Abstract
The health of people in sub-Saharan Africa is a major global concern. However, data are weak, and little is known about how people in the region perceive their health or their health care. We used data from the Gallup World Poll in 2012 to document sub-Saharan Africans’ perceived health status, their satisfaction with health care, their contact with medical professionals, and the priority they attach to health care. In comparison to other regions of the world, sub-Saharan Africa has the lowest ratings for well-being and the lowest satisfaction with health care. It also has the second lowest perception of personal health, after only the former Soviet Union and its satellites. HIV prevalence is positively correlated with perceived improvements in health care in countries with high prevalence. This is consistent with an improvement in at least some health care services as a result of the largely aid-funded rollout of antiretroviral treatment. Even so, sub-Saharan Africans do not prioritize health care as a matter of policy, although donors are increasingly shifting their aid efforts in sub-Saharan Africa toward health.
Africa is the continent with the highest mortality rates, and it is the only continent where deaths from infectious disease still outnumber deaths from chronic disease.[1] As documented below, spending on health care in sub-Sarahan Africa is low. A typical figure is around $100 per capita in 2005 price-adjusted terms, about half of which is spent in the private sector.
A large share of Western aid to developing countries goes to sub-Saharan Africa. In addition, the region’s share of Western aid increased from 29 percent in 1978–79 to 41 percent in 2008–09.[2]
Aid to sub-Saharan African countries has increasingly been targeted toward health.[3] The region experienced remarkable gains in life expectancy after 1950. However, in the countries that were most seriously affected by the HIV/AIDS epidemic, much or all of the gain was lost by 2000.[4]
Recently—especially since 2005, with help from the US President’s Emergency Plan for AIDS Relief (PEPFAR) and from the Global Fund to Fight AIDS, Tuberculosis, and Malaria—antiretroviral therapy has become more widely available. According to the Joint United Nations Programme on HIV/AIDS (UNAIDS), 9.7 million people (out of nearly 30 million eligible) were receiving antiretroviral therapy in low- and middle-income countries by December 2012.[5] At the same time, and especially in the last decade, there have been marked reductions in infant and child mortality in sub-Saharan Africa.[1]
Africa is also the continent with the poorest health data. Few African countries have complete vital registration systems. In addition, in contrast to the situation in high-income countries, there is a dearth of information on how Africans perceive their own health. The Afrobarometer surveys (see http://www.afrobarometer.org), which cover thirty-five countries, are an important resource for people’s opinions on governance, public-sector performance, and the priority that people attach to public health care. But these surveys provide little information about how people perceive their own health.
The Gallup Organization has been collecting data in sub-Saharan Africa since 2005, as part of its World Poll.[6] We used this rich resource to investigate perceptions of health and health care in the region in 2012. We also used the poll to compare outcomes in sub-Saharan Africa with those in other regions of the world.
We were also interested in the much-debated question of how the HIV/AIDS epidemic has affected people’s perceptions of health and health care. There is good evidence that, in the early days of the epidemic, the countries that were most affected by HIV/AIDS experienced declines in other health services, such as maternal and child health care services.[7] In these countries there was either an absolute decline in services or a decline relative to what would otherwise have been expected, according to preexisting trends or the situation in unaffected countries.
More recent studies have painted a more complex picture.[8,9] They show that some, but not all, services have seen a rebound since the rollout of antiretroviral therapy.
The evidence is hardly conclusive. However, it is possible that the first phase of the HIV/AIDS epidemic undermined the provision of maternal and child health care as resources were diverted. The subsequent expansion of antiretroviral therapy has been complementary with improvement in some other categories of health provision, such as blood tests. This has not been the case with child immunizations, perhaps because new or renovated facilities for HIV/AIDS patients can be used for multiple purposes.
Study Data And Methods
Our main source of data was the Gallup World Poll, which has been conducted since 2005 in more than 160 countries, and especially the data collected from twenty-eight sub-Saharan African countries in 2012. The poll is a multipurpose survey and is nationally representative in nearly all cases. It uses face-to-face interviews in local languages (fifty-eight languages in sub-Saharan Africa in 2012) to ask 1,000 adults per country ages fifteen and older (2,000 adults in Ethiopia, Nigeria, and South Africa) about various aspects of their lives, including health and well-being, emotions, recent experience with physical pain, life evaluation questions, and their perceptions of health and health care.
The survey also collects sociodemographic data that we used in the analysis below. The online Appendix[10] contains a full description of the survey design, as well as the questions used in the analysis.
We also used a range of publicly available data listed in the exhibit notes, such as the World Bank’s World Development Indicators[11] (for the period 2000–12) and data from UNAIDS[5] (for 2012). In addition, we used unit record data—that is, the raw data on individuals and households—from the Demographic and Health Surveys funded by the US Agency for International Development[12] to calculate HIV prevalence at the regional level for matching with data from the Gallup World Poll.
Our methods were essentially the tabulation and graphing of data from the surveys. One analysis used multivariate regression to estimate how our measures varied across people with different social and economic characteristics.
Weaknesses of the survey include the inability to ask questions in depth during face-to-face interviews in each country: Questions are limited in scope and number. In the absence of any directly measured health data—such things as height, weight, blood pressure, or blood work—there is no cross-check on self-reports, which is a common problem in community health surveys. Response rates are often a limitation in household surveys, but are not so here; as is typical in poor countries, response rates for the Gallup World Poll are very high. In these African countries in 2012, eighty-four percent of those designated to respond did and the median refusal rate was 6 percent.
Study Results
Sub-Saharan Africa In The Global Context
Sub-Saharan Africans’ overall evaluation of their well-being is lower than that of any other population in the world (Exhibit 1). The Gallup World Poll uses the Cantril ladder score as a measure of life evaluation, as explained in the notes to Exhibit 1. The relevant question in the survey makes no reference to happiness or other aspects of hedonic experience. Thus, it is a clean measure of life evaluation that is distinct from the emotion of happiness. At an average over sub-Saharan African countries of 4.39, —here an unweighted average of the sampling-weighted averages for each of the countries listed in Exhibit 2—well-being is the lowest in the table.
Exhibit 1.
Self-Reported Health And Well-Being Ratings For Regions Of The World, 2012
| Rating | |||||
|---|---|---|---|---|---|
| Region | Well-being | Quality of health care is okay | Unable to do normal activities | Had a lot of physical pain in previous day | Own health is okay |
| Sub-Saharan Africa | 4.39 | 42.4% | 24.8% | 30.3% | 75.5% |
| East Asia | 5.39 | 64.4 | 17.8 | 19.2 | 81.1 |
| Former communist countries | 5.34 | 51.1 | 29.1 | 27.5 | 69.6 |
| Latin America | 6.20 | 58.9 | 21.5 | 32.1 | 82.0 |
| MENA | 4.94 | 49.0 | 20.8 | 35.0 | 83.5 |
| N. Europe non-Anglo | 6.99 | 86.3 | 23.2 | 24.6 | 82.4 |
| South Asia | 4.90 | 64.9 | 24.7 | 26.7 | 80.6 |
| Southern Europe | 5.92 | 60.6 | 17.6 | 30.4 | 80.6 |
| Rich Anglo | 6.99 | 78.4 | 18.7 | 21.3 | 84.6 |
SOURCE Authors’ analysis of data from the Gallup World Poll.
NOTES Well-being is measured according to the Cantril ladder: Respondents are asked to imagine a ladder numbered from 0 (worst possible life for them) to 10 (best possible life) and to report where they see themselves. The numbers shown are regional averages. Other columns show averages of dichotomous indicators, where 1 is yes, and 0 is no, expressed as percentages. Within regions, each country is given equal weight, irrespective of population size. Where it is not obvious, the regions are as follows: “Former Communist” includes the former Soviet Union and its Eastern European satellites; “MENA” is north African countries and the Middle East; “N. Europe non-Anglo” is the non-English-speaking countries of northern Europe, excluding the satellites of the former Soviet Union; “Rich Anglo” is Australia, Canada, Ireland, New Zealand, the United Kingdom, and the United States. These selections correspond to different patterns of well-being around the world (see Note 11 in text).
Exhibit 2.
Health Statistics For Sub-Saharan African Countries In The 2012 Gallup World Poll
| Country In | perfect health | Ever seen a medical professional | Health spending per person | Health spending in the private sector | Quality of Health care is okay | HIV prevalence |
|---|---|---|---|---|---|---|
| Benin | 39% | 87% | $75 | 47% | 45% | 1.2% |
| Botswana | 24 | 80 | 734 | 39 | 57 | 23.4 |
| Burkina Faso | 24 | 84 | 81 | 50 | 42 | 1.1 |
| Cameroon | 22 | 93 | 128 | 69 | 48 | 4.6 |
| Chad | 30 | 83 | 65 | 73 | 47 | 3.1 |
| Comoros | 40 | —a | 59 | 42 | 24 | 0.1 |
| Congo | 41 | 80 | 109 | 33 | 38 | 3.3 |
| DR Congo | 19 | 87 | 32 | 66 | 32 | —a |
| Ethiopia | 52 | 78 | 52 | 42 | —a 1.4 | |
| Gabon | 24 | 92 | 515 | 47 | 30 | 5.0 |
| Ghana | 23 | 48 | 90 | 44 | 46 | 1.5 |
| Guinea | 34 | 79 | 67 | 73 | 21 | 1.4 |
| Kenya | 19 | 83 | 77 | 60 | 57 | 6.2 |
| Madagascar | 17 | 90 | 40 | 37 | 35 | 0.3 |
| Malawi | 36 | 67 | 77 | 27 | 64 | 10.0 |
| Mali | 42 | 79 | 73 | 55 | 31 | 1.1 |
| Mauritania | 38 | 75 | 129 | 39 | 31 | 1.1 |
| Niger | 34 | 88 | 39 | 45 | 37 | 0.8 |
| Nigeria | 38 | 72 | 139 | 63 | 49 | 3.7 |
| Rwanda | 27 | 67 | 134 | 43 | 65 | 2.9 |
| Senegal | 30 | 92 | 119 | 42 | 42 | 0.7 |
| Somalilandb | 55 | 48 | —a | —a | 49 | —a |
| South Africa | 20 | 77 | 942 | 52 | 46 | 17.3 |
| Sudan | 24 | 43 | 180 | 72 | 28 | 0.4 |
| Tanzania | 17 | 76 | 107 | 60 | 28 | 5.8 |
| Uganda | 23 | 81 | 128 | 74 | 41 | 7.2 |
| Zambia | 39 | 63 | 99 | 40 | 50 | 12.5 |
| Zimbabwe | 35 | 67 | —a | —a | 59 | 14.9 |
SOURCE Authors’ analysis. NOTES Health spending per capita is in 2005 purchasing power parity US dollars. Those numbers and the share of total healthcare spending that goes to the private sector are taken from the World Development Indicators (see Note 11 in text) and refer to the year 2011. HIV prevalence rates come from the Joint United Nations Programme on HIV/AIDS. Other statistics were calculated by the authors from the 2012 Gallup World Poll data.
[Not available. Please provide].
The Somaliland region, not Somalia.
Low well-being is largely a matter of low incomes in sub-Saharan Africa. As previous work has shown,[13,14] there is a nearly linear relationship around the world between average Cantril ladder scores and the logarithm of per capita gross domestic product (GDP). Sub-Saharan African countries are poor, and people in the region understand that their lives are much worse than they might be.
Sub-Saharan Africans are also relatively unhappy with their health care: Only 42.4 percent are satisfied with the availability of quality health care in the city or area in which they live (Exhibit 1). Again, this is the lowest level of satisfaction in the world. In fact, it is less than half of the level for the highest scoring region, the non-English-speaking countries of northern Europe.
A summary of Afrobarometer surveys[15] of countries in sub-Saharan Africa reports that 57 percent of respondents say that the government has done well or fairly well at improving basic health services, a percentage that declined between 2002 and 2013. Of course, the questions in the Afrobarometer and Gallup surveys have different wording, and the Afrobarometer surveys cover only publicly provided health care.
The percentages of people who had a health problem that prevented them from doing any of the things people their age can usually do were more equally distributed across the regions of the world (Exhibit 1). That was also the case for the questions about the respondent’s physical pain and satisfaction with his or her health. Sub-Saharan Africa is not last in any of these three questions. Nonetheless, the picture of self-reported health in the region is broadly negative.
Health Outcomes In Twenty-Eight Sub-Saharan African Countries
There was an astonishing range of health outcomes across the sub-Saharan African countries surveyed in the 2012 Gallup World Poll (Exhibit 2). The fraction of respondents who reported that they were in perfect health ranged from highs of more than 50 percent in Somaliland and in Ethiopia to only 17 percent in Madagascar and Tanzania. In Ghana, Somaliland, and Sudan, more than half of the population said that they had never had contact with a medical professional. In contrast, in Cameroon, Gabon, and Senegal, the fractions were less than 10 percent.
The cross-country correlation between those in perfect health and those who had never had contact with a medical professional was −0.285. But note that the within-country correlations are small and vary in sign across countries. People in poor health are more likely to seek out medical attention. However, if this were the main reason for the negative cross-country correlation between perfect health and having ever seen medical personnel, it would show up within countries, too. The fact that it does not do so suggests that some other mechanism is at work.
Health spending varied even more widely by country (Exhibit 2). South Africa and Botswana, both relatively wealthy and both with high HIV prevalence, spent $942 and $734 per person, respectively.
The median for all countries was $109 per head, but the Democratic Republic of the Congo, Ethiopia, Madagascar, and Niger spent less than half of that. In any case, $109 a year does not buy much health care. At these levels of spending, there is a correlation of 0 between spending on health care and the fraction of respondents who had ever had contact with a medical professional.
Much of the literature on health in poor countries focuses on the provision of health care by the state.[16] This may be because, since the Alma-Ata Declaration of 1978[17] established the goal of primary health care for all people, that provision is seen as desirable in itself. At least some of the questions about attitudes toward health care, as in the Afrobarometer, relate to the government’s role in providing basic health services.
Yet Exhibit 2 shows that privately provided health care is important in sub-Saharan Africa. In twelve of the twenty-eight countries listed, at least half of all health care spending is in the private sector. And in only one country (Malawi) does the private sector account for less than a third of all health care spending.
The private sector tends to be somewhat more important in places where little is spent overall. The literature[16,18] on health care provision in poor countries suggests that private providers can often deliver as good service as the state where the state has low capacity, especially for routine care. The private provision of health care also does not suffer from the problems of mass absenteeism of health care providers that often mar public-sector provision.[18,19]
Of course, the limited capacity of the state undercuts not only the public provision of health care, but also government regulation of private health care providers. Both public and private providers have distinct strengths and weaknesses.[18] Unqualified and unregulated practitioners in the private sector can provide very bad care indeed.
The highest correlation among results in Exhibit 2 (0.51) was between HIV prevalence and the fraction of respondents who approved of the health care system. There was a positive correlation between per capita GDP (in purchasing power parity US dollars) and HIV prevalence. However, the correlation between approval of the health care system and HIV prevalence is not attributable to variations in income: The partial correlation after allowing for the log of GDP per capita was 0.48. It should be noted, however, that the countries with the highest HIV prevalence at the beginning of the epidemic were those with the best-developed health systems.[7]
Health Outcomes At The Individual Level
The Gallup data allow a look beneath the aggregate level and show how perceptions and self-reported health and well-being vary across age, sex, income level, and other variables. The results (presented in detail in the Appendix)[10] are predictable in some cases but also contain some surprises.
The effects of age on life evaluation provide the first surprise: The average life evaluation did not differ by age in sub-Saharan African countries. This is in sharp contrast to the famous U-shape age profile of life evaluation in the United Kingdom, the United States, and other high-income English-speaking countries of the world. In those countries, early and later years are evaluated highly, with the lowest levels of well-being occurring in the middle years.[20]
One possible explanation for the U-shape profile is that it occurs only in countries where there are strong social security systems and programs that provide health care coverage for the elderly—which is certainly not the case in sub-Saharan Africa. Yet the other variables considered in this analysis were correlated with well-being in similar ways to correlations in high-income countries. For example, women evaluated their lives more highly than men, and income and education brought greater well-being, with a coefficient in line with the situation in other countries.[21]
Compared to single or married people, those who were divorced, separated, and widowed people (the “other” category of marital status) reported lower levels of well-being. Similarly, people with two or more children living in the household reported lower well-being than people with one or no children at home.
We also examined the correlates of two measures of self-reported health, in which the respondent reported whether he or she was in perfect health and whether his or her health was satisfactory. These two questions are posed separately, and both are distinct from the question about whether or not health care was satisfactory.
Not surprisingly, in sub-Saharan Africa, both measures declined with age. However, perfect health deteriorated more rapidly at young ages, while satisfactory health deteriorated more rapidly at older ages. Better off, more educated, and more religious people (those who reported that religion was very important in their lives) were in better health, compared to women and those who were widowed, separated, or divorced.
Confidence in sub-Saharan African health care systems (the “health care is okay” variable in Exhibit 2) varied sharply by country. However, within countries there was very little variation by age or marital status. Women, people with more education, and those with higher incomes had more confidence in their country’s system, compared to men, those with less education, and those with lower incomes. [please provide]. This is surprising, because the groups with more confidence are also more likely to experience health care and—one might have thought—to understand its weaknesses. Perhaps they simply have limited experience with which to compare.
There was a huge cross-country variation in the numbers of people who ever had contact with the medical system in sub-Saharan African countries (Exhibit 2). In addition, our regression analysis shows that the probability of ever having had contact with a medic or other health care provider in the system increased with age. The probability was also higher for women and for people who were married, had children, were more educated, or were more religious, compared to men, those who were not married, had no children, were less educated or were less religious. The relationship between being religious and having had contact with the medical system may reflect the role of religious institutions in providing health care in much of the region.
Perceptions Of Health Care And The HIV/AIDS Epidemic
One controversial issue in both the literature and the donor community is the effect of the HIV/AIDS epidemic on health care, both before and after the dramatic increase in aid after 2004 from PEPFAR and the Global Fund. This issue has been studied over a range of periods.[7–9]
Perhaps the most obvious story here is that, before the aid for the disease, HIV/AIDS simply put additional strains on already weak health care systems, undermining previously provided services such as those related to mother and child health. With the inflow of funds from PEPFAR, the Global Fund, and other donors after 2004, that undermining might have been reversed if the expanded facilities and numbers of medical personnel were used not only for the delivery of antiretroviral therapy, but also for other services.
A more negative possibility, which has been a concern, is that new services displaced old ones—for example, by bidding nurses away from what they had previously been doing in some countries.[8] A 2014 study[9] paints a relatively positive picture, with mother and child health services improving in the affected regions and countries after 2004.
Blood tests for pregnant women are now routinely given to prevent mother-to-child transmission of the virus, and this has certainly led to an increase in blood tests and possibly in some other antenatal services. For both Karen Grépin[8] and Josephine Duh,[9] the effects differ for different kinds of service provision.
The most relevant question in the Gallup World Poll is whether the respondent believes health care has improved over the previous five years. The respondent can answer “yes,” “stayed the same,” or “got worse”: We coded the three responses as 1, 0, and –1. Exhibit 3 plots the average score for perceived improvement in health care against the HIV prevalence estimates reported in Exhibit 2. Note first that in all of the countries except Sudan and Tanzania, people thought that the quality of health care had increased over the previous five years.
Exhibit 3.
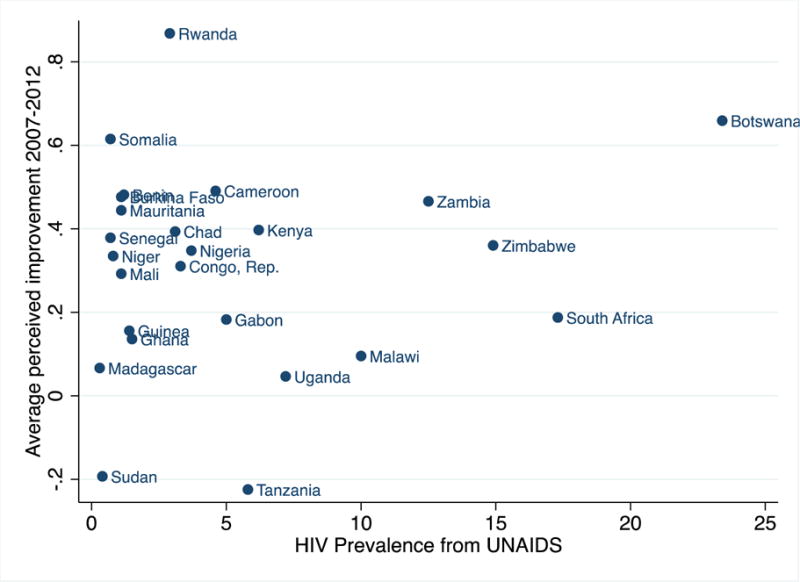
Perceived Improvement In Health Care, 2007–12, And HIV Prevalence, 2012, In Sub-Saharan African Countries In The 2012 Gallup World Poll
Source/Notes: SOURCE Authors’ analysis of data from the Gallup World Poll and the Joint United Nations Programme on HIV/AIDS. NOTE For the point marked Somalia, the prevalence data relate to Somalia, and the perceived improvement data relate to the Somaliland region.
The correlation between perceived change in the quality of health care and HIV prevalence is only 0.21, which is not significantly different from zero. Thus, according to these measures, people’s perception of whether or not health care had improved did not vary according to the level of HIV prevalence in their country.
The results for individual countries are also interesting. Botswana is a case in which high HIV prevalence brought substantial improvements in health care and this shows up clearly in Exhibit 3. Similarly, among the countries with an HIV prevalence of at least 5 percent—Botswana, Gabon, Kenya, Malawi, South Africa, Tanzania, Uganda, Zambia, and Zimbabwe—there was a positive relationship between prevalence and perceived improvement in health care. The fact that there was no overall positive correlation is because, among the countries with a low prevalence, a wide range of health care improvements came about through other factors.
The Gallup World Poll also asks respondents their expectations of health care improvement in the following five years. The results for this variable—which we also coded 1, 0, or –1—were higher on average than the perception of health care in the previous five years: 47 percent expected net improvements, as opposed to only 36 percent who reported seeing improvements in the previous five years. Even so, there was a high cross-country correlation between the past and the future. Expectations about future improvements in health care were no more correlated with HIV prevalence than were the perceptions of past improvements.
In summary, there is no evidence in Exhibit 3 that countries with high HIV prevalence had any systematic decline in the quality of health care in 2007–12. If anything, the reverse seems to be true, at least among the countries most affected by HIV. And note again from Exhibit 2 that the countries with high HIV prevalence were also those with the highest fraction of respondents who were satisfied with the quality of their health care in 2012, a correlation that is significant. All of this gives a mildly positive picture of the relationship between health care perceptions and HIV prevalence, at least in the most recent years.
To check that these findings were not confounded by a relationship between economic growth and improvements in health care, we used World Bank data on the rate of growth of GDP per capita from 2000 to 2012, as well as the separate growth rates from 2000 to 2005 and from 2005 to 2012. None of the growth rates had a significant correlation with perceptions of health care improvement.
In many of the affected countries in sub-Saharan Africa, the HIV prevalence rate varies within countries by region. These regional HIV prevalence rates within countries can be estimated from successive rounds of the Demographic and Health Surveys, in some of which respondents are administered tests for the HIV virus so that their measured HIV status does not depend on what they themselves know. We used the prevalence estimates for the subset of regions that we could match to the regional information in the Gallup World Poll, which gave us 140 observations from fifteen countries between 2003 and 2012. Of the 140 regions, 86 were observed in the four-year period 2009–12. For these regions, we calculated the average HIV prevalence rates of people ages 15–49, which is the age range of respondents in the Demographic and Health Surveys.[12]
Clearly, these data—with their age restriction, limited number of countries, and range of years—are less than perfect. However, having 140 observations as opposed to only 24, which is the case in Exhibit 3, gave us a better chance of observing any patterns that exist.
Exhibit 4 presents more details than Exhibit 3 does, although some countries in Exhibit 3—including Botswana—are missing from Exhibit 4. Exhibit 4 confirms the overall lack of a pattern when all regions in all countries are pooled. Furthermore, as in Exhibit 3, there is a suggestion of a negative relationship between perceived improvements in health care and HIV prevalence where the prevalence is low, and of a positive relationship in the regions with high HIV prevalence.
Exhibit 4.
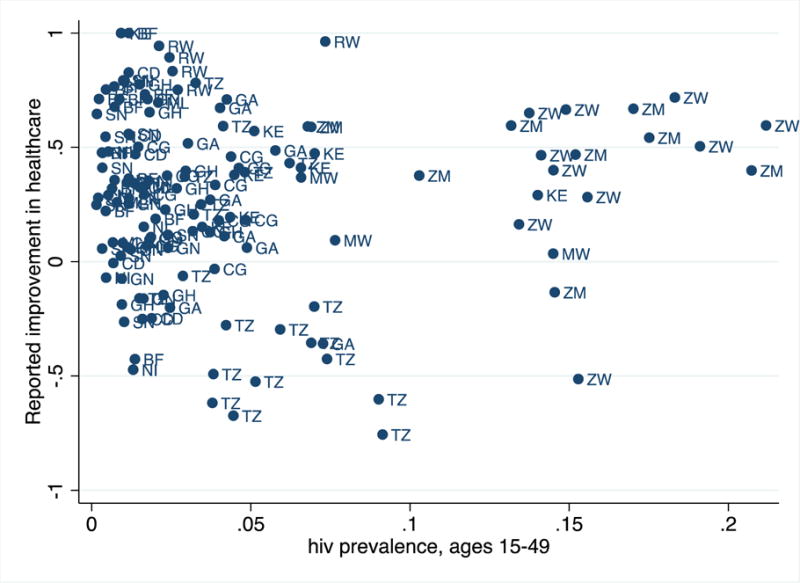
Perceived Improvement In Health Care, In 2007–12, And HIV Prevalence For Those Ages 15–49, 2012, By Demographic And Health Survey Regions
Source/Notes: SOURCE Authors’ analysis of data from the Demographic and Health Surveys and the Gallup World Poll. NOTES We used Demographic and Health Survey codes for the countries: BF is Burkina Faso, CD is the Democratic Republic of the Congo, CG is Congo, GA is Gabon, GH is Ghana, GN is Guinea, KE is Kenya, MW is Malawi, NI is Niger, RW is Rwanda, SN is Senegal, TZ is Tanzania, ZM is Zambia, and ZW is Zimbabwe.
We examine the relationship within countries by running the regression on the data in Exhibit 4 with the addition of country dummies, there was a negative but insignificant relationship between whether health care was perceived to have improved and the rate of HIV prevalence. We examined whether this relationship was different when we accounted for education (which was positively correlated with HIV prevalence) and urbanization (which was uncorrelated with HIV prevalence in the data shown in Exhibit 4). However, the presence of these two factors in the regression had little effect.
In summary, one explanation for the data in Exhibit 4 is that [please provide] a high rate of HIV prevalence in the population by itself reduced the perceived effectiveness of the health care system. We can see this negative relation in the countries with low HIV prevalence today, just as was the case in all countries in the early years of the epidemic.
In recent years, however, countries with high HIV prevalence have attracted a great deal of health-related aid, which may have helped improve their citizens’ perceptions of their health care systems. Exhibit 4 also shows some evidence that, within countries with high HIV prevalence—such as Tanzania, Zambia, and Zimbabwe—there was a negative relationship across regions within each country between perceived improvement and HIV prevalence. That would be the case if health aid were not well allocated within countries.
Sub-Saharan Africans’ Perceptions Of Their Most Urgent Needs
Health aid to sub-Saharan Africa from high-income countries has recently increased much more rapidly than nonhealth aid. However, there have been occasional questions about whether this is a response to sub-Saharan African demands or is something that the richer countries are choosing to do for reasons of their own. The latter view has been argued in general by Angus Deaton,[4] and more specifically, using Afrobarometer data, by Homi Kharas[22] and Benjamin Leo.[3]
The Gallup World Poll asks respondents to name the issues that should be the highest priority for their government. Respondents are presented with the following options: health care, education, providing new jobs, improving agriculture, providing electricity, and tackling corruption. Health care is not the highest priority, which is also the case in the Afrobarometer surveys.[3,22] Averaged over all sub-Saharan African countries (with each country equally weighted), 31.0 percent of people picked new jobs as their top priority, and 21.0 percent picked improving agriculture. Tackling corruption was next, at 14.4 percent. Education and health care were chosen by 13.6 and 13.5 percent of the respondents, respectively. Providing electricity was picked by only 6.3 percent.
When we examined the correlation between these preferences, we found that people who prioritized agriculture also prioritized new jobs. This suggests that these choices share an underlying factor, the importance of better livelihoods.
We also found a strong negative correlation across countries between prioritizing health care and HIV prevalence as listed in Exhibit 2. Countries with the highest HIV rates had the most advanced health care systems at the start of the epidemic.[3] As a result, people in those countries may feel that their governments are already paying enough attention to health care.
The 2012 Gallup World Poll did not ask about HIV/AIDS as a priority. However, when that question was asked in a previous survey, it ranked third— after poverty reduction and hunger reduction and ahead of providing more jobs, reducing child mortality, reducing maternal mortality, and improving education.
Of course, just because people in sub-Saharan Africa do not see health care as the highest priority does not mean that aid agencies are incorrect to prioritize it. People in the region may be poorly informed (for example, about the possible effects of better health care on their health and thus on their livelihoods) or, after centuries of high morbidity, they may not believe that the government (or anyone else) is capable of providing any meaningful relief. But even if they are well informed, it might also be the case that aid agencies believe—correctly or incorrectly—that they are more effective at saving lives than at generating economic growth.
Conclusion
We used data from Gallup’s World Poll to examine how sub-Saharan Africans perceive their well-being, health, and health care systems. The people of the region rate their well-being lower than do the people of any other region in the world. The same is true of sub-Saharan Africans’ perception of the health care that they receive. Even so, people in the region do not feel that improving health care should be the highest priority for their governments. Nonetheless, donors are increasingly focusing their aid efforts in sub-Saharan Africa on health.
Does HIV prevalence make health care even worse? Our results suggest that this is likely true, except where HIV prevalence is highest. In these heavily affected countries, there may well have been positive spillovers from external funding for HIV into the more general health care system.
Acknowledgments
Angus Deaton’s work is supported by the Gallup Organization and by the National Institute of Aging through both the National Bureau of Economic Research (Grant Nos. 5R01AG040629–02 and P01 AG05842–14) and Princeton University’s Roybal Center for Translational Research on Aging (Grant No. P30 AG024928). Deaton is a consultant to the Gallup Organization. The authors are grateful to Anne Case for comments on earlier versions and to Josephine Duh for comments and assistance with the regional HIV prevalence data from the Demographic and Health Surveys.
Biographies
Angus S. Deaton (deaton@princeton.edu) is the Dwight D. Eisenhower Professor of International Affairs and Professor of Economics and International Affairs at the Woodrow Wilson School, Princeton University, in New Jersey.
Robert Tortora was principal scientist and chief methodologist at the Gallup Organization, in Washington, D.C., when this article was written. He is now a Senior Fellow of Survey Methodology at ICF International in Rockville, Maryland.
Contributor Information
Angus S. Deaton, Princeton University, Princeton, NJ
Robert Tortora, Gallup Organization, Washington, DC.
Notes
- 1.United Nations World mortality report 2013 [Internet] New York (NY): UN; 2013. [cited 2015 Jan 14]. Available from: http://www.un.org/en/development/desa/population/publications/pdf/mortality/WMR2013/World_Mortality_2013_Report.pdf. [Google Scholar]
- 2.Organization for Economic Cooperation and Development. Measuring aid: 50 years of DAC statistics—1961–2011 [Internet] Paris: OECD; 2011. Apr, [cited 2015 Jan 14]. Available from http://www.oecd.org/dac/stats/documentupload/MeasuringAid50yearsDACStats.pdf. [Google Scholar]
- 3.Leo B. Is anyone listening? Does US foreign assistance target people’s top priorities? [Internet] Washington (DC): Center for Global Development; 2013. Dec 2, [cited 2015 Jan 16]. (Working Paper No. 348 Available from: http://www.cgdev.org/sites/default/files/anyone-listening-us-foreign-assistance-target-top-needs_final.pdf. [Google Scholar]
- 4.Deaton A. The great escape: health, wealth, and the origins of inequality. Princeton (NJ): Princeton University Press; 2013. [Google Scholar]
- 5.Joint United Nations Programme on HIV/AIDS. AIDS by the numbers [Internet] Geneva: UNAIDS; 2013. [cited 2015 Jan 14]. Available from http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2013/JC2571_AIDS_by_the_numbers_en.pdf. [Google Scholar]
- 6.Gallup. How does the Gallup World Poll work? [Internet] Washington (DC): Gallup; 2014. Oct 14, [cited 2015 Jan 16]. Available from: http://www.gallup.com/178667/gallup-world-poll-work.aspx. [Google Scholar]
- 7.Case A, Paxson C. The impact of the AIDS pandemic on health services in Africa: evidence from Demographic and Health Surveys. Demography. 2001;48(2):675–97. doi: 10.1007/s13524-011-0026-3. [DOI] [PubMed] [Google Scholar]
- 8.Grépin KA. HIV donor funding has both boosted and curbed the delivery of different non-HIV health services in sub-Saharan Africa. Health Aff (Millwood) 2012;31(7):1406–14. doi: 10.1377/hlthaff.2012.0279. [DOI] [PubMed] [Google Scholar]
- 9.Duh JI (Brattle Group, San Francisco, CA) Spillovers of AIDS treatment on maternal and child health services in sub-Saharan Africa [Internet] 2014 Sep 25; [cited 2015 Jan 16]. Unpublished Paper. Available from: https://dl.dropboxusercontent.com/u/42616247/AIDS-MCHServices_JDuh.pdf.
- 10.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 11.World Bank. World Development Indicators [Internet] Washington (DC): World Bank; p. c 2015. [cited 2015 Jan 16]. Available from: http://data.worldbank.org/data-catalog/world-development-indicators. [Google Scholar]
- 12.US Agency for International Development. The DHS Program: demographic and health surveys [Internet] Rockville (MD): ICF International; [cited 2015 Jan 16]. Available from: http://www.dhsprogram.com. [Google Scholar]
- 13.Deaton A. Income, health, and well-being around the world: evidence from the Gallup World Poll. J Econ Perspect. 2008;22(2):53–72. doi: 10.1257/jep.22.2.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stevenson B, Wolfers J. Economic growth and subjective well-being: reassessing the Easterlin paradox. Washington (DC): Brookings Institution; 2008. (Brookings Papers on Economic Activity). [Google Scholar]
- 15.Asunka J. What people want from government: basic services performance ratings, 34 countries [Internet] 2013 Dec 11; Afrobarometer. [cited 2015 Jan 14]. Available from http://www.afrobarometer.org/files/documents/policy_brief/ab_r5_policybriefno5.pdf.
- 16.Filmer D, Hammer JS, Pritchett LH. Weak links in the chain II: a prescription for health policy in poor countries. World Bank Res Obs. 2002;17(1):47–66. [Google Scholar]
- 17.World Health Organization. Declaration of Alma-Ata [Internet] Geneva: WHO; 1978. Sep, [cited 2015 Jan 16]. Available from: http://www.who.int/publications/almaata_declaration_en.pdf. [Google Scholar]
- 18.Das J, Hammer J. Which doctor? Combining vignettes and item response to measure clinical competence. J Dev Econ. 2005;78(2):348–83. [Google Scholar]
- 19.Chaudhury N, Hammer J, Kremer M, Muralidharan K, Rogers FH. Missing in action: teacher and health worker absence in developing countries. J Econ Perspect. 2006;20(1):91–116. doi: 10.1257/089533006776526058. [DOI] [PubMed] [Google Scholar]
- 20.Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet. 2014 Nov 6; doi: 10.1016/S0140-6736(13)61489-0. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sacks DW, Stevenson B, Wolfers J. The new stylized facts about income and subjective well-being. Emotion. 2012;12(6):1181–7. doi: 10.1037/a0029873. [DOI] [PubMed] [Google Scholar]
- 22.Kharas H. A reality check on African aid [Internet] Washington (DC): Brookings Institution; 2008. Feb 20, [cited 2015 Jan 14]. Available from: http://www.brookings.edu/research/opinions/2008/02/20-african-aid-kharas. [Google Scholar]


