Abstract
Racial disparities in health tend to be more pronounced at the upper ends of the socioeconomic (SES) spectrum. Despite having access to above average social and economic resources, nonpoor African Americans and Latinos report significantly worse health compared to nonpoor Whites. We combine data from the parents and children of the 1979 National Longitudinal Survey of Youth (NLSY79) to address two specific research aims. First, we generate longitudinal SES trajectories over a 33-year period to estimate the extent to which socioeconomic mobility is associated with exposure to discrimination (acute and chronic) across different racial/ethnic groups (nonHispanic Whites, nonHispanic Blacks, and Hispanics). Then we determine if the disparate relationship between SES and self-rated health across these groups can be accounted for by more frequent exposure to unfair treatment. For Whites, moderate income gains over time result in significantly less exposure to both acute and chronic discrimination. Upwardly mobile African Americans and Hispanics, however, were significantly more likely to experience acute and chronic discrimination, respectively, than their socioeconomically stable counterparts. We also find that differential exposure to unfair treatment explains a substantial proportion of the Black/White, but not the Hispanic/White, gap in self-rated health among this nationally representative sample of upwardly mobile young adults. The current study adds to the debate that the shape of the SES/health gradient differs, in important ways, across race and provides empirical support for the diminishing health returns hypothesis for racial/ethnic minorities.
Keywords: racial disparities, discrimination, lifecourse SES, self-rated health, African Americans, Hispanics
Introduction
In the United States, racial disparities in health are well established across a diverse set of outcomes (Williams 2012). These inequalities are primarily the result of excessive rates of chronic disease among racial minorities (Geronimus et al. 2011; Harper et al. 2012; Murray et al. 2006). NonHispanic Blacks face rates of hypertension, diabetes, and obesity that are 25%, 49%, and 59% higher, respectively, than those found among nonHispanic Whites, while Hispanics experience rates of diabetes and obesity that are 25% and 20% higher, respectively than their nonHispanic White counterparts (NCHS 2016). Despite the amount of attention that has been paid to documenting these stark racial disparities in morbidity and mortality, many questions remain regarding the social and economic conditions that give rise to such unequal chances of an outcome that, quite literally, determines who lives and who dies.
One of the strongest predictors of health is socioeconomic status (SES) – so much so, that it is considered to be a fundamental cause of health disparities (Phelan et al. 2010). The association between SES and health has been shown to be positive, linear, and monotonic, such that with each additional increase in socioeconomic standing, we expect an individual's health to improve in a step-wise fashion (Adler and Rehkopf 2008). This SES/health gradient has been noted across a wide range of settings as well as historical time periods (Adler and Stewart 2010; Braveman et al. 2010; Elo 2009). However, among some racial/ethnic groups the association between SES and health is not as straightforward as was once thought. For example, Black/White disparities in health are often more pronounced among high as opposed to low SES subpopulations and upward mobility does not seem to bring similar improvements in health for African Americans compared to Whites (Colen et al. 2006; Colen 2011; Farmer and Ferraro 2005; Williams and Sternthal 2010). For Hispanics, particularly those born outside the U.S. (Williams et al. 2010), the association between SES and health is so tenuous that investigators have coined the term Hispanic health paradox to describe this particularly unexpected finding and spent much of the previous three decades trying to determine if the Hispanic health paradox is “real” or primarily the result of multiple data artifacts (Markides and Eschbach 2005; Ruiz et al. 2013; Smith and Bradshaw 2006; Vega et al. 2013).
Clearly more research is needed to understand, on a deeper level, why some racial/ethnic groups stand poised to benefit, with respect to their health, from gains in their socioeconomic standing while others do not experience similar positive effects. One potential explanation for this finding is that for racial minorities, ascending the socioeconomic hierarchy does not guarantee fewer encounters with discrimination, or unfair treatment (For the purposes of this paper, the terms discrimination and unfair treatment will be used interchangeably. Unless otherwise specified, they refer to forms of discrimination, or unfair treatment, that are unattributed to any specific social characteristic such as race, ethnicity, gender, age, etc.). In fact, some studies have revealed the opposite – that individuals with higher levels of SES tend to report more instances of interpersonal discrimination (Everson-Rose et al. 2015) or that the association between unfair treatment and health is significantly more pronounced among higher vs. lower SES groups (Fuller-Rowell et al. 2012; Hudson et al. 2012; Hudson et al. 2013).
The proposed study seeks to examine if and how exposure to discrimination can help to explain why nonpoor African Americans and Latinos tend to report worse health compared to nonpoor Whites, despite typically having access to above average socioeconomic resources via educational attainment, occupational prestige, or family income. We use data from two cohorts of the National Longitudinal Survey of Youth 1979 (NLSY79) to address two specific research aims. First, we estimate the extent to which longitudinal SES trajectories are associated with exposure to discrimination across different racial/ethnic groups (nonHispanic Whites, nonHispanic Blacks, and Hispanics). Then, we determine if the disparate relationship between SES and self-rated health across these racial/ethnic groups can be accounted for by more frequent exposure to racial discrimination.
SES and Health
The relationship between SES and health is one of the most consistent and persistent findings within the health disparities literature (Adler and Rehkopf 2008). It has been shown across a wide range of outcomes, SES indicators, subpopulations, and time periods that as SES increases, physical wellbeing also improves (Braveman et al. 2010; Elo 2009; Phelan et al. 2010). Although there remains some debate regarding whether the mechanisms through which SES influences health are largely a result of differential access to material resources or primarily psychosocial in nature (Demakakos et al. 2008; Link et al. 2013; Link et al. 2008; Lynch et al. 2000; Marmot 2004; Matthews et al. 2010; Seeman et al. 2014), there is overwhelming evidence to suggest that SES is a fundamental cause of population health disparities (Clouston et al. 2016; Phelan et al. 2010).
And yet, despite the seemingly ubiquitous nature of this association, there is a growing body of evidence to suggest that the association between SES and health depends on race. Some studies note the existence of diminishing returns to SES among African Americans (Colen et al. 2006; Geronimus et al. 2006; Farmer and Ferraro 2005; Hudson et al. 2012; Hudson et al. 2013; Kahn and Fazio 2005). Not only does it appear that the impact of SES on general indicators of physical wellbeing, such as self-rated health and functional impairment, might be muted for African Americans compared to Whites (Kahn and Fazio 2005; Farmer and Ferraro 2005), newer research suggests that these differences might occur on a deeper physiological or cellular level. For example, Geronimus et al. (2006; 2015) demonstrate that allostatic load scores and telomere length are similar for working-age poor and nonpoor Blacks but significantly different for their White counterparts. Diminishing health returns to SES for African Americans is apparent when fluctuations in socioeconomic resources are taken into account across generations as well as within a single generation. Colen et al. (2006) report significant reduction in the odds of low birthweight following increases in family income over time only for White but not Black NLSY79 respondents who spent their childhoods in or near poverty.
Among Hispanics, the relationship between SES and health is less apparent – so much so, that researchers frequently employ the term, Hispanic health paradox, to refer to the unexpected population health patterning displayed by this racial/ethnic group, which reports relatively low levels of SES but tends to experience better than average health outcomes (Markides and Eschbach 2005; Ruiz et al. 2013; Smith and Bradshaw 2006; Vega et al. 2009). This pattern is more consistently noted when examining rates of death (Hummer et al. 2007) as opposed to specific disease outcomes, health behaviors, or biological risk profiles (Abraido-Lanza et al. 2005; Bates et al. 2008; Crimmins et al. 2007) as well as among certain Hispanic subgroups, particularly Mexican-Americans (Markides and Eschbach 2005) and recent immigrants to the U.S. (Williams et al. 2010). It is thought that better adherence to healthier diets, lower rates of smoking, and higher levels of social support could be protecting the health of Latinos in the U.S. despite their low SES, at least during the first decade of time spent in the U.S. before acculturation becomes more complete (Abraido-Lanza et al. 2005). Although much debate remains regarding the underlying factors that are driving this quizzical finding, with some investigators arguing that the HHP is not even real but simply the result of data artifact (Palloni and Arias 2004; Smith and Bradshaw 2006), there remains ample evidence to suggest that the association between SES and health is less pronounced among Hispanics than Whites.
Discrimination and Health
Exposure to discrimination has been posited as an explanation, at least in part, for the stark and consistent racial disparities in health. Despite the fact that for most individuals experiences of unfair treatment remain a relatively rare event with most respondents reporting that they “never,” “rarely,” or “sometimes” encounter interpersonal discrimination, a rapidly growing literature links experiences of unfair treatment to subsequent morbidity and even mortality (Lewis et al. 2015; Pascoe and Richman 2009). There is some evidence that the association between unfair treatment and wellbeing might be more pronounced for mental as opposed to physical health outcomes (Lewis et al. 2015; Paradies et al. 2015; Schmitt et al. 2014; Williams and Mohammed 2009) although a recent meta-analysis concluded that this difference is not statistically significant (Pascoe and Richman 2009).
Discrimination has been assessed using a number of different indicators, some of which capture unattributed unfair treatment while others identify unfair treatment that the respondent specifically ascribes to a sociodemographic characteristic such as race, ethnicity, sex, etc. (Bastos et al. 2010). There is not consensus in the literature concerning which approach provides a more valid measure of interpersonal discrimination. Some investigators argue that in order to more accurately estimate the effects, health and otherwise, of racial discrimination, respondents should identify the underlying reason for reported unfair treatment (Krieger 2012), while other researchers note that it is often difficult and possibly disadvantageous for a respondent to be required to attribute discrimination to a particular sociodemographic characteristic (Lewis et al. 2015; Williams et al. 2012). This might be especially problematic for individuals who occupy more than one disadvantaged social status, such as women of color, for whom separating out the underlying source of unfair treatment might be all but impossible. Of particular importance for the current study, there appears to be little difference in the impacts of racial, as opposed to other forms, of discrimination on health (Williams and Mohammed 2009) suggesting that similarly physiological reactions underlie the human response to unfair treatment, regardless of the underlying cause. Moreover, general (unattributed) as opposed to specific (attributed) measures of discrimination tend to be just as or more strongly associated with a variety of negative health outcomes including coronary artery calcification (Lewis et al. 2006), hypertension (Roberts et al. 2008), and cigarette smoking (Chae et al. 2008).
The two most widely used discrimination measures, particularly among studies that explore its impact on health, are Williams' major events discrimination scale (MEDS) and everyday discrimination scale (EDS) as well as Krieger's experiences of discrimination scale. The MEDS and EDS, which are used in the current study, invite respondents to report instances of unfair treatment in a two-step process, the first of which inquires about the frequency of discriminatory occurrences while the second asks about the sociodemographic attribute likely to be driving this interpersonal interaction. On the other hand, Krieger's experiences of discrimination scale requires that respondents report instances of discrimination that have happened specifically as a result of their race; thus, study participants must simultaneously recall an event while attributing the cause of this event to an underlying characteristic (Krieger 2012; Lewis et al. 2015). Although the psychometric properties of both measures are convincing (Bastos et al. 2010), there are concerns that a one-step approach leads to artificially inflated reports of discrimination primarily due to interviewer effects and response bias (Lewis et al. 2015; Williams and Mohammed 2009) while a two-step approach captures unfair treatment that is not specifically attributed to one's race (Krieger 2012).
The biological pathway through which discrimination is thought to negatively influence physical wellbeing is the human stress response. The stress process model has long served as a powerful theoretical framework through which to gain a deeper understanding of population health patterns and inequalities (Pearlin 1989; Turner 2009). At its core, this theory emphasizes the interaction between exposures to psychosocial stressors and access to coping resources in the production of health and illness (Thoits 2010). Thus, holding the number or efficacy of coping resources constant, we expect individuals who encounter more frequent or more challenging stressors to have worse health outcomes than individuals facing fewer or less challenging stressors (Schwartz and Meyer 2010). In more recent years, the stress model has been expanded to place a greater emphasis on macro-level social conditions, such as the role of social statuses (race, sex, etc.) and neighborhood conditions, that are likely to unequally pattern exposure to psychosocial stressors across population subgroups (Aneshensel 2009).
It is thought that by interpreting unfair treatment as a psychosocial threat, an individual's stress response system will be activated - most notably, via his/her HPA axis- thus releasing a potent cocktail of hormones and biochemical (e.g. cortisol and epinephrine) that, in turn, trigger a cascade of physiological changes (e.g. increased heart rate, blood pressure, and respiration) specifically produced to deal with the perceived threat (Brondolo et al. 2008; Cohen et al. 2006; Cunningham et al. 2012; Friedman et al. 2009; Fuller-Rowell et al. 2012;). As the concept of allostatic load predicts, the worst health outcomes will be seen among those who have this stress response repeatedly activated over time or who cannot turn off this physiological cascade once it is initiated (Geronimus et al. 2006; McEwen 1998; Seeman et al. 2001). Thus, with respect to the production of racial disparities in health, the chronicity rather than the severity of exposure to discrimination is often considered to be stronger predictor of worse outcomes, either across subgroups or over time. This is supported by a growing body of empirical evidence which shows that everyday discrimination is more consistently associated with higher rates of morbidity and mortality than acute instances of unfair treatment (Paradies 2006; Williams and Mohammed 2009). This finding echoes similar results from the broader stress literature that reveal chronic, as opposed to acute, stressors tend to more strongly predictive of suboptimal health outcomes (Cohen, Kessler, and Gordon 1997).
Although the link between discrimination and health is most apparent for cardiovascular outcomes, particularly those that have been studied within a laboratory setting or using continuous, real-time monitoring (Brondolo et al. 2009), they remain somewhat mixed and require further investigation and replication before definitive conclusions can be drawn (Chae et al. 2010; Lewis et al. 2006, 2009). Greater exposure to unfair treatment has been demonstrated to result in significantly higher daytime blood pressure readings as well as worse nocturnal blood pressure recovery patterns, more rapid heart rates, and elevated cortisol secretions (Smart Richman et al. 2010; Tomfohr et al. 2010; Zieders et al. 2014). These findings are particularly notable since this type of physiological reactivity is a key pathway through which stressful environmental stimuli is thought to impact subsequent health outcomes and, in particular, has been implicated in the emergence of hypertension and other negative cardiovascular outcomes (D'Agostino et al. 2008; Din-Dzietham et al. 2004). A key question for researchers in this area is the extent to which results from experimental studies can be generalized to more diverse populations.
The empirical evidence linking discrimination to health generated from community-based or observational research is less straightforward but, nonetheless, provides preliminary support for the notion that exposure to unfair treatment is likely to negatively impact physical wellbeing. Several studies reveal that the frequency of discrimination is predictive of worse health across a wide range of physical health outcomes including all-cause mortality (Barnes et al. 2008), chronic health conditions (Gee et al. 2007, Ryan et al. 2006), self-reported health (Borrell et al. 2006; Harris et al. 2006; Schulz et al. 2006), asthma incidence (Coogan et al. 2014), coronary artery calcification (Lewis et al. 2006), obesity (Cozier et al. 2014; Hunte 2011; Hunte and Williams 2009), low birthweight and preterm birth (Lauderdale 2006; Mustillo et al. 2004), breast cancer incidence (Taylor et al. 2007), and uterine fibroids (Wise et al. 2007). Exposure to interpersonal discrimination has also been implicated in important subclinical physiological processes that are thought to be a marker of accelerated aging such as higher allostatic load scores (Brody et al. 2014; Ong et al. 2017) and shorter telomeres (Chae et al. 2014). However, these findings are not consistent across all outcomes or subpopulations. For example, the association between discrimination and health appears more pronounced for mental as opposed to physical outcomes (Williams and Mohammed 2009) and somewhat quizzically is sometimes stronger among Whites than nonWhites (Hunte and Williams 2009).
The extent to which exposure to unfair treatment is key mechanism through racial disparities in health are produced remains unclear (Williams and Mohammed 2009). A few notable studies provide preliminary evidence that perceived discrimination is, at the very least, one reason why the Black/White gap in health outcomes remains relatively unchanged despite an ever-increasing average life expectancy, widespread medical advancements, and more inclusive health care coverage. Mustillo and colleagues (2004) demonstrate that perceived racial discrimination explains as much or more of the Black/White disparity in poor birth outcomes (low birthweight and preterm birth) as maternal education, income, cigarette smoking, alcohol consumption, and depressive symptomatology taken together. These findings are further supported by research that found women of Arab descent living in California were significantly more likely to give birth to a low birthweight or preterm baby in the six-month period following September 11th than in the six-month period before this date (Lauderdale 2006). This result is particularly noteworthy since (1) Arab and Arab American women typically have very healthy pregnancies and consistently low rates of LBW and PTB and (2) similar increases were not noted among any other racial/ethnic group during the same time period. Furthermore, Tomfohr et al. (2010) report that encounters of everyday discrimination fully accounted for differences in nocturnal blood pressure dipping between African Americans and Whites. There is also mounting evidence that differential exposure to unfair treatment across race is driving important racial/ethnic inequalities in both sleep quantity and quality (Tomfohr et al. 2012).
The extant literature concerning discrimination and health suffers from some notable shortcomings that the current study was specifically designed to address. First, many existing studies rely on small or convenience samples that are not nationally representative. While this might help to understand how the health of a specific group is impacted by unfair treatment, these findings should not be used to generalize to the U.S. population as a whole. Second, few studies are specifically designed to determine the extent to which exposure to discrimination can help to explain the stark racial disparities in health that currently characterize the American social landscape. Third, the way in which unfair treatment is captured differs substantially across studies, with some investigators relying on indicators with unproven psychometric properties. Fourth, much of what we know about the association between discrimination and health has been derived from cross-sectional research, thus our ability to discern the true causal ordering that undergirds this statistical relationship remains methodologically hampered.
Most notably, few extant studies examine how encounters with discrimination differ across both race and SES, and an even smaller number then link these unequal exposures to subsequent health outcomes. Among a sample of African Americans, Hudson and colleagues (2012) demonstrate that more frequent encounters with unfair treatment predict an increased risk of depression for high SES men but not their low SES counterparts. In a similar study that examined differences across race among a nationally representative cohort of young adults, Hudson et al. (2013) report that for Whites but not Blacks, the association between discrimination and self-rated health is more pronounced at higher levels of SES. There is also preliminary evidence to suggest that more frequent encounters with unfair treatment predict less healthy diurnal cortisol rhythms but only among low as opposed to high SES African Americans (Fuller-Rowell 2012). Clearly, much more work is needed to begin to understand, on a deeper level, how race and SES interact to produce health disparities and the extent to which these complex trends can be explained by differential exposure to discrimination.
To this end, the current study combines prospective cohort data from two NLSY surveys, the 1979 cohort (NLSY79) and the young adult cohort (NLSY79-YA) to answer the following research questions:
As SES increases over time, are individuals exposed to significantly less acute and chronic discrimination?
Does this association vary across race, such that upwardly mobile Whites are significantly less likely than upwardly mobile nonWhites to encounter instances of unfair treatment?
Can this differential exposure to discrimination account, at least in part, for racial disparities in health among individuals experiencing upward mobility?
Data and Methods
Description of the Data
The National Longitudinal Study of Youth is a prospective cohort study that began in 1979 by enrolling a nationally representative sample of young men and women between the ages of 14 and 21. This data collection effort was originally undertaken to investigate the labor market experiences and outcomes of young adults as they completed high school and began college, entered the work force, and established their own households. Racial minorities, low-income individuals, and members of the armed forces were oversampled. In addition to gathering data on educational attainment and employment, the original 1979 cohort also provided a wealth of information on childbearing and childrearing. To this end, all children born to female members of the 1979 cohort were followed up over time and form the basis of the NLSY79-Young Adult survey. Prospective data was collected on these children biennially from 1986 until 2012. As of 2012, the ages of the young adult cohort ranged from 14 to 41 years and African American and Hispanic respondents accounted for 28% and 19%, respectively, of the total sample.
For the purposes of this study, overall health was assessed using a measure of self-rated health. NLSY79 young adults were asked to describe their present health as excellent, very good, good, fair, or poor. Our decision to use this particular health indicator to capture overall health status was due to three important considerations. First, this type of simple, straightforward survey question has been repeatedly shown to be a powerful predictor of subsequent morbidity and mortality, even more so than physician examination (DeSalvo et al. 2006; Idler and Benyamini 1997; Jylha 2009). Second, our study sample is relatively young and most have yet to develop chronic illnesses or serious health conditions, which are easier to capture with more specific indicators. Finally, self-rated health is a commonly used measure of overall wellbeing particular within the health disparities literature; thus, our findings will be easily and directly comparable to a wide swathe of the existing research.
Questions concerning discrimination were incorporated into the 2012 round of the NLSY79-YA survey and form the analytical basis of the current study. Experiences of acute discrimination were captured using the Major Experiences of Discrimination Scale (Williams et al. 1997; Kessler et al. 1999), while exposure to chronic discrimination was assessed by means of the Everyday Discrimination Scale (Williams et al. 1997). These multi-item measures were originally developed by Williams and colleagues (Williams et al. 1997) and possess several methodological advantages (Bastos et al. 2010; Krieger 2005), including their strong psychometric properties, comprehensive and respondent driven approach to capturing experiences with unfair treatment, their clarity and the ease with which it is understood by participants, and their comparability across studies.
Due to existing time constraints and considerable demands already placed on survey respondents, shortened versions of both discrimination scales were incorporated into existing data collection efforts. The Major Experiences of Discrimination Scale (MEDS) was limited to 5 questions that asked respondents if they ever encountered unfair treatment in the following settings: educational attainment, occupational advancement (hiring, promotion, and dismissal), and police harassment. Thus, this indicator is a lifetime rating of discrimination exposure. Only NLSY79-YA who were 21 years of age or older in 2012 were asked to complete the MEDS, since individual questions inquired about discrimination in settings that affected young people once they transitioned from adolescence to adulthood. The version of the Everyday Discrimination Scale (EDS) that was used in the NLSY79-YA survey contained 9 questions about chronic, as opposed to acute, instances of unfair treatment. For example, participants were asked, “In your day to day life, how often have any of the following happened to you? You have been treated with less courtesy than other people.” Response categories ranged from (1) very often; (2) fairly often; (3) not too often; (4) hardly ever; to (5) never and were reverse coded, so that higher scores indicated more exposure to chronic discrimination. Similar to the wording used in the MEDS, this indicator does not require that the respondent recall a specific time period during which the unfair treatment occurred. For both discrimination measures, respondents had the opportunity to attribute reported unfair treatment to specific sociodemographic categories including race or ethnicity; however, small cell sizes across income trajectories prevented us from incorporating these data into the current study. A full description of both the MEDS and the EDS is presented in Appendix A.
In the NLSY79-YA, race/ethnicity is based upon how the original NLSY79 female participant (ie. mother) was identified. We divided young adults into three distinct racial/ethnic groups: nonHispanic Whites, nonHispanic Blacks, and Hispanics. We excluded any respondent who did not fall within one of these three racial categories due to small cell sizes. Since the NLSY79-YA sample is comprised of children born to original NLSY79 female respondents, nativity status did not vary across Hispanic young adults.
For the current study, SES is captured using a time-varying indicator of household income that combines detailed information from both the NLSY79 and NLSY79-YA surveys for the years between 1979 and 2012. If, in a given year, the respondent was less than 21 years of age, did not work full-time, or did not live independently, we used parents' income to generate this measure. If all three inclusion criteria were met, we relied on the young adult's household income of the NLSY79 to calculate these SES trajectories. Latent growth curve analysis (LGCA) was employed to identify which NLSY79-YA respondents experienced downward mobility, upward mobility, or socioeconomic stability based on these income trajectories. We used household income to capture SES fluctuations over time because it (1) comprehensively captures the amount of economic resources available to the NLSY79 respondent, regardless of if he/she (or her mother) is currently in the labor force; (2) is consistently measured and can easily be adjusted for temporal changes by accounting for inflation whereas educational attainment or occupational prestige across generations cannot; (3) provides an indicator with enough variation both across respondents and over time to allow us to create stable SES trajectories; and (4) is correlated with parental educational attainment and occupational prestige – two indicators that do not as consistently vary over time and for which we have substantial amounts of missing data, particularly among fathers and stay at home mothers.
LGCA identifies clusters of individuals who follow similar pathways along some variable over a specific unit of time (e.g. age or year) (Jones and Nagin 2007 Jones and Nagin 2013). The method is a specialized application of finite mixture modeling using maximum likelihood to estimate the trajectory of each group, the proportion of the entire sample assigned to each group, and the probability of group membership for all observations (Jones and Nagin 2007; Nagin 2005). Unlike growth curve models, which assume that the entire population shares similar risks and follows similar trajectories over time, group-based models allow clusters of individuals to adhere to distinct time-varying trajectories (Jones and Nagin 2007; Nagin 2005; Nagin and Odgers 2010). Although the groups are approximations and do not reflect actual entities, they provide a useful classification scheme for describing developmental pathways over time (Nagin 2005; Nagin and Odgers 2010; Nagin and Tremblay 2005; Petts 2009).
In the current study, we assign individuals into groups based on fluctuations in household income between 1979 and 2012. We used the following model to predict income as a polynomial function of age:
where y is total family income for individuals in group j and β1, β2, and β3 are population parameters that determine the shape of the trajectory. Because each trajectory can theoretically have its own unique shape, we estimate a unique set of parameters for each group (Nagin 2005). After examining BIC/AIC values and posterior probabilities, completing a visual inspection of graphs, and in keeping with prior research on income trajectories in the United States (e.g. Cerdá, Johnson-Lawrence, and Galea 2011), we finished with a 5-group LGCA model. The largest group (40%) experienced moderate upwardly mobility, while two other groups – the socioeconomically stable (30%) and the slow upwardly mobile (22%) – also accounted for a sizeable proportion of the sample. Only 3% of NLSY79 young adults could be classified as downwardly mobile. Finally, a small group (5%) had household incomes that were relatively high and grew steadily over time.
We control for a number of potential confounders in multivariate regression models, all of which were assessed in 2012. These include respondent's age, sex (male vs. female), marital status (not married, married, divorced, separated, widowed; cohabiting), region of residence (Northeast; Midwest; South; West), and employment status (neither in school or working; in school; working; in school and working).
Analytic Strategy
A series of multilevel regression models were estimated to determine (1) whether the association between SES and acute or chronic discrimination significantly differed across the three racial/ethnic groups and (2) the extent to which differential exposure to acute or chronic discrimination could explain, at least in part, lower levels of self-rated health among upwardly mobile Blacks and Hispanics compared to upwardly mobile Whites. Ordered logit models were used to predict categorical outcomes including acute discrimination and self-rated health, while linear regression models were employed to generate findings for continuous outcomes such as chronic discrimination scores. Since we are estimating regression models for both continuous and categorical outcomes, we report slope coefficients (b) as opposed to odds ratios (OR) in Tables 2 through 4 to maintain consistency.
Table 2. Results from Multilevel Regression Models Predicting Acute and Chronic Discrimination Scores by Race and Mobility Trajectory among NLSY Young Adults.
| Acute Discrimination | Chronic Discrimination | |||||
|---|---|---|---|---|---|---|
| b | SEa | b | SEa | |||
|
|
||||||
| Race | ||||||
| NH White | Ref | Ref | ||||
| NH Black | 0.6700 | *** | 0.142 | 0.8444 | * | 0.370 |
| Hispanic | 0.1306 | 0.169 | -0.8594 | * | 0.399 | |
| Income Trajectory | ||||||
| Stable | Ref | Ref | ||||
| Downward | -0.1684 | 0.586 | -0.3052 | 1.435 | ||
| Slow Upward | 0.5744 | ** | 0.207 | 0.2923 | 0.570 | |
| Moderate Upward | -0.2669 | * | 0.133 | -1.0700 | *** | 0.291 |
| Rapid Upward | -0.4648 | + | 0.253 | -1.1761 | ** | 0.446 |
| Race*Income Interaction | ||||||
| Black*Downward | 0.5045 | 0.634 | 0.0652 | 1.616 | ||
| Black*Slow Upward | -0.4561 | + | 0.243 | 0.3410 | 0.688 | |
| Black*Mod Upward | 0.4244 | * | 0.199 | 0.9179 | + | 0.507 |
| Black*Rapid Upward | -0.0490 | 0.598 | 1.1842 | 0.835 | ||
| Hispanic*Downward | 0.3384 | 0.755 | -2.3653 | 1.839 | ||
| Hispanic*Slow Upward | -0.3423 | 0.281 | 0.1950 | 0.743 | ||
| Hispanic*Mod Upward | -0.0386 | 0.231 | 1.3033 | * | 0.515 | |
| Hispanic*Rapid Upward | -0.3664 | 0.520 | -0.3508 | 0.892 | ||
| N | 4,371 | 5,250 | ||||
Source: NLSY79-Young Adult Survey
Note: All regression models controlled for age, sex, marital status, region of residence, and employment status.
Robust standard errors were calculated using the Huber/White correction method and clustered at the level of the original NLSY79 mother.
p < 0.001;
p < 0.01;
p < 0.05;
p < 0.10
Table 4. Results from Multilevel Ordered Logit Regression Models Predicting Self Rated Health by Race and Chronic Discrimination among Upwardly Mobile NLSY Young Adults.
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| b | SEa | b | SEa | |||
|
|
||||||
| Race | ||||||
| NH White | Ref | Ref | ||||
| NH Black | -0.2543 | ** | 0.084 | -0.1354 | 0.085 | |
| Hispanic | -0.3270 | ** | 0.100 | -0.3180 | ** | 0.100 |
| Chronic Discrimination | -0.0623 | *** | 0.006 | |||
| Age | -0.0406 | *** | 0.009 | -0.0390 | *** | 0.009 |
| Female | -0.2131 | *** | 0.065 | -0.2848 | *** | 0.065 |
| Marital Status | ||||||
| Not Married | Ref | Ref | ||||
| Married | 0.2778 | ** | 0.099 | 0.1979 | * | 0.099 |
| Divorced/Sep/Widow | -0.1046 | 0.197 | -0.0893 | 0.197 | ||
| Cohabiting | -0.2421 | * | 0.096 | -0.2301 | * | 0.096 |
| Region | ||||||
| Northeast | Ref | Ref | ||||
| Midwest | -0.0327 | 0.112 | -0.0512 | 0.111 | ||
| South | 0.0638 | 0.107 | 0.0248 | 0.106 | ||
| West | -0.1119 | 0.123 | -0.1215 | 0.121 | ||
| Employment Status | ||||||
| Neither | Ref | Ref | ||||
| In School | 0.5649 | ** | 0.210 | 0.5067 | * | 0.211 |
| Working | 0.5791 | *** | 0.142 | 0.5502 | *** | 0.145 |
| In School & Working | 0.8608 | *** | 0.153 | 0.8034 | *** | 0.156 |
| N | 3,534 | 3,534 | ||||
Source: NLSY79-Young Adult Survey
Note: All regression models controlled for age, sex, marital status, region of residence, and employment status.
Robust standard errors were calculated using the Huber/White correction method and clustered at the level of the original NLSY79 mother.
p < 0.001;
p < 0.01;
p < 0.05;
p < 0.10
NLSY79-YA data have a hierarchical structure wherein multiple young adults are nested within families. Multilevel models allow us to deconstruct the variation in the dependent variable in two ways – across individuals and across families. Because it would be unrealistic to assume that error terms are uncorrelated if NLSY79 respondents were born to the same mother and grew up in the same family, our regression models estimate random intercepts—that is, the model provides an average intercept, as well as a variance parameter that summarizes individual-specific deviations from the average intercept. As such, our models parse between-individual and between-family variation in self-rated health, conditional on the variables included in the model. Given the nonindependence of error terms and the presence of heteroskedasticity, we calculated robust standard errors using the Huber/White correction method and clustered them at the highest level of aggregation - the original NLSY79 family. All analyses were based on maximum likelihood estimation and conducted using Stata/MP 14.2.
We restrict our study sample to all NLSY79 young adults who were 18 years or older in 2012 and had nonmissing values for at least one discrimination measure as well asself-rated health. Because the MEDS was only administered to NLSY79 young adults who were 21 or older, while the EDS was administered to all NLSY79-YA participants, our sample size differs across these two discrimination measures, ranging from 4,412 respondents (acute discrimination) to 5,248 (chronic discrimination). Proportions of missing data for the both the MEDS and EDS were exceedingly low, at 1.6% and 0.13%, respectively.
To handle issues of missing data on additional variables, we relied on multiple imputation techniques to generate values for all covariates included in descriptive and multivariate analyses. Evidence from the relationships of missing data with individual time varying and time invariant characteristics suggests the data are not missing completely at random (unconditional on the observed covariates) which makes typical approaches such as listwise deletion inappropriate (Allison 2001). In the imputation phase, the procedures use a diverse set of predictors to estimate five sets of plausible values for each missing value. The imputed values in the five data sets include a random component based on draws from the posterior predictive distribution of the missing data under a posited Bayesian model and, under the missing-at-random assumption - a more plausible assumption than is made by listwise deletion - provide unbiased estimates of variance (Allison 2001). Following von Hippel (2007), we impute values for all variables in a given model and then delete observations with missing data on self-rated health.
Results
Descriptive findings are presented in Table 1. Among this sample of NLSY79 young adults, 45% were nonHispanic White, 34% were nonHispanic Black, and 21% were Hispanic. This overrepresentation of nonwhite respondents allowed us to generate stable comparisons across race and SES. Regarding the classification of income trajectories we generated using LGCA, the majority of NLSY79 young adults fall into one of three categories – socioeconomically stable (30%), slow upward mobility (22%), and moderate upward mobility (40%). Only a small proportion were found to adhere to either downwardly mobile (3%) or rapid upwardly mobile (5%) trajectories. Furthermore, we found substantial racial disparities in income trajectories, with larger proportions of nonHispanic Blacks and Hispanics experiencing downward mobility or slow upward mobility and smaller proportions experiencing moderate or rapid upward mobility compared to nonHispanic Whites.
Table 1. Descriptive Statistics for NLSY Young Adults by Race of Respondent.
| NH Whites | NH Blacks | Hispanics | ||
|---|---|---|---|---|
|
|
||||
| Race | ||||
| NH White | 45.24 | |||
| NH Black | 33.54 | |||
| Hispanic | 21.22 | |||
| Income Trajectory | ||||
| Stable | 29.70 | 25.73 | 33.16 | 32.68 |
| Downward | 2.99 | 1.14 | 5.79*** | 2.51+ |
| Slow Upward | 21.98 | 8.25 | 36.68*** | 28.01*** |
| Moderate Upward | 40.32 | 56.42 | 23.06*** | 33.3*** |
| Rapid Upward | 5.01 | 8.46 | 1.31*** | 3.5*** |
| Acute Discrimination | ||||
| None | 61.52 | 69.97 | 50.39 | 62.39 |
| 1-2 Times | 23.56 | 19.58 | 28.58*** | 23.52** |
| 3+ Times | 14.92 | 10.45 | 21.02*** | 14.09** |
| Chronic Discrimination | 17.49 (6.22) | 16.88 (5.72) | 18.61*** (6.82) | 17.01 (5.98) |
| Age | 25.93 (4.74) | 25.14 (4.44) | 26.82*** (5.01) | 26.21*** (4.65) |
| Sex | ||||
| Male | 48.48 | 48.93 | 46.34 | 50.90 |
| Female | 51.52 | 51.07 | 53.66+ | 49.10 |
| Marital Status | ||||
| Not Married | 60.76 | 57.31 | 67.86 | 56.91 |
| Married | 18.69 | 23.49 | 11.93*** | 19.12* |
| Divorced/Sep/Widow | 4.40 | 3.37 | 5.79* | 4.40 |
| Cohabiting | 16.15 | 15.83 | 14.42** | 19.57* |
| Region | ||||
| Northeast | 13.85 | 15.71 | 11.75 | 13.20 |
| Midwest | 24.38 | 34.48 | 20.14* | 9.61*** |
| South | 41.70 | 32.17 | 61.22*** | 31.15 |
| West | 20.08 | 17.64 | 6.93*** | 46.05*** |
| Employment Status | ||||
| Neither | 7.98 | 5.31 | 11.02 | 8.89 |
| In School | 4.51 | 3.58 | 5.39 | 5.12 |
| Working | 62.48 | 62.27 | 61.16*** | 64.99*** |
| In School & Working | 25.03 | 28.84 | 22.43*** | 21.01*** |
| N | 5,250 | 2,375 | 1,761 | 1,114 |
Source : NLSY79-Young Adult Survey
p < 0.001;
p < 0.01;
p < 0.05;
p < 0.10
A sizable fraction of the NLSY79-YA sample report exposure to both acute and chronic discrimination. Overall, 38% of respondents experienced at least one instance of acute discrimination, with almost 15% report frequent occurrences (3 or more) of acute discrimination. The mean chronic discrimination score for the entire sample was 17.50 with a standard deviation of 6.2. Table 1 reveals sizeable racial differences in exposure to unfair treatment among this young adult population. Most notably, nonHispanic Blacks experienced acute discrimination more frequently that nonHispanic Whites, with 29% and 21% of Blacks reporting 1-2 and 3+ instances of acute discrimination, respectively, compared to only 20% and 10% of Whites. Similarly, mean chronic discrimination scores were significantly higher among nonHispanic Blacks (18.61) than nonHispanic Whites (16.88). For Hispanics, racial disparities in exposure to unfair treatment follow a slightly different pattern. Hispanics are more likely than nonHispanic Whites to experience moderate (24% vs. 20%) and frequent (14% vs. 10%) instances of acute discrimination but just as likely as their White counterparts to experience chronic discrimination (17.01 vs. 16.88). Table 1 also reveals significant disparities across race with respect to age and sex of the respondent, marital status, region of the country, and employment status, with more pronounced differences noted between Blacks and Whites than Hispanics and Whites.
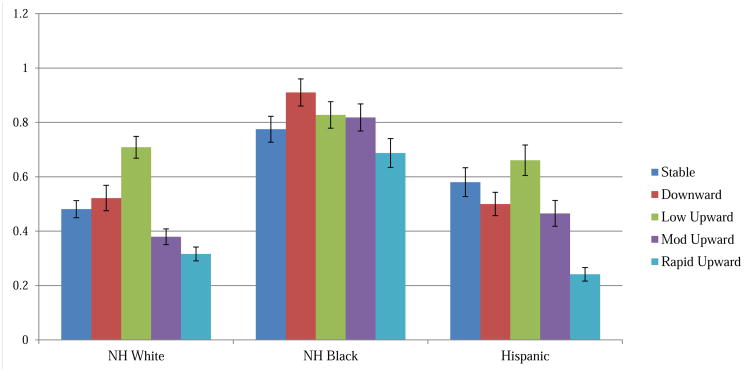
We present the distribution of unfair treatment by race and mobility status in Figures 1 and 2 and find greater racial disparities in the patterning of exposure for acute as opposed to chronic discrimination. As Figure 1 makes evident, nonHispanic Whites and Hispanics who are upwardly mobile (moderate and rapid) tend to experience less acute discrimination than those who are socioeconomically stable or downwardly mobile. For example, among Whites, mean acute discrimination scores for moderate and rapid upwardly mobile respondents are 0.38 and 0.32, respectively, compared to 0.48 for socioeconomically stable respondents. Blacks follow a different pattern with respect to exposure to acute unfair treatment. Upward socioeconomic mobility does not appear to shield nonHispanic Black NLSY79 young adults from encountering instances of acute discrimination. In fact, Black moderately upwardly mobile respondents report more experiences (0.82) of acute discrimination than their Black socioeconomically stable counterparts (0.78).
Figure 1. Mean Acute Discrimination Scores by Race & Income Trajectory.
Note: Acute discrimination scores can range from a minimum of 0 to a maximum of 5.
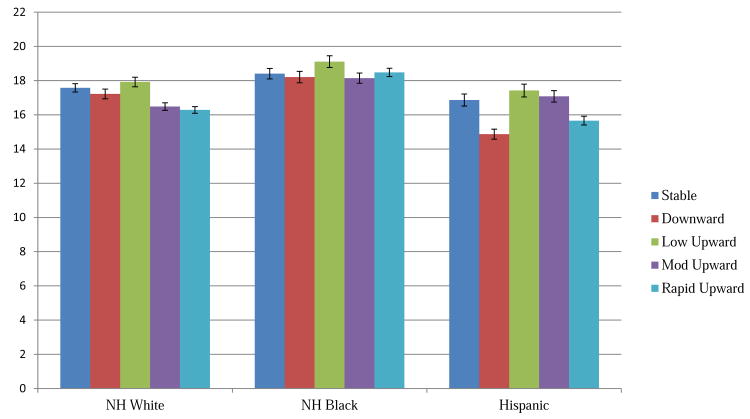
Figure 2. Mean Chronic Discrimination Scores by Race & Income Trajectory.
Note: Chronic discrimination scores can range from a minimum of 0 to a maximum of 45.
Figure 2 reveals similar trends regarding the distribution of chronic discrimination across race and income trajectory, albeit less pronounced than those presented in Figure 1 for acute discrimination. With the exception of downwardly mobile young adults, exposure to chronic discrimination tends to decrease as nonHispanic White and Hispanic respondents become more upwardly mobile. For nonHispanic Whites, mean chronic discrimination scores decreased from 17.6 in the socioeconomically stable category to 16.5 and 16.3 in the moderate and rapid upwardly mobile categories. However, the trend of falling levels of chronic unfair treatment with rising levels of mobility is not evident among Black NLSY79-YA respondents. On average, socioeconomically stable Black young adults report chronic discrimination scores of 18.4, while their counterparts in the slow, moderate, and rapid upwardly mobile groups report chronic discrimination scores of 19.1, 18.1, and 18.5.
In Table 2, we present findings from multilevel regression analyses designed to test whether the racial differences we notice in the association between income trajectories and unfair treatment vary significantly across race. All multivariate models controlled for age, sex, marital status, region of residence, and employment status. Regression results reveal that compared to nonHispanic Whites, nonHispanic Blacks face 95% higher odds [1-e(0.6700) * 100] of experiencing acute discrimination. Regarding the association between socioeconomic mobility and exposure to acute discrimination, respondents in the moderate and rapid upwardly mobile categories face 24% [1-e(-0.2669) * 100] and 37% [1-e(-0.4648) * 100] lower odds, respectively, of experiencing acute discrimination compared to those in the socioeconomically stable category although regression coefficient for the rapid upwardly mobile fails to reach statistical significance (p < 0.05). Results for chronic discrimination echo those found for acute discrimination with two notable exceptions. First, although Black NLSY79-YA respondents report significantly higher chronic discrimination scores (b = 0.8444) than Whites, Hispanic NLSY79-YA respondents report significantly lower chronic discrimination scores (b = -0.8594) than members of the referent group. Second, young adults in both the moderate and rapid upward mobility categories revealed significantly lower chronic discrimination scores (b = -1.07 and -1.18, respectively) compared to young adults in the socioeconomically stable group.
Of particular interest for this study, we find evidence of significant interactions between race and income on exposure to unfair treatment among respondents who experienced both slow and moderate upward mobility, with more pronounced racial differences noted for African Americans than Hispanics. For nonHispanic Whites, those whose income trajectories moderately rose over time faced 24% [1-e(-0.2669) * 100] lower odds of encountering acute discrimination. However, for nonHispanic Blacks, those whose income trajectories moderately rose over time faced 17% [1-e(-0.2669+0.4244) * 100] higher odds of encountering acute discrimination. Similarly, within the slow upward mobility category, nonHispanic Whites had a 77% [1-e(0.5744) * 100] increase in the odds of acute discrimination while nonHispanic Blacks had a 13% [1-e(0.5744+-0.4561) * 100] increase in the odds of acute discrimination.
With respect to the association between socioeconomic mobility and chronic discrimination exposure, we only found empirical evidence of racial disparities for those experiencing moderate income gains over time. These tended to be more pronounced among Hispanics than nonHispanic Blacks. White NLSY79 young adults in the moderate upwardly mobile group reported mean chronic discrimination scores that were 1.07 lower than White NLYS young adults in the socioeconomically stable group. However, nonHispanic Black respondents whose incomes moderately increased experienced only 0.15 [-1.0700 + 0.9179] fewer instances of chronic discrimination than their nonHispanic White counterparts, while Hispanic respondents in this mobility group experienced 0.23 [-1.0700 + 1.3033] more instances of chronic discrimination.
Tables 3 and 4 reveal results from statistical analyses regressing self-rated health on acute discrimination and chronic discrimination, respectively, among upwardly mobile NLSY79 young adults. We highlight how the magnitude of the regression coefficients for race (NH Black and Hispanic) change from Model 1 to Model 2 once we control for discrimination in order to determine the extent to which differential exposure to unfair treatment is likely to restrict the health returns to upward mobility for racial minorities. Model 1 of Table 3 illustrates that upwardly mobile nonHispanic Blacks and Hispanics face 17% [1-e(-0.1850) * 100] and 29% [1-e(-0.3392) * 100], respectively, lower odds of being in good health than nonHispanic Whites, net of the effects of age, sex, marital status, region of residence, and employment status. Once we adjust for differential exposure to acute discrimination, the magnitude of the regression coefficient for Blacks decreases by 58% from -0.185 to -0.078 and fails to retain statistical significance (p < 0.05), while the coefficient for Hispanics only decreases by 6% from -0.3392 to -0.3193 and remains statistically significant (p < 0.05). These findings suggest that higher than expected exposure to acute discrimination helps, at least in part, to explain why African Americans do not tend to experience the same beneficial health returns to upward mobility that Whites typically do.
Table 3. Results from Multilevel Ordered Logit Regression Models Predicting Self Rated Health by Race and Acute Discrimination among Upwardly Mobile NLSY Young Adults.
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| b | SEa | b | SEa | |||
|
|
||||||
| Race | ||||||
| NH White | Ref | Ref | ||||
| NH Black | -0.1850 | * | 0.093 | -0.0782 | 0.095 | |
| Hispanic | -0.3392 | ** | 0.106 | -0.3193 | ** | 0.105 |
| Acute Discrimination | ||||||
| None | Ref | |||||
| 1-2 Times | -0.4322 | *** | 0.087 | |||
| 3+ Times | -0.5913 | *** | 0.125 | |||
| Age | -0.0426 | *** | 0.011 | -0.0405 | *** | 0.011 |
| Female | -0.2785 | *** | 0.071 | -0.3425 | *** | 0.071 |
| Marital Status | ||||||
| Not Married | Ref | Ref | ||||
| Married | 0.3018 | ** | 0.100 | 0.2711 | ** | 0.100 |
| Divorced/Sep/Widow | -0.0871 | 0.197 | -0.0343 | 0.196 | ||
| Cohabiting | -0.2113 | * | 0.098 | -0.1870 | + | 0.098 |
| Region | ||||||
| Northeast | Ref | Ref | ||||
| Midwest | -0.0780 | 0.126 | -0.1058 | 0.125 | ||
| South | -0.0076 | 0.121 | -0.0301 | 0.121 | ||
| West | -0.1399 | 0.135 | -0.1359 | 0.134 | ||
| Employment Status | ||||||
| Neither | Ref | Ref | ||||
| In School | 0.5626 | + | 0.310 | 0.5578 | + | 0.304 |
| Working | 0.6925 | *** | 0.150 | 0.7025 | *** | 0.151 |
| In School & Working | 0.9704 | *** | 0.167 | 0.9532 | *** | 0.167 |
| N | 2,890 | 2,890 | ||||
Source: NLSY79-Young Adult Survey
Note: All regression models controlled for age, sex, marital status, region of residence, and employment status.
Robust standard errors were calculated using the Huber/White correction method and clustered at the level of the original NLSY79 mother.
p < 0.001;
p < 0.01;
p < 0.05;
p < 0.10
Similar results concerning chronic discrimination are presented in Table 4. Among upwardly mobile young adults, nonHispanic Blacks and Hispanics experience 23% [1-e(-0.2543) * 100] and 28% [1-e(-0.3270) * 100] lower odds of being in better health than nonHispanic Whites. These estimates are slightly different than those found in Table 3 due to our reliance on a larger sample size that resulted from fewer missing values on the measure of chronic as opposed to acute discrimination. Once we account for more frequent exposure to chronic discrimination among racial minorities, the regression coefficient for nonHispanic blacks decrease by 47% from -0.2543 to -0.1354 and no longer remained statistical significance (p < 0.05), while the regression coefficient for Hispanics only decrease by 3% from -0.3270 to -0.3180. In both Tables 3 and 4, we also note that older ages, being female, and cohabiting were significantly associated with worse self-rated health, while being married as well as being employed, in school, or being employed and in school were significantly associated with worse self-rated health.
Discussion
As the analyses presented here reveal, we find evidence of striking racial/ethnic differences in exposure to unfair treatment. In contrast to other studies which reveal Whites reporting more frequent encounters of discrimination than nonWhites (Williams and Mohammed 2009), the Black and Hispanic young adults in our study demonstrate higher levels of acute and chronic discrimination. Although we cannot say with certainty what is driving these findings, it could be a result of our reliance on a younger cohort of survey participants who might be more comfortable reporting instances of unfair treatment than older cohorts, especially in an era in which subtle forms of discrimination are more common than explicit instances of unfair treatment (Bonilla-Silva 2006).
We also note key differences in the association between SES and encounters with unfair treatment across race. For Whites, moderate income gains over time resulted in significantly less exposure to both acute and chronic discrimination. African Americans, on the other hand, could not count on reaping these potentially health protective benefits from upward mobility. In fact, African Americans whose incomes moderately increased over time were significantly more likely to experience acute discrimination and just as likely to experience chronic discrimination than their socioeconomically stable counterparts. Although we did not find evidence of racial disparities in the association between socioeconomic mobility and acute discrimination for Hispanics, a similar pattern emerges when examining outcomes for chronic discrimination. For Hispanics, income gains over time actually increase the frequency of encounters of chronic discrimination. Thus, it appears that regarding exposure to unfair treatment, upward mobility serves a protective function for Whites but places African Americans and Hispanics at a greater risk.
Although this result is somewhat surprising, it is not unsubstantiated in the literature given that other investigators have found exposure to discrimination to be more frequent or the relationship between unfair treatment and health to be more pronounced among high as opposed to low SES groups (Fuller-Rowell et al. 2012; Hudson et al. 2012; Hudson et al. 2013). Hudson et al. (2012) demonstrate that the positive association between both acute and chronic discrimination and depression is more pronounced among African Americans with the highest levels of educational attainment (16+ years) and household incomes (>= $55,000). Similarly, Fuller-Rowell and colleagues (2012) find that for African Americans reports of perceived discrimination are associated with flatter (less healthy) diurnal cortisol trajectories, but this relationship appears to be significantly less pronounced among higher rather than lower SES participants. These findings lend credence to the argument that the “payoffs” typically associated with gains in SES are likely to be muted for members of racial minorities due to their continued exposure to race-based unfair treatment despite having access to more than adequate levels of socioeconomic resources.
Although the current study provides additional evidence that higher SES African Americans are more likely to report instances of discrimination, it does not shed light on why this social trend might be occurring. Researchers have posited it might be due to increased exposure to Whites in more integrated educational, occupational, or neighborhood settings (Gee 2002; Fuller-Rowell 2012), while others underscore the fact that nonpoor African Americans might be more likely to notice unfair treatment than their poor counterparts (Hudson et al. 2012), thus differences in discrimination within race but across SES is being driven more by disparate reporting than actual unequal exposure. This finding might also largely result from the frustration and discouragement higher status African Americans experience by not being able to socially and economically benefit from upward mobility to the same extent as similarly situated Whites (Colen 2011; Lewis et al. 2015). Given that we are unable to further explore the extent to which these potential explanations account for differences in the association between discrimination and health across SES using the NLSY79-YA, we look toward future research efforts to conduct more pointed analyses and provide more indepth insights into this specific issue.
Our findings also lend credence to the idea that racial disparities in health result, at least in part, from exposure to discrimination among a group of upwardly mobile young adults – a group that is typically thought of as having access to higher than average social and economic resources. We show that, even after controlling for a whole host of potential confounders (age, sex, marital status, region of residence, and employment status), the health of African Americans still lags well behind that of Whites. Once we account for the increased likelihood of encountering unfair treatment among African Americans, the Black/White gap in self-rated health is reduced to such an extent as to render it statistically insignificant.
Although the number of studies designed to explore the effects of discrimination on health have been steadily increasing in recent years, there are few research efforts that directly test whether exposure to discrimination is a driving force behind the remarkably persistent racial disparities in health that characterize American society today (Lewis et al. 2015; Williams and Mohammed 2009). Our study provides preliminary evidence to support this notion and echoes previous results linking exposure to unfair treatment to Black/White inequalities in poor birth outcomes (Lauderdale 2006; Mustillo et al. 2004), nocturnal blood pressur dipping (Tomfohr et al. 2010), and sleep patterns (Tomfohr et al. 2012).
We do not, however, find that exposure to either acute or chronic discrimination explained much, if any, of why Hispanic young adults in our sample report worse self-rated health than their White counterparts. This result is even more striking given that all of the Hispanic NLSY79 young adults were born in the U.S., with a sizeable majority to parents who, themselves, were not immigrants. Sternthal et al. (2015) note that native-born Hispanics report frequency of discrimination similar to nonHispanic Blacks, while their foreign-born counterparts report instances of unfair treatment similar to nonHispanic Whites. This is not to suggest, however, that unfair treatment does not matter for members of this racial/ethnic group or that it does not negatively impact their health. On the contrary, there is a rapidly growing body of evidence to support the idea that discrimination erodes the mental and physical health of individuals from a wide range of racial/ethnic backgrounds, including those who identify as Hispanic or Latino (Everson-Rose et al. 2015; Gee and Walsemann 2009; Gee et al. 2007; Ryan et al. 2006).
The paucity of a mediating effect of discrimination on health for Hispanics that we report could stem from a lack of cultural resonance among the questions that comprised the acute and chronic discrimination measures or could be highly dependent upon level of acculturation. There is some evidence to suggest that Hispanics understand and answer questions about self-rated health differently than other racial/ethnic groups and changes the longer they live in the U.S. (Acevedo-Garcia et al. 2010; Finch et al. 2002; Viruell-Fuentes 2011). Primarily due to data constraints, we were unable to further investigate this key difference in the association between discrimination and self-rated health across race in the current paper, but it remains an interesting avenue for future research.
Limitations
The findings from the current study should be viewed in the context of some important methodological shortcomings. First, the classification system we used as a result of LGCA to classify respondents as downwardly mobile, upwardly mobile, and socioeconomically stable does not reflect actual divisions but instead identify groups of individuals who adhere to similar income trajectories. Thus, it is unclear how generalizable our findings will be to other datasets in which respondents experience very different fluctuations in income over time. We chose this more data driven analytic approach to identifying mobility trajectories because of the many problems inherent in quantifying comparing changes in SES over time and across disparate subgroups.
Second, we relied on family income, as opposed to educational attainment or occupational prestige, to determine the socioeconomic status of NLSY79 young adults. This was done purposefully since the majority of our respondents had not moved beyond the lifecourse stage known as emerging adulthood -– a period of time characterized by entrance into or exit from college, frequent changes in employment, and transitional living situations - thus making comparisons based on educational attainment and/or occupational prestige difficult and imprecise. By 2012, more than half of the study sample was less than 25 years old, the age at which educational attainment is typically assessed. Moreover, we rely on data from 1979 to 2012 to estimate mobility trajectories. During this period of time the NLSY79 young adults were children and adolescents who were nowhere near completing their schooling. Given these data constraints, we would not be able to determine if educational attainment reflected achieved social status or was simply a reflection of the respondent's young age. This is not to suggest, however, that the effects of discrimination on health do not operate through or otherwise depend on educational attainment. Other investigators have found evidence to suggest that African Americans with higher levels of educational attainment report more instances of racial discrimination (Hunt et al. 2007; Borrell et al. 2006; Krieger et al. 2011).
Household income as an indicator of SES offered several advantages to a study, such as ours, that was designed to examine the association between socioeconomic mobility, discrimination, and health over time among a sample of young adults, many of whom have not yet completed their education or gained a solid foothold on their career paths. It is more likely to comprehensively capture the financial resources available to a respondent if he/she is not currently working full-time by focusing on an expansive rather than restrictive measure of SES that is captured at the household rather than the individual level. Moreover, there is substantial variation in family income, both over time and across respondents, that allows us to more accurately discern relatively small fluctuations in SES. We do not know the extent to which our findings are consistent across disparate indicators of socioeconomic status.
Third, our measures of acute and chronic discrimination reflect exposure to unattributed unfair treatment rather than unfair treatment that has been attributed to the respondent's race and/or ethnicity. Although we would have preferred to rely on more specific indicators that directly tied a respondent's report of discrimination to his/her racial group identity, small cell sizes across income trajectories prevented us from doing so. It should be noted, however, that using more general measures of unfair treatment allows us to capture instances of discrimination that stem from multiple group identities or for which the respondent is not sure how to accurately assess attribution. This could be particularly useful in more accurately gauging frequency of unfair treatment among women of color for whom it might be difficult to compartmentalize discriminatory experiences as primarily stemming from one's race or gender. Moreover, the existing literature regarding the health effects of unfair treatment includes examples of both types of discrimination (unattributed and attributed) indicators (Lewis et al. 2015); thus, our approach is not without precedent.
Finally, due to the cross-sectional nature of our discrimination measure and our outcome variable, self-rated health, we were unable to fully examine changes in key indicators of interest over time. Thus, the conclusions that can be drawn regarding the effect of discrimination on health and the extent to which this differs across race and SES are limited in scope and require further replication using methodological approaches that can more stringently account for unobservables. By integrating income data from both the NLSY79 young adults and their parents, however, we were able to construct longitudinal income trajectories using data that spanned up to 33 years to predict both discrimination and self-rated health in 2012. Thus, our results are not completely based on cross-sectional data. Since the NLSY79-YA survey is a prospective cohort study for which interviews are conducted biennially, it is possible that in the future we will be able to examine how exposure to discrimination, SES, and health all fluctuate over time, thus gaining a clearer understanding of the complex ways in which these social conditions shape the life chances of Americans as they move through successive lifecourse stages.
Conclusion
The association between SES and health is typically thought to be remarkably consistent, whether it is across time, place, or health outcome. However, more recent research has begun to call this seemingly evident “truth” into question. As more evidence comes to light, it appears that shape of the SES/health gradient might differ across race. The current study adds to this debate by providing additional evidence that for young African American and Hispanic Americans, gains in SES might result in more as opposed to less exposure to discrimination and these encounters with unfair treatment explain a sizeable proportion of the Black/White gap in self-rated health among upwardly mobile, young adults in the U.S.
Our findings can and should be taken to suggest that efforts to alleviate poverty, while incredibly important in their own right, will not be enough to eradicate or at least substantially lessen racial disparities in health. When it comes to designing public health interventions or public policies to reduce these inequalities, nonpoor subpopulation are often overlooked. This is not only unfortunate but results in a lost opportunity to affect change. Although absolute levels of morbidity and mortality tend to be higher among lower SES groups, the racial gaps in outcomes tend to be substantially more pronounced among higher SES groups. The results of this study lend credence to the idea that in order to reduce racial disparities in health, we need to seriously address the unfair treatment racial minorities experience – not only acute instances of discrimination but those slights that occur on a daily basis, and do so among the poorest segments of our society as well as among those who are somewhat better off.
Research Highlights.
In the U.S., racial disparities in health remain pronounced, even among nonpoor populations.
We estimate exposure to discrimination for young adults across five different SES trajectories.
Upwardly mobile nonWhites report more instances of unfair treatment than Whites.
Differences in discrimination account for sizeable proportion of Black/White gap in health.
Unequal exposure to unfair treatment does not explain much of Hispanic/White disparity.
Acknowledgments
This research was supported in part by P2C-HD058484 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development awarded to the Ohio State University Institute for Population Research. NLSY79 Young Adult data used in this research were collected under NIH grant R01HD037078 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (PI Elizabeth C. Cooksey). The NLSY79 survey is sponsored and directed by the U.S. Bureau of Labor Statistics. Both surveys are conducted by the Center for Human Resource Research at The Ohio State University with interviews conducted by the National Opinion Research Center at the University of Chicago. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Bureau of Labor Statistics.
Appendix A. Description of Major Experiences and Everyday Discrimination Scale Used in NLSY-YA Survey, 2012
| Description of Discrimination Measures | Response Categories |
|---|---|
| Major Experiences of Discrimination Scale (MEDS) | |
| In the following questions, we are interested in the way other people have treated you or your beliefs about how other people have treated you. Can you tell me if any of the following has ever happened to you: | |
|
Yes/No |
| Everyday Discrimination Scale (EDS) | |
| In your day-to-day life, how often have any of the following happened to you? | |
|
Very oftenFairly oftenNot too often Hardly EverNever |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Cynthia G Colen, Department of Sociology, Ohio State University.
David M. Ramey, Department of Sociology & Criminology, Penn State University.
Elizabeth C. Cooksey, Department of Sociology & Director, Center for Human Resource Research.
David R. Williams, Florence Sprague Norman & Laura Smart Norman Professor of Public Health, Harvard University.
References
- Abraido-Lanza AF, Chao MT, Florez KR. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Soc Sci Med. 2005;61:1243–1255. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acevedo-Garcia D, Bates LM, Osypuk TL, McArdle N. The effect of immigrant generation and duration on self-rated health among US adults 2003–2007. Soc Sci Med. 2010;71:1161–1172. doi: 10.1016/j.socscimed.2010.05.034. [DOI] [PubMed] [Google Scholar]
- Adler NE, Rehkopf DH. US disparities in health: descriptions, causes, and mechanisms. Annu Rev Publ Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- Adler NE, Stewart J. Health disparities across the lifespan: meaning, methods, and mechanisms. Ann NY Acad Sci. 2010;1186:5–23. doi: 10.1111/j.1749-6632.2009.05337.x. [DOI] [PubMed] [Google Scholar]
- Allison PD. Missing Data: Sage University Papers Series on Quantitative Applications in the Social Sciences. Sage; Thousand Oaks, CA: 2001. pp. 07–136. [Google Scholar]
- Aneshensel CS. Neighborhood as a social context of the stress process. In: Avison W, Aneshensel CS, Schieman S, Wheaton B, editors. Advances in the Conceptualization of the Stress Process. Springer; New York: 2009. pp. 35–52. [Google Scholar]
- Barnes LL, de Leon CFM, Lewis TT, Bienias JL, Wilson RS, Evans DA. Perceived discrimination and mortality in a population-based study of older adults. Am J Public Health. 2008;98:1241–1247. doi: 10.2105/AJPH.2007.114397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastos JL, Celeste RK, Faerstein E, Barros AJ. Racial discrimination and health: a systematic review of scales with a focus on their psychometric properties. Soc Sci Med. 2010;70:1091–1099. doi: 10.1016/j.socscimed.2009.12.020. [DOI] [PubMed] [Google Scholar]
- Bates LM, Acevedo-Garcia D, Alegría M, Krieger N. Immigration and generational trends in body mass index and obesity in the United States: results of the National Latino and Asian American Survey, 2002–2003. Am J Public Health. 2008:98, 70–77. doi: 10.2105/AJPH.2006.102814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonilla-Silva E. Racism without Racists: Color-blind Racism and the Persistence of Racial Inequality in the United States. Rowman and Littlefield; Maryland: 2006. [Google Scholar]
- Borrell LN, Kiefe CI, Williams DR, Diez-Roux AV, Gordon-Larsen P. Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA study. Soc Sci Med. 2006;63:1415–1427. doi: 10.1016/j.socscimed.2006.04.008. [DOI] [PubMed] [Google Scholar]
- Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health. 2010;100:S186–S196. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Lei MK, Chae DH, Yu T, Kogan SM, Beach SR. Perceived discrimination among African American adolescents and allostatic load: A longitudinal analysis with buffering effects. Child Dev. 2014;85:989–1002. doi: 10.1111/cdev.12213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brondolo E, Libby DJ, Denton EG, Thompson S, Beatty DL, Schwartz J, Sweeney M, Tobin JN, Cassells A, Pickering TG, Gerin W. Racism and ambulatory blood pressure in a community sample. Psychosom Med. 2008;70:49–56. doi: 10.1097/PSY.0b013e31815ff3bd. [DOI] [PubMed] [Google Scholar]
- Chae DH, Lincoln KD, Adler NE, Syme SL. Do experiences of racial discrimination predict cardiovascular disease among African American men? The moderating role of internalized negative racial group attitudes. Soc Sci Med. 2010;71:1182–1188. doi: 10.1016/j.socscimed.2010.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chae DH, Nuru-Jeter AM, Adler NE, Brody GH, Lin J, Blackburn EH, Epel ES. Discrimination, racial bias, and telomere length in African-American men. Am J Prev Med. 2014;46:103–111. doi: 10.1016/j.amepre.2013.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouston SA, Rubin MS, Phelan JC, Link BG. A Social History of Disease: Contextualizing the Rise and Fall of Social Inequalities in Cause-Specific Mortality. Demography. 2016;53:1631–1656. doi: 10.1007/s13524-016-0495-5. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kessler RC, Gordon LU. Measuring Stress: A Guide for Health and Social Scientists. Oxford University Press; New York: 1997. [Google Scholar]
- Cohen S, Schwartz JE, Epel E, Kirschbaum C, Sidney S, Seeman T. Socioeconomic status, race, and diurnal cortisol decline in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Psychosom Med. 2006;68:41–50. doi: 10.1097/01.psy.0000195967.51768.ea. [DOI] [PubMed] [Google Scholar]
- Colen CG. Addressing racial disparities in health using life course perspectives. DuBois Rev. 2011;8:79–94. [Google Scholar]
- Colen CG, Geronimus AT, Bound J, James SA. Maternal upward socioeconomic mobility and black-white disparities in infant birthweight. Am J Public Health. 2006;96:2032–2039. doi: 10.2105/AJPH.2005.076547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coogan PF, Yu J, O'Connor GT, Brown TA, Cozier YC, Palmer JR, Rosenberg L. Experiences of racism and the incidence of adult-onset asthma in the Black Women's Health Study. Chest. 2014;145:480–485. doi: 10.1378/chest.13-0665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cozier YC, Yu J, Coogan PF, Bethea TN, Rosenberg L, Palmer JR. Racism, segregation, and risk of obesity in the Black Women's Health Study. Am J Epidemiol. 2014;179:875–83. doi: 10.1093/aje/kwu004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Kim JK, Alley DE, Karlamangla A, Seeman T. Hispanic paradox in biological risk profiles. Am J Public Health. 2007;97:1305–1310. doi: 10.2105/AJPH.2006.091892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham TJ, Seeman TE, Kawachi I, Gortmaker SL, Jacobs DR, Kiefe CI, Berkman LF. Racial/ethnic and gender differences in the association between self-reported experiences of racial/ethnic discrimination and inflammation in the CARDIA cohort of 4 US communities. Soc Sci Med. 2012;75:922–931. doi: 10.1016/j.socscimed.2012.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, Kannel WB. General cardiovascular risk profile for use in primary care the Framingham Heart Study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- Demakakos P, Nazroo J, Breeze E, Marmot M. Socioeconomic status and health: the role of subjective social status. Soc Sci Med. 2008;67:330–340. doi: 10.1016/j.socscimed.2008.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. J Gen Intern Med. 2006;21:267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Din-Dzietham R, Nembhard WN, Collins R, Davis SK. Perceived stress following race-based discrimination at work is associated with hypertension in African–Americans. The metro Atlanta heart disease study, 1999–2001. Soc Sci Med. 2004;58:449–461. doi: 10.1016/s0277-9536(03)00211-9. [DOI] [PubMed] [Google Scholar]
- Elo IT. Social class differentials in health and mortality: Patterns and explanations in comparative perspective. Annu Rev Sociol. 2009;35:553–572. [Google Scholar]
- Everson-Rose SA, Lutsey PL, Roetker NS, Lewis TT, Kershaw KN, Alonso A, Roux AVD. Perceived Discrimination and Incident Cardiovascular Events The Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2015;182:225–234. doi: 10.1093/aje/kwv035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60:191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- Finch BK, Hummer RA, Reindl M, Vega WA. Validity of self-rated health among Latino (a) s. Am J Epidemiol. 2002;155:755–759. doi: 10.1093/aje/155.8.755. [DOI] [PubMed] [Google Scholar]
- Friedman EM, Williams DR, Singer BH, Ryff CD. Chronic discrimination predicts higher circulating levels of E-selectin in a national sample: the MIDUS study. Brain Behav Immun. 2009;23:684–692. doi: 10.1016/j.bbi.2009.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller-Rowell TE, Doan SN, Eccles JS. Differential effects of perceived discrimination on the diurnal cortisol rhythm of African Americans and Whites. Psychoneuroendocrino. 2012;37:107–118. doi: 10.1016/j.psyneuen.2011.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health. 2002;92:615–623. doi: 10.2105/ajph.92.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC, Spencer MS, Chen J, Takeuchi D. A nationwide study of discrimination and chronic health conditions among Asian Americans. Am J Public Health. 2007;97:1275–1282. doi: 10.2105/AJPH.2006.091827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee G, Walsemann K. Does health predict the reporting of racial discrimination or do reports of discrimination predict health? Findings from the National Longitudinal Study of Youth. Soc Sci Med. 2009;68:1676–1684. doi: 10.1016/j.socscimed.2009.02.002. [DOI] [PubMed] [Google Scholar]
- Geronimus AT, Bound J, Colen CG. Excess black mortality in the United States and in selected black and white high-poverty areas, 1980-2000. Am J Public Health. 2011:101, 720–729. doi: 10.2105/AJPH.2010.195537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. Weathering and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Pearson JA, Linnenbringer E, Schulz AJ, Reyes AG, Epel ES, Lin J, Blackburn EH. Race-ethnicity, poverty, urban stressors, and telomere length in a Detroit community-based sample. J Health Soc Behav. 2015;56:199–224. doi: 10.1177/0022146515582100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper S, Rushani D, Kaufman JS. Trends in the black-white life expectancy gap, 2003-2008. J Amer Med Assoc. 2012;307:2257–2259. doi: 10.1001/jama.2012.5059. [DOI] [PubMed] [Google Scholar]
- Harris R, Tobias M, Jeffreys M, Waldegrave K, Karlsen S, Nazroo J. Racism and health: the relationship between experience of racial discrimination and health in New Zealand. Soc Sci Med. 2006;63:1428–1441. doi: 10.1016/j.socscimed.2006.04.009. [DOI] [PubMed] [Google Scholar]
- Hudson DL, Bullard KM, Neighbors HW, Geronimus AT, Yang J, Jackson JS. Are benefits conferred with greater socioeconomic position undermined by racial discrimination among African American men? J Mens Health. 2012;9:127–136. doi: 10.1016/j.jomh.2012.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson DL, Puterman E, Bibbins-Domingo K, Matthews KA, Adler NE. Race, life course socioeconomic position, racial discrimination, depressive symptoms and self-rated health. Soc Sci Med. 2013;97:7–14. doi: 10.1016/j.socscimed.2013.07.031. [DOI] [PubMed] [Google Scholar]
- Hummer RA, Powers DA, Pullum SG, Gossman GL, Frisbie WP. Paradox found (again): infant mortality among the Mexican-origin population in the United States. Demography. 2007;44:441–457. doi: 10.1353/dem.2007.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt MO, Wise LA, Jipguep MC, Cozier YC, Rosenberg L. Neighborhood racial composition and perceptions of racial discrimination: evidence from the Black Women's Health Study. Soc Psychol Quart. 2007;70:272–289. [Google Scholar]
- Hunte HE. Association between perceived interpersonal everyday discrimination and waist circumference over a 9-year period in the Midlife Development in the United States cohort study. Am J Epidemiol. 2011;173:1232–1239. doi: 10.1093/aje/kwq463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunte HE, Williams DR. The association between perceived discrimination and obesity in a population-based multiracial and multiethnic adult sample. Am J Public Health. 2009;99:1285–1292. doi: 10.2105/AJPH.2007.128090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- Jones BL, Nagin DS. Advances in Group-Based Trajectory Modeling and an SAS Procedure for Estimating Them. Sociol Method Res. 2007;35:542–571. [Google Scholar]
- Jones BL, Nagin DS. A Stata Plugin for Estimating Group-Based Models. [accessed May 6, 2014];Working Paper. 2012 http://ssrc.indiana.edu/seminars/wimdocs/2013-03-29_nagin_trajectory_stata-plugin-info.pdf.
- Jones Bobby L, Nagin DS. A Note on a Stata Plugin for Estimating Group-Based Models. Sociol Method Res. 2013;42:608–613. [Google Scholar]
- Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. 2009;69:307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Kahn JR, Fazio EM. Economic status over the life course and racial disparities in health. J Gerontol B-Psychol. 2005;60:S76–S84. doi: 10.1093/geronb/60.special_issue_2.s76. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40:208–230. [PubMed] [Google Scholar]
- Krieger N. Methods for the scientific study of discrimination and health: an ecosocial approach. Am J Public Health. 2012;102:936–944. doi: 10.2105/AJPH.2011.300544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Kosheleva A, Waterman PD, Chen JT, Koenen K. Racial discrimination, psychological distress, and self-rated health among US-born and foreign-born Black Americans. Am J Public Health. 2011;101:1704–1713. doi: 10.2105/AJPH.2011.300168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61:1576–1596. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- Lauderdale DS. Birth outcomes for Arabic-named women in California before and after September 11. Demography. 2006;43:185–201. doi: 10.1353/dem.2006.0008. [DOI] [PubMed] [Google Scholar]
- Lewis TT, Barnes LL, Bienias JL, Lackland DT, Evans DA, De Leon CFM. Perceived discrimination and blood pressure in older African American and white adults. J Gerontol A Biol Sci Med Sci. 2009;64A:1002–1008. doi: 10.1093/gerona/glp062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Cogburn CD, Williams DR. Self-reported experiences of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Annu Rev Clin Psycho. 2015;11:407–440. doi: 10.1146/annurev-clinpsy-032814-112728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Everson-Rose SA, Powell LH, Matthews KA, Brown C, Karavolos K, Sutton-Tyrrell K, Jacobs E, Wesley D. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: the SWAN Heart Study. Psychosom Med. 2006;68:362–368. doi: 10.1097/01.psy.0000221360.94700.16. [DOI] [PubMed] [Google Scholar]
- Link BG, Carpiano RM, Weden MM. Can honorific awards give us clues about the connection between socioeconomic status and mortality? Am Sociol Rev. 2013;78:192–212. [Google Scholar]
- Link BG, Phelan JC, Miech R, Westin EL. The resources that matter: fundamental social causes of health disparities and the challenge of intelligence. J Health Soc Behav. 2008;49:72–91. doi: 10.1177/002214650804900106. [DOI] [PubMed] [Google Scholar]
- Lynch JW, Smith GD, Kaplan GA, House JS. Income inequality and mortality: importance to health of individual income, psychosocial environment, or material conditions. Brit Med J. 2000;320:1200–1204. doi: 10.1136/bmj.320.7243.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides KS, Eschbach K. Aging, migration, and mortality: current status of research on the Hispanic paradox. J Gerontol B-Psychol. 2005;60:S68–S75. doi: 10.1093/geronb/60.special_issue_2.s68. [DOI] [PubMed] [Google Scholar]
- Marmot M. The Status Syndrome: How Your Social Standing Affects Your Health and Life Expectancy. Bloomsbury; London: 2004. [Google Scholar]
- Matthews KA, Gallo LC, Taylor SE. Are psychosocial factors mediators of socioeconomic status and health connections? Ann NY Acad Sci. 2010;1186:146–173. doi: 10.1111/j.1749-6632.2009.05332.x. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators. New Engl J Med. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- Murray CJ, Kulkarni SC, Michaud C, Tomijima N, Bulzacchelli MT, Iandiorio TJ, Ezzati M. Eight Americas: investigating mortality disparities across races, counties, and race-counties in the United States. Plos Med. 2006;3:1513–1524. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustillo S, Krieger N, Gunderson EP, Sidney S, McCreath H, Kiefe CI. Self-reported experiences of racial discrimination and Black-White differences in preterm and low-birthweight deliveries: the CARDIA Study. Am J Public Health. 2004;94:2125–2131. doi: 10.2105/ajph.94.12.2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagin DS. Group-Based Modeling of Development. Harvard University Press; Cambridge, MA: 2005. [Google Scholar]
- Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psycho. 2010;6:109–138. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- Nagin DS, Tremblay RE. Developmental Trajectory Groups: Fact or Useful Statistical Fiction? Criminology. 2005;43:873–904. [Google Scholar]
- National Center for Health Statistics. Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities. Hyattsville; Maryland: 2016. [PubMed] [Google Scholar]
- Ong AD, Williams DR, Nwizu U, Gruenewald T. Everyday unfair treatment and multisystem biological dysregulation in African-American adults. Cultural Diversity and Ethnic Minority Psychology. 2017;23:27–35. doi: 10.1037/cdp0000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palloni A, Arias E. Paradox lost: explaining the Hispanic adult mortality advantage. Demography. 2004;41:385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006;35:888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, Gupta A, Kelaher M, Gee G. Racism as a determinant of health: a systematic review and meta-analysis. Plos One. 2015;10:1–48. doi: 10.1371/journal.pone.0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135:531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI. The sociological study of stress. J Health Soc Behav. 1989;30:241–256. [PubMed] [Google Scholar]
- Petts RJ. Family and religious characteristics' influence on delinquency trajectories from adolescence to young adulthood. Am Sociol Rev. 2009;74:465–483. [Google Scholar]
- Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities theory, evidence, and policy implications. J Health Soc Behav. 2010;51:S28–S40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- Ruiz JM, Steffen P, Smith TB. Hispanic mortality paradox: a systematic review and meta-analysis of the longitudinal literature. Am J Public Health. 2013;103:e52–e60. doi: 10.2105/AJPH.2012.301103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan AM, Gee GC, Laflamme DF. The association between self-reported discrimination, physical health and blood pressure: findings from African Americans, Black immigrants, and Latino immigrants in New Hampshire. J Health Care Poor U. 2006;17:116–132. doi: 10.1353/hpu.2006.0092. [DOI] [PubMed] [Google Scholar]
- Schmitt MT, Branscombe NR, Postmes T, Garcia A. The consequences of perceived discrimination for psychological well-being: a meta-analytic review. Psychol Bull. 2014;140:921–948. doi: 10.1037/a0035754. [DOI] [PubMed] [Google Scholar]
- Schulz AJ, Gravlee CC, Williams DR, Israel BA, Mentz G, Rowe Z. Discrimination, symptoms of depression, and self-rated health among African American women in Detroit: results from a longitudinal analysis. Am J Public Health. 2006;96:1265–1270. doi: 10.2105/AJPH.2005.064543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz S, Meyer IH. Mental health disparities research: The impact of within and between group analyses on tests of social stress hypotheses. Soc Sci Med. 2010;70:1111–1118. doi: 10.1016/j.socscimed.2009.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. P Natl Acad Sci. 2001;98:4770–4775. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman M, Merkin SS, Karlamangla A, Koretz B, Seeman T. Social status and biological dysregulation: The “status syndrome” and allostatic load. Soc Sci Med. 2014;118:143–151. doi: 10.1016/j.socscimed.2014.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart Richman L, Pek J, Pascoe E, Bauer DJ. The effects of perceived discrimination on ambulatory blood pressure and affective responses to interpersonal stress modeled over 24 hours. Health Psychol. 2010;29:403–411. doi: 10.1037/a0019045. [DOI] [PubMed] [Google Scholar]
- Smith DP, Bradshaw BS. Rethinking the Hispanic paradox: death rates and life expectancy for US non-Hispanic White and Hispanic populations. Am J Public Health. 2006;96:1686–1692. doi: 10.2105/AJPH.2003.035378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sternthal MJ, Slopen N, Williams DR. Racial disparities in health. Du Bois Rev. 2011;8:95–113. doi: 10.1017/S1742058X11000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor TR, Williams CD, Makambi KH, Mouton C, Harrell JP, Cozier Y, Palmer JR, Rosenberg L, Adams-Campbell LL. Racial discrimination and breast cancer incidence in US Black women: The Black Women's Health Study. Am J Epidemiol. 2007;166:46–54. doi: 10.1093/aje/kwm056. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Stress and health major findings and policy implications. J Health Soc Behav. 2010;51:S41–S53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- Tomfohr L, Cooper DC, Mills PJ, Nelesen RA, Dimsdale JE. Everyday discrimination and nocturnal blood pressure dipping in black and white Americans. Psychosom Med. 2010;72:266–272. doi: 10.1097/PSY.0b013e3181d0d8b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomfohr L, Pung MA, Edwards KM, Dimsdale JE. Racial differences in sleep architecture: the role of ethnic discrimination. Bio Psycho. 2012;89:34–38. doi: 10.1016/j.biopsycho.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RJ. Understanding health disparities: The promise of the stress process model. In: Avison WR, Aneshensel CS, Schieman S, Wheaton B, editors. Advances in the Conceptualization of the Stress Process. Springer; New York: 2009. pp. 3–21. [Google Scholar]
- Vega WA, Rodriguez MA, Gruskin E. Health disparities in the Latino population. Epidemiol Rev. 2009;31:99–112. doi: 10.1093/epirev/mxp008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viruell-Fuentes EA, Morenoff JD, Williams DR, House JS. Language of interview, self-rated health, and the other Latino health puzzle. Am J Public Health. 2011;101:1306–1313. doi: 10.2105/AJPH.2009.175455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Hippel PT. Regression with missing Ys: An improved strategy for analyzing multiply imputed data. Sociol Methodol. 2007;37:83–117. [Google Scholar]
- Williams DR. Miles to go before we sleep racial inequities in health. J Health Soc Behav. 2012;53:279–295. doi: 10.1177/0022146512455804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Jackson PB. Social sources of racial disparities in health. Health Affair. 2005;24:325–334. doi: 10.1377/hlthaff.24.2.325. [DOI] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Mohammed SA, Leavell J, Collins C. Race, socioeconomic status, and health. Ann NY Acad Sci. 2010;1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93:200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Sternthal M. Understanding racial-ethnic disparities in health sociological contributions. J Health Soc Behav. 2010;51:S15–S27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health socio-economic status, stress and discrimination. J Health Psychol. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Wise LA, Palmer JR, Cozier YC, Hunt MO, Stewart EA, Rosenberg L. Perceived racial discrimination and risk of uterine leiomyomata. Epidemiology. 2007;18:747–757. doi: 10.1097/EDE.0b013e3181567e92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeiders KH, Hoyt LT, Adam EK. Associations between self-reported discrimination and diurnal cortisol rhythms among young adults: The moderating role of racial–ethnic minority status. Psychoneuroendocrino. 2014;50:280–288. doi: 10.1016/j.psyneuen.2014.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]