Abstract
Background and objectives
Comprehensive evaluations are required to safeguard voluntarism and minimize harm to living kidney donors. This process is lengthy, invasive, and emotionally challenging, with up to one fifth of potential donors opting out. We aimed to describe donors’ experiences of the evaluation process.
Design, setting, participants, & measurements
We conducted 14 focus groups involving 123 kidney donors who completed donation from three transplant centers (Australia and Canada). Transcripts were analyzed thematically.
Results
We identified six themes reflecting donors’ experiences of evaluation. The themes that related to perseverance included emotional investment (prioritizing the recipient’s health, desperation for a normal life, protecting eligibility, shame of disappointing others, and overcoming opposition), undeterred by low risks (medical confidence and protection, worthwhile gamble, inherent invincibility, and normalizing risks), and mental preparation (avoiding regret, resolving decisional ambivalence, and managing expectations of recovery). The challenges included underlying fears for health (processing alarming information, unsettling uncertainty, and preoperative panic), system shortfalls (self-advocacy in driving the process, stressful urgency, inconsistent framing of safety, unnerving bodily scrutiny, questioning risk information, and draining finances); and lifestyle interference (living in limbo, onerous lifestyle disruption, and valuing flexibility).
Conclusions
Previous donors described an emotional investment in donating and determination to protect their eligibility, despite having concerns for their health, financial and lifestyle disruption, and opposition from their family or community. Our findings suggest the need to prepare donors for surgery and recovery, minimize anxiety and lifestyle burdens, ensure that donors feel comfortable expressing their fears and concerns, reduce unnecessary delays, and make explicit the responsibilities of donors in their assessment process.
Keywords: kidney donation, evaluation, assessment, focus groups, qualitative research, Panic, Shame, Uncertainty, Focus Groups, Investments, Emotions, Living Donors, Risk, Fear, Tissue and Organ Procurement, Anxiety, Life Style, Australia, Canada
Introduction
Living kidney donor transplantation offers the best outcomes for many patients with ESRD, but their donors must accept potential risks and uncertainty regarding long-term outcomes (1–3). Informed consent and comprehensive evaluations are necessary to safeguard donor voluntarism, exclude unsuitable donors, minimize harm and risk factors, and organize support for living donors (1,4,5). The evaluation can be lengthy, invasive, and anxiety provoking (6–9), and it is estimated that up to 22% of potential donors opt out of evaluation (10).
Donors undergo rigorous assessment of their mental and physical health, relationship with the recipient, motivations, expectations, lifestyle, finances, social support, and understanding of risks (11,12). Difficulty navigating an unfamiliar health care system can cause considerable stress (6–8). Many donors report anxiety and ambivalence about undergoing surgery (13–15). Some donors are very intent on donating and therefore, unable to fully comprehend the risks or conceal their concerns to protect their eligibility (16).
There are sparse data on the reasons why donors accept health risks, their experiences of being assessed, and how they persevere with evaluation. We aimed to describe kidney donors’ experiences of the evaluation process to inform strategies to prepare donors for the donation and possible outcomes.
Materials and Methods
This is study is part of a larger study examining donors’ priorities for outcomes. We reported our study according to the consolidated criteria for reporting qualitative studies framework (17).
Participant Selection
Participants were recruited from three transplant units in Australia (Westmead Hospital and Monash Medical Centre) and Canada (St. Paul’s Hospital). A researcher phoned donors to invite them to participate. Purposive sampling was used, whereby donors were selected to include diverse demographic and donation characteristics. All adult kidney donors from the past 20 years who were English speaking and able to provide informed consent were eligible to participate. Participants were reimbursed Australian/Canadian $50. Ethics approval was obtained from the Western Sydney Local Health District, Monash Health, and the University of British Columbia and Providence Health Care Research Ethics Board.
Data Collection
The question guide (Supplemental Table 1) was on the basis of a systematic review of donors’ experiences (18) and discussion among the research team. The 2-hour focus groups were conducted in a hotel meeting room. One facilitator (C.S.H., A.F.R., or A.T.) moderated the groups, and a cofacilitator recorded notes. Each group was audiorecorded and transcribed verbatim. Focus groups were ceased when saturation was achieved (no new information was elicited in subsequent groups) within each country (19).
Analyses
Grounded theory and thematic analysis were used to analyze the data (20). C.S.H. initially read through the transcripts to inductively identify preliminary concepts. The transcripts were coded using HyperRESEARCH (ResearchWare Inc., version 3.5.2) software, in which C.S.H. reviewed the transcripts line by line and assigned themes to each segment. The themes were iterated by comparing within and across groups and with feedback from A.F.R., K.E.M., and A.T., who ensured that all data were captured.
Results
We convened 14 focus groups with 123 donors from July of 2015 to July of 2016 (median =9 participants per group; interquartile range, 8–10; minimum =5; maximum =12). The demographic and donation characteristics are provided in Tables 1 and 2. The participants were ages 27–78 years old (mean =55 years old; SD=11.5) and included 78 (63%) women. The time since donation ranged from 2 months to 16 years (mean =3.6 years; SD=3.1). One hundred and one (82%) participants donated to a family member, nine (7%) donated to an unrelated recipient, six (5%) were nondirected (anonymous) donors, and 19 (15%) donated through a paired exchange.
Table 1.
Demographic characteristics of the participants (n=123)
| Characteristics | n (%) |
|---|---|
| Sex | |
| Women | 78 (63) |
| Men | 45 (37) |
| Country | |
| Australia | 67 (54) |
| Canada | 56 (46) |
| Age, yra,d | |
| 20–29 | 1 (1) |
| 30–39 | 11 (9) |
| 40–49 | 27 (22) |
| 50–59 | 36 (29) |
| 60–69 | 34 (28) |
| 70–79 | 13 (11) |
| Ethnicity^ | |
| White | 100 (81) |
| Asian/South Asian | 12 (10) |
| Middle Eastern | 5 (4) |
| Otherb | 6 (5) |
| Highest level of educationa | |
| University degree | 59 (48) |
| Diploma/certificate | 25 (20) |
| Secondary school: grade 12 | 24 (17) |
| Secondary school: grade 10 | 17 (14) |
| Total household income per year (USD)a,c | |
| $0–$24,079 | 16 (13) |
| $24,080–$50,169 | 29 (24) |
| $50,170–$80,271 | 30 (24) |
| >$80,271 | 42 (34) |
| Employment statusa | |
| Full time | 68 (55) |
| Part time/casual | 22 (18) |
| Retired/pensioner | 24 (20) |
| Not employed | 7 (6) |
| Marital statusa | |
| Married/de facto relationship | 96 (78) |
| Divorced | 7 (6) |
| Widowed | 6 (5) |
| Separated | 6 (5) |
| Single | 5 (4) |
| Partner (not living with) | 2 (2) |
USD, United States Dollars.
Total N≠123 due to nonresponse.
Includes South American, African, Pacific Islander, and First Nation (Canada).
As defined by the Australian Bureau of Statistics 2011 Census Survey (converted to USD).
Age at the time of participating in the focus group.
Table 2.
Donation characteristics (n=123)
| Characteristics | n (%) |
|---|---|
| Time since donation, yra | |
| <1 | 13 (11) |
| 1–3 | 59 (48) |
| 4–6 | 35 (29) |
| 7–10 | 9 (7) |
| >10 | 6 (5) |
| Relationship to recipient | |
| Spouse | 39 (32) |
| Parent | 33 (27) |
| Sibling | 23 (19) |
| Friend/colleague | 9 (7) |
| Child | 6 (5) |
| Other relative (aunt, grandparent, in-law, cousin) | 7 (6) |
| Nondirected | 6 (5) |
| Kidney exchange | |
| Yes | 19 (15) |
| No | 104 (85) |
| Postdonation complications | |
| Mental health | 8 (7) |
| Hypertension | 7 (6) |
| Chronic pain | 3 (2) |
| Hydrocele | 2 (2) |
| Otherb | 11 (9) |
| Recipient outcome | |
| Alive and functioning graft | 113 (92) |
| Graft failure or death | 10 (8) |
Total N≠123 due to nonresponse.
Includes hyperthyroidism, low BP, kidney stones, gall stones, hernia, blood clots, endometriosis, gout, high cholesterol, scleritis, and osteoporosis.
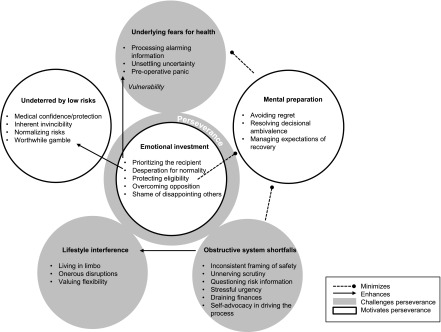
Six themes were identified. The relationships among themes are depicted in Figure 1. Quotations are provided in Table 3.
Figure 1.
Thematic schema. Living kidney donors were emotionally invested in the donation, which sustained their commitment throughout the evaluation process, despite underlying fears and uncertainty about their health, difficulty navigating the transplant process, and increasing interference with their work and lifestyle. Their desire to help the recipient and improve their own lifestyle also led them to view low risks as a worthwhile gamble. Emotional support and medical confidence reassured donors of their safety, helped them resolve ambivalence, and helped them prepare for their recovery and possible disappointment. Difficulties navigating the hospital system to access information and psychosocial services and speed up the process left some participants feeling unprepared, with unaddressed concerns. Their desperation to protect their eligibility prevented donors from seeking support and disclosing their apprehensions.
Table 3.
Selected illustrative quotations
| Theme | Illustrative Quotations |
|---|---|
| Emotional investment | |
| Shame of disappointing others | One thing I thought was wrong … We’re ready to go in virtually the next day, and I’m having a psychiatric test. That should have been the first thing I had, and I’ve now found out all these things that you didn’t know but someone’s waiting for me, and if I was starting to get frightened, I wouldn’t be game at that stage to say, “No.” Whereas at the start … you can go back home with your head held high and say, “It didn’t work out.” (Woman, related donor, Australia, 70s) |
| Desperation for a normal life | I’m glad you say selfish, because that’s what drove me, and I can only kind of admit it now. He got admitted into hospital six times 1 yr. We said our goodbyes so many times. It was just so draining … And then this came up. I put hand my up faster than anybody in this room. I was like, “Right, a solution, let’s go and fix it.” (Woman, related donor, Australia, 60s) |
| Basically, my doctor told me … because I have a really high case of diabetes in my family, so he was like, “I really would prefer not to use you, because more likely than not you are going to have diabetes when you are old,” but I mean, for us, there was no choice. (Woman, related donor, Canada, 30s). | |
| Prioritizing the recipient’s health | I went in there blind, mean … I didn’t ask questions … I didn’t care. I’d do anything for my family. (Woman, related donor, Australia, 50s) |
| But that was a big barrier, like the unknown for myself … because they say, when you donate, there’s a risk that something could happen to you, but in the end, I said to myself my brother needs it more than yourself. Because you do have that fear regardless. Once I put him first, everything just pretty much went away. (Man, related donor, Australia, 30s) | |
| So if I were to continue as a donor, I had to take treatment [for an infection] … But they didn’t tell me that [until] about 4 months on. But by that time, I was emotionally connected to being a donor, an anonymous donor. I had very personal reasons for doing it. So it was hard for me to just back out and kind of give up. (Woman, unrelated donor, Canada, 50s) | |
| Protecting eligibility | When I was going through the test, one of my great fears was that I wouldn’t be able to donate a kidney. I don’t know how that would have affected me, because I was so committed to wanting to do it. I was sort of nervous right up until they said “you are a match.” (Man, nondirected donor, Canada, 60s) |
| That's a scary one actually, seeing a psych. It would be awful if I got so far. (Woman, spousal donor, Australia, 50s) | |
| They took away my surgery date … I really wanted [this specific person] to get my kidney. So I basically had to beg to get my surgery date back … it was really hard to convince the doctors that I was going to be okay. (Woman, nondirected donor, Canada, 40s) | |
| Overcoming opposition | Well [my family], honestly, mine weren’t with me, but it didn’t make me think twice about it … I’d have put them to the side and thought about my own family. So it’ a hard choice; but in the end, you think it’s my choice and my choice only. That’s what I thought. (Woman, related donor, Australia, 50s) |
| Because of customs of race and religion, people frown upon you … but it didn’t deter me from doing it. I didn’t put race, religion, or anything into it … they say it’s God that brought you into the world so that you should go to him. But you’re helping, you’re going into the ground anyway, so why not? (Woman, related donor, Australia, 40s) | |
| My best friend reacted much like your family. Was probably the only big fight we’ve ever had in about 25 yr. At the end of it, I just said, you know what, you don’t get a vote. The only one who got a vote was my husband; nobody else got a vote. (Woman, unrelated donor, Canada, 50s) | |
| Undeterred by low risks | |
| Worthwhile gamble | They didn't give you any guarantees; they did throw statistics at you. But you could be an anomaly, and for whatever reason, it doesn't work. But all of us got to that place, where it doesn't matter. If it’s a year, it’s a year. But we have to do something, so we have to try. (Man, related donor, Canada, 40s) |
| They couldn’t guarantee, even though I ticked all the boxes, that I wouldn’t develop renal failure. But I could have developed it with two kidneys. (Woman, related donor, Australia, 60s) | |
| Inherent invincibility | I wasn’t really worried about any of the outcomes. I knew I was a healthy individual. I didn’t really have any concerns. (Woman, nondirected donor, Canada, 40s) |
| I mean I haven’t won the lottery yet, so I’m the rule, not the exception. (Woman, unrelated donor, Canada, 30s) | |
| Normalizing risks | The information was that taking my kidney away is not likely to cause any problem. People live very healthy and long and active lives with one kidney. (Man, related donor, Australia, 60s) |
| She was my inspiration. I went home, and I said to everybody, “I met this lady and son, and if that lady can do it, I can do it.” (Woman, related donor, Australia, 50s) | |
| Medical confidence and protection | They put you through such a stringent testing process … We don’t go into it thinking “Oh my god, am I going to make it?” (Woman, related donor, Canada, 50s) |
| The surgeon was very reassuring … I think it was more the confidence of how he spoke about the procedures he’d undertaken in his career. (Man, related donor, Australia, 20s) | |
| I did ask about life expectancy … He was very careful to tell me the data isn’t really there … So the answer he gave me is basically you have gone through all these tests. If something is going to show up, it would show up. I guess in my mind I was okay with that answer. (Man, nondirected donor, Canada, 60s) | |
| I was paying attention to postkidney op pregnancy studies … once you’ve passed the 2-yr mark, it makes zero difference. (Woman, unrelated donor, Canada, 30s) | |
| Underlying fears for health | |
| Processing alarming information | You can’t help but look behind the curtain and start poking around, like, will it hurt? … don’t start trolling the internet looking for these things, because you are going to find bad stories, and they are going to freak you out. (Man, unrelated donor, Canada, 40s) |
| Well I guess it does give you twinges of qualm as you are told the risks. And it does make you catch your breath maybe. (Woman, spousal donor, Australia, 50s) | |
| Your primary motive is that you want to help your person. But simultaneously, you’re weighing your own risks. (Woman, unrelated donor, Canada, 30s) | |
| They were going to take my mum’s … and my mum’s pretty old, and I said, “No. Take mine.” That made it easier for me. (Man, related donor, Australia, 30s) | |
| Preoperative panic | I don’t think it hit me until 5 min before when I was lying on the stretcher going into the operating room. (Man, related donor, Canada, 70s) |
| A week before the operation, for final checkup, I sat in the park. I suddenly realized, “I got a family; what happens if?” I don't think I got the support or counselling. (Man, related donor, Australia, 50s) | |
| Unsettling uncertainty | They didn’t follow up with donors for like the last decade really. So this is all pretty new. (Man, related donor, Canada, 50s) |
| He was very careful to tell me the data isn’t really there. (Man, nondirected donor, Canada, 60s) | |
| One of my biggest concerns afterwards was what would be the long-term repercussions, because back at the time we did our transplant (10+ yr ago), there was no ruling data on long-term impacts. (Man, 50s, Sydney) | |
| Mental preparation | |
| Resolving decisional ambivalence | I was a little bit anxious. I didn’t really want to donate at the beginning, because I’d met my partner later on, so we hadn’t been really together that long, and I kind of felt a bit of guilt if my daughter actually got sick … but then after a while, I thought well, she’s healthy. It’s really an unreasonable fear and yeah. (Woman, spousal donor, Australia, 40s) |
| Also going to get all the testing done by myself, I knew that was going to be one of the hard days for me, and I did it, and I broke down in tears; that was a real moment for me to say, “Hey, can I do it? Do I want to do it?” That was kind of one of my hard days. (Man, related donor, Australia, 40s) | |
| Avoiding regret | I very selfishly was worried about how it would affect my marriage. Am I going to feel like he owes me a debt? Is it going to make things weird between us? What if he doesn’t treat it properly? … They got me a social worker to talk through this issue … they said, you really need to think of it as a gift. And you know that, but I think articulating it out loud made a difference. (Woman, spousal donor, Canada, 40s) |
| Managing expectations of recovery | They say about risks, maybe they do they generalize it. But they don’t tell you specifically what can happen. So it doesn’t mean anything. (Man, related donor, Canada, 50s) |
| I would like those statistics, but later on, when you've already said I’ll do it, and then you have your tests and you're into it. (Man, related donor, Australia, 40s) | |
| There’s a Facebook page for kidney donors. I would ask the questions there, and it was more helpful than the actual hospital. Because it was life experience, so it was people that went through it, so they knew exactly what it was like. So, I found it very helpful. (Woman, spousal donor, Australia, 50s) | |
| System shortfalls | |
| Unnerving bodily scrutiny | He didn’t actually use the word “fat,” but “we won’t take, because you’re too overweight.” He was totally unprofessional … My weight has been a sore point. (Woman, Australia, 50s) |
| I wasn’t even a family member, and it wasn’t even someone I knew very well; they went through it [the risks] so many times … I almost started pulling out the world’s tiniest violin. (Woman, nondirected donors, 30s, Canada) | |
| Self-advocacy in driving the process | The amount of information we got was pretty much nil; we were prompting them every step of the way for dates, times, any scope of information we could get. We were pushing for it the whole time. It was never given freely. It was never given clearly. It was just a mess… (Man, unrelated donor, Australia, 30s) |
| I got to speak to my surgeon; he said, “This whole process is like buying a car. You have to do the research. You have to look deeper, because you can’t rely on people to spoon-feed you the information.” … As soon as he said that, every bit of grey just went to black and white … that made everything heaps better for me (Man, related donor, Australia, 20s) | |
| Stressful urgency | I do think they could’ve showed a little more zip to the process. I know it’s expensive to do all the screening, but when your loved one is not well, and you just see them going downhill, and being with them through their dialysis is the most frightening thing I’ve ever seen. (Man, related donor, Canada, 60s) |
| Inconsistent framing of safety | The psychiatrist. It’s like they were trying to convince you not to do it. It’s like, “You don’t have to do it if you don’t want to. You could possibly die. This could possibly happen.” And I’m like, “No. It’s all right. My brother’s sick. He needs it.” But they kept strumming in your ear, “Are you sure?” I don’t know if that’s part of the process. (Man, related donor, Australia, 30s) |
| I didn’t know if he was trying to scare me to make sure I was going to go ahead with the operation or going to chicken out. (Man, spousal donor, Australia, 60s) | |
| Questioning risk information | Maybe even a resource sheet of valid references … Because a lot of the time, I was told information, but I didn’t have a way of checking it or validating it… (Man, unrelated donor, Canada, 60s) |
| I think it’s a grey area. I mean, if you start listing complications, no one’s going to donate. I also think, you know, they don’t all tell you the truth. You know, [because] they all say well people have it, nothing happens, everything’s okay. But I think that’s also not true. (Man, spousal donor, Canada, 50s) | |
| Draining finances | It was a dent in the career a little bit … I think the financial assistance offered isn’t adequate. That’s just it wasn’t worth pursuing really. (Man, unrelated donor, Australia, 30s) |
| I did research on life insurance. And how it would impact getting life insurance because of course, I hadn’t had kidney yet. So that was in the back of my mind, and that’s one of the things that I was researching, looking for studies on (Woman, unrelated donor, Canada, 30s) | |
| Lifestyle interference | |
| Living in limbo | My whole life was on hold. I had work and training to do, and I couldn’t do any of that until this was behind us. So I thought it could have been a quicker (Man, unrelated donor, Canada, 50s) |
| So it was, it was very difficult to stick with it. Because I had other things I wanted to do that I couldn’t get started on because of this whole process and not knowing anything about what the date would be … So it was really difficult. I eventually had to tell them, “If you don’t tell me a date, like soon, despite all this time, I’m going to have to back out.” Because what I wanted to do, what else I want to do was important to me… (Woman, nondirected donor, Canada, 60s) | |
| Onerous lifestyle disruption | It was more about organizing everything around it … organizing work, organizing kids, organizing people. So it wouldn’t have stopped us, but it obviously took a lot of planning … They rang me and said, “Well, we can do it next week” and “No, I’m not ready for next week.” (Woman, related donor, Australia, 40s) |
| I work casually, and I got told one test, allow an hour. When I got there, “Sorry. Didn’t you get told, it’s A, B, C.” And that happened quite a lot … So, that was one of the annoying things I could have changed that shift and not missed financial benefit. (Woman, unrelated donor, Australia, 50s) | |
| If there was potential to group all the tests together in a consecutive day, it would be beneficial to a lot people, I think. (Man, related donor, Australia, 20s) | |
| Valuing flexibility | I was fortunate I could use my sick leave and be away from work. But I think for anyone else who didn’t have that, that might be tough. (Woman, related donor, Canada, 50s) |
Emotional Investment
Desperation for a Normal Life.
Donation was seen as a “privilege” that provided the chance to “fix” their recipients health and family life. Even if they had risk factors, they believed there was “no other choice.” Incompatible donors were relieved to find “a plan B” through paired exchange.
Shame of Disappointing Others.
Directed donors felt a responsibility to “pass” their assessments to avoid disappointing the recipient and the recipient’s family. At the final psychosocial evaluation, participants felt that it was too late to let the recipient down. Nondirected donors became “emotionally connected” to being a donor.
Prioritizing the Recipient’s Health.
Participants felt “blind[ed]” to information about risks—“I didn’t care if I lived or died, because it was my daughter.” Some were willing to “live with” short-lived and “manageable” consequences, like pain. Some were so “focused” on the recipient that postdonation outcomes were “an afterthought.”
Protecting Eligibility.
The possibility of being ineligible caused anxiety. Some maintained a strict diet and exercise regimen to ensure that they were accepted. Donors were careful to say “all the right words” to “pass” the evaluation. Nondirected and unrelated donors were frustrated by repetitive questioning of their comprehension of risks and having to “convince” the hospital to accept them. Some related donors were not worried about being questioned, because they felt that their motives were straightforward.
Overcoming Opposition.
“The hardest things” were family opposition or the recipient’s reluctance for them to donate. Unrelated donors believed their family preferred someone closer to the recipient to donate. Some faced disapproval from their religious community, regarding the violation of bodily integrity. This left them feeling isolated—“people could not relate to me, so I couldn’t talk to them.”
Undeterred by Low Risks
Worthwhile Gamble.
Participants, irrespective of time since donation, felt “comforted” by statistics showing “very minimal” risks of morbidity and mortality that were no higher than “somebody living with two kidneys.” The “very positive” data conveyed that their safety was a “nonissue.” Participants felt guilty for prioritizing their own safety.
Inherent Invincibility.
Unrelated and nondirected donors, in particular, felt confident in their safety. They believed that they were the “rule, not the exception” when considering low risks of harm—“[if] it’s 1/2000 or 1/500, that’s not going to be me.”
Normalizing Risks.
Participants viewed surgery as a common risk to take, equating it to “the chance you take every time you drive.” Nephrectomy was considered a “benign” procedure, because they were aware of others who had donated safely or were born with one kidney.
Medical Confidence and Protection.
The “stringent” medical evaluations convinced participants that they were unlikely to face complications. The surgeon was “the calming person before the storm” due to the positive and authoritative tone. Participants trusted their clinicians to protect them from harm—“the [doctors] don’t want to make another patient.” For Canadian donors, receiving waitlist priority helped to justify taking the risk.
Mental Preparation
Avoiding Regret.
Participants were uncertain how they would cope if the transplant failed, and many expected to feel “devastated.” They relinquished control over the “gift”—“It’s like any gift you give. You give, and you hope for the best.” Others avoided thinking about rejection. Some women feared recipient nonadherence would “change the dynamic of their relationship.”
Resolving Decisional Ambivalence.
Some participants were undecided about donating but continued with evaluation while “getting positive results.” They appreciated receiving reassurance from the psychosocial team, and support from family created a sense that they were not alone. They psychologic evaluation gave them some “closure.”
Managing Expectations of Recovery.
Donors sought practical advice to prepare for their recovery. Some preferred to hear previous donors’ experience of recovery “rather than the aggregate” outcome. Some watched videos of surgery and felt reassured by the “simplicity” of the process. Websites were used to find statistics about surgical outcomes, but some wanted local statistics relevant to their unit.
Underlying Fears for Health
Processing Alarming Information.
It was challenging for participants to process information about complications, because this conflicted with their determination to donate. They were confronted by graphic details of surgery and had fears “at the back of their minds” about mortality and ESRD.
Unsettling Uncertainty.
Even small possibilities of harm were troubling for some participants, because “you could be an anomaly.” Some participants described fears relating to their awareness of gaps in current knowledge of living donor outcomes.
Preoperative Panic.
Some participants were overcome with fear just before surgery and worried about the consequences for their family if they died. Men believed that they had avoided their fears.
System Shortfalls
Self-Advocacy in Driving the Process.
Some participants were surprised that they had to drive the evaluation. They had to “do [their] own research” to learn their eligibility status and arrange further tests—“we were prompting them every step of the way for dates, times, any scope of information.” Some felt that they discovered financial support too late or had to “ask for it.”
Stressful Urgency.
The “long and exhausting” evaluation, “devastating” delays, and “unnecessary” duplication of tests caused donors to fear their recipient would deteriorate on dialysis. Some believed that they had to pressure the transplant team to progress and felt that they should have been “fast track[ed]” through the system.
Inconsistent Framing of Safety.
Participants were confused by the “highly inconsistent” messages from different transplant professionals—“My surgeon [will] say, high-five we’re in … you see another surgeon, and they say you could die.” The reiteration of dangers and questioning of their commitment to donate by the surgeon and psychosocial team felt like they “were trying to convince you not to do it.”
Questioning Risk Information.
For some participants, information sessions were seen as unrealistically positive regarding postdonation outcomes—“everyone’s up there saying this is wonderful.” They were concerned when the transplant team could not provide more details about mortality statistics, such as the study population. They felt that they had no way of “checking” information. Some believed that risk estimates were “overinflated” so that “you can’t complain later.”
Unnerving Bodily Scrutiny.
Some participants felt uneasy about becoming a “patient” and exposing their body and lifestyle to examination. Abnormal test results and delays in receiving results caused them to fear the worst—“I had myself halfway into palliative care.” Some were shocked by their surgeon’s apparent lack of “bedside manner” and upset by being labeled overweight. They felt that they were treated like “just a number,” diminishing the “massive thing you are going through.”
Draining Finances.
Costs for transport, accommodation, and lost income accumulated throughout evaluation. Some found the financial assistance “wasn’t worth pursuing.” One participant reported being fired due to the leave required for recovery. Some Canadian donors had concerns about increased costs for health, life, and travel insurance postdonation.
Lifestyle Interference
Living in Limbo.
Participants felt their “whole life was on hold” while waiting for their surgery date and had to be “ultracareful with [their] body.” Some nondirected donors questioned their commitment to the donation with increasing delays. They wanted to be given realistic estimates of the workup timeframe.
Valuing Flexibility.
Donors valued the flexibility of the transplant team in organizing tests around their work schedule. Workplace flexibility, reimbursement of travel expenses, and income support alleviated financial anxieties, and some felt that this made it possible for them to donate.
Onerous Lifestyle Disruption.
The evaluation was disruptive to their work and lifestyle. Participants traveling long distances to the transplant center would have preferred to undergo tests closer to their home. Preparing for the surgery took a lot of organization, particularly for donors with young children. Many had family members to “back [them] up” financially or practically.
Discussion
The emotional investment in giving their organs sustained donors’ commitment throughout the evaluation process, despite having underlying fears about their health, encountering opposition from others, and managing lifestyle disruptions and financial hardship. They were determined to improve the recipient’s health and their family life. Although information about postdonation outcomes was concerning to donors, they trusted their clinicians to protect them from harm. They strived to protect their eligibility by adhering to a healthy lifestyle, and some concealed their concerns to show confidence in their decision. They also faced expenses and disruptions to their lifestyle to attend appointments and discovered their need to drive the evaluation forward and find information. Increasing delays and uncertainty left donors in a state of limbo and anxiety, because they feared that their intended recipient would deteriorate on dialysis or wanted to avoid the commencement of dialysis.
Some differences in the donors’ perspectives were apparent, particularly by donor type, age, sex, and ethnicity. For related donors, the chance to improve the recipient’s wellbeing outweighed concerns about their own risks, which they regarded as negligible and unjustifiable as a reason to not donate. Unrelated and younger donors gave more consideration to long-term health outcomes, feeling more vulnerable or distanced from the recipient. Nondirected donors had confidence in their safety, because they believed that they were in optimal health. Most donors feared failing their evaluations. Unrelated and nondirected donors described more intense questioning of their motivations, suitability, and understanding of risks, likely reflective of different approaches for evaluating these donors. Women described concerns about tensions in their relationship with the recipient. Ethnic minority donors faced opposition from their families and religious communities due to beliefs about bodily integrity, which has been described previously (21).
Donors were undeterred by low risks of complications and long-term health problems. Some donors recalled ignoring information that contradicted their decision to donate. This reflects an analysis of the dialogue between potential donors and transplant professionals, which found that donors express disinterest in risk information, because their decision is “entrenched” (22). This accords with cognitive dissonance theory, the tendency to minimize inconsistency between our thoughts and actions (23). Clinicians have also expressed skepticism that donors understand risks (24).
Psychosocial support enabled donors to resolve issues causing ambivalence or anxiety (for example, the possibility of the graft rejection). The need to protect their eligibility left some donors unwilling to disclose their concerns. Other studies have also found that directed and nondirected donors feel anxious about undergoing psychosocial assessment due to their determination to donate and attempt to manage how they are perceived, and some conceal experiences that might exclude them (16,22,25). We found that some donors who were men were overcome with anxiety before their operation, which supports findings from a study that used self-administered anxiety scales (26).
Our multinational study included a large sample of donors with a range of demographic and donation characteristics. However, we only included English-speaking participants. The applicability of the findings may be uncertain in health care systems outside of Australia and Canada, particularly those without universal access to health care and reimbursement programs. In the United States, many donors are uninsured (27), and eligibility for reimbursement is means tested (28). Differences are also likely to exist within programs in Australia and Canada. However, we achieved saturation within each country and found similar findings to other studies, suggesting the broader relevance of our findings (6–8). We also relied on the donor’s recall of their experience. However, donors discussed sensitive issues, such as ambivalence, which they had not expressed before donation. Variability in perspectives on risks may reflect changes to the messages provided by clinicians. We only included participants who had completed donation, and the barriers experienced by those who opt out might be different. Nondonors have reported some similar barriers (e.g., financial issues, concerns about risks, and family opposition) (10,29).
Guidelines focus on ensuring psychologic suitability, motivation, and voluntariness and informing donors of possible outcomes (5,30). Conflicts between the goals of clinicians and those of donors may not be addressed in guidelines. Comprehensive risk information can be confronting or irrelevant to donors. A “cooling-off” period and requiring donors to drive the evaluation ensure that donors make a considered decision (12,31). These practices can exacerbate stress for donors and prolong lifestyle intrusion. Caution to detect coercion and assess risk comprehension can cause donors to feel scrutinized and reluctant to express their anxieties. We suggest framing a component of the psychosocial evaluation as an opportunity to communicate and resolve concerns without feeling under threat of jeopardizing their eligibility.
We also suggest the need to provide donors with support to cope with anxiety, lifestyle disruption, and cultural barriers during evaluation. Some donors did not understand that they must drive the evaluation, because the transplant team is unwilling to push potential donors to complete the testing. Making explicit the expectations and responsibilities of potential donors and providing better information about the process and expected timeframe can prepare donors for the commitment of undergoing assessment. Transplant centers should also strive to improve efficiencies in the evaluation process (11). An independent live donor advocate, social worker, or patient navigator could facilitate comprehensive support by addressing donors’ needs and concerns as they emerge, assess risk comprehension, and provide culturally sensitive interventions to address family conflict.
Psychosocial interventions are needed to address donors’ fears of surgery, mitigate the anxiety of testing, facilitate social and family support, and prepare them for changes to their relationship and the possibility of graft failure or being ruled out as a donor. For emotional preparation, some donors found it useful to discuss their concerns about graft failure and relationship problems with psychologists or social workers and coped by relinquishing control over their “gift.” Information about surgery, complications, and recovery needs to be individualized to donors’ preferences (e.g., statistics or narratives of previous donor’s experiences).
Future studies should include donors from diverse cultural and linguistic backgrounds to better understand the challenges of evaluation in these groups, particularly given the low rates of kidney donation among ethnic minorities (32,33). The experiences of nondirected donors should be studied further. Although our study identifies some challenges that may influence the retention of donors, there is a need to understand the barriers for donors who opt out (10). Our findings may inform strategies for improving the process of evaluation, which would warrant further studies to evaluate effective practices (e.g., timing of the psychosocial assessment).
For potential donors, their emotional investment in the donation intensifies during evaluation and drives their perseverance and determination to protect their eligibility, despite having concerns for their health, facing financial and lifestyle disruption, and facing family and community opposition. Their determination to donate can also limit their comprehension of risk information and disclosure of their fears and concerns, thus leading to inadequate mental preparation for donation. Increased attention to the psychosocial challenges of evaluation is needed, which may include addressing donors’ concerns, preparing for surgery and recovery, mitigating lifestyle burdens and anxiety, clarifying donor’s responsibilities, and reducing delays in the evaluation.
Disclosures
None.
Supplementary Material
Acknowledgments
We thank all of the living kidney donors who generously gave their time to share their insights and perspectives.
C.S.H. is supported by National Health and Medical Research Council (NHMRC) postgraduate scholarship GNT1092741 and NHMRC program grant APP1092579. J.S.G. is supported by a foundation award from the Canadian Institute of Health Research. A.T. is supported by NHMRC fellowship APP1106716. The project is funded by Australian Research Council grant DE120101710.
The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, and approval of the manuscript.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.03550417/-/DCSupplemental.
References
- 1.Reese PP, Boudville N, Garg AX: Living kidney donation: Outcomes, ethics, and uncertainty. Lancet 385: 2003–2013, 2015 [DOI] [PubMed] [Google Scholar]
- 2.Terasaki PI, Cecka JM, Gjertson DW, Takemoto S: High survival rates of kidney transplants from spousal and living unrelated donors. N Engl J Med 333: 333–336, 1995 [DOI] [PubMed] [Google Scholar]
- 3.Lumsdaine JA, Wray A, Power MJ, Jamieson NV, Akyol M, Andrew Bradley J, Forsythe JL, Wigmore SJ: Higher quality of life in living donor kidney transplantation: Prospective cohort study. Transpl Int 18: 975–980, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Gill JS: Living kidney donation at a crossroads: What steps do we need to take now? Transplantation 100: 1180–1181, 2016 [DOI] [PubMed] [Google Scholar]
- 5.Kidney Disease: Improving Global Outcomes (KDIGO) Living Kidney Donor Work Group : KDIGO clinical practice guidelines on the evaluation and follow-up care of living kidney donors (November 2015 Public Review Draft). Available at: http://www.kdigo.org/clinical_practice_guidelines/LivingDonor/KDIGO%20Living%20Donor%20GL%20Public%20Review%20Draft%20November%202015.pdf. Accessed January 1, 2017
- 6.Shaw RM: Rethinking elements of informed consent for living kidney donation: Findings from a New Zealand study. Health Sociol Rev 24: 109–122, 2015 [Google Scholar]
- 7.Brown JB, Karley ML, Boudville N, Bullas R, Garg AX, Muirhead N: Living kidney donors’ experiences with the health care system. Soc Work Health Care 46: 53–68, 2008 [DOI] [PubMed] [Google Scholar]
- 8.Sanner MA: The donation process of living kidney donors. Nephrol Dial Transplant 20: 1707–1713, 2005 [DOI] [PubMed] [Google Scholar]
- 9.Arunachalam C, Garrues M, Biggins F, Woywodt A, Ahmed A: Assessment of living kidney donors and adherence to national live donor guidelines in the UK. Nephrol Dial Transplant 28: 1952–1960, 2013 [DOI] [PubMed] [Google Scholar]
- 10.Thiessen C, Kulkarni S, Reese PP, Gordon EJ: A call for research on individuals who opt out of living kidney donation: Challenges and opportunities. Transplantation 100: 2527–2532, 2016 [DOI] [PubMed] [Google Scholar]
- 11.Moore DR, Serur D, Rudow DL, Rodrigue JR, Hays R, Cooper M; American Society of Transplantation: Living donor kidney transplantation: Improving efficiencies in live kidney donor evaluation–recommendations from a consensus conference. Clin J Am Soc Nephrol. 10: 1678–1686, 2015 [DOI] [PMC free article] [PubMed]
- 12.Bailey P, Edwards A, Courtney AE: Living kidney donation. BMJ 354: i4746, 2016 [DOI] [PubMed] [Google Scholar]
- 13.Timmerman L, Ismail SY, Luchtenburg AE, Zuidema WC, IJzermans JN, Busschbach JJ, Weimar W, Massey EK: Exploring knowledge about dialysis, transplantation, and living donation among patients and their living kidney donors. Int J Behav Med 22: 580–589, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dew MA, DiMartini AF, DeVito Dabbs AJ, Zuckoff A, Tan HP, McNulty ML, Switzer GE, Fox KR, Greenhouse JB, Humar A: Preventive intervention for living donor psychosocial outcomes: Feasibility and efficacy in a randomized controlled trial. Am J Transplant 13: 2672–2684, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Valapour M, Kahn JP, Bailey RF, Matas AJ: Assessing elements of informed consent among living donors. Clin Transplant 25: 185–190, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hildebrand L, Melchert TP, Anderson RC: Impression management during evaluation and psychological reactions post-donation of living kidney donors. Clin Transplant 28: 855–861, 2014 [DOI] [PubMed] [Google Scholar]
- 17.Tong A, Sainsbury P, Craig J: Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care 19: 349–357, 2007 [DOI] [PubMed] [Google Scholar]
- 18.Tong A, Chapman JR, Wong G, Kanellis J, McCarthy G, Craig JC: The motivations and experiences of living kidney donors: A thematic synthesis. Am J Kidney Dis 60: 15–26, 2012 [DOI] [PubMed] [Google Scholar]
- 19.Kuper A, Lingard L, Levinson W: Critically appraising qualitative research. BMJ 337: a1035, 2008 [DOI] [PubMed] [Google Scholar]
- 20.Corbin J, Strauss A: Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory, 3rd Ed., Thousand Oaks, CA, Sage Publications, 2008 [Google Scholar]
- 21.Ismail SY, Massey EK, Luchtenburg AE, Claassens L, Zuidema WC, Busschbach JJV, Weimar W: Religious attitudes towards living kidney donation among Dutch renal patients. Med Health Care Philos 15: 221–227, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cunningham AC: The Living Donor Study: The Concepts and Frames of Living Kidney Donors, St. Lucia, QLD, Australia, The University of Queensland, 2015 [Google Scholar]
- 23.Festinger L: A Theory of Cognitive Dissonance, Stanford, CA, Stanford University Press, 1962 [Google Scholar]
- 24.Tong A, Chapman JR, Wong G, Craig JC: Living kidney donor assessment: Challenges, uncertainties and controversies among transplant nephrologists and surgeons. Am J Transplant 13: 2912–2923, 2013 [DOI] [PubMed] [Google Scholar]
- 25.Tong A, Craig JC, Wong G, Morton J, Armstrong S, Schollum J, Cross N: “It was just an unconditional gift.” Self reflections of non-directed living kidney donors. Clin Transplant 26: 589–599, 2012 [DOI] [PubMed] [Google Scholar]
- 26.Lopes A, Frade IC, Teixeira L, Oliveira C, Almeida M, Dias L, Henriques AC: Depression and anxiety in living kidney donation: Evaluation of donors and recipients. Transplant Proc 43: 131–136, 2011 [DOI] [PubMed] [Google Scholar]
- 27.Gibney EM: Lifetime insurance benefit for living donors: Is it necessary and could it be coercive? Am J Transplant 16: 7–8, 2016 [DOI] [PubMed] [Google Scholar]
- 28.Wiseman AC: Removing financial disincentives to organ donation: An acceptable next step? Clin J Am Soc Nephrol 7: 1917–1919, 2012 [DOI] [PubMed] [Google Scholar]
- 29.Thiessen C, Jaji Z, Joyce M, Zimbrean P, Reese P, Gordon EJ, Kulkarni S: Opting out: A single-centre pilot study assessing the reasons for and the psychosocial impact of withdrawing from living kidney donor evaluation. [published online ahead of print March 3, 2017] J Med Ethics : 10.1136/medethics-2016-103512 [DOI] [PubMed] [Google Scholar]
- 30.Tong A, Chapman JR, Wong G, de Bruijn J, Craig JC: Screening and follow-up of living kidney donors: A systematic review of clinical practice guidelines. Transplantation 92: 962–972, 2011 [DOI] [PubMed] [Google Scholar]
- 31.Hays RE: Informed consent of living kidney donors: Pitfalls and best practice. Curr Transplant Rep 2: 29–34, 2015 [Google Scholar]
- 32.Franklin PM, Crombie AK: Live related renal transplantation: Psychological, social, and cultural issues. Transplantation 76: 1247–1252, 2003 [DOI] [PubMed] [Google Scholar]
- 33.Purnell TS, Hall YN, Boulware LE: Understanding and overcoming barriers to living kidney donation among racial and ethnic minorities in the United States. Adv Chronic Kidney Dis 19: 244–251, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.