Abstract
Exercise, particularly Tai Chi, has many known benefits, especially in reducing fall risk. However, exercise studies have tended to exclude older adults with dementia (OAD), who may be at high fall risk but have difficulty participating in formal exercise programs. This paper describes development and feasibility testing of a Tai Chi fall risk reduction exercise protocol, the positive emotion–motivated Tai Chi (PEM-TC) program for OAD, and explores strategies that facilitate their participation in and adherence to exercise programs. Preliminary data indicates that difficulties in delivering exercise to OAD may be eased by using the Sticky Hands Tai Chi teaching technique. Family members may have the optimum advantage in using Sticky Hands because of established emotional connections with their OAD.
Keywords: dementia, Tai Chi exercise, Sticky Hands, emotional intervention approach
Falls and adverse consequences are common in older adults with dementia (OAD). Due to cognitive and physical frailties, OAD experience a three-fold risk of falling compared to adults who are unimpaired (Buchner & Larson, 1987), and when falling, OAD have a three- to four-fold risk of severe fall-related injuries or mortality (van Doorn et al., 2003). Specific cognition-related motor functions (e.g., dual-task performance) are early markers of Alzheimer’s disease (AD), and their deterioration may add to fall risk (Holtzer et al., 2007). Anticipated growth in the number of OAD, a high incidence of falls and injuries among them, and the burden that dementia poses to family caregivers, emphasize the need for evidence-based fall prevention efforts.
Physical and mental benefits of exercise are widely recognized, but the extent to which OAD can benefit from them is uncertain. Currently, this area of research faces three challenges: (a) inconsistent effects of exercise training on health-related physical fitness outcomes in OAD (Hauer, Becker, Lindemann, & Beyer, 2006; Heyn, Abreu, & Ottenbacher, 2004); (b) inadequacy of one exercise treatment for all participants regardless of cognitive capability (Hauer et al., 2006); and (c) lack of adaptations necessary for OAD to enhance exercise adherence. With few exceptions (Arkin, 1999; Brill, Drimmer, Morgan, & Gordon, 1995; Teri et al., 1998), program adaptations and feasibility have not been examined. OAD often have difficulty following instructions, verbalizing their needs, and initiating activities on their own, thus creating challenges for engaging and maintaining them in an exercise program. This article describes a Tai Chi fall risk reduction exercise protocol, the positive emotion–motivated Tai Chi (PEM-TC) program for OAD, and explores its feasibility for overcoming these challenges.
TAI CHI EXERCISE FOR OAD
In a meta-analysis of multicenter trials of multifactorial strategies to reduce falls in older adults, sponsored by the National Institutes of Aging and Nursing Research, short-term exercises, particularly balance training, were found to reduce falls and fall-related injuries in the elderly (Province et al., 1995). A Tai Chi intervention had the lowest incidence ratio (IR) with a significant decrease (IR = 0.63, p = .01) in the risk for falling (Province et al., 1995). Since this study, data continue to support Tai Chi’s wide spectrum of benefits in reducing anxiety, falls and related injuries, and in improving mood and self-esteem, cardiorespiratory functions, muscle strength, flexibility, and balance (Lan, Lai, & Chen, 2002; Wu, 2002).
Tai Chi has drawn increasing attention within rehabilitation and the geriatric communities as an exercise for improving balance and decreasing fall risks. Tai Chi emphasizes slow movements that enhance body alignment and improve balance, so are suitable and safe for older adults (Christou, Yang, & Rosengren, 2003; Hartman et al., 2000; Hong, Li, & Robinson, 2000; Li, Harmer, Fisher, & McAuley, 2004; Li et al., 2005; Li et al., 2001; Taylor-Piliae, Haskell, Stotts, & Froelicher, 2006; Wolf et al., 1996; Wong, Lin, Chou, Tang, & Wong, 2001; Wu, 2002; Xu et al., 2004; Zeeuwe et al., 2006). An additional benefit is that Tai Chi participants may continue practicing after the study ends, suggesting its long-term feasibility as an exercise of choice by older adults (Li et al., 2005). However, Tai Chi study participants who experienced dramatic fall reductions were largely cognitively intact older adults. Few studies address how patients with cognitive impairment, such as AD, could benefit from Tai Chi. Most fall prevention studies have excluded older adults who did not cooperate or were significantly cognitively impaired, whether these OAD could not or would not follow exercise instruction is unclear.
Exercise adherence is another important consideration (Li et al., 2005; Nowalk, Prendergast, Bayles, D’Amico, & Colvin, 2001). In a cohort of long-term care residents with dementia, combined forms of exercises (including Tai Chi), did not reduce falls, compared to controls (Nowalk et al., 2001). Lack of treatment differences may have been due to a low adherence rate, suggesting the need for individualized interventions that can be adapted to patients’ varying and changing capabilities (Nowalk et al., 2001). Jensen and colleagues (2003) hypothesized an association between level of cognitive impairment and exercise adherence and program effects. Using data from nine residential facilities in Sweden, participants in the lower Mini-Mental State Examination (MMSE) (<19) group were reported to have lower exercise adherence (42% vs. 67%, p < .01), and were less likely to have a reduction in fall risk compared with those in the higher MMSE (≥19) group ( Jensen et al., 2003). These data underscore the difficulty in getting cognitively impaired older adults to comply with an exercise program and further justify the need to develop a program specifically for them.
Successful Exercise/Physical Activity Training With OAD
Despite these challenges, evidence of success of exercise intervention for OAD is increasing. In institutionalized demented patients (including AD, MMSE <21, mean 16) with histories of falling, mobility performance can be improved by 16 weeks of exercise training (Toulotte, Fabre, Dangremont, Lensel, & Thevenon, 2003). The 10 participants in the exercise group were divided into 2 groups of 5, attended 45-minute exercise sessions twice weekly, and were supervised by 2 physicians. Participants performed exercises to improve muscular strength, proprioception, static and dynamic balance, and flexibility. These participants showed significant improvement in all domains of outcome measures including balance, walk speed, and flexibility, compared with 10 controls who continued their daily routines. Authors acknowledged that participants always had difficulty understanding the instructions in a subsequent session and could not remember their instructors’ names, but were enthusiastic during the training sessions. Little information was given regarding motivation and adherence over the 16-week period.
It is likely that program modifications, although sparse in the literature, are keys to success in training. Brill and colleagues (1995) found that utilizing simple exercise movements with continual repetition through 1:1 instruction were the keys to making a strength and flexibility training program for OAD successful. This was a program at a skilled nursing facility led by a professional trainer over 11 weeks, at 3 times per week, for 20 minutes per session. All participants, including the most severely demented individuals (MMSE 5–22), could follow the exercise routine with 100% attendance. Arkin (1999) conducted a student-supervised 1:1 community rehabilitation program. Multimodality interventions on language performance, cognitive decline, physical fitness, and mood were provided to 24 persons with early-to-moderate stage of AD. Although labor intensive, the transportation, supervision, and motivational support that students provided led to improved exercise adherence. Teri and colleagues (1998) reported high exercise adherence in 153 community-dwelling AD (mean MMSE 18, mean age 78) patients by using family caregivers as exercise facilitators. Health professionals provided strength, flexibility, and balance training to persons with AD through home visits 2 times a week for the first 3 weeks, followed by weekly sessions for 4 weeks, and then biweekly sessions for the next 4 weeks. Alternating with professional trained exercise days, caregivers facilitated the exercise or accompanied the patients to walk for at least 30 minutes. Patients’ adherence to the program was encouraging: 100% of participants were compliant with part of the exercise recommendations, and 38% completed all exercises that were assigned each week. These studies indicate that AD patients, who are provided with 1:1 exercise facilitation and positive motivational reinforcement, can participate in and adhere to an exercise program.
In sum, we believe that part of the difficulties with existing exercise interventions has been a lack of clear attention to the link between cognitive impairment and remaining cognitive function, together with approaches that minimize the former and optimize the latter. Using techniques to improve motivation and emphasize procedural type training routines may lead to improved adherence and performance of an exercise routine in participants with dementia. While Tai Chi has many benefits that could help OAD, whether or not these benefits actually do accrue to them is unknown. Factors affecting our ability to answer such questions hinge on knowledge of the capacity and willingness of OAD to participate effectively and, perhaps more importantly, on modifications to exercise protocols that can enhance adherence and effectiveness, such as choice, individualization, and use of the emotional memory enhancement effect to reinforce exercise learning and motivation.
PEM-TC PROTOCOL: RATIONALE AND INTERVENTION DEVELOPMENT
The PEM-TC protocol was developed for use with community-dwelling people with AD, who were ambulatory (with or without assistive devices, able to take one step without assistance) and medically stable.
Definition of PEM-TC
PEM-TC is a training approach that has two unique aspects: one is the use of positive emotion–motivators (PEMs) incorporated into the Tai Chi experience, another is the use of hand touch in Tai Chi teaching. These aspects were intended to enhance enjoyment of the exercise program, reduce the program’s cognitive demand, and improve adherence and learning.
Emotional–Memory Enhancement Effect
The rationale for the PEM approach is based on use of spared mental functions in AD, that is, brain mechanisms and circuits (e.g., the basal ganglia, the cerebellum and supplementary areas) that govern primary emotional responses (Yao & Algase, 2006, 2008), and implicit memory (Budson & Price, 2005), that is, unconscious, procedural memory that develops as a result of a repetitive task. Implicit memory is evident when a person can stay on task (or improve) despite their inability to consciously recollect memories that facilitate the task. These spared functions can be optimized by using appropriate intervention techniques.
Emotional–memory enhancement effect refers to the phenomenon that emotional arousal leads to enhanced memory. Although data to date have been mixed as to whether memory enhancement effect is intact in AD (Hamann, Monarch, & Goldstein, 2000; Kazui et al., 2000; Kensinger, Brierley, Medford, Growdon, & Corkin, 2002; Moayeri, Cahill, Jin, & Potkin, 2000), emotional reactions (as measured by patterns of arousal ratings, skin-conductance responses, etc.) in these patients are normal. Discrepancies noted in studies of the memory enhancement effect for OAD may be due to confounding effects of degree of damage to the amygdala (Mori et al., 1999), type of emotional stimuli and richness of information available (Kensinger et al., 2002), easiness of the recall test (Mori et al., 1999), and test mode (i.e., real-life stories vs. pictures, semantic vs. procedural instruction) in relevant studies.
Studies showed that although patients with AD exhibit deficits in explicit memory and in conceptual memory tasks that rely on the cortical areas damaged in AD, implicit cue–outcome learning (Eldridge, Masterman, & Knowlton, 2002; Hussian, 1982) is unaffected. It can be argued that patients may benefit from implicit learning using primary emotional stimulation as positive reinforcement, even late in the disease process.
Sticky Hands Technique
Considering declining abilities in initiating movements and in language skills as dementia advances, PEM-TC uses the Sticky Hands technique to pair a family caregiver with the OAD. Sticky Hands in Tai Chi is a training technique practiced with a partner. The idea is for the partners to help each other to learn the various movements by sticking to, or maintaining contact with, each other. The original goal of this technique is to learn to use sensitivity, not brute force, to disrupt the opponent’s balance by attacking his or her center of gravity (Patience T’ai Chi Association, 2007). Sticky Hands in this study is primarily a way to deliver sensory assistance from an exercise partner’s bodily movements (kinesthetic facilitation), and to minimize the cognitive challenge that Tai Chi moves may pose to the participant. In our opinion, a main part of this technique involves teaching the participant and caregiver to maintain palm contact as a way of teaching movements and enhancing balance; the second value of this technique is its reliance on and promotion of a comfortably intimate interaction between the two persons.
Selection of Tai Chi Movements
Tai Chi movements demand body alignment and stance balance and are usually performed in a semi-squat position to enhance loading of the muscles and motion ranges of the lower limb and joints. Whereas conventional Tai Chi focuses on practicing Tai Chi postural sequences, repetitions of single Tai Chi postures leads to faster and more accurate neuromuscular activations that are crucial for an effective response to slips and trips (Gatts & Woollacott, 2006). Studies have shown that simplified, short forms of Tai Chi-based movements improve balance and reduce the risk of falls in the elderly (Li et al., 2005; Wolf et al., 1996; Wu, 2002). For this protocol, exercise moves were carefully selected and developed to incorporate the Sticky Hands technique, preserve the essence of Tai Chi’s balance improvement properties, and be simple. There were six main exercise moves selected that focus on weight shifts in multiple directions: hip and ankle rotations; ankle and knee flexion; trunk rotation; stepping motions forward, backward, and laterally; and unipedal stance on the basis of Yang-style Tai Chi forms. Warm-up and cool-down procedures were also adapted from Tai Chi forms that emphasize breathing and relaxation, in addition to balance and mobility training.
Positive Emotion Motivators to Enhance Adherence
The PEM-TC protocol builds upon an established emotional connection existing between the caregiver and the person with dementia. During Tai Chi practice, caregiver partners perform implicit instruction (kinesthetic facilitation, i.e., sensory assistance from their own body movements through the Sticky Hands technique), and explicit verbal cuing with each exercise move. Additionally, caregiver’s encouragement and recognition of the participant’s performance are emphasized throughout the intervention to reinforce their motivation to continue exercise.
Further, to understand what common motivators work better for OAD, pleasure-inducing events for each participant were identified using the Pleasant Events Schedule-AD-Short Form (PES-AD) (Logsdon & Teri, 1997) at enrollment. The PES-AD checklist asks caregivers to rate whether their patient now enjoys each of 20 activities (yes or no), and how frequently they engaged in each activity during the prior month. Pleasure-inducing events identified are later incorporated into the Tai Chi intervention, as either an exercise background or an incentive/reward for practicing Tai Chi.
PEM-TC PROTOCOL IMPLEMENTATION
Design
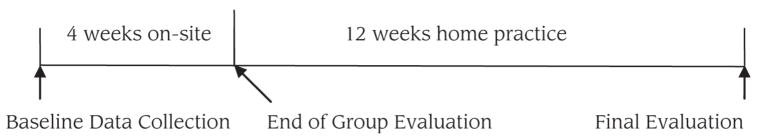
As out main goal was to determine feasibility and acceptability of the PEM-TC protocol for persons with AD and their caregivers, we used a pretest/posttest design, with participants serving as their own controls. Data collection was performed at 3 points: baseline, end of the 4-week on-site group sessions, and end of the 12-week home exercise period (see Figure 1).
Figure 1.
Study design.
The Institutional Review Board–Medicine at the University of Michigan approved all procedures. Preventive safety measures (environmental hazards assessment, i.e., uneven floors, shoe fit) were performed by caregivers at home to prevent accidental falls while practicing.
Participants
The protocol was tested on 20 participants, consisting of 10 persons with probable or possible AD and 10 caregivers. The AD patient–caregiver dyads were recruited from the Aging/Dementia Research Registry at the Michigan Alzheimer’s Disease Research Center (MADRC). Individuals with frontotemporal or Parkinson’s dementia and those for whom standing physical exercise is contraindicated were not considered candidates for this protocol. A family caregiver/friend who was actively involved with the patient and willing to participate and facilitate the group and home exercise sessions was a requirement. Caregivers were free of cognitive or physical impairments that might render them unable to facilitate the Tai Chi instruction.
Mean age of the AD participants was 79.2 ± 6.6 (range 63.1–86.8). Mean MMSE score was 17.20 ± 6.1 (range 6–23). Most of the participants had multiple medical conditions, such as hypertension, diabetes, congestive heart failure, and osteoporosis. Caregivers were spouses (n = 5) and daughters (n = 4) with a mean age 65 years ± 13, there was also one paid caregiver (22 years old). There were 8 of the 10 dyads that completed final assessment (attrition rate 20%). One dyad dropped out of the study after the group class because of significant changes in a medical condition unrelated to the research project. The other dyad did not return calls for a final follow-up.
Measures
Feasibility Measures
Family caregivers filled out a standardized patient Tai Chi practice log to track Tai Chi practice time per session, participant’s response and acceptance to the Tai Chi program, and possible reasons if the participant failed to cooperate. The research investigator recorded caregivers’ attendance at group training sessions, answered questions, and provided individual support during telephone conversations. An anonymous postprogram self-reported survey about caregivers’ perceived benefits, barriers, and experiences with the Tai Chi program were offered to caregivers at the end of the 16th week.
Outcome Measures
Effects of the program on participants’ mobility performance were assessed with two functional tests: Timed Up and Go and unipedal stance that are robust functional mobility tests feasible for OAD (Vellas et al., 1997; van Iersel, Munneke, Esselink, Benraad, & Olde Rikkert, 2008). Similar to Brill et al. (1995), a traffic cone was placed at end points (6 meters apart for gait speed and 3 meters for Timed Up and Go test), and a staff member walked alongside for safety and to encourage the OAD to cross over the end point. The participant was positioned next to a wall with handrails when unipedal stance was tested.
Intervention
The PEM-TC protocol was a 16-week Tai Chi intervention. It included a 4 week, 2 times a week on-site exercise class led by trainers, followed by a 12 week, 3 times a week home exercise regime. There were three to four dyads that were considered the optimal size for one trainer and one assistant. Trainers were experienced exercise instructors accustomed to working with older adults. All exercise groups began with 5 minutes of warm-up and ended with 5 minutes of cooldown-adapted Tai Chi movements, which emphasize breathing and relaxation. Each group class met for 60 minutes to allow questions, answers, and interaction between trainers and participant dyads. After 2 weeks of group training, all dyads were asked to start an additional session each week at home, in order to make a smooth transition to the home exercise stage. During home sessions, family caregivers led their respective patient to practice a 20-minute Tai Chi session (plus warm up and cooldown) 3 times per week for an additional 12 weeks. The 12-week Tai Chi practice period was chosen to follow other Tai Chi exercise programs with cognitively intact persons (Hartman et al., 2000; Taylor-Piliae et al., 2006) and balance training programs in participants with dementia (Teri et al., 1998).
We arranged an individualized home practice schedule on the basis of the Positive Emotional Motivators (PEMs) identified and the lifestyle of each participant. That is, if a particular type of song/music was among the pleasant events for the participant, favorite song/music was used as the exercise background, substituting the otherwise standardized relaxation musical accompaniment. If participant enjoys outings, readings, or reviewing family pictures together with others, caregivers were encouraged to use them as an incentive and reward for practicing Tai Chi. When appropriate, caregivers started with the PEM with the highest score, kept a watchful eye on its effectiveness, and modified it as needed with consultation from the investigators. If multiple PEMs were identified, different PEMs were allowed to be used interchangeably. Thus, variations in exercise schedule existed yet the dose of the home exercise, that is, 3 days per week (20 min minimum for each), remained fixed. A weekly phone call and a monthly refresher group class were provided to monitor the progress of home practice and to ensure the fidelity of participants’ exercise. All participants were encouraged to maintain their usual level of activity, but not initiate either a new exercise or physical therapy program while participating in the research project.
RESULTS
Program Feasibility
All participants (N = 10 group dyads) attended all 8 group sessions. As reported in the exercise log, eight dyads completed an average of 541 ± 325 total minutes (range 120–885) of the prescribed 720-minute home program. Shortfalls in Tai Chi home practicing time were attributed mostly to AD participant illness and to caregiver issues such as caregiver’s own health condition and depression. Exit interviews with participating caregivers suggested that they enjoyed the program structure and format, finding the 4-week group and 12-week home exercise length generally appropriate. Many caregivers reported that their roles had fulfilled more of a care provider function than a primary exercise activity for themselves. The feasibility of the PEM-TC program on participants with dementia was corroborated by anonymous postprogram caregiver report (see Table 1).
TABLE 1.
Caregivers’ Perceived Benefits, Obstacles, Recommendations, and Experiences of the PEM-TC Program
| Benefits to caregivers |
| “Helped my wife and myself both try to stay active.” |
| “It was useful to have the same experience to do (with my husband).” |
| “Helps me spend more time with my family member.” |
| “It is more difficult for me to do things slowly so it was useful and relaxing for me.” |
| “Working on my mom slowing my speed.” |
| “My knees hurt often. I can not walk much but they are ok when I do Tai Chi.” |
| “I keep the records and the schedule for the Tai Chi, which exercises my brain.” |
| Obstacles to Tai Chi practice |
| “Making sure that we keep doing it when one does not have a structured class.” |
| “It is more fun to do it in a group.” |
| “I think this is a wonderful program, but to keep it going I need to make a special effort to find time, to maintain continuity, and trying to get motivated.” |
| “The group environment makes me more motivated but I can do them while my sister joins in (the exercise).” |
| Possible improvements or additional comments |
| “I liked it and will continue.” |
| “I think the program and staff are excellent.” |
| “For me, I see no change necessary.” |
| “Maybe more weeks of exercise with group.” |
| Caregivers’ overall experience of the program |
| “I have done Tai Chi in the past and really like it, as I feel it helps to slow me down, is healthy for me, and it has been very beneficial for me to do it with my spouse. I think it would be helpful for people with dementia.” |
| “It is very helpful and she could do it.” “It got my wife interested in exercising.” |
| “I found hand contact helped a great deal.” “It helped his balance a lot.” |
| “Helped my mom remember movements and what to do.” |
| “Hand contact helped a sense of balance and coordination.” |
| “The program is excellent. It makes him get up off his chair where he watches too much TV. I trust that the program will help both his body and mind.” |
| “Exercise that was slow and is beneficial, the music was really nice and help-ful. A good time to unwind at the end of the day before dinner.” |
| “It helped to keep our balance some of the time. The closer contact was also very nice (hand contact).” |
PEMs Incorporation
Our data indicated that fundamentally enjoyable activities/events were shared by a majority of the patients. Being with family was the top enjoyable event for all subjects rated by caregivers. Table 2 reports the ranking of pleasant events by participants.
TABLE 2.
Top Ten Pleasant Events as Rated on The Pleasant Events Schedule–AD
| Event | Rank |
|---|---|
| Being with family | 1 |
| Watching TV | 2 |
| Meals with family | 3 |
| Being complimented | 4 |
| Listening to music | 5 |
| Laughing | 6 |
| Discussing past events | 7 |
| Reading stories | 8 |
| Being outside | 9 |
| Snacks | 10 |
It was reported from four dyads (three daughters and one spouse) that Sticky Hands alone worked and no special items on the PES-AD were needed, since the participants with AD were always agreeable whenever their exercise partners initiated the Tai Chi sessions. A wife of one participant considered having hand contact with her husband while practicing Tai Chi as spending quality time together. She wrote that although she and the husband live in the house together, “having quality time together always makes him happy.” The active involvement with caregivers is pleasure-inducing, particularly for AD patients who live alone. The visits of the exercise partners (in these cases daughters) in themselves may have represented a major source of enjoyment to AD participants. The full attention patients received while practicing Tai Chi together with their daughters might have brought them a lot more motivation and enjoyment.
Sticky Hands worked to strengthen mutual attention within the dyad and provided a base of support especially when practicing weight shifting and unipedal stance as Tai Chi demands. See example caregiver evaluations related to hand contact in Table 1. Congruent with our hypothesis, it was not only a means for participants to develop physical sensitivity to their partner’s motions, but also served as a social and emotional engagement opportunity to connect with the Tai Chi partner.
Preliminary Participant Outcomes
AD participants gained an average of 2 seconds (an improvement of 16% from baseline) on Timed Up and Go (TUG) performances after 4 weeks of intervention (see Table 3). Van Iersel and associates reported that a 9% change in individual’s TUG had a sensitivity of 93% for detection of clinically relevant change (van Iersel et al., 2008). However, improvement gained from the group training decreased somewhat after the home practice period.
TABLE 3.
Mean Mobility Performance Measured at Three Data Collection points (mean ± SD)
| Measure | Baseline (N = 10) | End of Group (N = 10) | End of Home (n = 8) |
|---|---|---|---|
| Timed up and goa | 11.8 ± 4.8 | 9.9 ± 3.2 | 11.0 ± 4.8 |
| t value | 2.24 | .68 | |
| p value | .052 | ns | |
| Unipedal stance timeb | 3.7 ± 4.5 | 6.6 ± 8.4 | 6.3 ± 3.0 |
| t value | −1.92 | −1.01 | |
| p value | .086 | ns |
Best time.
Preferred leg.
DISCUSSION
The PEM-PC protocol was developed based upon the knowledge that brain structures supporting the processing of emotions are relatively spared in dementias like AD as compared to structures supporting cognitive processes. Positive emotion-oriented communication may be used to transmit other types of interventions for these patients, such as motor learning using Tai Chi (Yao & Algase, 2006, 2008).
Participants’ Tai Chi completion rates signaled program feasibility for OAD. All attrition occurred following completion of all group training sessions. The low attrition rate of 20% in the pilot testing is promising since 50% is typically associated with most exercise programs with demented participants (Kramer et al., 2003). In our experience, paring with a family caregiver and the use of Sticky Hands seemed to be the most powerful exercise motivators that worked for participants. These motivators may have aided in building: (a) physical sensitivity to their partner’s motions and confidence to exercises; and (b) connectivity with partners. Research has demonstrated that a somatosensory stimulus at the fingertip can provide orientation information that enhances control of upright stance. Fingertip contact with a rigid stationary surface has a remarkable stabilizing effect, attenuating body sway despite whether the contact forces are adequate to provide mechanical support ( Jeka, Oie, & Kiemel, 2000).
We adapted the traditional Tai Chi teaching method—the Sticky Hands technique—to use hand touch and mirroring as a way of teaching movements and enhancing balance. This way of using the Sticky Hands technique has not been seen in studies on human subjects, but has been reported in an artificial intelligence engineering project that provided physical rehabilitation support to persons in need. The project presented a system for playing Sticky Hands with a robot (Hale & Pollick, 2000). Scientists on the project acknowledged the importance of making the robot an emotional being in implementing this technique. The strategy that they used was the configuration of eye contact between the robot and the rehabilitation subject (Hale & Pollick, 2000). The configuration simulates the role that emotion plays in meaningful behaviors in our living world. This engineering study reinforces our strategy of using Sticky Hands as an emotional means of enhancing motor learning and posture control in persons with AD.
Our pilot testing results indicated that motivating patients with AD to participate in exercise is feasible. Dementia patient’s ability to plan and perform activities that were once enjoyed may be gradually reduced, due to the inevitable decline in cognitive functioning (Logsdon & Teri, 1997). However, “Being with family/loved ones” is a top ranked PEM supported strategy of motivating patients to participate in an exercise program by utilizing family caregivers as partners. Significant others of persons with AD may have the optimum advantage in using the Sticky Hands technique because of the emotional connections already established between them. This suggests that family caregivers are uniquely positioned to assist in developing and implementing a home exercise program for their relatives with dementia.
Exercises, whether recreational or therapeutic, have shown to be mentally and physically beneficial to older adults. Tai Chi has been reported to have both physiological and psychosocial benefits, and is safe and effective in promoting balance control and reducing falls. Family caregivers of demented older adults are largely spouses or adult relatives who are facing the challenge of declining physical health themselves. In this sense, a Tai Chi exercise program delivered by lay family caregivers may not only decrease risks for falling in patients, but also improve the well-being and quality of life of caregivers. It has the potential to serve as a cost-effective model in improving exercise in AD patients as well their family caregivers.
In conclusion, this study represents an effort to develop strategies that enhance physical function for OAD. Using an adapted positive emotion–motivated Tai Chi facilitated by family caregivers, may be practically appropriate for OAD, who represent a rapidly increasing population worldwide. With further study, benefits of the program may also be found in enhancing cognition, physical functioning in persons with other forms of dementia, caregiver well-being, and the relationship between OAD and their caregivers.
Acknowledgments
This study was supported by the American Academy of Nursing/John A. Hartford Foundation BAGNC Program, the NIA Claude Pepper Older Adults Independence Center (AG024824), Michigan Center for Health Intervention Pilot Grant (P30 NR009000), University of Michigan Integrative Medicine Pilot Grant Awards (G006238), and was conducted in collaboration with the Mobility Research Center University of Michigan and Michigan Alzheimer’s Disease Research Center (MADRC). The authors also acknowledge support of the Department of Veterans Affairs Research and Development and the Dorothy and Herman Miller Fund for Mobility Research in Older Adults. The authors wish to thank Eric Pear, Wendy Champoux, Debbie Strasburg, and Ayowale Oladeji for their support in developing and conducting the assessments and interventions and Donna Algase for her mentoring throughout the project.
References
- Arkin SM. Elder rehab: A student-supervised exercise program for Alzheimer’s patients. The Gerontologist. 1999;39:729–735. doi: 10.1093/geront/39.6.729. [DOI] [PubMed] [Google Scholar]
- Brill PA, Drimmer AM, Morgan LA, Gordon NF. The feasibility of conducting strength and flexibility programs for elderly nursing home residents with dementia. The Gerontologist. 1995;35(2):263–266. doi: 10.1093/geront/35.2.263. [DOI] [PubMed] [Google Scholar]
- Buchner D, Larson EB. Falls and fractures in patients with Alzheimer-type dementia. Journal of the American Medical Association. 1987;257:1492–1495. [PubMed] [Google Scholar]
- Budson AE, Price BH. Memory dysfunction. The New England Journal of Medicine. 2005;352:692–699. doi: 10.1056/NEJMra041071. [DOI] [PubMed] [Google Scholar]
- Christou EA, Yang Y, Rosengren KS. Taiji training improves knee extensor strength and force control in older adults. Journals of Gerontology Series A: Biological Sciences & Medical Sciences. 2003;58A:763–766. doi: 10.1093/gerona/58.8.m763. [DOI] [PubMed] [Google Scholar]
- Eldridge LL, Masterman D, Knowlton BJ. Intact implicit habit learning in Alzheimer’s Disease. Behavioral Neuroscience. 2002;116(4):722–726. [PubMed] [Google Scholar]
- Gatts SK, Woollacott MH. Neural mechanisms underlying balance improvement with short term Tai Chi training. Aging-Clinical & Experimental Research. 2006;18(1):7–19. doi: 10.1007/BF03324635. [DOI] [PubMed] [Google Scholar]
- Hale JG, Pollick FE. Playing ‘sticky hands’ with a humanoid robot; First IEEE-RAS International Conference on Humanoid Robots (Humanoids 2000); September 7–8.Boston: Massachusetts Institute of Technology; 2000. [Google Scholar]
- Hamann SB, Monarch ES, Goldstein FC. Memory enhancement for emotional stimuli is impaired in Alzheimer’s disease. Neuropsychology. 2000;14(1):82–92. [PubMed] [Google Scholar]
- Hartman CA, Manos TM, Winter C, Hartman DM, Li B, Smith JC. Effects of T’ai Chi training on function and quality of life indicators in older adults with osteoarthritis. Journal of the American Geriatrics Society. 2000;48:1553–1559. doi: 10.1111/j.1532-5415.2000.tb03863.x. [DOI] [PubMed] [Google Scholar]
- Hauer K, Becker C, Lindemann U, Beyer N. Effectiveness of physical training on motor performance and fall prevention in cognitively impaired older persons: A systematic review. American Journal of Physical Medicine & Rehabilitation. 2006;85(10):847–857. doi: 10.1097/01.phm.0000228539.99682.32. [DOI] [PubMed] [Google Scholar]
- Heyn P, Abreu BC, Ottenbacher KJ. The effects of exercise training on elderly persons with cognitive impairment and dementia: A meta-analysis. Archives of Physical Medicine & Rehabilitation. 2004;85(10):1694–1704. doi: 10.1016/j.apmr.2004.03.019. [DOI] [PubMed] [Google Scholar]
- Holtzer R, Friedman R, Lipton RB, Katz M, Xue X, Verghese J. The relationship between specific cognitive functions and falls in aging. Neuropsychology. 2007;21:540–548. doi: 10.1037/0894-4105.21.5.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong Y, Li JX, Robinson PD. Balance control, flexibility, and cardio-respiratory fitness among older Tai Chi practitioners. British Journal of Sports Medicine. 2000;34:29–34. doi: 10.1136/bjsm.34.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussian RA. Stimulus control in the modification of problematic behavior in elderly institutionalized patients. International Journal of Behavioral Geriatrics. 1982;1(1):33–42. [Google Scholar]
- Jeka J, Oie KS, Kiemel T. Multisensory information for human postural control: Integrating touch and vision. Experimental Brain Research. 2000;134(1):107–125. doi: 10.1007/s002210000412. [DOI] [PubMed] [Google Scholar]
- Jensen J, Nyberg L, Gustafson Y, Lundin-Olsson L. Fall and injury prevention in residential care-effects in residents with higher and lower levels of cognition. Journal of the American Geriatrics Society. 2003;51:627–635. doi: 10.1034/j.1600-0579.2003.00206.x. [DOI] [PubMed] [Google Scholar]
- Kazui H, Mori E, Hashimoto M, Hirono N, Imamura T, Tanimukai S, et al. Impact of emotion on memory: Controlled study of the influence of emotionally charged material on declarative memory in Alzheimer’s disease. British Journal of Psychiatry. 2000;177:343–347. doi: 10.1192/bjp.177.4.343. [DOI] [PubMed] [Google Scholar]
- Kensinger EA, Brierley B, Medford N, Growdon JH, Corkin S. Effects of normal aging and Alzheimer’s disease on emotional memory. Emotion. 2002;2(2):118–134. doi: 10.1037/1528-3542.2.2.118. [DOI] [PubMed] [Google Scholar]
- Kramer AF, Colcombe SJ, McAuley E, Eriksen KI, Scalf P, Jerome GJ, et al. Enhancing brain and cognitive function of older adults through fitness training. Journal of Molecular Neuroscience. 2003;20:213–221. doi: 10.1385/JMN:20:3:213. [DOI] [PubMed] [Google Scholar]
- Lan C, Lai JS, Chen SY. Tai Chi Chuan: An ancient wisdom on exercise and health promotion. Sports Medicine. 2002;32(4):217–224. doi: 10.2165/00007256-200232040-00001. [DOI] [PubMed] [Google Scholar]
- Li F, Harmer P, Fisher KJ, McAuley E. Tai Chi: Improving functional balance and predicting subsequent falls in older persons. Medicine & Science in Sports & Exercise. 2004;36:2046–2052. doi: 10.1249/01.mss.0000147590.54632.e7. [DOI] [PubMed] [Google Scholar]
- Li F, Harmer P, Fisher KJ, McAuley E, Chaumeton N, Eckstrom E, et al. Tai Chi and fall reductions in older adults: A randomized controlled trial. Journals of Gerontology Series A: Biological Sciences & Medical Sciences. 2005;60(2):187–194. doi: 10.1093/gerona/60.2.187. [DOI] [PubMed] [Google Scholar]
- Li F, Harmer P, McAuley E, Duncan TE, Duncan SC, Chaumeton N, et al. An evaluation of the effects of Tai Chi exercise on physical function among older persons: A randomized controlled trial. Annals of Behavioral Medicine. 2001;23:139–146. doi: 10.1207/S15324796ABM2302_9. [DOI] [PubMed] [Google Scholar]
- Logsdon RG, Teri L. The Pleasant Events Schedule–AD: Psychometric properties and relationship to depression and cognition in Alzheimer’s disease patients. The Gerontologist. 1997;37:40–45. doi: 10.1093/geront/37.1.40. [DOI] [PubMed] [Google Scholar]
- Moayeri SE, Cahill L, Jin Y, Potkin SG. Relative sparing of emotionally influenced memory in Alzheimer’s disease. Neuroreport. 2000;11:653–655. doi: 10.1097/00001756-200003200-00001. [DOI] [PubMed] [Google Scholar]
- Mori E, Ikeda M, Hirono N, Kitagaki H, Imamura T, Shimomura T. Amygdalar volume and emotional memory in Alzheimer’s disease. American Journal of Psychiatry. 1999;156:216–222. doi: 10.1176/ajp.156.2.216. [DOI] [PubMed] [Google Scholar]
- Nowalk MP, Prendergast JM, Bayles CM, D’Amico FJ, Colvin GC. A randomized trial of exercise programs among older individuals living in two long-term care facilities: The Falls FREE program. Journal of the American Geriatrics Society. 2001;49(7):859–865. doi: 10.1046/j.1532-5415.2001.49174.x. [DOI] [PubMed] [Google Scholar]
- Patience T’ai Chi Association. Tai Chi push hands and Wing Chun sticky hands: A comparison. 2007. [Retrieved June 25, 2007]. from http://www.patiencetaichi.com/public/main.cfm.
- Province MA, Hadley EC, Hornbrook MC, Lipsitz LA, Miller JP, Mulrow CD, et al. The effects of exercise on falls in elderly patients: A preplanned meta-analysis of the FICSIT trials. Journal of the American Medical Association. 1995;273:1341–1347. [PubMed] [Google Scholar]
- Taylor-Piliae RE, Haskell WL, Stotts NA, Froelicher ES. Improvement in balance, strength, and flexibility after 12 weeks of Tai chi exercise in ethnic Chinese adults with cardiovascular disease risk factors. Alternative Therapies in Health & Medicine. 2006;12(2):50–58. [PubMed] [Google Scholar]
- Teri L, McCurry SM, Buchner DM, Logsdon RG, LaCroix AZ, Kukull WA, et al. Exercise and activity level in Alzheimer’s disease: A potential treatment focus. Journal of Rehabilitation Research & Development. 1998;35(4):411–419. [PubMed] [Google Scholar]
- Toulotte C, Fabre C, Dangremont B, Lensel G, Thevenon A. Effects of physical training on the physical capacity of frail, demented patients with a history of falling: A randomized controlled trial. Age and Ageing. 2003;32:67–73. doi: 10.1093/ageing/32.1.67. [DOI] [PubMed] [Google Scholar]
- Vellas BJ, Wayne SJ, Romero L, Baumgartner RN, Rubenstein LZ, Gerry PJ. One-leg balance is an important predictor of injurious falls in older persons. Journal of the American Geriatrics Society. 1997;45:735–738. doi: 10.1111/j.1532-5415.1997.tb01479.x. [DOI] [PubMed] [Google Scholar]
- van Doorn C, Gruber-Baldini AL, Zimmerman S, Hebel JR, Port CL, Baumgarten M, et al. Dementia as a risk factor for falls and fall injuries among nursing home residents. Journal of the American Geriatrics Society. 2003;51(9):1213–1218. doi: 10.1046/j.1532-5415.2003.51404.x. [DOI] [PubMed] [Google Scholar]
- van Iersel MB, Munneke M, Esselink RA, Benraad CE, Olde Rikkert MG. Gait velocity and the timed-up-and-go test were sensitive to changes in mobility in frail elderly patients. Journal of Clinical Epidemiology. 2008;61:186–191. doi: 10.1016/j.jclinepi.2007.04.016. [DOI] [PubMed] [Google Scholar]
- Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T. Reducing frailty and falls in older persons: An investigation of tai chi and computerized balance training. Journal of the American Geriatrics Society. 1996;44:489–497. doi: 10.1111/j.1532-5415.1996.tb01432.x. [DOI] [PubMed] [Google Scholar]
- Wong AM, Lin YC, Chou SW, Tang FT, Wong PY. Coordination exercise and postural stability in elderly people: Effect of Tai Chi Chuan. Archives of Physical Medicine & Rehabilitation. 2001;82:608–612. doi: 10.1053/apmr.2001.22615. [DOI] [PubMed] [Google Scholar]
- Wu G. Evaluation of the effectiveness of Tai chi for improving balance and preventing falls in the older population—A review. Journal of the American Geriatrics Society. 2002;50:746–754. doi: 10.1046/j.1532-5415.2002.50173.x. [DOI] [PubMed] [Google Scholar]
- Xu D, Hong Y, Li J, Chan K. Effects of Tai Chi exercise on proprioception of ankle knee joints in older people. British Journal of Sports Medicine. 2004;38:50–54. doi: 10.1136/bjsm.2002.003335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao L, Algase DL. Environmental ambiance as a new window on wandering. Western Journal of Nursing Research. 2006;28(1):89–104. doi: 10.1177/0193945905282355. [DOI] [PubMed] [Google Scholar]
- Yao L, Algase DL. Emotional intervention strategies for dementia-related behavior: A theory synthesis. Journal of Neuroscience Nursing. 2008;40(2):106–115. doi: 10.1097/01376517-200804000-00010. [DOI] [PubMed] [Google Scholar]
- Zeeuwe PE, Verhagen AP, Bierma-Zeinstra SM, van Rossum E, Faber MJ, Koes BW. The effect of Tai Chi Chuan in reducing falls among elderly people: Design of a randomized clinical trial in the Netherlands. BMC Geriatrics. 2006;6:6. doi: 10.1186/1471-2318-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]