Abstract
Given the high prevalence and risk of stroke associated with atrial fibrillation (AF), detection strategies have important public health implications. The ongoing prospective, single-arm, open-label, multicenter REVEAL AF trial is evaluating the incidence of previously undetected AF using an insertable cardiac monitor (ICM) in patients without prior AF or device implantation, but who could be at risk for AF due to their demographic characteristics, +/- non-specific but compatible symptoms. Enrollment required an elevated AF risk profile defined as CHADS2≥3 or CHADS2=2 plus one or more of the following: coronary artery disease, renal impairment, sleep apnea or chronic obstructive pulmonary disease. Exclusions included stroke or transient ischemic attack occurring in the previous year. Of 450 subjects screened, 399 underwent a device insertion attempt, and 395 were included in the final analysis (Reveal XT: n=122; Reveal LINQ: n=273; excluded: n=4). Participants were primarily identified by demographic characteristics and the presence of nonspecific symptoms, but without prior documentation of “overt” AF. The most common symptoms were palpitations (51%), dizziness/lightheadedness/pre-syncope (36%), and shortness of breath (36%). Over 100 subjects were enrolled in each pre-defined CHADS2 subgroup (2, 3 and ≥4). AF risk factors not included in the CHADS2 score were well represented (prevalence≥15%). Procedure and/or device related serious adverse events were low, with the miniaturized Reveal LINQ ICM having a more favorable safety profile than the predicate Reveal XT (all: n=13 [3.3%]; LINQ: n=6 [2.2%]; XT: n=7 [5.7%]). These data demonstrate that REVEAL AF was successful in enrolling its target population, high risk patients were willing to undergo ICM monitoring for AF screening, and ICM use in this group is becoming increasingly safe with advancements in technology. A clinically meaningful incidence of device detected AF in this study will inform clinical decisions regarding ICM use for AF screening in patients at risk.
Keywords: Atrial fibrillation, screening, insertable cardiac monitor
Introduction
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia and is a leading cause of morbidity and mortality. Approximately 33.5 million patients worldwide in 2010 had been diagnosed with AF and the figure is projected to double by mid-century.[1]-[5] This increasing burden of AF will likely lead to a higher incidence of stroke, systemic embolism, heart failure, and death: known sequelae of this arrhythmia.
The true burden of AF may be even higher than currently estimated. Although some patients are aware of their AF episodes, up to two-thirds of patients are asymptomatic, having so-called “silent AF.” [6], [7] Importantly, silent AF carries the same risks as symptomatic AF.[8] Indeed, monitoring studies with previously implanted cardiac devices have demonstrated an association between asymptomatic AF episodes of brief duration and increased risk of stroke/systemic embolism in such patients.[9]-[13] Of concern, AF may only be diagnosed after complications like ischemic stroke have occurred.[14], [15] Given the high prevalence and risk associated with AF, there is considerable interest in: the development of screening strategies to detect AF and hopefully modify morbidity and mortality by early institution of preventive therapies, such as oral anticoagulation (OAC); to do so in patients with or without underlying electrical disorders necessitating pacemaker or defibrillator implantation; and to understand if the consequences of “silent AF” are as significant in patients without underlying device-requiring disorders as in those with them. The key issues related to AF screening, as with screening for any disease, are: 1) who to screen and 2) how to screen to optimize treatment and cost-effectiveness.
To be useful and cost-effective, a screening strategy needs to balance the correct detection tool with the targeted at-risk population. Common devices used to screen for atrial fibrillation range from non-invasive devices using smartphone, hand-held, and wearable platforms employing external ECG, and/or pulse detection to provide snapshot screening, to insertable cardiac monitors (ICMs; subcutaneous ECG recorders) that provide continuous long-term monitoring for up to three years.[16]-[19] In a lower risk population, a simpler, less invasive, and cheaper test may be sufficient. In a higher risk population that is a) more likely to develop AF and b) at higher risk of morbidity/mortality secondary to the disease, a minimally invasive tool with a better detection rate yet potentially higher cost might be justified. However, the patient acceptance, safety and efficacy of such a strategy are unknown.
The REVEAL AF study (NCT01727297) is designed to evaluate the incidence of AF using an ICM device in patients with elevated risk profiles.[20] Although follow up for the primary endpoint is ongoing, enrollment is complete and all patients have undergone their baseline visit and device insertion. In this manuscript, we report selected baseline demographic data, patient acceptance of the REVEAL AF ICM monitoring strategy, and procedure and safety details of ICM insertion. During the course of the trial, a new miniaturized ICM became commercially available and was implemented in the study. As such, REVEAL AF provides a unique opportunity to characterize the safety profile of evolving ICM technology within a patient population suspected to be at high risk for AF.
Materials and Methods
The REVEAL AF trial design has been described in detail previously.[20] Briefly, REVEAL AF (NCT01727297) is an ongoing prospective, single-arm, open-label, multicenter, clinical study that enrolled patients in 58 centers in the United States and Europe between November 2012 and June 2015. Four hundred and fifty adults suspected to have or be at risk of AF (due to demographics and/or symptoms) with elevated AF risk profiles based on CHADS2 score plus additional markers were enrolled in the study. Elevated risk for AF per CHADS2 was defined as a score ≥ 3 or a CHADS2 score = 2 with at least one of the following additional risk factors documented: coronary artery disease, renal impairment, sleep apnea, or chronic obstructive pulmonary disease. Patients were excluded if they had an ischemic stroke or a transient ischemic attack in the previous 12 months, or a history of hemorrhagic stroke. All consented patients were required to have a minimum of 24 hours of external ECG assessment (using Holter monitoring or other techniques) within the previous 90 days prior to enrollment or before device insertion. Patients were excluded from the trial if AF was diagnosed by external monitoring. Baseline demographics, medical history, blood samples for biomarker analysis (as possible predictors), echocardiogram, and a quality of life questionnaire were collected. This study was conducted in accordance with the Declaration of Helsinki. The protocol was approved by each site’s institutional Review Board or Ethics Committee and all patients provided written informed consent prior to participating in the study.
The ICM (Reveal XT or Reveal LINQ, Medtronic, plc, Dublin, Ireland) procedure occurred within 6 weeks of study enrollment and was performed in accordance with each hospital’s standard insertion practice and the Medtronic Reveal ICM insertion instructions. The Medtronic REVEAL ICM insertion instructions for the Reveal XT device require a single-incision procedure with normal aseptic techniques. A small subcutaneous pocket slightly smaller than the width of the device is created, the device is inserted into the pocket with electrodes facing outward, and secured to underlying tissue using the suture holes on the device header. For the LINQ device, the Medtronic REVEAL ICM insertion instructions require use of conventional antiseptic and local anesthetic procedures. The skin adjacent to the incision location is pinched, and the incision tool provided with the device is used to make a less than 1 cm incision. The insertion tool preloaded with the LINQ device is then inserted and rotated 180 degrees to create a pocket approximately 8 mm under the skin. The plunger on the insertion tool is pushed to deliver the device into the pocket approximately 10mm past the incision. Details on device insertion were collected, including device location and orientation, suture placement, and R-wave diagnostic sensing. Device programing was set to maximize the device's storage of ECG recordings of AF episodes.[20] Patients are being followed for a minimum of 18 and maximum of 30 months. Procedure and device related adverse events (AEs) were adjudicated by investigators as well as an independent Clinical Events Committee (CEC) composed of non-industry employed physicians. CEC adjudication was conducted via quorum, with at least three voting members of the CEC. Procedure-related AEs were defined as an adverse event that occurs due to any procedure related to the implantation or surgical modification of the system. Device related adverse events were defined as an adverse event that occurred due to the Reveal XT or Reveal LINQ device. AEs are considered serious if an event led to death or serious deterioration in the health of a subject (as indicated by a life-threatening illness or injury, permanent impairment of a body structure or a body function, in-patient hospitalization or prolonged hospitalization, or medical or surgical intervention to prevent permanent impairment to a body structure or a body function).
Statistics
Baseline characteristics are summarized using descriptive statistics. Continuous variables are presented as mean ± standard deviation. Categorical variables are presented as count and percentage. All analyses were completed using SAS version 9.4 (SAS Institute, Cary, NC).
EnSite NavXTM system (St. Jude Medical, St. Paul, USA) was used to construct the LA geometry and a voltage map of the antral region of the 4 PVs using a segmented cardiac CT template with/out fusion of the images.
Results
Demographics
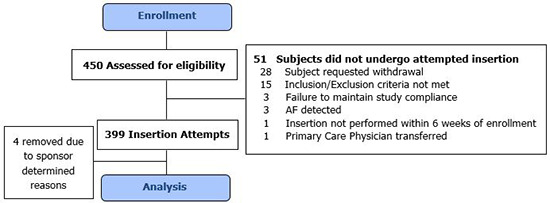
Four hundred and fifty subjects were enrolled at 58 sites. Of these, 51 did not undergo a Reveal ICM insertion attempt due to subject withdrawal (n=28), not meeting inclusion/exclusion criteria (n=15), failure to maintain study compliance (n=3), AF detected prior to device insertion (n=3), device insertion not completed within 6 weeks of enrollment (n=1), and a change in primary care physician (n=1). Consequently, 399 subjects (US: n=306, Europe: n=93) underwent an insertion attempt. Of these, four subjects at a single site were excluded for sponsor determined reasons. Thus, 395 subjects at 57 sites were included in the present analysis [Figure. 1].
Figure 1. Subject flow diagram.
Sixty nine percent (69%) of subjects received the Reveal LINQ ICM and 31% of subjects received the predicate Reveal XT ICM device[Figure 2]. Baseline demographics and medical history are presented in [Table 1]. Subjects aged 38-92 years were enrolled, with a mean age of 72 ± 10 years. Seventy eight percent of the study population was aged ≥65 years. Males accounted for 52% of the study population. At least 100 patients have been enrolled and undergone an insertion attempt in each pre-defined CHADS2 subgroup (2, 3 and ≥4). Due to errors in scoring, one patient with a CHADS2 score of 1, and one patient with a CHADS2 score of 2 without additional protocol-specified AF risk factors underwent device insertion.
Figure 2. Image of Reveal XT (left) and LINQ (right) devices.

Table 1. Baseline patient characteristics.
| Characteristic | All attempted insertions (N = 395) |
| Device inserted/attempted | |
| Reveal LINQ | 273 (69.1%) |
| Reveal XT | 122 (30.9%) |
| Demographics | |
| Age, years | |
| Mean ± Standard Deviation | 71.6 ± 9.8 |
| Age category | |
| Under 65 | 88 (22.3%) |
| 65 to 75 | 131 (33.2%) |
| 75 and older | 176 (44.6%) |
| Gender | |
| Male | 207 (52.4%) |
| ; Female | 188 (47.6%) |
| Body mass index (BMI) | |
| Mean ± Standard Deviation | 31.2 ± 6.5 |
| CHADS2 score | |
| 1 | 1 (0.3%) |
| 2 | 158 (40.0%) |
| 3 | 131 (33.2%) |
| ; 4 | 105 (26.6%) |
| Reason AF is suspected | |
| Symptoms | 93 (23.5%) |
| Demographics | 62 (15.7%) |
| Both symptoms and demographics | 240 (60.8%) |
| Symptoms within 3 months of consent | |
| None | 38 (9.6%) |
| Chest pain | 80 (20.3%) |
| Dizziness/lightheadedness/presyncope | 142 (35.9%) |
| Rapid heart beat | 81 (20.5%) |
| Shortness of breath | 142 (35.9%) |
| Edema | 51 (12.9%) |
| Fatigue/weakness | 119 (30.1%) |
| Palpitations | 201 (50.9%) |
| Syncope | 77 (19.5%) |
| Other | 20 (5.1%) |
| Medical history | |
| Renal Dysfunction | 64 (16.2%) |
| Congestive Heart Failure | 81 (20.5%) |
| Coronary Artery Disease | 234 (59.2%) |
| Hypertension | 370 (93.7%) |
| COPD | 76 (19.2%) |
| Sleep apnea | 104 (26.3%) |
| Diabetes | 249 (63.0%) |
| Vascular disease | |
| Cerebrovascular accident (stroke) | 80 (20.3%) |
| Transient Ischemic Attack | 76 (19.2%) |
Most subjects were suspected to have AF based on both symptoms and demographics (61%), followed by symptoms alone (24%). The most common symptoms were palpitations (51%), dizziness, lightheadedness or pre-syncope (36%), and shortness of breath (36%). Less common symptoms included fatigue/weakness (30%), rapid heartbeat (21%), chest pain (20%), syncope (20%) and edema (13%).
Hypertension was present in 94% of subjects. Other common demographic characteristics included diabetes (63%), coronary artery disease (59%), sleep apnea (26%) and heart failure (21%). Twenty percent of patients had a previous stroke and 19% had a previous transient ischemic attack greater than 12 months prior to enrollment.
Insertion Procedure
Procedure data are presented in [Table 2]. The most common insertion location was between the 1st and 4th rib close to the sternum for both devices (Reveal XT: n=76 [62%]; LINQ: n=129 [47%]). Twenty five percent of Reveal XT (n=30) and 17% of LINQ devices (n=45) were placed between the 1st and 4th rib, but more lateral to the sternum. LINQ devices were also frequently placed inferior to the 4th rib close to the sternum (n=70 [26%]), whereas Reveal XT devices were not (n=6, 4.9%). The ICM was most frequently oriented vertically for the Reveal XT (n=67 [55%]), and at a 45 degree angle for Reveal LINQ (n=232 [85%]). The Reveal XT device was often sutured during the insertion (n=107, [88%]), whereas few LINQ devices were sutured (n=13 [5%]). Ninety-eight percent (n=385) of ICM devices were inserted with electrodes directed outwards, as recommended by the manufacturer, and R-wave diagnostic sensing was completed on 96% of ICMs.
Table 2. Insertion procedure.
| LINQ(N=272) | Reveal XT(N=122) | All insertions(N=394) | |
| Device location | |||
| Between clavicle and 1st rib (close to sternum) | 2 (0.7%) | 2 (1.6%) | 4 (1.0%) |
| Between clavicle and 1st rib | 0 (0.0%) | 4 (3.3%) | 4 (1.0%) |
| Between 1st and 4th rib (close to sternum) | 129 (47.4%) | 76 (62.3%) | 205 (52.0%) |
| Between 1st and 4th rib | 45 (16.5%) | 30 (24.6%) | 75 (19.0%) |
| Inferior to 4th rib (close to sternum) | 70 (25.7%) | 6 (4.9%) | 76 (19.3%) |
| Inferior to 4th rib | 19 (7.0%) | 4 (3.3%) | 23 (5.8%) |
| Other | 7 (2.6%) | 0 (0.0%) | 7 (1.8%) |
| Device orientation | |||
| Horizontal | 7 (2.6%) | 4 (3.3%) | 11 (2.8%) |
| Vertical | 21 (7.7%) | 67 (54.9%) | 88 (22.3%) |
| 45 degrees | 232 (85.3%) | 42 (34.4%) | 274 (69.5%) |
| 135 degrees | 10 (3.7%) | 3 (2.5%) | 13 (3.3%) |
| Other | 2 (0.7%) | 6 (4.9%) | 8 (2.0%) |
| Device sutured during insertion | 13 (4.8%) | 107 (87.7%) | 120 (30.5%) |
| Electrodes outward (as recommended) | 263 (96.7%) | 122 (100%) | 385 (97.7%) |
| R-wave diagnostic sensing completed | 259 (95.2%) | 119 (97.5%) | 378 (95.9%) |
Safety
Procedure and device related AEs are displayed in [Table 3]. For subjects receiving the Reveal XT device, 4.1% (n=5) and 5.7% (n=7) experienced a procedure and device related AE, respectively. Procedure related AEs included impaired healing (including pruritus or erythema, n=2), insertion site infection (n=2), and insertion site pain/irritation (n=2). Device-related AEs associated with the Reveal XT ICM included insertion site infection (n=1), discomfort (n=1), and insertion site pain/irritation (n=5).
Table 3. Procedure and device related adverse events.
*One subject accounts for two different Reveal XT procedure related events. Neither was deemed serious by CEC or site.
| Combined results | Reveal XT(N=122) | Reveal LINQ(N=272 + 1 attempt) | ||||||
| Total | Serious per CEC | Serious per investigator | Total | Serious per CEC | Serious per investigator | |||
| Device and/or procedure related | 11 (10*, 8.2%) | 7 (5.7%) | 2 (1.6%) | 9 (3.3%) | 6 (2.2%) | 4 (1.5%) | ||
| Procedure related | 6 (5*, 4.1%) | 3 (2.5%) | 1 (0.8%) | 5 (1.8%) | 4 (1.5%) | 3 (1.1%) | ||
| Device related | 7 (5.7%) | 6 (4.9%) | 1 (0.8%) | 7 (2.6%) | 5 (1.8%) | 3 (1.1%) | ||
| Individual results | ||||||||
| Device dislocation/ device site erosion | Device and/or procedure related | 0 | 0 | 0 | 4 (1.5%) | 4 (1.5%) | 3 (1.1%) | |
| Procedure related | 0 | 0 | 0 | 3 (1.1%) | 3 (1.1%) | 2 (0.7%) | ||
| Device related | 0 | 0 | 0 | 4 (1.5%) | 4 (1.5%) | 3 (1.1%) | ||
| Impaired healing (including pruritus or erythema) | Device and/or procedure related | 2 (1.6%) | 0 | 0 | 2 (0.7%) | 0 | 0 | |
| Procedure related | 2 (1.6%) | 0 | 0 | 1 (0.4%) | 0 | 0 | ||
| Device related | 0 | 0 | 0 | 1 (0.4%) | 0 | 0 | ||
| Insertion site infection | Device and/or procedure related | 2 (1.6%) | 2 (1.6%) | 1 (0.8%) | 0 | 0 | 0 | |
| Procedure related | 2 (1.6%) | 2 (1.6%) | 1 (0.8%) | 0 | 0 | 0 | ||
| Device related | 1 (0.8%) | 1 (0.8%) | 0 | 0 | 0 | 0 | ||
| Insertion site pain / irritation | Device and/or procedure related | 6 (4.9%) | 4 (3.3%) | 0 | 1 (0.4%) | 0 | 0 | |
| Procedure related | 2 (1.6%) | 1 (0.8%) | 0 | 0 | 0 | 0 | ||
| Device related | 5 (4.1%) | 4 (3.3%) | 0 | 1 (0.4%) | 0 | 0 | ||
| Oversensing | Device and/or procedure related | 0 | 0 | 0 | 1 (0.4%) | 1 (0.4%) | 0 | |
| Procedure related | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Device related | 0 | 0 | 0 | 1 (0.4%) | 1 (0.4%) | 0 | ||
| Shock/ dyspnea | Device and/or procedure related | 0 | 0 | 0 | 1 (0.4%) | 1 (0.4%) | 1 (0.4%) | |
| Procedure related | 0 | 0 | 0 | 1 (0.4%) | 1 (0.4%) | 1 (0.4%) | ||
| Device related | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Discomfort | Device and/or procedure related | 1 (0.8%) | 1 (0.8%) | 1 (0.8%) | 0 | 0 | 0 | |
| Procedure related | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Device related | 1 (0.8%) | 1 (0.8%) | 1 (0.8%) | 0 | 0 | 0 | ||
Overall, the CEC classified three (2%) procedure related AEs and six (5%) device related AEs as serious for the Reveal XT device. Serious procedure related AEs included two insertion site infections that were resolved by device explant and one case of pain around the device at the insertion site. Device related AEs classified as serious by the CEC included four cases of pain around the device at the insertion site, one case of discomfort and one case of insertion site infection. All of these events resulted in device explant.
Subjects receiving the Reveal LINQ device had a lower rate of procedure or system related adverse events, with 1.8% (n=5) experiencing a procedure related AE and 2.6% (n=7) experiencing a device related AE. Procedure related AEs included device dislocation/site erosion (n=3), impaired healing (n=1), and shock/dyspnea (n=1). The patient who experienced shock/dyspnea had a reaction to antibiotic administration prior to device insertion (see below). Device related AEs observed with Reveal LINQ included device dislocation/site erosion (n=4), impaired healing (n=1), insertion site pain/irritation (n=1) and oversensing (n=1).
For Reveal LINQ, the CEC classified four (1%) procedure related AEs as serious. These included three situations in which the device migrated out of the incision pocket. In addition, one subject had an allergic reaction to antibiotic administration prior to device insertion. This subject was stabilized and transferred to the ICU, and did not receive a LINQ device. The CEC also classified five (2%) device related AEs as serious. These included four situations in which the device migrated out of the incision pocket. Additionally, one patient experienced poor device sensing. This was resolved by repositioning the device, which required an invasive procedure.
There was occasional disagreement between the CEC and investigators in terms of severity of AEs. CEC and investigator classifications are presented in Table 3. Investigators considered fewer events to be serious compared with the CEC.
Discussion
Considering the frequency of AF and the severity of its clinical sequelae, there is a clear need for rigorous AF screening programs, especially for patients at higher risk. Screening strategies should balance the cost and invasiveness of a diagnostic device with a population’s level of risk for AF. In a lower risk population where the consequences of missing even short AF episodes are lower, a simpler, less expensive test with a lower detection rate may be sufficient as an initial step. Such tests include blood pressure monitors with AF detection and hand-held ECG devices (including smart phones). While the benefit of these systems includes low cost and non-invasive nature, they are limited by their ability to provide only a snapshot into the overall frequency and burden of AF in an individual patient.
Wearable ECG systems and ICMs have been developed in order to facilitate continuous AF screening in higher risk populations. While wearable ECG devices have the advantage of being non-invasive, they are limited in the duration (1-4 weeks) of continuous monitoring afforded, and are susceptible to subject compliance challenges. Subcutaneous ICMs improve compliance by inhibiting removal/nonuse and provide continuous monitoring for up to three years.[21] However, the minimally invasive nature of these devices warrants their use in a higher risk patient population. AF detection by pacemakers and ICDs have provided proof of concept of AF detection with an implanted device, but they have done so only in patients with concomitant electrical disorders, which may or may not be reflective of event rates and significance in a broader population of patients.
Accordingly, a number of ongoing trials employ ICMs to screen for AF in patients without a previous history of this arrhythmia, but who are at higher risk for AF and subsequent stroke if AF is present. These include REVEAL AF, PREDATE AF (NCT01851902), ASSERT II (NCT01694394), and LOOP (NCT02036450). The REVEAL AF study is specifically assessing the value of ICM monitoring in a patient population suspected to be at high risk for AF based on a modified CHADS2 score. The baseline data from this study demonstrate that a) the study enrolled its target population and will be able to evaluate the efficacy of the envisioned screening strategy, b) there are patients at high risk for AF willing to undergo ICM monitoring, and c) ICMs are safe for use in this population, and are becoming safer with advancements in technology.
Subject demographics
To be clinically impactful, it is important that diagnosis be linked to clear recommendations for a meaningful change in therapy (e.g. initiation of OAC therapy for stroke prevention). In the current REVEAL AF study, a modified CHADS2 scoring system was used to guide patient enrollment. The CHADS2 and CHA2DS2-VASc scoring systems provide a framework for identifying patients that would benefit from OAC to decrease their risk of stroke due to AF. Of note, the risk factors for developing AF overlap heavily with the risk factors for stroke in the CHADS2 and CHA2DS2-VASc systems. Consequently, a high CHADS2 or CHA2DS2-VASc score might not only identify patients at high risk of stroke due to AF, but also those that are at high risk of developing AF. There have been a number of recent analyses that support this supposition.[22]-[27]
In REVEAL AF, subjects were required to have a CHADS2 score ≥ 3 or a CHADS2 score = 2 with at least one of the following additional AF risk factors documented: coronary artery disease, renal impairment, sleep apnea, or chronic obstructive pulmonary disease. Here we report that REVEAL AF was successful in enrolling patients in the originally defined target population. Each pre-defined CHADS2 subgroup (2, 3 and ≥4) was well represented (>100 subjects), and a reasonable prevalence of AF risk factors used to guide enrollment for subjects with a CHADS2 score of two was attained. Specifically, coronary artery disease, renal impairment, sleep apnea, and chronic obstructive pulmonary disease were all present in over 15% of the population. Of these risk factors, coronary artery disease was the most common, occurring in 59% of subjects. By achieving our target population, the REVEAL AF study will be able to determine the efficacy of the originally designed screening strategy. As such, when the follow up (minimum of 18 months to a maximum of 30 months) for the primary endpoint (AF detection) is complete in early 2017, a greater understanding will be attained of how predictive the risk factors specified above are for AF development. Importantly, these demographic characteristics reflect those reported for ischemic stroke populations in large epidemiological studies,[15], [28], [29] which further highlights the clinical importance of screening the REVEAL AF patient population for primary stroke prevention. In REVEAL AF, also planned are assessments of possible genetic and circulating biomarkers as predictors of AF and or associated adverse consequences. Moreover, if the frequency of AF detection is substantial (for example higher than 10-20%), there will be significant implications for screening of large segments of our older population as well as the need for larger phase 3 trials.
Patient acceptance
In addition to efficacy, patient acceptance is a key aspect of a successful screening paradigm. In the REVEAL AF study, we were able to meet our enrollment goal of 450 subjects. This indicates that there are patients believed to be at high risk for AF who are willing to participate in an ICM screening strategy. The higher prevalence of subjects enrolled with symptoms compared to those without may reflect greater patient acceptance in this cohort. The study did have enrollment challenges, evident by a 2.5 year enrollment period for 450 subjects across 58 centers. While this may be due in part to inclusion/exclusion requirements of the study, the 2.5 year timeframe likely reflects some subject concern around engaging in an ICM screening strategy for AF detection. Additionally, 6% of consented subjects did not receive an ICM due to subject withdrawal. Patient acceptance will likely evolve with future clinical evidence and technological advances that increase device safety and/or reduce patient burden. This is supported by the observation that over twice as many subjects were inserted with the newer miniaturized Reveal LINQ ICM than the predicate XT device in this study, despite the LINQ ICM only being commercially available during the second half of the enrollment period.
Safety of ICM Monitoring in Patients at High Risk for AF
In order for adoption of ICM’s as a method to detect AF in a high-risk population, the overall safety of the device and procedure must be demonstrated. While the safety of predicate ICM devices have been characterized in different patient populations,[30]-[36] prior investigations have not specifically evaluated safety in individuals suspected to be at high risk for AF outside the context of post-stroke cardiac monitoring. Moreover, limited data exist on the safety of the new miniaturized Reveal LINQ ICM, as this device has only been commercially available since 2014.
In REVEAL AF, we observed a low rate of serious procedure and/or device related adverse events (3%), which primarily included a low reported incidence of device dislocation/site erosion, insertion site infection, and insertion site pain/irritation. The miniaturized Reveal LINQ ICM had an improved safety profile compared with the predicate Reveal XT device. Specifically, in patients who received the Reveal XT, serious procedure related adverse events occurred in 2.5% of patients, and serious device related adverse events occurred in 4.9%. In the Reveal LINQ subgroup, procedure-related serious AEs occurred in 1.5% of patients, and serious device related AEs occurred in 1.8%. Importantly, these rates are in line which those recently reported for the Reveal LINQ device (≤2%) in both clinical trial[37], [38] and real world settings.[37] Overall, these data add to the mounting evidence supporting the safety of ICM insertion in broad patient populations, and highlights that ICM safety is improving with advancements in technology. Importantly, if a clinically meaningful yield of AF detection is observed in REVEAL AF and other ongoing trials, these safety data will support clinical adoption of ICM-based screening programs.
Conclusion
AF remains an important cause for morbidity and mortality, particularly by increasing the risk of ischemic stroke. In higher risk populations, where therapy may be significantly altered, more intensive screening tools that provide a longer monitoring period may be employed. Data from REVEAL AF demonstrate a portion of patients believed to be at high risk for AF are willing to undergo ICM screening, and ICM devices are safe for use in this population, and becoming safer with evolving technology. If successful, REVEAL AF and other ongoing studies may have a substantial impact on informing clinical care for patients at high risk for AF.
Conflict Of Interests
None.
Disclosures
Drs. Reiffel, Gersh, Kowey, Wachter, Halperin and Verma are consultants for, and receive modest honoraria from Medtronic. Rachelle Kaplon and Erika Pouliot are employed by and stock owners of, Medtronic.
References
- 1.Chugh S S, Blackshear J L, Shen W K, Hammill S C, Gersh B J. Epidemiology and natural history of atrial fibrillation: clinical implications. J. Am. Coll. Cardiol. 2001 Feb;37 (2):371–8. doi: 10.1016/s0735-1097(00)01107-4. [DOI] [PubMed] [Google Scholar]
- 2.Chugh Sumeet S, Havmoeller Rasmus, Narayanan Kumar, Singh David, Rienstra Michiel, Benjamin Emelia J, Gillum Richard F, Kim Young-Hoon, McAnulty John H, Zheng Zhi-Jie, Forouzanfar Mohammad H, Naghavi Mohsen, Mensah George A, Ezzati Majid, Murray Christopher J L. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014 Feb 25;129 (8):837–47. doi: 10.1161/CIRCULATIONAHA.113.005119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Go A S, Hylek E M, Phillips K A, Chang Y, Henault L E, Selby J V, Singer D E. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA. 2001 May 09;285 (18):2370–5. doi: 10.1001/jama.285.18.2370. [DOI] [PubMed] [Google Scholar]
- 4.Miyasaka Yoko, Barnes Marion E, Gersh Bernard J, Cha Stephen S, Bailey Kent R, Abhayaratna Walter P, Seward James B, Tsang Teresa S M. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006 Jul 11;114 (2):119–25. doi: 10.1161/CIRCULATIONAHA.105.595140. [DOI] [PubMed] [Google Scholar]
- 5.Naccarelli Gerald V, Varker Helen, Lin Jay, Schulman Kathy L. Increasing prevalence of atrial fibrillation and flutter in the United States. Am. J. Cardiol. 2009 Dec 01;104 (11):1534–9. doi: 10.1016/j.amjcard.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 6.Quirino Gianluca, Giammaria Massimo, Corbucci Giorgio, Pistelli Paolo, Turri Elena, Mazza Antonio, Perucca Antonello, Checchinato Catia, Dalmasso Maurizio, Barold S Serge. Diagnosis of paroxysmal atrial fibrillation in patients with implanted pacemakers: relationship to symptoms and other variables. Pacing Clin Electrophysiol. 2009 Jan;32 (1):91–8. doi: 10.1111/j.1540-8159.2009.02181.x. [DOI] [PubMed] [Google Scholar]
- 7.Strickberger S Adam, Ip John, Saksena Sanjeev, Curry Ken, Bahnson Tristram D, Ziegler Paul D. Relationship between atrial tachyarrhythmias and symptoms. Heart Rhythm. 2005 Feb;2 (2):125–31. doi: 10.1016/j.hrthm.2004.10.042. [DOI] [PubMed] [Google Scholar]
- 8.Savelieva I, Camm A J. Clinical relevance of silent atrial fibrillation: prevalence, prognosis, quality of life, and management. J Interv Card Electrophysiol. 2000 Jun;4 (2):369–82. doi: 10.1023/a:1009823001707. [DOI] [PubMed] [Google Scholar]
- 9.Capucci Alessandro, Santini Massimo, Padeletti Luigi, Gulizia Michele, Botto GianLuca, Boriani Giuseppe, Ricci Renato, Favale Stefano, Zolezzi Francesco, Di Belardino Natale, Molon Giulio, Drago Fabrizio, Villani Giovanni Q, Mazzini Elena, Vimercati Marco, Grammatico Andrea. Monitored atrial fibrillation duration predicts arterial embolic events in patients suffering from bradycardia and atrial fibrillation implanted with antitachycardia pacemakers. J. Am. Coll. Cardiol. 2005 Nov 15;46 (10):1913–20. doi: 10.1016/j.jacc.2005.07.044. [DOI] [PubMed] [Google Scholar]
- 10.Glotzer Taya V, Daoud Emile G, Wyse D George, Singer Daniel E, Ezekowitz Michael D, Hilker Christopher, Miller Clayton, Qi Dongfeng, Ziegler Paul D. The relationship between daily atrial tachyarrhythmia burden from implantable device diagnostics and stroke risk: the TRENDS study. Circ Arrhythm Electrophysiol. 2009 Oct;2 (5):474–80. doi: 10.1161/CIRCEP.109.849638. [DOI] [PubMed] [Google Scholar]
- 11.Glotzer Taya V, Hellkamp Anne S, Zimmerman John, Sweeney Michael O, Yee Raymond, Marinchak Roger, Cook James, Paraschos Alexander, Love John, Radoslovich Glauco, Lee Kerry L, Lamas Gervasio A. Atrial high rate episodes detected by pacemaker diagnostics predict death and stroke: report of the Atrial Diagnostics Ancillary Study of the MOde Selection Trial (MOST). Circulation. 2003 Apr 01;107 (12):1614–9. doi: 10.1161/01.CIR.0000057981.70380.45. [DOI] [PubMed] [Google Scholar]
- 12.Healey Jeff S, Connolly Stuart J, Gold Michael R, Israel Carsten W, Van Gelder Isabelle C, Capucci Alessandro, Lau C P, Fain Eric, Yang Sean, Bailleul Christophe, Morillo Carlos A, Carlson Mark, Themeles Ellison, Kaufman Elizabeth S, Hohnloser Stefan H. Subclinical atrial fibrillation and the risk of stroke. N. Engl. J. Med. 2012 Jan 12;366 (2):120–9. doi: 10.1056/NEJMoa1105575. [DOI] [PubMed] [Google Scholar]
- 13.Shanmugam Nesan, Boerdlein Annegret, Proff Jochen, Ong Peter, Valencia Oswaldo, Maier Sebastian K G, Bauer Wolfgang R, Paul Vince, Sack Stefan. Detection of atrial high-rate events by continuous home monitoring: clinical significance in the heart failure-cardiac resynchronization therapy population. Europace. 2012 Feb;14 (2):230–7. doi: 10.1093/europace/eur293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ben Freedman S, Lowres Nicole. Asymptomatic Atrial Fibrillation: The Case for Screening to Prevent Stroke. JAMA. 2015 Nov 10;314 (18):1911–2. doi: 10.1001/jama.2015.9846. [DOI] [PubMed] [Google Scholar]
- 15.Friberg Leif, Rosenqvist Mårten, Lindgren Arne, Terént Andreas, Norrving Bo, Asplund Kjell. High prevalence of atrial fibrillation among patients with ischemic stroke. Stroke. 2014 Sep;45 (9):2599–605. doi: 10.1161/STROKEAHA.114.006070. [DOI] [PubMed] [Google Scholar]
- 16.Albers Gregory W, Bernstein Richard A, Brachmann Johannes, Camm John, Easton J Donald, Fromm Peter, Goto Shinya, Granger Christopher B, Hohnloser Stefan H, Hylek Elaine, Jaffer Amir K, Krieger Derk W, Passman Rod, Pines Jesse M, Reed Shelby D, Rothwell Peter M, Kowey Peter R. Heart Rhythm Monitoring Strategies for Cryptogenic Stroke: 2015 Diagnostics and Monitoring Stroke Focus Group Report. J Am Heart Assoc. 2016 Mar 15;5 (3) doi: 10.1161/JAHA.115.002944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Desteghe Lien, Raymaekers Zina, Lutin Mark, Vijgen Johan, Dilling-Boer Dagmara, Koopman Pieter, Schurmans Joris, Vanduynhoven Philippe, Dendale Paul, Heidbuchel Hein. Performance of handheld electrocardiogram devices to detect atrial fibrillation in a cardiology and geriatric ward setting. Europace. 2017 Jan;19 (1):29–39. doi: 10.1093/europace/euw025. [DOI] [PubMed] [Google Scholar]
- 18.Tieleman R G, Plantinga Y, Rinkes D, Bartels G L, Posma J L, Cator R, Hofman C, Houben R P. Validation and clinical use of a novel diagnostic device for screening of atrial fibrillation. Europace. 2014 Sep;16 (9):1291–5. doi: 10.1093/europace/euu057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Uittenbogaart Steven B, Verbiest-van Gurp Nicole, Erkens Petra M G, Lucassen Wim A M, Knottnerus J André, Winkens Bjorn, van Weert Henk C P M, Stoffers Henri E J H. Detecting and Diagnosing Atrial Fibrillation (D2AF): study protocol for a cluster randomised controlled trial. Trials. 2015 Oct 23;16 () doi: 10.1186/s13063-015-1006-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reiffel James, Verma Atul, Halperin Jonathan L, Gersh Bernard, Tombul Selcuk, Carrithers John, Sherfesee Lou, Kowey Peter. Rationale and design of REVEAL AF: a prospective study of previously undiagnosed atrial fibrillation as documented by an insertable cardiac monitor in high-risk patients. Am. Heart J. 2014 Jan;167 (1):22–7. doi: 10.1016/j.ahj.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 21.Tomson Todd T, Passman Rod. The Reveal LINQ insertable cardiac monitor. Expert Rev Med Devices. 2015 Jan;12 (1):7–18. doi: 10.1586/17434440.2014.953059. [DOI] [PubMed] [Google Scholar]
- 22.Welles Christine C, Whooley Mary A, Na Beeya, Ganz Peter, Schiller Nelson B, Turakhia Mintu P. The CHADS2 score predicts ischemic stroke in the absence of atrial fibrillation among subjects with coronary heart disease: data from the Heart and Soul Study. Am. Heart J. 2011 Sep;162 (3):555–61. doi: 10.1016/j.ahj.2011.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tu Hans T H, Campbell Bruce C V, Meretoja Atte, Churilov Leonid, Lees Kennedy R, Donnan Geoffrey A, Davis Stephen M. Pre-stroke CHADS2 and CHA2DS2-VASc scores are useful in stratifying three-month outcomes in patients with and without atrial fibrillation. Cerebrovasc. Dis. 2013;36 (4):273–80. doi: 10.1159/000353670. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell L Brent, Southern Danielle A, Galbraith Diane, Ghali William A, Knudtson Merril, Wilton Stephen B. Prediction of stroke or TIA in patients without atrial fibrillation using CHADS2 and CHA2DS2-VASc scores. Heart. 2014 Oct;100 (19):1524–30. doi: 10.1136/heartjnl-2013-305303. [DOI] [PubMed] [Google Scholar]
- 25.Ntaios George, Lip Gregory Y H, Makaritsis Konstantinos, Papavasileiou Vasileios, Vemmou Anastasia, Koroboki Eleni, Savvari Paraskevi, Manios Efstathios, Milionis Haralampos, Vemmos Konstantinos. CHADS₂, CHA₂S₂DS₂-VASc, and long-term stroke outcome in patients without atrial fibrillation. Neurology. 2013 Mar 12;80 (11):1009–17. doi: 10.1212/WNL.0b013e318287281b. [DOI] [PubMed] [Google Scholar]
- 26.Saliba Walid, Gronich Naomi, Barnett-Griness Ofra, Rennert Gad. Usefulness of CHADS2 and CHA2DS2-VASc Scores in the Prediction of New-Onset Atrial Fibrillation: A Population-Based Study. Am. J. Med. 2016 Aug;129 (8):843–9. doi: 10.1016/j.amjmed.2016.02.029. [DOI] [PubMed] [Google Scholar]
- 27.Chamberlain Alanna M, Agarwal Sunil K, Folsom Aaron R, Soliman Elsayed Z, Chambless Lloyd E, Crow Richard, Ambrose Marietta, Alonso Alvaro. A clinical risk score for atrial fibrillation in a biracial prospective cohort (from the Atherosclerosis Risk in Communities [ARIC] study). Am. J. Cardiol. 2011 Jan;107 (1):85–91. doi: 10.1016/j.amjcard.2010.08.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.PN Renjen, MA Beg, K Ahmad. Epidemiological study of incidence and risk factors of Ischemic stroke subtypes according to Trial of ORG 10172 in acute stroke treatment criteria: A 3 years, hospital-based study. International Journal of Medicine and Public Health. 2015;1:50–54. [Google Scholar]
- 29.Kolominsky-Rabas P L, Weber M, Gefeller O, Neundoerfer B, Heuschmann P U. Epidemiology of ischemic stroke subtypes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based study. Stroke. 2001 Dec 01;32 (12):2735–40. doi: 10.1161/hs1201.100209. [DOI] [PubMed] [Google Scholar]
- 30.Christensen L M, Krieger D W, Højberg S, Pedersen O D, Karlsen F M, Jacobsen M D, Worck R, Nielsen H, Aegidius K, Jeppesen L L, Rosenbaum S, Marstrand J, Christensen H. Paroxysmal atrial fibrillation occurs often in cryptogenic ischaemic stroke. Final results from the SURPRISE study. Eur. J. Neurol. 2014 Jun;21 (6):884–9. doi: 10.1111/ene.12400. [DOI] [PubMed] [Google Scholar]
- 31.Kapa Suraj, Epstein Andrew E, Callans David J, Garcia Fermin C, Lin David, Bala Rupa, Riley Michael P, Hutchinson Mathew D, Gerstenfeld Edward P, Tzou Wendy, Marchlinski Francis E, Frankel David S, Cooper Joshua M, Supple Gregory, Deo Rajat, Verdino Ralph J, Patel Vickas V, Dixit Sanjay. Assessing arrhythmia burden after catheter ablation of atrial fibrillation using an implantable loop recorder: the ABACUS study. J. Cardiovasc. Electrophysiol. 2013 Aug;24 (8):875–81. doi: 10.1111/jce.12141. [DOI] [PubMed] [Google Scholar]
- 32.Krahn A D, Klein G J, Yee R, Takle-Newhouse T, Norris C. Use of an extended monitoring strategy in patients with problematic syncope. Reveal Investigators. Circulation. 1999 Jan 26;99 (3):406–10. doi: 10.1161/01.cir.99.3.406. [DOI] [PubMed] [Google Scholar]
- 33.Pachulski Roman, Cockrell James, Solomon Hemant, Yang Fang, Rogers John. Implant evaluation of an insertable cardiac monitor outside the electrophysiology lab setting. PLoS ONE. 2013;8 (8) doi: 10.1371/journal.pone.0071544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rojo-Martinez Esther, Sandín-Fuentes María, Calleja-Sanz Ana I, Cortijo-García Elisa, García-Bermejo Pablo, Ruiz-Piñero Marina, Rubio-Sanz Jerónimo, Arenillas-Lara Juan F. [High performance of an implantable Holter monitor in the detection of concealed paroxysmal atrial fibrillation in patients with cryptogenic stroke and a suspected embolic mechanism]. Rev Neurol. 2013 Sep 16;57 (6):251–7. [PubMed] [Google Scholar]
- 35.Sanna Tommaso, Diener Hans-Christoph, Passman Rod S, Di Lazzaro Vincenzo, Bernstein Richard A, Morillo Carlos A, Rymer Marilyn Mollman, Thijs Vincent, Rogers Tyson, Beckers Frank, Lindborg Kate, Brachmann Johannes. Cryptogenic stroke and underlying atrial fibrillation. N. Engl. J. Med. 2014 Jun 26;370 (26):2478–86. doi: 10.1056/NEJMoa1313600. [DOI] [PubMed] [Google Scholar]
- 36.Tondo C, Tritto M, Landolina M, DE Girolamo Pg, Bencardino G, Moltrasio M, Dello Russo A, Della Bella P, Bertaglia E, Proclemer A, DE Sanctis V, Mantica M. Rhythm-symptom correlation in patients on continuous monitoring after catheter ablation of atrial fibrillation. J. Cardiovasc. Electrophysiol. 2014 Feb;25 (2):154–60. doi: 10.1111/jce.12292. [DOI] [PubMed] [Google Scholar]
- 37.Mittal Suneet, Sanders Prashanthan, Pokushalov Evgeny, Dekker Lukas, Kereiakes Dean, Schloss Edward J, Pouliot Erika, Franco Noreli, Zhong Yan, DI Bacco Marco, Pürerfellner Helmut. Safety Profile of a Miniaturized Insertable Cardiac Monitor: Results from Two Prospective Trials. Pacing Clin Electrophysiol. 2015 Dec;38 (12):1464–9. doi: 10.1111/pace.12752. [DOI] [PubMed] [Google Scholar]
- 38.Rogers John D, Sanders Prashanthan, Piorkowski Christopher, Sohail M Rizwan, Anand Rishi, Crossen Karl, Khairallah Farhat S, Kaplon Rachelle E, Stromberg Kurt, Kowal Robert C. In-office insertion of a miniaturized insertable cardiac monitor: Results from the Reveal LINQ In-Office 2 randomized study. Heart Rhythm. 2017 Feb;14 (2):218–224. doi: 10.1016/j.hrthm.2016.11.001. [DOI] [PubMed] [Google Scholar]


