Abstract
Cardiac paragangliomas are rare tumors of neural crest origin, most frequently seen in the left atrium. There are mixed opinions regarding the most appropriate imaging study for diagnosis and evaluation. We describe the novel utility of 18-F-Fluorodeoxyglucose positron emission tomography/magnetic resonance imaging in the case of a 42-year-old male with cardiac paraganglioma.
Keywords: 18F-Fluorodeoxyglucose positron emission tomography/magnetic resonance imaging, cardiac paraganglioma, neuroendocrine tumor
A 42-year-old male was referred to our hospital with left-sided chest pain. He had a history of smoking, atrial fibrillation, hypertension, and hyperlipidemia. On examination, his vital signs were normal. Physical examination, electrocardiogram, transthoracic echocardiogram, and laboratory tests were normal. Cardiac computed tomography (CT) showed a well-defined mass with intense contrast enhancement located between the left superior pulmonary vein and pulmonary artery, above the left anterior descending artery (LAD), which provided a feeding artery [Figure 1]. To further characterize the mass, we performed a hybrid positron emission tomography/magnetic resonance imaging (PET/MRI) using Philips Ingenuity TF PET/MR (Philips Healthcare, Andover, MA, USA). PET/MRI showed a 3 cm × 1.8 cm epicardial mass abutting the LAD, demonstrating intermediate signal on T1-weighted image, hyperintense signal on T2-weighted image [Figure 2a], and avid contrast enhancement [Figure 2b]. The mass also was hypermetabolic with maximum standard uptake value of 16 [Figure 3a]. There were no hypermetabolic foci in the rest of the body [Figure 3b].
Figure 1.

Axial intravenous contrast-enhanced computed tomography image shows an intensely enhancing well-defined mass (arrow) between the left superior pulmonary vein and the pulmonary artery and abutting the left anterior descending artery
Figure 2.
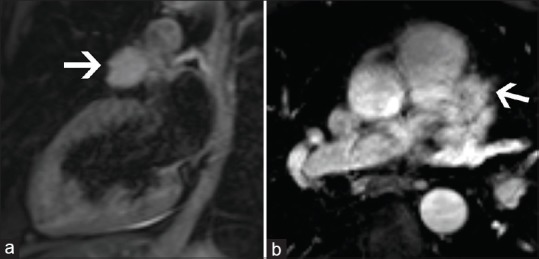
Hybrid 18F-Fluorodeoxyglucose positron emission tomography/magnetic resonance (Philips Ingenuity TF PET/MR Philips Healthcare, Andover, MA, USA) was performed. (a) Vertical long axis T2-weighted magnetic resonance image shows a hyperintense epicardial mass measuring 3 cm × 1.8 cm abutting the left anterior descending artery. (b) Axial postcontrast T1 fat suppressed magnetic resonance imaging shows intense contrast enhancement of the mass
Figure 3.
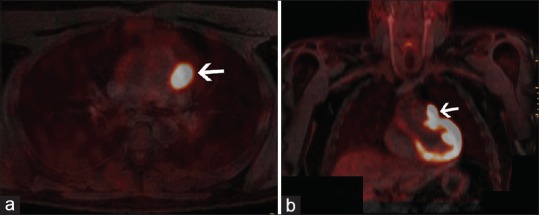
Axial (a) and coronal (b) hybrid 18F-Fluorodeoxyglucose positron emission tomography/magnetic resonance images of the same patient show the mass to be intensely hypermetabolic with standard uptake value of 16. No other hypermetabolic mass is seen to suggest metastatic disease
Based on the location, absence of metastases, signal characteristics, contrast enhancement, and metabolic activity, the diagnosis of paraganglioma was considered along with sarcoma as a less likely differential diagnosis. On cardiopulmonary bypass, the mass was dissected off the epicardium and left pulmonary artery. The feeding artery from the LAD was identified and clipped.
On pathology, there was a faint bluish and tan-red mass with attached tan-yellow soft fatty tissue and measured 2.9 cm × 2.8 cm × 1.9 cm [Figure 4]. Serial sectioning revealed a soft homogeneous red-pink cut surface with no necrosis or hemorrhage. Histology showed a lobulated tumor with well-defined borders. Zellballen cell nests with rich vascular network and intervening fibrous bands with moderate nuclear atypical and salt-and-pepper chromatin pattern were seen, consistent with paraganglioma [Figure 5]. Immunostains for chromogranin and synaptophysin were positive. Immunostain for S-100 was positive in sustentacular cells. The patient was discharged in stable condition 5 days later.
Figure 4.

Gross surgical specimen of faint blue and tan-red muscular soft tissue with attached tan-yellow soft fatty tissue measuring 2.9 cm × 2.8 cm × 1.9 cm
Figure 5.
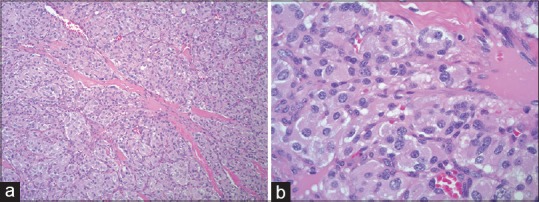
Histopathological image at 100× magnification (a) a tumor with classic Zellballen cell nests with rich vascular network and intervening fibrous bands. The same histopathological image at 400× (b) moderate nuclear atypia with “salt-and-pepper” chromatin pattern. This was consistent with paraganglioma
Discussion
Cardiac paragangliomas are rare tumors (<1%)[1] of neural crest origin originating from visceral paraganglial cells of the left atrium or the aorta.[2] They are most commonly seen in the left atrium, with mean age of 36–40 years, no gender predilection and are functional in 35%–50%.[3] Clinically, these can present without symptoms or with generalized complaints and signs of catecholamine excess.[4] The extreme variability in symptoms suggests a broad differential, which necessitates further investigation. There are many imaging options available, with no standard consensus on the most appropriate studies.
Wang et al. suggest a combination of iodine121/131 labeled metaiodobenzylguanidine (MIBG), MRI, and coronary angiography as the appropriate tools for preoperative diagnosis,[5] while El-Ashry et al. recommend contrast-enhanced CT chest, abdomen and pelvis, cardiac MRI, and MIBG scan.[6] Further, Tomasian et al. report on the potential power of a combination of cardiovascular magnetic resonance with various image acquisition sequences in multiple orientations and PET-CT studies.[3]
To the best of our knowledge, this case is the first reported use of a novel PET/MRI technology in the evaluation of cardiac paraganglioma. PET/MRI is an innovative imaging tool that combines the advantages of two powerful imaging modalities. While MRI has high spatial resolution, tissue characterization capabilities, and can evaluate cardiac function, PET is unparalleled in providing metabolic information. With the use of hybrid PET/MRI, the MRI component helps in characterizing the mass and accurately localizing the tumor and its relationship to adjacent structures including coronary arteries. The PET component provides metabolic information, without the need for a separate examination. MRI also provides attenuation correction information for the PET scan, which is comparable to that of CT attenuation but without the added radiation dose. In addition, with PET/MRI, we were able to exclude metastatic disease in the rest of the body, aligning with the benign nature associated with >90% of paragangliomas. Thus, PET/MRI provides a comprehensive one-stop shop evaluation of cardiac paraganglioma.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Butany J, Nair V, Naseemuddin A, Nair GM, Catton C, Yau T. Cardiac tumours: Diagnosis and management. Lancet Oncol. 2005;6:219–28. doi: 10.1016/S1470-2045(05)70093-0. [DOI] [PubMed] [Google Scholar]
- 2.Orringer MB, Sisson JC, Glazer G, Shapiro B, Francis I, Behrendt DM, et al. Surgical treatment of cardiac pheochromocytomas. J Thorac Cardiovasc Surg. 1985;89:753–7. [PubMed] [Google Scholar]
- 3.Tomasian A, Lai C, Ruehm S, Krishnam MS. Cardiovascular magnetic resonance and PET-CT of left atrial paraganglioma. J Cardiovasc Magn Reson. 2010;12:1. doi: 10.1186/1532-429X-12-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yadav PK, Baquero GA, Malysz J, Kelleman J, Gilchrist IC. Cardiac paraganglioma. Circ Cardiovasc Interv. 2014;7:851–6. doi: 10.1161/CIRCINTERVENTIONS.114.001856. [DOI] [PubMed] [Google Scholar]
- 5.Wang JG, Han J, Jiang T, Li YJ. Cardiac paragangliomas. J Card Surg. 2015;30:55–60. doi: 10.1111/jocs.12455. [DOI] [PubMed] [Google Scholar]
- 6.El-Ashry AA, Cerfolio RJ, Singh SP, McGiffin D. Cardiac paraganglioma. J Card Surg. 2015;30:135–9. doi: 10.1111/jocs.12479. [DOI] [PubMed] [Google Scholar]


