Abstract
Background:
To assess the clinical consequences of AcrySof toric intraocular lens (IOL) and Hoya toric IOL implantation to correct preexisting corneal astigmatism in patients undergoing cataract surgery.
Materials and Methods:
In this study, we examined 55 eyes of 45 patients with at least 1.00 D corneal astigmatism who were scheduled for cataract surgery. After phacoemulsification, toric IOL was inserted and axis was aligned. We observed the patients, uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), keratometry, manifest refraction, and IOL axis alignment 6 months after surgery.
Results:
After 6 months, the UDVA was 0.17 ± 0.17 logMAR in the AcrySof group and 0.17 ± 0.18 logMar in the Hoya group. More than 78% of eyes in the AcrySof group and 80% of eyes in the Hoya toric IOL achieved a UDVA of 20/40 or better. In the AcrySof group, the mean preoperative corneal astigmatism was 2.73 ± 0.92 D. The mean postoperative refractive astigmatism was 0.84 ± 0.63 D. In the Hoya group, the preoperative corneal astigmatism was 2.58 ± 0.76 D and the postoperative refractive astigmatism was 0.87 ± 0.66 D (P < 0.05). The mean AcrySof IOL axis rotation was 1.88° ± 3.05°. In the Hoya group, the mean axis rotation was 1.53° ± 3.66°. All changes in visual and refractive data before and after surgery were statistically significant (P < 0.05). There was no significant difference between the two groups regarding refractive and visual outcome after surgery (P > 0.05 for all).
Conclusion:
Implantation of AcrySof toric IOL and Hoya toric IOL was an effective way to correct preexisting corneal astigmatism in cataract surgery.
Keywords: Cataract surgery, corneal astigmatism, toric intraocular lens
Introduction
Cataract and astigmatism are two common reasons of visual loss in the world. The first cause of cataract is aging, but other reasons include systemic diseases such as diabetes mellitus, ocular trauma, drugs (such as steroids), radiotherapy, and congenital and hereditary anomaly diseases.[1]
Cataract surgery by replacement of the innate lens with an artificial intraocular lens (IOL) is the most commonly used surgical technique worldwide.[2] Toric IOLs were presented by Shimizu et al. in 1994 to correct preexisting corneal astigmatism.[3] Nearly 60% of cataractous eyes have at least 0.75 D of corneal astigmatism.[2,4] Correction of corneal astigmatism can be achieved with various techniques including selective location of the phacoemulsification incision, corneal relaxing incisions, limbal relaxing incisions, or excimer laser keratectomy. All these methods have restrictions including the amount of astigmatism that can be treated and long-term mechanical instability.[5] Toric IOLs offer a more stable and predictable method for correction of pre-existing corneal astigmatism.[6]
Previous studies have reported the clinical results of implantation of different forms of toric IOL.[5,6,7,8,9] Effective visual outcomes depended on both careful alignment of the toric IOL with its proposed axis and insignificant postoperative rotation. Nearly 3% of cylindrical power is lost for every 1° of rotation from the axis.[3] The aim of this prospective study is to assess the refractive and visual consequences of the AcrySof toric IOL (Alcon, Fort Worth, TX, USA) and Hoya toric IOL (Hoya, Naka-Ochiai, Shinjuku-ku, Tokyo, Japan) implantation in cataract patients with astigmatism, and to compare the results of these two IOLs.
Patients and Methods
In the present study, we examined 55 eyes of 45 patients who underwent cataract surgery with placement of AcrySof toric IOL and Hoya toric IOL between 2011 and 2013.
The criteria for consideration were visually significant cataract that needed surgery and regular astigmatism, documented with topography, of more than 1.00 D. The exclusion criteria were irregular astigmatism, macular degeneration and retinal disease, history of glaucoma, corneal disease, previous corneal or intraocular surgery, and history of ocular inflammation.
For all patients, we performed complete ophthalmic examinations before cataract surgery, including slit-lamp examination, tonometry with Goldmann applanation tonometer, ophthalmoscopy with dilated pupil, and manifest and cycloplegic refraction if possible. Elevation based topography (Scheimpflug Pentacam; OCULUS Optikgerate GmbH, Wetzlar, Germany) was done to rule out irregular astigmatism for all patients. Keratometry and axial length were measured with automated keratometer (IOLMaster; Carl Zeiss Meditec Jena, Germany).
Furthermore, logMAR corrected distance visual acuity (CDVA) and uncorrected distance visual acuity (UCDA) were measured for all patients. For each eye, in order to define the axis of IOL and proper IOL model, we entered preoperative patient information such as steep and flat k values and their axis to online toric IOL calculator, as proposed by the manufacturer (www.acrysoftoriccalculator.com, www.hoyatoriccalculator.com). SRK/T formula was used for spherical IOL power for emmetropia in all patients. Phacoemulsification was done by two skilled surgeons under topical anesthesia. Before each cataract surgery, the horizontal meridian of the cornea was marked by use of ink in an upright position. On the operating bed, IOL axis was marked on the cornea by means of Mendez gauge and toric marker. Phacoemulsification was done through a 2.8-mm clear corneal incision. After phacoemulsification, toric IOL was injected into the capsular bag and IOL was rotated carefully to align the cylinder axis with signed steep meridian. IOL axis alignment was checked again after softly washing the ophthalmic visco-surgical device (OVD).
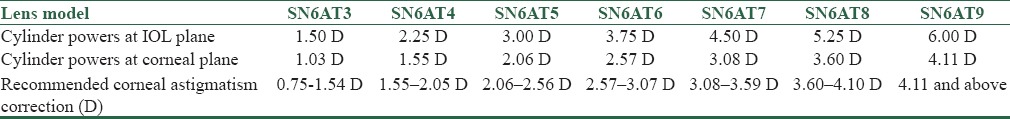
There are seven types of AcrySof toric IOL: SN6AT3, SN6AT4, SN6AT5, SN6AT6, SN6AT7, SN6AT8, and SN6AT9. AcrySof toric IOL has been approved by Food and Drug Association (FDA) for seven cylindrical powers, 1.50 D, 2.25 D, 3.00 D, 3.75 D, 4.50 D, 5.25 D, and 6.00 D, at the IOL plane.
The manufacture's information about all the lens models, cylindrical powers, and suggested corneal astigmatism correction range is presented in Table 1. The IOL has a 6.00 mm diameter and an overall length of 13.0 mm. The lens power ranges from +6.0 to +30.0 D.[10]
Table 1.
AcrySof toric intraocular lens (IOL) models
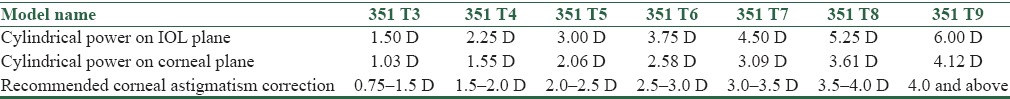
Models of Hoya toric IOL are shown in Table 2. The IOL has 6.00 mm diameter and a total length of 12.5 mm.[11]
Table 2.
Hoya toric intraocular lens (IOL) models
All patients were examined 1 day and 6 months postoperatively. After 6 months, we checked them for UCDA and CDVA with Snellen chart, refraction, keratometry, and IOL axis alignment. For evaluation of rotational stability, manifest refraction was measured 1 day and 6 months after surgery and presumed rotation was calculated with the use of vector analysis.
Statistical analysis
All data were collected in an Excel database (Microsoft Office 2003) and analyzed using SPSS for Windows (version 16.0; SPSS Inc., Chicago, IL, USA). Decimal uncorrected distance visual acuity (UDVA) and CDVA were converted into logMAR for the mathematical and statistical calculations. Paired samples t-tests were used to analyze visual acuity and astigmatism parameters within each group. Power vector analysis of astigmatic change (Alpin's method[12]) was used to quantify the contribution of lens to the residual refractive error. P value less than 0.05 was considered statistically significant.
Results
Patients
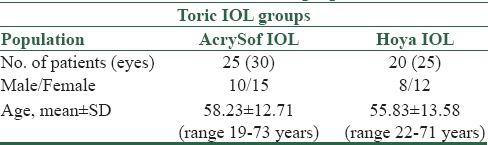
Refractive and corneal astigmatism were analyzed in 30 eyes with an AcrySof toric IOL and in 25 eyes with a Hoya toric IOL. Patient characteristics are presented in Table 3.
Table 3.
Patient demographics
Visual acuity
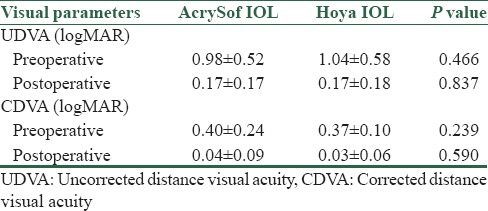
The mean logMAR UCVA significantly improved from 0.98 ± 0.52 and 1.04 ± 0.58 preoperatively to 0.17 ± 0.17 and 0.17 ± 0.18 postoperatively in the AcrySof and Hoya groups, respectively (P < 0.05). At 6 months, more than 78% of the eyes in the AcrySof group achieved a UCVA of 20/40 or better and 80% of eyes in the Hoya group achieved a UCVA of 20/40 or better.
Preoperatively, the mean logMAR CDVA was 0.40 ± 0.24 and 0.37 ± 0.10 in the AcrySof and Hoya groups, respectively. The improvement in CDVA from preoperatively to postoperatively was statistically significant in the two groups (P < 0.05).
The differences in preoperative and postoperative visual acuities between groups were not statistically significant (all P > 0.05). Comparisons of preoperative and postoperative visual parameters are shown in Table 4.
Table 4.
Visual acuity before and after IOL implantation
Refractive and corneal astigmatism
Preoperatively, there were no significant differences in corneal (P = 0.263) and refractive astigmatism (P = 0.152) between the two groups [Table 5].
Table 5.
Preoperative and postoperative astigmatism
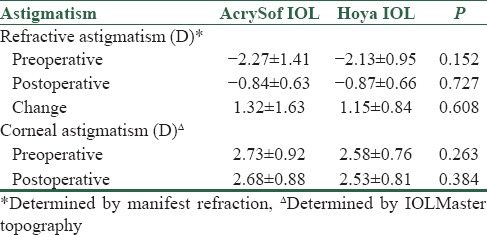
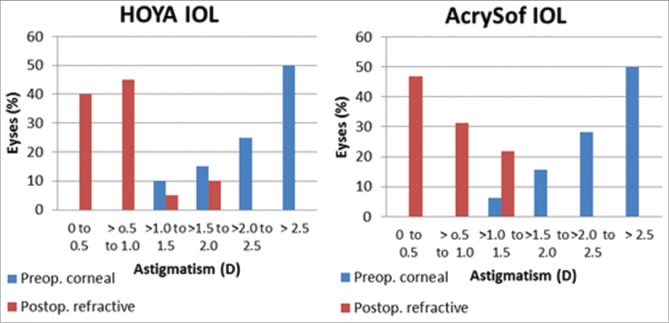
Postoperatively, refractive astigmatism was significantly decreased in AcrySof and Hoya groups (P < 0.05). There were no statistically significant differences between groups in astigmatic outcomes [Table 5]. At 6 months, refractive astigmatism was 0.50 D or less in 46.9% and 40% of eyes, and 1.00 D or less in 78.1% and 85% of eyes in AcrySof and Hoya groups, respectively. The mean residual refractive astigmatism was statistically significantly lower than preoperative corneal values in both groups (P < 0.05) [Figure 1].
Figure 1.
The preoperative corneal astigmatism and 6 months postoperative residual refractive astigmatism in the two groups
Rotational stability
The mean AcrySof IOL axis rotation was 1.88°±3.05° (range 0°–10°). Of the 30 IOL cases assessed 6 months postoperatively, 90.6% were within ±5° of the operation axis and all were within ±10°. No eye had secondary surgery to reposition the IOL axis within 6 months of postoperative assessment in this group.
In the Hoya group, the mean axis rotation was 1.53°±3.66° (range 0°–12°). Of the 25 IOLs assessed, 90% were within ±5° of the operative axis and 96% were within 10°. One IOL (4%) with more than ±10° of rotation at 6 months was rotated 12° from the operative axis. The IOL was repositioned after 6 months.
There was no statistical difference in rotational stability between the two IOL types (P = 0.245).
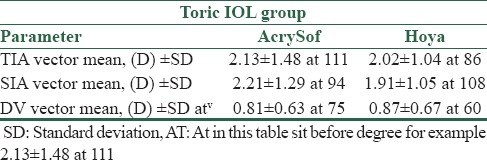
Vector analysis
Table 6 shows the results of the vectorial astigmatism analysis. In the AcrySof toric IOL group, the amount of surgically induced astigmatism (SIA) was not significantly different from the target-induced astigmatism (TIA) (P = 0.158), and difference vector (DV) was different from zero (P = 0.00). In the Hoya toric IOL group, there was no significant difference between SIA and TIA (P = 0.315) and DV was different from zero (P = 0.00).
Table 6.
Vector analysis
Discussion
Using toric IOL to correct corneal astigmatism is a relatively new surgical choice in patients with cataract and previous corneal astigmatism. In this study, we implanted foldable toric AcrySof IOL in 30 eyes of 25 patients and toric Hoya IOL in 25 eyes of 20 patients with preexisting corneal astigmatism of more than 1.00 D. Then, we investigated visual consequence and compared the consequences of the two IOLs.
To our knowledge, this is the first article that compares these two IOLs and also investigates the visual outcome of toric Hoya IOL. The results confirmed that after surgery and implantation of toric IOL, postoperative refractive astigmatism was significantly decreased in AcrySof and Hoya groups (P = 0.00). No significant differences were found between the results of the two groups of patients (P > 0.05). In the AcrySof group with a mean preoperative corneal astigmatism of 2.73 ± 0.92 D, the refractive astigmatism was reduced to 0.84 ± 0.63 D postoperatively. In the other group, preoperative corneal astigmatism and postoperative refractive astigmatism were 2.58 ± 0.76 and 0.87 ± 0.66, respectively, after 6 months. At 6 months, residual refractive astigmatism was 0.50 D or less in 46.9% and 40% of eyes and 1.00 D or less in 78.1% and 85% of eyes in AcrySof and Hoya groups, respectively.
Our results are comparable to those of other studies by different investigators. Ahmed et al.[9] showed the reduction of mean refractive astigmatism after AcrySof implantation from 1.7 ± 0.4 D preoperatively to 0.4 ± 0.4 D postoperatively. In the study that was performed by Mendicute,[7] bilateral implantation of AcrySof was performed; after implantation of AcrySof, the amount of astigmatism reduced from −2.34 ± 1.28 D to −0.72 ± 0.43 D.
De Silva et al.[8] described 65% astigmatic reduction after MicroSil 6116TU toric IOL implantation (mean preoperative corneal astigmatism was 3.08 ± 0.76 D, while the mean refractive astigmatism at 6 months after surgery was 1.23 ± 0.90 D). Zuberbuhler et al.[13] observed that posterior chamber AcrySof toric IOL implantation was an effective choice to correct preexisting astigmatism in cataract surgery. Noel et al.[14] reported residual refractive astigmatism after implantation of AcrySof to be less than 0.75 D in 74% of eyes and less than 1.00 D in 91% of eyes. In Ahmed's study,[9] residual astigmatism was 1.00 D or less in 90% of eyes. Bauer[3] reported 91% of eyes with residual astigmatism of 1.00 D or less.
In the present study, the UDVA achieved after 6 months was 0.17 ± 0.17 logMAR in the AcrySof group and 0.17 ± 0.18 logMAR in the Hoya group. More than 78% of eyes in the AcrySof group and 80% of eyes in the Hoya group achieved a UDVA of 20/40 or better. We found no significant difference between UDVA of patients in the two IOL groups. This outcome shows that these two IOLs provide good correction of UDVA in patients with cataract and corneal astigmatism. We compared our results with those of other studies. In the study conducted by Mendicute et al.,[7] 93.3% of patients achieved 20/40 or better UDVA and 66.6% of eyes achieved 20/25 or better UDVA. Ahmed et al.[9] reported that by using of AcrySof toric IOL, bilateral UDVA improved to 20/40 or better in 99% of patients and 20/20 or better in 63% of them. Noel et al.[14] reported that more than 90% of patients had a UDVA of 20/40 or better after AcrySof IOL implantation. Delsiva et al.[8] reported that more than 79% of eyes had 20/35 or better UDVA after implantation of the MicroSil 6116TU toric IOL. Bauer et al.[14] reported a UDVA of 20/25 in 80% of eyes and 20/40 or better in 90% of patients. Shimuzu et al.[3] reported that the best corrected visual acuity 3 months postoperatively was 20/25 or better in 77% of eyes after implantation of toric IOL.
Rotational stability is very important to reach better visual consequences of toric IOLs. Multiple causes may result in unwanted postoperative IOL rotation. Incomplete washing of OVD and early postoperative IOP (intraocular pressure) fluctuation both result in rotational instability. Most IOLs, rotation occurs in the early postoperative period. When the anterior and posterior capsules are fused, IOL rotation rate decreases.[15,16] IOL model and haptic design play a very important role in the amount of IOL rotation; for example, in Shimuzu's study, 41% of eyes had IOL rotation greater than 10° with C-LOOP haptic.[3]
In our study, after 6 months, the mean AcrySof IOL axis rotation was 1.88° ± 3.05°. In this group, after 6 months, 90.6% of IOL axis was within ±5° of the operation axis and all were within ±10°. In the Hoya group, mean axis rotation was 1.53°± 3.66°, 90% of eyes were within ±5° of operative axis and 95% of them were within ±10°. One eye of this group needed realignment of axis in the operation room. There was no statistically significant difference in the rotational stability between the two IOL types. Other studies showed similar results. Ahmed et al.[9] reported IOL rotation of 5° or less in 91% and 10° or less in 99% of eyes. In Mendicute's study, 77% of eyes had a rotation of 5° or less and 97% of them had 10° or less[7]. Chang et al.[17] also showed that 99% of eyes had 10° or less rotation with AcrySof IOL implantation.
Conclusion
The results of this study show that the implantation of AcrySof toric IOL and Hoya toric IOL is an effective choice to correct preexisting corneal astigmatism in cataract surgery. No significant difference was found in the clinical outcomes of the two IOLs. Further studies with larger samples and longer follow-up should be conducted to compare the efficacy and safety of these IOLs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Agresta B, Knorz MC, Donatti C, Jackson D. Visual acuity improvements after implantation of toric intraocular lenses in cataract patients with astigmatism: A systematic review. BMC Ophthalmol. 2012;12:41. doi: 10.1186/1471-2415-12-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hoffer KJ. Biometry of 7,500 cataractous eyes. Am J Ophthalmol. 1980;90:360–8. doi: 10.1016/s0002-9394(14)74917-7. [DOI] [PubMed] [Google Scholar]
- 3.Shimizu K, Misawa A, Suzuki Y. Toric intraocular lenses: Correcting astigmatism while controlling axis shift. J Cataract Refract Surg. 1994;20:523–6. doi: 10.1016/s0886-3350(13)80232-5. [DOI] [PubMed] [Google Scholar]
- 4.Hoffmann PC, Hütz WW. Analysis of biometry and prevalence data for corneal astigmatism in 23,239 eyes. J Cataract Refract Surg. 2010;36:1479–85. doi: 10.1016/j.jcrs.2010.02.025. [DOI] [PubMed] [Google Scholar]
- 5.Grabow HB. Intraocular correction of refractive errors. In: Kershner RM, editor. Refractive Keratotomy for Cataract Surgery and the Correction of Astigmatism. Thorofare, NJ: Slack Inc; 1994. pp. 79–115. [Google Scholar]
- 6.Mingo-Botín D, Muñoz-Negrete FJ, Won Kim HR, Morcillo-Laiz R, Rebolleda G, Oblanca N. Comparison of toric intraocular lenses and peripheral corneal relaxing incisions to treat astigmatism during cataract surgery. J Cataract Refract Surg. 2010;36:1700–8. doi: 10.1016/j.jcrs.2010.04.043. [DOI] [PubMed] [Google Scholar]
- 7.Mendicute J, Irigoyen C, Aramberri J, Ondarra A, Montés-Micó R. Foldable toric intraocular lens for astigmatism correction in cataract patients. J Cataract Refract Surg. 2008;34:601–7. doi: 10.1016/j.jcrs.2007.11.033. [DOI] [PubMed] [Google Scholar]
- 8.De Silva DJ, Ramkissoon YD, Bloom PA. Evaluation of a toric intraocular lens with a Z-haptic. J Cataract Refract Surg. 2006;32:1492–8. doi: 10.1016/j.jcrs.2006.04.022. [DOI] [PubMed] [Google Scholar]
- 9.Ahmed II, Rocha G, Slomovic AR, Climenhaga H, Gohill J, Grégoire A, et al. Canadian Toric Study Group. Visual function and patient experience after bilateral implantation of toric intraocular lenses. J Cataract Refract Surg. 2010;36:609–16. doi: 10.1016/j.jcrs.2009.10.044. [DOI] [PubMed] [Google Scholar]
- 10.“Acrysof IQ Toric IOL Surgeon Keys for Success and Acknowledgment.” Acrysof IQ Toric IOL Resource Center. [Last accessed on 2014 Jan 01]. Available from: http://www.alconsurgical.com/pdfs/TOR11392MS.pdf/
- 11.Hoya Surgical Optic, Tokyo, Japan. [Last accessed on 2014 Jan 01]. Available from: http://www.hoyasurgicaloptics.com/ap/product/hoya-toric/
- 12.Alpins N. Astigmatism analysis by the Alpins method. J Cataract Refract Surg. 2001;27:31–49. doi: 10.1016/s0886-3350(00)00798-7. [DOI] [PubMed] [Google Scholar]
- 13.Zuberbuhler B, Signer T, Gale R, Haefliger E. Rotational stability of the AcrySof SA60TT toric intraocular lenses: A cohort study. BMC Ophthalmol. 2008;8:8. doi: 10.1186/1471-2415-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bauer NJ, de Vries NE, Webers CA, Hendrikse F, Nuijts RM. Astigmatism management in cataract surgery with the AcrySof toric intraocular lens. J Cataract Refract Surg. 2008;34:1483–8. doi: 10.1016/j.jcrs.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 15.Myers TD, Olson RJ. Comparison of the effects of viscoelastic agents on clinical properties of the Unfolder lens injection system. J Cataract Refract Surg. 1999;25:953–8. doi: 10.1016/s0886-3350(99)00085-1. [DOI] [PubMed] [Google Scholar]
- 16.Pereira FA, Milverton EJ, Coroneo MT. Miyake-Apple study of the rotational stability of the Acrysof toric intraocular lens after experimental eye trauma. Eye (Lond) 2010;24:376–8. doi: 10.1038/eye.2009.150. [DOI] [PubMed] [Google Scholar]
- 17.Chang DF. Comparative rotational stability of single-piece open-loop acrylic and plate-haptic silicone toric intraocular lenses. J Cataract Refract Surg. 2008;34:1842–7. doi: 10.1016/j.jcrs.2008.07.012. [DOI] [PubMed] [Google Scholar]