Abstract
This is the case of a 78-year-old male patient that underwent a cardiac magnetic resonance (CMR) due to shortness of breath. An unanticipated diagnosis of a giant pseudoaneurysm with a “guitar-like” appearance was made and patient was sent for urgent ventriculoplasty. CMR offered striking illustrative images allowing for previously unsuspected diagnosis to be made and patient's therapeutic management modified. Moreover, in this case, we emphasize the paramount importance of differentiating between true aneurysms, pseudoaneurysms, clefts, and diverticuli since each pathology has completely different management and prognosis that vary from benign to potentially fatal if not immediately treated.
Keywords: Acute myocardial infarction mechanical complication, cardiac magnetic resonance, giant pseudoaneurysm
CASE REPORT
A 78-year-old male patient was admitted to hospital due to onset of shortness of breath on exertion over the past month. Patient was diabetic and suffered from chronic obstructive pulmonary disease but had no other cardiovascular risk factors. He has never experienced angina symptoms even though approximately 2 months before admission had experienced some abdominal pain with vomit and fever that lasted for <48 h. At admission, he was tachycardic with an otherwise unremarkable clinical examination. Electrocardiogram showed sinus tachycardia with q wave and ST segment elevation on the lateral leads. Cardiac troponin was mildly elevated but stable during three consecutive measurements over 24 h, and the brain natriuretic peptide was elevated. Transthoracic echocardiogram, due to a very poor acoustic window, was deemed almost inconclusive. Parasternal long axis view and very poor apical views did not show evidence of global systolic dysfunction, significant valve disease, or pericardial effusion. Contrast echocardiography might have provided crucial additional information improving diagnostic accuracy, but at the time, it was not being routinely performed. Therefore, to better characterize cardiac function, a cardiac magnetic resonance (CMR) was arranged.
CMR scan showed a giant pseudoaneurysm [Figure 1] of the lateral wall [Figure 2, arrows] with laminar thrombus [Figure 2, arrowheads] and bilateral pleural effusion [Figure 2, curved arrows]. Pseudoaneurysm with a “guitar-like” appearance [Figure 2, panel A] was expanding in systole [Figure 2, panel B] and restricting in diastole [Figure 2, panel C] causing an ejection fraction of nearly 10% despite normal contractility and viability [Figure 2, panel D] of all other segments. Pseudoaneurysm wall showed no late gadolinium enhancement [Figure 2, panel D] since myocardium was absent and only pericardium was impeding the heart from a lethal rupture.
Figure 1.
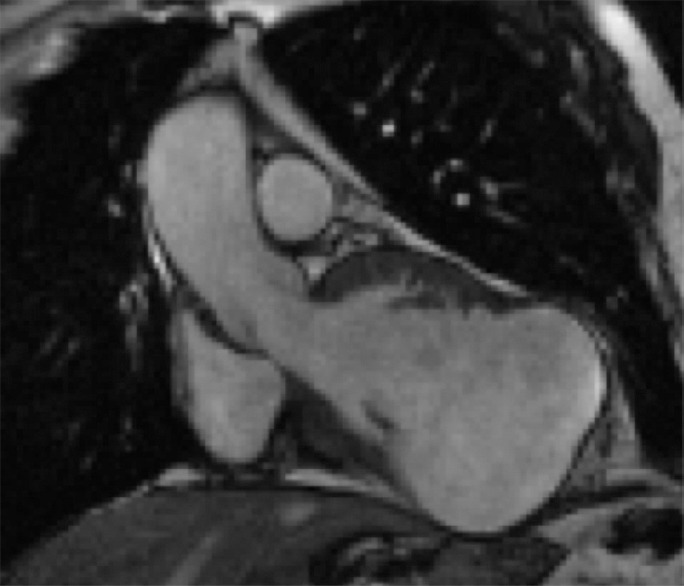
Cardiac magnetic resonance image of a giant pseudo-aneurysm of the lateral wall with a “guitar-like” appearance
Figure 2.
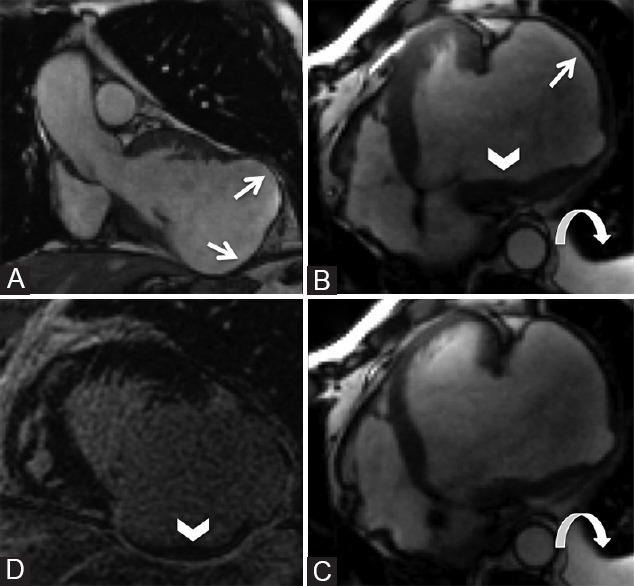
Giant pseudoaneurysm of the lateral wall (arrows) with laminar thrombus (arrowheads) and bilateral pleural effusion (curved arrows). Pseudoaneurysm with a “guitar-like” appearance (panel A) expanding in systole (panel B) and restricting in diastole (panel C) causing an ejection fraction of nearly 10% despite normal contractility and viability (panel D) of all other segments
Urgent coronary angiogram was performed showing proximal left circumflex occlusion with diffuse atherosclerosis but no significant lesions on the other coronary vessels. Cardiac surgery consult was deemed necessary to decide following management. An urgent cardiac surgery was performed that confirmed CMR findings. A big pseudoaneurysm with some thrombotic deposition was observed and was excluded with a Dacron patch. Coronary artery bypass graft was not performed.
DISCUSSION
Cardiac pseudoaneurysms represent a mechanical complication of late reperfused myocardial infarction (MI) with rupture contained only by pericardium. Rupture of the free wall may have catastrophic consequences occurring in 4% of patients after MI and in 23% of those who die of it.[1] Correct differential diagnosis with other myocardial wall abnormalities such as clefts, diverticuli, and true aneurysms are of paramount prognostic importance.
Myocardial clefts (also known as crypts) are described as “V-shaped invaginations”, penetrating >50% into healthy myocardium, obliterating during systole without regional wall motion abnormalities (RWMA).[2] Myocardial diverticuli represent areas of congenital wall weakness characterized by a myocardial outpouching in its entire thickness, without RWMA but extension beyond normal myocardial margins.[3] Both diverticuli and clefts may be seen in healthy individuals or denote an additional sign of congenital heart diseases, such as pentalogy of Cantrell (for diverticuli) or hypertrophic cardiomyopathy (for cleft), representing usually innocent bystanders without need for specific treatment.
True aneurysms on the other hand show a broad neck with a thin aneurysmal wall that develops due to scarring, showing a-or dyskinesia. They usually form as a consequence of an extensive MI, rarely rupture and more often cause thrombus formation, ventricular arrhythmias, or heart failure. Pseudoaneurysms result from MI or thoracic trauma and are a form of a myocardial rupture aborted by the pericardium. Their main characteristic that differentiates them from true aneurysm is that the pseudo-aneurysmal sack is wider than the entrance neck, and the thin wall is formed from pericardium rather than scarred myocardium.
From a CMR point of view, differential diagnosis by means of short and long axis cine images is rather upfront. Early and late gadolinium enhancement sequences are mandatory not only to assess viability and extent/pattern of scar but also to evaluate the presence of thrombosis. In selected occasions and especially when in front of diagnostically challenging cases, a more detailed anatomic imaging may be necessary, including fast spin echo sequences T1 or proton density-weighted and first pass perfusion sequences.
In our case, diagnosis of a pseudoaneurysm was straightforward since entrance neck was wide, but aneurysmal sack was even wider with thin wall, laminar thrombus deposition and complete absence of myocardium. CMR provided a new unsuspected diagnosis and given the unexpected life-threatening findings, scan was completed as soon as all necessary diagnostic information was gathered, and patient was sent for urgent ventriculoplasty.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Pollak H, Nobis H, Mlczoch J. Frequency of left ventricular free wall rupture complicating acute myocardial infarction since the advent of thrombolysis. Am J Cardiol. 1994;74:184–6. doi: 10.1016/0002-9149(94)90098-1. [DOI] [PubMed] [Google Scholar]
- 2.Johansson B, Maceira AM, Babu-Narayan SV, Moon JC, Pennell DJ, Kilner PJ, et al. Clefts can be seen in the basal inferior wall of the left ventricle and the interventricular septum in healthy volunteers as well as patients by cardiovascular magnetic resonance. J Am Coll Cardiol. 2007;50:1294–5. doi: 10.1016/j.jacc.2007.06.026. [DOI] [PubMed] [Google Scholar]
- 3.Aquaro GD, Di Bella G, Strata E, Deiana M, De Marchi D, Pingitore A, et al. Cardiac magnetic resonance findings in isolated congenital left ventricular diverticuli. Int J Cardiovasc Imaging. 2007;23:43–7. doi: 10.1007/s10554-006-9120-9. [DOI] [PubMed] [Google Scholar]


