of 15°] the head at the atlanto-occipital joint) has been considered as the ideal position for direct laryngoscopy. The marker used for proper SP is alignment of the external auditory meatus with the sternum of the patients. Greenland et al.[2] described that alignment of external auditory meatus and sternal notch in same horizontal plain in supine makes it an optimum position for endotracheal intubation. Medline search showed scant literature that attempted to investigate the optimal position of the head for direct laryngoscopy. However, one study by Schmitt and Mang found that elevating the head higher than what is needed for a conventional SP may improve laryngeal exposure in some patients.[3]
The aim of our present study was to evaluate the glottic view in SP and further head elevation (HE) by 1.5-inch during direct laryngoscopy. Second, to evaluate the intubating conditions obtained with the two positions. A quantitative scale of intubation difficulty was used objectively for comparing the ease of endotracheal intubations - The Intubation Difficulty Scale (IDS).[4]
Material and Methods
Ethical approval for this study was provided by the NIMS Institutional Ethics Committee Hyderabad India 20th May 2013. With No EC/NIMS/1386/2013 and CTRI number CTRI/2014/11/005168. Informed written consent was obtained from the patients who were enrolled for the study.
The optimal SP was considered when external auditory meatus and sternal notch are at same horizontal plane in supine position of the patient[5] and we compared whether further neck flexion during direct laryngoscopy in patients undergoing surgery under general anesthesia can change Cormack-Lehane grading (CLG)[6] and variables of IDS. Hundred adult patients scheduled for elective surgery requiring endotracheal intubation under general anesthesia were recruited in this study. Study participants were randomized into two groups of 50 each by computer-generated random numbers. The study protocol included two laryngoscopies. In Group A (n = 50), the head position of the patient was in standard “SP” during first laryngoscopy (i.e. Laryngoscopy in Sniffing position- LS) and tracheal intubation was performed. Glottic visualization was assessed by CLG and IDS for intubation difficulty. During the second laryngoscopy (i.e., Laryngoscopy in Head Elevated position - LE), head of the patient was further elevated by placing 1.5-inch cushion under the head and trachea was intubated and again CLG and IDS variables were noted. Whereas in other group, i.e. Group B (n = 50) patient was placed with an HE of 1.5 inches over the standard SP during the first laryngoscopy (LE) and tracheal intubation was performed and during second laryngoscopy (LS) patient was placed in standard SP and intubation was done. IDS were note on both occasions. In each of the patient, angle of neck flexion was measured in both intubating positions using software “ Flash and Math Angle of Elevation”, version 1.0.0. Developed by Douglas Ensley, Ph.D. Professor of Mathematics, Shippensburg University, PA, USA.
All patients scheduled for elective surgical procedures and requiring general anesthesia with endotracheal intubation were enrolled in this study. All patients belonged to American Society of Anesthesiologists physical status (ASA) I and II and aged between 18 and 65 years with Mallampati Grade I and II. We have excluded patients with ASA physical status III and above, structural deformities involving face and airway, reactive airway disease, cervical spine pathology, neck masses, raised intracranial tension, and patients requiring rapid sequence intubation.
A thorough preoperative anesthetic evaluation was performed and the following airway measurements were noted. Mouth opening (<3.5 cm), thyromental distance (<6.5 cm), sternomental distance (<12 cm), modified Mallampati classification (Class III and IV), neck circumference (>40 cm), neck extension (<35°), and body mass index (BMI) (>30 kg/m2). Values mentioned in the brackets represents cutoff for predicting difficult airway.
IDS was used to quantify complexity of intubation during both intubating positions, it consists of seven independent parameters recorded by an independent observer after each intubation. Degree of difficulty is scored as easy, slight, moderate to major difficulty, and impossible with scores being “0,” “0–5,” “>5” and “∞”, respectively.[4]
Anesthetic management
Premedication consisted of tablet alprazolam 0.25 mg and ranitidine 150 mg night before and on the morning of surgery. In the operating room, baseline heart rate-systolic blood pressure, diastolic blood pressure, and peripheral oxygen saturation (SpO2) were monitored. Injection glycopyrrolate 0.1 mg, Intravenous (IV) was given 5 minutes before induction of anesthesia. Analgesia was provided with injection fentanyl 2 mcg/kg IV. All the patients were preoxygenated with 100% oxygen for 3 min. Standard induction included injection thiopentone sodium 4 mg/kg IV or until the loss of eyelash reflex and injection atracurium 0.5 mg/kg IV for muscle relaxation to facilitate intubation. Macintosh number 3 or 4 laryngoscope blade was used depending on the laryngoscopist preference. Group A included the patients placed in the standard SP during first laryngoscopy (LS) by placing a cushion under the head such that external auditory meatus and sternal notch are at same horizontal plane (some patients required additional 0.5-inch gel foams beneath the cushion for this horizontal alignment). Angle of the neck flexion was noted. Laryngoscopic view of the glottis was noted and tracheal intubation was performed and IDS was scored. Then, the endotracheal tube was removed, mask ventilation was performed and after 40 s, second laryngoscopy (LE) was performed with a further HE by placing a 1.5-inch cushion over first one, and angle of neck flexion was measured. Laryngoscopic view and IDS were noted and the tracheal intubation was done. Throughout the procedure vitals were monitored.
In Group B, the patients were placed with an HE of 1.5 inches over the standard SP during the first laryngoscopy (LE) and the laryngeal view was noted, tracheal intubation was done and IDS was scored. Then, the endotracheal tube was removed mask ventilation was performed and after 40 s, second laryngoscopy (LS) was performed with the patients in the SP by removing the 1.5-inch cushion. Angle of the neck flexion was noted in both occasions. The laryngeal view and the intubating parameters were noted.
Glottic visualization during LS and LE was assessed by CLG and intubation difficulty was assessed with the IDS. This scale is based on the determination of seven parameters recorded by an independent observer after each intubation. Study ends at this point, and the intended surgical procedure was contemplated.
Sample size estimation was based on the key outcome variable, i.e. difference in IDS between sniffing and head elevated positions in the same patient. Considering the nonparametric nature of the outcome variable, sample size was determined by inequality test for one mean suitable for paired data using double exponential distribution (Wilcoxon equivalent). Input variables were the difference to detect of 1, alpha error 0.05, and power of 0.8. Because of lack of prior information for variability, we used conservative data for the standard deviation (SD), i.e., 3. The minimum sample size was estimated to be 49 for alpha error of 0.05 and 73 for alpha error of 0.01. However, to get best estimates for sample size estimates, especially the variability in differences for the scores for future studies, we performed the study in 100 patients. PASS 2008 version 08.0.1 for windows was used to facilitate sample size estimation (Hintz J [2008] PASS 2008, NCSS, LLC, Kaysvillie, Utah).
Statistical analysis
Descriptive statistics were calculated for continuous variables as mean, standard deviation (mean ± SD), median, and interquartile range and for categorical variables as frequency distribution and percentage (n [%]). Student's paired t-test for continuous variables distributed normally, marginal homogeneity test for ordered categorical variables and Chi-square test and Fisher's exact test when the expected cell values were <5. Categorical variables were used to compare the two intubating positions. P < 0.05 was regarded as statistically significant. Statistical analysis was carried out using Statistical Package for Social Sciences (SPSS) Software (Version 17.0, SPSS, Inc, Chicago, IL, USA).
Results
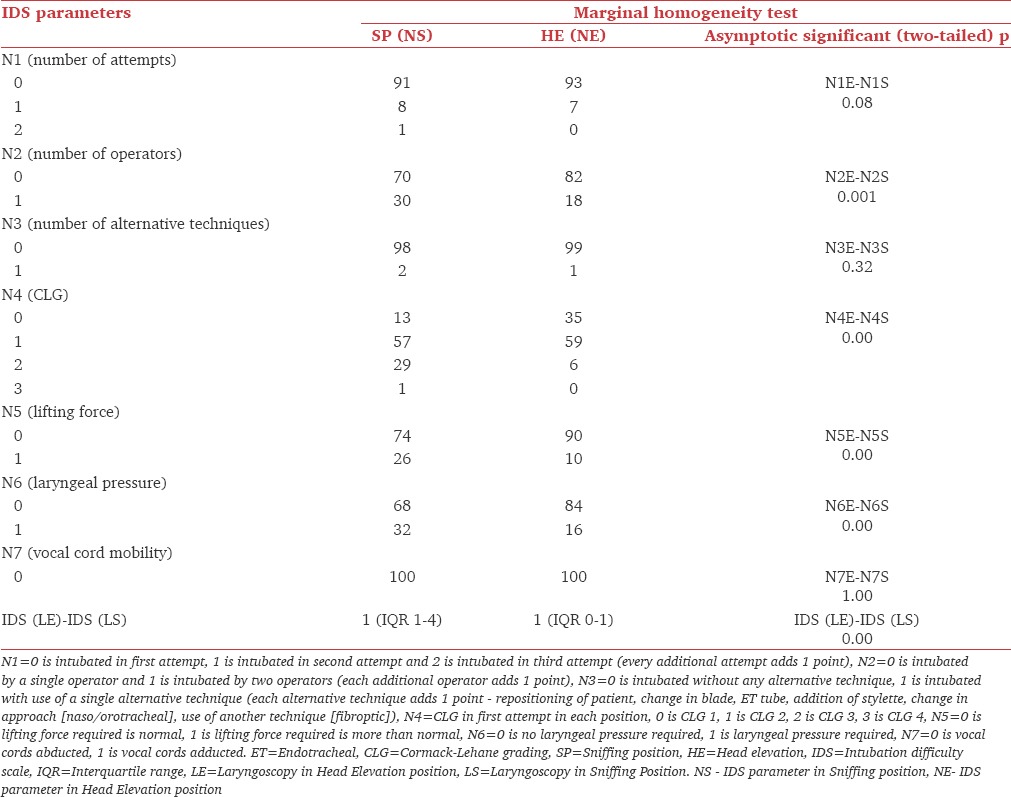
All the 100 patients were analyzed. There were no dropouts during the study. CONSORT flow diagram of the study was shown in [Figure 1]. Demographic parameters were charted [Table 1]. The IDS variables were compared between both intubating positions using marginal homogeneity test and their statistical significance was shown in the Table 2.
Figure 1.
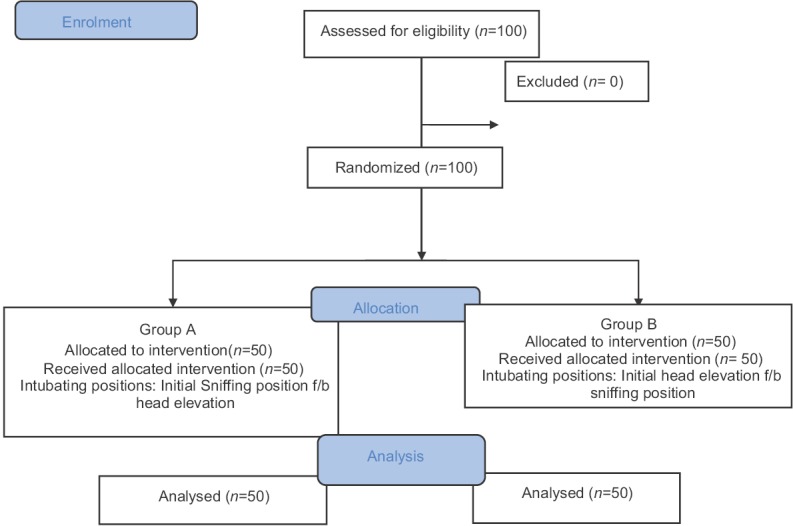
CONSORT flow diagram
Table 1.
Patient characteristics
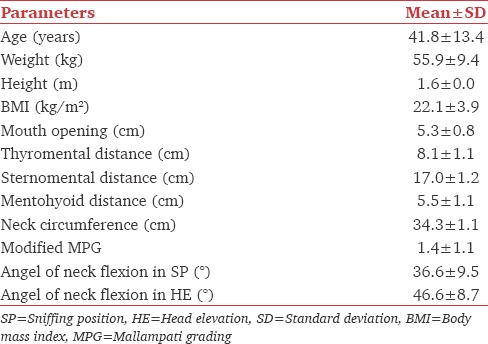
Table 2.
Intubation difficulty scale variables in two groups with P values
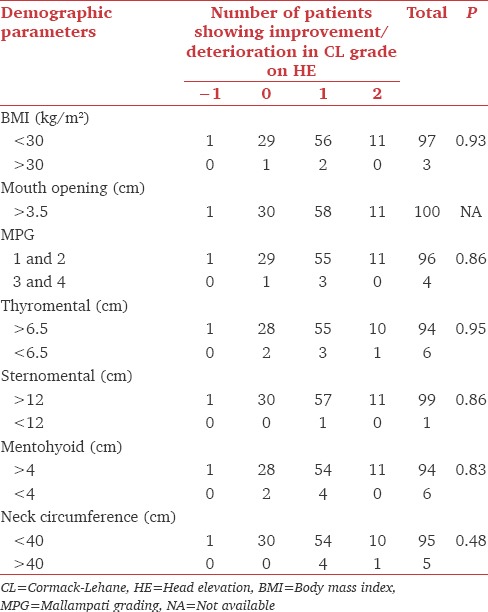
Further, analysis of number of grades of improvement in laryngeal view by HE in respect to each parameter are shown in [Table 3]. We observed that out of 97 patients with BMI <30 kg/m2, in 11 patients there was improvement by two grades (i.e. CLG regressed by 2), and in 56 patients there was improvement by 1 grade, no improvement was observed in 29 participants. Whereas, in 3 patients with BMI >30 kg/m2, 1-grade improvement was observed in two patients and no change of view in one patient. Moreover, similarly, improvement in number of CLG on further HE was shown with reference to mouth opening, Mallampati grading, thyromental distance, sternomental distance, mentohyoid distance, and neck circumference were shown in the Table 3. In our study, one patient showed deterioration in CLG by 1, but he was intubated successfully in the first attempt.
Table 3.
Change in number of grades of Cormack-Lehane upon head elevation for each parameter
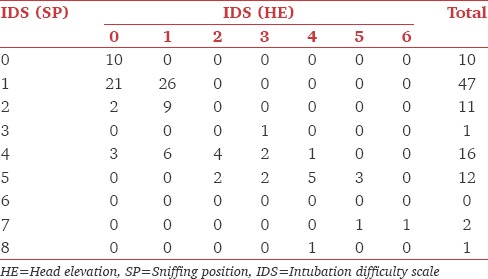
Changes in CLG from SP to HE are shown in Table 4. There were 13 patients with Cormack-Lehane view of 1 in sniffing as well as in HE. In 26 patients who were in CLG 2a, there was improvement to CLG 1 in 18 patients, remained in same grade in seven patients, and one patient worsened to 2b. Of 32 patients who were in grade 2b, four patients improved to CLG 1 and 23 improved to CLG 2a and five remained in same grade. Of 28 patients who were in Grade 3, 7 improved to 2a, 16 improved to 2b and 5 patients remained in same grade. One patient in grade 4 improved to Grade 3. Similarly improvement in IDS from SP to HE were cross-tabulated and shown in Table 5.
Table 4.
Cross tabulation of Cormack-Lehane grading in sniffing position and head elevation
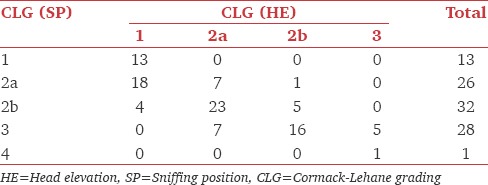
Table 5.
Change in intubation difficulty scale from sniffing position to head elevation
Discussion
Glottis visualization is key to the success of direct laryngoscopy and intubation. Optimal position of the patient's head and neck at the time of laryngoscopy and intubation can improve the outcome. The results of the present study showed better visualization of glottis, improvement in CLG (P = 0.00), and superior IDS (P = 0.00) on further flexion of the neck over SP during direct laryngoscopy and tracheal intubation in patients requiring general anesthesia. This was in agreement with Levitan et al.[7] who studied on seven cadavers using a straight laryngoscopy blade and concluded that increasing HE and laryngoscopy angle (neck flexion) significantly improves percentage of glottic opening (POGO) scores during laryngoscopy. In another study by Adnet et al.,[8] where they compared the SP with simple head extension for laryngoscopic view reported no significant advantage of SP in improvement of glottic visualization. Lee et al.[9] examined laryngeal exposure in the head-flat position and in the 25° backup position in 40 nonobese adult patients. The authors reported an improvement in the POGO score from 42.2% in the head-flat position to 66.8% in the backup position. However, glottic exposure alone may not be a complete representative for intubation difficulty. Hence, we evaluated IDS,[4] which was not done in any of these studies.
Although it is believed that in the SP the oral, pharyngeal, and laryngeal axes are aligned, in the present study as CLG was improved (P = 0.00) and lifting force (P = 0.00) of the laryngoscopic blade required was less suggesting better alignment of these axes in further neck flexion. However, Adnet et al.[4] using magnetic resonance imaging, found that it is not possible to achieve anatomic alignment of the laryngeal, pharyngeal, and the mouth axes in the neutral, simple head extension, or the SP. However, the limitation of this study was it involved nonanesthetised individuals and laryngoscope blade was not used.
This study was designed to apply IDS to objectively assess the effect of dynamically increasing HE and associated neck flexion on the quality of laryngeal view and ease of intubation. Quantifying the amount of HE in each patient is difficult to dynamically measure, so we used a standard 1.5-inch (≅3.80 cm) pillow over standard SP. Lifting the patient's head, however, also changes the directional force along the laryngoscope handle, as well as the operator's angle of view down the lumen of the blade. Choosing the same laryngoscopist to perform all laryngoscopies minimizes this bias.
Our study results showed significant advantage of further HE over SP in obtaining better intubating conditions. The total IDS was better in patients with HE position as compared to SP (P = 0.00). Of the seven variables of IDS, N2 (number of operators) (P = 0.001), N4 (CLG) (P = 0.00), N5 (Lifting force) (P = 0.00), and N6 (laryngeal pressure) (P = 0.00) have gained statistical significance. This is inconsistence with Hochman and coauthors,[10] who studied the effects of neck positioning, on the force required for optimal laryngeal exposure. They concluded that increasing HE and neck flexion increased the incidence of full laryngeal exposure with less required force. In our study, a significant number of patients intubated in the SP required more than one operator, external laryngeal manipulation, and use of increased force during laryngoscopy compared to those intubated in the HE position.
SP is traditionally considered as a standard position for intubation. Horton et al.[11] measured the angle of neck flexion in standard SP. The mode value of angle was 35° to the horizontal. In our study, mean angle of neck flexion in SP was 36.56° and in further HE was 46.62°, which improved the glottic visualization.
Crossover design of the study helped us to eliminate interindividual variation, but it was associated with additional airway manipulation. However, major airway trauma or sore throat were absent in this study.
An important limitation of this study was failure to blind observers due to obvious differences in head position. Study has less number of patients with predictors of difficult airway.
Conclusions
We conclude that HE/further flexion of the neck is better in respect to glottic visualization, number of operators, laryngeal pressure, and lifting force required for intubation over standard SP as assessed by IDS. Hence, HE position was found to be statistically and clinically significant over standard SP.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Prakash S, Rapsang AG, Mahajan S, Bhattacharjee S, Singh R, Gogia AR. Comparative evaluation of the sniffing position with simple head extension for laryngoscopic view and intubation difficulty in adults undergoing elective surgery. Anesthesiol Res Pract. 2011;2011:297913. doi: 10.1155/2011/297913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greenland KB, Edwards MJ, Hutton NJ. External auditory meatus-sternal notch relationship in adults in the sniffing position: A magnetic resonance imaging study. Br J Anaesth. 2010;104:268–9. doi: 10.1093/bja/aep390. [DOI] [PubMed] [Google Scholar]
- 3.Schmitt HJ, Mang H. Head and neck elevation beyond the sniffing position improves laryngeal view in cases of difficult direct laryngoscopy. J Clin Anesth. 2002;14:335–8. doi: 10.1016/s0952-8180(02)00368-9. [DOI] [PubMed] [Google Scholar]
- 4.Adnet F, Borron SW, Racine SX, Clemessy JL, Fournier JL, Plaisance P, et al. The intubation difficulty scale (IDS): Proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology. 1997;87:1290–7. doi: 10.1097/00000542-199712000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Rao SL, Kunselman AR, Schuler HG, DesHarnais S. Laryngoscopy and tracheal intubation in the head-elevated position in obese patients: A randomized, controlled, equivalence trial. Anesth Analg. 2008;107:1912–8. doi: 10.1213/ane.0b013e31818556ed. [DOI] [PubMed] [Google Scholar]
- 6.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–11. [PubMed] [Google Scholar]
- 7.Levitan RM, Mechem CC, Ochroch EA, Shofer FS, Hollander JE. Head-elevated laryngoscopy position: Improving laryngeal exposure during laryngoscopy by increasing head elevation. Ann Emerg Med. 2003;41:322–30. doi: 10.1067/mem.2003.87. [DOI] [PubMed] [Google Scholar]
- 8.Adnet F, Baillard C, Borron SW, Denantes C, Lefebvre L, Galinski M, et al. Randomized study comparing the “sniffing position” with simple head extension for laryngoscopic view in elective surgery patients. Anesthesiology. 2001;95:836–41. doi: 10.1097/00000542-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Lee BJ, Kang JM, Kim DO. Laryngeal exposure during laryngoscopy is better in the 25 degrees back-up position than in the supine position. Br J Anaesth. 2007;99:581–6. doi: 10.1093/bja/aem095. [DOI] [PubMed] [Google Scholar]
- 10.Hochman II, Zeitels SM, Heaton JT. Analysis of the forces and position required for direct laryngoscopic exposure of the anterior vocal folds. Ann Otol Rhinol Laryngol. 1999;108:715–24. doi: 10.1177/000348949910800801. [DOI] [PubMed] [Google Scholar]
- 11.Horton WA, Fahy L, Charters P. Defining a standard intubating position using “angle finder”. Br J Anaesth. 1989;62:6–12. doi: 10.1093/bja/62.1.6. [DOI] [PubMed] [Google Scholar]


