Abstract
No agreement exists on the most appropriate timing of orthodontic treatment in patients with cleft lip and palate. The aim of this study is to investigate the effect of early orthodontic treatment on development of the dental arches and alveolar bone.
A dental casts analysis was performed on 28 children with cleft lip and palate before orthodontic treatment (T0; mean age, 6.5 ± 1.7) and at the end of active treatment (T1; mean age, 9.2 ± 2.1 years). The considered variables were: intercanine and intermolar distances; dental arch relationships, evaluated according to the modified Huddart/Bodenham system.
The study group was divided into 2 samples according to the age at T0: Group A (age < 6 years) and Group B (age ≥ 6 years). A statistical comparison of the treatment effects between the 2 samples was performed.
Patients in Group A exhibited a greater increase of intercanine distance (8 mm versus 2.7 mm; P<0.001), intermolar distance (7.2 mm versus 5 mm; P = 0.06), and Huddart/Bodenham score (7.1 versus 3; P < 0.05) when compared with patients in Group B.
Early orthodontic treatment strongly improved the dental arch relationship, since subjects starting the therapy before the age of 6 had a better response in terms of anterior maxillary expansion.
Keywords: Cleft lip and palate, early orthodontic treatment, maxillary growth deficiency
Cleft of the lip and palate (CLP) is the most common human congenital malformation affecting the facial region. Cleft lip and palate occurs at the time of early embryogenesis from a failure in fusion of medial nasal and maxillary processes that results in orofacial clefting involving the upper lip, alveolus and/or primary palate.1 The development of CLP is associated with genetic and environmental factors.2
The most severe type of defect is the complete cleft of the lip, alveolar process, and palate, which can be either unilateral CLP (UCLP) or bilateral CLP (BCLP). The most widely adopted management strategy includes the surgical reconnection of the cleft anatomical structures followed by their development to gain proper appearance, occlusion, and speech.3
Maxillary growth in operated CLP patients is often decreased in the 3 dimensions. The most important cause of growth inhibition seems to be the iatrogenic effect of surgical intervention and the subsequent constriction induced by scar tissue.4 However, some authors attribute such a deficiency to the developmental hypoplasia of both the alveolar and palatal soft and hard tissues, as well as to functional factors.5 The maxillary growth deficiency affects the dental arches relationship on the vertical, sagittal, and transverse planes, frequently resulting in anterior and/or posterior crossbite occurring in the early dentition.6
Orthodontic treatment of CLP patients during the deciduous and mixed dentition period has been recommended to create more favorable conditions for midfacial growth, normalize the intermaxillary basal relationship, and prevent or eliminate functional disturbances.7 The most common orthodontic procedures include maxillary expansion to correct the reduced transverse dimension, incisor alignment and proclination to resolve crowding, rotations and anterior crossbites; and maxillary protraction to reduce maxillary retrusion.
Despite the agreement on the need of orthodontic treatment in the multidisciplinary management of CLP patients, controversy still exists on the best timing to start such a therapy.
The aim of this retrospective study is to investigate the effect of timing and method of early orthodontic treatment on development of the dental arches in growing subjects with various types of orofacial cleft. Particularly, we compared occlusal changes in children starting orthodontic therapy before 6 years of age with those in subjects starting treatment later.
The null hypothesis was that there was no significant difference between the 2 groups with regard to treatment effects on widening of the maxillary dentition and on the correction of interarch discrepancy.
METHODS
The principles outlined in the Declaration of Helsinki were followed throughout this study and all data were obtained in a clinical context as part as a standardized treatment regime with full acceptance from the parents.
Data of 76 patients (54 males, 22 females; mean age 7.2 years), with various types of orofacial cleft, consecutively referred to the Orthodontic Section of the Academic Hospital of Parma, Italy, between 2004 and 2015, were retrieved and analyzed. Variables evaluated included: gender, type of cleft, type of orthodontic treatment, and age at different times of follow-up. According to the type of cleft, patients were subclassified as follows: UCLP; BCLP; cleft palate (CP), and cleft soft palate (CSP).
All patients had dental casts taken before the orthodontic treatment (T0). For 28 patients (17 males, 11 females) dental casts taken at the end of the interceptive orthodontic treatment (T1) were also available. To evaluate the influence of age on treatment response, children of such a group were subclassified according to the age at the beginning of the orthodontic treatment: Group A (age < 6 years) and Group B (age ≥ 6 years). The characteristics of the samples are reported in Table 1.
TABLE 1.
Demographics of the Groups
| T0 | T1 | |||||||
| Gender | Age (Y, Mo) | Gender | Age (Y, Mo) | |||||
| Cleft Type | n | M | F | Mean ± SD | n | M | F | Mean ± SD |
| All clefts | 76 | 54 | 22 | 7.2 ± 3.6 | 28 | 17 | 11 | 9.2 ± 2.1 |
| UCLP | 53 (70%) | 38 | 16 | 7.3 ± 3.6 | 20 (72%) | 13 | 7 | 9.3 ± 2 |
| BCLP | 13 (17%) | 12 | 1 | 7.3 ± 3.7 | 4 (14%) | 3 | 1 | 9.1 ± 1.9 |
| CP | 5 (6.5%) | 1 | 4 | 7.2 ± 3.6 | 2 (7%) | 0 | 2 | 10.2 ± 1.8 |
| CSP | 5 (6.5%) | 3 | 2 | 7.3 ± 3.9 | 2 (7%) | 1 | 1 | 9.9 ± 1.6 |
BCLP, bilateral cleft lip and palate; CP, cleft palate; CSP, cleft soft palate, F, female; M, male; Mo, months; n, number of patients; UCLP, unilateral cleft lip and palate; Y, years.
Dental Study Models Analysis
All models were cast in white plaster and in centric occlusion and labeled with identification numbers attached to the base of the models.
Dental cast analysis, performed at T0 and T1, took into account the following variables: a) maxillary arch widths measured with a Beerendonk sliding calliper (measuring size 0–80 mm in tenths of mm). Particularly, intermolar width was measured as the distance between the mesiopalatal cusp tips of the first molars; intercanine width was measured as the distance between the cusp tips (Fig. 1); b) dental arch relationships, categorized according to the modified Huddart/Bodenham system (MHB).8,9 This numerical scoring system requires all maxillary teeth to be scored according to their buccolingual relationship to the corresponding mandibular tooth, except for the lateral incisors, which may be missing or in an abnormal position in CLP subjects (Fig. 2). The MHB system is used for the deciduous, mixed, and permanent dentition. The number of teeth scored changes, depending on age: before 6 years, the first permanent molars are not scored, even if erupted and therefore the maximum range of scores is between −24 and +8. After the age of 6, first permanent molars are scored if present; otherwise, the midpoint of the maxillary alveolar ridge is used. In this case, the maximum range of scores is −30 to +10.
FIGURE 1.
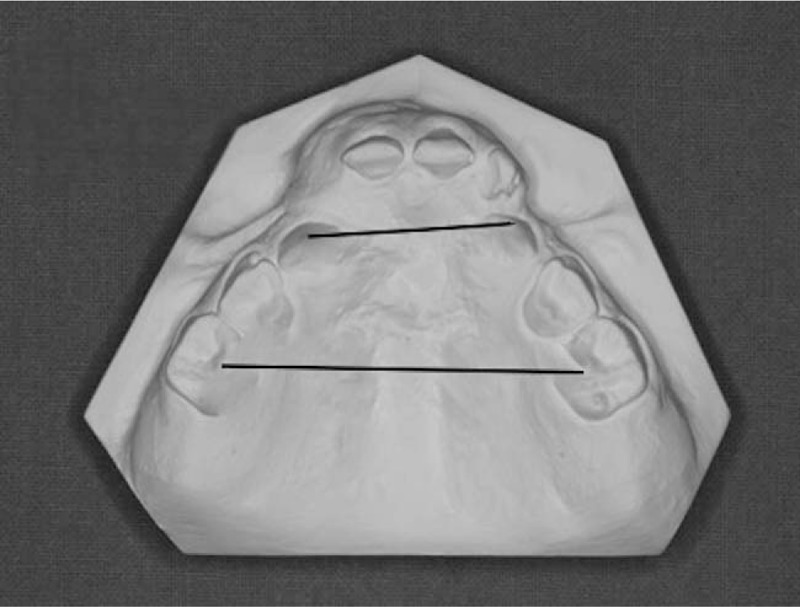
Transversal linear measurements on the study casts.
FIGURE 2.
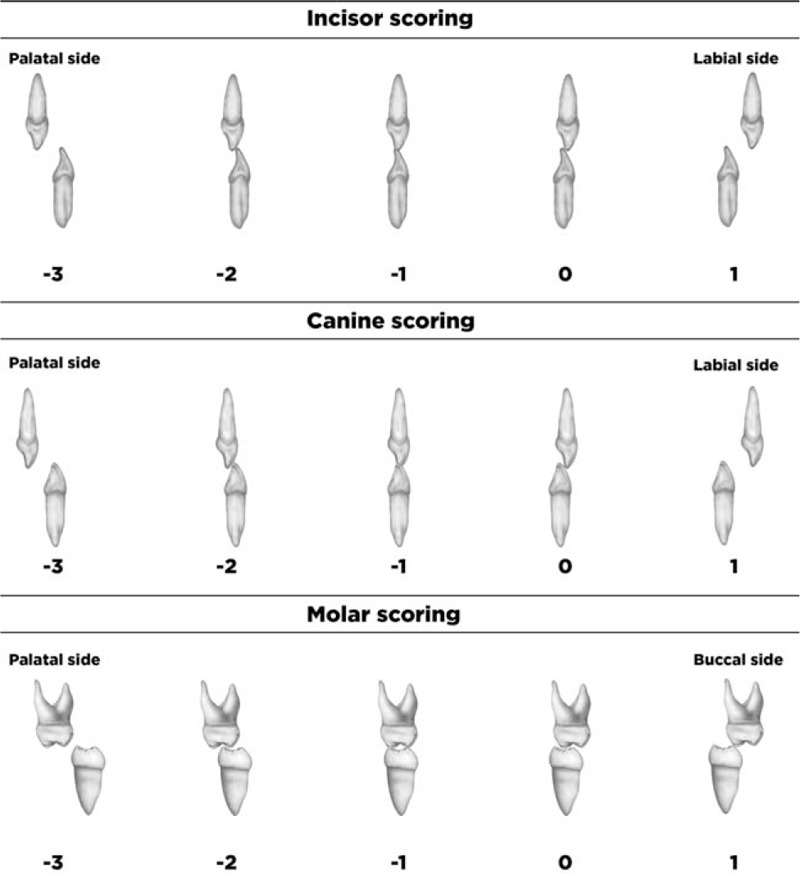
Diagram representing the modified Huddart and Bodenham scoring system. Redrawn from Tothill and Mossey (2007).15 The following modifications were taken into account: premolars were scored as for primary molars; if a central incisor was missing, the other central incisor was used to score the missing incisor; where canines were unerupted, the canine score was determined by the midpoint of the maxillary alveolar ridge; if a premolar was absent (for example, due to noneruption or hypodontia), then a score was allocated equivalent to the adjacent premolar, if erupted. Where no premolars were erupted, the score was determined by the midpoint of the maxillary ridge, in a similar way as previously described. The sum of the scores (the total score) reflected the interarch discrepancy.
Orthodontic Treatments
Orthodontic treatment includes maxillary expansion to correct the reduced transverse dimension, maxillary protraction to reduce maxillary retrusion, and incisor alignment and proclination to resolve crowding, rotations, and anterior crossbites.
Transverse expansion of the maxilla was obtained through the quad-helix appliance (0.038 inches/0.965 mm Blue Elgiloy), soldered to bands on the maxillary primary second molars or permanent first molars (Fig. 3). The appliance was initially activated to provide a force of 200 g per side; subsequent reactivations were done extraorally at 6-week intervals.
FIGURE 3.

Intraoral view of a quad helix appliance.
To achieve maxillary protraction, a posteroanterior orthopedic force carried out by a Delaire facial mask connected to an intraoral double arch appliance was applied. Two heavy (700 and 350 g on each side) elastics were attached from the soldered intraoral hooks in the cuspid area to the support bar of the facemask. The direction of the forward force was 15° downward in relation to the occlusal plane. Patients were instructed to wear the facemask for 12 hours per day, including at night.
Maxillary incisor rotation, lingual inclination, and anterior cross-bite were variously corrected by using partial fixed and removable orthodontic appliances.
Statistical Methods
The data was evaluated for normality using the Shapiro–Wilk test. Descriptive statistics were calculated for all variables at T0, and for variations from T0 to T1 either in the overall group of patients and in subgroups A and B. Differences between types of cleft at T0 were established through the analysis of variance and Tukey post-hoc tests.
Paired t tests were used to investigate the overall treatment effect by comparing the longitudinal changes in T0 and T1.
The following statistical comparisons were carried out with the independent t test: starting form: differences between the subgroup A and the subgroup B at T0; and treatment effects: T0-T1 changes in the subgroup A versus T0–T1 changes in the subgroup B.
Data were analyzed with the IBM-SPSS version 20 statistical software. Statistical significance was tested at P < 0.05. The power of the study was calculated on the basis of the difference between T0 and T1 in the treated group for a relevant variable (intercanine distance) as reported in a previous longitudinal investigation of similar nature and on the basis of the standard deviation of this difference.10 The power exceeded 0.80 at an α level of 0.05.
Method Error
To test the precision of the measurements, 25 dental casts were randomly selected and were remeasured by the same operator (FP) after a 1-month interval. No systematic error was detected.
Random errors were estimated with the Dahlberg formula. The errors for linear measurements ranged from 0.1 mm for intercanine distance, to 0.2 mm for intermolar distance. The intraobserver agreement for MHB score, analyzed by the weighted kappa statistic, was good (kappa = 0.62).
RESULTS
Maxillary Arch Width and Dental Arch Relationship at T0
There were no significant differences in the measurements of intercanine and intermolar distances of the patients in the different cleft groups (Table 2).
TABLE 2.
Mean Values of Measurements at T0 and Statistical Comparisons Between the Types of Cleft
| UCLP (n = 53) | BCLP (n = 13) | CP (n = 5) | CSP (n = 5) | UCLP Versus BCLP | UCLP Versus CP | UCLP Versus CSP | BCLP Versus CP | BCLP Versus CSP | CP Versus CSP | |
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |||||||
| Maxillary arch width | ||||||||||
| Intercanine distance (mm) | 25.7 ± 4.2 | 25.7 ± 4.5 | 25.6 ± 4.3 | 25.4 ± 4.4 | NS | NS | NS | NS | NS | NS |
| Intermolar distance (mm) | 35.5 ± 4.8 | 35.5 ± 4.8 | 35.4 ± 5 | 35.4 ± 5.1 | NS | NS | NS | NS | NS | NS |
| Dental arch relationship | ||||||||||
| HB total score | −7.5 ± 6.3 | −10.7 ± 5.3 | 2 ± 3.8 | −2 ± 3.4 | NS | ** | NS | ** | * | NS |
Statistical comparisons were performed with analysis of variance and Tukey post-hoc tests (P < 0.05).
BCLP, bilateral cleft lip and palate; CP, cleft palate; CSP, cleft soft palate; n, number of patients; UCLP, unilateral cleft lip and palate.
*P < 0.05;
**P < 0.01.
A statistically significant difference for MHB score was found between UCLP versus CP (P < 0.01); BCLP versus CP (P < 0.01), and BCLP versus CSP (P < 0.05).
Treatment Outcome
Table 3 reports the effects of treatment by comparing changes observed after the T0-T1 period. Significant differences were highlighted for all the variables: the mean intercanine widening was 4.7 mm (P < 0.001) and the mean intermolar widening was 5.3 mm (P < 0.05); a mean MHB score of 4.8 was gained (P < 0.05).
TABLE 3.
Comparisons of Changes After Treatment (T0-T1) Within the Study Group (n = 28)
| T0 | T1 | |||||
| Mean | SD | Mean | SD | Difference | P | |
| Maxillary arch width | ||||||
| Intercanine distance (mm) | 24.7 | 4.3 | 29.4 | 4.3 | 4.7 | 0.0003‡ |
| Intermolar distance (mm) | 34 | 4.9 | 39.3 | 4.6 | 5.3 | 0.01* |
| Dental arch relationship | ||||||
| HB total score | −6 | 0.2 | −1.4 | 5.1 | 4.6 | 0.002† |
Statistical comparisons were performed with paired t test (P < 0.05).
HB, Huddart/Bodenham.
*P < 0.05.
†P < 0.01.
‡P < 0.001.
Comparison of Treatment Outcome Between Group A (Age < 6 Years at T0) and Group B (Age ≥ 6 Years at T0)
Analysis of the starting forms showed that Group A (age <6 years) and Group B (age ≥ 6 years) had no statistically significant differences in maxillary arch width and dental arch relationship at T0 (Table 4).
TABLE 4.
Comparison of Starting Forms (T0) Between Groups of Different Ages
| < 6 Y (n = 12) | ≥6 Y (n = 16) | |||||
| Mean | SD | Mean | SD | Difference | P | |
| Maxillary arch width | ||||||
| Intercanine distance (mm) | 23 | 3.4 | 25.8 | 4.4 | −2.8 | 0.41 |
| Intermolar distance (mm) | 31.1 | 3.2 | 35.6 | 5 | −4.5 | 0.31 |
| Dental arch relationship | ||||||
| HB total score | −7.2 | 7.0 | −5 | 5.5 | −2.2 | 0.17 |
Statistical comparisons were performed with independent t test (P < 0.05).
HB, Huddart/Bodenham.
Statistical comparison of T0–T1 changes (Table 5) showed a significant difference between Group A and Group B for the anterior maxillary expansion and interarch relationship: Group A exhibited a greater increase of inter-canine distance (mean value: 8 versus 2.7 mm; P < 0.001) and MHB score (mean value: 7.1 versus 3; P < 0.05) than group B. Regarding intermolar distance, patients in Group A gained a mean widening of 7.2 mm compared with 5 mm in Group B (P = 0.06, close to significance).
TABLE 5.
Comparison of Changes After Treatment (T0–T1) Between Groups of Different Ages
| < 6 Y (n = 12) | ≥6 Y (n = 16) | |||||
| Mean | SD | Mean | SD | Difference | P | |
| Maxillary arch width | ||||||
| Intercanine distance (mm) | 8 | 4.4 | 2.7 | 3.3 | 5.3 | 0.0005† |
| Intermolar distance (mm) | 7.2 | 4.9 | 5 | 3.9 | 2.2 | 0.06 |
| Dental arch relationship | ||||||
| HB total score | 7.1 | 6.0 | 3 | 6.8 | 4.1 | 0.04* |
Statistical comparisons were performed with independent t test (P < 0.05).
HB, Huddart/Bodenham.
*P < 0.05.
†P < 0.001.
DISCUSSION
The role of the orthodontist is central in the interdisciplinary management of orofacial clefts. Therapeutic intervention usually starts during the neonatal period with treatment of displaced alveolar segments, and follows throughout the deciduous and mixed dentition phases with the management of the skeletal and dental components of the developing dentition. Most of the patients will receive orthodontic therapy during adolescence, and sometimes into adulthood.11
The continuous and often progressive nature of cleft-related orthodontic problems over the stages of growth and dental eruption makes it difficult to use routine orthodontic approaches. Treatment recommendations can be found for nearly every age; however, no clear-cut guidelines for optimal timing or method of intervention have been developed.
Many indices have been proposed to measure clinical outcomes related to different aspects of anatomical form and function in parts affected by the clefting process, usually reflecting specific interests of different disciplines.12 The primary purpose of this study was to compare the effectiveness of orthodontic treatment for maxillary hypoplasia on cleft patients starting the therapy at different ages. The sample of children was subclassified according to the age the interceptive orthodontic treatment was initiated.
The MHB system was selected from systems for assessing the severity of malocclusions since: it can be applied to any cleft type at any age, making its use easy in many different study samples;9 while the rest of indices utilize ordinal or categorical scales, the MHB follows a continuous 32-point scale before the age of 6, and a 40-point scale after that age. The large scoring range improves the level of sensitivity in the differentiation of the severity between the categories, and it tends to make the data more likely to be normally distributed, allowing the powerful, parametric statistical analysis.13
In addition, MHB is the sole index that does not require calibration; it is simple and objective, showing similar rates of reliability among trained and nontrained operators.14,15 Moreover, a recent systematic review evaluating indices to assess malocclusion in CLP patients based on the WHO criteria, recommended the MHB system as the index of choice.16
The disadvantage of the MHB system is that it does not consider the skeletal component of the malocclusion, not differentiating dental cross-bites from skeletal discrepancies leading to cross-bites. Also, it cannot differentiate between a generalized mild and a localized severe malocclusion, and it cannot assess the vertical discrepancies.
In this, the study group includes various subtypes of orofacial clefts that may exhibit different anatomical characteristics and maxillary growth patterns. Nevertheless, no statistically significant differences were found between UCLP and BCLP in terms of maxillary constriction and interarch discrepancy.
Notably, initial casts measurements of intercanine and intermolar distance were similar among the various subtypes of cleft. A possible explanation of such a finding may be that the sample is quite homogeneous with regard to the technique and timing of the preceding surgical approach. The maxillary growth patterns of CLP patients are affected by the iatrogenic effect of surgical repair, which has been demonstrated to be strongly related to the experience of the surgeon and the organization of the multidisciplinary team-work.17 The lack of statistical significance between groups at T0 demonstrates that patients had no differences in the initial maxillary dental arch dimensions. Such findings confirm the sample homogeneity and ensure the effectiveness of statistical comparisons of treatment outcomes.
The mean MHB score for the BCLP group was −10.7, and for UCLP −7.5. This indicates constriction of the maxillary dental arch respective to the mandibular dental arch. Although such a difference is not statistically significant, the characteristics of the initial dentoskeletal disharmony seem to be more severe in the BCLP group.
The mean MHB scores for the CP and CSP groups were 2 and −2, respectively. This also indicates constriction of the maxillary dental arch respective to the mandibular, even if to a lesser extent than in BCLP and UCLP. Maxillary arch constriction was therefore present in both the CP and the BCLP groups, which is in agreement with previous studies.18,19 Arch constriction may be related to palatal closure, which often includes incisions along the dental arches. The scars produced may induce inward deflection of the dentoalveolar processes, resulting in anterior and transverse crossbites. Unexpectedly, the preorthodontic occlusal scheme is worse in CSP patients compared with CP patients. However, such a finding may be biased because of the very small number of patients in the CSP and CP groups.
As reported by Tindlund et al20 and Vasant et al,21 in the present study outcomes of orthodontic treatment have been considered regardless of the subtype of clefting. Results of the T0–T1 interval showed a significant effect of therapy in terms of improvement of maxillary arch width as well as of dental arch relationship. The maxillary canine and molar width were increased of 4.7 and 5.3 mm, respectively, resulting in a mean increase of 4.8 on the MHB index. Consequently, maxillary changes have contributed to the favorable intermaxillary outcomes.
The orthodontic treatment induced a significantly greater improvement in the intercanine region when compared with the intermolar region. A differential expansion in the anterior region is frequently necessary in patients with CLP that usually exhibit a greater constriction of the intercanine width compared with the intermolar because of the medial shift of the smaller segment.22,23 Such a result can be obtained with common appliances such as the quad helix. This flexible device delivers light forces, and induces anteriorly divergent expansion by increasing the distance between the cleft segments. The transversal changes of our sample are in accordance with those in other studies performed on CLP patients, reporting similar arch width increases after maxillary expansion with the quad-helix appliance.10,20,21,24
Although early orthodontic therapy was effective for the improvement of maxillary arch dimensions and dental arch relationship in both the deciduous and mixed dentition groups, children starting the therapy before the age of 6 showed a more favorable change in maxillary expansion, especially in the canine region. In fact, the mean intercanine widening was 8 mm in Group A and 2.7 mm in Group B; the mean intermolar widening was 7.2 and 5 mm in Groups A and B, respectively.
The optimal timing of orthodontic interventions on CLP patients is still matter of great controversy.
The aims and supposed advantages of an early phase of treatment include improvement of alveolar development in the cleft site by “unlocking” overlapped maxillary segments; improvement in masticatory function by eliminating crossbites; improvement in permanent tooth eruption and alignment; improvement in speech development and in nasal breathing by expanding the maxilla, and providing more space for the tongue.7 In fact, maxillary transverse and sagittal deficiency can be associated with functional problems as narrowing of the pharyngeal airway, increased nasal resistance, and alterations in tongue posture, resulting in upper airway constriction and mouth breathing.25
Children with CLP have structural and functional changes of the upper airway, which may play a role in the pathophysiology of respiratory disorders.26,27 Accordingly, several studies have reported an increased risk of sleeping disordered breathing and obstructive sleep apnea (OSA) in cleft population.28–30
The management of OSA may require various craniofacial procedures both in growing subjects and in adults 31,32; notably, early orthopaedic maxillary expansion has been reported to enhance respiratory function and reduce symptoms of OSA in children.33–35
The orthopaedic response seems to be more favorable in younger patients, and closely connected with sutural growth of the upper jaw. Thus, Delaire et al36 reported favorable skeletal maxillary effects in deciduous and mixed dentition, showing that after 12 years of age the response is mainly dentoalveolar.
Early interceptive orthodontic treatment reduces some of the typical CLP patient stigmata, and creates a more favorable basis for subsequent conventional orthodontic treatments. Moreover, an improvement of soft-tissue profile is of obvious psychosocial importance.37,38
On the other hand, the main argument against primary dentition treatment is that it does not pass the “burden versus benefit of treatment” test. There is currently no evidence that the additional treatment provided at an early stage either eliminates the need for mixed dentition intervention, or can provide results not achievable through a single phase of treatment in the mixed dentition. The effectiveness of age-related orthodontic approaches to CLP patients has not been evaluated through randomized control trials. Therefore, it is not possible at the moment to state that one management strategy is better than another.
The greater increase of the intercanine width observed in the present evaluation is in agreement with findings from other studies,24 and it may be associated with the severe constriction of the anterior region in patients with CLP, which is commonly more pronounced compared with noncleft individuals. It is the opinion of the authors that this outcome should be preferred, as early management of transverse deficiencies in CLP patients usually requires a greater amount of anterior maxillary expansion with segment rotation, secondary to the collapse of the buccal segment on the cleft side. Consequently, these findings demonstrate that a practical advantage of expanding maxillary segments in the primary dentition is the ease of skeletal movement and segment rotation. Importantly, interceptive treatment of functional crossbite is recommended because it eliminates the lateral functional mandibular shift, preventing the development of skeletal asymmetry and of muscle function disturbances.39 In addition, early correction of anterior crossbite can give the additional benefit of maximizing anterior development of the maxillary dentoalveolar process.
Management of maxillary width at earlier periods does not necessarily preclude the need for additional expansion later, raising again the question of the “benefit versus burden” of these additional phases of treatment. Future directions of research should be focused on monitoring long-term outcomes with longer longitudinal follow-up of patients.
Footnotes
The authors report no conflicts of interest.
REFERENCES
- 1.Johnston MC, Avery JK, Hartsfield JK., Jr Riolo ML, Cangialosi TJ, Hartsfield JK, Jr, et al. Prenatal craniofacial development. Essentials for Orthodontic Practice 3rd edMercer Island, WA: Essential Press; 2012. 61–90. [Google Scholar]
- 2.Hartsfield JK., Jr Dean JA. Clinical genetics for the dental practitioner. McDonald and Avery's Dentistry for the Child and Adolescent 10th edSt. Louis, MO: Mosby; 2015. 87–109. [Google Scholar]
- 3.Mossey PA, Little J, Munger RG, et al. Cleft lip and palate. Lancet 2009; 374:1773–1785. [DOI] [PubMed] [Google Scholar]
- 4.Shaw WC, Asher-McDade C, Brattstrom V, et al. A six-center international study of treatment outcome in patients with clefts of the lip and palate: part 1. principles and study design. Cleft Palate Craniofac J 1992; 29:393–397. [DOI] [PubMed] [Google Scholar]
- 5.Kozelj V. The basis for presurgical orthopedic treatment of infants with unilateral complete cleft lip and palate. Cleft Palate Craniofac J 2000; 37:26–32. [DOI] [PubMed] [Google Scholar]
- 6.Mars M, Asher-McDade C, Brattstrom V, et al. A six-center international study of treatment outcome in patients with clefts of the lip and palate: part 3. Dental arch relationships. Cleft Palate Craniofac J 1992; 29:405–408. [DOI] [PubMed] [Google Scholar]
- 7.Long REJ, Semb G, Shaw WC. Orthodontic treatment of the patient with complete clefts of lip, alveolus, and palate: lessons of the past 60 years. Cleft Palate Craniofac J 2000; 37:533-1–533-13. [Google Scholar]
- 8.Huddart AG, Bodenham RS. The evaluation of arch form and occlusion in unilateral cleft palate subjects. Cleft Palate J 1972; 9:194–209. [PubMed] [Google Scholar]
- 9.Mossey PA, Clark JD, Gray D. Preliminary investigation of a modified Huddart/Bodenham scoring system for assessment of maxillary arch constriction in unilateral cleft lip and palate subjects. Eur J Orthod 2003; 25:251–257. [DOI] [PubMed] [Google Scholar]
- 10.de Medeiros Alves AC, Garib DG, Janson G, et al. Analysis of the dentoalveolar effects of slow and rapid maxillary expansion in complete bilateral cleft lip and palate patients: a randomized clinical trial. Clin Oral Investig 2016; 20:1837–1847. [DOI] [PubMed] [Google Scholar]
- 11.Vig KW, Mercado AM. Overview of orthodontic care for children with cleft lip and palate, 1915-2015. Am J Orthod Dentofac Orthop 2015; 148:543–556. [DOI] [PubMed] [Google Scholar]
- 12.Jones T, Al-Ghatam R, Atack N, et al. A review of outcome measures used in cleft care. J Orthod 2014; 41:128–140. [DOI] [PubMed] [Google Scholar]
- 13.Dobbyn LM, Weir JT, MacFarlane TV, et al. Calibration of the modified Huddart and Bodenham scoring system against the GOSLON/5-year-olds’ index for unilateral cleft lip and palate. Eur J Orthod 2012; 34:762–767. [DOI] [PubMed] [Google Scholar]
- 14.Gray D, Mossey PA. Evaluation of a modified Huddart/Bodenham scoring system for assessment of maxillary arch constriction in unilateral cleft lip and palate subjects. Eur J Orthod 2005; 27:507–511. [DOI] [PubMed] [Google Scholar]
- 15.Tothill C, Mossey PA. Assessment of arch constriction in patients with bilateral cleft lip and palate and isolated cleft palate: a pilot study. Eur J Orthod 2007; 29:193–197. [DOI] [PubMed] [Google Scholar]
- 16.Altalibi M, Saltaji H, Edwards R, et al. Indices to assess malocclusions in patients with cleft lip and palate. Eur J Orthod 2013; 35:772–782. [DOI] [PubMed] [Google Scholar]
- 17.Shaw WC, Dahl E, Asher-McDade C, et al. A six-center international study of treatment outcome in patients with clefts of the lip and palate: part 5. General discussion and conclusions. Cleft Palate Craniofac J 1992; 29:413–418. [DOI] [PubMed] [Google Scholar]
- 18.Nyström M, Ranta R. Effect of timing and method of closure of isolated cleft palate on development of dental arches from 3 to 6 years of age. Eur J Orthod 1994; 16:377–383. [DOI] [PubMed] [Google Scholar]
- 19.Heidbuchel KL, Kuijpers-Jagtman AM, Kramer GJ, et al. Maxillary arch dimensions in bilateral cleft lip and palate from birth until four years of age in boys. Cleft Palate Craniofac J 1998; 35:233–239. [DOI] [PubMed] [Google Scholar]
- 20.Tindlund RS, Rygh P, Boe OE. Intercanine widening and sagittal effect of maxillary transverse expansion in patients with cleft lip and palate during the deciduous and mixed dentitions. Cleft Palate Craniofac J 1993; 30:195–207. [DOI] [PubMed] [Google Scholar]
- 21.Vasant M, Menon S, Kannan S. Maxillary expansion in cleft lip and palate using quad helix and rapid palatal expansion screw. Med J Armed Forces India 2009; 65:150–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heidbuchel KL, Kuijpers-Jagtman AM. Maxillary and mandibular dental-arch dimensions and occlusion in bilateral cleft lip and palate patients from 3 to 17 years of age. Cleft Palate Craniofac J 1997; 34:21–26. [DOI] [PubMed] [Google Scholar]
- 23.Ayub PV, Janson G, Gribel BF, et al. Analysis of the maxillary dental arch after rapid maxillary expansion in patients with unilateral complete cleft lip and palate. Am J Orthod Dentofac Orthop 2016; 149:705–715. [DOI] [PubMed] [Google Scholar]
- 24.Li W, Lin J. Dental arch width stability after quadhelix and edgewise treatment in complete unilateral cleft lip and palate. Angle Orthod 2007; 77:1067–1072. [DOI] [PubMed] [Google Scholar]
- 25.McNamara J, Lione R, Franchi L, et al. The role of rapid maxillary expansion in the promotion of oral and general health. Prog Orthod 2015; 16:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maclean JE, Hayward P, Fitzgerald DA, et al. Cleft lip and /or palate and breathing during sleep. Sleep Med Rev 2009; 13:345–354. [DOI] [PubMed] [Google Scholar]
- 27.Smith CB, Walker K, Badawi N, et al. Impact of sleep and breathing in infancy on outcomes at three years of age for children with cleft lip and/or palate. Sleep 2014; 37:919–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Muntz H, Wilson M, Park A, et al. Sleep disordered breathing and obstructive sleep apnea in the cleft population. Laryngoscope 2008; 118:348–353. [DOI] [PubMed] [Google Scholar]
- 29.Robison JG, Otteson TD. Increased prevalence of obstructive sleep apnea in patients with cleft palate. Arch Otolaryngol Head Neck Surg 2011; 137:269–274. [DOI] [PubMed] [Google Scholar]
- 30.MacLean JE, Fitzsimons D, Fitzgerald DA, et al. The spectrum of sleep-disordered breathing symptoms and respiratory events in infants with cleft lip and/or palate. Arch Dis Child 2012; 97:1058–1063. [DOI] [PubMed] [Google Scholar]
- 31.Alexander NS, Schroeder JW. Pediatric obstructive sleep apnea syndrome. Pediatr Clin North Am 2013; 60:827–840. [DOI] [PubMed] [Google Scholar]
- 32.Brevi B, Di Blasio A, Di Blasio C, et al. Which cephalometric analysis for maxillo-mandibular surgery in patients with obstructive sleep apnoea syndrome? Acta Otorhinolaryngol Ital 2015; 35:332–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Villa MP, Rizzoli A, Miano S, et al. Efficacy of rapid maxillary expansion in children with obstructive sleep apnea syndrome: 36 months of follow-up. Sleep Breath 2011; 15:179–184. [DOI] [PubMed] [Google Scholar]
- 34.Marino A, Ranieri R, Chiarotti F, et al. Rapid maxillary expansion in children with obstructive sleep apnoea syndrome (OSAS). Eur J Paediatr Dent 2012; 13/1:57–63. [PubMed] [Google Scholar]
- 35.Pirelli P, Saponara M, Guilleminault C. Rapid maxillary expansion (RME) for pediatric obstructive sleep apnea: a 12-year follow-up. Sleep Med 2015; 16:933–935. [DOI] [PubMed] [Google Scholar]
- 36.Delaire J, Verdon P, Lumineau JP, et al. Some results of extra-oral tractions with front-chin rest in the orthodontic treatment of class 3 maxillomandibular malformations and of bony sequelae of cleft lip and palate. Rev Stomatol Chir Maxillofac 1972; 73:633–642. [PubMed] [Google Scholar]
- 37.Tindlund RS, Rygh P. Soft-tissue profile changes during widening and protraction of the maxilla in patients with cleft lip and palate compared with normal growth and development. Cleft Palate Craniofac J 1993; 30:454–568. [DOI] [PubMed] [Google Scholar]
- 38.Di Blasio A, Mandelli G, Generali I, et al. Facial aesthetic and childhood. Eu J Paediatr Dent 2009; 10:131–134. [PubMed] [Google Scholar]
- 39.Piancino MG, Kyrkanides S. Understanding Masticatory Function in Unilateral Crossbites. Iowa: John Wiley & Sons; 2016. [Google Scholar]


