Abstract
In the CNS, iron in several proteins is involved in many important processes such as oxygen transportation, oxidative phosphorylation, myelin production, and the synthesis and metabolism of neurotransmitters. Abnormal iron homoeostasis can induce cellular damage through hydroxyl radical production, which can cause the oxidation and modification of lipids, proteins, carbohydrates, and DNA. During ageing, different iron complexes accumulate in brain regions associated with motor and cognitive impairment. In various neurodegenerative diseases, such as Alzheimer’s disease and Parkinson’s disease, changes in iron homoeostasis result in altered cellular iron distribution and accumulation. MRI can often identify these changes, thus providing a potential diagnostic biomarker of neurodegenerative diseases. An important avenue to reduce iron accumulation is the use of iron chelators that are able to cross the blood–brain barrier, penetrate cells, and reduce excessive iron accumulation, thereby affording neuroprotection.
Introduction
Iron is involved in many fundamental biological processes in the brain including oxygen transportation, DNA synthesis, mitochondrial respiration, myelin synthesis, and neurotransmitter synthesis and metabolism.1 Iron homoeostasis is needed to maintain normal physiological brain function, whereas misregulation of iron homoeostasis can cause neurotoxicity through different mechanisms. Homoeostatic mechanisms provide the conditions for optimum cell function by maintaining an equilibrium of available iron concentrations between cellular compartments and buffering molecules, and preventing toxic effects caused by excessive concentrations of free iron.2,3 When iron concentrations exceed the cellular iron sequestration capacity of storage proteins or other molecules, the concentration of iron in the labile iron pool (panel) can increase, which could be harmful and lead to oxidative damage and cell death.4
In healthy ageing, selective accumulation of iron occurs in several brain regions and cell types, with iron mainly bound within ferritin and neuromelanin (panel).5,6 However, the accumulation of iron in specific brain regions, greater than that reported in healthy ageing, occurs in many neurodegenerative diseases and is often associated with oxidative stress and cellular damage. Whether the iron accumulation noted in neurodegenerative diseases is a primary event or a secondary effect is unclear. Ageing is the major risk factor for neurodegeneration. Age-related accumulation of iron might be an important factor that contributes to neurodegenerative processes.
The development of diagnostic and therapeutic strategies involves the use of disease-specific animal models and non-invasive imaging approaches, such as MRI and ultrasound imaging (sonography). In this Review, we discuss the cellular and molecular distribution of iron in healthy brains as they age, summarising factors that might be responsible for age-dependent increases of iron in different areas of the human brain; dysregulation of iron homeostasis in prevalent neurodegenerative diseases, including Alzheimer’s disease, Parkinson’s disease, and multiple sclerosis; iron accumulation in less prevalent disorders such as Friedreich’s ataxia, aceruloplasminaemia and neuroferritinopathy (both categorically referred to as neurodegeneration with brain iron accumulation), Huntington’s disease, and restless legs syndrome; the use of iron chelators as a potential therapy for the aforementioned diseases and disorders; and finally, discuss advances in mapping brain iron distributions with high-field MRI.
Regulation of cellular iron
Peripheral iron uptake
Iron released as ferrous iron from specific cells (ie, macrophages, hepatocytes) via ferroportin, is oxidised by ferroxidase ceruloplasmin and binds to circulating apo-transferrin (panel); in enterocytes, hephaestin, a ceruloplasmin analogue, might have this role.7 Peripheral cellular iron uptake mainly involves endocytosis of the diferric transferrin–transferrin receptor 1 (TFR1; panel) complex; iron is then transported from the endosomes into the cell cytoplasm via the divalent metal ion transporter 1 (DMT1; panel). Iron enters the intracellular labile iron pool, some of which will be incorporated into iron-containing proteins (for energy metabolism in mitochondria) or stored in ferritin, as a soluble, non-toxic, bioavailable form; additionally, iron can be stored in lysosomes within ferritin and haemosiderin.1,2,8
Ferroportin transports ferrous iron out of some cells (eg, hepatocytes, enterocytes, macrophages) to bind circulating apo-transferrin after oxidation by ceruloplasmin or other related ferroxidases, such as hephaestin. Circulating hepcidin (panel) regulates systemic iron homoeostasis by interacting with ferroportin when iron is abundant, which results in ferroportin internalisation and degradation, thereby blocking iron exportation from cells.3 As circulating iron concentrations decrease, hepcidin synthesis decreases, and iron exportation by ferroportin resumes.1,9,10
In many mammalian tissues (eg, hepatocytes and macrophages), cellular iron homoeostasis is regulated at the level of the translation of the mRNAs of proteins involved in iron metabolism, such as TFR1, DMT1, ferritin, and ferroportin.11 Two cytosolic iron sensors, the iron regulatory proteins (IRPs) IRP1 and IRP2 (panel; appendix), regulate iron metabolism post-transcriptionally.12
Brain iron uptake
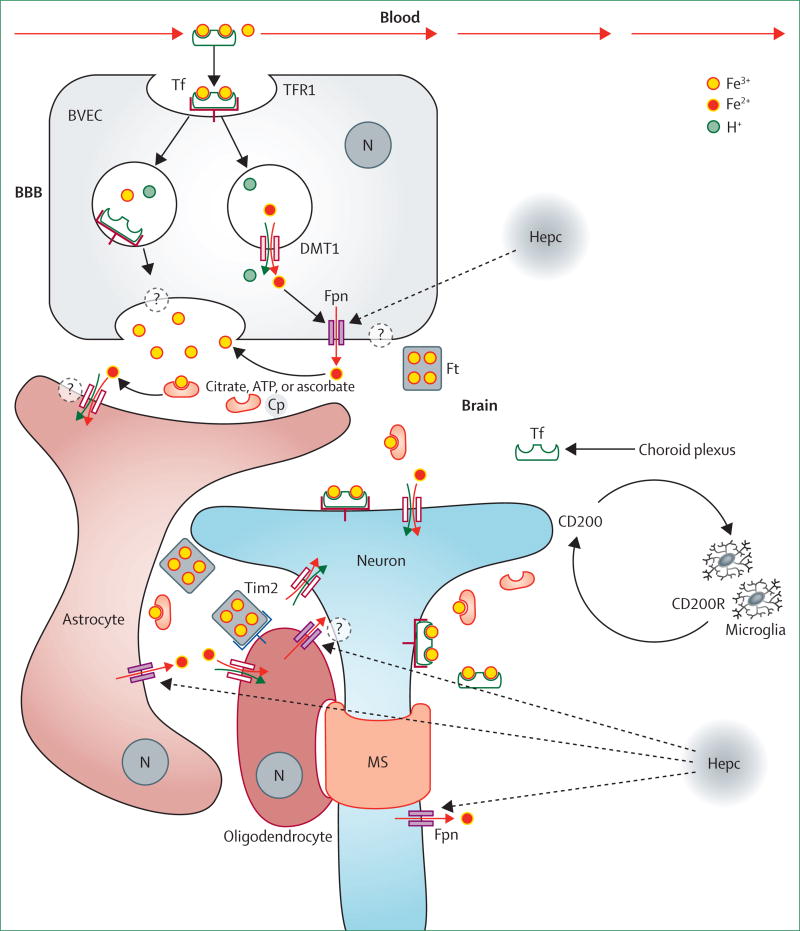
Figure 1 summarises present understanding of iron homoeostasis in the brain. Iron crosses the vascular endothelial cells of the blood–brain barrier, mainly bound to transferrin via the transferrin–TFR1 system; TFR1 is highly expressed on the luminal side of endothelial cells.20 Iron released into the cytoplasmic iron pool is thought to then be exported at the abluminal membrane by unknown pathways, which might involve ferroportin or other transporters. Iron released in the extracellular compartment could then be taken up by other cells, such as astrocytes and neurons, either as low molecular weight complexes (eg, citrate, ATP, ascorbate) or after binding to transferrin via the transferrin–TFR pathways in neurons.16 Iron continually moves between neurons, microglia, and astrocytes, but how these cells acquire and release iron is not fully understood.21
Figure 1. Brain iron metabolism.
Iron enters the endothelial cells of the blood–brain barrier as a low molecular weight complex, or via transferrin receptor-1 mediated endocytosis of transferrin, or independently as non-transferrin-bound iron.13–16 Transferrin receptors line the lumen of the brain and bind circulating differic–transferrin facilitating iron uptake into brain vascular endothelial cells via receptor–mediated endocytosis. Whether there is a DMT1–ferroportin-independent pathway to release ferric iron or differic-transferrin by exocytosis of recycling endosomes is unclear (vesicular export pathway, left side in brain vascular endothelial cells). Transferrin is synthesised by the choroid plexus or oligodentrocytes so that any ferric iron released from the abluminal side of the endothelial cells can form complexes with transferrin or alternatively low molecular weight molecules (eg, ascorbate, citrate, or ATP) to form non-transferrin-bound iron. Citrate and ATP can be released from the astrocytes. Whether there is a DMT1–ferroportin-dependent (non-vesicular export, right side in brain vascular endothelial cells) pathway to release ferrous iron, which would be rapidly converted to ferric iron via ceruloplasmin in the abluminal membranes, is also unknown. The glycosylphosphatidylinositol-anchored form of ceruloplasmin is highly expressed by astrocytes in the mammalian CNS and is physically associated with ferroportin.17 Astrocytes are ideally positioned to take up iron from the circulation and distribute it to other cells in the CNS. Astrocytes have the iron influx and efflux mechanisms needed for cell-to-cell transport of iron. DMT1 is expressed by astrocytes and probably mediates iron influx into these glial cells.17 Iron can be stored as ferritin in astrocytes and exported by a mechanism that involves ferroportin and ceruloplasmin.18 Oligodentrocytes might take up iron via the ferritin receptor Tim-2, or non-transferrin-bound iron via DMT1, or other non-vesicular iron import mechanisms. Neurons and microglia can influx iron via transferrin–transferrin receptor mediated uptake and efflux iron via ferroportin. IRPs (1 and 2), DMT1, and −IRE DMT1 (non-IRE form of DMT1 protein) are expressed mostly by astrocytes. Increased iron regulatory proteins expression might lead to increased expression of the +IRE form of DMT1.19 The role of hepcidin in orchestrating the regulation of egress from cells via ferroportin in different brain cells remains unclear. Neuron axons are wrapped with the myelin sheath, which is made of oligodendrocytes in an iron-dependent manner. Microglia form an association with neurons via CD200/CD200R to maintain the quiescent state. Microglia might take up iron via transferrin receptor and release iron via ferroportin. Dashed lines represent unknown regulation of iron. Solid arrows show iron movement. Reproduced and adapted from Mills and colleagues,8 by permission of Future Science. BBB=blood–brain barrier. TFR=transferrin receptor. Tf=transferrin. Fe2+=ferrous iron. Fe3+=ferric iron. BVEC=brain vascular endothelial cells. Cp=ceruloplasmin. Fpn=ferroportin. DMT1=divalent metal ion transporter 1. Ft=ferritin. IRP=iron regulatory protein. IRE=iron responsive or regulatory element. Hepc=hepcidin. N=nucleus. MS=myelin sheath. ?=unknown pathway or mechanism. CD200=OX-2 membrane glycoprotein. CD200R=CD200 receptor.
Transferrin is synthesised in the brain by the choroid plexus and by oligodendrocytes, but is only secreted in the choroid plexus.16 Neurons are thought to acquire most of their iron via the transferrin–TFR system, and it is likely that they can export iron via ferroportin because many neurons co-express TFR and ferroportin.22 Iron needs to be transported down the axons of neurons to synapses, although the mechanisms are unknown.23 IRPs and iron responsive elements (IREs) regulators are present in the brain, although their role in brain iron homoeostasis is unclear. Gene knock-out studies on mice have shown that IRP2 is particularly important in cellular iron homoeostasis.24
Because the perivascular end-foot processes of astrocytes ensheath the abluminal membrane of the blood–brain barrier25 and form direct connections to neurons, astrocytes are thought to play a key part in regulating brain iron absorption.18 Astrocytes do not express TFR, but might take up iron at the blood–brain barrier via DMT1, which is expressed at the end-foot processes associated with the blood–brain barrier.26 Ferroportin and glycophosp hatidylinositol-anchored ceruloplasmin (the ferroxidase that oxidises ferrous iron) constitute the major efflux pathway in astrocytes.27 An absence of ceruloplasmin can result in iron accumulation in the brain and neurodegeneration.17
Large amounts of iron, needed for axon myelination, are present in oligodendrocytes.28,29 Oligodendrocytes might extract iron from adjacent blood vessels30 or uptake it from interstitial ferritin through the ferritin receptor.16 Little is known about iron metabolism in microglia but, in the course of microglial activation, iron uptake is thought to increase and iron exportation is down-regulated.31,32 Iron is mostly found as ferritin and transferrin in oligodendrocytes,28,33 whereas, in astrocytes and microglia the iron form remains undefined.29
During neuroinflammation, glial cells are activated, which perturbs iron homoeostasis.34,35 In-vitro studies show that short-term stimulation (by use of tumour necrosis factor α, interleukin 6, or lipopolysaccharide) for up to 18 h increases iron accumulation in neurons and microglia (assayed by atomic absorption spectroscopy) but not in astrocytes. This accumulation is associated with changes in the two iron transporters, DMT1 and ferroportin; stimulated hippocampal neurons showed substantial increases in DMT1 and decreased concentrations of ferroportin, whereas microglia showed increased DMT1 protein concentrations but no changes in ferroportin. No change in iron content was detected in astrocytes, although DMT1 increased after stimulus, and only lipopolysaccharide induced a small decrease in ferroportin concentrations.36 These results suggest that changes in ferroportin concentrations do not necessarily change the efflux of iron from cells. Moreover, hepcidin concentrations rapidly increased in astrocytes and microglia after activation with the inflammatory stimuli, although hepcidin was undetectable in neurons. After 6 h, secreted hepcidin provoked a decrease of ferroportin in astrocytes, microglia, and neurons and an increase in DMT1 in microglia. To summarise, inflammatory stimuli and hepcidin induced iron accumulation in only neurons and microglia.36
Iron changes in brain ageing
Increased concentrations of total iron with ageing might be caused by several factors that include increased blood–brain barrier permeability, inflammation, redistribution of iron within the brain, and changes in iron homoeostasis.37,38 Ageing processes might compromise the iron homoeostatic system,39 leading to an excess of iron that is not efficiently chelated by storage proteins or other molecules. The accumulation of iron in neurons might induce damage by apoptosis. Glial iron accumulation can also induce an inflammatory state through an increased release of pro-inflammatory cytokines40 and result in a self-propelling cycle of neuroinflammation and neurodegeneration.41
Total iron concentrations increase with age in the substantia nigra, putamen, globus pallidus, caudate nucleus, and cortices6,42–44 but why this increase is selective for some areas of the brain is unclear. Regional distribution of total iron in a healthy adult brain is heterogeneous; the highest iron concentrations were detected in the basal ganglia (putamen, globus pallidus, and caudate nucleus), whereas low concentrations were detected in the cortical grey matter, white matter, midbrain, and cerebellum, and the lowest iron concentrations were in the pons, locus coeruleus, and medulla.6,43,45–47 Regional heterogeneity of brain iron and its change with age have both been confirmed in vivo by MRI.48–51 Other changes that occur with age include the distribution of iron between its various molecular forms (ferritin, neuromelanin, transferrin, haemosiderin, and others) and the distribution between neurons and glial cells, all of which are only partly understood.28
Detailed human studies on the effects of ageing on the accumulation of iron, neuromelanin, and ferritin have been made in the substantia nigra and locus coeruleus.5,6 These studies provide an important base to investigate the role of iron in the neurodegenerative mechanisms of Parkinson’s disease, which prinicipally involves substantia nigra and locus coeruleus. In healthy individuals, total iron concentration in the locus coeruleus remains stable throughout life and is lower than in the substantia nigra, in which there is a linear increase in total iron concentration with age.6,52 In the substantia nigra, ferritin heavy chain and ferritin light chain concentrations increase with age, whereas these are constant in the locus coeruleus; therefore iron could contribute to neurodegeneration in the substantia nigra more than in the locus coeruleus.5,6 Neuromelanin is present in neurons as neuromelanin-iron complexes in which the iron content varies depending on the neurons in each brain area.6,53 Concentration of neuromelanin-iron complex, which is the dominant form of iron in catecholaminergic neurons, increases with age in the substantia nigra and locus coeruleus.6 Iron histochemistry of healthy aged substantia nigra showed many deposits of reactive ferric iron in glial cells and neuromelanin-free neurons by Perls’ staining. In neuromelanin-containing neurons, reactive ferric iron deposits were not observed by Perls’ staining, because iron is sequestered by neuromelanin into a stable complex, as shown by electron paramagnetic resonance and Mössbauer spectroscopy.5,6,21 The amount of neuromelanin-iron complexes increases with age in neurons of the premotor cortex, putamen, and cerebellum, thus showing increased mobilisation of iron in these neurons during ageing. However, the amount of intraneuronal iron bound to neuromelanin varies in the neurons of different brain regions.53
There is an increased pro-inflammatory state in the brains of the elderly. Glial cell numbers increase in the normal ageing brain, and there is increased immunoreactivity of astrocytic and microglial markers. At the same time, the permeability of the blood–brain barrier increases with ageing. Such ageing-related changes can lead to region-specific increases in brain iron.37,38,54
In the microglia and astrocytes of the cortex, cerebellum, hippocampus, basal ganglia, and amygdala, iron deposits histochemically detected and ferritin concentrations generally increase with age. Oligodendrocytes contain the largest amount of iron, stored mainly as ferritin and transferrin, and concentration remains constant as people age.28 In the elderly brain, there is a subpopulation of ferritin-positive microglia cells and most of these cells have aberrant dystrophic-type morphology. Iron phagocytosed by the subpopulations of ferritin-positive microglia cells probably becomes a source of toxic species that cause cellular degeneration. Dystrophic and ferritin-positive microglia might contribute to the pathogenesis of neurodegenerative disorders because of altered microglial function.55 Although haem oxygenase 1 (HO-1) is considered to be cytoprotective, up-regulation of this enzyme in glia might contribute to neurodegeneration: as brains age, the prolonged action of HO-1 in astrocytes is likely to be involved in iron sequestration, intracellular oxidative stress, and mitochondrial insufficiency.56
Neurodegenerative mechanisms involving iron
Iron accumulation in brain cells needs to be tightly regulated to prevent toxic effects. Excess iron can induce oxidative stress by generating reactive oxygen species (ROS), notably the hydroxyl radical.31,57 ROS can damage DNA and mtDNA,58 affect DNA expression by epigenetic mechanisms,59 and oxidise proteins. Peroxidation of polyunsaturated fatty acids in membrane lipids60 by ROS can generate highly reactive aldehydes, such as 4-hydroxynonenal, which irreversibly modify proteins by carbonylation.61,62 ROS can induce the release of iron from mitochondrial iron–sulphur cluster proteins of the respiratory chain and other iron storage proteins, which will lead to further ROS production via Fenton’s reaction (panel). Disruption of iron homoeostasis can interfere with mitochondrial functions and as a result accelerate the progression of neurodegenerative mechanisms.63,64 Such increases in iron can induce neurodegenerative processes through mechanisms different from Fenton’s reaction. Cathecolamines, such as dopamine, might be oxidised to highly reactive or toxic quinones via the reduction of ferric iron or enzymatically.65–67 Ferric iron has been shown to participate in the conversion of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (a neurotoxin known to induce Parkinson’s disease-like symptoms) into the toxic metabolite 1-methyl-4-phenylpyridinium ion.68 Additionally, the neurodegenerative mechanisms leading to cell death caused by the 1-methyl-4-phenylpyridinium ion are thought to involve iron and changes in iron metabolism.69
The aggregation of proteins involved in neurodegenerative disorders (eg, α synuclein70 and hyper-phosphorylated tau protein) have been shown in vitro to be triggered by elevated ferric iron concentrations.71 Inclusion bodies containing damaged or aggregated proteins could cause endoplasmic reticulum stress, which is a common feature of several neurodegenerative diseases.72
Neurodegeneration that results from iron toxicity can lead to apoptosis73 and ferroptosis, an iron-specific form of non-apoptotic cell death.74
Iron in neurodegenerative disorders
Alzheimer’s disease
Defective homoeostasis of the redox-active metals iron and copper probably contributes to the neuropathology of Alzheimer’s disease. High concentrations of zinc, copper, and iron are present in the insoluble amyloid plaques and neurofibrillary tangles characteristic of Alzheimer’s disease. Focal accumulation of zinc, copper, and iron might deprive other brain tissues of these essential metals, leading to aberrant neuronal function.75 Abnormal homoeostasis of zinc, copper, and iron metal ions has been implicated in the misfolding process associated with the production of amyloid β (Aβ), from amyloid precursor protein (APP), hyperphosphorylated tau (found in the plaques and tangles), and contributing to neuronal oxidative stress.76 Tau accumulation in neurofibrillary tangles is associated with the induction of HO-1, a potent antioxidant, which has an important role in metabolising haem released from damaged mitochondria. Although the bilirubin that is generated in this process is an antioxidant,77 ferrous iron is released too, which might participate in Fenton’s reaction to produce hydroxyl radicals.
Most of the APP is cleaved by the non-amyloidogenic pathway: α secretase followed by γ secretase, to release N-terminal fragment p3, leaving APP intracellular domain in the membrane. Alternatively, APP can first be cleaved by β secretase and then γ secretase to produce Aβ (the neurodegenerative, amyloidogenic pathway).78 Stimulation of the α secretase pathway attenuates Aβ formation and accumulation of this peptide in the brain. The proteolytic activation of the inactive forms of α secretase and β secretase is modulated by furin.79 Excessive amounts of total iron will decrease furin activity because transcription of furin is modulated by cellular concentrations of iron, leading to decreased furin protein concentrations which thereby favours β secretase activity and enhances the amyloidogenic pathway. By contrast, iron deficiency will increase furin activity, thereby enhancing α secretase and stimulating the non-amyloidogenic pathway.78,80
Iron might modulate APP processing through the interaction of IRPs with a putative IRE in the 5’-untranslated region of its mRNA, located immediately upstream of an interleukin-1 responsive acute box domain.81 APP translation might therefore be up-regulated in conditions of iron excess, increasing the amount of APP available to enter the amyloidgenic pathway, which is favoured by decreased furin activity.78 Conversely, increases in interleukin-1 production, increase IRP binding to APP 5’-untranslated region, thereby decreasing APP production.81 IRP binding to IRE might interfere with APP translation and translocation across the endoplasmic reticulum membrane; the interference could be substantial because α secretase activity needs membrane-bound APP.81
APP was suggested to have ferroxidase activity,82 but this has not been confirmed by in-vitro studies with a peptide containing the iron-binding REXXE motif and the full-length protein.83,84 Microtubule-associated protein tau (MAPT) deficiency induces intracellular iron accumulation, which causes degeneration of dopaminergic neurons, leading to parkinsonism with dementia in mice.85 Tau deficiency impairs ferroportin iron export by retaining APP in the endoplasmic reticulum so that it can no longer be trafficked to the neuronal surface, where it can couple its ferroxidase activity to ferroportin.
Increased iron concentrations accompany Aβ aggregation in areas initially affected in Alzheimer’s disease and offer an opportunity for a MRI-based diagnosis. MRI scans of post-mortem human brains and a mouse model of Alzheimer’s disease show decreases in hippocampal T2* MRI, which is sensitive to the magnetic properties of iron86,87 or its spatial variance, attributed in part to iron in Aβ plaques.88–90 Although MRI resolution is not sufficient to detect individual plaques, T2* abnormalities that result from plaque aggregates might be detected with MRI. When clearly distinguished from potential confounders originating from haem iron, changes in hippocampal T2*-weighted MRI might be a valuable accompaniment to morphological changes in the development of a biomarker for the early stages of Alzheimer’s disease.91
Increases of iron in animal brains produce pronounced cognitive defects.92 Iron deposits in presenilin/APP transgenic mice models of Alzheimer’s disease93 colocalise with Aβ plaques,94,95 and increases in total brain iron coincide with early plaque formation.96 Overexpression of HO-1 in mice leads to iron loading and tau aggregation in the brain, which are characteristic of Alzheimer’s disease.97 HO-1 is up-regulated in the hippocampus and temporal cortex of patients with Alzheimer’s disease or mild cognitive impairment, which further implicates this haem-degrading enzyme in the pathogenesis of Alzheimer’s disease.98,99
Parkinson’s disease
Several studies have shown increases of total iron concentration in the substantia nigra of patients with Parkinson’s disease. Neuropathological studies that used accurate spectroscopic methods to measure total iron concentrations in specific brain regions, such as substantia nigra pars compacta and reticulata showed that iron concentrations in these regions increase with disease severity.100–103 Imaging methods, such as MRI and transcranial sonography, were not able to substantiate the relation between total iron concentration and disease severity because of the absence of accurate quantification for the iron content in different brain areas.104,105 The reason for total iron accumulation in the substantia nigra of patients with Parkinson’s disease is unclear, but various factors have been suggested: increased permeability or dysfunction of the blood–brain barrier;106,107 increased pro-inflammatory state;37 increase of lactoferrin receptors in neurons and microvessels;108 increased expression of DMT1 in dopamine neurons;109 altered iron transport by transferrin–TFR type 2;63 and mutations in genes relevant to iron transport and binding.110,111
In patients with Parkinson’s disease, semi-quantitative histochemical methods showed that iron deposits were present in the neurons and glia of the substantia nigra, putamen, and globus pallidus, with an increase of ferritin-loaded microglia cells in the substantia nigra.112 Ferric iron can, in vitro, catalyse the conversion of α-synuclein from the α-helix to the β-sheet conformation that is present in Lewy bodies.113,114 Redox-active iron accumulates in Lewy bodies in the substantia nigra of individuals with Parkinson’s disease.115 Increases of iron and a decrease of ferritin in the substantia nigra101,116–119 are indicative of high iron loading of ferritin.120 Reduced ferritin production might be caused by sustained IRP1 activity, noted in post-mortem Parkinson’s disease brains, which would reduce ferritin synthesis.121 Investigations have shown an increase in redox-active iron associated with neuromelanin in substantia nigra neurons of patients with Parkinson’s disease, probably as a result of decreased ferritin synthesis. Increased redox-active iron is higher in patients with the most severe neuronal loss and is absent in neurons without neuromelanin.122–124
High concentrations of iron detected in the substantia nigra of individuals with Parkinson’s disease might exceed the iron-buffering capacity of complexes, such as neuromelanin and ferritin, and could induce neurotoxicity.124 Intense microgliosis around extraneuronal neuromelanin (released by dying neurons) has been identified in the substantia nigra of patients with Parkinson’s disease.125,126 In-vitro and in-vivo studies have confirmed the ability of neuromelanin to activate microglia and induce death of dopamine neurons.127,128
Increased total iron content, detected by MRI, was reported in the red nuclei of patients with Parkinson’s disease and dyskinesia.129 In the temporal cortex and globus pallidus of patients with Parkinson’s disease, a decrease of total iron concentration was detected by inductively coupled plasma mass spectrometry.101,117,130
A contributing factor to the increased iron accumulation in Parkinson’s disease might be increased DMT1 activity or decreased ferroxidase activity of ceruloplasmin, both of which would increase total intracellular iron, as reported in an animal model of Parkinson’s disease109 and in patients.131–134 Ceruloplasmin dysfunction might be associated with Parkinson’s disease.135,136 Reduced ferroxidase activity of ceruloplasmin was noted in the CSF of patients with Parkinson’s disease together with increased CSF copper concentrations by comparison with controls,131 a condition which could contribute to the increased mobilisation of reactive iron and oxidative stress reported in Parkinson’s disease. Several missense variations in the gene encoding ceruloplasmin, which could affect the mobilisation of reactive iron, have been reported in a few patients with Parkinson’s disease.137
Despite the aforementioned increases of total and reactive iron content in brain areas of patients with Parkinson’s disease, increased concentrations of total serum iron are causally associated with a decreased risk of developing Parkinson’s disease, thus showing a potentially protective effect of peripheral iron.138,139 Studies have shown that reduced concentrations of systemic iron are associated with an increased risk of Parkinson’s disease.140–142 This increased risk is likely to be due to the need for adequate supplies of iron for the synthesis of neurotransmitters, such as dopamine, because iron is a cofactor of tyrosine hydroxylase (the key enzyme of dopamine synthesis). Moreover, low iron concentrations can reduce the neuronal deposits of ferritin, generating a condition in the substantia nigra neurons of patients with Parkinson’s disease.117,119
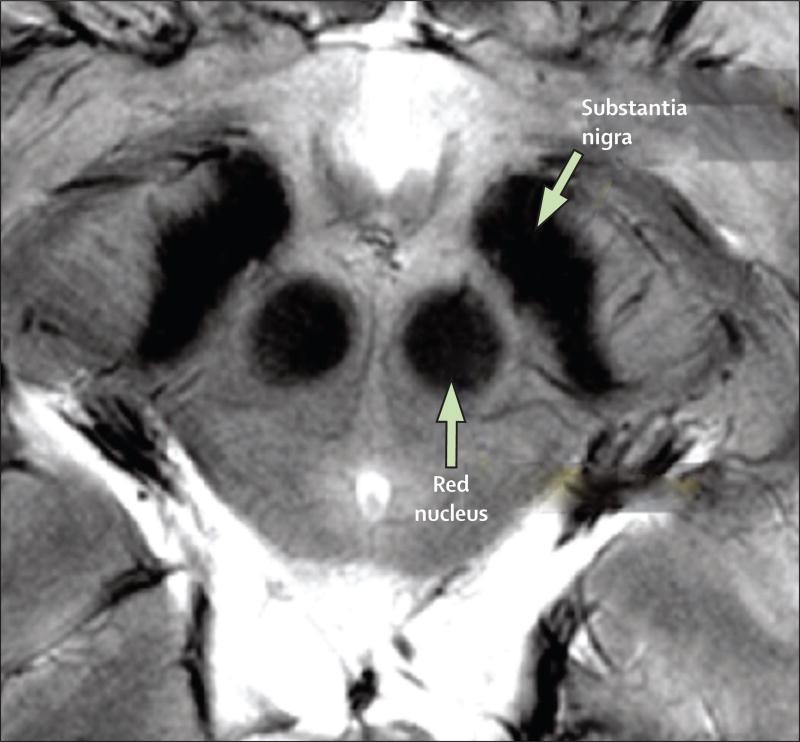
The characteristic iron accumulation in the substantia nigra of individuals with Parkinson’s disease can be detected in vivo with MRI143 (figure 2). MRI measures generally have been found to correlate with disability and thus might be used to monitor disease progression.104,144,145 Furthermore, the study of morphological and iron concentration changes in the midbrain and cerebellum might help to distinguish Parkinson’s disease from other disorders with similar symptoms, such as multiple system atrophy and progressive supranuclear palsy.146,147
Figure 2. MRI of iron in Parkinson’s disease.
T2*-weighted MRI of midbrain in a patient with early onset Parkinson’s disease. Substantia nigra and red nucleus, naturally high in iron, seem darker because of reduced T2*. In Parkinson’s disease, further iron accumulations144,145 and morphological changes143 are seen in substantia nigra; both are associated with disability. Reproduced from Cho and colleagues143 by permission of John Wiley & Sons.
Preliminary reports state that identification of neuromelanin (rather than iron) by MRI might be feasible in patients with Parkinson’s disease.148,149 Neuromelanin loss in the locus coeruleus and substantia nigra, together with the associated loss in the ability to sequester iron, might be a characteristic sign of Parkinson’s disease.150,151
Transcranial sonography might be a helpful technique in the diagnosis of Parkinson’s disease, Friedreich’s ataxia, Huntington’s disease, and restless leg syndrome and might be useful to differentiate between idiopathic Parkinson’s disease and atypical parkinsonian syndromes.152 An area of increased echogenicity (ie, propensity to generate ultrasound echo) in the substantia nigra can be visualised in about 90% of patients with Parkinson’s disease.105 Ultrasound investigation of post-mortem brains from healthy individuals showed a positive correlation between the echogenic area of the substantia nigra and concentration of iron and heavy and light chain ferritin, and a negative correlation between echogenicity and neuromelanin content of the substantia nigra. In Parkinson’s disease, loss of neuromelanin and an increase in iron concentration is noted in the substantia nigra. A positive association between iron and ferritin concentrations, and a negative association of neuromelanin content with the area of echogenicity of the substantia nigra could therefore provide a basis for diagnosis and therapeutic follow-up studies in patients with Parkinson’s disease.153 However, echogenicity is affected by other factors such as low spatial resolution, restricted field of view (ie, brain coverage), and non-specific echogenicity generated by inflammatory conditions.
Increased amounts of iron were assayed in the brains of both the 6-hydroxydopamine and the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine animal model of Parkinson’s disease,109,154 consistent with the increased expression of a DMT1 isoform (+IRE) reported in the substantia nigra of patients with Parkinson’s disease. Overexpression of DMT1 and iron accumulation was noted in the mesencephalon of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine animal models of Parkinson’s disease.109 Moreover, in the 6-hydroxydopamine model of Parkinson’s disease the degeneration of nigrostriatal dopaminergic neurons is associated with increased iron accumulation.155
Multiple sclerosis
Increased iron concentrations occur in specific brain regions in multiple sclerosis, most prominently in the deep grey matter structures, often with bilateral presentation. In white matter, iron deposits are usually located at sites of inflammation that are associated with blood vessels. Iron concentrations increase in many deep grey matter structures as multiple sclerosis progresses.156,157 The origins of iron accumulation are unexplained, but might be linked to inflammatory processes that alter the permeability of the blood–brain barrier thereby allowing iron-rich macrophages into the brain, and to disturbed axonal ion homoeostasis and aberrant expression of glutamate receptors, sodium channels, and voltage-gated calcium channels, leading to axonal calcium accumulation and degeneration.158 The inflammatory milieu associated with multiple sclerosis includes the activation of microglia and subsequent release of proinflammatory cytokines and ROS, inducing oxidative stress.40 Such an inflammatory milieu might cause the excessive breakdown of oligodendrocytes associated with demyelination, releasing additional redox-active ferrous iron into the brain and further enhancing oxidative stress.158 Microglia and macrophages take up the released ferrous iron (which is oxidised to ferric iron within the channels of heavy chain ferritin and stored within the light chain ferritin) and upregulate the concentration of ferritin, which can be seen at the edges of chronic white matter lesions and might be detectable in vivo with MRI.159–161 HO-1 is overexpressed in spinal cord astroglia in multiple sclerosis, which might lead to the induction of increased mitochondrial iron deposition in human multiple sclerosis plaques. In-vitro studies of rat astroglial cultures showed that proinflammatory cytokines (ie, interleukin 1β and tumour necrosis factor α) increased HO-1 expression after 6 days of incubation. Increased HO-1 expression promoted the sequestration of non-transferrin iron into the astroglial mitochondrial compartment, as assayed by 55Fe incorporation. Incubation with interferon β reverted the cytokine-dependent induction of HO-1 and the subsequent incorporation of iron into mitochondria.162
Friedreich’s ataxia
Several neurodegenerative disorders are the result of mutations in proteins that directly affect iron metabolism. Friedreich’s ataxia is the most common of the hereditary ataxias, with a prevalence of one case in 50 000 individuals in the white population. In Friedreich’s ataxia there is reduced expression of the mitochondrial protein frataxin caused by the expansion of unstable nucleotide repeats in a non-coding region of FXN. The severity is dependent on the number of nucleotide repeats.163 The most common mutation in FXN is an expanded GAA trinucleotide repeat in intron 1, which occurs in around 96% of patients with Friedreich’s ataxia. The highest concentrations of frataxin are in the heart, spinal cord, and dorsal root ganglia.57 The essential role of frataxin in mitochondrial iron metabolism is only partly understood, but frataxin probably regulates iron handling in mitochondria, and prevents iron from generating oxidative stress. Frataxin might act as an iron chaperone for the biosynthesis of iron–sulphur clusters and haem.57
The major consequences of frataxin deficiencies include the impairment of mitochondrial biosynthesis of proteins containing iron–sulphur clusters (eg, aconitase), deficiency of respiratory chain electron transporters on complexes I–III, iron overload in mitochondria, oxidative stress, and free radical accumulation leading to changes in cellular iron metabolism.164,165 Histological studies and MRI suggest that in human brains the highest iron accumulation occurs in the dentate nuclei of the cerebellum.166,167
Aceruloplasminaemia and neuroferritonopathy
The class of diseases known as neurodegeneration with brain iron accumulation encompasses a wide range of genetically distinct adult and paediatric neurological diseases.168–170 Aceruloplasminaemia and neuroferritinopathy are caused by mutations that target proteins directly implicated in iron metabolism. In other rare genetic diseases of this group, such as pantothenate kinase-associated neurodegeneration, phospholipase A2G6-associated neurodegeneration, and Kufor-Rakeb disease, mutations disrupt proteins with cellular functions different from iron metabolism, and the mechanisms that result in brain iron overload are undefined.169–173 Pantothenate kinase-associated neurodegeneration is characterised by an excess of iron especially in the globus pallidus, leading to a typical MRI pattern called eye of the tiger, and to a lesser extent, and later in the disease, in the substantia nigra.174,175 Pantothenate kinase–associated neurodegeneration results from mutations in PANK2, which encodes the mitochondrial enzyme pantothenate kinase that is implicated in coenzyme A biosynthesis and is important in many metabolic pathways (ie, lipids synthesis, citric acid cycle).176 Phospholipase A2G6-associated neurodegeneration is characterised by mutations in PLA2G6, which encodes a calcium-independent group VI phospholipase A2 that is important for homoeostatic membrane phospholipid metabolism.177 Typical iron accumulation in phospholipase A2G6-associated neurodegeneration often occurs in the globus pallidus and might affect the substantia nigra.178 Fatty acid hydroxylase-associated neurodegeneration leads to iron accumulation in the globus pallidus, with the substantia nigra possibly less affected.172 Fatty acid hydroxylase-associated neurodegeneration is caused by mutations in FA2H, which encodes fatty acid-2-hydroxylase, the enzyme that catalyses hydroxylation of free fatty acids in the sphingolipid biosynthesis pathway.179 Kufor-Rakeb disease is associated with mutated ATP13A2, which encodes a lysosomal type 5 P-type ATPase,180 whose physiological role remains to be elucidated. MRI iron patterns in Kufor-Rakeb disease are controversial, with iron deposition in the putamen and caudate nucleus in some cases,181 or without discernible iron deposition in other individuals.182 β-propeller protein-associated neurodegeneration is a X-linked disorder associated with a mutation in WDR45, which encodes a protein involved in autophagy. Brain imaging shows iron accumulation in the substantia nigra and globus pallidus of patients with β-propeller protein-associated neurodegeneration.183
The absence of functional multicopper oxidase ceruloplasmin in aceruloplasminaemia impairs cellular iron efflux and leads to iron accumulation in most parenchymal tissues, including the brain and particularly in the basal ganglia. In these iron overloaded areas of the brain, up to a ten-times increase was recorded in neurons and microglia, but widespread brain iron deposition can occur.170,175 The excessive iron accumulation results from the inability of astrocytes to mobilise their iron to be used by neurons.184
Neuroferritinopathy, a rare adult-onset condition presenting with a range of extrapyramidal movement disorders, is caused by mutations in light-chain–ferritin185 (the principal iron storage protein) resulting in loss of function and accumulation of iron in the globus pallidus, putamen, and dentate nuclei of the cerebellum.186 Mouse models of neuroferritinopathy show iron overload, neurodegeneration, and DNA damage.187,188
Neurodegeneration with brain iron accumulation is associated with excess iron accumulation in deep grey matter nuclei.169 MRI studies of neuroferritinopathy have suggested that the greatest accumulation of iron is in the basal ganglia and dentate nuclei, but thalamus and red nuclei can also be affected.185,189,190 In cases of severe neuroferritinopathy, the putamen and globus pallidus might have focal spots of low iron concentrations (eg, judged from increased T2*); this is attributed to increased tissue water content and cystic accumulation from inflammatory processes. By contrast, a more general involvement of deep grey matter nuclei (and grey matter in general) with respect to iron accumulation is seen in aceruloplasminaemia, but without evidence of cystic processes.191
Huntington’s disease
Huntington’s disease is a neurodegenerative disorder characterised by progressive motor, cognitive, and psychiatric deterioration. It is the most common of the polyglutamine diseases, affecting about one in 10 000 individuals worldwide. Huntington’s disease is caused by CAG trinucleotide repeats within exon 1 of HTT, the gene that encodes huntingtin. People with Huntington’s disease have between 36 and 121 CAG trinucleotide repeats, compared with between six and 34 in the wild type gene.192 The dominant polyglutamine expansion within the N-terminus of the huntingtin protein initiates events that lead to neuronal loss primarily within the striatum and cerebral cortex. In embryonic stem cells, huntingtin is iron-regulated and also involved in iron homoeostasis regulation.193 Alterations in brain iron metabolism with increased iron accumulation were identified by MRI in the striata of patients with Huntington’s disease194 and in particular the basal ganglia (caudate nucleus, putamen, and globus pallidus).195,196
Restless legs syndrome
Restless legs syndrome is characterised by reduced iron function. Autopsy and MRI investigations show decreased iron concentrations in the substantia nigra of patients with restless leg syndrome that are associated with disease severity.197,198 Iron misregulation is implicated in the pathology of restless leg syndrome, so that concentrations of TFR, IRP1, DMT1, ferroportin, and heavy-chain ferritin are decreased in dopaminergic neurons of the substantia nigra.198–200 Iron deficit conditions worsen symptomatology, whereas iron replacement therapy improves symptoms.198,201
Developments in MRI for brain iron detection
Development of high-field (7 T and above) MRI has great relevance to the study of brain iron. High-field MRI amplifies the paramagnetic effect of iron on T2* relaxation, leading to improved sensitivity, resolution,202 and a better resolution of confounding factors. For example, the confounding effect of tissue water content seen on T2* is minor at high-field strength. Additionally, studies at high-field strength show that the confounding effect of myelin on T2* can be accounted for by including frequency information, which is normally discarded.51,203,204 Myelin and iron decrease T2*, but have an opposing effect on frequency owing to the diamagnetic properties of myelin (as opposed to iron’s paramagnetic properties).204 This use of frequency to better quantify iron development will probably translate to clinical studies at lower MRI field strengths.
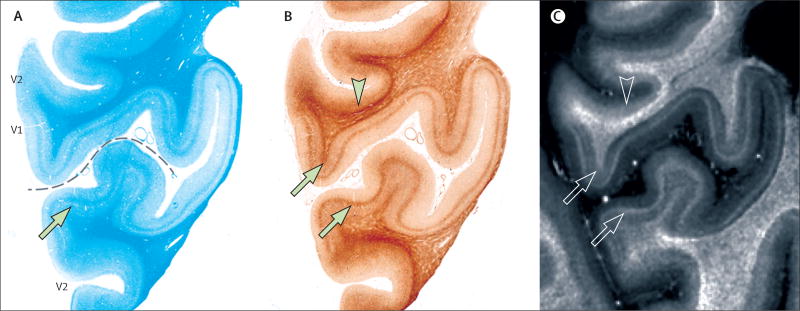
High-field MRI has great potential for the study of subtle variations in iron at low spatial resolution, even outside the regions of deep grey matter nuclei with high iron concentrations. For example, in a study of healthy brains substantial iron concentration variations were shown in the different cortical layers (figure 3). In-vivo and post-mortem investigations suggest focal iron accumulation in the white matter in multiple sclerosis160,161,206 and focal iron accumulation in the cortex in amyotrophic lateral sclerosis207 co-localise with microglia (appendix).160,207 Combined with other biochemical and structural tissue parameters derived from MRI, such measurements might help us to understand the complex pathophysiological processes underlying neurological disorders. For example, the sensitivity of MRI to tissue myelin content and integrity208,209 might help to establish the temporal relation between iron accumulation and the demyelinating process in multiple sclerosis.
Figure 3. MRI detection of fine-scale spatial variation in iron content in healthy brain tissue.
(A) Laminar variations shown in luxol fast blue myelin stain. Laminar patterns seem specific to functional areas V1 and V2. (B) Laminar patterns shown in Perls’ 3,3’-diaminobenzidine iron stain. (C) R2* (=1/T2*) obtained from 7T post mortem MRI. The dashed line indicates calcarine sulcus. Solid arrows, open arrows, and arrowheads show areas of increased iron in central and deep layers, and subcortical white matter. Reproduced from Fukunaga and colleagues205 with permission of Proceedings of the National Academy of Sciences.
Iron chelation as a potential therapy
Overview
The potential therapeutic use of iron chelators to remove excess iron from specific brain regions affected by neurodegenerative diseases has received much attention. To be effective, an iron chelator should be able to penetrate both cellular membranes and the blood–brain barrier, target the region of iron accumulation without depleting transferrin-bound iron from the plasma, and be able to remove chelatable iron from the site of accumulation or to transfer it to other biological proteins, such as circulating transferrin.210 Since most patients with neurodegenerative diseases will have normal systemic iron homoeostasis, low doses of the chelator need to be used to minimise side-effects. Furthermore, whether iron chelators can remove iron from conjugated iron containing proteins and molecules, such as neuromelanin, is unknown; the chelators in clinical use were developed to remove iron from ferritin and haemosiderin in grossly iron overloaded tissues, such as the liver and spleen, and to a lesser extent the heart. MRI is a promising technique to assess the efficacy of a treatment, although the quantitative accuracy of MRI might be dependent on the type and molecular distribution (eg, cluster size and oxidation state) of iron.211
Parkinson’s disease
The efficacy of iron chelation in the treatment of Parkinson’s disease has been studied in an animal model. Genetic (with transgenic expression of ferritin) or pharmacological (by clioquinol) iron chelation resulted in the reduction of reactive iron protecting mice from the toxic effects derived from 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine.212
A patient with moderate parkinsonism, who had a range of symptoms including dysarthria and orofacial dystonia, had iron accumulation in internal globi pallidi, dentate nuclei, substantia nigra, and red nuclei seen with T2*-weighted MRI. Deferiprone 30 mg/kg per day was given orally for 32 months. After 6 months many of the symptoms had improved, and after 1 year an improvement was recorded in the Unified Parkinson’s Disease Rating Scale score. T2*-weighted MRI showed a rapid decrease in iron accumulation in the bilateral dentate nuclei, with a milder and later reduction in the substantia nigra, but no significant changes in the red nuclei.213 From the initial findings of the beneficial effect of deferiprone, two clinical trials have investigated the safety and efficacy of deferiprone in double-blind placebo-controlled studies.214–216 T2*-weighted MRI, Unified Parkinson’s Disease Rating Scale motor scores, and ferritin (the iron storage protein) in the blood were analysed. Preliminary data from one of these studies suggested deferiprone, 30 mg/kg per day, slightly improved motor signs after 6 months of treatment, decreased motor handicap progression (mean change in Unified Parkinson’s Disease Rating Scale motor score=−2), and the substantia nigra iron content substantially decreased on T2*-weighted MRI after 1 year. Three of the 40 patients in the first study developed neutropenia or agranulocytosis, which were resolved rapidly with cessation of deferiprone.214,215 In the second clinical trial of deferiprone, patients with Parkinson’s disease received 20 mg/kg per day or 30 mg/kg per day for 6 months; both doses were well tolerated, there were minimum toxic effects, and decreases in iron in specific brain regions were detected by T2*-weighted MRI.216
Alzheimer’s disease
Crapper McLachlan and colleagues217 showed a substantial reduction in the rate of deterioration of daily living skills in 48 patients with Alzheimer’s disease who were given deferrioxamine (125 mg intramuscular two times a day, five times per week for 24 months) when compared with patients with Alzheimer’s disease given placebo. Despite such positive results, no other clinical studies of deferrioxamine have been reported.
Presently, only one family of metal-binding agents, PBT2 (5,7-dichloro-2-[(dimethylamino)-methyl]-8-hydroxyquinoline), is being tested in clinical trials for the treatment of Alzheimer’s disease and Huntington’s disease. PBT2 binds excesses of copper and zinc and possibly iron in the brain, thereby diminishing the amount of amyloid plaque formation and relocating these metal ions to depleted cellular and neuronal compartments.218 In a clinical trial of 78 patients with Alzheimer’s disease, 29 patients received PBT2 250 mg/day, 20 patients were given a lower dose of PBT2 (50 mg/day), and the remaining 29 patients were given placebo. Patients receiving 250 mg/day showed a substantial reduction in CSF of Aβ concentration, and some cognitive improvement (executive function) was noted.219
Friedreich’s ataxia
Boddaert and colleagues210 were the first to investigate the efficacy of deferiprone in patients with Friedreich’s ataxia. Treatment with 20 mg/kg per day or 30 mg/kg per day deferiprone for 6 months in nine patients with Friedreich’s ataxia aged between 14 and 23 years reduced the iron content in the dentate nuclei. This reduction was associated with neurological improvements in manipulative dexterity, speech fluency, and a reduction in neuropathy and ataxia gait, particularly in the youngest patients. A reduction in iron content was seen after 2 months of treatment and the effect was proportional to the concentration of initial accumulated iron. Boddaert and colleagues210 suggested that the form of iron chelated was a labile iron pool, with iron possibly being bound to enzymes, such as hydroxylases, and to ferritin. None of the other brain regions investigated (ie, pallidal nuclei, the thalamus, and cerebellar white matter region) showed any substantial changes in iron accumulation as detected by T2*-weighted MRI throughout chelation therapy. Velasco-Sanchez and colleagues220 administered deferiprone (20 mg/kg per day) and the antioxidant idebenone for 11 months to 20 patients with Friedreich’s ataxia aged between 8 and 25 years. MRI values in the dentate nuclei of participants showed a significant reduction of iron that was associated with significant recovery of kinetic functions, although gait and posture scores worsened.
Aceruloplasminaemia and neuroferritonopathy
Subcutaneous infusion of deferoxamine was reported to be effective in patients with aceruloplasminaemia.221 After 10 months of deferoxamine treatment in a 63-year-old patient with aceruloplasminaemia, Miyajima and colleagues222 showed decreases in brain iron by MRI, which were associated with a slight improvement in neurological symptoms. The oral chelator deferasirox was effective in a 59-year-old man to treat left-side choreoathetosis and an unsteady gait.223 Comparisons of deferiprone and deferoxamine treatments in a woman with aceruloplasminaemia, who showed marked MRI hypointensity, reduced T2* MRI signal in the dentate and red nuclei, thalamus, pulvinar, neostriatum, and putamen, showed that deferoxamine (20 mg/kg per day for 5 days a week for 8 months by subcutaneous bolus injection) evoked an increase in urinary iron excretion, a decrease in serum ferritin concentrations, and decreases in haemoglobin iron and serum iron.224 By contrast, deferiprone 75 mg/kg per day for 6 months had no effect; no MRI changes were seen in the brain regions after either chelation therapy.224
Chelation therapy has been reported to provide improvements, notably with deferiprone, and particularly for other neurodegeneration with brain iron accumulation diseases, but no improvement was seen in two patients with neuroferritinopathy.185
Conclusions and future directions
How the different brain regions maintain iron concentrations under normal circumstances, and the changes that occur with ageing and after an inflammatory insult, are not known. In peripheral iron-loading diseases, such as thalassaemias and haemochromatosis, no evidence has been reported of an increased incidence of neurodegeneration, nor of elevated concentrations of brain iron, despite the massive iron deposition in parenchymal tissues. We therefore suggest that the brain represents a privileged body compartment, which in normal circumstances does not respond to peripheral variations in iron status. Neurodegenerative diseases might be caused by changes in brain iron from compartments where iron is quiescent to other parts of the brain where iron is neurotoxic. The future challenge is to establish the mechanisms involved in brain iron changes on a disease by disease basis. We expect MRI to have an important role, possibly in a quantitative or a semi-quantitative manner. If brain iron patterns are characteristic of disease or disease stage, this might have a great effect on a diagnosis. Although total iron measures might be dominated by biologically inert forms sequestered in ferritin, neuromelanin, and other molecules, they might be predictive for bioactive iron species and, as such, have relevance for the study of disease. High-field MRI developments might advance the ability to map distributions of iron quantitatively, increasing knowledge of the pathogenesis of neurological disorders. Unfortunately, it is difficult to relate tissue iron concentrations to those in specific cell types, for which we presently rely on scarce information from studies done many years ago. Despite increases in the resolution of MRI images of iron distribution, MRI cannot measure concentrations of specific iron molecules in particular cells.
Processes involved with age-related and disease-related accumulation of iron and iron-induced inflammation in specific brain regions and cells are poorly understood. Future research should focus on the accurate mapping of iron in healthy brains, at different ages, and in neurodegenerative disorders to begin to interpret regional variations in brain iron. Because much of our present knowledge about iron homoeostasis relies on studies on young healthy rodents (whose iron pathways have some important differences to elderly human brains), valuable information might be gleaned from experiments on human induced pluripotent stem cells, primates, and in ex-vivo human brain tissues.
Supplementary Material
Search strategy and selection criteria.
We searched PubMed for articles published from Jan 1, 1958 to Aug 31, 2013, in English with the terms “iron in brain ageing”, “iron neurotoxicity”, “iron in neurodegenerative diseases” separately and each in combination with all the pathologies included in this review (Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, Friedreich’s ataxia, aceruloplasminaemia, neuroferritonopathy, Huntington’s disease, and restless legs syndrome,), “magnetic resonance imaging of brain iron”, “animal models of iron neurotoxicity”, and “iron chelation therapy”. We also identified papers through searches of the authors’ personal files.
Acknowledgments
FAZ and LZ were supported by Italian Ministry of Education, University, and Research—National Research Programme (PNR)—CNR Flagship “InterOmics” Project (PB·P05), by PNR—CNR Ageing program 2012–14, and by MIUR—Medical Research in Italy Project (RBNE08ZZN7). We thank Francesca A Cupaioli for her assistance in bibliographic research.
Panel: Glossary of terms
- Ceruloplasmin
A multicopper ferroxidase that oxidises ferrous iron (Fe2+) into the ferric form (Fe3+). Ceruloplasmin can exist as a soluble form in plasma and other fluids or as a membrane bound form (the glycophosphatidylinositol-anchored form of ceruloplasmin, which is highly expressed at the end-foot of astrocytes in the mammalian CNS).
- Divalent metal ion transporter 1 (DMT1)
The major transmembrane transporter of ferrous iron and other divalent metal cations into cells (eg, enterocytes). DMT1 has an important role in the efflux of ferrous iron from endosomes during the transferrin cycle.
- Ferritin
The major iron storage protein in which iron is stored in as a soluble, non-reactive, or bio-available form. In mammals, ferritin is a heteropolymer composed of two types of subunits, ferritin heavy chain and ferritin light chain; the ratio of heavy to light chain is tissue specific. The heavy chain shows ferroxidase activity, and converts ferrous iron to ferric iron before being stored inside the iron core, whereas the light chains have no ferroxidase activity but play an important part in the nucleation of the iron core inside the protein.
- Fenton’s reaction
Ferrous iron (Fe2+) reacts with hydrogen peroxide producing hydroxyl radicals, a highly reactive oxygen species (ROS).
- Ferroportin
The major exporter of iron out of some cells. Iron is exported in the form of ferrous iron therefore the catalytic activity of ferroxidase is needed. The associated ferroxidase oxidises exported ferrous iron into ferric iron and this function is mainly accomplished by hephaestin in the gut or by ceruloplasmin.
- Hepcidin
A small peptide secreted mainly by the liver and possibly other cell types, such as glial cells; secretion is dependent on the iron loading and inflammatory status, and controls the quantity of iron translocated by ferroportin out of cells. When hepcidin binds to ferroportin, this induces internalisation followed by degradation of the complex in lysosomes.
- Hephaestin
A membrane bound ceruloplasmin analogue that participates in iron export from enterocytes. Hephaestin acts as a multicopper ferroxidase, oxidising ferrous iron exported from enterocytes through ferroportin to ferric iron that can then be rapidly bound to circulating transferrin or other iron carrier proteins.
- Iron regulatory proteins (IRPs) and iron responsive or regulatory elements (IREs)
IRP1 and IRP2 are cytoplasmic proteins that specifically bind to IREs in mRNAs when iron is in low concentrations. IRPs do not bind to IREs at high iron concentrations. IREs are characteristic stem and loop structures of some mRNAs, with a defined secondary structure at their untranslated regions (UTRs). When IRPs are bound to IREs at the 5’-UTR of mRNAs translation is prevented, whereas when IRPs are not bound translation can proceed; by contrast, when IRPs are bound to 3’-UTR they stabilise mRNA allowing translation, whereas when IRPs are not bound nuclease degradation of the mRNA occurs.
- Neuromelanin
A complex polymeric molecule present in the human CNS, which is located in organelles surrounded by a double membrane. Neuromelanin pigment is able to accumulate different metals, mainly iron. Neuromelanin seems to be the most effective system for scavenging iron, which results in a long-term immobilisation of iron inside neurons. Pigmented neurons of the substantia nigra and locus coeruleus have the highest levels of neuromelanin in the brain.
- Transferrin
A high-affinity iron–binding protein (apo-transferrin or iron-free transferrin) that binds two ferric iron atoms, holo-transferrin or diferric transferrin, and is present in plasma, transports iron in serum, lymphatic system, and CSF, and delivers iron to cells via the transferrin cycle.
- Transferrin receptor (TFR)
TFR1, expressed on the membrane of most cells, is the main receptor for transferrin and selectively binds diferric transferrin to internalise it through receptor-mediated endocytosis (transferrin cycle). TFR2, the function of which is not well understood but is distinct from TFR1, is an iron sensor in the regulation of hepcidin expression.
- Labile iron pool
Chelatable and redox-active iron in complexes of low stability.
Footnotes
Contributors
All authors equally contributed to all parts of the Review. All authors revised the manuscript and approved the final version.
Declaration of interests
We declare no competing interests.
References
- 1.Crichton RR. Inorganic biochemistry of iron metabolism from molecular mechanisms to clinical consequences. Chichester: John Wiley & Sons; 2009. p. 461. [Google Scholar]
- 2.Hentze MW, Muckenthaler MU, Galy B, Camaschella C. Two to tango: regulation of Mammalian iron metabolism. Cell. 2010;142:24–38. doi: 10.1016/j.cell.2010.06.028. [DOI] [PubMed] [Google Scholar]
- 3.Wang J, Pantopoulos K. Regulation of cellular iron metabolism. Biochem J. 2011;434:365–81. doi: 10.1042/BJ20101825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kruszewski M. Labile iron pool: the main determinant of cellular response to oxidative stress. Mutat Res. 2003;531:81–92. doi: 10.1016/j.mrfmmm.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Zecca L, Gallorini M, Schunemann V, et al. Iron, Neuromelanin and ferritin content in the substantia nigra of normal subjects at different ages: consequences for iron storage and neurodegenerative processes. J Neurochem. 2001;76:1766–73. doi: 10.1046/j.1471-4159.2001.00186.x. [DOI] [PubMed] [Google Scholar]
- 6.Zecca L, Stroppolo A, Gatti A, et al. The role of iron and copper molecules in the neuronal vulnerability of locus coeruleus and substantia nigra during aging. Proc Natl Acad Sci USA. 2004;101:9843–48. doi: 10.1073/pnas.0403495101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andrews NC, Schmidt PJ. Iron homeostasis. Annu Rev Physiol. 2007;69:69–85. doi: 10.1146/annurev.physiol.69.031905.164337. [DOI] [PubMed] [Google Scholar]
- 8.Mills E, Dong XP, Wang F, Xu H. Mechanisms of brain iron transport: insight into neurodegeneration and CNS disorders. Future Med Chem. 2010;2:51–64. doi: 10.4155/fmc.09.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andrews NC. Forging a field: the golden age of iron biology. Blood. 2008;112:219–30. doi: 10.1182/blood-2007-12-077388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garrick MD, Garrick LM. Cellular iron transport. Biochim Biophys Acta. 2009;1790:309–25. doi: 10.1016/j.bbagen.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 11.Muckenthaler MU, Galy B, Hentze MW. Systemic iron homeostasis and the iron-responsive element/iron-regulatory protein (IRE/IRP) regulatory network. Annu Rev Nutr. 2008;28:197–213. doi: 10.1146/annurev.nutr.28.061807.155521. [DOI] [PubMed] [Google Scholar]
- 12.Wallander ML, Leibold EA, Eisenstein RS. Molecular control of vertebrate iron homeostasis by iron regulatory proteins. Biochim Biophys Acta. 2006;1763:668–89. doi: 10.1016/j.bbamcr.2006.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moos T, Morgan EH. Transferrin and transferrin receptor function in brain barrier systems. Cell Mol Neurobiol. 2000;20:77–95. doi: 10.1023/a:1006948027674. [DOI] [PubMed] [Google Scholar]
- 14.Moos T, Rosengren Nielsen T, Skjørringe T, Morgan EH. Iron trafficking inside the brain. J Neurochem. 2007;103:1730–40. doi: 10.1111/j.1471-4159.2007.04976.x. [DOI] [PubMed] [Google Scholar]
- 15.Ke Y, Qian ZM. Brain iron metabolism: neurobiology and neurochemistry. Prog Neurobiol. 2007;83:149–73. doi: 10.1016/j.pneurobio.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 16.Leitner DF, Connor JR. Functional roles of transferrin in the brain. Biochim Biophys Acta. 2012;1820:393–402. doi: 10.1016/j.bbagen.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 17.Jeong SY, David S. Glycosylphosphatidylinositol-anchored ceruloplasmin is required for iron efflux from cells in the central nervous system. J Biol Chem. 2003;278:27144–48. doi: 10.1074/jbc.M301988200. [DOI] [PubMed] [Google Scholar]
- 18.Dringen R, Bishop GM, Koeppe M, Dang TN, Robinson SR. The pivotal role of astrocytes in the metabolism of iron in the brain. Neurochem Res. 2007;32:1884–90. doi: 10.1007/s11064-007-9375-0. [DOI] [PubMed] [Google Scholar]
- 19.Huang E, Ong WY, Go ML, Connor JR. Upregulation of iron regulatory proteins and divalent metal transporter-1 isoforms in the rat hippocampus after kainate induced neuronal injury. Exp Brain Res. 2006;170:376–86. doi: 10.1007/s00221-005-0220-x. [DOI] [PubMed] [Google Scholar]
- 20.Jefferies WA, Brandon MR, Hunt SV, Williams AF, Gatter KC, Mason DY. Transferrin receptor on endothelium of brain capillaries. Nature. 1984;312:162–63. doi: 10.1038/312162a0. [DOI] [PubMed] [Google Scholar]
- 21.Zucca FA, Cupaioli FA, Zecca L. The role of iron in neurodegeneration. In: Milardi D, Rizzarelli E, editors. Neurodegeneration: metallostasis and proteostasis. RSC Publishing; 2011. pp. 174–211. [Google Scholar]
- 22.Boserup MW, Lichota J, Haile D, Moos T. Heterogenous distribution of ferroportin-containing neurons in mouse brain. Biometals. 2011;24:357–75. doi: 10.1007/s10534-010-9405-2. [DOI] [PubMed] [Google Scholar]
- 23.Moos T, Bernth N, Courtois Y, Morgan EH. Developmental iron uptake and axonal transport in the retina of the rat. Mol Cell Neurosci. 2011;46:607–13. doi: 10.1016/j.mcn.2010.12.013. [DOI] [PubMed] [Google Scholar]
- 24.Cooperman SS, Meyron-Holtz EG, Olivierre-Wilson H, Ghosh MC, McConnell JP, Rouault TA. Microcytic anemia, erythropoietic protoporphyria, and neurodegeneration in mice with targeted deletion of iron-regulatory protein 2. Blood. 2005;106:1084–91. doi: 10.1182/blood-2004-12-4703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abbott NJ, Rönnbäck L, Hansson E. Astrocyte-endothelial interactions at the blood-brain barrier. Nat Rev Neurosci. 2006;7:41–53. doi: 10.1038/nrn1824. [DOI] [PubMed] [Google Scholar]
- 26.Xu J, Ling EA. Studies of the ultrastructure and permeability of the blood-brain barrier in the developing corpus callosum in postnatal rat brain using electron dense tracers. J Anat. 1994;184:227–37. [PMC free article] [PubMed] [Google Scholar]
- 27.Wu LJ, Leenders AG, Cooperman S, et al. Expression of the iron transporter ferroportin in synaptic vesicles and the blood-brain barrier. Brain Res. 2004;1001:108–17. doi: 10.1016/j.brainres.2003.10.066. [DOI] [PubMed] [Google Scholar]
- 28.Connor JR, Menzies SL, St Martin SM, Mufson EJ. Cellular distribution of transferrin, ferritin, and iron in normal and aged human brains. J Neurosci Res. 1990;27:595–611. doi: 10.1002/jnr.490270421. [DOI] [PubMed] [Google Scholar]
- 29.Badaracco ME, Siri MV, Pasquini JM. Oligodendrogenesis: the role of iron. Biofactors. 2010;36:98–102. doi: 10.1002/biof.90. [DOI] [PubMed] [Google Scholar]
- 30.Connor JR, Menzies SL. Relationship of iron to oligodendrocytes and myelination. Glia. 1996;17:83–93. doi: 10.1002/(SICI)1098-1136(199606)17:2<83::AID-GLIA1>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- 31.Crichton RR, Ward RJ. Metal based neurodegeneration: from molecular mechanisms to therapeutic strategies. Chichester: J Wiley and Son; 2006. [Google Scholar]
- 32.Rathore KI, Redensek A, David S. Iron homeostasis in astrocytes and microglia is differentially regulated by TNF-α and TGF-β1. Glia. 2012;60:738–50. doi: 10.1002/glia.22303. [DOI] [PubMed] [Google Scholar]
- 33.Connor JR, Menzies SL. Cellular management of iron in the brain. J Neurol Sci. 1995;134(suppl):33–44. doi: 10.1016/0022-510x(95)00206-h. [DOI] [PubMed] [Google Scholar]
- 34.Lee P, Peng H, Gelbart T, Beutler E. The IL-6- and lipopolysaccharide-induced transcription of hepcidin in HFE-, transferrin receptor 2-, and beta 2-microglobulin-deficient hepatocytes. Proc Natl Acad Sci USA. 2004;101:9263–65. doi: 10.1073/pnas.0403108101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nemeth E, Rivera S, Gabayan V, et al. IL-6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidin. J Clin Invest. 2004;113:1271–76. doi: 10.1172/JCI20945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Urrutia P, Aguirre P, Esparza A, et al. Inflammation alters the expression of DMT1, FPN1 and hepcidin, and it causes iron accumulation in central nervous system cells. J Neurochem. 2013;126:541–49. doi: 10.1111/jnc.12244. [DOI] [PubMed] [Google Scholar]
- 37.Conde JR, Streit WJ. Microglia in the aging brain. J Neuropathol Exp Neurol. 2006;65:199–203. doi: 10.1097/01.jnen.0000202887.22082.63. [DOI] [PubMed] [Google Scholar]
- 38.Farrall AJ, Wardlaw JM. Blood-brain barrier: ageing and microvascular disease--systematic review and meta-analysis. Neurobiol Aging. 2009;30:337–52. doi: 10.1016/j.neurobiolaging.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 39.Killilea DW, Wong SL, Cahaya HS, Atamna H, Ames BN. Iron accumulation during cellular senescence. Ann N Y Acad Sci. 2004;1019:365–67. doi: 10.1196/annals.1297.063. [DOI] [PubMed] [Google Scholar]
- 40.Williams R, Buchheit CL, Berman NE, LeVine SM. Pathogenic implications of iron accumulation in multiple sclerosis. J Neurochem. 2012;120:7–25. doi: 10.1111/j.1471-4159.2011.07536.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xu J, Jia Z, Knutson MD, Leeuwenburgh C. Impaired iron status in aging research. Int J Mol Sci. 2012;13:2368–86. doi: 10.3390/ijms13022368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hallgren B, Sourander P. The effect of age on the non-haemin iron in the human brain. J Neurochem. 1958;3:41–51. doi: 10.1111/j.1471-4159.1958.tb12607.x. [DOI] [PubMed] [Google Scholar]
- 43.Ramos P, Santos A, Pinto NR, Mendes R, Magalhães T, Almeida A. Iron levels in the human brain: a post-mortem study of anatomical region differences and age-related changes. J Trace Elem Med Biol. 2014;28:13–17. doi: 10.1016/j.jtemb.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 44.Hebbrecht G, Maenhaut W, De Reuck J. Brain trace elements and aging. Nucl Instrum Methods Phys Res B. 1999;150:208–13. [Google Scholar]
- 45.Zecca L, Shima T, Stroppolo A, et al. Interaction of Neuromelanin and iron in substantia nigra and other areas of human brain. Neuroscience. 1996;73:407–15. doi: 10.1016/0306-4522(96)00047-4. [DOI] [PubMed] [Google Scholar]
- 46.Zecca L, Tampellini D, Rizzio E, Giaveri G, Gallorini M. The determination of iron and other metals by INAA in cortex, cerebellum and putamen of human brain and in their neuromelanins. J Radioanal Nucl Chem. 2001;248:129–31. [Google Scholar]
- 47.House E, Esiri M, Forster G, Ince PG, Exley C. Aluminium, iron and copper in human brain tissues donated to the Medical Research Council’s Cognitive Function and Ageing Study. Metallomics. 2012;4:56–65. doi: 10.1039/c1mt00139f. [DOI] [PubMed] [Google Scholar]
- 48.Bartzokis G, Tishler TA, Lu PH, et al. Brain ferritin iron may influence age- and gender-related risks of neurodegeneration. Neurobiol Aging. 2007;28:414–23. doi: 10.1016/j.neurobiolaging.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 49.Aquino D, Bizzi A, Grisoli M, et al. Age-related iron deposition in the basal ganglia: quantitative analysis in healthy subjects. Radiology. 2009;252:165–72. doi: 10.1148/radiol.2522081399. [DOI] [PubMed] [Google Scholar]
- 50.Bartzokis G, Lu PH, Tingus K, et al. Gender and iron genes may modify associations between brain iron and memory in healthy aging. Neuropsychopharmacology. 2011;36:1375–84. doi: 10.1038/npp.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bilgic B, Pfefferbaum A, Rohlfing T, Sullivan EV, Adalsteinsson E. MRI estimates of brain iron concentration in normal aging using quantitative susceptibility mapping. Neuroimage. 2012;59:2625–35. doi: 10.1016/j.neuroimage.2011.08.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zucca FA, Bellei C, Giannelli S, et al. Neuromelanin and iron in human locus coeruleus and substantia nigra during aging: consequences for neuronal vulnerability. J Neural Transm. 2006;113:757–67. doi: 10.1007/s00702-006-0453-2. [DOI] [PubMed] [Google Scholar]
- 53.Zecca L, Bellei C, Costi P, et al. New melanic pigments in the human brain that accumulate in aging and block environmental toxic metals. Proc Natl Acad Sci USA. 2008;105:17567–72. doi: 10.1073/pnas.0808768105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Block ML, Zecca L, Hong JS. Microglia-mediated neurotoxicity: uncovering the molecular mechanisms. Nat Rev Neurosci. 2007;8:57–69. doi: 10.1038/nrn2038. [DOI] [PubMed] [Google Scholar]
- 55.Lopes KO, Sparks DL, Streit WJ. Microglial dystrophy in the aged and Alzheimer’s disease brain is associated with ferritin immunoreactivity. Glia. 2008;56:1048–60. doi: 10.1002/glia.20678. [DOI] [PubMed] [Google Scholar]
- 56.Schipper HM, Song W, Zukor H, Hascalovici JR, Zeligman D. Heme oxygenase-1 and neurodegeneration: expanding frontiers of engagement. J Neurochem. 2009;110:469–85. doi: 10.1111/j.1471-4159.2009.06160.x. [DOI] [PubMed] [Google Scholar]
- 57.Crichton RR, Ward RJ. Metal based neurodegeneration: from molecular mechanisms to therapeutic strategies. 2. Chichester: J Wiley & Sons; 2014. [Google Scholar]
- 58.Melis JP, van Steeg H, Luijten M. Oxidative DNA damage and nucleotide excision repair. Antioxid Redox Signal. 2013;18:2409–19. doi: 10.1089/ars.2012.5036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kwok JB. Role of epigenetics in Alzheimer’s and Parkinson’s disease. Epigenomics. 2010;2:671–82. doi: 10.2217/epi.10.43. [DOI] [PubMed] [Google Scholar]
- 60.Catalá A. Lipid peroxidation of membrane phospholipids generates hydroxy-alkenals and oxidized phospholipids active in physiological and/or pathological conditions. Chem Phys Lipids. 2009;157:1–11. doi: 10.1016/j.chemphyslip.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 61.Dalle-Donne I, Giustarini D, Colombo R, Rossi R, Milzani A. Protein carbonylation in human diseases. Trends Mol Med. 2003;9:169–76. doi: 10.1016/s1471-4914(03)00031-5. [DOI] [PubMed] [Google Scholar]
- 62.Perluigi M, Coccia R, Butterfield DA. 4-Hydroxy-2-nonenal, a reactive product of lipid peroxidation, and neurodegenerative diseases: a toxic combination illuminated by redox proteomics studies. Antioxid Redox Signal. 2012;17:1590–609. doi: 10.1089/ars.2011.4406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mastroberardino PG, Hoffman EK, Horowitz MP, et al. A novel transferrin/TfR2-mediated mitochondrial iron transport system is disrupted in Parkinson’s disease. Neurobiol Dis. 2009;34:417–31. doi: 10.1016/j.nbd.2009.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Horowitz MP, Greenamyre JT. Mitochondrial iron metabolism and its role in neurodegeneration. J Alzheimers Dis. 2010;20(suppl 2):S551–68. doi: 10.3233/JAD-2010-100354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schipper HM, Kotake Y, Janzen EG. Catechol oxidation by peroxidase-positive astrocytes in primary culture: an electron spin resonance study. J Neurosci. 1991;11:2170–76. doi: 10.1523/JNEUROSCI.11-07-02170.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sulzer D, Zecca L. Intraneuronal dopamine-quinone synthesis: a review. Neurotox Res. 2000;1:181–95. doi: 10.1007/BF03033289. [DOI] [PubMed] [Google Scholar]
- 67.Paris I, Martinez-Alvarado P, Cárdenas S, et al. Dopamine-dependent iron toxicity in cells derived from rat hypothalamus. Chem Res Toxicol. 2005;18:415–19. doi: 10.1021/tx0497144. [DOI] [PubMed] [Google Scholar]
- 68.Di Monte DA, Schipper HM, Hetts S, Langston JW. Iron-mediated bioactivation of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) in glial cultures. Glia. 1995;15:203–06. doi: 10.1002/glia.440150213. [DOI] [PubMed] [Google Scholar]
- 69.Hare DJ, Adlard PA, Doble PA, Finkelstein DI. Metallobiology of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine neurotoxicity. Metallomics. 2013;5:91–109. doi: 10.1039/c2mt20164j. [DOI] [PubMed] [Google Scholar]
- 70.Li WJ, Jiang H, Song N, Xie JX. Dose- and time-dependent alpha-synuclein aggregation induced by ferric iron in SK-N-SH cells. Neurosci Bull. 2010;26:205–10. doi: 10.1007/s12264-010-1117-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Yamamoto A, Shin RW, Hasegawa K, et al. Iron (III) induces aggregation of hyperphosphorylated tau and its reduction to iron (II) reverses the aggregation: implications in the formation of neurofibrillary tangles of Alzheimer’s disease. J Neurochem. 2002;82:1137–47. doi: 10.1046/j.1471-4159.2002.t01-1-01061.x. [DOI] [PubMed] [Google Scholar]
- 72.Liu Y, Connor JR. Iron and ER stress in neurodegenerative disease. Biometals. 2012;25:837–45. doi: 10.1007/s10534-012-9544-8. [DOI] [PubMed] [Google Scholar]
- 73.Ott M, Gogvadze V, Orrenius S, Zhivotovsky B. Mitochondria, oxidative stress and cell death. Apoptosis. 2007;12:913–22. doi: 10.1007/s10495-007-0756-2. [DOI] [PubMed] [Google Scholar]
- 74.Dixon SJ, Lemberg KM, Lamprecht MR, et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell. 2012;149:1060–72. doi: 10.1016/j.cell.2012.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Roberts BR, Ryan TM, Bush AI, Masters CL, Duce JA. The role of metallobiology and amyloid-β peptides in Alzheimer’s disease. J Neurochem. 2012;120(suppl 1):149–66. doi: 10.1111/j.1471-4159.2011.07500.x. [DOI] [PubMed] [Google Scholar]
- 76.Sayre LM, Perry G, Harris PL, Liu Y, Schubert KA, Smith MA. In situ oxidative catalysis by neurofibrillary tangles and senile plaques in Alzheimer’s disease: a central role for bound transition metals. J Neurochem. 2000;74:270–79. doi: 10.1046/j.1471-4159.2000.0740270.x. [DOI] [PubMed] [Google Scholar]
- 77.Perry G, Nunomura A, Hirai K, et al. Is oxidative damage the fundamental pathogenic mechanism of Alzheimer’s and other neurodegenerative diseases? Free Radic Biol Med. 2002;33:1475–79. doi: 10.1016/s0891-5849(02)01113-9. [DOI] [PubMed] [Google Scholar]
- 78.Altamura S, Muckenthaler MU. Iron toxicity in diseases of aging: Alzheimer’s disease, Parkinson’s disease and atherosclerosis. J Alzheimers Dis. 2009;16:879–95. doi: 10.3233/JAD-2009-1010. [DOI] [PubMed] [Google Scholar]
- 79.Guillemot J, Canuel M, Essalmani R, Prat A, Seidah NG. Implication of the proprotein convertases in iron homeostasis: proprotein convertase 7 sheds human transferrin receptor 1 and furin activates hepcidin. Hepatology. 2013;57:2514–24. doi: 10.1002/hep.26297. [DOI] [PubMed] [Google Scholar]
- 80.Silvestri L, Camaschella C. A potential pathogenetic role of iron in Alzheimer’s disease. J Cell Mol Med. 2008;12:1548–50. doi: 10.1111/j.1582-4934.2008.00356.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rogers JT, Randall JD, Cahill CM, et al. An iron-responsive element type II in the 5’-untranslated region of the Alzheimer’s amyloid precursor protein transcript. J Biol Chem. 2002;277:45518–28. doi: 10.1074/jbc.M207435200. [DOI] [PubMed] [Google Scholar]
- 82.Duce JA, Tsatsanis A, Cater MA, et al. Iron-export ferroxidase activity of β-amyloid precursor protein is inhibited by zinc in Alzheimer’s disease. Cell. 2010;142:857–67. doi: 10.1016/j.cell.2010.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ebrahimi KH, Hagedoorn PL, Hagen WR. A synthetic peptide with the putative iron binding motif of amyloid precursor protein (APP) does not catalytically oxidize iron. PLoS One. 2012;7:e40287. doi: 10.1371/journal.pone.0040287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Honarmand Ebrahimi K, Dienemann C, Hoefgen S, Than ME, Hagedoorn PL, Hagen WR. The amyloid precursor protein (APP) does not have a ferroxidase site in its E2 domain. PLoS One. 2013;8:e72177. doi: 10.1371/journal.pone.0072177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lei P, Ayton S, Finkelstein DI, et al. Tau deficiency induces parkinsonism with dementia by impairing APP-mediated iron export. Nat Med. 2012;18:291–95. doi: 10.1038/nm.2613. [DOI] [PubMed] [Google Scholar]
- 86.Schenck JF. Magnetic resonance imaging of brain iron. J Neurol Sci. 2003;207:99–102. doi: 10.1016/s0022-510x(02)00431-8. [DOI] [PubMed] [Google Scholar]
- 87.Haacke EM, Cheng NY, House MJ, et al. Imaging iron stores in the brain using magnetic resonance imaging. Magn Reson Imaging. 2005;23:1–25. doi: 10.1016/j.mri.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 88.Jack CR, Jr, Wengenack TM, Reyes DA, et al. In vivo magnetic resonance microimaging of individual amyloid plaques in Alzheimer’s transgenic mice. J Neurosci. 2005;25:10041–48. doi: 10.1523/JNEUROSCI.2588-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nabuurs RJ, Hegeman I, Natté R, et al. High-field MRI of single histological slices using an inductively coupled, self-resonant microcoil: application to ex vivo samples of patients with Alzheimer’s disease. NMR Biomed. 2011;24:351–57. doi: 10.1002/nbm.1598. [DOI] [PubMed] [Google Scholar]
- 90.Antharam V, Collingwood JF, Bullivant JP, et al. High field magnetic resonance microscopy of the human hippocampus in Alzheimer’s disease: quantitative imaging and correlation with iron. Neuroimage. 2012;59:1249–60. doi: 10.1016/j.neuroimage.2011.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Holland D, Brewer JB, Hagler DJ, Fennema-Notestine C, Dale AM and the Alzheimer’s Disease Neuroimaging Initiative. Subregional neuroanatomical change as a biomarker for Alzheimer’s disease. Proc Natl Acad Sci USA. 2009;106:20954–59. doi: 10.1073/pnas.0906053106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schröder N, Figueiredo LS, de Lima MN. Role of brain iron accumulation in cognitive dysfunction: evidence from animal models and human studies. J Alzheimers Dis. 2013;34:797–812. doi: 10.3233/JAD-121996. [DOI] [PubMed] [Google Scholar]
- 93.Holcomb L, Gordon MN, McGowan E, et al. Accelerated Alzheimer-type phenotype in transgenic mice carrying both mutant amyloid precursor protein and presenilin 1 transgenes. Nat Med. 1998;4:97–100. doi: 10.1038/nm0198-097. [DOI] [PubMed] [Google Scholar]
- 94.Smith MA, Hirai K, Hsiao K, et al. Amyloid-beta deposition in Alzheimer transgenic mice is associated with oxidative stress. J Neurochem. 1998;70:2212–15. doi: 10.1046/j.1471-4159.1998.70052212.x. [DOI] [PubMed] [Google Scholar]
- 95.Falangola MF, Lee SP, Nixon RA, Duff K, Helpern JA. Histological co-localization of iron in Abeta plaques of PS/APP transgenic mice. Neurochem Res. 2005;30:201–05. doi: 10.1007/s11064-004-2442-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Leskovjan AC, Kretlow A, Lanzirotti A, Barrea R, Vogt S, Miller LM. Increased brain iron coincides with early plaque formation in a mouse model of Alzheimer’s disease. Neuroimage. 2011;55:32–38. doi: 10.1016/j.neuroimage.2010.11.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hui Y, Wang D, Li W, et al. Long-term overexpression of heme oxygenase 1 promotes tau aggregation in mouse brain by inducing tau phosphorylation. J Alzheimers Dis. 2011;26:299–313. doi: 10.3233/JAD-2011-102061. [DOI] [PubMed] [Google Scholar]
- 98.Schipper HM, Cissé S, Stopa EG. Expression of heme oxygenase-1 in the senescent and Alzheimer-diseased brain. Ann Neurol. 1995;37:758–68. doi: 10.1002/ana.410370609. [DOI] [PubMed] [Google Scholar]
- 99.Schipper HM, Bennett DA, Liberman A, et al. Glial heme oxygenase-1 expression in Alzheimer disease and mild cognitive impairment. Neurobiol Aging. 2006;27:252–61. doi: 10.1016/j.neurobiolaging.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 100.Dexter DT, Wells FR, Agid F, et al. Increased nigral iron content in postmortem parkinsonian brain. Lancet. 1987;330:1219–20. doi: 10.1016/s0140-6736(87)91361-4. [DOI] [PubMed] [Google Scholar]
- 101.Dexter DT, Wells FR, Lees AJ, et al. Increased nigral iron content and alterations in other metal ions occurring in brain in Parkinson’s disease. J Neurochem. 1989;52:1830–36. doi: 10.1111/j.1471-4159.1989.tb07264.x. [DOI] [PubMed] [Google Scholar]
- 102.Riederer P, Sofic E, Rausch WD, et al. Transition metals, ferritin, glutathione, and ascorbic acid in parkinsonian brains. J Neurochem. 1989;52:515–20. doi: 10.1111/j.1471-4159.1989.tb09150.x. [DOI] [PubMed] [Google Scholar]
- 103.Hirsch EC, Brandel JP, Galle P, Javoy-Agid F, Agid Y. Iron and aluminum increase in the substantia nigra of patients with Parkinson’s disease: an X-ray microanalysis. J Neurochem. 1991;56:446–51. doi: 10.1111/j.1471-4159.1991.tb08170.x. [DOI] [PubMed] [Google Scholar]
- 104.Péran P, Cherubini A, Assogna F, et al. Magnetic resonance imaging markers of Parkinson’s disease nigrostriatal signature. Brain. 2010;133:3423–33. doi: 10.1093/brain/awq212. [DOI] [PubMed] [Google Scholar]
- 105.Gröger A, Berg D. Does structural neuroimaging reveal a disturbance of iron metabolism in Parkinson’s disease? Implications from MRI and TCS studies. J Neural Transm. 2012;119:1523–28. doi: 10.1007/s00702-012-0873-0. [DOI] [PubMed] [Google Scholar]
- 106.Faucheux BA, Bonnet AM, Agid Y, Hirsch EC. Blood vessels change in the mesencephalon of patients with Parkinson’s disease. Lancet. 1999;353:981–82. doi: 10.1016/S0140-6736(99)00641-8. [DOI] [PubMed] [Google Scholar]
- 107.Kortekaas R, Leenders KL, van Oostrom JC, et al. Blood-brain barrier dysfunction in parkinsonian midbrain in vivo. Ann Neurol. 2005;57:176–79. doi: 10.1002/ana.20369. [DOI] [PubMed] [Google Scholar]
- 108.Faucheux BA, Nillesse N, Damier P, et al. Expression of lactoferrin receptors is increased in the mesencephalon of patients with Parkinson disease. Proc Natl Acad Sci USA. 1995;92:9603–07. doi: 10.1073/pnas.92.21.9603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Salazar J, Mena N, Hunot S, et al. Divalent metal transporter 1 (DMT1) contributes to neurodegeneration in animal models of Parkinson’s disease. Proc Natl Acad Sci USA. 2008;105:18578–83. doi: 10.1073/pnas.0804373105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Borie C, Gasparini F, Verpillat P, et al. and the French Parkinson’s disease genetic study group. Association study between iron-related genes polymorphisms and Parkinson’s disease. J Neurol. 2002;249:801–04. doi: 10.1007/s00415-002-0704-6. [DOI] [PubMed] [Google Scholar]
- 111.Guerreiro RJ, Bras JM, Santana I, et al. Association of HFE common mutations with Parkinson’s disease, Alzheimer’s disease and mild cognitive impairment in a Portuguese cohort. BMC Neurol. 2006;6:24. doi: 10.1186/1471-2377-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Jellinger K, Paulus W, Grundke-Iqbal I, Riederer P, Youdim MB. Brain iron and ferritin in Parkinson’s and Alzheimer’s diseases. J Neural Transm Park Dis Dement Sect. 1990;2:327–40. doi: 10.1007/BF02252926. [DOI] [PubMed] [Google Scholar]
- 113.el-Agnaf OM, Irvine GB. Aggregation and neurotoxicity of alpha-synuclein and related peptides. Biochem Soc Trans. 2002;30:559–65. doi: 10.1042/bst0300559. [DOI] [PubMed] [Google Scholar]
- 114.Uversky VN, Li J, Fink AL. Metal-triggered structural transformations, aggregation, and fibrillation of human alphasynuclein. A possible molecular NK between Parkinson’s disease and heavy metal exposure. J Biol Chem. 2001;276:44284–96. doi: 10.1074/jbc.M105343200. [DOI] [PubMed] [Google Scholar]
- 115.Castellani RJ, Siedlak SL, Perry G, Smith MA. Sequestration of iron by Lewy bodies in Parkinson’s disease. Acta Neuropathol. 2000;100:111–14. doi: 10.1007/s004010050001. [DOI] [PubMed] [Google Scholar]
- 116.Dexter DT, Carayon A, Vidailhet M, et al. Decreased ferritin levels in brain in Parkinson’s disease. J Neurochem. 1990;55:16–20. doi: 10.1111/j.1471-4159.1990.tb08814.x. [DOI] [PubMed] [Google Scholar]
- 117.Dexter DT, Carayon A, Javoy-Agid F, et al. Alterations in the levels of iron, ferritin and other trace metals in Parkinson’s disease and other neurodegenerative diseases affecting the basal ganglia. Brain. 1991;114:1953–75. doi: 10.1093/brain/114.4.1953. [DOI] [PubMed] [Google Scholar]
- 118.Mann VM, Cooper JM, Daniel SE, et al. Complex I, iron, and ferritin in Parkinson’s disease substantia nigra. Ann Neurol. 1994;36:876–81. doi: 10.1002/ana.410360612. [DOI] [PubMed] [Google Scholar]
- 119.Connor JR, Snyder BS, Arosio P, Loeffler DA, LeWitt P. A quantitative analysis of isoferritins in select regions of aged, parkinsonian, and Alzheimer’s diseased brains. J Neurochem. 1995;65:717–24. doi: 10.1046/j.1471-4159.1995.65020717.x. [DOI] [PubMed] [Google Scholar]
- 120.Griffiths PD, Dobson BR, Jones GR, Clarke DT. Iron in the basal ganglia in Parkinson’s disease. An in vitro study using extended X-ray absorption fine structure and cryo-electron microscopy. Brain. 1999;122:667–73. doi: 10.1093/brain/122.4.667. [DOI] [PubMed] [Google Scholar]
- 121.Faucheux BA, Martin ME, Beaumont C, et al. Lack of up-regulation of ferritin is associated with sustained iron regulatory protein-1 binding activity in the substantia nigra of patients with Parkinson’s disease. J Neurochem. 2002;83:320–30. doi: 10.1046/j.1471-4159.2002.01118.x. [DOI] [PubMed] [Google Scholar]
- 122.Jellinger K, Kienzl E, Rumpelmair G, et al. Iron-melanin complex in substantia nigra of parkinsonian brains: an x-ray microanalysis. J Neurochem. 1992;59:1168–71. doi: 10.1111/j.1471-4159.1992.tb08362.x. [DOI] [PubMed] [Google Scholar]
- 123.Good PF, Olanow CW, Perl DP. Neuromelanin-containing neurons of the substantia nigra accumulate iron and aluminum in Parkinson’s disease: a LAMMA study. Brain Res. 1992;593:343–46. doi: 10.1016/0006-8993(92)91334-b. [DOI] [PubMed] [Google Scholar]
- 124.Faucheux BA, Martin ME, Beaumont C, Hauw JJ, Agid Y, Hirsch EC. Neuromelanin associated redox-active iron is increased in the substantia nigra of patients with Parkinson’s disease. J Neurochem. 2003;86:1142–48. doi: 10.1046/j.1471-4159.2003.01923.x. [DOI] [PubMed] [Google Scholar]
- 125.McGeer PL, Itagaki S, Boyes BE, McGeer EG. Reactive microglia are positive for HLA-DR in the substantia nigra of Parkinson’s and Alzheimer’s disease brains. Neurology. 1988;38:1285–91. doi: 10.1212/wnl.38.8.1285. [DOI] [PubMed] [Google Scholar]
- 126.Langston JW, Forno LS, Tetrud J, Reeves AG, Kaplan JA, Karluk D. Evidence of active nerve cell degeneration in the substantia nigra of humans years after 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine exposure. Ann Neurol. 1999;46:598–605. doi: 10.1002/1531-8249(199910)46:4<598::aid-ana7>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 127.Zecca L, Wilms H, Geick S, et al. Human Neuromelanin induces neuroinflammation and neurodegeneration in the rat substantia nigra: implications for Parkinson’s disease. Acta Neuropathol. 2008;116:47–55. doi: 10.1007/s00401-008-0361-7. [DOI] [PubMed] [Google Scholar]
- 128.Zhang W, Phillips K, Wielgus AR, et al. Neuromelanin activates microglia and induces degeneration of dopaminergic neurons: implications for progression of Parkinson’s disease. Neurotox Res. 2011;19:63–72. doi: 10.1007/s12640-009-9140-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lewis MM, Du G, Kidacki M, et al. Higher iron in the red nucleus marks Parkinson’s dyskinesia. Neurobiol Aging. 2013;34:1497–503. doi: 10.1016/j.neurobiolaging.2012.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Yu X, Du T, Song N, et al. Decreased iron levels in the temporal cortex in postmortem human brains with Parkinson disease. Neurology. 2013;80:492–95. doi: 10.1212/WNL.0b013e31827f0ebb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Boll MC, Sotelo J, Otero E, Alcaraz-Zubeldia M, Rios C. Reduced ferroxidase activity in the cerebrospinal fluid from patients with Parkinson’s disease. Neurosci Lett. 1999;265:155–58. doi: 10.1016/s0304-3940(99)00221-9. [DOI] [PubMed] [Google Scholar]
- 132.Boll MC, Alcaraz-Zubeldia M, Montes S, Rios C. Free copper, ferroxidase and SOD1 activities, lipid peroxidation and NO(x) content in the CSF. A different marker profile in four neurodegenerative diseases. Neurochem Res. 2008;33:1717–23. doi: 10.1007/s11064-008-9610-3. [DOI] [PubMed] [Google Scholar]
- 133.Martínez-Hernández R, Montes S, Higuera-Calleja J, et al. Plasma ceruloplasmin ferroxidase activity correlates with the nigral sonographic area in Parkinson’s disease patients: a pilot study. Neurochem Res. 2011;36:2111–15. doi: 10.1007/s11064-011-0535-x. [DOI] [PubMed] [Google Scholar]
- 134.Olivieri S, Conti A, Iannaccone S, et al. Ceruloplasmin oxidation, a feature of Parkinson’s disease CSF, inhibits ferroxidase activity and promotes cellular iron retention. J Neurosci. 2011;31:18568–77. doi: 10.1523/JNEUROSCI.3768-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Patel BN, Dunn RJ, Jeong SY, Zhu Q, Julien JP, David S. Ceruloplasmin regulates iron levels in the CNS and prevents free radical injury. J Neurosci. 2002;22:6578–86. doi: 10.1523/JNEUROSCI.22-15-06578.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ayton S, Lei P, Duce JA, et al. Ceruloplasmin dysfunction and therapeutic potential for Parkinson disease. Ann Neurol. 2013;73:554–59. doi: 10.1002/ana.23817. [DOI] [PubMed] [Google Scholar]
- 137.Hochstrasser H, Bauer P, Walter U, et al. Ceruloplasmin gene variations and substantia nigra hyperechogenicity in Parkinson disease. Neurology. 2004;63:1912–17. doi: 10.1212/01.wnl.0000144276.29988.c3. [DOI] [PubMed] [Google Scholar]
- 138.Pichler I, Del Greco MF, Gögele M, et al. and the PD GWAS Consortium, and the International Parkinson’s Disease Genomics Consortium, and the Wellcome Trust Case Control Consortium 2, and the Genetics of Iron Status Consortium. Serum iron levels and the risk of Parkinson disease: a mendelian randomization study. PLoS Med. 2013;10:e1001462. doi: 10.1371/journal.pmed.1001462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Miyake Y, Tanaka K, Fukushima W, et al. and the Fukuoka Kinki Parkinson’s Disease Study Group. Dietary intake of metals and risk of Parkinson’s disease: a case-control study in Japan. J Neurol Sci. 2011;306:98–102. doi: 10.1016/j.jns.2011.03.035. [DOI] [PubMed] [Google Scholar]
- 140.Logroscino G, Chen H, Wing A, Ascherio A. Blood donations, iron stores, and risk of Parkinson’s disease. Mov Disord. 2006;21:835–38. doi: 10.1002/mds.20826. [DOI] [PubMed] [Google Scholar]
- 141.Savica R, Grossardt BR, Carlin JM, et al. Anemia or low hemoglobin levels preceding Parkinson disease: a case-control study. Neurology. 2009;73:1381–87. doi: 10.1212/WNL.0b013e3181bd80c1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Levenson CW, Cutler RG, Ladenheim B, Cadet JL, Hare J, Mattson MP. Role of dietary iron restriction in a mouse model of Parkinson’s disease. Exp Neurol. 2004;190:506–14. doi: 10.1016/j.expneurol.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 143.Cho ZH, Oh SH, Kim JM, et al. Direct visualization of Parkinson’s disease by in vivo human brain imaging using 7.0T magnetic resonance imaging. Mov Disord. 2011;26:713–18. doi: 10.1002/mds.23465. [DOI] [PubMed] [Google Scholar]
- 144.Gorell JM, Ordidge RJ, Brown GG, Deniau JC, Buderer NM, Helpern JA. Increased iron-related MRI contrast in the substantia nigra in Parkinson’s disease. Neurology. 1995;45:1138–43. doi: 10.1212/wnl.45.6.1138. [DOI] [PubMed] [Google Scholar]
- 145.Martin WR, Wieler M, Gee M. Midbrain iron content in early Parkinson disease: a potential biomarker of disease status. Neurology. 2008;70:1411–17. doi: 10.1212/01.wnl.0000286384.31050.b5. [DOI] [PubMed] [Google Scholar]
- 146.Savoiardo M. Differential diagnosis of Parkinson’s disease and atypical parkinsonian disorders by magnetic resonance imaging. Neurol Sci. 2003;24(suppl 1):S35–37. doi: 10.1007/s100720300036. [DOI] [PubMed] [Google Scholar]
- 147.Boelmans K, Holst B, Hackius M, et al. Brain iron deposition fingerprints in Parkinson’s disease and progressive supranuclear palsy. Mov Disord. 2012;27:421–27. doi: 10.1002/mds.24926. [DOI] [PubMed] [Google Scholar]
- 148.Nakane T, Nihashi T, Kawai H, Naganawa S. Visualization of neuromelanin in the substantia nigra and locus ceruleus at 1·5T using a 3D-gradient echo sequence with magnetization transfer contrast. Magn Reson Med Sci. 2008;7:205–10. doi: 10.2463/mrms.7.205. [DOI] [PubMed] [Google Scholar]
- 149.Sasaki M, Shibata E, Kudo K, Tohyama K. Neuromelanin-sensitive MRI. Basics, technique and clinical applications. Clin Neuroradiol. 2008;18:147–53. [Google Scholar]
- 150.Sasaki M, Shibata E, Tohyama K, et al. Neuromelanin magnetic resonance imaging of locus ceruleus and substantia nigra in Parkinson’s disease. Neuroreport. 2006;17:1215–18. doi: 10.1097/01.wnr.0000227984.84927.a7. [DOI] [PubMed] [Google Scholar]
- 151.Ohtsuka C, Sasaki M, Konno K, et al. Changes in substantia nigra and locus coeruleus in patients with early-stage Parkinson’s disease using Neuromelanin-sensitive MR imaging. Neurosci Lett. 2013;541:93–98. doi: 10.1016/j.neulet.2013.02.012. [DOI] [PubMed] [Google Scholar]
- 152.Bouwmans AE, Vlaar AM, Srulijes K, Mess WH, Weber WE. Transcranial sonography for the discrimination of idiopathic Parkinson’s disease from the atypical parkinsonian syndromes. Int Rev Neurobiol. 2010;90:121–46. doi: 10.1016/S0074-7742(10)90009-3. [DOI] [PubMed] [Google Scholar]
- 153.Zecca L, Berg D, Arzberger T, et al. In vivo detection of iron and Neuromelanin by transcranial sonography: a new approach for early detection of substantia nigra damage. Mov Disord. 2005;20:1278–85. doi: 10.1002/mds.20550. [DOI] [PubMed] [Google Scholar]
- 154.Song N, Wang J, Jiang H, Xie J. Ferroportin 1 but not hephaestin contributes to iron accumulation in a cell model of Parkinson’s disease. Free Radic Biol Med. 2010;48:332–41. doi: 10.1016/j.freeradbiomed.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 155.Oestreicher E, Sengstock GJ, Riederer P, Olanow CW, Dunn AJ, Arendash GW. Degeneration of nigrostriatal dopaminergic neurons increases iron within the substantia nigra: a histochemical and neurochemical study. Brain Res. 1994;660:8–18. doi: 10.1016/0006-8993(94)90833-8. [DOI] [PubMed] [Google Scholar]
- 156.Neema M, Arora A, Healy BC, et al. Deep gray matter involvement on brain MRI scans is associated with clinical progression in multiple sclerosis. J Neuroimaging. 2009;19:3–8. doi: 10.1111/j.1552-6569.2008.00296.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Ropele S, de Graaf W, Khalil M, et al. MRI assessment of iron deposition in multiple sclerosis. J Magn Reson Imaging. 2011;34:13–21. doi: 10.1002/jmri.22590. [DOI] [PubMed] [Google Scholar]
- 158.Lassmann H, van Horssen J, Mahad D. Progressive multiple sclerosis: pathology and pathogenesis. Nat Rev Neurol. 2012;8:647–56. doi: 10.1038/nrneurol.2012.168. [DOI] [PubMed] [Google Scholar]
- 159.Hammond KE, Metcalf M, Carvajal L, et al. Quantitative in vivo magnetic resonance imaging of multiple sclerosis at 7 Tesla with sensitivity to iron. Ann Neurol. 2008;64:707–13. doi: 10.1002/ana.21582. [DOI] [PubMed] [Google Scholar]
- 160.Bagnato F, Hametner S, Yao B, et al. Tracking iron in multiple sclerosis: a combined imaging and histopathological study at 7 Tesla. Brain. 2011;134:3602–15. doi: 10.1093/brain/awr278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Yao B, Bagnato F, Matsuura E, et al. Chronic multiple sclerosis lesions: characterization with high-field-strength MR imaging. Radiology. 2012;262:206–15. doi: 10.1148/radiol.11110601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Mehindate K, Sahlas DJ, Frankel D, et al. Proinflammatory cytokines promote glial heme oxygenase-1 expression and mitochondrial iron deposition: implications for multiple sclerosis. J Neurochem. 2001;77:1386–95. doi: 10.1046/j.1471-4159.2001.00354.x. [DOI] [PubMed] [Google Scholar]
- 163.Campuzano V, Montermini L, Moltò MD, et al. Friedreich’s ataxia: autosomal recessive disease caused by an intronic GAA triplet repeat expansion. Science. 1996;271:1423–27. doi: 10.1126/science.271.5254.1423. [DOI] [PubMed] [Google Scholar]
- 164.Pandolfo M. Friedreich ataxia: new pathways. J Child Neurol. 2012;27:1204–11. doi: 10.1177/0883073812448534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Ye H, Rouault TA. Human iron-sulfur cluster assembly, cellular iron homeostasis, and disease. Biochemistry. 2010;49:4945–56. doi: 10.1021/bi1004798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Waldvogel D, van Gelderen P, Hallett M. Increased iron in the dentate nucleus of patients with Friedrich’s ataxia. Ann Neurol. 1999;46:123–25. doi: 10.1002/1531-8249(199907)46:1<123::aid-ana19>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 167.Koeppen AH. Friedreich’s ataxia: pathology, pathogenesis, and molecular genetics. J Neurol Sci. 2011;303:1–12. doi: 10.1016/j.jns.2011.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Keogh MJ, Chinnery PF. Current concepts and controversies in neurodegeneration with brain iron accumulation. Semin Pediatr Neurol. 2012;19:51–56. doi: 10.1016/j.spen.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 169.Schipper HM. Neurodegeneration with brain iron accumulation–clinical syndromes and neuroimaging. Biochim Biophys Acta. 2012;1822:350–60. doi: 10.1016/j.bbadis.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 170.Rouault TA. Iron metabolism in the CNS: implications for neurodegenerative diseases. Nat Rev Neurosci. 2013;14:551–64. doi: 10.1038/nrn3453. [DOI] [PubMed] [Google Scholar]
- 171.Dusek P, Schneider SA. Neurodegeneration with brain iron accumulation. Curr Opin Neurol. 2012;25:499–506. doi: 10.1097/WCO.0b013e3283550cac. [DOI] [PubMed] [Google Scholar]
- 172.Gregory A, Hayflick SJ. Genetics of neurodegeneration with brain iron accumulation. Curr Neurol Neurosci Rep. 2011;11:254–61. doi: 10.1007/s11910-011-0181-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Schneider SA, Dusek P, Hardy J, Westenberger A, Jankovic J, Bhatia KP. Genetics and pathophysiology of neurodegeneration with brain iron accumulation (NBIA) Curr Neuropharmacol. 2013;11:59–79. doi: 10.2174/157015913804999469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Kruer MC, Hiken M, Gregory A, et al. Novel histopathologic findings in molecularly-confirmed pantothenate kinase-associated neurodegeneration. Brain. 2011;134:947–58. doi: 10.1093/brain/awr042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Kruer MC, Boddaert N, Schneider SA, et al. Neuroimaging features of neurodegeneration with brain iron accumulation. AJNR Am J Neuroradiol. 2012;33:407–14. doi: 10.3174/ajnr.A2677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Zhou B, Westaway SK, Levinson B, Johnson MA, Gitschier J, Hayflick SJ. A novel pantothenate kinase gene (PANK2) is defective in Hallervorden-Spatz syndrome. Nat Genet. 2001;28:345–49. doi: 10.1038/ng572. [DOI] [PubMed] [Google Scholar]
- 177.Morgan NV, Westaway SK, Morton JE, et al. PLA2G6, encoding a phospholipase A2, is mutated in neurodegenerative disorders with high brain iron. Nat Genet. 2006;38:752–54. doi: 10.1038/ng1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Kurian MA, Morgan NV, MacPherson L, et al. Phenotypic spectrum of neurodegeneration associated with mutations in the PLA2G6 gene (PLAN) Neurology. 2008;70:1623–29. doi: 10.1212/01.wnl.0000310986.48286.8e. [DOI] [PubMed] [Google Scholar]
- 179.Kruer MC, Paisán-Ruiz C, Boddaert N, et al. Defective FA2H leads to a novel form of neurodegeneration with brain iron accumulation (NBIA) Ann Neurol. 2010;68:611–18. doi: 10.1002/ana.22122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Ramirez A, Heimbach A, Gründemann J, et al. Hereditary parkinsonism with dementia is caused by mutations in ATP13A2, encoding a lysosomal type 5 P-type ATPase. Nat Genet. 2006;38:1184–91. doi: 10.1038/ng1884. [DOI] [PubMed] [Google Scholar]
- 181.Schneider SA, Paisan-Ruiz C, Quinn NP, et al. ATP13A2 mutations (PARK9) cause neurodegeneration with brain iron accumulation. Mov Disord. 2010;25:979–84. doi: 10.1002/mds.22947. [DOI] [PubMed] [Google Scholar]
- 182.Chien HF, Bonifati V, Barbosa ER. ATP13A2-related neurodegeneration (PARK9) without evidence of brain iron accumulation. Mov Disord. 2011;26:1364–65. doi: 10.1002/mds.23514. [DOI] [PubMed] [Google Scholar]
- 183.Hayflick SJ, Kruer MC, Gregory A, et al. β-Propeller protein-associated neurodegeneration: a new X-linked dominant disorder with brain iron accumulation. Brain. 2013;136:1708–17. doi: 10.1093/brain/awt095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Madsen E, Gitlin JD. Copper and iron disorders of the brain. Annu Rev Neurosci. 2007;30:317–37. doi: 10.1146/annurev.neuro.30.051606.094232. [DOI] [PubMed] [Google Scholar]
- 185.Chinnery PF, Crompton DE, Birchall D, et al. Clinical features and natural history of neuroferritinopathy caused by the FTL1 460InsA mutation. Brain. 2007;130:110–19. doi: 10.1093/brain/awl319. [DOI] [PubMed] [Google Scholar]
- 186.Keogh MJ, Jonas P, Coulthard A, Chinnery PF, Burn J. Neuroferritinopathy: a new inborn error of iron metabolism. Neurogenetics. 2012;13:93–96. doi: 10.1007/s10048-011-0310-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Vidal R, Miravalle L, Gao X, et al. Expression of a mutant form of the ferritin light chain gene induces neurodegeneration and iron overload in transgenic mice. J Neurosci. 2008;28:60–67. doi: 10.1523/JNEUROSCI.3962-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Deng X, Vidal R, Englander EW. Accumulation of oxidative DNA damage in brain mitochondria in mouse model of hereditary ferritinopathy. Neurosci Lett. 2010;479:44–48. doi: 10.1016/j.neulet.2010.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Ohta E, Takiyama Y. MRI findings in neuroferritinopathy. Neurol Res Int. 2012;2012:197438. doi: 10.1155/2012/197438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.McNeill A, Gorman G, Khan A, Horvath R, Blamire AM, Chinnery PF. Progressive brain iron accumulation in neuroferritinopathy measured by the thalamic T2* relaxation rate. AJNR Am J Neuroradiol. 2012;33:1810–13. doi: 10.3174/ajnr.A3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Fasano A, Colosimo C, Miyajima H, Tonali PA, Re TJ, Bentivoglio AR. Aceruloplasminemia: a novel mutation in a family with marked phenotypic variability. Mov Disord. 2008;23:751–55. doi: 10.1002/mds.21938. [DOI] [PubMed] [Google Scholar]
- 192.Walker FO. Huntington’s disease. Lancet. 2007;369:218–28. doi: 10.1016/S0140-6736(07)60111-1. [DOI] [PubMed] [Google Scholar]
- 193.Hilditch-Maguire P, Trettel F, Passani LA, Auerbach A, Persichetti F, MacDonald ME. Huntingtin: an iron-regulated protein essential for normal nuclear and perinuclear organelles. Hum Mol Genet. 2000;9:2789–97. doi: 10.1093/hmg/9.19.2789. [DOI] [PubMed] [Google Scholar]
- 194.Bartzokis G, Lu PH, Tishler TA, et al. Myelin breakdown and iron changes in Huntington’s disease: pathogenesis and treatment implications. Neurochem Res. 2007;32:1655–64. doi: 10.1007/s11064-007-9352-7. [DOI] [PubMed] [Google Scholar]
- 195.Bartzokis G, Cummings J, Perlman S, Hance DB, Mintz J. Increased basal ganglia iron levels in Huntington disease. Arch Neurol. 1999;56:569–74. doi: 10.1001/archneur.56.5.569. [DOI] [PubMed] [Google Scholar]
- 196.Jurgens CK, Jasinschi R, Ekin A, et al. MRI T2 Hypointensities in basal ganglia of premanifest Huntington’s disease. PLoS Curr. 2010;8:RRN1173. doi: 10.1371/currents.RRN1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Allen RP, Barker PB, Wehrl F, Song HK, Earley CJ. MRI measurement of brain iron in patients with restless legs syndrome. Neurology. 2001;56:263–65. doi: 10.1212/wnl.56.2.263. [DOI] [PubMed] [Google Scholar]
- 198.Allen RP, Earley CJ. The role of iron in restless legs syndrome. Mov Disord. 2007;22(suppl 18):S440–48. doi: 10.1002/mds.21607. [DOI] [PubMed] [Google Scholar]
- 199.Connor JR, Boyer PJ, Menzies SL, et al. Neuropathological examination suggests impaired brain iron acquisition in restless legs syndrome. Neurology. 2003;61:304–09. doi: 10.1212/01.wnl.0000078887.16593.12. [DOI] [PubMed] [Google Scholar]
- 200.Connor JR, Wang XS, Patton SM, et al. Decreased transferrin receptor expression by Neuromelanin cells in restless legs syndrome. Neurology. 2004;62:1563–67. doi: 10.1212/01.wnl.0000123251.60485.ac. [DOI] [PubMed] [Google Scholar]
- 201.Ondo WG. Intravenous iron dextran for severe refractory restless legs syndrome. Sleep Med. 2010;11:494–96. doi: 10.1016/j.sleep.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 202.Duyn JH. The future of ultra-high field MRI and fMRI for study of the human brain. Neuroimage. 2012;62:1241–48. doi: 10.1016/j.neuroimage.2011.10.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Langkammer C, Schweser F, Krebs N, et al. Quantitative susceptibility mapping (QSM) as a means to measure brain iron? A post mortem validation study. Neuroimage. 2012;62:1593–99. doi: 10.1016/j.neuroimage.2012.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Duyn J. MR susceptibility imaging. J Magn Reson. 2013;229:198–207. doi: 10.1016/j.jmr.2012.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Fukunaga M, Li TQ, van Gelderen P, et al. Layer-specific variation of iron content in cerebral cortex as a source of MRI contrast. Proc Natl Acad Sci USA. 2010;107:3834–39. doi: 10.1073/pnas.0911177107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Bian W, Harter K, Hammond-Rosenbluth KE, et al. A serial in vivo 7T magnetic resonance phase imaging study of white matter lesions in multiple sclerosis. Mult Scler. 2013;19:69–75. doi: 10.1177/1352458512447870. [DOI] [PubMed] [Google Scholar]
- 207.Kwan JY, Jeong SY, Van Gelderen P, et al. Iron accumulation in deep cortical layers accounts for MRI signal abnormalities in ALS: correlating 7 tesla MRI and pathology. PLoS One. 2012;7:e35241. doi: 10.1371/journal.pone.0035241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Yablonskiy DA, Luo J, Sukstanskii AL, Iyer A, Cross AH. Biophysical mechanisms of MRI signal frequency contrast in multiple sclerosis. Proc Natl Acad Sci USA. 2012;109:14212–17. doi: 10.1073/pnas.1206037109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Sati P, van Gelderen P, Silva AC, et al. Micro-compartment specific T2* relaxation in the brain. Neuroimage. 2013;77:268–78. doi: 10.1016/j.neuroimage.2013.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Boddaert N, Le Quan Sang KH, Rötig A, et al. Selective iron chelation in Friedreich ataxia: biologic and clinical implications. Blood. 2007;110:401–08. doi: 10.1182/blood-2006-12-065433. [DOI] [PubMed] [Google Scholar]
- 211.Hocq A, Brouette N, Saussez S, Luhmer M, Gillis P, Gossuin Y. Variable-field relaxometry of iron-containing human tissues: a preliminary study. Contrast Media Mol Imaging. 2009;4:157–64. doi: 10.1002/cmmi.275. [DOI] [PubMed] [Google Scholar]
- 212.Kaur D, Yantiri F, Rajagopalan S, et al. Genetic or pharmacological iron chelation prevents MPTP-induced neurotoxicity in vivo: a novel therapy for Parkinson’s disease. Neuron. 2003;37:899–909. doi: 10.1016/s0896-6273(03)00126-0. [DOI] [PubMed] [Google Scholar]
- 213.Kwiatkowski A, Ryckewaert G, Jissendi Tchofo P, et al. Long-term improvement under deferiprone in a case of neurodegeneration with brain iron accumulation. Parkinsonism Relat Disord. 2012;18:110–12. doi: 10.1016/j.parkreldis.2011.06.024. [DOI] [PubMed] [Google Scholar]
- 214.Devos D, Moreau C, Kluza V, et al. Disease modifying strategy based upon iron chelation in Parkinson’s disease: a translational study. Neurology. 2012;78(suppl) P02.240. [Google Scholar]
- 215.Moreau C, Devedjian J-C, Kluza J, et al. Targeting brain chelatable iron as a therapeutic strategy for Parkinson’s disease. Translational and clinical studies. Am J Hematol. 2013;88:e36. (abstr) [Google Scholar]
- 216.Dexter D, Ward R, Crichton R, Kallo V, Srai SK. Altered brain iron homeostasis in Parkinson’s disease and potential for iron chelation therapy. Am J Hematol. 2013;88:e163. (abstr) [Google Scholar]
- 217.Crapper McLachlan DR, Kruck TP, Kalow W, et al. Intramuscular desferrioxamine in patients with Alzheimer’s disease. Lancet. 1991;337:1304–08. doi: 10.1016/0140-6736(91)92978-b. [DOI] [PubMed] [Google Scholar]
- 218.Crouch PJ, Savva MS, Hung LW, et al. The Alzheimer’s therapeutic PBT2 promotes amyloid-β degradation and GSK3 phosphorylation via a metal chaperone activity. J Neurochem. 2011;119:220–30. doi: 10.1111/j.1471-4159.2011.07402.x. [DOI] [PubMed] [Google Scholar]
- 219.Lannfelt L, Blennow K, Zetterberg H, et al. on behalf of the PBT2-201-EURO study group. Safety, efficacy, and biomarker findings of PBT2 in targeting Aβ as a modifying therapy for Alzheimer’s disease: a phase IIa, double-blind, randomised, placebo-controlled trial. Lancet Neurol. 2008;7:779–86. doi: 10.1016/S1474-4422(08)70167-4. [DOI] [PubMed] [Google Scholar]
- 220.Velasco-Sánchez D, Aracil A, Montero R, et al. Combined therapy with idebenone and deferiprone in patients with Friedreich’s ataxia. Cerebellum. 2011;10:1–8. doi: 10.1007/s12311-010-0212-7. [DOI] [PubMed] [Google Scholar]
- 221.Loréal O, Turlin B, Pigeon C, et al. Aceruloplasminemia: new clinical, pathophysiological and therapeutic insights. J Hepatol. 2002;36:851–56. doi: 10.1016/s0168-8278(02)00042-9. [DOI] [PubMed] [Google Scholar]
- 222.Miyajima H, Takahashi Y, Kamata T, Shimizu H, Sakai N, Gitlin JD. Use of desferrioxamine in the treatment of aceruloplasminemia. Ann Neurol. 1997;41:404–07. doi: 10.1002/ana.410410318. [DOI] [PubMed] [Google Scholar]
- 223.Suzuki Y, Yoshida K, Aburakawa Y, et al. Effectiveness of oral iron chelator treatment with deferasirox in an aceruloplasminemia patient with a novel ceruloplasmin gene mutation. Intern Med. 2013;52:1527–30. doi: 10.2169/internalmedicine.52.0102. [DOI] [PubMed] [Google Scholar]
- 224.Mariani R, Arosio C, Pelucchi S, et al. Iron chelation therapy in aceruloplasminaemia: study of a patient with a novel missense mutation. Gut. 2004;53:756–58. doi: 10.1136/gut.2003.030429. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.