Abstract
Mild traumatic brain injury (TBI) persistent post-concussion syndrome (PPCS) and post-traumatic stress disorder (PTSD) are epidemic in United States Iraq and Afghanistan War veterans. Treatment of the combined diagnoses is limited. The aim of this study is to assess safety, feasibility, and effectiveness of hyperbaric oxygen treatments (HBOT) for mild TBI PPCS and PTSD. Thirty military subjects aged 18–65 with PPCS with or without PTSD and from one or more blast-induced mild-moderate traumatic brain injuries that were a minimum of 1 year old and occurred after 9/11/2001 were studied. The measures included symptom lists, physical exam, neuropsychological and psychological testing on 29 subjects (1 dropout) and SPECT brain imaging pre and post HBOT. Comparison was made using SPECT imaging on 29 matched Controls. Side effects (30 subjects) experienced due to the HBOT: reversible middle ear barotrauma (n = 6), transient deterioration in symptoms (n = 7), reversible bronchospasm (n = 1), and increased anxiety (n = 2; not related to confinement); unrelated to HBOT: ureterolithiasis (n = 1), chest pain (n = 2). Significant improvement (29 subjects) was seen in neurological exam, symptoms, intelligence quotient, memory, measures of attention, dominant hand motor speed and dexterity, quality of life, general anxiety, PTSD, depression (including reduction in suicidal ideation), and reduced psychoactive medication usage. At 6-month follow-up subjects reported further symptomatic improvement. Compared to Controls the subjects' SPECT was significantly abnormal, significantly improved after 1 and 40 treatments, and became statistically indistinguishable from Controls in 75% of abnormal areas. HBOT was found to be safe and significantly effective for veterans with mild to moderate TBI PPCS with PTSD in all four outcome domains: clinical medicine, neuropsychology, psychology, and SPECT imaging. Veterans also experienced a significant reduction in suicidal ideation and reduction in psychoactive medication use.
Keywords: hyperbaric oxygen, traumatic brain injury, persistent post concussion syndrome, post traumatic stress disorder, single photon emission computed tomography, cognitive assessment, brain injury treatment, combat veterans
INTRODUCTION
Blast-induced traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD) remain the two most common afflictions of U.S. military service personnel who served in the Iraq and Afghanistan Wars. A Rand Report1 estimates that 300,000 (18.3%) of 1.64 million military service members who have deployed to these war zones have PTSD or major depression and 320,000 (19.5%) have experienced a TBI. Overall, approximately 546,000 have one of the three diagnoses and 82,000 have symptoms of all three [Note: For the present study the authors are using the Rand Report1's definitions of TBI (from the Centers for Disease Control and Prevention 2008): “a trauma to the head that either temporarily or permanently disrupts the brain's function,” mild TBI (mTBI): “a Glasgow Coma Scale of 13-15… (The Glasgow Coma Scale is a 15 point scale that measures a patient's best eye-opening, motor, and verbal responses),” and PTSD: “an anxiety disorder that occurs after a traumatic event in which a threat of serious injury or death is experienced or witnessed and to which the individual's response involved intense fear, helplessness, or horror.” mTBI disruption of brain function lasting longer than 3–6 months is the persistent post-concussion syndrome (PPCS), according to Diagnostic and Statistical Manual IV-Text Revised (DSM-IV-TR) criteria listed in the Methods Section. PPCS is synonymous with the diagnosis of TBI used in military medical reports quoted herein].
The frequency of the combined diagnoses in veterans of mild TBI and PTSD has been estimated at 5–7%.2 With a probable diagnosis of mild TBI the combined diagnosis incidence rises to 33–39%.2 A Walter Reed Army Institute of Research post-deployment survey of 4,618 soldiers reported 15.2% of injuries with history of loss of consciousness or altered mental status.3 That study also found that 43.9% of those with history of loss of consciousness and 27.3% of those with history of altered mental status met criteria for PTSD. Separating the two diagnoses of PPCS and PTSD, however, has been very difficult. When adjustments were made for PTSD and depression by logistic regression analysis, the only symptom unique to mild TBI was headache. Due to this difficulty in differentiation no attempt was made to separate the two diagnoses in this study based on symptoms alone.
Evidence-based treatment for PTSD exists, but problems with access to and quality of treatment have been problematic in the military.1 Treatment of the chronic symptomatic manifestation of mild TBI, the PPCS, is limited. Most of TBI rehabilitation and medical management is based primarily on expert opinion.1 Treatment consists of off-label use of Food and Drug Administration (FDA) blackbox-labeled psychoactive medications, counseling, stimulative, and adaptive strategies.
Hyperbaric oxygen therapy (HBOT) is the use of increased atmospheric pressure and hyperoxia as drugs to treat disease pathophysiology through gene expression and suppression.4,5 Treatment effects are a function of dose and timing of intervention in the disease process. Historically, HBOT doses of 203–304 kPa have been applied to 15 typically reimbursed acute or chronic wound and infection diagnoses.5,6,7 Lesser doses have been used mainly for chronic neurological conditions.8
Oxygen toxicity9,10 is a concern in the testing of hyperbaric oxygen to treat PPCS and PTSD. The most extreme form of oxygen toxicity is a grand mal seizure.9,10 A study of HBOT on sub-acute moderate to severe TBI at 203 kPa11 reported a 9% seizure rate. Less severe toxic/harmful effects12 were demonstrated in the Wolf et al.13 blast-induced mTBI/PPCS study using a dose of 243 kPa. At doses less than 203 kPa, side effects and toxicity in chronic brain injury patients have been noted only with prolonged courses of HBOT, i.e., 70–500 treatments.14
Low-pressure HBOT has been applied to chronic traumatic brain wounding in moderate and severe TBI cases15,16,17,18,19,20,21,22,23 and replicated in a controlled animal study.24 The first HBOT-treated cases of mild TBI were in patients with blast-induced PPCS with25 or without26 PTSD. Clinical and cognitive improvements in a series of subsequent off-label cases in 2008 prompted the present study to assess safety and feasibility, and assess outcomes with standard cognitive testing and functional brain imaging. In all of the early cases and those of other neurological disorders the improvements noted after HBOT were captured on single photon emission computed tomography (SPECT) brain imaging with an improvement in the texture of the scans manifest as a visual smoothing of an abnormal pattern of brain blood flow to the pattern of blood flow seen in neurologically normal people. This study attempted to capture this smoothing pattern mathematically with a texture analysis. In addition, since the publication of the preliminary results of the present study27 other authors have reported similar13,28,29,30 results with similar28,30 and different13,29 doses of hyperbaric therapy, and conflicting results,12,29,31,32 using different doses of hyperbaric therapy. The prior report of preliminary data27 noted that the findings needed confirmation with larger numbers and a stronger design. This report confirms and strengthens the previous findings with a larger number, a 6-month symptom follow-up, and the addition of a SPECT control group.
SUBJECTS AND METHODS
Design
This is a prospective case-control institutional review board approved pilot study. The original design was for 15 active duty or retired military service members with mild-moderate blast TBI PPCS and 15 service members with mild-moderate TBI PPCS and PTSD. Early recruitment was dominated by patients with the combined diagnoses so the study design was changed to recruitment of the first 30 subjects with either PPCS or PPCS with PTSD. The final treated subject cohort was matched to a group of anonymized SPECT imaged population controls from a previous study (unpublished data).
The study methods were described in a previous report.27 Subjects were screened, enrolled, examined, completed symptom questionnaires, neuropsychological and psychological testing, and SPECT imaged before and after the first HBOT and then within 5 days after the full series of twice a day, 5 days per week HBOTs at 152 kPa/60 minutes. Six months following the 40th HBOT, subjects responded to a phone questionnaire. Subject flow is shown in Figure 1.
Figure 1.
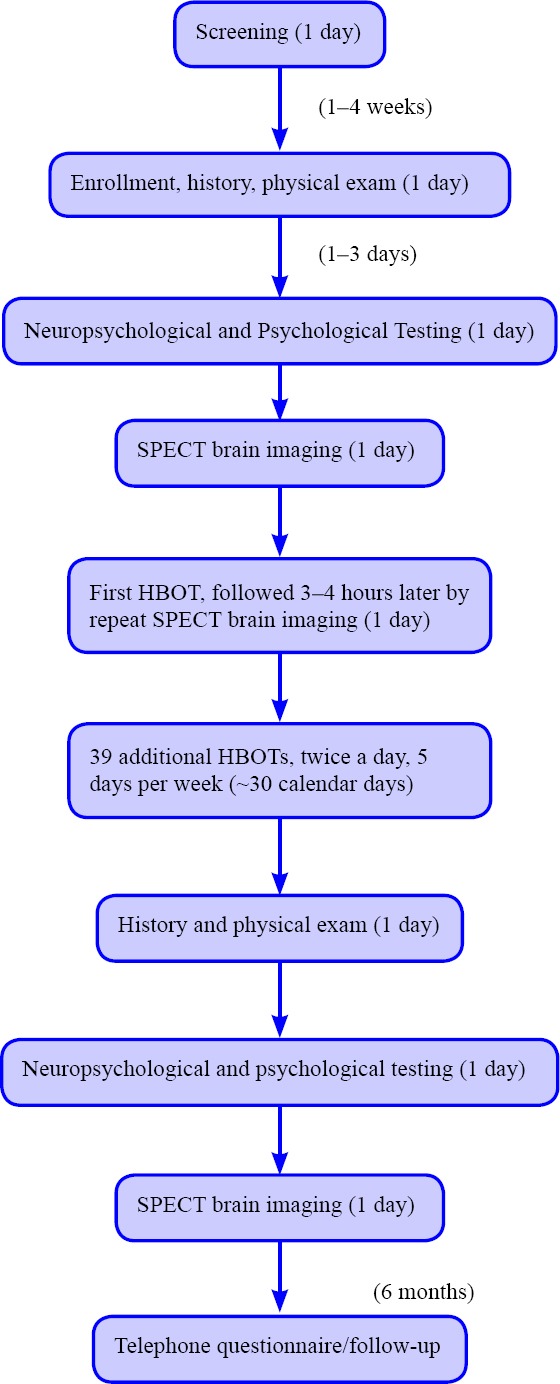
Flow chart of the study.
Subjects
There were 30 active duty or retired military service men and women (18–65 years old) with one or more mild-to-moderate blast TBIS characterized by loss of consciousness that were a minimum of 1 year old and occurred after 9/11/01. All subjects were diagnosed by military or civilian specialists with chronic TBI/PPCS or TBI/PPCS/PTSD. Loss of consciousness (LOC) was estimated by each patient and the principal investigator (P.I.) based on patient recollection, details of the event, and bystander reports to patient. When anterograde memory loss exceeded 30 minutes, could not be distinguished from LOC, and medical records were not available subjects were deemed moderate TBI. Prior diagnoses of TBI/PPCS and PTSD were confirmed or refuted by using clinical interviews, symptom lists, the rivermead post concussion symptoms questionnaire33 (PCS; > 3 on at least 3 questions),34 the PTSD Checklist-Military35 (total > 50),1 and diagnostic and Statistical Manual-IV Text Revised (DSM-IV TR) criteria for the diagnoses.36 All subjects and population normals gave informed consent under approval of the louisiana state university institutional review board, LSU IRB #7051 (Clinicaltrials.gov identifier: NCT00760734) and LSU IRB #3511, respectively.
The DSM-IV-TR criteria used for diagnosis of PPCS was:
1) a history of head trauma that has caused significant cerebral concussion;
2) evidence from neuropsychological testing or quantified cognitive assessment of difficulty in attention (concentrating, shifting focus of attention, performing simultaneous cognitive tasks), or memory (learning or recalling information);
3) three or more of the following occur shortly after the trauma and last at least 3 months: a) Becoming fatigued easily, b) Disordered sleep, c) Headache, d) Vertigo or dizziness, e) Irritability or aggression with little or no provocation, f) Anxiety, depression, or affective lability, g) Changes in personality (e.g., social or sexual inappropriateness), h) Apathy or lack of spontaneity;
4) the symptoms in criteria 2) and 3) have their onset following head trauma or else represent a substantial worsening of pre-existing symptoms;
5) the disturbance causes significant impairment in social or occupational functioning and represents a significant decline from a previous level of functioning (in school-aged children, the impairment may be manifested by a significant worsening in school or academic performance dating from the trauma);
6) the symptoms do not meet criteria for dementia due to head trauma and are not better accounted for by another mental disorder (e.g., amnestic disorder due to head trauma, personality change due to head trauma).36
Exclusion Criteria: Subjects with significant pulmonary disease, medical co-morbidities with significant risk for HBOT or that confounded testing, claustrophobia, pre-morbid neurological diagnoses, and substance abuse were excluded. subjects were counseled to give maximal effort and effort-tested Pre-HBOT, but those who scored below accepted cutoffs were not excluded from the study. bronchospasm unresponsive to medication was the sole criteria for subject removal.
Symptom scoring
Patient-prioritized symptoms and symptoms from the P.I.'s standard questionnaire27 (Additional Table 1 (125.6KB, pdf) ) were recorded pre-treatment and scored by the subject after the last HBOT as “better” (improved), “worse” (deteriorated), or “same” (no change). Six months following the last HBOT subjects were queried by phone about the status of all symptoms as “better, worse, or same” compared to pre-HBOT and post-40 HBOTs.
List and Schedule of Psychometric Measures, When Administered, and Domain Measured
Psychometric testing
Outcome variables are listed in Additional Table 1 (125.6KB, pdf) and include: Wechsler Adult Intelligence Scale-IV Full Scale IQ (WAIS-IV),37 Wechsler Abbreviated Scale of Intelligence (WASI),38 Wechsler Memory Scale-IV Delayed Memory Index and Visual Working Memory Index (WMS-IV),39 Rivermead Post Concussion Symptom Questionnaire (RPCSQ),33 Test of Variables of Attention (TOVA),40 the Stroop Test,41 Finger Tapping and Grooved Pegboard Tests,42 the Paragraph memory subtest of the Rivermead Behavioural Memory Test,43 PTSD Checklist-Military (PCL-M),35 the Perceived Quality of Life (PQOL),44 Generalized Anxiety Disorder Scale (GAD-7),45 the Patient's Health Questionnaire (PHQ-9),46 and the Percent Back To Normal Ratings (PBTN)47 for cognitive, emotional, and physical functioning. These measures were administered before and after completing the 40 HBOT treatments. The Michigan Alcohol Screening Test (MAST),48 Drug Abuse Screening Test (DAST),49 Green Word Memory Test (WMT),50 Wechsler Test of Adult Reading (WTAR),51 the Combat Experience Scale (CES),52 and the Disability Rating Scale53 were administered pre-treatment only. Choice of tests was guided by past experience and the medical literature. Practice and test/retest effects were minimized or accounted for by using alternate tests, e.g. WAIS-IV on pre-test and WASI post-test, and by including the Reliable Change Analysis on the WMS-IV primary outcome variables of Delayed Memory Index and Visual Working Memory Index (the first 5 subjects were tested with the WAIS III, after which the newly issued WAIS IV was used for the remaining 26 subjects).
SPECT brain blood flow imaging
Subjects underwent SPECT brain blood flow imaging on a Picker Prism 3000 XP Triple-Head gamma camera system (Cleveland, Ohio, USA) before, within 3–4 hours after the first HBOT, and within five days after the 40th HBOT. Acquisition, processing, and formatting were previously described.27 Control subjects were imaged between 1998 and 2002 under identical conditions with the same radiopharmaceutical/dose in the same nuclear medicine department on an earlier model Picker Prism 3000 XP Triple-Head gamma camera system. The raw data from their scans was re-processed and re-formatted by the same technologist in identical fashion to treated subjects using the software on the later model Picker XP.
SPECT texture analysis
Transverse processed images were analyzed with open source DICOM software package OsirixTM, using a first order texture analysis of count histograms54 to register improvements in heterogeneity of blood flow55 seen in previously treated chronic TBI subjects.15 Mean counts/pixel (MCP), standard deviation of counts/pixel, and coefficient of variation (CV) (standard deviation as a percent of mean) of counts/pixel were measured for five gray and two white matter circular regions of interest (ROIs) at designated sites in each hemisphere on all three scans for each patient and then separately for the individual scans for the Controls.27 The nuclear technologist was not blinded to group or sequence of scans. Averages were determined for each ROI of each measured parameter for Control and pre-HBOT scans, compared to each other, and to post-1 and post-40 HBOT scans. Statistical analysis was performed as described below. A decrease in CV (improvement in texture) was the primary SPECT outcome.
SPECT three-dimensional surface reconstruction
Three-dimensional reconstruction was performed by a single nuclear technologist using the method developed by Picker International using Picker software whereby brain blood flow is computer indexed to frontal lobe blood flow. A frontal lobe surface defect was identified on a selected transverse slice. Processed/filtered transverse slices were then featured with a 100% window such that all pixels render a white image. Counts were slowly subtracted by decreasing the window threshold until the defect was visible as a full thickness black defect in the contour of the cortex. As the defect emerged and was registered in proper anatomic proportion to the rest of frontal cortical blood flow the numerical window level was taken as the determination threshold for the entire brain. Three separate determinations were made for each scan and the final threshold taken as an average of the three determinations. The technologist was blind to the final image reconstruction due to software restrictions that only allow threshold determination, but not blind to dates of scans. Color is aesthetic.
HBOT
HBOT was performed in monoplace hyperbaric chambers on a protocol the investigators developed in 1989.15 Patients were compressed and decompressed at 1–2 pound per square inch on 100% oxygen to 152 kPa for 60 minutes total dive time, twice/day with a 3–4 hours surface interval, 5 days/week, for 40 HBOTs.
Statistical analysis
Values of psychometric tests were acquired pre-HBOT and post-40 HBOTs; SPECT parameters were acquired pre-HBOT, post-1 HBOT, and post-40 HBOTs. For each SPECT ROI at each time point mean, standard deviation, median, range (minimum and maximum), and 95% confidence interval around the estimated mean were calculated for mean of counts/pixel, standard deviation of counts/pixel, and CV of counts/pixel. Changes in psychometric and SPECT parameters between pairs of time points (pre-HBOT to post-1-HBOT, pre-HBOT to post-40-HBOTs, and post-1-HBOT to post-40-HBOTs) were similarly summarized, using the Tinn-R version 2.3.7.1 (http://tinn-r.soft112.com), with the inclusion of a nominal P-value indicating whether or not the mean change was significantly different from zero. The P values were obtained by the paired Student t test if the changes were nearly normally distributed, or by the non-parametric Wilcoxon Signed-Ranks test if the changes were significantly non-normally distributed by the Anderson-Darling test. No multiplicity adjustments were applied to P values in this exploratory study; all P values should be considered descriptive, not inferential. One subject who withdrew before completion of treatment and post-treatment testing was included in the demographic data and safety/feasibility analysis, but excluded from the per-protocol analysis (outcome testing). Reliable Change Score analysis (Wechsler Advanced Clinical Practice software) to assess practice and/or test-retest effect was performed on Visual Working Memory Index (VWMI) and Delayed Memory Index (DMI) of the Wechsler Memory Scale-IV.39
RESULTS
Demographics of samples
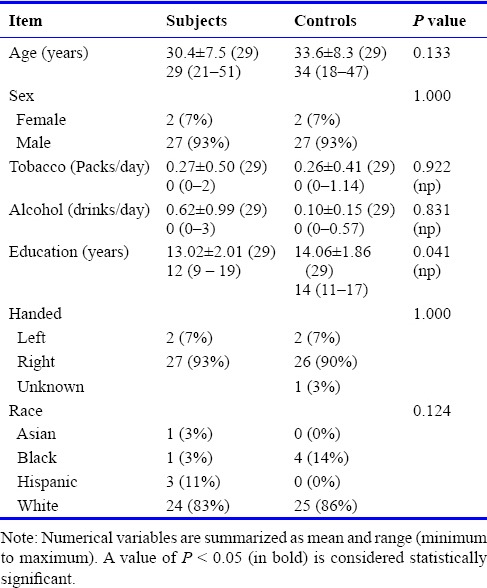
Recruitment began 9/17/2008 and ended 8/15/2010 with the enrollment of 30 subjects. Six-month followup ended 3/23/2011. Sample demographics are reported in Table 1 (Subject Demographics) for the 30 enrolled subjects and Table 2 (Subject and Control Characteristics) for the 29 subjects who completed the protocol along with 29 matched SPECT Controls. One subject withdrew from the study due to an ear infection, bronchospasm, and middle ear barotrauma; he was excluded from all data analyses. The only significant difference between subjects and Controls was years of formal education (greater for Controls); however, many study subjects had military and trade school education/training that was not counted.
Table 1.
Subject demographics of mild traumatic brain injury persistent post-concussion syndrome with or without post-traumatic stress disorder
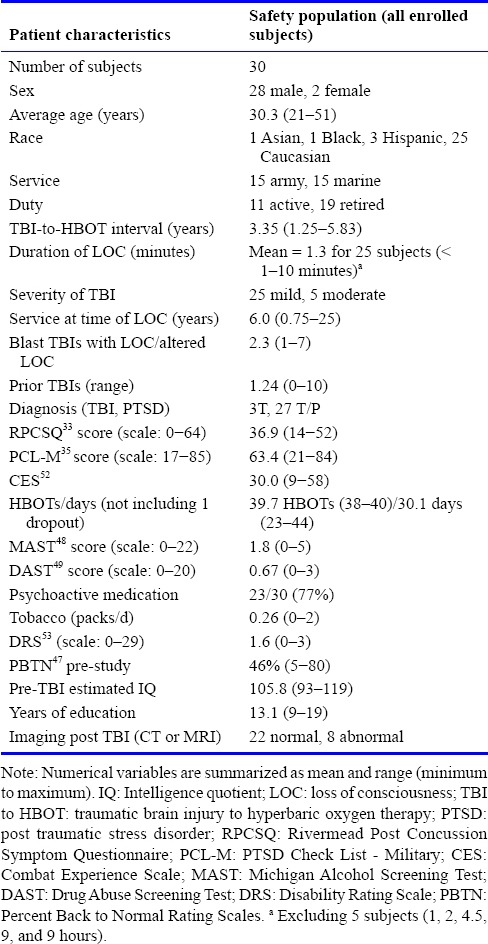
Table 2.
Subject and control characteristics (29 subjects)
Symptoms
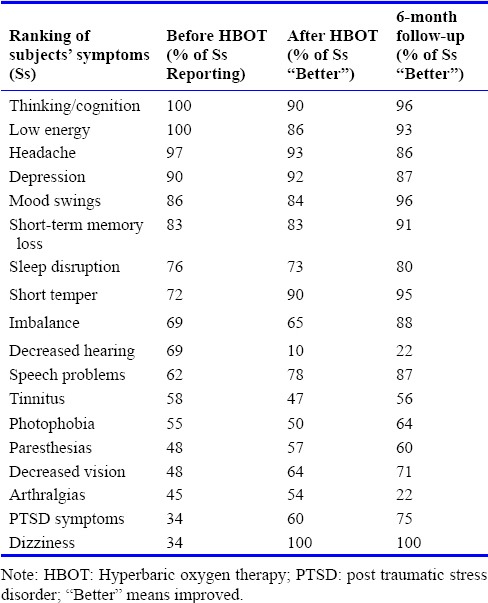
Symptom outcomes immediately and 6 months post treatment are reported in Table 3 (symptoms before, immediately after, and 6 months after treatment). Dizziness, present in only 34% of subjects, was the most responsive of all symptoms, improving in 100% of subjects. The 75–100% of the 29 subjects reported problems with thinking, low energy, headaches, depression, mood swings, short-term memory loss, and a disruption of their sleep; 73–93% of these subjects experienced improvement after 40 HBOTs. Decreased hearing and tinnitus were the least responsive symptoms. The 28 of 29 subjects (97%) responded to 6-month phone follow-up and reported further improvement in 14/18, deterioration in 3/18, and no change in 1/18 symptom(s) in Table 3. Fifty percent (11/22) of subjects who were on psychoactive or analgesic prescription medication before HBOT decreased or discontinued their medication usage during HBOT; four others discontinued their medication prior to treatment and were able to maintain their abstinence from medication by the end of treatment. One subject increased narcotic medication due to worsened back pain and another subject increased Trazodone for sleep. Two other subjects restarted or transiently initiated benzodiazepines.
Table 3.
Symptoms of mild traumatic brain injury persistent post-concussion syndrome with or without post-traumatic stress disorder before, immediately, and 6 months after treatment
Side effects
Due to the HBOT were: 1) mild reversible middle ear barotrauma (MEBT) (n = 6), five of these at the outset of upper respiratory infections, 2) transient deterioration in some symptoms that resolved over the next 4–6 HBOTs (n = 7), 3) anxiety associated with exacerbation of PTSD (2 subjects, one of which had chest pain/gastroesophageal reflux), and 4) bronchospasm (n = 1). Increased anxiety was not due to confinement. Side effects unrelated to the HBOT were: 1) non-cardiac chest pain (n = 2), 2) recurrent ureterolithiasis (n = 1). Four of these side effects (anxiety-2, exacerbation of headache-1, and ureterolithiasis-1) were considered significant adverse events per protocol definition due to a hospital emergency department visit. Anxiety was treated with re-institution of clonazepam in one subject and a time-limited lorazepam prescription in the other. One subject, bronchospasm patient above, dropped out due to a bullous myringitis, and time limitations in New Orleans. Eleven subjects experienced protocol breaks due primarily to adverse events (above); 10 of these 11 finished the protocol.
Psychometric measures
A summary of pre- to post-HBOT neuropsychological (IQ, memory, attention) and psychological (PTSD, depression, Quality of Life) outcomes are shown in Table 4 (Summary of pre- to post-HBOT neuropsychological and psychological outcomes). Significant improvement was recorded on 7 of 13 cognitive measures, one measure showed a trend toward improvement, and the other 5 showed no significant change.
Table 4.
Summary of pre- to post-HBOT neuropsychological and psychological outcomes
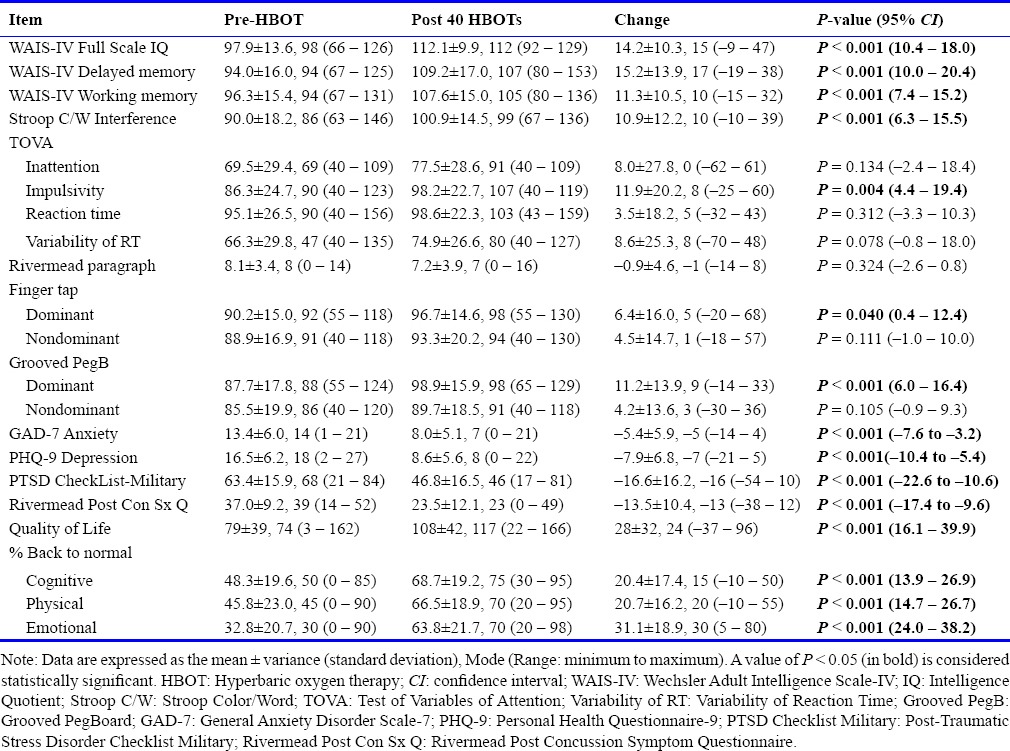
Full Scale IQ, Visual Working Memory, Delayed Memory, and Stroop Test showed the largest improvements at P < 0.001, and one measure of attention improved, TOVA Impulsivity (P = 0.004). Reliable Change Score analysis on the 24 subjects with WMS IV showed significant changes in Visual Working Memory Index (P = 0.003) and Delayed Memory Index (P = 0.029)
Subjects experienced significant improvement in anxiety, depression, post-concussion symptoms, and self-assessed cognitive, physical, and emotional functioning. After HBOT 12 of 23 subjects (52%) no longer met the PCL-M threshold criteria for diagnosis of PTSD,1 experiencing an average 18.8-point reduction in the PCL-M. Ten of 12 subjects who expressed suicidal ideation prior to the HBOT did not express suicidal thoughts after treatment (McNemar's Test; P = 0.012). One subject with anxiety and an adverse event (emergency department visit for increased anxiety) during treatment had increased suicidal ideation after treatment. Eighteen of the 24 subjects (75%) who indicated significant anxiety on several items of the GAD-7 before treatment were no longer anxious after treatment (McNemar's Test; P < 0.0001). One subject who was not anxious pre-treatment expressed increased anxiety post-treatment.
Four subjects failed the Green Word Memory effort test (score < 82.5% for the 3 primary subtests), however, their pre-HBOT PCL-M scores were significantly higher than the other 25 subjects (80 vs. 61, P = 0.022). Re-analysis of demographic data (Table 2) and Table 4 data without these 4 subjects (Additional file 1 (241.5KB, pdf) ) changed the Finger Tapping Dominant Hand result from significantly positive to a positive trend and the TOVA Variability RT from a positive trend to non-significant, and showed that the subjects who failed the WMT had a greater delay to treatment and greater increase in FSIQ after HBOT than those who passed the WMT.
Re-Analysis of All Variables by Green Pass/Fail
Medication increase/decrease or sleep improvement during/immediately after HBOT and sleep improvement 6 months after HBOT had minimal effect on outcome instruments (Additional file 2 (221.6KB, pdf) ). Contribution of moderate TBI subjects to the data pool was analyzed in Additional file 3 (162.3KB, pdf) . A greater percentage of moderate TBI subjects were Asian or Black and decreased the dosage or discontinued their psychoactive medications by the conclusion of HBOT than the mild TBI subjects.
Association of Improvements in Sleep and Medication with Changes in NeuroPsych and SPECT Variables
Contribution of Moderate TBI to Composite Data.
SPECT brain blood flow imaging
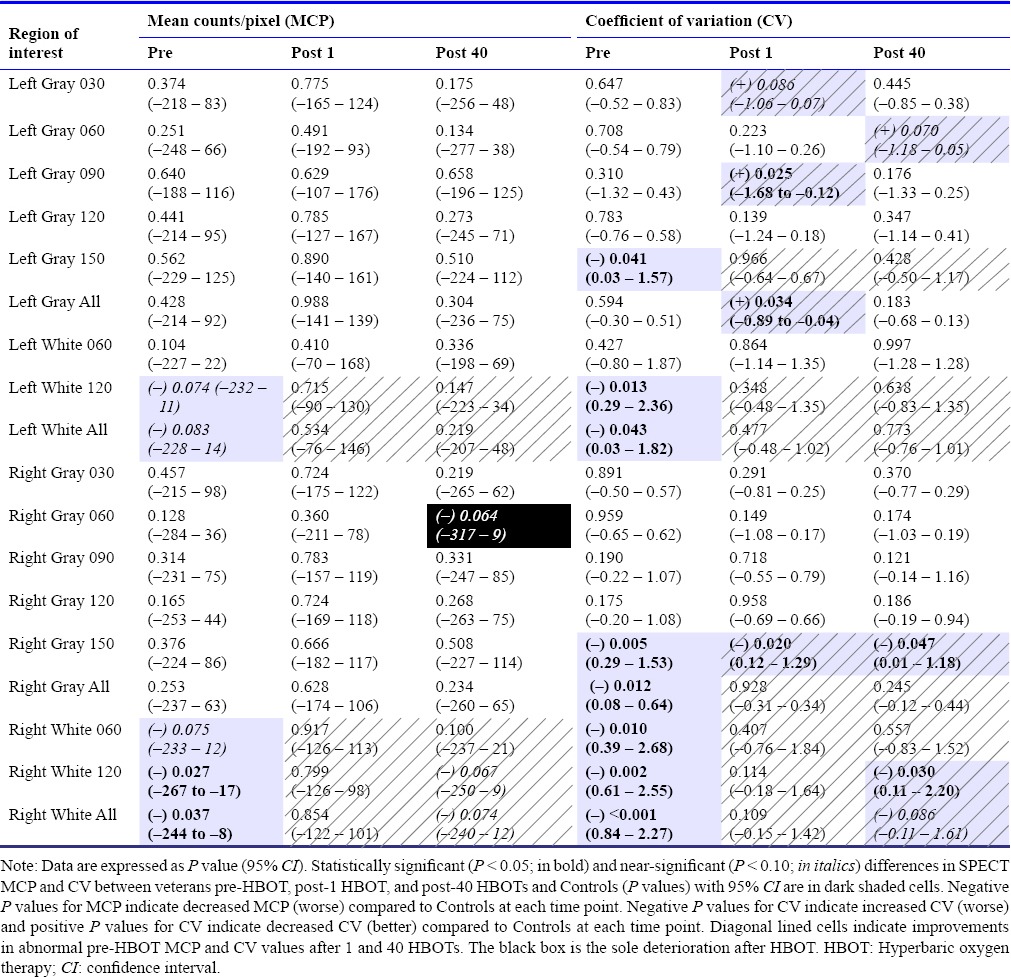
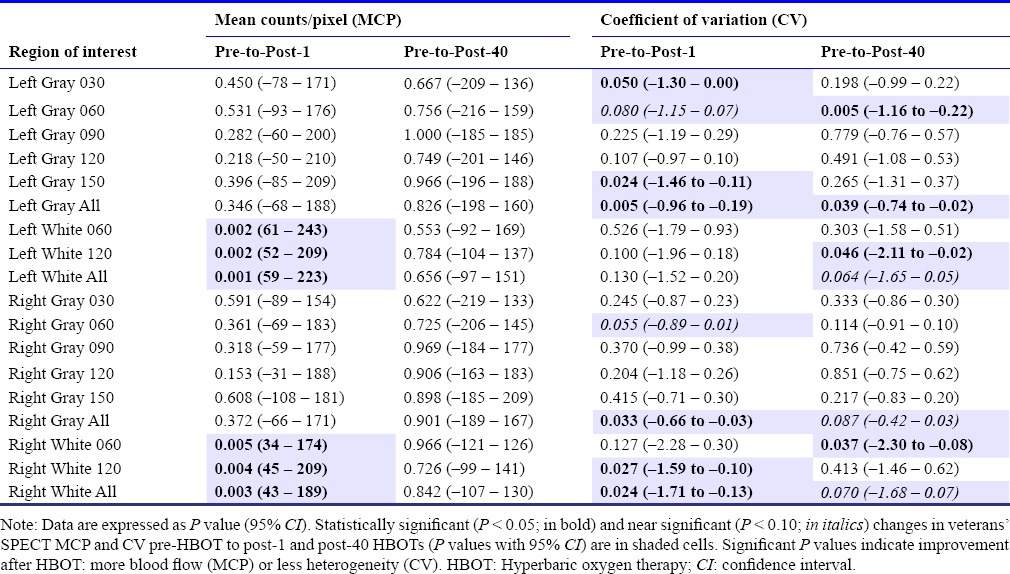
Significantly and near-significantly different values for SPECT MCP and CV between veterans pre-HBOT and Controls, changes in veteran SPECT MCP and CV after one and 40 HBOTs, and changes in veterans SPECT MCP and CV after 1 and 40 HBOTs compared to Controls were abstracted from full data sets in Additional files 4 (169.7KB, pdf) , 5 (279.4KB, pdf) and presented in Tables 5–7.
Table 5.
Brain blood flow and texture assessment of brain blood flow in veterans compared to Controls
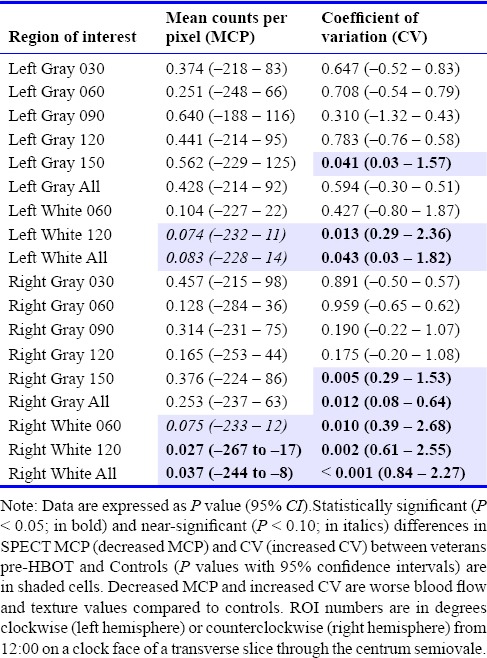
Table 7.
Comparison of veterans’ brain blood flow and texture of brain blood flow to Controls before, after 1, and after 40 HBOTs.
Analysis of SPECT Data
Approach of SPECT MCP and CV at baseline, post-1 HBOT, and post-40 HBOTs to Control Subjects’ MCP and CV
Compared to Controls, brain blood flow (MCP) and texture (CV) in veterans pre-HBOT (Table 5) were worse, giving the visual appearance of a coarsely heterogeneous pattern. After 1 and 40 HBOTs veterans' SPECT texture improved while blood flow improved only after one HBOT, (Table 6), demonstrating the more normal visual smoothing pattern. Compared to Controls (Table 7), abnormal veterans' white matter blood flow pre-HBOT improved after 1 and 40 HBOTs, becoming statistically indistinguishable from Controls, while abnormal texture improved after 1 and 40 HBOTs in all eight abnormal ROIs, becoming statistically indistinguishable from Controls in 75% of abnormal ROIs. In addition, after 1 and 40 HBOTs veterans showed improved texture in ROIs that were not significantly different from Controls pre-HBOT. Overall, after 1 and 40 HBOTs veterans' abnormal SPECT brain scans showed a progression to a more normal visually smooth pattern of blood flow.
Table 6.
Changes in veterans’ brain blood flow and texture of brain blood flow after 1 and 40 HBOTs
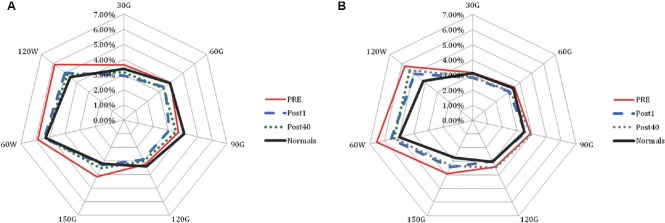
Radar graphs of SPECT data from Additional file 4 (169.7KB, pdf) , from which P values in Table 7 are derived, are presented in Figure 2. A visual representation of the texture change towards a normal pattern of blood flow on the radar graphs for a sample veteran before and after HBOT compared to a sample Control subject is presented in both transverse slices and three dimensional surface reconstructions in Figure 3.
Figure 2.
Radar graph of left (A) and right (B) hemisphere.
Note: Average CV for each ROI of Controls (Normals) vs. Veterans (Pre, Post 1, and Post 40 HBOTs). Error bars omitted for viewing clarity. CV: Coefficient of variation; ROI: region of interest.
Figure 3.
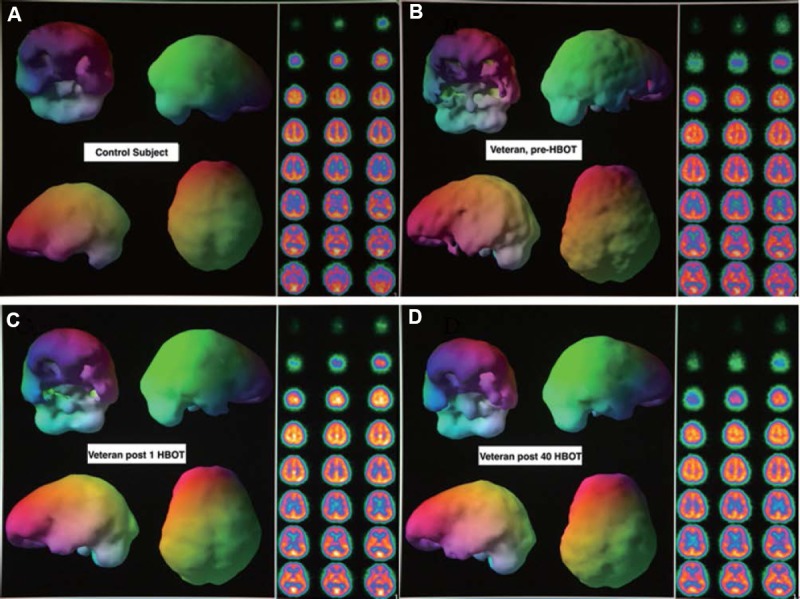
Transverse zoom slices and three-dimensional surface reconstruction of control subject (A) and veteran pre-HBOT (B), after 1 HBOT (C), after 40 HBOTs (D) SPECT brain blood flow scan.
Note: Colors for the slices represent gradations of blood flow from highest to lowest: white, yellow, orange, purple, blue, black. Color scheme in the threedimensional reconstructions are aesthetic and embedded in the Picker software.
DISCUSSION
Forty HBOTs at 152 kPa/60 minutes on a twice/day, 5 days/week schedule is feasible and safe with no long-lasting significant adverse events. Of the three significant events related to the HBOT only increased headache has been reported in mTBI/PPCS/HBOT studies.27,30,56 The other two significant adverse events, exacerbation of anxiety, were not collected in a previous report of low-pressure oxygen toxicity effects,14 reported in other studies of HBOT in PPCS and PPCS/PTSD using similar or greater doses of HBOT on a once/day schedule,13,26,28,29,30,31,32 nor reported in other studies of HBOT-induced side effects.6 We suspect they were due to the intense twice a day dosing schedule, as was reversible MEBT (16% of subjects), which occurred during the prodrome and early clinical phase of upper respiratory infections and was likely due to the immunosuppressive effects of HBOT.57 Twice a day dosing may also explain the bronchospasm/reduction in peak flow in one subject and increased anxiety in two PTSD subjects. Pulmonary oxygen toxicity with decrease in small airways conductance58 is typically only seen with higher pressures or prolonged continuous exposures.
The transient symptomatic deterioration at approximately 20 HBOTs is a phenomenon observed in our treatment of other chronic neurological patients that has been incorporated into consent forms. This did not require intervention or discontinuance of treatment. Simultaneously, many other patients reported an improvement in symptoms at this point, also documented in Wolf et al.13 [Figure 2, ImPACT scores at Exposure Interval 5 (20 treatments)]. We speculate that this mid-point in the protocol represents a transition in brain wound adaptation/transformation to the repetitive effects of intermittent hyperoxia and pressure since it corresponds to the time (25 treatments) at which physical changes/improvements were noted in HBOT-treated rats on the same protocol59 and the plateau for the angiogenic phase in HBOT-treated human osteoradionecrosis.60
Effectiveness of HBOT for blast TBI and PTSD
The major findings in this study were: 1) the significant improvements and magnitude of improvements in all outcome instruments (symptoms, cognition, mood, quality of life, and imaging) that were reproducible (strengthened P values) from the first 16 subjects27 to the final 14 subjects, 2) the abnormal brain blood flow pattern that became nearly indistinguishable from Controls after treatment, 3) one of the longest follow-up periods of any HBOT/PPCS study, 4) the increased symptom improvement six months post treatment, and 5) the reduction in suicidal ideation. Effect sizes and confidence intervals were substantial. These findings were mirrored by a reciprocal reduction or elimination of psychoactive and narcotic prescription medication usage, and maintained abstinence from the same medication discontinued immediately pre-HBOT.
Headache is a known marker of TBI PPCS and distinguishes TBI PPCS from PTSD in blast brain-injured U.S. soldiers.3 The significant reduction in headaches suggests treatment of TBI and the organic injury of TBI established by our subjects' loss of consciousness.61,62 It also is consistent with and reaffirms the previous animal work on HBOT in chronic TBI wounding59 at a similar dose of HBOT (152 kPa/90 minutes twice/day, 7 days/week). These findings are similar to the findings in the previously mentioned human experience with moderate to severe chronic TBI,15,16,17,18,19,20,21,22,23 and blast-induced mTBI uncomplicated by PTSD.26 Collectively, they suggest treatment of cerebral wounds from TBI.
The PTSD symptom reduction is one of the greatest reductions in PTSD symptoms in a four-week period with any reported treatment63 and combined with the effect on PPCS outcomes represents the only reported treatment for the combined diagnoses of blast-induced PPCS and PTSD. The 18.8-point reduction in PCL-M is greater than the PCL-M reduction in 13/16 RCTs of second-line interventions in military-related PTSD.64 Half of the subjects no longer met the PCL-M threshold criteria for diagnosis of PTSD. A lesser reduction of PTSD symptoms has been confirmed in all three DoD-funded HBOT studies.13,29,30 Spontaneous recovery of PPCS or PTSD 3.35 years after injury and further improvement in PPCS symptoms 6 months post-treatment is contrary to the natural history of TBI, PTSD, and TBI with PTSD in veterans.65 Coupled with the significant cognitive improvements demonstrated by Reliable Change Score analysis these outcomes argue for cause and effect of HBOT in PPCS and PTSD.
The magnitude of these cognitive and affective improvements was criticized based on historically minimal or absent decreases in intellectual function after simple mild TBI.66,67 This magnitude of improvement is likely due in part to treatment of both TBI and PTSD,63,68,69 treatment of patients with multiple TBIs,70 treatment of combined blast and blunt TBI, use of the broad 25th–75th percentile range as “normal,” and reporting of an infrequent measure of concussion damage, full scale IQ. It also suggests a bias in neuropsychological testing of patients in which the definition of “normal” or “average” intellectual ability is construed to mean no damage or deficit. Our subjects complained of a reduction in their basic intellectual abilities and that they were not back to their “normal” cognitive levels, yet their FSIQ and VWM were “normal” and “average” before treatment. According to the patients, their complaints were often dismissed or attributed to emotional factors or even malingering. After treatment their FSIQ, memory, and other cognitive scores improved significantly to above “normal”/average levels, underscoring that they were not “normal”/average or at their previous normal level after their concussion(s). The treatment results were independent of effort (Green Word Memory Test) and greater than would be expected by test-retest/practice effects (Reliable Change Score analysis). Accepting “Average” as a post-injury assessment of “normal” can lead to inaccurate judgments and suggests that general intellectual ability and memory outcome instruments should be more commonly employed in PPCS treatment studies.
Subjects experienced large emotional improvements. 83% of subjects with suicidal ideation and 75% of subjects with panic attacks experienced a reduction or cessation in suicidal ideation or panic attacks after treatment. This is the first report of reduction in suicidal ideation or panic attacks in a hyperbaric therapy study on veterans. Self-reported Quality of Life and the subjects' estimate of the percent of their pre-deployment “normal” level of function also improved significantly. The reductions in suicidal ideation, panic attacks, and psychoactive medication use have implications for the current suicide epidemic in veterans. This is particularly meaningful, considering the contribution of psychoactive medication to veteran suicides.71
All of the veterans' non-imaging deficits, and improvements after HBOT, were explained by the brain blood flow findings. The main blood flow abnormalities, lower blood flow and coarse texture, were found in the white matter consistent with the primary injury site in mTBI.72,73 These abnormalities were statistically normalized or near normalized after HBOT. The improved texture corresponds to the pattern of blood flow seen in normal people (Figure 3) and HBOT-treated patients with a variety of chronic neuropathologies (trauma, carbon monoxide poisoning, decompression sickness, near-drowning, cerebral palsy)17,18,74,75 in the past two decades and is consistent with the findings reported with perfusion CT using our protocol of HBOT 152 kPa on chronic severe TBI, anoxic, and stroke patients.76 Taken together, the overall unchanged blood flow (MCP) and decreased range of blood flow (improved CV) after 40 HBOTs suggests that HBOT normalized brain blood flow by simultaneously decreasing elevated brain blood flow and increasing lowered brain blood flow.
The unchanged total amount of brain blood flow after 40 treatments is different from the findings in the first 16 subjects of this study reported with statistical parametric mapping27 and other SPECT HBOT chronic TBI studies19,28 which noted increased brain blood flow after a course of HBOT. These discrepancies are likely due to differences in analytic methodologies and the heterogeneity of the samples/injuries. The common finding is HBOT-induced improvement in either amount or pattern of brain blood flow. Based on flow-metabolism-function coupling77,78,79,80 these improvements in blood flow are physiologically responsible for the improvements in symptoms, physical exam, cognition, emotional state, and quality of life experienced by our subjects. Collectively, the SPECT/HBOT/TBI literature15,16,17,18,19,20,21,22,23,28 suggests the utility of SPECT in TBI81 and as a surrogate endpoint in mTBI/PPCS.82
The different effects of one and 40 HBOTs on brain blood flow (Table 6) reaffirmed the findings on the first 16 subjects,27 suggesting different metabolic/physiology effects of a single vs. 40 consecutive HBOTs in chronically injured brain. These effects are inconsistent with placebo effects documented with SPECT.83,84 In addition, the symptom and cognitive improvements in subjects occurred progressively and were apparent at 40 HBOTs, similar to Wolf et al.,13 not after the first HBOT, underscoring that the cognitive and symptom improvements were related to the brain blood flow normalization after 40 HBOTs. This is consistent with the SPECT and cognitive improvements after 40 treatments in Boussi-Gross et al.28 and the cognitive improvements after more than 35 treatments in Golden and Neubauer et al.20
HBOT is a treatment for acute, subacute, or chronic wounds in any anatomical location.5,6 In the preliminary report27 it was argued that HBOT was treating the microscopic white matter wounds of TBI. Recent reports in animals and humans have proven the existence of primarily perivascular white matter wounds in chronic blast-induced TBI,85,86 which are similar in location to the perivascular white matter wounds of chronic cerebral decompression sickness,87 the original wound to which we applied HBOT 152 kPa in 1990.88 The presence of white matter wounds is consistent with the reductions in white matter blood flow in the present study. The global symptomatic, cognitive, affective, physical exam, and imaging improvements in our studies and the studies of others13,16,19,20,26,28,30,31,32,76 are consistent with the known wound-healing effects of HBOT on the diffuse cerebral microscopic wounds of TBI.
The microscopic wound model, however, does not explain the surprising improvement of PTSD symptoms in the subjects. Persistence of PTSD has demonstrated long-term evidence of brain wounding,89 yet no pathological90 or imaging70 signature is evident. PTSD shares some of the same anatomical areas involved with TBI/PPCS.89,91,92,93 We speculate that in the course of treating the TBI/PPCS wounds the pathways for recurring pathological thoughts of PTSD are interrupted similar to interruption of cardiac re-entrant rhythms with medication or ablation therapies. This speculation is supported by the successful treatment of PTSD with stellate ganglion block.94 The mechanism of action is possibly modulation of gene expression. A recent study reveals genetic influences on the development of PTSD and shared genetic risk between PTSD and schizophrenia, bipolar, and major depressive disorder.95 HBOT may be suppressing these genes in a similar fashion to in vitro studies.96,97,98,99
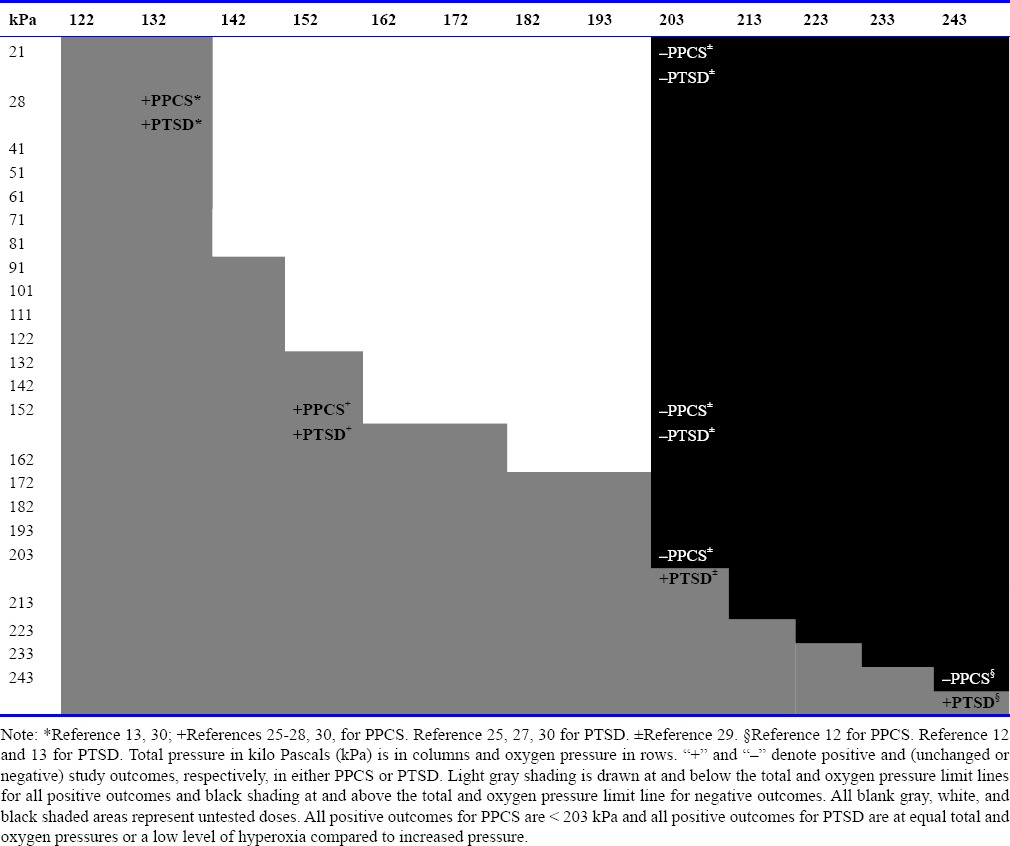
The significant outcomes in this study demand interpretation in the context of the subsequent more rigorous,28,30 and multi-dosing studies13,29 and their confusing results/conclusions.13,29,30,31,32,100,101,102 Since the first application of HBOT 152 kPa to Veterans with mTBI/PPCS and PTSD25 other researchers have: 1) duplicated HBOT-induced mTBI/PPCS improvements with the same HBOT 152 kPa dose using a stronger experimental design,29,31 2) demonstrated positive13,30 and negative (”harmful”)12 effects with different doses of HBOT (243 kPa oxygen, 122 kPa and 132 kPa air), and 3) demonstrated neutral29 or indeterminate31,32 effects with three alternate doses (203 kPa pressure/21 kPa oxygen, 152 kPa oxygen, or 203 kPa oxygen). HBOT PTSD studies have shown benefit at 152 kPa oxygen,25,27,30 203 kPa oxygen,29 243 kPa oxygen,13 132/122 kPa air,13,30 and no benefit at 203 kPa pressure/(21 kPa oxygen or 152 kPa oxygen).29 The two recent studies by Wolf and colleagues100,101 preclude comparative dosing analysis due to lack of actual data; both publications featured derived data/statistics. All of these studies except the recent Wolf's studies100,101 are summarized in Table 8. Since HBOT is a combination therapy of increased pressure and increased oxygen4,5 the discrepancies in experimental results for all studies and diagnoses are best explained by the effects of different doses of hyperbaric therapy on different neuropathologies, multi-dose study designs, mis-definitions of HBOT and sham, confusing statistical analyses, and erroneous conclusions.4,5,102,103,104 A dose-response relationship with both oxygen and pressure is strongly suggested by Table 9. The oxygen component of this dose argument has been supported by others.104 The data12,13,25,26,27,28,29,30,31,32 suggest that the pure 152 kPa dose of oxygen and the 132/122 kPa air pressurization doses are beneficial in PPCS with or without PTSD (Table 8) and that the 152 kPa oxygen dose has durability (present study with 6-month phone follow-up).
Table 8.
Summary of Department of Defense-funded and civilian studies on HBOT in mild TBI/PPCS.
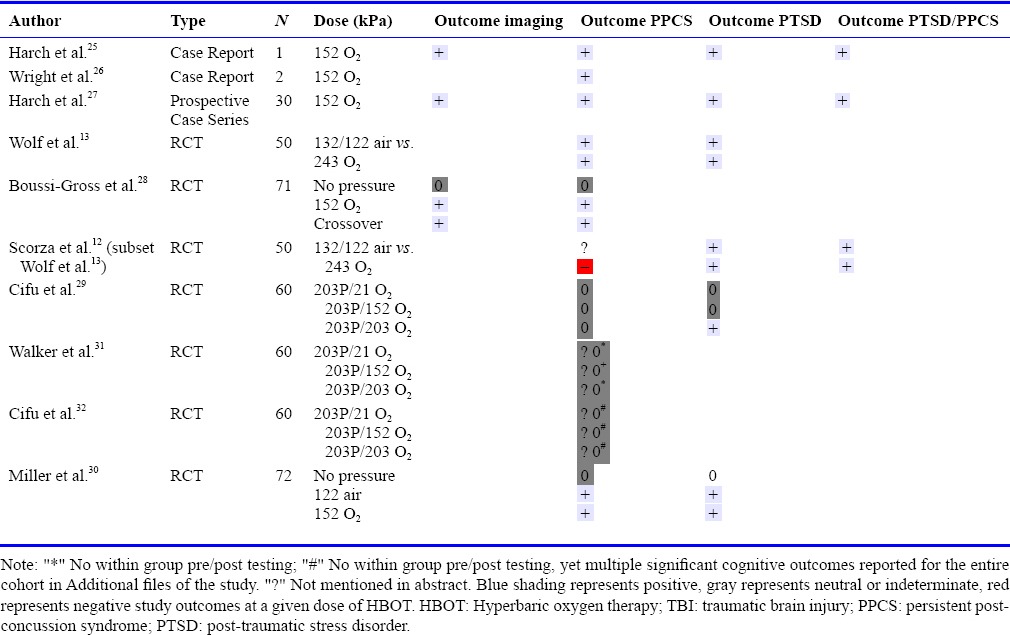
Table 9.
Oxygen and pressure dose relationship of studies in Table 8
Alternative explanations posited for our data and the data of the DoD-funded studies13,29,30,31,32 are placebo, relocation, Hawthorne, test/retest and practice effects, and the “ritual of HBOT”,30 collectively referred to as Non-Treatment Effects. All of these Non-Treatment Effects, except relocation and ritual, were previously addressed in multiple publications.27,63,68 They cannot explain the multiplicity of positive findings across all domains in our study, especially the imaging findings,27,63,68 and are refuted by the disparity in reported data from all of the mTBI studies reviewed above.12,13,25,26,27,28,29,30,31,32 Placebo and relocation effects should be greatest in beautiful Pensacola, Florida, but this study site had the least positive or neutral effects.29,31,32 The bulk of improvements accrued in the first 20 treatments in Miller et al.,30 were absent in the 203 kPa pressure studies,29,31,32 occurred after 20 treatments in the Wolf et al.'s13 air group, and were present in the first 20 treatments, lost in the second 20 treatments, and regained in the post-treatment period in Wolf et al.'s13 HBOT group. These disparities are not consistent with placebo effects where more placebo would be expected to have increasing and sustained effects. In addition, durability of placebo effects105 and further improvement after placebo treatment are uncommon. Rather, they are consistent with the 3 patterns of improvement identified in a review of placebo-drug studies that differentiate true drug effects of different doses of HBOT from the 61 placebo effect patterns.106
A more recent explanation, the “ritual” of the hyperbaric chamber experience30 is a theoretical contribution to placebo effect and is likely a component of the placebo effect, but it was argued based on the mischaracterization of sham in previous articles. It is inconsistent with the varied results in the DoD studies above. All of these studies contained the same “ritual” experience as the present study and should have had the same positive results. They did not. In addition, ritual does not explain the improvement of cognition and blood vessel density in an animal model of mTBI59 that used the original human protocol of 152 kPa oxygen, a near identical dose of hyperbaric therapy to the present study.
The more likely alternative to the multiple non-treatment and placebo effects explanations is the one that is consistent with the data, the biology of hyperbaric therapy,6 and Occam's razor.107 HBOT is a known therapy for wounds whose effects are dependent on dose. Mild TBI/PPCS is characterized by persistent white matter microscopic wounds.85,86 HBOT in this study is treating the microscopic white matter wounds of chronic TBI and the associated psychiatric condition of PTSD that invests these wounds. The differences in results between clinical studies are due to differences in doses of hyperbaric therapy.
A single dose of HBOT can induce excitability and neural plasticity of hippocampal neurons in normal rat brain slices108 while repetitive doses in an injury model have shown neurogenesis.109 The mechanism of action of HBOT in central nervous system (CNS) wounds are unknown but likely similar to those in non-CNS wounds.6 HBOT exerts its wound-healing effects by expression and suppression of oxygen and pressure sensitive genes.96 A single HBOT to human microvascular endothelial cells upregulated and downregulated 8,101 genes in 24 hours and enhanced vascular network formation. The primary gene clusters affected were the anti-inflammatory genes and genes that code for cell growth and proliferation. These gene-activating effects and tissue responsiveness are dependent on the dose of hyperbaric oxygen and pressure applied.4,97,98,99 The improvements, neutral, or negative effects of hyperbaric therapy in the multiple studies13,25,26,27,28,29,30,31,32 reflect the doses of pressure and hyperoxia that were applied to chronic brain wounds in the various studies. Some doses are effective, some are ineffective, and one is harmful in the treatment of PPCS, PTSD, and PPCS with PTSD. Repair of chronic brain wounds by trophism is supported by the durability of the clinical improvements in our subjects. At 6-month follow-up all subjects not only maintained improvement, but also reported further improvement.
Historical protocols have demonstrated that 30–40 HBOTs are necessary for healing of chronic non-CNS wounds,6 similar to the number of treatments in our study, however, it is half the number of HBOTs (80) that we have used clinically in more severe cases.15,16,17,18,19,20,21,22,23 In our original animal pilot study we compared 40 and 80 HBOTs to 40 sham air treatments and found a greater effect on memory and blood vessel density with 80 HBOTs vs. 40 HBOTs.110 This became the final protocol of the animal model.59 The animal studies and previous clinical experience with chronic moderate to severe TBI15,16,17,18,19,20,21,22,23,76 suggests our subjects might show further improvement with additional HBOT as was shown in Wright et al.'s use of the 152 kPa protocol.26
The limitations of the present study were unblinded investigators, and lack of a treatment control group. Placebo/non-treatment effects were discussed above. Investigator bias likely contributed to the magnitude of some of the P.I.'s symptom and physical exam recording and author SRA's neuropsychological testing, but are unlikely to account for the majority of the effects or the consistency and magnitude of the effects across all domains. This is particularly true for the SPECT subject/SPECT Control Group analyses where the investigators did not interact with the subjects and performed their analyses months to years after the subjects had completed their final imaging. Lack of a treatment control group is addressed with the placebo discussion and the results of the treatment-controlled studies. Currently, we are conducting a randomized controlled study of HBOT 152 kPa in civilians and military subjects with mTBI PPCS without clinical PTSD.
In conclusion, a 30-day course of 40 HBOT treatments delivered at 152 kPa/60 minutes, twice/day, 5 days/week, to military subjects with PPCS of mild-moderate blast-induced TBI with or without PTSD was safe with no persistent adverse events. Acute adverse events were more common than in other studies and the investigator's historical experience, but were felt to be due to the intense dosing schedule. Subjects experienced significant improvements in PPCS and PTSD symptoms, physical exam abnormalities, cognition, depression, anxiety, quality of life, and brain blood flow that cannot be explained with non-treatment effects; they are more consistent with the known wound-healing effects of HBOT on the diffuse cerebral microscopic wounds of TBI. Moreover, symptomatic improvements increased further during the 6-month post-treatment period. Compared to the matched Controls, TBI/PTSD subjects' brain blood flow was abnormal, but became visually more normal and statistically near-indistinguishable from Controls after 1 and 40 HBOTs. The main blood flow abnormalities and changes in blood flow after HBOT were in the white matter, the primary site of injury in mTBI. Simultaneously and most importantly, subjects experienced a significant reduction in suicidal ideation and anxiety, possibly the most significant finding in the study given the current veteran suicide epidemic. At the same time they were able to discontinue or decrease the dosage of their psychoactive medications and 52% no longer met the criteria for PTSD. These data comprise the strongest evidence and only treatment to date for the combined diagnoses of blast-induced PPCS with PTSD, and thus represent the best evidence-based medicine111 for these dual-diagnoses.68
Acknowledgments
The authors acknowledge the important and extensive contributions of John C. Pezzullo, Ph.D. (statistics), Logan M. Harch (SPECT texture analysis of patients and normals), Paul K. Staab, M.D. (supervision of hyperbaric treatment and attendance of patients), Phillip J. Tranchina (SPECT processing), William A. Duncan, Ph.D. and the late Honorable Martin Hoffmann, ex-Secretary of the Army, for their steadfast support and help in soliciting donations for this study, Soldiers Angels, The Audubon Society, New Orleans Steamboat Company, the Alliance for Natural Health, the National WWII Museum, and Westwego Swamp Boat Tours. Thanks to Sean Bal and Ray Crowell, our hyperbaric technicians, for their expert and safe delivery of hyperbaric oxygen therapy, Wanda Phillips for review of all of the study records, and Amy Trosclair of the BRI for overseeing the disbursement of funds.
Footnotes
Conflicts of interest
Dr. Harch owns a small hyperbaric medicine consulting company. He derives income from the treatment facility that is the primary location of his medical practice. He is on the board of directors of the International Hyperbaric Medical Association, a non-profit professional organization, and derives no income from this organization. Dr. Fogarty is president of the International Hyperbaric Medical Foundation (IHMF), a non-profit corporation that promotes education, research, and teaching in hyperbaric medicine. He also owns a holding company for a mobile hyperbaric clinic. Dr. Andrews has no competing financial interests. Juliette Lucarini, is co-owner of the hyperbaric consulting company with Paul G. Harch, M.D. Dr. Van Meter owns a hyperbaric equipment leasing company and contracts with hospitals to provide hyperbaric medicine physician staffing. Dr. Van Meter also owns the treatment facility. Partial presentation of a small subset of data at HBOT 2014 (The 9th International Symposium on Hyperbaric Oxygenation: Roadmap for the Future). Presented two slides on P values for the cognitive and quality of life outcomes for the first 24 subjects, compared to the first 15 subjects, in a lecture on review of the science and literature of HBOT in persistent post-concussion syndrome. None of the imaging, demographics, and content of the tables in this manuscript were presented at that meeting.
Research ethics
The study protocol was approved by the Louisiana State University Institutional Review Board. The study followed international and national regulations in accordance with the Declaration of Helsinki. The trial was registered with ClinicalTrials.gov (identifier: NCT00760734).
Data sharing statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
Open peer reviewers
Xue-jun Sun, Second Military Medical University, China; Vincenzo Zanon, University of Padova, Italy.
Additional files
Additional Table 1 (125.6KB, pdf) : List and Schedule of Psychometric Measures, When Administered, and Domain Measured.
Additional file 1 (241.5KB, pdf) : Re-Analysis of All Variables by Green Pass/Fail.
Additional file 2 (221.6KB, pdf) : Association of Improvements in Sleep and Medication with Changes in NeuroPsych and SPECT Variables.
Additional file 3 (162.3KB, pdf) : Contribution of Moderate TBI to Composite Data.
Additional file 4 (169.7KB, pdf) : Analysis of SPECT Data.
Additional file 5 (279.4KB, pdf) : Approach of SPECT MCP and CV at baseline, post-1 HBOT, and post-40 HBOTs to Control Subjects' MCP and CV.
Funding: The Marine Corps Law Enforcement Foundation, The Semper Fi Fund, The Coalition to Salute Americas Heroes, John and Resa Wing, the Harch Hyperbaric Research Fund of the Baromedical Research Institute of New Orleans, Frederick Lowther, Mr. Chris Anderson of the Van Kampen Foundation, Stanley Horton, John Staley IV, N.Y. Community Trust, Louis and Candace Hughes Trust, James Rooney, Marshall Wallach, Mr. Poindexter, Richard and Meg Lyon, The Sutton Foundation, The Caulkins Family, George Wood, Mr. Caleb Gates, New Orleans Natural Resource Group, Rubie and Bryan Bell, Margaret Hoffmann, John and Virginia Weinmann, Peter Roy Carney, John Fox, Dr. Warren Thomas, Joan C. White, James Wallace, Isabel Sanders, Edgar Jannotta, Thomas Petrie, Health Freedom Foundation, Tim and Libby Brown Foundation, Lisa Ethier, Operation Homefront Louisiana, Mr. Theodore Solomon, and Shoney's Restaurant (Gretna, LA). Twenty-five doses of the SPECT agent Ethyl Cysteinate Dimer were donated by Dupont Merck Pharma Radiopharmaceuticals, North Billerica, MA, USA for use in LSU IRB #3511, Tc99m ECD SPECT Brain Imaging in Neurologically Normal Individuals and Neurologically and Cognitively Abnormal Nitrogen Tetroxide Exposed Patients.
REFERENCES
- 1.Tanielian T, Jaycox LH. Arlington, VA, USA: Center for Military Health Policy Research, The Rand Corporation; 2008. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. [Google Scholar]
- 2.Carlson KF, Kehle SM, Meis LA, et al. Prevalence, assessment, and treatment of mild traumatic brain injury and posttraumatic stress disorder: a systematic review of the evidence.J Head Trauma Rehabil. 2011;26:103–115. doi: 10.1097/HTR.0b013e3181e50ef1. [DOI] [PubMed] [Google Scholar]
- 3.Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. Soldiers returning from Iraq. N Engl J Med. 2008;358:453–463. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- 4.Harch PG. Hyperbaric oxygen therapy for post-concussion syndrome: contradictory conclusions from a study mischaracterized as sham-controlled. J Neurotrauma. 2013;30:1995–1999. doi: 10.1089/neu.2012.2799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harch PG. Hyperbaric oxygen in chronic traumatic brain injury: oxygen, pressure, and gene therapy. Med Gas Res. 2015;5:9. doi: 10.1186/s13618-015-0030-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weaver LK. 13th ed. Durham, NC: 2014. Hyperbaric Oxygen Therapy Indications. The Hyperbaric Oxygen Therapy Committee Report. [Google Scholar]
- 7.Centers for Medicare and Medicaid Services National Coverage Determination (NCD) Hyperbaric Oxygen Therapy (2029). National Coverage Determinations (NCD) Manual, Publication Number 100-3, Chapter 1, Part 1, Section 20.29, effective date 6/19/2006. http://www.cms.hhs.gov/mcd/viewncd.asp?ncd_id=20.29&ncd_version=3&basket=ncd%3A20.29%3A3%3AHyperbaric+Oxygen+Therapy .
- 8.Harch PG. HBO therapy in global cerebral ischemia/anoxia and coma, Chapter 20. In: Jain KK, editor. Textbook of Hyperbaric Medicine. 6th ed. Cham, Switzerland: Springer; 2017. pp. 269–319. [Google Scholar]
- 9.U.S. Navy Diving Manual, Revision 6, Vol. 1, Sec. 3-9.2.2.2, Symptoms of CNS Oxygen toxicity, pgs. 42-3.Chapter 3: Underwater Physiology and Diving Disorders. 3-9 Indirect Effects of Pressure on the Human Body. SS521-AG-PRO-010, 9010-LP-106-0957. Published by direction of Commander, Naval Sea Systems Command, 4/15/2008 [Google Scholar]
- 10.Clark JM. Oxygen toxicity. In: Bennett P, Elliott D, editors. The Physiology and Medicine of Diving. 4th Edition. Chapter 6. London: W.B. Saunders Company, LTD; 1993. pp. 121–169. [Google Scholar]
- 11.Lin JW, Tsai JT, Lee LM, et al. Effect of hyperbaric oxygen on patients with traumatic brain injury. Acta Neurochir Suppl. 2008;101:145–149. doi: 10.1007/978-3-211-78205-7_25. [DOI] [PubMed] [Google Scholar]
- 12.Scorza KA, McCarthy W, Miller RS, Carne W, Wolf GW. Orlando, FL, USA: Undersea and Hyperbaric Medical Society Annual Meeting; 2013. Hyperbaric oxygen effects on PTSD and mTBI symptoms: a subset analysis. [Google Scholar]
- 13.Wolf G, Cifu D, Baugh L, Carne W, Profenna L. The effect of hyperbaric oxygen on symptoms after mild traumatic brain injury. J Neurotrauma. 2012;29:2606–2612. doi: 10.1089/neu.2012.2549. [DOI] [PubMed] [Google Scholar]
- 14.Harch PG. Flagstaff: 2002. The dosage of hyperbaric oxygen in chronic brain injury. The Proceedings of the 2nd International Symposium on Hyperbaric Oxygenation for Cerebral Palsy and the Brain-Injured Child. [Google Scholar]
- 15.Harch PG, Van Meter KW, Gottlieb SF, Staab P. HMPAO SPECT brain imaging and low pressure HBOT in the diagnosis and treatment of chronic traumatic, ischemic, hypoxic, and anoxic encephalopathies. Undersea Hyperb Med. 1994;21:30. [Google Scholar]
- 16.Neubauer RA, Gottlieb SF, Pevsner NH. Hyperbaric oxygen for treatment of closed head injury. South Med J. 1994;87:933–936. doi: 10.1097/00007611-199409000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Harch PG, Van Meter KW, Neubauer RA, Gottlieb SF. Use of HMPAO SPECT for assessment of response to HBO in ischemic/hypoxic encephalopathies. In: Jain KK, editor. Appendix, Textbook of Hyperbaric Medicine. 2nd ed. Seattle, WA, USA: Hogrefe and Huber Publishers; 1996. pp. 480–491. [Google Scholar]
- 18.Harch PG, Neubauer RA. Hyperbaric Oxygen Therapy in Global Cerebral Ischemia/Anoxia and Coma. In: Jain KK, editor. Textbook of Hyperbaric Medicine. Chapter 18. Seattle, WA, USA: Hogrefe and Huber Publishers; 1999. pp. 319–345. [Google Scholar]
- 19.Golden ZL, Neubauer R, Golden CJ, Greene L, Marsh J, Mleko A. Improvement in cerebral metabolism in chronic brain injury after hyperbaric oxygen therapy. Int J Neurosci. 2002;112:119–131. doi: 10.1080/00207450212027. [DOI] [PubMed] [Google Scholar]
- 20.Golden Z, Golden CJ, Neubauer RA. Improving neuropsychological function after chronic brain injury with hyperbaric oxygen. Disabil Rehabil. 2006;28:1379–1386. doi: 10.1080/09638280600638364. [DOI] [PubMed] [Google Scholar]
- 21.Harch PG, Neubauer RA. Hyperbaric oxygen therapy in global cerebral ischemia/anoxia and coma. In: Jain KK, editor. Textbook of Hyperbaric Medicine. 3rd Revised Edition. Chapter 18. Seattle, WA, USA: Hogrefe and Huber Publishers; 2004. pp. 223–261. [Google Scholar]
- 22.Harch PG, Neubauer RA. Hyperbaric oxygen therapy in global cerebral ischemia/anoxia and coma. In: Jain KK, editor. Textbook of Hyperbaric Medicine. 5th Revised Edition. Chapter 19. Seattle, WA, USA: Hogrefe and Huber Publishers; 2009. pp. 235–274. [Google Scholar]
- 23.Harch PG, Neubauer RA, Uszler JM, James PB. Appendix: Diagnostic Imaging and HBO Therapy. In: Jain KK, editor. Chapter 44, Textbook of Hyperbaric Medicine. 5th Revised Edition. Seattle, WA, USA: Hogrefe and Huber Publishers; 2009. pp. 505–519. [Google Scholar]
- 24.Harch PG, Kriedt C, Van Meter KW, Sutherland RJ. Hyperbaric oxygen therapy improves spatial learning and memory in a rat model of chronic traumatic brain injury. Brain Res. 2007;1174:120–129. doi: 10.1016/j.brainres.2007.06.105. [DOI] [PubMed] [Google Scholar]
- 25.Harch PG, Fogarty EF, Staab PK, Van Meter K. Low pressure hyperbaric oxygen therapy and SPECT brain imaging in the treatment of blast-induced chronic traumatic brain injury (post-concussion syndrome) and post traumatic stress disorder: a case report. Cases J. 2009;2:6538. doi: 10.1186/1757-1626-0002-0000006538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wright JK, Zant E, Groom K, Schlegel RE, Gilliland K. Case report: Treatment of mild traumatic brain injury with hyperbaric oxygen. Undersea Hyperb Med. 2009;36:391–399. [PubMed] [Google Scholar]
- 27.Harch PG, Andrews SR, Fogarty EF, et al. A phase I study of low-pressure hyperbaric oxygen therapy for blast-induced post-concussion syndrome and post-traumatic stress disorder. J Neurotrauma. 2012;29:168–185. doi: 10.1089/neu.2011.1895. [DOI] [PubMed] [Google Scholar]
- 28.Boussi-Gross R, Golan H, Fishlev G, et al. Hyperbaric oxygen therapy can improve post concussion syndrome years after mild traumatic brain injury - randomized prospective trial. PLoS One. 2013;8:e79995. doi: 10.1371/journal.pone.0079995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cifu DX, Hart BB, West SL, Walker W, Carne W. The effect of hyperbaric oxygen on persistent postconcussion symptoms. J Head Trauma Rehabil. 2014;29:11–20. doi: 10.1097/HTR.0b013e3182a6aaf0. [DOI] [PubMed] [Google Scholar]
- 30.Miller RS, Weaver LK, Bahraini N, et al. Effects of hyperbaric oxygen on symptoms and quality of life among service members with persistent postconcussion symptoms: a randomized clinical trial. JAMA Intern Med. 2015;175:43–52. doi: 10.1001/jamainternmed.2014.5479. [DOI] [PubMed] [Google Scholar]
- 31.Walker WC, Franke LM, Cifu DX, Hart BB. Randomized, Sham-controlled, feasibility trial of hyperbaric oxygen for service members with postconcussion syndrome: cognitive and psychomotor outcomes 1 week postintervention. Neurorehabil Neural Repair. 2014;28:420–432. doi: 10.1177/1545968313516869. [DOI] [PubMed] [Google Scholar]
- 32.Cifu DX, Walker WC, West SL, et al. Hyperbaric oxygen for blast-related postconcussion syndrome: three-month outcomes. Ann Neurol. 2014;75:277–286. doi: 10.1002/ana.24067. [DOI] [PubMed] [Google Scholar]
- 33.King NS, Crawford S, Wenden FJ, Moss NE, Wade DT. The Rivermead Post Concussion Symptoms Questionnaire: a measure of symptoms commonly experienced after head injury and its reliability. J Neurol. 1995;242:587–592. doi: 10.1007/BF00868811. [DOI] [PubMed] [Google Scholar]
- 34.Sterr A, Herron KA, Hayward C, Montaldi D. Are mild head injuries as mild as we think. Neurobehavioral concomitants of chronic post-concussion syndrome? BMC Neurol. 2006;6:7. doi: 10.1186/1471-2377-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.PTSD Checklist-Military. 2009. http://wwwnmcphc.med.navy.mil/deployment_health/frm_ptsdmilitary.aspx .
- 36.4th ed., text rev. Washington, DC, USA: Author; 2000. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 37.WAIS-IV. http://pearsonassess.com/HAIWEB/Cultures/en-us/Productdetail.htm?Pid=015-8980-808?Mode=summary.2009 .
- 38.WASI. 2009. http://pearsonassess.com/haiweb/cultures/en-us/productdetail.htm?pid=015-8981-502 .
- 39.WMS-IV. 2009. http://pearsonassess.com/HAIWEB/Cultures/en-us/Productdetail.htm?Pid=8895-800 .
- 40.Greenberg L. Test of Variables of Attention Continuous Performance Test. USA: Universal Attention Disorders, Inc; 1996. [Google Scholar]
- 41.Lesak M, Howieson D, Loring D. Neuropsychological Assessment. 4th Edition. New York: Oxford University Press; 2004. [Google Scholar]
- 42.Reitan RM, Wolfson D. Tucson, AZ, USA: Neuropsychology Press; 1993. The Halstead-Reitan Neuropsychological Test Battery: Theory and Clinical Interpretation. [Google Scholar]
- 43.Wilson B, Cockburn J, Baddeley A. The Rivermead Behavioural Memory Test. Reading, UK: Thames Valley Test Company; 1985. [Google Scholar]
- 44.Patrick DL, Danis M, Southerland LI, Hong G. Quality of life following intensive care. J Gen Intern Med. 1988;3:218–223. doi: 10.1007/BF02596335. [DOI] [PubMed] [Google Scholar]
- 45.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 46.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Powell JM, Machamer JE, Temkin NR, Dikmen SS. Self-report of extent of recovery and barriers to recovery after traumatic brain injury: a longitudinal study. Arch Phys Med Rehabil. 2001;82:1025–1030. doi: 10.1053/apmr.2001.25082. [DOI] [PubMed] [Google Scholar]
- 48.MAST Revised. 2009. http://counsellingresource.com/quizzes/alcoholmast/index.html .
- 49.Gavin DR, Ross HE, Skinner HA. Diagnostic validity of the drug abuse screening test in the assessment of DSM-III drug disorders. Br J Addict. 1989;84:301–307. doi: 10.1111/j.1360-0443.1989.tb03463.x. [DOI] [PubMed] [Google Scholar]
- 50.Lesak M, Howieson D, Loring D. Neuropsychological Assessment. 4th Edition. New York: Oxford University Press; 2004. p. 776. [Google Scholar]
- 51.Wechsler D. Wechsler Test of Adult Reading (WTAR)-Manual. San Antonio, TX, USA: The Psychological Corporation; 2001. [Google Scholar]
- 52.Keane T, Fairbank J, Caddell J, Zimering R, Taylor K, Mora C. Clinical evaluation of a measure to assess combat exposure. Psychol Assess. 1989;1:53–55. [Google Scholar]
- 53.Rappaport M, Hall KM, Hopkins K, Belleza T, Cope DN. Disability rating scale for severe head trauma: coma to community. Arch Phys Med Rehabil. 1982;63:118–123. [PubMed] [Google Scholar]
- 54.Dougherty G. Quantitative CT in the measurement of bone quantity and bone quality for assessing osteoporosis. Med Eng Phys. 1996;18:557–568. doi: 10.1016/1350-4533(96)00011-2. [DOI] [PubMed] [Google Scholar]
- 55.Shields TG, Duff PM, Evans SA, et al. Correlation between 99Tcm-HMPAO-SPECT brain image and a history of decompression illness or extent of diving experience in commercial divers. Occup Environ Med. 1997;54:247–253. doi: 10.1136/oem.54.4.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wolf EG, Prye J, Michaelson R, Brower G, Profenna L, Boneta O. Hyperbaric side effects in a traumatic brain injury randomized clinical trial. Undersea Hyperb Med. 2012;39:1075–1082. [PubMed] [Google Scholar]
- 57.Rossignol DA. Hyperbaric oxygen therapy might improve certain pathophysiological findings in autism. Med Hypotheses. 2007;68:1208–1227. doi: 10.1016/j.mehy.2006.09.064. [DOI] [PubMed] [Google Scholar]
- 58.Thorsen E, Aanderud L, Aasen T. Effects of a standard hyperbaric oxygen treatment protocol on pulmonary function. Eur Respir J. 1998;12:1442–1445. doi: 10.1183/09031936.98.12061442. [DOI] [PubMed] [Google Scholar]
- 59.Harch PG, Kriedt C, Van Meter KW, Sutherland RJ. Hyperbaric oxygen therapy improves spatial learning and memory in a rat model of chronic traumatic brain injury. Brain Res. 2007;1174:120–129. doi: 10.1016/j.brainres.2007.06.105. [DOI] [PubMed] [Google Scholar]
- 60.Marx RE, Johnson RP. Problem wounds in oral and maxillofacial surgery: the role of hyperbaric oxygen. In: Davis JC, Hunt TK, editors. Problem Wounds: The Role of Oxygen, Chapter 4. New York: Elsevier Science Publishing Co; 1988. pp. 65–123. [Google Scholar]
- 61.Lidvall HF. Letter: Recovery after minor head injury. Lancet. 1975;1:100. doi: 10.1016/s0140-6736(75)91103-4. [DOI] [PubMed] [Google Scholar]
- 62.Symonds C. Concussion and its sequelae. Lancet. 1962;1:1–5. [Google Scholar]
- 63.Harch PG, Andrews SR, Fogarty E, Amen DG, Lucarini J, Van Meter KW. Response to letter to the editor by Wortzel and colleagues. J Neurotrauma. 2012;29:2425–2430. [Google Scholar]
- 64.Steenkamp MM, Litz BT, Hoge CW, Marmar CR. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314:489–500. doi: 10.1001/jama.2015.8370. [DOI] [PubMed] [Google Scholar]
- 65.Congress of the United States, Congressional Budget Office. A CBO Study: The Veterans Health Administration's Treatment of PTSD and Traumatic Brain Injury Among Recent Combat Veterans. 2012. http://timemilitaryfileswordpresscom/2012/02/02-09-ptsd-1pd .
- 66.Wortzel HS, Arciniegas DB, Anderson CA, Vanderploeg RD, Brenner LA. A phase I study of low-pressure hyperbaric oxygen therapy for blast-induced post-concussion syndrome and post-traumatic stress disorder: a neuropsychiatric perspective. J Neurotrauma. 2012;29:2421. doi: 10.1089/neu.2012.2426. [DOI] [PubMed] [Google Scholar]
- 67.Armistead-Jehle P, Lee D. Response to the Harch Group's “A phase I study of low-pressure hyperbaric oxygen therapy for blast-induced post-concussion syndrome and post-traumatic stress disorder”. J Neurotrauma. 2012;29:2513–2515. doi: 10.1089/neu.2012.2400. [DOI] [PubMed] [Google Scholar]
- 68.Harch PG, Andrews SR, Pezzullo JC. Response to the letter to the editor by Armistead-jehle and Lee on Harch et al., “A phase I study of low-pressure hyperbaric oxygen therapy for blast-induced post-concussion syndrome and post-traumatic stress disorder”. J Neurotrauma. 2012;29:2516–2519. doi: 10.1089/neu.2012.2608. [DOI] [PubMed] [Google Scholar]
- 69.Belanger HG, Proctor-Weber Z, Kretzmer T, Kim M, French LM, Vanderploeg RD. Symptom complaints following reports of blast versus non-blast mild TBI: does mechanism of injury matter. Clin Neuropsychol? 2011;25:702–715. doi: 10.1080/13854046.2011.566892. [DOI] [PubMed] [Google Scholar]
- 70.Petrie EC, Cross DJ, Yarnykh VL, et al. Neuroimaging, behavioral, and psychological sequelae of repetitive combined blast/impact mild traumatic brain injury in Iraq and Afghanistan war veterans. J Neurotrauma. 2014;31:425–436. doi: 10.1089/neu.2013.2952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. http://www.cchr.org/documentaries/the-hidden-enemy.html .
- 72.Kraus MF, Susmaras T, Caughlin BP, Walker CJ, Sweeney JA, Little DM. White matter integrity and cognition in chronic traumatic brain injury: a diffusion tensor imaging study. Brain. 2007;130:2508–2519. doi: 10.1093/brain/awm216. [DOI] [PubMed] [Google Scholar]
- 73.Lipton ML, Gulko E, Zimmerman ME, et al. Diffusion-tensor imaging implicates prefrontal axonal injury in executive function impairment following very mild traumatic brain injury. Radiology. 2009;252:816–824. doi: 10.1148/radiol.2523081584. [DOI] [PubMed] [Google Scholar]
- 74.Barratt DM, Harch PG, Van Meter K. Decompression illness in divers: a review of the literature. Neurologist. 2002;8:186–202. doi: 10.1097/00127893-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 75.Van Meter KW, Weiss L, Harch PG, et al. Should the pressure be off or on in the use of oxygen in the treatment of carbon monoxide-poisoned patients? Ann Emerg Med. 1994;24:283–288. doi: 10.1016/s0196-0644(05)83748-5. [DOI] [PubMed] [Google Scholar]
- 76.Churchill S, Weaver LK, Deru K, et al. A prospective trial of hyperbaric oxygen for chronic sequelae after brain injury (HYBOBI) Undersea Hyperb Med. 2013;40:165–193. [PubMed] [Google Scholar]
- 77.Meyer JS, Sawada T, Kitamura A, toyoda M. Cerebral oxygen, glucose, lactate, and pyruvate metabolism in stroke. Therapeutic considerations. Circulation. 1968;37:1036–1048. doi: 10.1161/01.cir.37.6.1036. [DOI] [PubMed] [Google Scholar]
- 78.Raichle ME, Grubb RL, Jr, Gado MH, Eichling JO, Ter-Pogossian MM. Correlation between regional cerebral blood flow and oxidative metabolism. In vivo studies in man. Arch Neurol. 1976;33:523–526. doi: 10.1001/archneur.1976.00500080001001. [DOI] [PubMed] [Google Scholar]
- 79.Gur RC, Gur RE, Obrist WD, et al. Sex and handedness differences in cerebral blood flow during rest and cognitive activity. Science. 1982;217:659–661. doi: 10.1126/science.7089587. [DOI] [PubMed] [Google Scholar]
- 80.Obrist WD, Gennarelli TA, Segawa H, Dolinskas CA, Langfitt TW. Relation of cerebral blood flow to neurological status and outcome in head-injured patients. J Neurosurg. 1979;51:292–300. doi: 10.3171/jns.1979.51.3.0292. [DOI] [PubMed] [Google Scholar]
- 81.Raji CA, Tarzwell R, Pavel D, et al. Clinical utility of SPECT neuroimaging in the diagnosis and treatment of traumatic brain injury: a systematic review. PLoS One. 2014;9:e91088. doi: 10.1371/journal.pone.0091088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Robb MA, McInnes PM, Califf RM. Biomarkers and Surrogate Endpoints: Developing Common Terminology and Definitions. JAMA. 2016;315:1107–1108. doi: 10.1001/jama.2016.2240. [DOI] [PubMed] [Google Scholar]
- 83.Beauregard M. Effect of mind on brain activity: evidence from neuroimaging studies of psychotherapy and placebo effect. Nord J Psychiatry. 2009;63:5–16. doi: 10.1080/08039480802421182. [DOI] [PubMed] [Google Scholar]
- 84.Jarcho JM, Mayer EA, London ED. Neuroimaging placebo effects: new to ols generate new questions. Clin Pharmacol Ther. 2009;86:352–354. doi: 10.1038/clpt.2009.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ryu J, Horkayne-Szakaly I, Xu L, et al. The problem of axonal injury in the brains of veterans with histories of blast exposure. Acta Neuropathol Commun. 2014;2:153. doi: 10.1186/s40478-014-0153-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shively SB, Horkayne-Szakaly I, Jones RV, Kelly JP, Armstrong RC, Perl DP. Characterisation of interface astroglial scarring in the human brain after blast exposure: a post-mortem case series. Lancet Neurol. 2016;15:944–953. doi: 10.1016/S1474-4422(16)30057-6. [DOI] [PubMed] [Google Scholar]
- 87.Palmer AC, Calder IM, Yates PO. Cerebral vasculopathy in divers. Neuropathol Appl Neurobiol. 1992;18:113–124. doi: 10.1111/j.1365-2990.1992.tb00773.x. [DOI] [PubMed] [Google Scholar]
- 88.Harch PG. Late treatment of decompression illness and use of SPECT brain imaging. In: Moon RE, Sheffield PJ, editors. Treatment of Decompression Illness, 45th Workshop of the Undersea and Hyperbaric Medical Society. Kensington, MD, USA: Undersea and Hyperbaric Medical Society; 1996. pp. 203–242. [Google Scholar]
- 89.O'Doherty DC, Chitty KM, Saddiqui S, Bennett MR, Lagopoulos J. A systematic review and meta-analysis of magnetic resonance imaging measurement of structural volumes in posttraumatic stress disorder. Psychiatry Res. 2015;232:1–33. doi: 10.1016/j.pscychresns.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 90.Lucassen PJ, Pruessner J, Sousa N, et al. Neuropathology of stress. Acta Neuropathol. 2014;127:109–135. doi: 10.1007/s00401-013-1223-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kennedy JE, Jaffee MS, Leskin GA, Stokes JW, Leal FO, Fitzpatrick PJ. Posttraumatic stress disorder and posttraumatic stress disorder-like symptoms and mild traumatic brain injury. J Rehabil Res Dev. 2007;44:895–920. doi: 10.1682/jrrd.2006.12.0166. [DOI] [PubMed] [Google Scholar]
- 92.Umile EM, Sandel ME, Alavi A, Terry CM, Plotkin RC. Dynamic imaging in mild traumatic brain injury: support for the theory of medial temporal vulnerability. Arch Phys Med Rehabil. 2002;83:1506–1513. doi: 10.1053/apmr.2002.35092. [DOI] [PubMed] [Google Scholar]
- 93.Wang Z, Neylan TC, Mueller SG, et al. Magnetic resonance imaging of hippocampal subfields in posttraumatic stress disorder. Arch Gen Psychiatry. 2010;67:296–303. doi: 10.1001/archgenpsychiatry.2009.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mulvaney SW, Lynch JH, Hickey MJ, et al. Stellate ganglion block used to treat symptoms associated with combat-related post-traumatic stress disorder: a case series of 166 patients. Mil Med. 2014;179:1133–1140. doi: 10.7205/MILMED-D-14-00151. [DOI] [PubMed] [Google Scholar]
- 95.Duncan LE, Ratanatharathorn A, Aiello AE, et al. Largest GWAS of PTSD (N=20 070) yields genetic overlap with schizophrenia and sex differences in heritability. doi: 10.1038/mp.2017.77. doi: 101038/mp201777.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Godman CA, Chheda KP, Hightower LE, Perdrizet G, Shin DG, Giardina C. Hyperbaric oxygen induces a cytoprotective and angiogenic response in human microvascular endothelial cells. Cell Stress Chaperones. 2010;15:431–442. doi: 10.1007/s12192-009-0159-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chen Y, Nadi NS, Chavko M, Auker CR, McCarron RM. Microarray analysis of gene expression in rat cortical neurons exposed to hyperbaric air and oxygen. Neurochem Res. 2009;34:1047–1056. doi: 10.1007/s11064-008-9873-8. [DOI] [PubMed] [Google Scholar]
- 98.Oh S, Lee E, Lee J, Lim Y, Kim J, Woo S. Comparison of the effects of 40% oxygen and two atmospheric absolute air pressure conditions on stress-induced premature senescence of normal human diploid fibroblasts. Cell Stress Chaperones. 2008;13:447–458. doi: 10.1007/s12192-008-0041-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kendall AC, Whatmore JL, Harries LW, Winyard PG, Eggleton P, Smerdon GR. Different oxygen treatment pressures alter inflammatory gene expression in human endothelial cells. Undersea Hyperb Med. 2013;40:115–123. [PubMed] [Google Scholar]
- 100.Wolf EG, Baugh LM, Kabban CM, Richards MF, Prye J. Cognitive function in a traumatic brain injury hyperbaric oxygen randomized trial. Undersea Hyperb Med. 2015;42:313–332. [PubMed] [Google Scholar]
- 101.Shandley S, Wolf EG, Schubert-Kappan CM, et al. Increased circulating stem cells and better cognitive performance in traumatic brain injury subjects following hyperbaric oxygen therapy. Undersea Hyperb Med. 2017;44:257–269. doi: 10.22462/5.6.2017.6. [DOI] [PubMed] [Google Scholar]
- 102.Harch PG. Hyperbaric oxygen therapy for mild traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD): explaining the discrepancy between civilian and military studies. 2015. http://www.hyperbaricmedicalfoundation.org .
- 103.Harch PG. Department of defense trials for hyperbaric oxygen and TBI: issues of study design and questionable conclusions. Undersea Hyperb Med. 2013;40:469–470. [PubMed] [Google Scholar]
- 104.Figueroa XA, Wright JK. Hyperbaric oxygen: B-level evidence in mild traumatic brain injury clinical trials. Neurology. 2016;87:1400–1406. doi: 10.1212/WNL.0000000000003146. [DOI] [PubMed] [Google Scholar]
- 105.Finniss DG, Kaptchuk TJ, Miller F, Benedetti F. Biological, clinical, and ethical advances of placebo effects. Lancet. 2010;375:686–695. doi: 10.1016/S0140-6736(09)61706-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Quitkin FM. Placebos, drug effects, and study design: a clinician's guide. Am J Psychiatry. 1999;156:829–836. doi: 10.1176/ajp.156.6.829. [DOI] [PubMed] [Google Scholar]
- 107. http://www.britannica.com/EBchecked/topic/424706/Occamsrazor .
- 108.Garcia AJ, 3rd, Putnam RW, Dean JB. Hyperbaric hyperoxia and normobaric reoxygenation increase excitability and activate oxygen-induced potentiation in CA1 hippocampal neurons. J Appl Physiol (1985) 2010;109:804–819. doi: 10.1152/japplphysiol.91429.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zhang T, Yang QW, Wang SN, et al. Hyperbaric oxygen therapy improves neurogenesis and brain blood supply in piriform cortex in rats with vascular dementia. Brain Inj. 2010;24:1350–1357. doi: 10.3109/02699052.2010.504525. [DOI] [PubMed] [Google Scholar]
- 110.Harch PG, Kriedt CL, Weisand MP, Van Meter KW, Sutherland RJ. Low pressure hyperbaric oxygen therapy induces cerebrovascular changes and improves complex learning/memory in a rat open head bonk chronic brain contusion model. Undersea Hyperb Med. 1996;23(Suppl):48. [Google Scholar]
- 111.Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn't. BMJ. 1996;312:71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
List and Schedule of Psychometric Measures, When Administered, and Domain Measured
Re-Analysis of All Variables by Green Pass/Fail
Association of Improvements in Sleep and Medication with Changes in NeuroPsych and SPECT Variables
Contribution of Moderate TBI to Composite Data.
Analysis of SPECT Data
Approach of SPECT MCP and CV at baseline, post-1 HBOT, and post-40 HBOTs to Control Subjects’ MCP and CV