Abstract
Airway management is essential for safe anesthesia and endotracheal intubation is the most important procedure by which critically ill patients can be better managed, especially if done quickly and successfully. This study aimed to compare the techniques of intubation through laryngeal mask airway (LMA) using a bougie versus video laryngoscopy (VL) regarding to intubation success and the quality of intubation indices in patients with difficult airways. This randomized clinical trial was performed on 96 patients aged 16–76 years with Mallampati class 3 or 4 who underwent elective surgery. Once the demographics were recorded, patients were randomly divided into two groups and the first group intubated with VL, and the second group intubated through laryngeal mask using a bougie. Then vital signs, arterial oxygen saturation, the time required for successful intubation, and ease of intubation were recorded. Here t-tests, chi-square, Fisher exact tests, and analysis of variance for repeated measurement were used to analyze the data in SPSS software. The overall success rates of intubation in VL and LMA groups were 46 (96%) and 44 (92%), respectively. The mean duration of intubation for the LMA and VL groups was 18.70 ± 6.73 and 14.21 ± 4.14 seconds, respectively (P < 0.001). Moreover, visual analogue scale score for pain in throat was significantly lower in VL group than LMA (1.65 ± 0.76 vs. 1.33 ± 0.52). Moreover, easy intubation in bougie group was 50%, while the easy intubation in VL was 73% (P = 0.023). In addition, incidence of cough was 31% in the LMA with bougie group and 9% in VL group (P = 0.005). The VL technique is an easier method and has a shorter intubation time than LMA using bougie, and causes a lower incidence of coughing, laryngospasm in patients that need intubation. Moreover, cough and discomfort in the throat tend to be less in VL, and the LMA could be used as replacement of VL in hard situations.
Keywords: intratracheal intubation, laryngoscopes, laryngeal mask, surgical equipment
INTRODUCTION
Although airways can be managed largely in accordance with the desire of a person with experience and training, airway management is difficult and even seems impossible in some cases even for very experienced people so that all team members can face struggle and frustration. Endotracheal intubation in the difficult airway has always considered a serious problem in elective or emergency surgery.1 There are several techniques to control the airway, including laryngeal mask airway (LMA), which is used to create an open airway.2,3 The technique, although achieving a success rate of almost 100% when placed in the operating room, is likely to have a lower rate in emergency situations. Other advantages include no need for laryngoscopy, lower respiratory tract invasion, better patient tolerance and less cough.4 Glottis and trachea manipulations are required less frequently in the LMA technique.5 It does not reduce the risk of aspiration, especially in fasting patients.6,7 There is another airway management technique in which after placing the LMA, a bougie is passed with the tip placed inside the trachea.8,9,10 After removing the mask, the endotracheal tube is railroaded over the bougie into the trachea and thus there will be a completely safe airway.
Video laryngoscopy (VL) can be considered as an effective alternative to direct laryngoscopy in patients with difficult airways and has been reported in various studies to achieve a very high success rate.11,12,13 Despite the many advantages, there exist some disadvantages including high cost and non-availability in all hospitals to use the VL, no studies have been designed to compare intubation through LMA using a bougie versus VL. Therefore, we aimed to compare the rate of intubation success and the quality of intubation indices between two techniques that showed higher success rate of laryngeal masks in patients with difficult airways.
SUBJECTS AND METHODS
This study was a prospective single blinded clinical trial that conducted on 96 patients admitted to ValiAsr and Amir Al-mo'menin hospitals in Arak, Iran for elective surgery, who were enrolled according to inclusion and exclusion criteria after providing informed consent. The study protocol was approved by the ethic committee of Arak University of Medical Sciences (with the Code of Ethics: IR.ARAKMU.REC.1394.43) and was registered in the Iranian Registry of Clinical Trials with the registration No. IRCT2015102214056N6. Sample size of study was calculated by considering type one error (α = 0.05) and power (1 – β = 0.80). Based on results of a recent study the minimum sample size in each group was calculated to be 35.
Inclusion criteria were over 15 years old and no history of anesthesia in recent last year. Moreover, patients who affected to ASA I and II and who were Malampati III and IV were included in study. The exclusion criteria were patients with a history of underlying cardiac and respiratory problems and coagulation problems or pregnant women were excluded from the study due to semi-emergency conditions and relative instability of patients.
Demographics characteristics including age, sex, body mass index (BMI), vital signs, and arterial oxygen saturation were recorded before patients underwent cardiac monitoring. After all patients were treated with 100% oxygen for 5 minutes, the induction of anesthesia was performed with propofol 2 mg/kg and fentanyl 1 μg/kg and then succinylcholine 1 mg/kg was injected with midazolam 0.015 mg/kg.
After informed consent was given by eligible patients, block randomization was used for random allocation of patients to randomly divide into two groups. The block size was 4. Both groups were well matched for age, gender distribution, and BMI. In the first group, the intubation was performed with the VL, C-mac VL (8403 ZX), that manufactured by STORTZ and the balde number 3 and 4 was used based on the patient bulk. In second group, a bougie was passed through an already inserted LMA based on patient's weight, allowing its tip to be placed into the larynx. Then we tried to remove the mask and the endotracheal tube was railroaded over the bougie into the trachea. The LMA Classic (venticare) manufactured by Flexicare Medical Limited company in UK and Gum Elastic Bougie (portex) is manufactured in Mexico were used. Then, an anesthetist colleague (attend) measured and recorded the time required for successful intubation, and ease of intubation. Moreover, heart rate (HR), mean blood pressure (MBP), and oxygen saturation (SO2) were recorded in four times at baseline, in induction time, 5 and 10 minutes after induction. An anesthesiologist expert evaluated the easy or difficult of intubation as easy (without problem), mild (with a moderate pressure in laryngoscopy) and difficult (severe pressure in laryngoscopy). The intubation time calculated for VL and LMA groups from putting the blade or LMA in the patient's mouth until confirming the intubation with Etco2. In the other word intubation time calculated from the beginning of the procedure until intubation is confirmed with bilateral chest auscultation and confirmation of end-tidal carbon dioxide in the monitor.
Thirty minutes after tracheal extubation in the recovery room, a 10-point visual analogue scale (VAS) was used to ask the patient about sore throat, cough, and laryngospasm were recorded. The rate of intubation success and the quality of intubation indices were the study outcomes and compare between two groups. Paired t-test, chi-square, Fisher exact test and analysis of variance (ANOVA) for repeated measurement were used to analyze the data that was entered in SPSS software (IBM Corp., Armonk, NY, USA). Significant level was considered at 0.05.
RESULTS
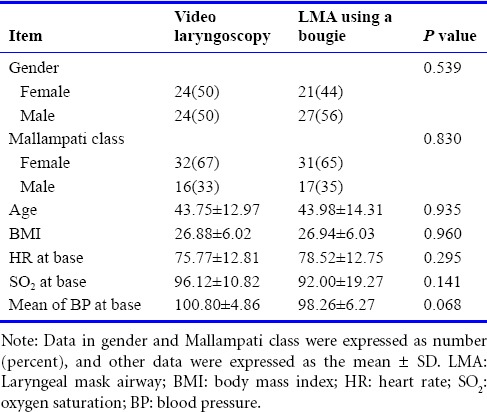
In this clinical trial, 96 patients (51 males and 45 females) were selected for elective surgery. The Overall Success Rate of Intubation in VL and LMA groups were 46 (96%) and 44 (92%), respectively. Unsuccessful patients excluded from study and fiberoptic tube was used for them. Table 1 shows the demographic characteristics of the patients in two groups. The ages of the patients ranged from 16 to 76 years, with an average of 43.80 ± 13.23 years. The mean age of the subjects was 43.75 ± 12.97 years in the VL group and 43.98 ± 14.31 years in the LMA with bougie group, showing no statistical difference between the two groups (P = 0.935). In the LMA group, 65% patients were in class III, and the VL group included 67% patients in class III, with no difference between the two groups (P = 0.830). Moreover, the mean of BMI in study patients were not significantly different between the two study groups (P = 0.960). Furthermore, the two groups were also balanced and there was no difference between them. In addition, the vital signs including HR, SO2, and MBP at the baseline were same in two groups.
Table 1.
The baseline comparison between the two techniques of intubation including LMA using a bougie and video laryngoscopy based on gender, mallampati class, age, BMI and vital signs
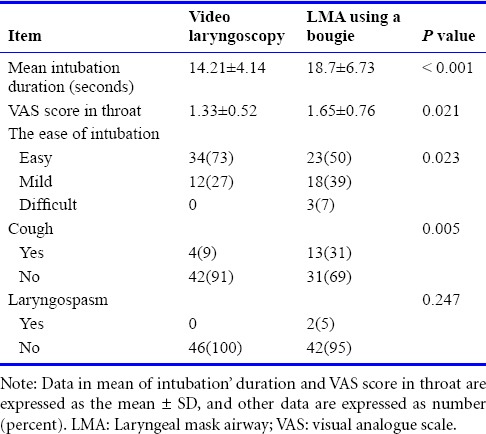
Our results for comparing two groups are depicted in Table 2. The mean duration of intubation for the LMA and VL groups was 18.70 ± 6.73 and 14.21 ± 4.14 seconds, respectively (P < 0.001). According to independent t-test a significant difference observed between the two groups in the mean duration of intubation and the bougie may be inferior to the VL in this regard (P < 0.001). Moreover, the pain in throat based on the VAS score was significantly lower in VL group than LMA (1.65 ± 0.76 vs. 1.33 ± 0.52). Regarding the ease of intubation, the ratio of easy intubation was 50.1% in LMA group and 73.4% in the LA group, and intergroup difference was statistically significant with chi-square test (P = 0.023). The incidence of cough in the LMA group was calculated to be 31% while the cough incidence for VL group estimated as 9% and this difference between two study groups was statistically significant (P = 0.005). According to the results, the incidence of postoperative laryngospasm in patients who were intubated with bougie was 4.2%, while no laryngospasm occurred in other patients who were intubated with VL, but this difference was not significant (P = 0.247).
Table 2.
Comparison of VAS score, the ease of intubation and incidence of postoperative laryngospasm between the two techniques of intubation including LMA using a bougie and video laryngoscopy
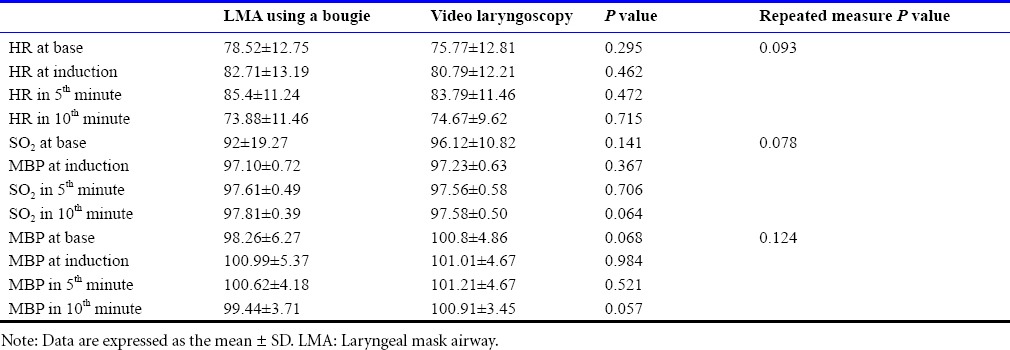
The results of our study compared the efficacy of the two-intubation techniques on vital signs including HR, SO2 and MBP at the baseline, at the time of induction, at the 5th and 10th minutes after the induction. Based on our results there was no statistical significant difference between two groups based on t-test in mean of HR, SO2 and MBP in each time of induction. Moreover, the analysis of variance for repeated measurement did not showed significant trend in the mean of HR, SO2 and MBP at the sequential measured times between two groups (P > 0.05; Table 3).
Table 3.
Comparison of heart rate (HR), arterial oxygen saturation (SO2) and mean blood pressure (MBP) at the base, induction, 5th and 10th minutes after induction between LMA using a bougie and video laryngoscopy groups
DISCUSSION
The results of our study show that the time required for intubation in the bougie group is higher than that in the VL group. Consistent with our study, a study to compare the use of VL and LMA intubation in patients with normal airway anatomy showed that the glidescope can speed up the intubation process and increase the success rate of intubation.14 In addition, the optical stylus was shown in another study lower mean speed of intubation than the use of bougie (20.8 vs. 30.0 seconds) and could therefore be considered a better method than the use of bougie in difficult intubation.15]
Our results suggest that, the patients in the bougie group may be more difficult to intubate than those in the VL group. In a study to compare several techniques of tracheal intubation, the video laryngoscope was concluded to provide a good view of the throat and vocal cords, but multiple repetitions are required during intubation.16 In addition, Weiss et al.17 showed that since VL does not impair the normal intubation procedure, it can be used as a safe and beneficial tool for teaching and supervising endotracheal intubation in children. On the other hand, VL is more effective than direct laryngoscopy because the vocal cords can be better viewed on the monitor screen in difficult laryngoscopies where there is no clear view. As noted by other studies, a variety of newly designed VLs can be used in the management of most difficult intubations or in severe and life threatening cases.17,18,19,20,21]
In our study, no difference observed between the two techniques in terms of the incidence of laryngospasm as airway complications. Cough is the a symptom that seems to occur less after intubation using VL because the VL can give a better view of the larynx in difficult intubations and reduce the rate of complications. Moreover, the pain score in sore throat has lower mean in VL group than LMA group. On the other hand, a review study in 2010 showed a very low incidence of airway complications such as postoperative hoarseness and cough in the LMA group.9]
In our study, there was no significant difference in vital signs including HR, SO2 and mean of BP in the intubation time and after the procedure in both groups. Montazari et al.22 found that the hemodynamic changes produced by LMA are significantly lower than those produced by the face mask and endotracheal intubation, and tracheal irritation is the leading cause of the hemodynamic changes associated with endotracheal intubation in patients during general anesthesia. Intubation often causes hemodynamic responses at two distinct stages of laryngoscopy and endotracheal intubation, and the motion of laryngoscope blade itself causes tracheal irritation and hemodynamic changes. Many studies seem to agree that less irritation of the larynx is observed in the use of VL where a good view of the larynx is available. In addition, it is not also necessary to move and manipulate the head and neck to create a more appropriate view.22 In the present study, no difference was observed between the two intubation techniques in terms of the effects on heart rate. Regarding the efficacy of intubation through LMA using a bougie versus VL on mean arterial blood pressure, no significant difference was seen between the two groups at all times. The results of a study to compare the hemodynamic effects produced by two LMAs and direct laryngoscopy techniques showed that despite the increase in blood pressure and heart rate, no significant difference can be seen between the techniques in any of the time points compared to the baseline and that the hemodynamic response to intubation is similar in both groups.10 In another studies to compare the hemodynamic responses to LMA using laryngoscopy and endotracheal intubation technique, changes in all parameters measured in the LMA technique were significantly lower than other methods and make the technique suitable to prevent hemodynamic responses.10,23,24]
Our study compared the efficacy of the two intubation techniques on arterial oxygen saturation and found that no significant difference appeared after the induction between the two groups. The overall success rate of intubation in the two study groups was up to 94% and this rate was significantly higher in VL group. Based on other studies, the success rates of bougie have been reported to range from 74% to 99% in difficult intubation.25 In a study by Shah et al.26 to determine the success rate of endotracheal intubation in the emergency department using a plastic bougie, the device was found to have a success rate of 73.7% when used as a means of airway management in patients with difficult airways.
However, this study has some limitations. We cannot conduct a double-blinded study to remove the diagnosis and patients biases together. Moreover, did not offer any convincing justification for these results, which have not been found in other studies. The advantages and disadvantages of various intubation techniques in different situations were examined in another study, which described the use of VL as a means of improving the speed of intubation and the rate of successful intubation in difficult and emergency situations and giving a good view of the glottis.20 There are, however, some advantages and disadvantages (including complexity, uncertainty, high cost and limited availability) as with every technique or device, which shows a different success rate, depending on its different characteristics in any circumstances. However, we must finally choose our technique of intubation according to the situation because no one method is necessarily well suited to every situation.
In summary, the efficacy of intubation with VL and the LMA with bougie techniques on the heart rate and the incidence of airway complications such as postoperative sore throat and laryngospasm have no significant difference regarding to complication and pain. Nevertheless, a lower level of postoperative cough and laryngospasm was measured in the VL group and VL technique was easier, had a shorter intubation time than the method using LMA and bougie. However, laryngospasm tend to be less in VL but not differ significantly with LMA. However, both techniques have their own advantages and disadvantages, and LMA with bougies can be used for intubation in patients with difficult airways in cases where the other option (VL technique) is not available.
Acknowledgments
The researchers would like to thank the Clinical Research Center of Valiasr Hospital in Arak and the Deputy of Research of Arak University of Medical Sciences for assistance in developing this research.
Footnotes
Conflicts of interest
None declared.
Research ethics
The study protocol was approved by the ethical committee of Arak University of Medical Sciences (approval number IR.ARAKMU.RRC.1394.43). The study followed international and national regulations in accordance with the Declaration of Helsinki. The trial was registered with Iranian Registry Clinical Trial (identifier: IRCT2015102214056N6).
Data sharing statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
Open peer reviewers:
Ozan Akca, University of Louisville, USA; Takkin Lo, Loma Linda University, USA
Funding: This work was supported by Arak University of Medical Sciences (No. 2184).
REFERENCES
- 1.Miller RD, Eriksson LI, Fleisher LA, Wiener-Kronish JP, Young WL. Miller's Anesthesia. Philadelphia, PA, USA: Elsevier Health Sciences; 2009. [Google Scholar]
- 2.Nicholson A, Cook TM, Smith AF, Lewis SR, Reed SS. Supraglottic airway devices versus tracheal intubation for airway management during general anaesthesia in obese patients. Cochrane Database Syst Rev. 2013:CD010105. doi: 10.1002/14651858.CD010105.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xue FS, Liao X, Liu HP, Xiong J, Yuan YJ, Liu JH. Use of the gum elastic bougie during endotracheal intubation in emergent patients with difficult airways. J Emerg Med. 2015;48:472–473. doi: 10.1016/j.jemermed.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 4.Vaida SJ, Gaitini D, Ben-David B, Somri M, Hagberg CA, Gaitini LA. A new supraglottic airway, the Elisha Airway Device: a preliminary study. Anesth Analg. 2004;99:124–127. doi: 10.1213/01.ANE.0000123492.26499.63. [DOI] [PubMed] [Google Scholar]
- 5.Kaplan A, Crosby GJ, Bhattacharyya N. Airway protection and the laryngeal mask airway in sinus and nasal surgery. Laryngoscope. 2004;114:652–655. doi: 10.1097/00005537-200404000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Shin SD, Ahn KO, Song KJ, Park CB, Lee EJ. Out-of-hospital airway management and cardiac arrest outcomes: a propensity score matched analysis. Resuscitation. 2012;83:313–319. doi: 10.1016/j.resuscitation.2011.10.028. [DOI] [PubMed] [Google Scholar]
- 7.Tanabe S, Ogawa T, Akahane M, et al. Comparison of neurological outcome between tracheal intubation and supraglottic airway device insertion of out-of-hospital cardiac arrest patients: a nationwide, population-based, observational study. J Emerg Med. 2013;44:389–397. doi: 10.1016/j.jemermed.2012.02.026. [DOI] [PubMed] [Google Scholar]
- 8.Combes X, Sauvat S, Leroux B, et al. Intubating laryngeal mask airway in morbidly obese and lean patients: a comparative study. Anesthesiology. 2005;102:1106–1109. doi: 10.1097/00000542-200506000-00008. discussion 5A. [DOI] [PubMed] [Google Scholar]
- 9.Yu SH, Beirne OR. Laryngeal mask airways have a lower risk of airway complications compared with endotracheal intubation: a systematic review. J Oral Maxillofac Surg. 2010;68:2359–2376. doi: 10.1016/j.joms.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 10.Zhang GH, Xue FS, Sun HY, et al. Comparative study of hemodynamic responses to orotracheal intubation with intubating laryngeal mask airway. Chin Med J (Engl) 2006;119:899–904. [PubMed] [Google Scholar]
- 11.Aziz MF, Healy D, Kheterpal S, Fu RF, Dillman D, Brambrink AM. Routine clinical practice effectiveness of the Glidescope in difficult airway management: an analysis of 2,004 Glidescope intubations, complications, and failures from two institutions. Anesthesiology. 2011;114:34–41. doi: 10.1097/ALN.0b013e3182023eb7. [DOI] [PubMed] [Google Scholar]
- 12.Nouruzi-Sedeh P, Schumann M, Groeben H. Laryngoscopy via Macintosh blade versus GlideScope: success rate and time for endotracheal intubation in untrained medical personnel. Anesthesiology. 2009;110:32–37. doi: 10.1097/ALN.0b013e318190b6a7. [DOI] [PubMed] [Google Scholar]
- 13.Powell L, Andrzejowski J, Taylor R, Turnbull D. Comparison of the performance of four laryngoscopes in a high-fidelity simulator using normal and difficult airway. Br J Anaesth. 2009;103:755–760. doi: 10.1093/bja/aep232. [DOI] [PubMed] [Google Scholar]
- 14.Fun WL, Lim Y, Teoh WH. Comparison of the GlideScope video laryngoscope vs. the intubating laryngeal mask for females with normal airways. Eur J Anaesthesiol. 2007;24:486–491. doi: 10.1017/S0265021506002067. [DOI] [PubMed] [Google Scholar]
- 15.Evans A, Morris S, Petterson J, Hall JE. A comparison of the Seeing Optical Stylet and the gum elastic bougie in simulated difficult tracheal intubation: a manikin study. Anaesthesia. 2006;61:478–481. doi: 10.1111/j.1365-2044.2006.04539.x. [DOI] [PubMed] [Google Scholar]
- 16.Malik MA, O'Donoghue C, Carney J, Maharaj CH, Harte BH, Laffey JG. Comparison of the Glidescope, the Pentax AWS, and the Truview EVO2 with the Macintosh laryngoscope in experienced anaesthetists: a manikin study. Br J Anaesth. 2009;102:128–134. doi: 10.1093/bja/aen342. [DOI] [PubMed] [Google Scholar]
- 17.Kaplan MB, Ward DS, Berci G. A new video laryngoscope-an aid to intubation and teaching. J Clin Anesth. 2002;14:620–626. doi: 10.1016/s0952-8180(02)00457-9. [DOI] [PubMed] [Google Scholar]
- 18.Healy DW, Maties O, Hovord D, Kheterpal S. A systematic review of the role of videolaryngoscopy in successful orotracheal intubation. BMC Anesthesiol. 2012;12:32. doi: 10.1186/1471-2253-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weiss M, Schwarz U, Dillier CM, Gerber AC. Teaching and supervising tracheal intubation in paediatric patients using videolaryngoscopy. Paediatr Anaesth. 2001;11:343–348. doi: 10.1046/j.1460-9592.2001.00681.x. [DOI] [PubMed] [Google Scholar]
- 20.Niforopoulou P, Pantazopoulos I, Demestiha T, Koudouna E, Xanthos T. Video-laryngoscopes in the adult airway management: a topical review of the literature. Acta Anaesthesiol Scand. 2010;54:1050–1061. doi: 10.1111/j.1399-6576.2010.02285.x. [DOI] [PubMed] [Google Scholar]
- 21.Shippey B, Ray D, McKeown D. Use of the McGrath videolaryngoscope in the management of difficult and failed tracheal intubation. Br J Anaesth. 2008;100:116–119. doi: 10.1093/bja/aem303. [DOI] [PubMed] [Google Scholar]
- 22.Rai MR, Dering A, Verghese C. The Glidescope system: a clinical assessment of performance. Anaesthesia. 2005;60:60–64. doi: 10.1111/j.1365-2044.2004.04013.x. [DOI] [PubMed] [Google Scholar]
- 23.Perelló-Cerdà L, Fàbregas N, Lopez AM, et al. ProSeal Laryngeal Mask Airway Attenuates Systemic and Cerebral Hemodynamic Response During Awakening of Neurosurgical Patients: A Randomized Clinical Trial. J Neurosurg Anesthesiol. 2015;27:194–202. doi: 10.1097/ANA.0000000000000108. [DOI] [PubMed] [Google Scholar]
- 24.Montazari K, Hashemi KNSJ. Comparison of hemodynamic changes after insertion of laryngeal mask airway, facemask and endotracheal intubation. Acta Med Iran. 2004;42:437–440. [Google Scholar]
- 25.Baker JB, Maskell KF, Matlock AG, Walsh RM, Skinner CG. Comparison of Preloaded Bougie versus Standard Bougie Technique for Endotracheal Intubation in a Cadaveric Model. West J Emerg Med. 2015;16:588–593. doi: 10.5811/westjem.2015.4.22857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shah KH, Kwong BM, Hazan A, Newman DH, Wiener D. Success of the gum elastic bougie as a rescue airway in the emergency department. J Emerg Med. 2011;40:1–6. doi: 10.1016/j.jemermed.2008.04.045. [DOI] [PubMed] [Google Scholar]


