Abstract
Background:
Catheter ablation (ABL) for non-valvular AF (NVAF) is recommended for symptomatic patients refractory to medical therapy and its success is related to the duration of the arrhythmia prior to intervention.Our aim was to assess the early utilization and the factors that prompted ABL in patients hospitalized for new onset NVAF.
Methods:
Using de-identified administrative discharge records for hospitalizations and emergency department (ED) visits, we determined the patients who had a first-time (since 1991) health record diagnosis of AF between2005 - 2011. We linked ambulatory surgery encounters for ABL based on ICD 9 code occurring within two years of initial hospitalization. After excluding other cardiac arrhythmias, atrio-ventricular nodal ablation or pacemaker/defibrillator placement and cardiac valve disease, bivariate comparisons were made with those who did not undergo ABL.
Results:
During the study period,3,440 of 424,592 patients (0.81%) hospitalized for new onset NVAF underwent ABL. Parameters significantly (p<0.001) associated with ABL compared tonon-ABL patientsincluded: principal diagnosis of AF (55% vs 25%), age 35-64 yrs (46.1% vs. 22.4%), male (58.9% vs. 48.2%), private insurance (46.6% vs. 21.1%), Caucasian (81.0% vs.71.6%), lower frequency of ED visit < 6 months before index AF hospitalization (10.7% vs. 15.9%), lower severityofillness at time of AF diagnosis (16.5% vs. 35.6%) anda lower prevalence ofmajor comorbidities (p< 0.001).
Conclusions:
Ablation has low utilization for treatment of new onset NVAF within two years of diagnosis. Earlier utilization of ABL may reduce health care burden related to NVAF and requires further evaluation.
Keywords: Ablation, Atrial fibrillation, Frequency, Epidemiology
Introduction
The current age-adjusted incidence of atrial fibrillation (AF) is13.4 per 1000 person-years[1]and the prevalence ofAF is projected to be over 10 million in the United States by 2050.[2]These patients are at risk for several morbidities requiring recurrent hospitalization, thus contributing to a huge economic burden from direct and indirect costs. [3]-[5]Medical management of non-valvular (NV)AF for rhythm control has moderate success,with median time to recurrence ranging from 74 - 487 days, reflecting frequentrelapses within first two years. [6], [7]The natural history of AF typically progresses fromparoxysmal episodes (PAF) triggered by premature atrial complexes from pulmonary veins or non pulmonary vein locations such as superior vena cava and posterior wall of left atrium, to persistent AF (PeAF) due to rotors, and substrate remodeling.[8]-[13]These patients present frequently with symptoms, however somepatients areasymptomatic with persistent AF of unknown duration. The mean duration of PAF is approximately 1.7 yrs before progressing to PeAF as noted in data from tertiary care centers.[14]
Clinical trials have shown superiority of ABL over medical therapy when used as second line intervention, and equivalent as first line treatment.[15]-[19] The reported frequency of maintaining sinus rhythm after ABL at one year varies approximately from 60-80%,[16], [17], [19], [20]with PAF requiring less extensive ablation compared to PeAF, achievinggreater success in maintaining sinus rhythm,[21][22]and resulting in fewer procedure related adverse events. [23]The defined success of ABL (non-recurrence of AF > 30 sec) isdependent on the type of AF prior to intervention[24] and theoverall duration of AF.[14] Evidence reflects superior control of AF when ABL is performed early in the course of the disease and is thereforerecommended for those who are refractory or intolerant to therapy with at least one drug.[25]-[27]
Our aim was to determine the frequency and predictors of early catheter ablation (< 2 years) in Californiaby a case control study of new onset AF. We hypothesized that hospitalization or emergency department visits represent severely symptomatic AF and may reflect a population with increased likelihood of referral for ABL.
Materials and Methods
This case control study was approved by the State of California Committee for the Protection of Human Subjects, and by the UC Davis institutional review board. The database utilized constituted patient discharge information from hospitalizations (PDD), emergency department (ED) and ambulatory surgery (AS) encounters from California non-federal hospitals.After linking the PDD, ED and AS databases, we identifiedthe patientshospitalized with a diagnosis of AF (427.31)between Jan 1, 2005 to Dec 31, 2011, and then excluded all the cases with any prior discharge diagnosis of AF, back to 1990. Among these cases that had an incident hospitalization with a diagnosis of AF after Jan 1 2005, we identified all those who underwent an endovascular ablation (ICD-9-CM = 37.34) between Jan 1, 2005- Dec 31, 2011. We excluded all patientsthat also had a diagnosis of atrial flutter (427.32), supraventricular tachycardia (427.0), ventricular tachycardia (427.1), underwent an open surgical ablation (only procedure =37.34) and all cases that had pacemaker implant (37.80-37.87) coupled with a diagnosis of sino-atrial node dysfunction (427.81) or atrio-ventricular block (426.0-426.1). Rural and urban hospitals were defined basedon recommendations by Office of Statewide Health Planning and Development (OSHPD) with areas under 250 persons/ square mile considered as rural.Comorbidities were defined using the Elixhauser comorbidity index (Healthcare Cost and Utilization Project V3.7), which identifies 29 major comorbidities based on ICD-9-CM codeslisted as being present at the time the admission of first admission with AF.[28] Patients with valve disease were excluded and the remainder were considered to have NVAF. Patients with dementia, human immunodeficiency disease, alcohol abuse, active cancer or psychosis were also excluded. We reviewed approximately 200 hospitalization records to verify the accuracy of the inclusions and exclusions.
All patient refined (APR)-DRGs are measures to assess patient characteristics for resource utilization as an all payer alternative to Medicare system (MS)-DRG and has four levels of severity.We applied this previously described measure called “the severity-of-illness (SOI)” utilizing a software (APR-DRG version 24; 3M) at the time of the hospital admission (minor, moderate, severe and extreme).[29-31]Many of the co-morbidities defined by this algorithm are known risk factors associated with AF.
We compared demographic and clinical characteristics of cases that underwent ABL within two years to controls who never underwent ablation during the study period. Predictors undergoing ABL were analyzed using a proportional hazard model that included demographic variables, clinical variables, SOI, insurance status, and intercurrent hospitalization with a principal diagnosis of AF as a time dependent covariate. SAS version 9.3 was used for all statistical analyses. Continuous variables were expressed as mean + SD. Categorical variables were presented as percentages. Uni-variate analysis was performed with a χ2 test for nominal variables and Fisher’s exact test was applied for outcomes fewer than 5 events per cell. Analysis was performed using multivariable proportional hazard modeling to predict outcomes. A p-value < 0.05 was considered significant.
Results
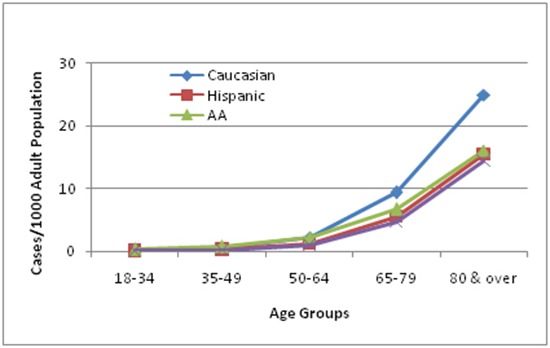
Among the total adult population in California (28,068,224), 424,492cases had a first-time hospitalization with a diagnosis of NVAF between 2005-2011, averaging 60,000 admissions per year. [Figure 1]Of these cases, 106,942 patients (25.2%) were admitted for a principal diagnosis of NVAF and 317,650patients (74.8%) had a secondary diagnosis of NVAF. The majority of these patients (75.9%) were >65 yrs old; the number of males (2.39/1000) and females (2.38/ 1000) were comparable.The payer source for the majority of the cases, was medicare (69%)and approximately one fifth had private insurance. [Table 1] There was a slight decrease in the number of cases with a first time admission for NVAF from 60,484 in 2005 to 56,829 in 2009; in 2011, there was an increase to 62,439.[Figure 1A] Most patients were hospitalized in an urban facility (94.3%). Two- thirds of the patients were admitted with moderate or major severity of illness, while a third were either EDadmissions or mild severity of illness.Approximately 60% the patients had hypertension (HTN); diabetes mellitus (DM), heart failure (HF),chronic obstructive pulmonary disease (COPD), obesity were relatively frequent. [Table 2]The prevalence of AFwas higher among Caucasians compared to other races/ethnic groups.[Figure 2]
Figure 1A. Number of hospitalizations or emergency department visits for non valvular atrial fibrillation (NVAF) between 2005-2011.
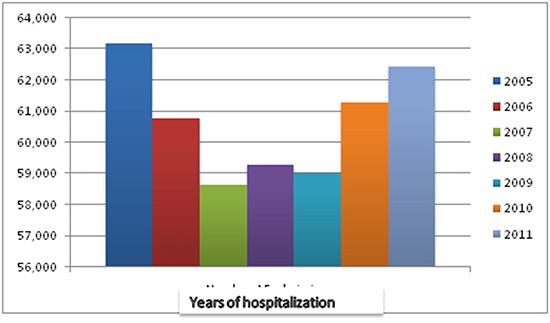
Table 1. Baseline characteristics of patients admitted for first time diagnosis of Non valvular atrial fibrillation (NVAF) 2005-2011 in non federal hospitals in California.
AF- Atrial fibrillation
| Characteristics | Total population | Percent | |
| All Patients with new AF in 2005 though 2011 | 424,592 | 100.0 | |
| New AF prin DX (427.31) | 106,942 | 25.2 | |
| New AF any secondary diagnosis (427.31) | 317,650 | 74.8 | |
| Patient Age | 18-34 | 6,335 | 1.5 |
| 35-49 | 21,640 | 5.1 | |
| 50-64 | 74,212 | 17.5 | |
| 65-79 | 155,568 | 36.6 | |
| 80 or older | 166,837 | 39.3 | |
| Patient sex | Male | 209,371 | 49.3 |
| Female | 215,221 | 50.7 | |
| Payer source (index admission) | Medicare | 293,791 | 69.2 |
| Medicaid | 20,782 | 4.9 | |
| Private, incl. HMO | 90,337 | 21.3 | |
| Self-pay | 10,561 | 2.5 | |
| No charge | 8,463 | 2.0 | |
| Other | 658 | 0.2 | |
| Race/ethnicity (index admission) | White | 304,451 | 71.7 |
| Hispanic | 51,114 | 12.0 | |
| Black | 21,000 | 4.9 | |
| Asian/Pacific Islander | 31,500 | 7.4 | |
| Other | 16,527 | 3.9 | |
| Inpatient admission within 6 months preceding new AF admission | 56,017 | 13.2 | |
| ED visit within 6 month of new AF admission | 67,502 | 15.9 | |
| Outpatient admission within 6 months preceding new AF admission | 32,834 | 7.7 | |
| Rural location (index admission hospital) | Urban | 400,317 | 94.3 |
| Rural | 24,275 | 5.7 | |
| Admission year | 2005 | 63,164 | 14.9 |
| 2006 | 60,787 | 14.3 | |
| Admission year | 2007 | 58,625 | 13.8 |
| 2008 | 59,275 | 14.0 | |
| 2009 | 59,010 | 13.9 | |
| 2010 | 61,292 | 14.4 | |
| 2011 | 62,439 | 14.7 | |
Table 2. Comorbidities associated with new diagnosis of Non valvular Atrial Fibrillation.
ED- Emergency department
| Co morbidities | n | % | |
| Discharge severity | ED Case | 98,478 | 23.2 |
| Minor | 43,355 | 10.2 | |
| Moderate | 132,453 | 31.2 | |
| Major | 115,209 | 27.1 | |
| Extreme | 35,097 | 8.3 | |
| Congestive heart failure | 105,645 | 24.9 | |
| Valvular disease | 40,071 | 9.4 | |
| Pulmonary circulation disease | 20,283 | 4.8 | |
| Peripheral vascular disease | 38,312 | 9.0 | |
| Paralysis/Other neurological disorders | 45,540 | 10.7 | |
| Chronic pulmonary disease | 92,533 | 21.8 | |
| Diabetes | 109,886 | 25.9 | |
| Hypertension | 254,573 | 60.0 | |
| Renal failure | 56,342 | 13.3 | |
| Liver disease | 8,629 | 2.0 | |
| Rheumatoid arthritis/collagen vas | 11,981 | 2.8 | |
| Coagulopthy | 17,387 | 4.1 | |
| Obesity | 50,225 | 11.8 | |
| Deficiency Anemias | 88,903 | 20.9 | |
| Depression | 33,786 | 8.0 | |
| Coronary artery disease | 54,968 | 12.9 | |
Figure 2A. Gender variation is ablation for non valvular atrial fibrillation (NVAF) among all patients admitted with new onset NVAF.
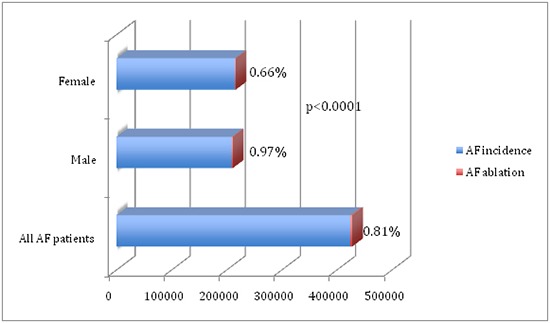
ABL was performed < 2 years from the first hospitalization/ ED visit in 3440 (0.81%) of the total number of cases admitted during the study period.[Table 3] The number of ablations peaked at 564 (0.95%) in this population in 2008, followed by a decline [Figure 1B] (p<0.0001). ABL wasmorelikely to be performed in cases admitted specifically for NVAF (1.8%) as opposed those that had to a secondary diagnosis of NVAF(0.49%) (p<0001). Males were more likely to undergo ABL (1%) compared to females (0.7%, p<0.001) and Caucasians (0.92%) morethan other ethnicities (p<0.001).There were no differences in rural vs urban ABL.Patients with private insurance (1.8%) were more likely to have ABL than those with Medicare (0.5%, p<0.001) or other insurance, although a majority of the patients were > 65 yrs and had Medicare coverage.[Table 3]
Table 3. Results: Predictors of early ablation for non –valvular atrial fibrillation (NVAF).
| Ablation (n=3440) (%) | No ablation (n=421152) (%) | P value | |
|---|---|---|---|
| Principal Diagnosis of NVAF | 24.9 | 1.8 | <0.0001 |
| Secondary Diagnosis of NVAF | 75.1 | 0.5 | <0.0001 |
| Patient age (yrs) | |||
| 18-34 | 1.45 | 1.5 | <0.0001 |
| 35-49 | 1.86 | 5.0 | |
| 50-64 | 1.69 | 17.3 | |
| 65-79 | 0.80 | 36.6 | |
| 80 or older | 0.27 | 39.5 | |
| Male | 49.2 | 0.97 | <0.0001 |
| Female | 50.8 | 0.66 | |
| Payer source | |||
| Medicare | 45.3 | 69.4 | |
| Medicaid | 3.4 | 4.9 | <0.0001 |
| Private | 46.6 | 21.1 | |
| Race | |||
| White | 71.6 | 0.92 | |
| Hispanic | 12.1 | 0.54 | <0.0001 |
| Black | 5.0 | 0.38 | |
| Asian/Pacific Islander | 7.4 | 0.51 | |
| Other | 3.9 | 0.83 | |
| Discharge Severity | |||
| ED case | 23.1 | 1.1 | |
| Minor | 10.1 | 1.76 | <0.0001 |
| Moderate | 31.2 | 0.77 | |
| Major | 27.2 | 0.42 | |
| Extreme | 8.3 | 0.25 | |
| Co Morbidities: | |||
| Heart failure | 15.4 | 25.0 | <0.0001 |
| Coronary artery disease | 8.8 | 13.0 | <0.0001 |
| Peripheral vascular disease | 3.4 | 9.1 | <0.0001 |
| Prior stroke/neuro disorders | 3.7 | 10.8 | <0.0001 |
| Pulmonary disease | 14.8 | 21.9 | <0.0001 |
| Obesity | 11.3 | 11.8 | ns |
| Diabetes | 15.8 | 26.0 | <0.001 |
| Hypertension | 49.6 | 60.0 | <0.001 |
| Renal Failure | 4.8 | 13.3 | <0.001 |
Figure 1B. Percentage of ablations for NVAF every year.
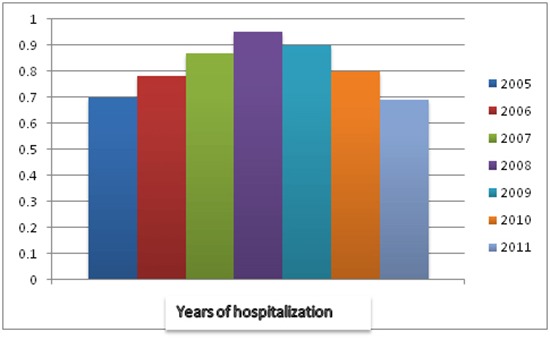
Figure 2B. Racial distribution of hospitalization or emergency department visits for NVAF in non federal hospitals in California (2010).
Risk-adjusted predictors included: admission for principal diagnosis of NVAF (HR=2.1), younger age (HR= 3.9); age (50-64 vs >80); male (HR=1.2), private insurance (HR=1.8vs. Medicaid); Caucasian (HR= 2.1 vs. Hispanic), mild severity of illness (HR=1.4). There was less coronary artery disease, peripheral vascular disease, stroke/ neurological disorders, DM, HTN, HF, renal failure, and COPD, but no difference in obesity between ABL and non ABL groups. [Table 4]
Table 4. Predictors of ablation of patients hospitalized for atrial fibrillation.
| Ablation (n=3440) | No ablation (n=421152) | P value | |
| Heart failure (%) | 15.4 | 25 | <0.001 |
| Coronary artery disease | 8.8 | 13 | <0.001 |
| Peripheral vascular disease | 3.4 | 9.1 | <0.001 |
| Prior stroke/neuro disorders | 3.7 | 10.8 | <0.001 |
| Pulmonary disease | 14.8 | 21.9 | <0.001 |
| Obesity | 11.3 | 11.8 | Ns |
| Diabetes | 15.8 | 26 | <0.001 |
| Hypertension | 49.6 | 60 | <0.001 |
| Renal failure | 4.8 | 13.3 | <0.001 |
Discussion
The prevalence of AF is high,[2], [32]primarily attributable to its association with aging, HTN, DM,HF, sleep apnea, pulmonary diseases and obesity.[33]-[37]Worldwideadmissions for AF have increased from 35 to 110/10,000 population between 1996-2006, likely due to the augmented prevalence of these risk factors.[2]However, because of the presence of asymptomatic episodes of AF, the exact prevalence is unknown.[38]-[40]In this study, we attempted to determine if these epidemiologic data correlate with an increase in hospitalizations/ ED visitsfor AF in California. We found that the average admissions for AF have been ~ 60,000/ year without a significant change between 2005-2011,[Figure 1A], although this could reflect improved ambulatory care of AF patients.
Similar to previously described associations,in our large study from a California multiethnic population, two-thirds of the patients were over 65 yrs of age, with a third each in the age groups 65-79 yrs and > 80 yrs. AF has been reported to have an increased frequency in males although there are more women with this arrhythmia due to their longer life expectancy.[33], [41] By contrast,in our NVAF population, we found equal prevalence of women and men among those hospitalized for NVAF, which is likely due to a higher association of valvular heart disease among women in the afore mentioned study.[33]As has been previously described, there was also a Caucasian preponderance of NVAF in our cohort.[42]Two- thirds of our patients were admitted with moderate or major illnesses, while a third were either ED admissions or had mild severity of illness, confirming the widely known association of AF to acute ailments.
Due to lack of a specific ICD-9 code, we excluded other arrhythmias and considered ABL as specific for AF when associated in the principal position at the time of hospitalization. We also excluded patients with implantable cardiac devices to avoid those who could have AV node ablation. We decided on an approximate interval of two years as “ early” for these patients to have received follow-up care and to have declared themselves in need of invasive management based on natural progression of NVAF and clinical trials of medical management previously described.[7], [14], [43]
Several studies have shown that the outcomes of ABL are superior with shorter duration of AF. [44]-[48]However, despite these salutary results and advances in ABL technology, this procedure is performed in < 1% of patients within two years after the initial hospitalization in our population and includes racial and gender disparities. The Caucasian preponderance could at least partially reflect income and insurance status, however, these variables were adjusted for in the statistical analysis. The majority of California’s population resides in urban areas with medical centers in all major cities providing ABL for NVAF, which is reflected by most of our population. In a study from a national inpatient sample of patients with AF, (NIS) by Patel et al, about 2.9% of patients with underwent ABL, with a significant increase in ABL through a twelve year study period.[49] However this study sample does not represent new onset AF. The results are also weighted, as NIS represents a stratified random sample and does not include all patients, in contrast to our study in which we were able to account for all first time diagnosis of NVAF admissions. Our finding of a low ABL rate is concordant with regional variations in ABL that were noted among the US hospitals by Patel et al. In contrast to their investigation, we found that ABL was more frequent in patients with private insurance than Medicare. Consistent with the study by Bhave et al [43]of Medicare population, male Caucasians were more likely to undergo ABL in our group, even though one third of our patients were <65 yrs. In theirstudy,althoughthe majority wastreated bycardiologists, only about 15% consulted an electrophysiologist and about 1% underwent ABL, which is similar to that of our cohort. Most patients were managed by rate control with about a third also receiving anticoagulation in their study.[43]This finding supported by low ABL rates in our study suggests that rhythm control of AF by intervention is not widely recognized as a potential treatment.
At the present time, failure of AF ABL isdefined as recurrence of >30 sec of monitored AF., which is challenging to identify.[27], [50]Outcomes of clinical significance such as mortality, stroke or hospitalization for AF, have not been clearly documented.The Heart Rhythm Society recommends against ABL as an indication to prevent stroke; it favors using the CHADS2VASC risk scorefor prophylactic anticoagulation. [51]These factors may contribute to underutilization of ABL in the relatively early phase of the natural history of AF, when ABL is most effective. AF burden demonstrated in our study from California is disproportionately high compared to the number of trained electrophysiologists nationwide during the same period[52] and may indicate lack of access to care. The physician reimbursement for AF ABL is also poor for the complexity and duration of the procedure, compared to simple ablations, which could contribute to diminished interest in this beneficial procedure.
This study is a retrospective investigation with the inherent limitations of that method. We did not capture outpatient visits that could have led to ABL, and therefore our results reflect only the data pertaining to patients hospitalized with a first time diagnosis of NVAF. Any prior ablation outside California, if not coded at index hospitalization would not be identified from this method. There is also noICD 9 code specific for AF ABL; therefore our method of analysis may have missed capturing this procedure. There also may have been missed diagnoses by the coders, but the validity of the data is supported by periodic audits performed for billing purposes in most of hospitals in this study.We have also reviewed sample charts to ensure accuracy of exclusion and inclusion criteria. Although the purpose of our study was to determine early ablation (within two years of first hospitalization/ ED visit), patients may have undergone ABL later than that interval.
Conclusions
Our investigation suggests limited acceptance of ABL within two years of first hospitalization for NVAF in a multi-ethnic population and may reflect the need for greater awareness, improved education and access to care including ABL, as well as enhanced definition of clinical outcomes of this intervention.
Conflict Of Interests
None.
Disclosures
None.
References
- 1.Schnabel Renate B, Yin Xiaoyan, Gona Philimon, Larson Martin G, Beiser Alexa S, McManus David D, Newton-Cheh Christopher, Lubitz Steven A, Magnani Jared W, Ellinor Patrick T, Seshadri Sudha, Wolf Philip A, Vasan Ramachandran S, Benjamin Emelia J, Levy Daniel. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet. 2015 Jul 11;386 (9989):154–62. doi: 10.1016/S0140-6736(14)61774-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miyasaka Yoko, Barnes Marion E, Gersh Bernard J, Cha Stephen S, Bailey Kent R, Abhayaratna Walter P, Seward James B, Tsang Teresa S M. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006 Jul 11;114 (2):119–25. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]
- 3.Wu Eric Q, Birnbaum Howard G, Mareva Milena, Tuttle Edward, Castor Adam R, Jackman Warren, Ruskin Jeremy. Economic burden and co-morbidities of atrial fibrillation in a privately insured population. Curr Med Res Opin. 2005 Oct;21 (10):1693–9. doi: 10.1185/030079905X65475. [DOI] [PubMed] [Google Scholar]
- 4.Turakhia Mintu P, Shafrin Jason, Bognar Katalin, Goldman Dana P, Mendys Philip M, Abdulsattar Younos, Wiederkehr Daniel, Trocio Jeffrey. Economic Burden of Undiagnosed Nonvalvular Atrial Fibrillation in the United States. Am. J. Cardiol. 2015 Sep 01;116 (5):733–9. doi: 10.1016/j.amjcard.2015.05.045. [DOI] [PubMed] [Google Scholar]
- 5.January Craig T, Wann L Samuel, Alpert Joseph S, Calkins Hugh, Cigarroa Joaquin E, Cleveland Joseph C, Conti Jamie B, Ellinor Patrick T, Ezekowitz Michael D, Field Michael E, Murray Katherine T, Sacco Ralph L, Stevenson William G, Tchou Patrick J, Tracy Cynthia M, Yancy Clyde W. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014 Dec 02;130 (23):2071–104. doi: 10.1161/CIR.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 6.Roy Denis, Talajic Mario, Nattel Stanley, Wyse D George, Dorian Paul, Lee Kerry L, Bourassa Martial G, Arnold J Malcolm O, Buxton Alfred E, Camm A John, Connolly Stuart J, Dubuc Marc, Ducharme Anique, Guerra Peter G, Hohnloser Stefan H, Lambert Jean, Le Heuzey Jean-Yves, O'Hara Gilles, Pedersen Ole Dyg, Rouleau Jean-Lucien, Singh Bramah N, Stevenson Lynne Warner, Stevenson William G, Thibault Bernard, Waldo Albert L. Rhythm control versus rate control for atrial fibrillation and heart failure. N. Engl. J. Med. 2008 Jun 19;358 (25):2667–77. doi: 10.1056/NEJMoa0708789. [DOI] [PubMed] [Google Scholar]
- 7.Singh BN, Singh SN, Reda DJ, Tang XC, Lopez B, Harris CL, Fletcher RD, Sharma SC, Atwood JE, Jacobson AK. Amiodarone versus sotalol for atrial fibrillation. N Engl J Med. 2005;352:1861–1872. doi: 10.1056/NEJMoa041705. [DOI] [PubMed] [Google Scholar]
- 8.Pandit Sandeep V, Berenfeld Omer, Anumonwo Justus M B, Zaritski Roman M, Kneller James, Nattel Stanley, Jalife José. Ionic determinants of functional reentry in a 2-D model of human atrial cells during simulated chronic atrial fibrillation. Biophys. J. 2005 Jun;88 (6):3806–21. doi: 10.1529/biophysj.105.060459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jaïs P, Haïssaguerre M, Shah D C, Chouairi S, Gencel L, Hocini M, Clémenty J. A focal source of atrial fibrillation treated by discrete radiofrequency ablation. Circulation. 1997 Feb 04;95 (3):572–6. doi: 10.1161/01.cir.95.3.572. [DOI] [PubMed] [Google Scholar]
- 10.Wijffels M C, Kirchhof C J, Dorland R, Allessie M A. Atrial fibrillation begets atrial fibrillation. A study in awake chronically instrumented goats. Circulation. 1995 Oct 01;92 (7):1954–68. doi: 10.1161/01.cir.92.7.1954. [DOI] [PubMed] [Google Scholar]
- 11.Hayashi Kentaro, Fukunaga Masato, Yamaji Kyohei, An Yoshimori, Nagashima Michio, Hiroshima Kenichi, Ohe Masatsugu, Makihara Yu, Yamashita Kennosuke, Ando Kenji, Iwabuchi Masashi, Goya Masahiko. Impact of Catheter Ablation for Paroxysmal Atrial Fibrillation in Patients With Sick Sinus Syndrome - Important Role of Non-Pulmonary Vein Foci. Circ. J. 2016;80 (4):887–94. doi: 10.1253/circj.CJ-15-1384. [DOI] [PubMed] [Google Scholar]
- 12.Mohanty Sanghamitra, Mohanty Prasant, Di Biase Luigi, Trivedi Chintan, Morris Eli Hamilton, Gianni Carola, Santangeli Pasquale, Bai Rong, Sanchez Javier E, Hranitzky Patrick, Gallinghouse G Joseph, Al-Ahmad Amin, Horton Rodney P, Hongo Richard, Beheiry Salwa, Elayi Claude S, Lakkireddy Dhanunjaya, Madhu Reddy Yaruva, Viles Gonzalez Juan F, Burkhardt J David, Natale Andrea. Long-term follow-up of patients with paroxysmal atrial fibrillation and severe left atrial scarring: comparison between pulmonary vein antrum isolation only or pulmonary vein isolation combined with either scar homogenization or trigger ablation. Europace. 2016 Dec 29; () doi: 10.1093/europace/euw338. [DOI] [PubMed] [Google Scholar]
- 13.Takigawa Masateru, Takahashi Atsushi, Kuwahara Taishi, Okubo Kenji, Takahashi Yoshihide, Nakashima Emiko, Watari Yuji, Yamao Kazuya, Nakajima Jun, Takagi Katsumasa, Kimura Shigeki, Hikita Hiroyuki, Hirao Kenzo, Isobe Mitsuaki. Impact of Non-Pulmonary Vein Foci on the Outcome of the Second Session of Catheter Ablation for Paroxysmal Atrial Fibrillation. J. Cardiovasc. Electrophysiol. 2015 Jul;26 (7):739–46. doi: 10.1111/jce.12681. [DOI] [PubMed] [Google Scholar]
- 14.Hussein Ayman A, Saliba Walid I, Barakat Amr, Bassiouny Mohammed, Chamsi-Pasha Mohammed, Al-Bawardy Rasha, Hakim Ali, Tarakji Khaldoun, Baranowski Bryan, Cantillon Daniel, Dresing Thomas, Tchou Patrick, Martin David O, Varma Niraj, Bhargava Mandeep, Callahan Thomas, Niebauer Mark, Kanj Mohamed, Chung Mina, Natale Andrea, Lindsay Bruce D, Wazni Oussama M. Radiofrequency Ablation of Persistent Atrial Fibrillation: Diagnosis-to-Ablation Time, Markers of Pathways of Atrial Remodeling, and Outcomes. Circ Arrhythm Electrophysiol. 2016 Jan;9 (1) doi: 10.1161/CIRCEP.115.003669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walfridsson H, Walfridsson U, Nielsen J Cosedis, Johannessen A, Raatikainen P, Janzon M, Levin L A, Aronsson M, Hindricks G, Kongstad O, Pehrson S, Englund A, Hartikainen J, Mortensen L S, Hansen P S. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation: results on health-related quality of life and symptom burden. The MANTRA-PAF trial. Europace. 2015 Feb;17 (2):215–21. doi: 10.1093/europace/euu342. [DOI] [PubMed] [Google Scholar]
- 16.Wazni Oussama M, Marrouche Nassir F, Martin David O, Verma Atul, Bhargava Mandeep, Saliba Walid, Bash Dianna, Schweikert Robert, Brachmann Johannes, Gunther Jens, Gutleben Klaus, Pisano Ennio, Potenza Dominico, Fanelli Raffaele, Raviele Antonio, Themistoclakis Sakis, Rossillo Antonio, Bonso Aldo, Natale Andrea. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of symptomatic atrial fibrillation: a randomized trial. JAMA. 2005 Jun 01;293 (21):2634–40. doi: 10.1001/jama.293.21.2634. [DOI] [PubMed] [Google Scholar]
- 17.Pappone Carlo, Augello Giuseppe, Sala Simone, Gugliotta Filippo, Vicedomini Gabriele, Gulletta Simone, Paglino Gabriele, Mazzone Patrizio, Sora Nicoleta, Greiss Isabelle, Santagostino Andreina, LiVolsi Laura, Pappone Nicola, Radinovic Andrea, Manguso Francesco, Santinelli Vincenzo. A randomized trial of circumferential pulmonary vein ablation versus antiarrhythmic drug therapy in paroxysmal atrial fibrillation: the APAF Study. J. Am. Coll. Cardiol. 2006 Dec 05;48 (11):2340–7. doi: 10.1016/j.jacc.2006.08.037. [DOI] [PubMed] [Google Scholar]
- 18.Stabile Giuseppe, Bertaglia Emanuele, Senatore Gaetano, De Simone Antonio, Zoppo Franco, Donnici Giovanni, Turco Pietro, Pascotto Pietro, Fazzari Massimo, Vitale Dino Franco. Catheter ablation treatment in patients with drug-refractory atrial fibrillation: a prospective, multi-centre, randomized, controlled study (Catheter Ablation For The Cure Of Atrial Fibrillation Study). Eur. Heart J. 2006 Jan;27 (2):216–21. doi: 10.1093/eurheartj/ehi583. [DOI] [PubMed] [Google Scholar]
- 19.Jaïs Pierre, Cauchemez Bruno, Macle Laurent, Daoud Emile, Khairy Paul, Subbiah Rajesh, Hocini Mélèze, Extramiana Fabrice, Sacher Fréderic, Bordachar Pierre, Klein George, Weerasooriya Rukshen, Clémenty Jacques, Haïssaguerre Michel. Catheter ablation versus antiarrhythmic drugs for atrial fibrillation: the A4 study. Circulation. 2008 Dec 09;118 (24):2498–505. doi: 10.1161/CIRCULATIONAHA.108.772582. [DOI] [PubMed] [Google Scholar]
- 20.Pappone Carlo, Vicedomini Gabriele, Augello Giuseppe, Manguso Francesco, Saviano Massimo, Baldi Mario, Petretta Andrea, Giannelli Luigi, Calovic Zarko, Guluta Vladimir, Tavazzi Luigi, Santinelli Vincenzo. Radiofrequency catheter ablation and antiarrhythmic drug therapy: a prospective, randomized, 4-year follow-up trial: the APAF study. Circ Arrhythm Electrophysiol. 2011 Dec;4 (6):808–14. doi: 10.1161/CIRCEP.111.966408. [DOI] [PubMed] [Google Scholar]
- 21.Takahashi Yoshihide, O'Neill Mark D, Hocini Méléze, Reant Patricia, Jonsson Anders, Jaïs Pierre, Sanders Prashanthan, Rostock Thomas, Rotter Martin, Sacher Frédéric, Laffite Stephane, Roudaut Raymond, Clémenty Jacques, Haïssaguerre Michel. Effects of stepwise ablation of chronic atrial fibrillation on atrial electrical and mechanical properties. J. Am. Coll. Cardiol. 2007 Mar 27;49 (12):1306–14. doi: 10.1016/j.jacc.2006.11.033. [DOI] [PubMed] [Google Scholar]
- 22.Bhargava Mandeep, Di Biase Luigi, Mohanty Prasant, Prasad Subramanyam, Martin David O, Williams-Andrews Michelle, Wazni Oussama M, Burkhardt J David, Cummings Jennifer E, Khaykin Yaariv, Verma Atul, Hao Steven, Beheiry Salwa, Hongo Richard, Rossillo Antonio, Raviele Antonio, Bonso Aldo, Themistoclakis Sakis, Stewart Kelly, Saliba Walid I, Schweikert Robert A, Natale Andrea. Impact of type of atrial fibrillation and repeat catheter ablation on long-term freedom from atrial fibrillation: results from a multicenter study. Heart Rhythm. 2009 Oct;6 (10):1403–12. doi: 10.1016/j.hrthm.2009.06.014. [DOI] [PubMed] [Google Scholar]
- 23.Zhao R-C, Han W, Han J, Yu J, Guo J, Fu J-L, Li Z, Zhao R-Z. Observation of the efficacy of radiofrequency catheter ablation on patients with different forms of atrial fibrillation. Eur Rev Med Pharmacol Sci. 2016 Oct;20 (19):4141–4147. [PubMed] [Google Scholar]
- 24.Oral Hakan, Veerareddy Srikar, Good Eric, Hall Burr, Cheung Peter, Tamirisa Kamala, Han Jihn, Fortino Jackie, Chugh Aman, Bogun Frank, Pelosi Frank, Morady Fred. Prevalence of asymptomatic recurrences of atrial fibrillation after successful radiofrequency catheter ablation. J. Cardiovasc. Electrophysiol. 2004 Aug;15 (8):920–4. doi: 10.1046/j.1540-8167.2004.04055.x. [DOI] [PubMed] [Google Scholar]
- 25.Cappato Riccardo, Calkins Hugh, Chen Shih-Ann, Davies Wyn, Iesaka Yoshito, Kalman Jonathan, Kim You-Ho, Klein George, Natale Andrea, Packer Douglas, Skanes Allan, Ambrogi Federico, Biganzoli Elia. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol. 2010 Feb;3 (1):32–8. doi: 10.1161/CIRCEP.109.859116. [DOI] [PubMed] [Google Scholar]
- 26.Srivatsa Uma N, Danielsen Beate, Anderson Ivan, Amsterdam Ezra, Pezeshkian Nayereh, Yang Yingbo, White Richard H. Risk predictors of stroke and mortality after ablation for atrial fibrillation: the California experience 2005-2009. Heart Rhythm. 2014 Nov;11 (11):1898–903. doi: 10.1016/j.hrthm.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 27.January Craig T, Wann L Samuel, Alpert Joseph S, Calkins Hugh, Cigarroa Joaquin E, Cleveland Joseph C, Conti Jamie B, Ellinor Patrick T, Ezekowitz Michael D, Field Michael E, Murray Katherine T, Sacco Ralph L, Stevenson William G, Tchou Patrick J, Tracy Cynthia M, Yancy Clyde W. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2014 Dec 02;64 (21):e1–76. doi: 10.1016/j.jacc.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 28.Steiner Claudia, Elixhauser Anne, Schnaier Jenny. The healthcare cost and utilization project: an overview. Eff Clin Pract. 2002 Jun 29;5 (3):143–51. [PubMed] [Google Scholar]
- 29.Romano P S, Chan B K. Risk-adjusting acute myocardial infarction mortality: are APR-DRGs the right tool? Health Serv Res. 2000 Mar;34 (7):1469–89. [PMC free article] [PubMed] [Google Scholar]
- 30.White Richard H, Geraghty Estella Marie, Brunson Ann, Murin Susan, Wun Ted, Spencer Fred, Romano Patrick S. High variation between hospitals in vena cava filter use for venous thromboembolism. JAMA Intern Med. 2013 Apr 08;173 (7):506–12. doi: 10.1001/jamainternmed.2013.2352. [DOI] [PubMed] [Google Scholar]
- 31.Zlotnik Alexander, Cuchi Miguel Alfaro, Pérez Pérez Maria Carmen. Lifting the weight of a diagnosis-related groups family change: a comparison between refined and non-refined DRG systems for top-down cost accounting and efficiency indicators. HIM J. 2015;44 (2):12–9. [PubMed] [Google Scholar]
- 32.Go A S, Hylek E M, Phillips K A, Chang Y, Henault L E, Selby J V, Singer D E. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001 May 09;285 (18):2370–5. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 33.Benjamin E J, Levy D, Vaziri S M, D'Agostino R B, Belanger A J, Wolf P A. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994 Mar 16;271 (11):840–4. [PubMed] [Google Scholar]
- 34.Feinberg W M, Blackshear J L, Laupacis A, Kronmal R, Hart R G. Prevalence, age distribution, and gender of patients with atrial fibrillation. Analysis and implications. Arch. Intern. Med. 1995 Mar 13;155 (5):469–73. [PubMed] [Google Scholar]
- 35.Krahn A D, Manfreda J, Tate R B, Mathewson F A, Cuddy T E. The natural history of atrial fibrillation: incidence, risk factors, and prognosis in the Manitoba Follow-Up Study. Am. J. Med. 1995 May;98 (5):476–84. doi: 10.1016/S0002-9343(99)80348-9. [DOI] [PubMed] [Google Scholar]
- 36.Tsang Teresa S M, Petty George W, Barnes Marion E, O'Fallon W Michael, Bailey Kent R, Wiebers David O, Sicks JoRean D, Christianson Teresa J H, Seward James B, Gersh Bernard J. The prevalence of atrial fibrillation in incident stroke cases and matched population controls in Rochester, Minnesota: changes over three decades. J. Am. Coll. Cardiol. 2003 Jul 02;42 (1):93–100. doi: 10.1016/s0735-1097(03)00500-x. [DOI] [PubMed] [Google Scholar]
- 37.Gami Apoor S, Hodge Dave O, Herges Regina M, Olson Eric J, Nykodym Jiri, Kara Tomas, Somers Virend K. Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J. Am. Coll. Cardiol. 2007 Feb 06;49 (5):565–71. doi: 10.1016/j.jacc.2006.08.060. [DOI] [PubMed] [Google Scholar]
- 38.Albina Gastón, De Luca Julián, Conde Diego, Giniger Alberto. Atrial fibrillation: an observational study with outpatients. Pacing Clin Electrophysiol. 2014 Nov;37 (11):1485–91. doi: 10.1111/pace.12462. [DOI] [PubMed] [Google Scholar]
- 39.Simantirakis E N, Papakonstantinou P E, Chlouverakis G I, Kanoupakis E M, Mavrakis H E, Kallergis E M, Arkolaki E G, Vardas P E. Asymptomatic versus symptomatic episodes in patients with paroxysmal atrial fibrillation via long-term monitoring with implantable loop recorders. Int. J. Cardiol. 2017 Mar 15;231 ():125–130. doi: 10.1016/j.ijcard.2016.12.025. [DOI] [PubMed] [Google Scholar]
- 40.Romanov Alexander, Martinek Martin, Pürerfellner Helmut, Chen Shaojie, De Melis Mirko, Grazhdankin Igor, Ponomarev Dmitry, Losik Denis, Strelnikov Artem, Shabanov Vitaliy, Karaskov Alexander, Pokushalov Evgeny. Incidence of atrial fibrillation detected by continuous rhythm monitoring after acute myocardial infarction in patients with preserved left ventricular ejection fraction: results of the ARREST study. Europace. 2017 Jan 08; () doi: 10.1093/europace/euw344. [DOI] [PubMed] [Google Scholar]
- 41.Stewart S, Hart C L, Hole D J, McMurray J J. Population prevalence, incidence, and predictors of atrial fibrillation in the Renfrew/Paisley study. Heart. 2001 Nov;86 (5):516–21. doi: 10.1136/heart.86.5.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alonso Alvaro, Agarwal Sunil K, Soliman Elsayed Z, Ambrose Marietta, Chamberlain Alanna M, Prineas Ronald J, Folsom Aaron R. Incidence of atrial fibrillation in whites and African-Americans: the Atherosclerosis Risk in Communities (ARIC) study. Am. Heart J. 2009 Jul;158 (1):111–7. doi: 10.1016/j.ahj.2009.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bhave Prashant D, Lu Xin, Girotra Saket, Kamel Hooman, Vaughan Sarrazin Mary S. Race- and sex-related differences in care for patients newly diagnosed with atrial fibrillation. Heart Rhythm. 2015 Jul;12 (7):1406–12. doi: 10.1016/j.hrthm.2015.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Scherr Daniel, Khairy Paul, Miyazaki Shinsuke, Aurillac-Lavignolle Valerie, Pascale Patrizio, Wilton Stephen B, Ramoul Khaled, Komatsu Yuki, Roten Laurent, Jadidi Amir, Linton Nick, Pedersen Michala, Daly Matthew, O'Neill Mark, Knecht Sebastien, Weerasooriya Rukshen, Rostock Thomas, Manninger Martin, Cochet Hubert, Shah Ashok J, Yeim Sunthareth, Denis Arnaud, Derval Nicolas, Hocini Meleze, Sacher Frederic, Haissaguerre Michel, Jais Pierre. Five-year outcome of catheter ablation of persistent atrial fibrillation using termination of atrial fibrillation as a procedural endpoint. Circ Arrhythm Electrophysiol. 2015 Feb;8 (1):18–24. doi: 10.1161/CIRCEP.114.001943. [DOI] [PubMed] [Google Scholar]
- 45.Pathak Rajeev K, Middeldorp Melissa E, Lau Dennis H, Mehta Abhinav B, Mahajan Rajiv, Twomey Darragh, Alasady Muayad, Hanley Lorraine, Antic Nicholas A, McEvoy R Doug, Kalman Jonathan M, Abhayaratna Walter P, Sanders Prashanthan. Aggressive risk factor reduction study for atrial fibrillation and implications for the outcome of ablation: the ARREST-AF cohort study. J. Am. Coll. Cardiol. 2014 Dec 02;64 (21):2222–31. doi: 10.1016/j.jacc.2014.09.028. [DOI] [PubMed] [Google Scholar]
- 46.Matsuo Seiichiro, Lellouche Nicolas, Wright Matthew, Bevilacqua Michela, Knecht Sébastien, Nault Isabelle, Lim Kang-Teng, Arantes Leonardo, O'Neill Mark D, Platonov Pyotr G, Carlson Jonas, Sacher Frederic, Hocini Mélèze, Jaïs Pierre, Haïssaguerre Michel. Clinical predictors of termination and clinical outcome of catheter ablation for persistent atrial fibrillation. J. Am. Coll. Cardiol. 2009 Aug 25;54 (9):788–95. doi: 10.1016/j.jacc.2009.01.081. [DOI] [PubMed] [Google Scholar]
- 47.Walters Tomos E, Nisbet Ashley, Morris Gwilym M, Tan Gabriel, Mearns Megan, Teo Eliza, Lewis Nigel, Ng AiVee, Gould Paul, Lee Geoffrey, Joseph Stephen, Morton Joseph B, Zentner Dominica, Sanders Prashanthan, Kistler Peter M, Kalman Jonathan M. Progression of atrial remodeling in patients with high-burden atrial fibrillation: Implications for early ablative intervention. Heart Rhythm. 2016 Feb;13 (2):331–9. doi: 10.1016/j.hrthm.2015.10.028. [DOI] [PubMed] [Google Scholar]
- 48.Takigawa Masateru, Takahashi Atsushi, Kuwahara Taishi, Okubo Kenji, Takahashi Yoshihide, Watari Yuji, Takagi Katsumasa, Fujino Tadashi, Kimura Shigeki, Hikita Hiroyuki, Tomita Makoto, Hirao Kenzo, Isobe Mitsuaki. Long-term follow-up after catheter ablation of paroxysmal atrial fibrillation: the incidence of recurrence and progression of atrial fibrillation. Circ Arrhythm Electrophysiol. 2014 Apr;7 (2):267–73. doi: 10.1161/CIRCEP.113.000471. [DOI] [PubMed] [Google Scholar]
- 49.Patel Nileshkumar, Deshmukh Abhishek, Thakkar Badal, Coffey James O, Agnihotri Kanishk, Patel Achint, Ainani Nitesh, Nalluri Nikhil, Patel Nilay, Patel Nish, Patel Neil, Badheka Apurva O, Kowalski Marcin, Hendel Robert, Viles-Gonzalez Juan, Noseworthy Peter A, Asirvatham Samuel, Lo Kaming, Myerburg Robert J, Mitrani Raul D. Gender, Race, and Health Insurance Status in Patients Undergoing Catheter Ablation for Atrial Fibrillation. Am. J. Cardiol. 2016 Apr 01;117 (7):1117–26. doi: 10.1016/j.amjcard.2016.01.040. [DOI] [PubMed] [Google Scholar]
- 50.Verma Atul, Champagne Jean, Sapp John, Essebag Vidal, Novak Paul, Skanes Allan, Morillo Carlos A, Khaykin Yaariv, Birnie David. Discerning the incidence of symptomatic and asymptomatic episodes of atrial fibrillation before and after catheter ablation (DISCERN AF): a prospective, multicenter study. JAMA Intern Med. 2013 Jan 28;173 (2):149–56. doi: 10.1001/jamainternmed.2013.1561. [DOI] [PubMed] [Google Scholar]
- 51.Lip G Y H. Recommendations for thromboprophylaxis in the 2012 focused update of the ESC guidelines on atrial fibrillation: a commentary. J. Thromb. Haemost. 2013 Apr;11 (4):615–26. doi: 10.1111/jth.12140. [DOI] [PubMed] [Google Scholar]
- 52.Deering Thomas F, Clair Walter K, Delaughter M Craig, Fisher Westby G, Garlitski Ann C, Wilkoff Bruce L, Gillis Anne M. A Heart Rhythm Society Electrophysiology Workforce study: current survey analysis of physician workforce trends. Heart Rhythm. 2010 Sep;7 (9):1346–55. doi: 10.1016/j.hrthm.2010.07.026. [DOI] [PubMed] [Google Scholar]


