Abstract
Background and Aims:
Efficacy of epidural analgesia depends on placement of the epidural catheter at the appropriate level. Manual palpation using surface landmarks to identify the desired intervertebral level may not be a reliable method. Ultrasonography (USG) is an alternative technique but requires training and may increase procedure time. The objective of this study was to compare the accuracy of ultrasound (US) imaging with manual palpation for locating the intervertebral level.
Material and Methods:
We included postoperative adult patients without an epidural catheter who were scheduled to have a chest radiograph in the recovery room. A radio-opaque marker was placed at random at an intervertebral space along the thoracic or lumbar spine of the patient (in the field of the chest radiograph). The level of intervertebral space corresponding to the radio-opaque marker was determined by palpation technique by one anesthetist. Two other anesthetists (A and B) blinded to the result of manual palpation, independently used USG to determine the level of intervertebral space. A consultant radiologist assessed the radiographs to determine the correct position of the marker, which was judged to be the accurate space.
Results:
We recruited a total of 71 patients, of which 64 patients were included in the final analysis. Accurate identification by manual method was 31/64 (48%), by US A was 27/64 (42%) and by US B was 22/64 (34%). The difference in accuracy between manual palpation and US imaging was not statistically significant (P = 0.71).
Conclusion:
US imaging may not be superior to manual palpation for identifying intervertebral level.
Keywords: Epidural, intervertebral level, ultrasound
Introduction
The technique of epidural anesthesia has come a long way since 1949 when Manuel Martinez Curbelo used a Tuohy needle and a small urethral catheter to provide continuous lumbar epidural anesthesia.[1] Better understanding of physiology, equipment, and newer drugs has made epidural, a safe, and reliable technique for use in the perioperative period. To minimize adverse effects such as sensorimotor blockade and also to improve mobility in the immediate postoperative period, a lower concentration of local anesthetic is preferred for analgesia. The efficacy of epidural analgesia therefore depends on the precise placement of epidural catheter. Conventionally, manual palpation method using anatomical surface landmarks is used to identify the desired intervertebral space. This has been questioned and may not be a reliable method.[2] Ultrasonography (USG) has established a niche in various aspects of medical fields and is often preferred over computed tomography and magnetic resonance imaging because of its noninvasiveness, relatively inexpensive and with no associated radiation hazards. USG can be used as an alternative to or in addition to manual palpation method to identify the intervertebral space to place the epidural catheter.[3,4,5,6,7] However, it requires training and some degree of competence and skill to understand the sonoanatomy and may increase duration of the procedure. The depth of epidural space has been studied in the past; however, the use of USG for identification of the intervertebral space has not been studied before.[4] Hence, we conducted this study to compare the accuracy of ultrasound (US) imaging with manual palpation for locating the intervertebral space.
The objective of this study was to compare the accuracy of US imaging with manual palpation for locating the intervertebral level.
Material and Methods
Design
This was a prospective nonrandomized crossover study conducted at a tertiary care cancer center. The study was approved by Institutional Review Board of our institute. This study was registered in clinical trial registry-India (CTRI/2014/08/004923). Written informed consent was obtained from all patients recruited in the study.
Participants
All adult patients more than 18 years of age, who were scheduled to have a chest X-ray in the postoperative period, were included in the study. Patients with epidural catheter in situ were excluded to prevent an anesthetist involved in the study from guessing the possible interspace level based on the location of the epidural catheter and the surgery performed. Age, height, weight, and body mass index (BMI) were recorded for all patients included in the study.
Assessments and interventions
An anesthetist not involved with USG, before the chest X-ray was taken, randomly placed a radio-opaque marker in any one intervertebral space in the area to be covered by chest X-ray. There were two groups of assessors, manual palpation group (Group A) and US group (Group B). Group A consisted of three anesthetists with each having a minimum of 5-year experience and regularly performed epidural catheter placement. Group A anesthetist determined the level of intervertebral space corresponding to the radio-opaque marker by the manual palpation method. For the manual palpatory method, the patient was examined in the lateral position, with the neck and legs flexed. The most prominent spinous process in the nape of the neck was considered as C7 and the intervertebral spaces were counted caudally in the thoracic region. A horizontal line was drawn between the inferior angles of the scapulae. If the spinous process was palpated along this horizontal line drawn, it is predicted to be T7. Furthermore, to countercheck, the L4 vertebra was identified using Tuffier's line (line joining the highest points of the iliac crests) and the spinous processes were counted in cephalad direction till the marked intervertebral space [Figure 1].
Figure 1.
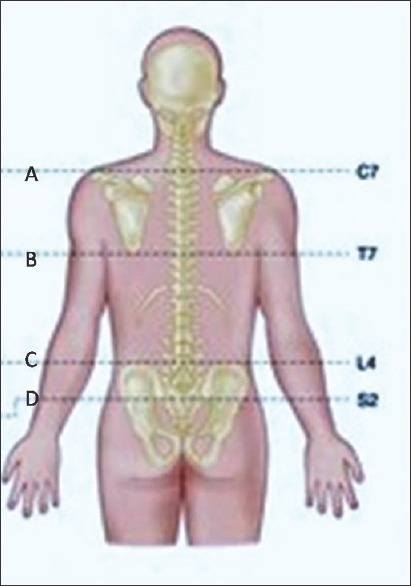
Anatomical landmarks (A) Line passing through C7 vertebra. (B) Line passing through inferior angle of the scapula (T7). (C) Tuffier's line through the highest point on iliac crest (L4). (D) Line passing through posterior superior iliac spine (S2)
Group B (US imaging group) consisted of two anesthetists (Anesthetist X and Anesthetist Y) who were trained and proficient in US imaging. Both the anesthetists participating in this study had at least 5 years’ experience with the use of USG and use it routinely in their practice.
Anesthetist X and Y were blinded to the result of manual palpation and independently used USG to determine the level of marker corresponding to the intervertebral space. They used sonosite M-Turbo (Sonosite™ Inc., Bothell, WA, USA) with curved array low-frequency probe (2-5MHz) for its wide field of view and deeper penetration. An initial depth setting was adjusted to 10 cm; however, depth, focus, and gain settings were adjusted as needed during the scanning process to produce an optimal image. Since this study was performed in postoperative recovery room, all patients were scanned in lateral position. Standard procedure of identification and counting of vertebrae was followed. Liberal amounts of US gel were applied to the skin over the lumbar region and maintaining a parasagittal oblique view; probe was slid in a caudad direction until a horizontal hyperechoic line of the sacrum was visualized. The gap between the line of sacrum and the saw-tooth appearance of the L5 lamina was taken as L5– S1 intervertebral space. This was followed by identification of other interspaces by moving cephalad from lumbosacral interspace and thus identifying the level of the radio-opaque marker.
Group C consisted of a consultant radiologist with a minimum of 5 years’ experience in radiology. The level of intervertebral space determined by the radiologist was considered as the correct position of the marker and assumed to be a gold standard for the purpose of this study. We compared the level of intervertebral space identified by Groups A and B with that obtained from Group C. We also recorded the interspace level deviations in both groups A and B from the correct interspace identified by the radiologist.
Outcome measures
The primary outcome was to compare the accuracy of determining the level of intervertebral space using palpation technique versus USG. The secondary outcome measure was to find out the existence of interobserver variability when using USG.
Statistical analysis and sample size calculation
We assumed accuracy of 30% in manual palpation group and 60% in USG group based on previous studies. To achieve 90% power and an alpha error of 0.05, a sample size of 64 was needed to detect 30% difference between the groups. Statistical test used for the study was 2-sided Fisher's exact test. Results are expressed as percentages. The following agreement between assessments such as (a) between manual palpation and radiological assessment, (b) between US and radiological assessment, and (c) inter-observer agreement between the two US operators was studied using Cohen's kappa statistics.
Results
We recruited a total of 71 patients in this study, of which the radio-opaque marker was not visualized on chest radiograph in seven patients. For the study, X-rays not showing the markers were not repeated. A total of 64 patients were included in the final analysis.
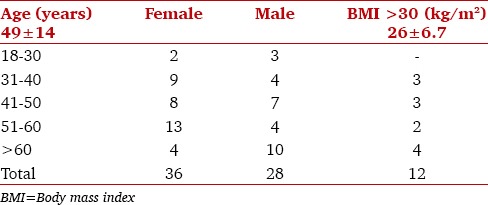
The mean age of patients was 49 years, height was 159 cm, weight was 64 kg, and BMI was 26 kg/m2. Male-to-female ratio was 28/36 [Table 1].
Table 1.
Demographic data
In our study, we found that accurate identification by manual method was 31/64 (48%), by US A was 27/64 (42%) and by US B was 22/64 (34%). The difference in accuracy between manual palpation and US imaging was not statistically significant (P = 0.71).
A total of 24/64 (37.5%) in manual methods, 30/64 (46.9%) in USG A, and 30/64 (46.9%) the marker was identified as one space higher or lower than the actual level [Table 2].
Table 2.
Identification of intervertebral space by ultrasound (ultrasonography) or manual method
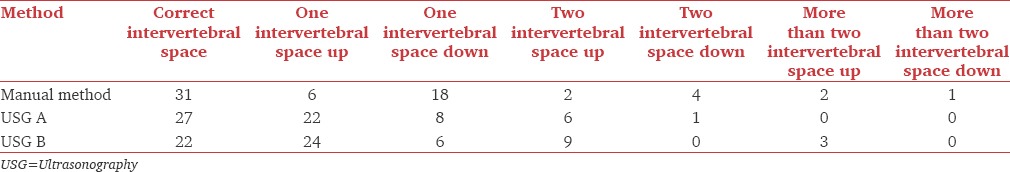
We found that the marker was identified as more than one space away from the correct interspace in nine patients in the manual group, seven in USG A, and 12 in USG B group.
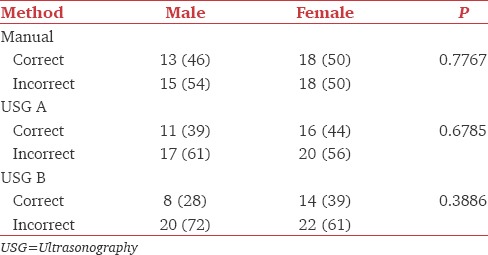
In a subgroup of obese patients (BMI ≥30 kg/m2) (post hoc analysis), there was no difference with 5 out of 12 (P = 1) accurate identification in both manual and US groups. Furthermore, there was no difference in accuracy based on gender [Table 3 – Gender subgroup analysis, post hoc analysis].
Table 3.
Gender subgroup analysis (post hoc analysis)
Discussion
Identification of correct intervertebral space is essential as epidural analgesia is one of the components of balanced anesthesia and also the mainstay of postoperative analgesia. Conventionally, the intervertebral space is identified using bony anatomical landmarks such as Tuffier's line or spinous process of seventh cervical vertebra, and the desired interspace is located with manual palpation cephalad or caudad, respectively. Surgical site dictates the level of the intervertebral space for epidural catheter placement. To ensure a functionally adequate epidural both in the intraoperative and postoperative period, the intervertebral space should be identified correctly. This can at times be challenging and technically difficult in some patients particularly in anatomical abnormalities, obese, and elderly. In addition, there can be considerable interpersonnel variability in identification of the intervertebral space level.
US of the lumbar spine is currently widely used in the field of anesthesiology to help perform epidural anesthesia.[3,4,5,6,7,8,9,10,11] The concept of using US for visualization of epidural space was first described by Cork et al.[3] Currie first described the measurement of the depth to the extradural space using US and found that there was a high degree of correlation between these measurements and the subsequent depth of insertion of the Tuohy needle.[4] US imaging is non-invasive, safe and its use in anesthesia is rapidly expanding, but there are limitations with this technique. Balki stated that incorporating the use of lumbar spine US scanning into day-to-day clinical practice may improve the ease of performing epidurals as well as add to patient safety and comfort.[7] There are very few clinicians with the expertise to use US to guide central neuraxial blocks. US through a promising modality with broadening range of application in the field of anesthesia presents with a certain degree of difficulty when it comes to the spine. Anatomically, the spinal cord/epidural space is protected by a very complex, articulated encasement of bones, ligaments, and adjacent muscles that have homogeneous density. This not only makes the US of spine challenging but also demands a certain degree of technical skill and proficiency.
Our aim in conducting this study was to compare the accuracy of determining the level of intervertebral space using palpation technique versus USG by comparing it with a gold standard (i.e. X-ray).
In our study, manual method was found to be more accurate (48%) than US (42% - operator A, 34% - operator B) though not statistically significant, in identifying the correct intervertebral space. There were differences in the accuracy between the two US operators as well (42% vs. 34%). Both of these could be attributed to the difficulty encountered during the use of US for imaging of the spine which is challenging as previously mentioned. Furthermore, the structures needed to be visualized are located deeper than the other structures which the anesthetists are familiar with the US (peripheral nerve blocks and central lines).
Our accuracy for correct identification in USG group was significantly lower (42%/34% accuracy) than that found by Furness et al. (71% accuracy).[8] Furness et al. showed that US imaging predicted the correct level significantly more accurately (71%) than palpation for identifying intervertebral level (30%).[8] Watson et al. found the accuracy of US to be 76% in identifying the correct interspace.[9] In contrast, our study showed that manual palpation was more accurate (48%) than what was previously reported by Broadbent et al.(29%).[2]
Whitty et al. found in their study that there was poor agreement between palpation and US estimation of the specific lumbar interspace, and when there was disagreement, the US estimate was more often higher than the palpation estimate. However, they did not compare palpation and US to a “gold standard” imaging technique (e.g., radiograph).[10]
A systematic review and meta-analysis of US imaging for lumbar punctures and epidural catheterizations done by Shaikh et al. showed US imaging as a useful adjunct which can reduce multiple attempts, risk of failed or traumatic lumbar punctures, and epidural catheterizations.[11]
Obese patients can introduce additional degree of difficulty in both the techniques, US and manual palpation. Abnormal curvature of the spine obscures the anatomical landmarks which are necessary for correct localization of the intervertebral space. Similarly, manual palpation is more difficult and unpredictable in obese patients. For USG, image quality depends on how much adipose tissue exists between the skin and the tip of the spinous process as when the depth increases for penetration of the US beam the image quality may be inaccurate. With respect to obese patients, there are studies which have shown US to be superior than manual methods, but our study shown no such difference.[6]
Grau et al. studied the usefulness of USG in epidural catheter placements in patients with presumed difficult epidural punctures, 30% of whom were obese parturients and found that in these patients with US measurement of the epidural space depth the quality of epidural anesthesia was enhanced.[6]
On basis of the results of our study, we can recommend that currently, US-guided central neuraxial blocks should only be performed by practitioners who have a sound knowledge of spinal sonoanatomy. In the rest, US-guided central neuraxial blocks may be used to complement manual palpation while identifying the intervertebral space.
The strengths of our study were that this was a crossover study. This eliminated bias caused by patient variability. Furthermore, we used X-rays along with the expertise of a radiologist which is the gold standard in identifying the correct interspace.
The limitations of our study were that the US was performed by anesthesiologists and not radiologists. There is a learning curve and considerable interindividual difference in expertise associated with US. However, if US is to be used for this procedure, it will always be an anesthesiologist and not a radiologist performing the procedure due to practical and logistic reasons inside an operation theatre.
The second limitation is that the spine anatomy would change to some extent with the position of the patient. The palpation and US were both performed in lateral position with lumbar flexion whereas the chest X-ray was taken in the supine position with no flexion at lumbar spine.[12]
Conclusion
US imaging may not be superior to manual palpation for identifying intervertebral level. Anesthetists should not assume that a spinal or epidural needle is at the interspace they believe it to be. In future, it is expected that US technology is likely to make this procedure simpler, more accurate, and widely applicable. Additional studies by anesthesiologists to establish the role of US in performing central neuraxial blocks keeping in mind uniform positioning in all the groups which are needed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Waurick K, Waurick R. History and technique of epidural anaesthesia. Anasthesiol Intensivmed Notfallmed Schmerzther. 2015;50:476–82. doi: 10.1055/s-0041-100845. [DOI] [PubMed] [Google Scholar]
- 2.Broadbent CR, Maxwell WB, Ferrie R, Wilson DJ, Gawne-Cain M, Russell R. Ability of anaesthetists to identify a marked lumbar interspace. Anaesthesia. 2000;55:1122–6. doi: 10.1046/j.1365-2044.2000.01547-4.x. [DOI] [PubMed] [Google Scholar]
- 3.Cork RC, Kryc JJ, Vaughan RW. Ultrasonic localization of the lumbar epidural space. Anesthesiology. 1980;52:513–6. doi: 10.1097/00000542-198006000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Currie JM. Measurement of the depth to the extradural space using ultrasound. Br J Anaesth. 1984;56:345–7. doi: 10.1093/bja/56.4.345. [DOI] [PubMed] [Google Scholar]
- 5.Darrieutort-Laffite C, Hamel O, Glémarec J, Maugars Y, Le Goff B. Ultrasonography of the lumbar spine: Sonoanatomy and practical applications. Joint Bone Spine. 2014;81:130–6. doi: 10.1016/j.jbspin.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 6.Grau T, Leipold RW, Conradi R, Martin E. Ultrasound control for presumed difficult epidural puncture. Acta Anaesthesiol Scand. 2001;45:766–71. doi: 10.1034/j.1399-6576.2001.045006766.x. [DOI] [PubMed] [Google Scholar]
- 7.Balki M. Locating the epidural space in obstetric patients-ultrasound a useful tool: Continuing professional development. Can J Anaesth. 2010;57:1111–26. doi: 10.1007/s12630-010-9397-y. [DOI] [PubMed] [Google Scholar]
- 8.Furness G, Reilly MP, Kuchi S. An evaluation of ultrasound imaging for identification of lumbar intervertebral level. Anaesthesia. 2002;57:277–80. doi: 10.1046/j.1365-2044.2002.2403_4.x. [DOI] [PubMed] [Google Scholar]
- 9.Watson MJ, Evans S, Thorp JM. Could ultrasonography be used by an anaesthetist to identify a specified lumbar interspace before spinal anaesthesia? Br J Anaesth. 2003;90:509–11. doi: 10.1093/bja/aeg096. [DOI] [PubMed] [Google Scholar]
- 10.Whitty R, Moore M, Macarthur A. Identification of the lumbar interspinous spaces: Palpation versus ultrasound. Anesth Analg. 2008;106:538–40. doi: 10.1213/ane.0b013e31816069d9. [DOI] [PubMed] [Google Scholar]
- 11.Shaikh F, Brzezinski J, Alexander S, Arzola C, Carvalho JC, Beyene J, et al. Ultrasound imaging for lumbar punctures and epidural catheterisations: Systematic review and meta-analysis. BMJ. 2013;346:f1720. doi: 10.1136/bmj.f1720. [DOI] [PubMed] [Google Scholar]
- 12.Lin N, Li Y, Bebawy JF, Dong J, Hua L. Abdominal circumference but not the degree of lumbar flexion affects the accuracy of lumbar interspace identification by Tuffier's line palpation method: An observational study. BMC Anesthesiol. 2015;15:9. doi: 10.1186/1471-2253-15-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


