Abstract
The discoid meniscus is a rare anomaly of the knee that affects mostly the lateral meniscus and is often asymptomatic. The osteochondritis dissecans is a disorder of the subchondral bone and articular cartilage and occurs frequently associated with the discoid lateral meniscus. In the present case, we showed the evolution of this association related to surgical treatment. A patient with lateral knee pain and a magnetic resonance depicting a torn discoid lateral meniscus and osteochondritis dissecans of the lateral femoral condyle was treated with partial meniscectomy and meniscal sutures. After 1 year, the symptoms reappeared, and a new meniscal repair was performed to treat a bucket-handle tear, while cartilage was apparently intact. After 4 years, there was a new recurrence of symptoms, and the knee developed a valgus deformity. Cartilage was treated with microfractures, and a subsequent distal femoral osteotomy associated with lateral meniscal scaffold was performed. The patient was followed up clinically, with radiographs and magnetic resonance for 5 years with an improvement of the results up to 2 years and no signs of deterioration of results over time.
Keywords: discoid meniscus, knee, osteochondritis dissecans, meniscal scaffold, cartilage
Introduction
The discoid meniscus is a rare anomaly of the knee that occurs in the younger population, with different symptoms. The discoid meniscus looks larger and has a different histological structure compared with the normal meniscus. 1 2 The first mention appeared in Young 3 and Dickhaut. 4 More frequent is the lateral involvement. The incidence is difficult to define given the frequent asymptomatic presentation. 5 6 7 8 9
The osteochondritis dissecans (OCD) is characterized by the complete or partial separation of a fragment of cartilage and subchondral bone; usually in young patients. 10 Its incidence is relatively low. 11 12 The lateral femoral condyle (LFC) is interested in 13 to 16% of the cases. 10 13 14 The pathogenesis is debated. 10 15 16 17 18 19 20 21 It has been frequently observed the combination of discoid lateral meniscus with the OCD of the LFC. 22 23 24 25
The case report described the evolution of these two diseases as consequence of the treatment in a young patient.
Case Description
A 10-year-old boy complained a right posterolateral knee pain and feeling of giving way of the knee during sports and walking with no history of trauma. Physical examination revealed pain at lateral palpation; the knee was normally aligned and stable, with a full range of motion. Magnetic resonance (MR) showed the presence of an OCD of the LFC. Arthroscopy revealed a longitudinal lesion of the discoid lateral meniscus with posterior detachment. Meniscal regularization and posterior anchorage with one Fast-fix (Smith & Nephew, Andover, Massachusetts, United States) was performed. Cartilage lesions were not observed. After 1 year the knee pain during and after physical activity with effusion reappeared with pain on the lateral compartment. The OCD persisted on MR ( Fig. 1 ). The injured area appeared in area 4 in the anteroposterior radiographic view and in the C region in the sagittal view according to Cahill and Berg. 26 Arthroscopy showed a bucket-handle tear of the lateral meniscus without cartilage pathology; the meniscus was sutured with two Fast-fix, and the parameniscal region was sacrificed to favor bleeding. After 4 years, recurrence of pain occurred mainly under loading conditions with frequent episodes of effusion treated with arthrocentesis and anti-inflammatory therapy. Imaging showed the persistence of OCD of the LFC with the presence of an intra-articular loose body, and 16 degrees of valgus deformity of the knee. Arthroscopy confirmed a grade 4 OCD of the LFC (1 cm × 1.5 cm), almost complete absence of the meniscal body and a loose small cartilaginous fragment that was removed. Because of the limited size of the osteochondral lesion, microfractures were performed. A subsequent limb realignment and scaffolding of the lateral meniscus was planned after finishing the rehabilitation protocol. After 3 months the patient underwent a lateral opening-wedge distal femoral osteotomy (DFO) (7.5 degrees) ( Fig. 2 ) and partial meniscal replacement with a 4.5 cm meniscal scaffold (Actifit; Orteq, London, United Kingdom). The arthroscopic evaluation revealed a partial repair of the osteochondral defect ( Fig. 3 ).
Fig. 1.
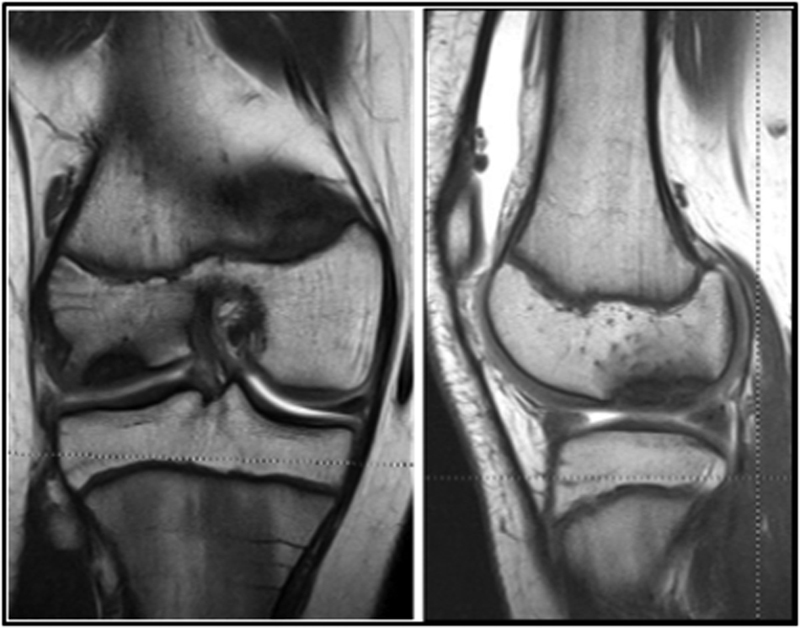
MR scans show OCD of the LFC. LFC, lateral femoral condyle; MR, magnetic resonance; OCD, osteochondritis dissecans.
Fig. 2.
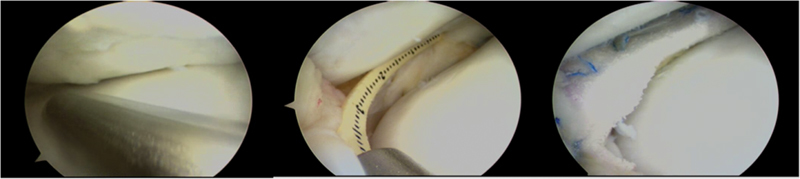
Arthroscopic treatment of meniscal defect with the scaffold. Partial repair of the osteochondral lesion of the LFC can be seen. LFC, lateral femoral condyle.
Fig. 3.

Lateral opening-wedge distal femoral osteotomy.
Clinical assessment before the last surgery with Lysholm and Tegner scores, and the visual analog scale showed 72, 3, and 8 points, respectively. Follow-up evaluations at 1 year (100, 4, and 0 points, respectively) and 2 years (100, 7, and 0 points, respectively) showed a marked clinical improvement with a return to high-impact sports, such as rugby. Subsequent yearly evaluations showed no deterioration of results.
The radiographic evaluation performed at 3 years confirmed the complete healing of DFO and the maintenance of limb alignment. The DFO plate was then removed in combination with a second-look arthroscopy to assess the status of the meniscal scaffold and to perform a biopsy of the scaffold tissue. At the histological evaluation by polarized light microscopy, the scaffold was rich in roundish, large, and active cells, and smaller cell differentiated into chondrocytes; moreover, plasmacytes, macrophages, and rare lymphocytes as related to a foreign body reaction were observed.
Discussion
In 1982, Glasgow 27 first described the relationship between the OCD of the LFC and discoid lateral meniscus. Smillie 21 and Aichroth et al 24 recognized the meniscal tear among the causes OCD, and this association was confirmed in other studies. 25 28 The hypothesis is that damaged discoid meniscus produces abnormal contact forces on the weak growing osteochondral structures. On the contrary, many authors pointed out the association between intact discoid lateral meniscus and OCD of the LFC. 14 25 The peculiar meniscus ultrastructure would lead to an abnormal load transmission. In this context, meniscal regularization would be resolutive. 22
OCD of the LFC has been reported following total meniscectomy for the discoid lateral meniscus. 12 29 30 Therefore, the meniscus may not be a determining factor. Meniscectomy, as known, causes a decrease of the contact area and an increase in pressure peak on the articular surface. In this case, OCD may be a consequence of meniscectomy. However, the OCD does not develop in all growing subjects undergoing meniscectomy so that other factors may be involved. There are no reported similar cases after partial meniscectomy. 31
In some cases, there is a valgus alignment of the knee after meniscectomy, which could lead to a further increase in pressure forces the lateral compartment. 12 30 For this reason, patients who undergo this procedure should be monitored over time.
In our case, the patient came to our attention with an OCD documented only on imaging studies, probably due to the initial involvement of the deeper osteochondral layers. With the evidence of the meniscal tear and the posterior meniscal instability, we proceed to the partial meniscectomy and fixation of the posterior region as suggested. 32 33 34 35
The new meniscal tear confirms that discoid meniscus is weaker than normal 1 2 and this would justify total meniscectomy of torn discoid meniscus, as suggested by some authors. 12 36 However, due to the importance of preserving the lateral meniscus to prevent the progression of osteoarthritis, 37 38 39 40 41 42 43 we tried to preserve as much tissue as possible using meniscal sutures. Although some literature is unanimous on the possible healing of osteochondral lesions after a partial meniscectomy, 22 in our case we observed the persistence of OCD on MR and patient's symptoms and the progression of valgus deformity. It is not possible to define exactly whether the partial meniscal resection determined this condition in such a young and active man or the presence of an abnormal and dysfunctional tissue. The osteochondral lesion highlighted during the third surgery was initially treated with microfracture, which is afunctional, and minimally invasive treatment. 30 However, on considering the young age of the patient, the active level, the progressive alteration of the mechanical axis with lateral overload and the almost complete absence of the lateral meniscus, a subsequent surgery was planned. With DFO, we tried to reduce overloading of the lateral compartment, thus allowing the scaffold implantation and protecting the repaired osteochondral lesion.
A careful follow-up of the patient through multiple clinical and serial radiographic evaluations allowed assessing no recurrence of symptoms, nor the onset of degenerative changes.
References
- 1.Cui J H, Min B H. Collagenous fibril texture of the discoid lateral meniscus. Arthroscopy. 2007;23(06):635–641. doi: 10.1016/j.arthro.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 2.Papadopoulos A, Kirkos J M, Kapetanos G A. Histomorphologic study of discoid meniscus. Arthroscopy. 2009;25(03):262–268. doi: 10.1016/j.arthro.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 3.Young R B. London, United Kingdom: Williams and Nortage; 1889. The external semilunar cartilage as a complete disc. [Google Scholar]
- 4.Dickhaut S C, DeLee J C. The discoid lateral-meniscus syndrome. J Bone Joint Surg Am. 1982;64(07):1068–1073. [PubMed] [Google Scholar]
- 5.Greis P E, Bardana D D, Holmstrom M C, Burks R T. Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg. 2002;10(03):168–176. doi: 10.5435/00124635-200205000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Ikeuchi H. Arthroscopic treatment of the discoid lateral meniscus. Technique and long-term results. Clin Orthop Relat Res. 1982;(167):19–28. [PubMed] [Google Scholar]
- 7.Nathan P A, Cole S C. Discoid meniscus. A clinical and pathologic study. Clin Orthop Relat Res. 1969;64(64):107–113. [PubMed] [Google Scholar]
- 8.Jeannopoulos C L. Observations on discoid menisci. J Bone Joint Surg Am. 1950;32-A(03):649–652. [PubMed] [Google Scholar]
- 9.Dickason J M, Del Pizzo W, Blazina M E, Fox J M, Friedman M J, Snyder S J. A series of ten discoid medial menisci. Clin Orthop Relat Res. 1982;(168):75–79. [PubMed] [Google Scholar]
- 10.Aichroth P. Osteochondritis dissecans of the knee. A clinical survey. J Bone Joint Surg Br. 1971;53(03):440–447. [PubMed] [Google Scholar]
- 11.Lindén B. The incidence of osteochondritis dissecans in the condyles of the femur. Acta Orthop Scand. 1976;47(06):664–667. doi: 10.3109/17453677608988756. [DOI] [PubMed] [Google Scholar]
- 12.Mizuta H, Nakamura E, Otsuka Y, Kudo S, Takagi K. Osteochondritis dissecans of the lateral femoral condyle following total resection of the discoid lateral meniscus. Arthroscopy. 2001;17(06):608–612. doi: 10.1053/jars.2001.19979. [DOI] [PubMed] [Google Scholar]
- 13.Hughston J C, Hergenroeder P T, Courtenay B G. Osteochondritis dissecans of the femoral condyles. J Bone Joint Surg Am. 1984;66(09):1340–1348. [PubMed] [Google Scholar]
- 14.Deie M, Ochi M, Sumen Y et al. Relationship between osteochondritis dissecans of the lateral femoral condyle and lateral menisci types. J Pediatr Orthop. 2006;26(01):79–82. doi: 10.1097/01.bpo.0000191554.34197.fd. [DOI] [PubMed] [Google Scholar]
- 15.Fairbank H AT. Osteochondritis dissacans. Br J Surg. 1933;21:67–82. [Google Scholar]
- 16.Cahill B R, Phillips M R, Navarro R.The results of conservative management of juvenile osteochondritis dissecans using joint scintigraphy. A prospective study Am J Sports Med 19891705601–605., discussion 605–606 [DOI] [PubMed] [Google Scholar]
- 17.Anderson A F, Lipscomb A B, Coulam C. Antegrade curettement, bone grafting and pinning of osteochondritis dissecans in the skeletally mature knee. Am J Sports Med. 1990;18(03):254–261. doi: 10.1177/036354659001800306. [DOI] [PubMed] [Google Scholar]
- 18.Ficat P, Arlet J, Mazières B. Osteochondritis dissecans and osteonecrosis of the lower end of the femur. Value of bone marrow functional exploration [in French] Sem Hop. 1975;51(28):1907–1916. [PubMed] [Google Scholar]
- 19.Caffey J, Madell S H, Royer C, Morales P.Ossification of the distal femoral epiphysis J Bone Joint Surg Am 195840-A03647–654., passim [PubMed] [Google Scholar]
- 20.Mubarak S J, Carroll N C. Familial osteochondritis dissecans of the knee. Clin Orthop Relat Res. 1979;(140):131–136. [PubMed] [Google Scholar]
- 21.Smillie I S. Treatment of osteochondritis dissecans. J Bone Joint Surg Br. 1957;39-B(02):248–260. doi: 10.1302/0301-620X.39B2.248. [DOI] [PubMed] [Google Scholar]
- 22.Yoshida S, Ikata T, Takai H, Kashiwaguchi S, Katoh S, Takeda Y. Osteochondritis dissecans of the femoral condyle in the growth stage. Clin Orthop Relat Res. 1998;(346):162–170. [PubMed] [Google Scholar]
- 23.Irani R N, Karasick D, Karasick S. A possible explanation of the pathogenesis of osteochondritis dissecans. J Pediatr Orthop. 1984;4(03):358–360. doi: 10.1097/01241398-198405000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Aichroth P M, Patel D V, Marx C L. Congenital discoid lateral meniscus in children. A follow-up study and evolution of management. J Bone Joint Surg Br. 1991;73(06):932–936. doi: 10.1302/0301-620X.73B6.1955439. [DOI] [PubMed] [Google Scholar]
- 25.Mitsuoka T, Shino K, Hamada M, Horibe S. Osteochondritis dissecans of the lateral femoral condyle of the knee joint. Arthroscopy. 1999;15(01):20–26. doi: 10.1053/ar.1999.v15.015002. [DOI] [PubMed] [Google Scholar]
- 26.Cahill B R, Berg B C. 99m-Technetium phosphate compound joint scintigraphy in the management of juvenile osteochondritis dissecans of the femoral condyles. Am J Sports Med. 1983;11(05):329–335. doi: 10.1177/036354658301100509. [DOI] [PubMed] [Google Scholar]
- 27.Glasgow M MS, Aichroth P M, Baird P RE. The discoid lateral meniscus: a clinical review. J Bone Joint Surg Br. 1982;64:245. [Google Scholar]
- 28.Fujikawa K, Tomatsu T, Matsu K, Koike A, Tanaka Y, Iseki F. Morphological analysis of meniscus and articular cartilage in the knee joint by means of arthrogram. J Jpn Orthop Assoc. 1978;52:203–215. [Google Scholar]
- 29.Räber D A, Friederich N F, Hefti F. Discoid lateral meniscus in children. Long-term follow-up after total meniscectomy. J Bone Joint Surg Am. 1998;80(11):1579–1586. doi: 10.2106/00004623-199811000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Hashimoto Y, Yoshida G, Tomihara T et al. Bilateral osteochondritis dissecans of the lateral femoral condyle following bilateral total removal of lateral discoid meniscus: a case report. Arch Orthop Trauma Surg. 2008;128(11):1265–1268. doi: 10.1007/s00402-007-0499-0. [DOI] [PubMed] [Google Scholar]
- 31.Baratz M E, Fu F H, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med. 1986;14(04):270–275. doi: 10.1177/036354658601400405. [DOI] [PubMed] [Google Scholar]
- 32.Klingele K E, Kocher M S, Hresko M T, Gerbino P, Micheli L J. Discoid lateral meniscus: prevalence of peripheral rim instability. J Pediatr Orthop. 2004;24(01):79–82. doi: 10.1097/00004694-200401000-00015. [DOI] [PubMed] [Google Scholar]
- 33.Pascarella A, Rava M, Iervolino G, Muscetti R. Menisco discoide laterale apparentemente integro: contributo casistico. GIOT. 2001;27:69–72. [Google Scholar]
- 34.Atay O A, Doral M N, Leblebicioglu G, Tetik O, Aydingoz U. Management of Discoid Lateral Meniscus Tears: Observations in 34 Knees. Arthroscopy. J Relat Surg. 2003;19(04):346–352. doi: 10.1053/jars.2003.50038. [DOI] [PubMed] [Google Scholar]
- 35.Adachi N, Ochi M, Uchio Y, Kuriwaka M, Shinomiya R. Torn discoid lateral meniscus treated using partial central meniscectomy and suture of the peripheral tear. Arthroscopy. 2004;20(05):536–542. doi: 10.1016/j.arthro.2004.01.028. [DOI] [PubMed] [Google Scholar]
- 36.Schenck R C, Jr, Goodnight J M. Osteochondritis dissecans. J Bone Joint Surg Am. 1996;78(03):439–456. [PubMed] [Google Scholar]
- 37.Lee D H, Kim T H, Kim J M, Bin S I. Results of subtotal/total or partial meniscectomy for discoid lateral meniscus in children. Arthroscopy. 2009;25(05):496–503. doi: 10.1016/j.arthro.2008.10.025. [DOI] [PubMed] [Google Scholar]
- 38.Bargar W L, Moreland J R, Markolf K L, Shoemaker S C, Amstutz H C, Grant T T. In vivo stability testing of post-meniscectomy knees. Clin Orthop Relat Res. 1980;(150):247–252. [PubMed] [Google Scholar]
- 39.Levy I M, Torzilli P A, Gould J D, Warren R F. The effect of lateral meniscectomy on motion of the knee. J Bone Joint Surg Am. 1989;71(03):401–406. [PubMed] [Google Scholar]
- 40.Levy I M, Torzilli P A, Warren R F. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64(06):883–888. [PubMed] [Google Scholar]
- 41.Radin E L, de Lamotte F, Maquet P. Role of the menisci in the distribution of stress in the knee. Clin Orthop Relat Res. 1984;(185):290–294. [PubMed] [Google Scholar]
- 42.Fairbank T J. Knee joint changes after meniscectmy. J Bone Joint Surg. 1848;30:664–670. [PubMed] [Google Scholar]
- 43.Walker P S, Erkman M J. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. 1975;(109):184–192. doi: 10.1097/00003086-197506000-00027. [DOI] [PubMed] [Google Scholar]


