Abstract
In the late 90's there was a change in both the route of transmission and the people at risk for sporotrichosis. This zoonotic cat-man alternative transmission route elicited changes in strategies to control the epidemic. There was a progressive increase in the number of cases involving especially children and the elderly. In addition to becoming hyperendemic, uncommon clinical pictures like immunoreactive clinical presentations or severe systemic cases have emerged. New species were identified and classified through molecular tools using more virulent clinical isolates, like S. brasiliensis, compared to the environmental isolates. Likewise, different species of Sporothrix have been associated with different geographic regions. The serological and molecular techniques are used as an auxiliary tool for the diagnosis and/or for species identification, although the isolation and the identification of Sporothrix spp. in clinical specimen is still the gold standard. Currently sporotrichosis epidemics requires the knowledge of the epidemiological-molecular profile to control the disease and the specific treatment. Itraconazole, potassium iodide, terfinafine, and amphotericin B are the available drugs in Brazil to treat sporotrichosis. The drug of choice, its posology, and treatment duration vary according to the clinical presentation, the Sporothrix species, and host immune status. New treatment choices, including a vaccine, are being developed; nevertheless, more clinical trials are required to confirm its efficacy.
Keywords: Diagnosis, Epidemiology, Molecular biology, Serology, Sporothrix, Therapeutics
INTRODUCTION
Sporotrichosis is a subacute or chronic infection, caused by thermodimorphic fungi of the genus Sporothrix. It is a cosmopolitan disease, occurring preferably in tropical and subtropical regions, and is considered the most frequent subcutaneous mycosis in Latin America, where it is endemic.1
Sporotrichosis was first described in 1898, by the medical student Benjamin Schenck, at the Johns Hopkins Hospital, in Baltimore, USA.2 The fungus isolated from skin lesions on the right upper limb of a patient treated by Schenck was evaluated by the pathologist Erwin F. Smith, and identified as a species belonging to the genus Sporotrichum. In 1900, Hektoen and Perkins reported another case in Chicago and proposed a new name, Sporothrix schenckii, although Sporotrichum schenckii was used for decades.3 Due to the reproduction characteristics of this genus, the binomial was changed to Sporothrix schenckii.4 Currently, the species involved in the human or animal disease, and other that are environmental, have been recognized.5
In the early 20th century, in France, sporotrichosis was a common disease, as were the reports of the extracutaneous clinical forms.3 In Brazil, Lutz and Splendore firstly described infections in rats and humans, demonstrating the presence of asteroid bodies in tissues, which are useful for the histopathological diagnosis of this mycosis.6
EPIDEMIOLOGY AND ETIOPATHOGENESIS
For a long time, sporotrichosis was known as the "rosebush mycosis", or the "gardener's mycosis", given that the infection usually resulted from the agent's inoculation on the skin or mucous membrane, by trauma with contaminated plant material. However, some cases of zoonotic transmission have been reported, as well as less frequent cases of inhaled infective fungal propagules, clinically presenting as a systemic mycosis.7,8
Occasionally, there may be an environmental transmission of sporotrichosis, classically associated with soil manipulation activities, whether for occupational or leisure reasons; in outbreaks such as those that occurred in the USA, especially in the Mississippi Valley, in the 80's, involving reforestation workers infected by pine trees and moss seedlings; also as microepidemics like that which occured in the early 90's, with people infected by the contact with hay stored in an abandoned house where Halloween parties were held; as well as large epidemics, such as that which occurred in the 40's, when three thousand miners in South Africa were infected by the contact with contaminated wood supporting beams, being considered the largest epidemic in the 20th century.9-11 More recently, 457 cases were described between 2007 and 2009 in a province in the northeast China, where the disease is endemic.12
The zoonotic transmission of sporotrichosis was described sporadically involving accidents with snakes and birds, also mosquito, rat, horse, squirrel, and fish bites.3,13,14 Epidemics were reported in Uruguay and, more recently, in Brazil and Argentina, related to armadillo hunting, given the close relation of the armadillo with the soil.15,16 The importance of the cat in zoonotic transmission was first noticed when an outbreak involving five people exposed to a sick animal was reported.17 In Brazil, the main zoonotic sporotrichosis outbreaks, involving humans and a small group of domestic cats, occurred in the states of São Paulo and Rio Grande do Sul, with an effective epidemiological control.18,19
In September 1997, the first cases of the greatest feline zoonotic transmission epidemic ever described were admitted at the Pedro Ernesto University Hospital, Rio de Janeiro. Three people from the same family were infected by a sick cat that died (authors' report, unpublished) (Figure 1). Then, the first publications about this epidemic, which is currently considered to be hyperendemic in the state of Rio de Janeiro, appeared.20,21 The capital city and the surrounding municipalities known as "Baixada Fluminense" are currently the most affected places where poor socioeconomic conditions are observed. The epidemiological profile is mainly characterized by children, elderly, and women, because these groups usually have direct and more frequent contact with these animals.22 Along with the consolidation of the urban epidemics, vulnerable patients also became a worrisome at-risk population, especially those infected by the human immunodeficiency virus.23 Since 2013, the notification is mandatory in the state of Rio de Janeiro, but not in the other Brazilian states. Therefore, prevalence and incidence measures are obtained mainly based on cases reported in the literature, certainly underestimating the real epidemiological importance, especially regarding outbreaks and epidemics.
Figure 1.

Ulcerated lesions on the hands of three members of the same family, at the beginning of the zoonotic transmission sporotrichosis epidemics in Rio de Janeiro, in 1997, treated at Hospital Universitário Pedro Ernesto
Although human or animal sporotrichosis cases were published in the states of Amazonas, Pará, Minas Gerais, Espírito Santo, São Paulo, Rio de Janeiro, Paraná, and Rio Grande do Sul, most cases occur in the South and Southeast Brazil.24
The advances in the microbiological knowledge along with the use of molecular tools led to important advances concerning epidemiological studies, enabling the identification of the Sporothrix species in 14 Brazilian states, indicating that sporotrichosis is more widespread than previously thought for the Brazilian territory.24
In Brazil, there are two important disease transmission routes for humans, a sapronotic route involving direct contact with the soil and decomposing organic matter; and a zoonotic route, in which felines participate actively in the disease transmission. The outbreaks from classic transmission route, in which S. schenckii and S. globosa prevail, required the removal of fungus sources in nature. The alternative transmission route, mainly involving horizontal animal transmission (cat-cat), as well as zoonotic transmission, requires different epidemic control strategies. Such measures include the street animals neutering and the treatment of sick cats, as well as the education about responsible ownership of animals, knowledge of the main aspect main aspects of Sporothrix transmission, especially in hyperendemic areas. Dead infected animals must be incinerated, rather than buried, thus avoiding S. brasiliensis dissemination in the soil and the pathogen progression in nature.
Even though sporotrichosis has been described worldwidely, there is a curious divergence regarding the geographic distribution and the incidence of the etiological agents.25 Indeed, some species are more ubiquitous than others. In Asia, especially China, S. globosa is estimated to be the etiological agent in 99.3% of the human sporotrichosis cases.26,27 In other endemic areas, such as Australia and South Africa (94%), also in North America and part of South America (89%), S. schenckii is the predominant species.26 In the South and Southeast Brazilian regions, S. brasiliensis (88%) is the main etiological agent of human and animal sporotrichosis.28,29
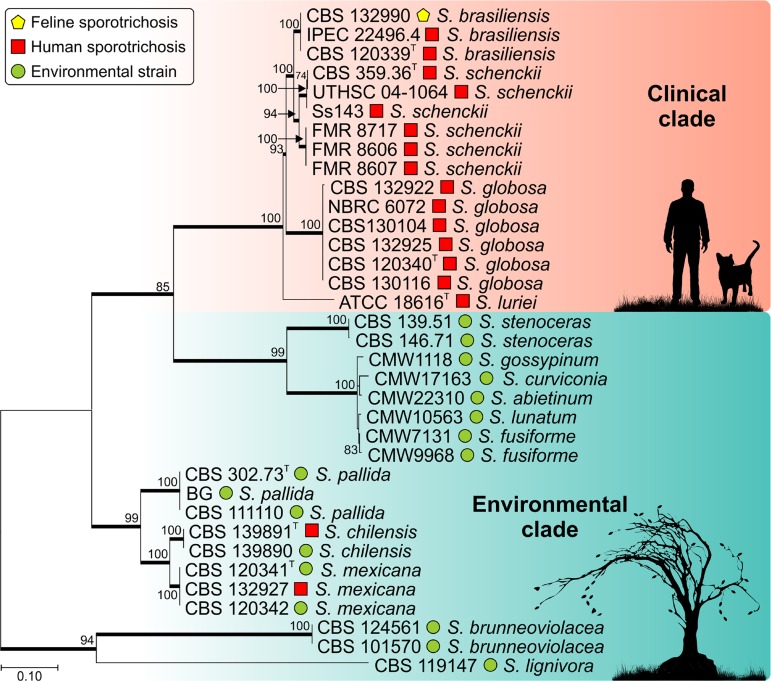
Over a century, since 1898, Sporothrix schenckii was described as the unique species responsible for the sporotrichosis cases.2,30 However, the advent of molecular biology techniques, directly applied to fungus taxonomy researches, demonstrated that the classic agent S. schenckii actually consists of a group of cryptic species, phylogenetically related. Currently, Sporothrix comprises 51 taxons, divided into a clinical clade (mostly human pathogens), including S. brasiliensis, S. schenckii, S. globosa, and S. luriei, an environmental clade, composed by some other species complexes, such as S. pallida and S. candida with five species each, S. inflata with three species, S. gossypina with 12 species, and S. stenoceras with six species (Figure 2).31,32
Figure 2.
Phylogenetic relations between the clinical and environmental clade members in Sporothrix, based on calmodulin sequences (exon 3-5). Available at GenBank (https://www.ncbi.nlm.nih.gov/genbank/). Method: Maximum likelihood The numbers close to the branches refer to resample percentages (1000 bootstrap)
It is noteworthy that such a phylogenetic split is accompanied by different ecological behaviors, considering that S. schenckii and S. globosa have already been isolated from humans, animals, and soil.33,34 Attempts to isolate S. brasiliensis from the soil have not been successful. However, this species is frequently isolated from human and feline clinical samples.28,35 Sporothrix luriei is a rare human sporotrichosis agent described from a single clinical isolate in South Africa.36,37 Historically, the overlapping of phenotypical characteristics has led to incorrect identification based only on micromorphological analyses of environmental species.
Environmental clade of Sporothrix species are rarely agents of human sporotrichosis, causing opportunistic infections. The infection route also involve traumatic inoculation of fungal propagules present in soil and organic matter. The S. pallida complex consists of five soil species, three of which are rare agents of human infection: S. chilensis, S. mexicana, and S. pallida.38-40 The environmental clade also includes S. stenoceras identified from cutaneous lesions in humans.41 These environmental species are usually low-virulence organisms to the warm-blooded, vertebrate host.38,42
Sporothrix spp. are thermodimorphic fungi, presenting the filamentous form (saprophytic phase) in nature or in vitro at 25°C, and developing yeast-like cells (parasitic phase) in the mammal host or in vitro at 35-37°C.43 This temperature-induced transition is an important morphological adaptation for the infection in mammals. The mycelium-to-yeast conversion occurs successfully among the species within the clinical clade (S. brasiliensis, S. schenckii, S. globosa, and S. luriei), while the environmental species (S. inflata, S. humicola, S. pallida, S. mexicana, S. chilensis, among others) show deficient morphological transition, producing few yeast-like cells. Perhaps, the successful emergence of S. brasiliensis in mammals, as well as the low virulence of environmental species may be related to the thermotolerance or thermosensitivity of these species, respectively.44 Another important virulence factor is the Sporothrix ability to produce melanin. Melanin induces fungal escape from the host's defenses, and is also considered a resistance factor against some antifungal drugs, such as amphotericin B, itraconazole and terbinafine.45,46
The virulence profiles change depending on the pathogen characteristics and the host defenses. Sporothrix brasiliensis is the most virulent species, due to its ability to invade tissue and lead to death, whereas S. schenckii has different levels of virulence and S. globosa exhibits little or no virulence in murine models.42,47-49 The environmental species of Sporothrix present low virulence in murine models, with low invasive potential, and the host is able to control the infection a few weeks after inoculation.38,42
The host's defense against the Sporothrix species has not yet been established. The fungus' cell wall components, especially the 70kDa glycoprotein (gp70), has a protective effect in the host, mediated by T-helper cells (Th1 in humans), but paradoxically, it also makes the adherence of conidia to the epithelium, increasing fungal invasive potential. The cell-mediated immune response seems to be responsible for eliminating or controlling infection. However, the humoral immune response elicits specific antibodies against the Sporothrix' cell wall.5,50 The dissemination of sporotrichosis is usually related to cellular immunity deficiencies, such as AIDS.51
CLINICAL ASPECTS
Usually, the clinical manifestations of sporotrichosis are divided into cutaneous and extracutaneous, the former is more frequent.22 After the zoonotic sporotrichosis epidemic in the state of Rio de Janeiro, new clinical presentations, uncommon until then, were identified. For this reason, a new classification was proposed, to better describe the clinical features of the patients cared by the reference sporotrichosis teams.52 In the present article, the authors propose an update of this clinical classification based on the group's expertise (Table 1).
Table 1.
Clinical classification of sporotrichosis
| Lymphocutaneous | |
| Fixed cutaneous | |
| Multiple inoculation | |
| Mucous membrane | |
| Ocular | |
| Nasal | |
| Others | |
| Systemic | |
| Osteoarticular | |
| Cutaneous disseminated | |
| Pulmonary | |
| Neurological | |
| Other locations/sepsis | |
| Immunoreactive | |
| Erythema nodosum | |
| Erythema multiforme | |
| Sweet's syndrome | |
| Reactive arthritis | |
| Spontaneous regression |
Modified from: Lopes-Bezerra, et al. 2006.52
Nearly 80% of the affected patients present the lymphocutaneous form.52 Initially, the lesion has a papulonodular appearance where the fungus was introduced into the skin, appearing between two to four weeks after the trauma. Afterwards, the lesion may ulcerate, and fistulize draining a purulent discharge. This is so-called the inoculation chancre. The lesions, usually nodules, progress along the regional lymphangitic channels, upwards or downwards depending on the anatomical site, after some weeks. Later, these nodules, may ulcerate, fistulize, and heal, caractherizing a gumma (Figures 3A and 3B). The fixed cutaneous form consists of a single lesion, usually similar to the inoculation chancre, with no regional lymphatic spreading (Figure 3C). In some occasions, the disease may appear as larger ulcers with well-defined and framed borders, or erythematous-scaly, papulopustular, vegetative, infiltrative, or crusty lesions (Figures 3D-F). Some patients exhibit multiple skin lesions, disseminated on the tegument, with no systemic invasion and polymorphic appearance, all of them arising at the same time. In general, these patients are immunocompetent individuals who describe having multiple traumas.
Figure 3.
A. Lymphocutaneous form in adults (ascending lymphangitis); B. lymphocutaneous form in a child's face (descending lymphangitis); C. fixed cutaneous form on the back of the hand; D, E, F. systemic form with disseminated skin lesions in an AIDS patient
Although any mucous membrane may be affected by sporotrichosis, the ocular mucosa is more commonly involved, causing conjunctivitis, episcleritis, uveitis, choroiditis, and retrobulbar lesions, among others (Figure 4A).53-55 When the lacrimal duct is affected, dacryocystitis may occur as sequela.56,57 The retrobulbar lesions, such as chorioretinitis, are more frequently related to hematogenous spread, and anterior lesions are associated with the fungal innoculation. The simultaneous affection of the ocular mucosa and the regional lymph nodes is not rare, and it is one of the causes of the Parinaud syndrome.58
Figure 4.
A. Granulomatous lesion at the upper eyelid ocular conjunctiva; B. primary lymphocutaneous lesion on the finger; and C. pseudovesicular lesions over an erythematous plaque on the back of the same patient - Sweet's syndrome (immunoreactive form)
The bones and joints may be involved by direct trauma, by the invasion through a preexisting overlying cutaneous lesion or secondary to a hematogenous spreading, the latter at highest risk of sepsis due to the deep site of infection. Osteoarticular sporotrichosis may appear as a monoarthritis associated or not with an overlying cutaneous lesions, as well as bone resorption and osteolytic lesions in the most severe cases.59,60 The synovial fluid exhibit increased cellularity mostly consisting of polymorphonuclear leukocytes, low glucose and high protein levels.
The respiratory transmission through the inhalation of Sporothrix propagules is acceptable, characterizing the primary pulmonary systemic form of sporotrichosis. The lungs may also be affected by the hematogenous spread, mainly in immunosuppressed patients presenting with the disseminated systemic form of sporotrichosis. The signs and symptoms may include coughing, dyspnea, hemoptoic, etc, depending on the type and site involved. Radiologic images, such as chest-radiography or computerized tomography, show diverse features. The upper lobes are mostly affected, presenting cavitary, reticulonodular infiltrative, or even fibrosis or tumoral aspects.61-64 Probably the disease is misdiagnosed in areas with high endemicity, either due to the lack of knowledge by the medical doctors, or to the unspecific clinical signs and symptoms.65
The imunosuppressed patients are at higher risk for bloodstream dissemination of sporotricosis due to alcoholism, or the chronic use of illicit drugs, the use of immunosuppressive medication, or secondary to immunodeficiency such as AIDS. In theses cases the bones and joints, the lungs and central nervous system, in addition to the skin and mucous membranes, are preferably affected, although any organ may be involved (Figures 3D-F). These patients also show heterogenous and polymorphic tegumentary lesions, and must have a special attention in their medical care, particularly AIDS. Moreover, they may develop systemic manifestations that include severe bone lesions, hematogenous disseminated skin and mucosal lesions, lung and spleen involvement, as well as the neurotropism shown by S. brasiliensis. They may progress to sepsis, leading to death.51,64,66 Curiously, systemic sporotrichosis reports in transplanted patients are not frequent. Similar to American tegumentary leishmaniasis, which is an important differential diagnosis, the centrofacial region is commonly affected in immunocompromised patients (authors' note).
At the other end, as occurs in other infectious diseases, some patients heal spontaneously, while others develop hypersensitivity clinical forms, such as erythema nodosum, erythema multiforme, and Sweet's syndrome due to an exacerbated immune response against the fungus. Also, reactive arthritis can occur, it is usually polyarticular and migratory, frequently disappearing with the specific treatment for sporotrichosis (Figures 4B-C).67-69
In general, the lesions heal leaving fibrotic scars that may alter the organ function depending on the site of infection, for instance, the tear duct or the lungs. Unaesthetic scars are particularly important in younger patients, especially in exposed areas, given that the disease leads to fibrosis, sometimes causing tissue or hair loss, such as eyelashes, in the case of bulbar conjunctival lesion.52
The children, the elderly, the pregnant women, and the immunosuppressed AIDS patients are groups that require a special attention.70,71 Children generally have more prolonged and frequent contact with animals and, therefore, are commonly infected. Nevertheless, they also exhibit a greater immunological resistance with limited lesions such as the fixed form, usually on the face; exhibiting slightly elevated serological titers.71 The facial contact with animals also predisposes this age group to ocular mucosal lesions. On the other hand, the task of taking care of animals is usually assigned to the elderly, especially females. In this age group, the host immune defense is declining, which means that, in many times, there may be a more extensive and severe clinical presentation of the disease.
DIFFERENTIAL DIAGNOSIS
Due to the diversity of clinical presentations, sporotrichosis may be clinically similar to many other infectious and non-infectious diseases, both tegumentary and systemic. The most common are tegumentary leishmaniasis, pyodermitis, cat-scratch disease, cutaneous nocardiosis, chromomycosis, syphilis, rosacea, granuloma annulare, pyoderma gangrenosum, osteomyelitis, arthritis with a different etiology, such as rheumatoid, also cutaneous and pulmonary tuberculosis, tumoral lesions, especially in the lungs and in the central nervous system, and meningitis, besides others. In regions of high endemicity, the epidemiological background must be taken into consideration.
LABORATORY DIAGNOSIS
Mycology
The gold standard for the diagnosis of sporotrichosis is the isolation and the identification of the Sporothrix species from clinical samples such as skin lesions, biopsy, aspirated from floating abscesses, as well as sputum, pus, synovial fluid, blood, and cerebrospinal fluid.8,72 It is a simple and low-cost diagnostic method, although it may not be useful for some systemic and atypical forms of sporotrichosis.52,73
Seldom, the direct microscopy (DM) made with potassium hydroxide (KOH) preparations, whether or not in dimethyl sulfoxide, exhibits fungal elements. When present in the tissue, Sporothrix spp. show several yeast-like structures, oval to round, and more commonly elongated, "cigar-shaped", measuring approximately 5-8 µm.74 Compared to the culture, DM presents low sensitivity and specificity, being positive in sporotrichosis mainly in immunosuppressed patients.75,76 Giemsa-stained smears, obtained from pus or biopsy imprints, enhance the test's sensitivity.8 On the other hand DM is more sensitive in animals, particularly felines, due to the great amount of fungal cells in the tissues, exhibiting sensitivity of nearly 85% compared to the culture.77 Sporothrix spp. grow in culture media used routinely, at room temperature (25ºC-30ºC), such as Sabouraud dextrose agar with chloramphenicol or gentamicin, added to inhibit bacteria; Mycosel agar containing cycloheximide, to reduce saprophytes, and BHI (Brain Heart Inffusion), an enriched medium.8,76 Sporothrix spp. is usually isolated in 4-6 days, for samples collected from skin lesions, and in 10-19 days, for extracutaneous lesions; time can also vary depending on the species of Sporothrix.73,76,78,79
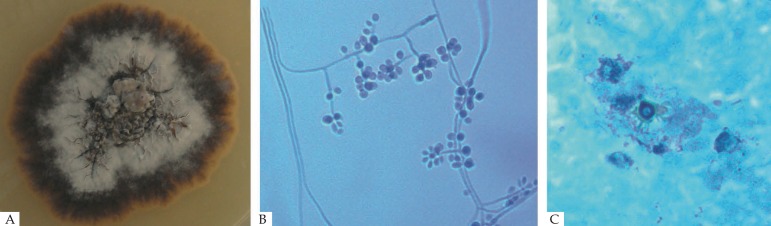
Colonies are identified phenotypically by the membranous appearance of the surface, off-white to cream color and a black halo, or they may be dark from the beginning, depending on the species, and on the nutritional and environmental conditions (Figure 5A). The colony microscopy of the clinical clade exhibit delicate branched septate hyaline hyphae, a conidiophore producing at the tip pyriform, oval to round, hyaline conidia, arranged sympodially as a bouquet, in addition to sessile pigmented conidia (Figure 5B).33,74 The thermodimorphism of the Sporothrix species of clinical interest is confirmed by reverting the mycelium-to-yeast form in BHI, after incubation at 37ºC. The yeast-like colony has a creamy color surface. For phenotypical confirmation of Sporothrix species, other culture media are used, such as corn meal agar to define the conidia shape and color. For instance, ovoid dematiaceous conidia suggest S. brasiliensis, while triangular conidia are characteristic of S. schenckii; it is also used to distinguish S. mexicana from S pallida.33 In addition to the thermotolerance of the Sporothrix isolates, the potato dextrose agar (PDA), a culture media poor in nutrients, is useful in comparying fungal morphology and growth (measured by the colony's diameter). Sporothrix brasiliensis forms dark black fast growing colonies. Exceptionally, Sporothrix isolates grow at temperatures above 37ºC, regardless of the species.
Figure 5.
A. Macromorphology of Sporothrix brasiliensis; B. Micromorphology reveals delicate, hyaline septate hyphae, conidiophore that originates primary hyaline conidia in a bouquet arrangement (cotton blue, x400); C. Asteroid body (Grocott, X400)
Assimilation of sugars such as glucose, raffinose, ribitol, and sucrose are some of the carbon compounds used in physiological tests; the Sporothrix isolates show different pattern of assimilation.79
Histopathology
The sensitivity of histopathology test in humans is low due to the paucity of fungal elements in the tissue. The inflammatory infiltrate is better observed by hematoxilyn-eosin stain, and PAS or methenamine silver is used to identify the fungal structures.8 According to the literature, fungal structures are present in 18 to 35.3% of the cases, depending on the technique.76,80,81 The tissue reaction consists of diffuse chronic granulomatous dermatitis, many times with a central abscess. The histological sections may exhibit hyperkeratosis, acanthosis, and intraepidermal microabscesses. The granuloma in palisade arrangement, consisting of a neutrophil and eosinophil central area, an intermediate layer with mononuclear cells, and lymphocytes and plasmacytes at the most external area, may be observed in skin lesions.82 The presence of asteroid bodies or Splendore-Hoeppli phenomenon may point to the diagnosis of sporotrichosis. It consists of an eosinophil material surrounding the fungal cell, probably a deposit of immunoglobulin attached to the microorganism wall. However, it can occur in other infectious or granulomatous diseases (Figure 5C).8
Serology
Different techniques of immunoelectrophoresis, agglutination, and immunodiffusion using crude antigenic fraction were proposed for the serodiagnosis of sporotrichosis, but the sensitivity and specificity were low.83,84 Consequently, they were replaced by more sensitive tests, such as the immunoenzymatics, especially ELISA (Enzyme Linked Immuno Sorbent Assay) and Western blotting, both with faster results. The use of serology, a fast and non-invasive test for the diagnosis of sporotrichosis, was possible when specific antigens were characterized and standardized. These tests are used as auxiliary tools for cutaneous forms and to diagnose systemic manifestation or atypical forms of sporotrichosis. They are useful for screening, to control treatment follow up and drug withdrawn in difficult clinical presentations. Serum antibody titers may also monitor relapses.52,85-87
Serological ELISA test using the SsCBF (Sporothix schenckii Con A-Binding Fraction), a cell wall antigen from the yeast phase of S. schenckii, has proven efficient for the detection of IgG antibodies in the serum of patients with cutaneous sporotrichosis.88 Tests performed in serum samples of patients with different clinical sporotrichosis forms resulted in high sensitivity and specificity rates, 90% and 80% respectively, in addition to high reactivity in feline serum samples.85,89 ELISA test using the SsCBF exhibited reactivity with other clinical specimens, such as cerebrospinal and synovial fluid, with high positivity and low cross-reaction rates.59,85 There is an effective clinical-serological correlation which allow therapeutic monitoring, and can be used whether to maintain or suspend the treatment of difficult cases.57,67,71 An exoantigen isolated from the filamentous form of S. schenckii was used in the ELISA test, with 97% of sensitivity, and 89% of specificity, when evaluating different serum samples from patients with sporotrichosis.86
Two other important cell wall components in Sporothrix spp have been studied as new biomarkers for sporotrichosis diagnosis, the glycoproteins of 60 kDa and 70 kDa, identified as 3-carboxy-muconate cyclase of the Sporothrix proteome, as glycoforms and isoforms.5 Such glycoproteins seem to behave as a factor of virulence, they are expressed in the most virulent Sporothrix isolates, and contribute to the fungus adherence and immunomodulation.48,90-93 The produced mAb P6E7 antibody against the gp70 caused in vivo protection through passive immunization of mice infected with S. schenckii. It is considered to be a strong candidate for a therapeutic vaccine against sporotrichosis.91,94
These tests are not commercially available, being restricted to certain research centers, especially due to the lack of Public Health financing in Brazil, where sporotrichosis is endemic or hyperendemic, depending on the country region.
Molecular
The phenotypical identification of the different Sporothrix species have, as a disadvantage, the use of tools that are usually laborious, longstanding, with variable results, especially for the species inserted in the clinical clade, which could lead to incorrect identification.39,95-97 Nowadays, the molecular boundaries among the Sporothrix spp. are defined, enabling the development of numerous genetic markers for recognition and identification of clinical specimens.44 The development of fast and low-cost genotyping methods is important for diagnosis, as well as for epidemiological studies, considering that the pathogenic species in Sporothrix differ in terms of their geographical range, virulence, and susceptibility to antifungal drugs.
DNA sequencing - PCR (Polymerase Chain Reaction) technique. The identification of Sporothrix isolates with clinical interest, which frequently infect the vertebrate host, may be performed by the amplification and partial sequencing of ribosomal operon, including the ITS1, 5.8s, and ITS2 regions. The ITS (Internal Transcript Spacer) region operates as a universal marker for the identification of Sporothrix.31 The human and animal origin specimens are distributed in the S. brasiliensis, S. schenckii, S. globosa, and S. luriei clades.32 The environmental Sporothrix species are located at a relatively large phylogenetic distance. However, it is worth noticing that, in the environmental clade, in addition to the ITS region, the use of protein coding genes for the recognition of cryptic species, especially in the S. pallida complex, will be required.38 Protein coding genes, such as the beta-tubulin (BT2), calmodulin (CAL), and the elongation factor 1α (EF-1α) may be used to increase the taxonomic resolutions among the clinical interest species, or even to identify rare agents within the S. pallida complex, in the environmental clade, such as S. pallida, S. mexicana, and S. chilensis. The region between the 3 and 5 exons of the calmodulin gene appears as the main marker for recognition of clinical interest Sporothrix.98-101 In addition to the possibility of identifying the infectious agent, protein-coding genes are commonly used in studies on genetic diversity, population structure, and molecular epidemiology of sporotrichosis.29
PCR-RFLP - the amplification of a target sequence in the fungus genome by means of PCR, followed by amplicon digestion with one or a combination of restriction enzymes (RFLP), has been successfully used to detect inter- and intra-specific variability in several fungus species. In clinical interest Sporothrix spp., the identification of morphologically similar species becomes possible with the use of PCR-RFLP. After the partial amplification of the calmodulin gene (exon 3-5), the amplicon digestion with the HhaI enzyme takes place, producing five different restriction profiles (species-specific), representing all species with medical importance.102 Some important advantages of this technique include low-cost, fast and easy execution, associated with the absence of need for advanced instruments.
Species-specific PCR - the identification of Sporothrix spp. may be performed by means of PCR, by using primers that selectively amplify DNA from S. brasiliensis, S. schenckii, S. globosa, S. mexicana, S. pallida, and S. stenoceras.103 Therefore, the primer sequences are preserved within a single target species and inter-specifically divergent. This technique is a low-cost, fast and robust molecular tool, capable of detecting and identifying small pathogen DNA based on isolated specimens, as well as complex biological samples (biopsy, soil, mixed cultures, etc.), with no need to isolate the pathogen.
Rolling Circle Amplification (RCA) is a method that provides high sensitivity and robustness, which may be applied from monosporic cultures to environmental samples, with potential for ecology studies.104 The identification of Sporothrix based on RCA has proven to be a reliable identification tool, alternative to DNA sequencing, although little used in the mycological diagnosis, despite being a simple and powerful technique, capable of synthesizing large DNA amounts based on very low initial concentrations.104,105
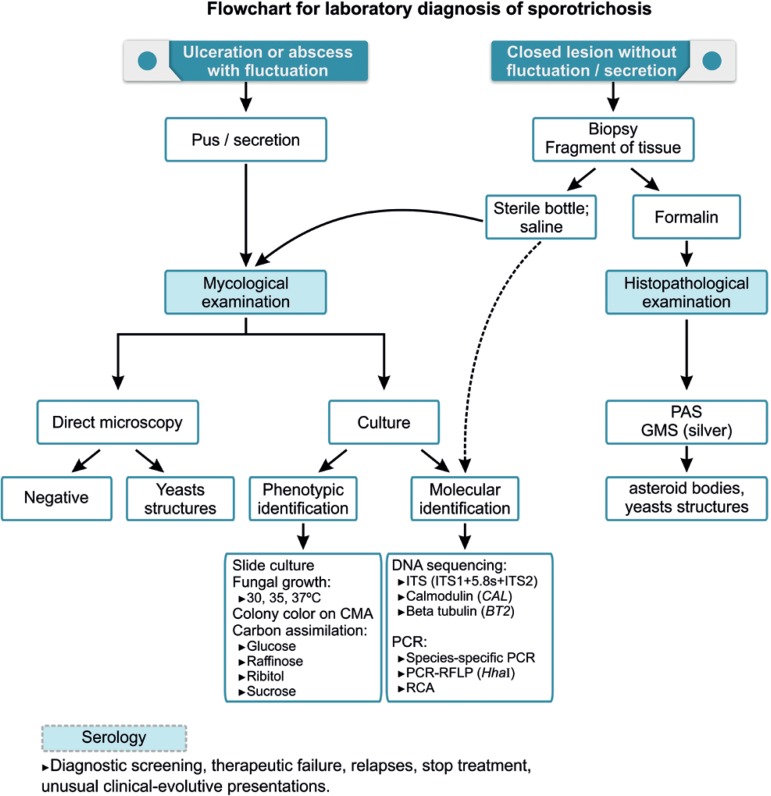
Figure 6 represents a flowchart that synthesizes the techniques used for laboratory diagnosis of sporotrichosis.
Figure 6.
Flowchart for laboratory diagnosis of sporotrichosis. GMS (Gomori methenamine silver); CMA (corn meal agar); 'C' - carbon; ITS (Internal Transcript Spacer); PCR (Polymerase Chain Reaction)
TREATMENT
The choice of treatment for sporotrichosis depends essentially on the clinical form of the disease, the host's immunological status, and the species of Sporothrix involved.
Drug
Itraconazole, potassium iodide, terbinafine, and amphotericin B are the drugs currently available in Brazil for treating sporotrichosis. The first three are administered orally, while the last one is administered intravenously.
Itraconazole is considered the drug of choice due to its effectiveness, safety, and posologic convenience, and it is classified having an AII scientific evidence level.72,106 It is a fungistatic drug that acts by inhibiting the synthesis of ergosterol in the fungus cell wall. It may be used in healthy patients with limited lesions, as well as in immunosuppressed patients and in the systemic form, but not in life-threatening cases of dissemination/sepsis. It is offered in 100mg capsules and must be administered along with the main meals, for better absorption. The dose ranges from 100 to 400mg/day, depending on the disease severity. The treatment should be started with 100mg/day, which is effective in most cases. It may be administered continuously or intermittently (pulse).107 The main adverse effects reported are headache and gastrointestinal disorders, which are, in most cases, tolerable. It is hepatotoxic, teratogenic, and embryotoxic, and may not be used in patients with liver diseases or in pregnant women (risk category C). Its greatest disadvantage is the possibility of drug interaction, as a consequence of the dependent metabolism on CYP 3A4 common to other several drugs. It may cause an increase or a reduction of serum drug concentrations frequently used by elderly patients usually affected, also these drugs may reduce or increase serum itraconazole levels. Childbearing women must be warned about the risk of oral contraceptive effect reduction. In addition, there is a risk of sudden death, especially in patients suffering from congestive heart failure, due to its negative inotropic effect on the cardiac muscle.108 Complete blood count, biochemistry, and liver function tests should be performed prior to the treatment and after 3-4 weeks. If serum levels are whithin normal ranges, the tests should only be repeated at the end of the treatment.
Potassium iodide (KI) has been used for treating sporotrichosis, since 1903, as initially suggested by Saboraud.7 At that time, specific antifungal drugs were not available and iodide was used for several infectious and non-infectious diseases. The KI mechanism of action is not yet completely understood, despite its already known action on the immune response, destructuring granulomas, on neutrophil chemotaxis, as well as on phagocytosis of Sporothrix cells.109,110 The scientific evidence level is AII, the same of itraconazole, and it may be prepared as saturated or concentrated solution. In the saturated solution, each drop contains 0.07g, and in the concentrated solution, 0.05g.111 Doses of up to 4-6g/day for adults are recommended. However, a recent study has demonstrated that doses of 1-2g/day for children, and 2-4g/day for adults, administered t.i.d with milk, juice or yogurt are effective to cure most patients.112 The treatment starts with lower doses, increasing daily in both intakes until the effective and tolerated dose is reached. This is especially useful for the elderly and for children, as it is available in the liquid form. KI is indicated for localized sporotrichosis cases in patients whose immunity is preserved, but it may also be used in immunoreactive forms, such as erythema nodosum or reactive arthritis, due to its immunomodulatory effect. It is contraindicated for patients with thyroid dysfunction, kidney failure, iodine allergy, autoimmune diseases, and in pregnant and nursing women (risk category D). Up to now, it is not indicated for patients who have deficiency of immune response, and extensive or systemic clinical manifestations. The main adverse events are metallic taste and nausea, followed by acneiform eruption. In addition to the laboratory tests for monitoring itraconazole use, for KI it is important to check the TSH and T4 serum levels during treatment, although a slight increase in TSH serum levels is considered to be physiological.111
Terbinafine, a fungicide allylamine that inhibits the synthesis of ergosterol in the fungus cell wall, is an excellent therapeutic option for patients with contraindications to itraconazole or KI use, as its effectiveness in the sporotrichosis treatment is well demonstrated.113,114 This medication is metabolized through the CYP2D6, which is not involved in many other drugs, thus it exhibits fewer drug interactions, and it is especially useful for elderly patients with other comorbidities. It is available in tablets of 125 and 250 mg facilitating pediatric administration. The recommended dose is 250 mg/day, but it may be increased up to 500 mg/day for adults. The pediatric dose depends on the child's weight and is the same recommended for treating dermatophytosis. It may cause headaches, nausea, taste alteration, and neutropenia. Terbinafine is contraindicated for patients with lupus erythematosus, and is considered a risk category B drug during pregnancy. Its use has not yet been tested for other clinical forms other than the cutaneous. The laboratory exams are the same as those for monitoring the treatment with itraconazole.
In severe, life-threatening cases, amphotericin B, deoxycholate or, preferably, liposomal, is recommended until the clinical improvement has been achieved, when it should be replaced by itraconazole.72 Amphotericin B is a polyene that links to the ergosterol of fungal membrane, modifying its permeability. When administered intravenously, amphotericin B is cardiotoxic and nephrotoxic, thereby requiring constant evaluation of kidney function and of the serum potassium levels. The total cumulative dose recommended ranges from 1 to 3g for deoxycholate presentation, or the corresponding liposomal dose. The precautions and types of amphotericin B administration for sporotrichosis treatment are the same as those used in other mycoses for which the drug is indicated. This is the only drug recommended for pregnant women with severe disease, given that it is not teratogenic, although it may worsen metabolic disorders that are already common during pregnancy. 115
Sporotrichosis treatment must be maintained until the clinical cure is reached, which usually occurs within 2 to 3 months. It is not necessary to maintain the drug use for 1 to 3 months after the cure, as previously recommended. Clinical cure is considered when there is no disease's activity, such as pus, exsudation, or crust in the skin lesions, even if a discrete erythema, fibrosis, or milia appear during the healing process. Systemic forms require longer treatment, ranging from 6 to 12 months.72
Miscellaneous
The local heat was initially used to treat chromomycosis, it is based on the fungus' thermosensitivity, and may be useful when conventional drugs are contraindicated.115,116 Cryosurgery using liquid nitrogen may be used as a therapeutic complement in refractory cases, especially when lesions are crusty and infiltrate, as well as in isolated cases of localized lesions in immunocompetent patients. Electrosurgery and surgical removal of small lesions constitute other therapeutic options in selected cases. All therapeutic methods described may be used as monotherapy or as adjuvant treatment. Photodynamic therapy was tested in vivo and in vitro for the treatment of skin sporotrichosis.117
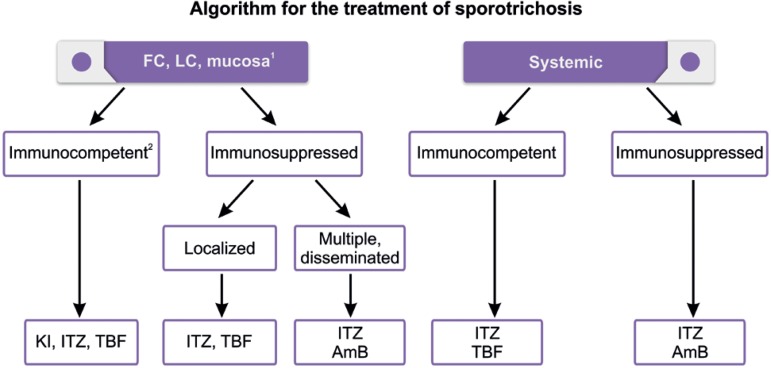
Figure 7 shows basic steps to guide the therapeutic choice in sporotrichosis, and table 2 provides the summary of the main drugs administered in sporotrichosis and their corresponding doses.
Figure 7.
Algorithm for the treatment of sporotrichosis. LC - lym phocutaneous; CF - fixed cutaneous; KI - potassium iodide; ITZ - itraconazole; TBF - terbinafine; AmB - amphotericin B
1Hyperkeratotic or refractory cutaneous lesions: heat, cryosurgery, electrosurgery, exci sion/drainage, Kl + ITZ or Kl + TBF
2Children, elderly, immunoreactive forms: Kl
Pregnant women: Heat, cryosurgery, AmB
Modified from: Orofino-Costa, et al. 201570
Table 2.
Main drugs used in sporotrichosis treatment with the corresponding dosages
| Continuous | Pulse | Continuous | Pulse | 1.42g/mL (0.07g/drop) | |
| Adult | 100-400mg/d2 | 400mg/d | 250-500mg/d4 | 500mg/d | 2- 4g/d |
| 7d/month | 7d/month | ||||
| Pediatric | 3-5mg/Kg/d3 | ------ | 62.5 - 250 mg/d5 | ---- | 1-2 g/d |
| Dosage | 1-2 x/d | 2x/d | 1-2 x/d | 1-2 x/d | 2 x/d |
| Laboratory control 6 | Blood count, biochemistry, LFT | Blood count, biochemistry, LFT | Blood count, biochemistry, LFT, TSH, T4L | ||
Take at mealtime;
Start at 100mg/d;
Maximum of 200mg/d;
Start at 250mg/d;
Dose varies according to weight;
Prior to treatment, at 3-4 treatment weeks, at the end of the treatment. LFT - liver function tests Adapted from: Orofino-Costa, et al. 201570
Other considerations
There are important differences regarding in vitro sensitivity to the main antifungal drugs and the different etiological agents, reinforcing the importance of the correct identification for properly treating sporotrichosis. Sporothrix brasiliensis presents the best response to antifungal drugs, while S. mexicana is more tolerant to drug action.118 Epidemiological analyses reveal that the in vitro susceptibility profile has been changing over time, emphasizing the emergence of S. brasiliensis isolates tolerant to itraconazole.119 In this context, potassium iodide, terbinafine, and posaconazole may be alternative drugs against S. brasiliensis, especially in refractory cases, or for those with no satisfactory in vivo response to itraconazole.96,112 KI has been used in association with itraconazole, for refractory mycosis in felines. However, its use in immunosuppressed humans needs to be better evaluated due to the possibility of changes in the immunological reactivity, and worsening of the underlying disease.120 This association has been used in humans with conidiobolomycosis.121 The effectiveness of this combination of drugs is probably due to the different mechanisms of action and synergism of both drugs. KI capsules still needs to be tested in humans regarding absorption, pharmacodynamics, and bioavailability for the effective dose adjustment in the treatment of sporotrichosis.
The drugs 5-fluorocytosine, caspofungin, and fluconazole do not exhibit in vitro antifungal activity against S. brasiliensis, S. schenckii, S. globosa, or S. mexicana.122,123 In vitro analyses indicate significant differences among the minimum concentrations required to inhibit the growth of Sporothrix spp. and the required concentration to reduce the number of colony-forming units, demonstrating the fungistatic and non-fungicide effect for the most available antifungal drugs.
PROGNOSIS
Immunocompetent individuals with skin or mucosal clinical forms usually heal in a short period of time, although fibrous scars are frequent complaints leading to functional or unesthetic sequelae. In immunosuppressed patients, especially AIDS, the disease may disseminate and cause death. Untreated patients with chronic skin lesions may develop severe clinical forms, with systemic manifestations, frequently requiring inpatient treatment.
PERSPECTIVES
For over a century, sporotrichosis was described as an occupational disease, with a strong rural profile. However, in the last decades Sporothrix spp. as a threat to the warm-blooded vertebrate hosts' health has emerged. The close relation between S. brasiliensis and the feline host is curious, so that it causes large epizooties in urban areas.124 Indeed, zoonotic pathogens are more often associated with emerging diseases than the non-zoonotic pathogens.125 This indicates the need to investigate the S. brasiliensis' transmission dynamics involving cats and humans. Such a transmission route (cat-man) broke a paradigm in a disease in which epidemiology had already been considered to be resolved, to a large extent. Ecological studies are important, given that the uncertainty regarding the fungus' reservoirs in the environment and reasons for the fluctuation of Sporothrix population still exists.
The knowledge of the epidemiological-molecular profile is essential to understand the dynamics of species occurrence, from the standpoint of both the characterization of a differentiated clinical standard and the response to the treatment, as well as the implementation of strategic Public Health policies intended to control epidemics. The low-cost molecular methods are important because they provide fast and accurate results, particularly during disease outbreaks. However, for countries with limited health budgets, isolating the Sporothrix in culture media is still the best diagnostic method, concerning both cost and positivity.
Investigations on the host-parasite interaction have evolved regarding both cell and humoral immune responses. However, recent researches involving 3-carboxy-muconate cyclase (gp60-gp70) and the humoral activity reconducted the seek for specific antigens that could be used in the diagnosis and antibodies based vaccines.5 Anti-gp70 antibodies are potentially useful for disease's therapy because they strongly reduce the host fungal burden, thus preventing Sporothrix adhesion to the extracellular matrix components, or inducing the yeasts opsonization in the host-pathogen interaction.126
The need to develop new antifungal drugs is encouraged by the increasing number of refractory cases resulting from the emergence of the resistance phenotype among the etiological agents.127 Currently, researches on alternative treatments for sporotrichosis reveal promising molecules, such as terpinen-4-ol and farnesol, miltefosine, TCAN26 (a structural analogous of miltefosine) and the H3 molecule (an inhibitor of the sterol methyltransferase enzyme).127-131 However, it should be pointed out that it is still necessary to use appropriate animal models and clinical tests to ensure the effectiveness and safety of treatment for such alternatives.
ACKNOWLEDGMENTS
The authors thank the technical team at the Mycology Laboratory at the Pedro Ernesto University Hospital (UERJ), for their support during all stages of preparation of this article. The authors also would like to thank Raphael da Silva Roma for his technical computer support and his assistance in preparing the figures.
QUESTIONS.
-
The most common clinical presentation of sporotrichosis in Brazil is:
lymphocutaneous
fixed cutaneous
osteoarticular
pulmonary
-
Concerning the sporotrichosis transmission, it may be stated that:
zoonotic transmission only takes place when the etiological agent is Sporothrix globosa
transmission by means of trauma only happens when the etiological agent is S. schenckii
c. respiratory transmission results from inhalation of Sporothrix conidia
respiratory transmission is restricted to specific geographic regions
-
The histopathological exam in sporotrichosis shows:
high sensitivity and low specificity
low sensitivity and high specificity
high sensitivity and high specificity
low sensitivity and low specificity
-
To isolate Sporothrix spp. the following basic fungus culture media are preferably used:
Cereal agar (Corn meal agar) and BHI (Brain Heart Infusion)
Mycosel agar and cereal agar (Corn meal agar)
Sabouraud agar and PDA (Potato Dextrose Agar)
Sabouraud dextrose agar and Mycosel agar
-
The asteroid body found on the dermis of the patients with sporotrichosis:
consists of non-specific inflammatory cells
confirms the diagnosis of sporotrichosis
represents a probable immunological reaction to the fungal cell
suggests the host’s immunodeficiency
-
It may be stated that serology for the diagnosis of sporotrichosis:
is only indicated for skin forms
does not provide a good clinical-laboratory correlation
is useful in diagnosing systemic and atypical manifestations
may not be used in organic fluids other than serum
-
Regarding infectious arthritis caused by Sporothrix spp., it is correct to state that:
it is almost always polyarticular and migratory
it is almost always monoarticular with phlogistic signs
adjacent skin lesions are not observed
it is polyarticular, but does not show phlogistic signs
-
Check the true statement regarding the laboratory diagnosis of sporotrichosis:
the direct microscopy is more sensitive and specific than the culture in humans
the gold standard is the isolation and identification of Sporothrix spp.
the histopathological exam, impregnated by silver, generally exhibits abundance of fungal structures
the molecular identification of the Sporothrix species has no diagnostic value.
-
Feline zoonotic sporotrichosis, predominant in the South and Southeast regions of Brazil, is mostly associated with the following Sporothrix species:
S. schenckii
S. lurei
S. brasiliensis
S. globosa
-
Examples of immunoreactive sporotrichosis clinical forms include:
erythema multiforme and meningitis
Sweet’s syndrome and erythema nodosum
infectious arthritis and erythema multiforme
Sweet’s syndrome and infectious arthritis
-
The choice treatment for localized cutaneous forms of sporotrichosis in immunocompetent people is:
terbinafine
fluconazole
griseofulvin
itraconazole
-
Recent advances in Sporothrix taxonomy have led to the identification of new clinical interest agents. The clinical clade includes the following species:
S. chilensis, S. pallida, S. mexicana, and S. globosa
S. brasiliensis, S. schenckii, S. chilensis, and S. pallida
S. brasiliensis, S. schenckii, S. globosa, and S. luriei
S. schenckii, S. globosa, S. mexicana, and S. luriei
-
Check the correct alternative regarding potassium iodide used in sporotrichosis treatment:
it is recommended for systemic forms with lung involvement
its mechanism of action is well established, inhibiting ergosterol synthesis
it is useful in treating immunoreactive forms due to its immunomodulatory effect
it is used in systemic forms with meningeal involvement
-
Check the alternative that includes the laboratory exams to be requested prior to starting treatment with itraconazole and as a therapeutic control:
biochemistry, blood count, and liver function tests
liver function tests, blood count, and TSH
blood count, liver function tests, and free T4
biochemistry, liver function tests, and TSH
-
If required, the drug that may be administered to pregnant women affected by sporotrichosis is:
fluconazole
itraconazole
amphotericin B
posaconazole
-
Among the actions below, check the one that is not recommended as a preventive measure against the propagation of zoonotic transmission sporotrichosis cases:
street animals neutering
removal of Sporothrix from soil and vegetation
treatment of sick animals
incineration of dead infected animals
-
Among the statements below, check the one in which the correlation between the etiological agent and the geographic distribution is appropriate:
S. brasiliensis in Mexico
S. globosa in Chile
S. pallida in the USA
S. globosa in China
-
The biochemical compound present in S. brasiliensis that may be related to its virulence is:
quinine
adrenalin
melanin
erythropoietin
-
The disease most commonly present in the differential diagnosis of lymphocutaneous sporotrichosis is:
tegumentary leishmaniasis
granuloma annulare
paracoccidioidomycosis
epidermoid carcinoma
-
The important biomarker present in the Sporothrix cell wall that can be used for the production of a therapeutic vaccine is the glycoprotein:
gp40
gp80
gp70
gp100
|
Answer key Behçet's Disease: a review with emphasis on dermatological aspects. An Bras Dermatol. 2017;92(4):452-64 | |||
| 1. A | 6. C | 11. D | 16. B |
| 2. C | 7. B | 12. C | 17. D |
| 3. D | 8. B | 13. C | 18. C |
| 4. D | 9. C | 14. A | 19. A |
| 5. C | 10. B | 15. C | 20. C |
| Papers Information for all members: The EMC-D questionnaire is now available at the homepage of the Brazilian Annals of Dermatology: www.anaisdedermatologia.org.br. The deadline for completing the questionnaire is 30 days from the date of online publication. |
Footnotes
Conflict of interests: None
Work performed at the Dermatology Department, Faculdade de Ciências Médicas, Universidade do Estado do Rio de Janeiro (FCM-UERJ), Rio de Janeiro, RJ, Brazil.
Financial support: None
REFERENCES
- 1.Conti Diaz IA. Epidemiology of sporotrichosis in Latin America. Mycopathologia. 1989;108:113–116. doi: 10.1007/BF00436061. [DOI] [PubMed] [Google Scholar]
- 2.Schenck BR. On refractory subcutaneous abscess caused by a fungus possibly related to the Sporotricha. Bull Johns Hopkins Hosp. 1898;93:286–290. [Google Scholar]
- 3.Kwon-Chung KJ, Bennett JE. Sporotrichosis. In: Kwon-Chung KJ, Bennett JE, editors. Medical Mycology. Philadelphia: Lea & Febiger; 1992. pp. 707–729. [Google Scholar]
- 4.Carmichael JW. Chrysosporium and some other aleuriosporic hyphomycetes. Can J Bot. 1962;40:1137–1173. [Google Scholar]
- 5.Rodrigues AM, Kubitschek-Barreira PH, Fernandes GF, de Almeida SR, Lopes-Bezerra LM, de Camargo ZP. Immunoproteomic analysis reveals a convergent humoral response signature in the Sporothrix schenckii complex. J Proteomics. 2015 Feb 06;115:8–22. doi: 10.1016/j.jprot.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 6.Lutz A, Splendore A. Sobre uma micose observada em homens e ratos. Rev Med S. Paulo. 1907;21:433–450. [Google Scholar]
- 7.Rippon JW. Sporotrichosis. In: Rippon JW, editor. Medical Mycology: the pathogenic fungi and the pathogenic actinomycetes. Philadelphia: WB Saunders; 1988. pp. 325–352. [Google Scholar]
- 8.Morris-Jones R. Sporotrichosis. Clin Exp Dermatol. 2002;27:427–431. doi: 10.1046/j.1365-2230.2002.01087.x. [DOI] [PubMed] [Google Scholar]
- 9.CDC Epidemiologic notes and reports multistate outbreak of sporotrichosis in seedling handlers. MMWR. 1988;37:652–653. [PubMed] [Google Scholar]
- 10.Dooley DP, Bostic PS, Beckius ML. Spook house sporotrichosis: A point-source outbreak of sporotrichosis associated with hay bale props in a Halloween haunted-house. Arch Intern Med. 1997;157:1885–1887. doi: 10.1001/archinte.157.16.1885. [DOI] [PubMed] [Google Scholar]
- 11.Helm MAF, Berman C. The clinical, therapeutic and epidemiological features of the sporotrichosis infection on the mines; Proceedings of the Transvaal Mine Medical Officers' Association. Sporotrichosis Infection on Mines of the Witwatersrand; Johannesburg: The Transvaal Chamber of Mines; 1947. pp. 59–74. [Google Scholar]
- 12.Song Y, Li SS, Zhong SX, Liu YY, Yao L, Huo SS. Report of 457 sporotrichosis cases from Jilin province northeast China, a serious endemic region. J Eur Acad Dermatol Venereol. 2013;27:313–318. doi: 10.1111/j.1468-3083.2011.04389.x. [DOI] [PubMed] [Google Scholar]
- 13.Saravanakumar PS, Eslami P, Zar FA. Lymphocutaneous sporotrichosis associated with a squirrel bite: case report and review. Clin Infect Dis. 1996;23:647–648. doi: 10.1093/clinids/23.3.647. [DOI] [PubMed] [Google Scholar]
- 14.Lacaz CS, Porto E, Martins JEC, Heins-Vaccari EM, Melo NT. Esporotricose e outras micoses gomosas. In: Lacaz CS, Porto E, Martins JEC, Heins-Vaccari EM, Melo NT, editors. Tratado de micologia médica. São Paulo: Sarvier; 2002. pp. 479–497. [Google Scholar]
- 15.Conti-Diaz IA. Sporotrichosis in Uruguay: epidemiologic and clinical aspects. Washington DC: Pan American Health Organization Scientific Publication; 1980. pp. 312–321. [Google Scholar]
- 16.Alves SH, Boettcher CS, Oliveira DC, Tronco-Alves GR, Sgaria MA, Thadeu P, et al. Sporothrix schenckii associated with armadillo hunting in Southern Brazil: epidemiological and antifungal susceptibility profiles. Rev Soc Bras Med Trop. 2010;43:523–525. doi: 10.1590/s0037-86822010000500010. [DOI] [PubMed] [Google Scholar]
- 17.Read SI, Sperling LC. Feline sporotrichosis. Transmission to man. Arch Dermatol. 1982;118:429–431. [PubMed] [Google Scholar]
- 18.Marques SA, Franco SRVS, Camargo RMP, Dias LDF, Haddad-Júnior V, Fabris VE. Esporotricose do gato doméstico (Felis catus): transmissão humana. Rev Inst Med Trop São Paulo. 1993;35:327–330. [PubMed] [Google Scholar]
- 19.Madrid IM, Mattei A, Martins A, Nobre M, Meireles M. Feline sporotrichosis in the southern region of Rio Grande do Sul, Brazil: clinical, zoonotic and therapeutic aspects. Zoonoses Public Health. 2010;57:151–154. doi: 10.1111/j.1863-2378.2008.01227.x. [DOI] [PubMed] [Google Scholar]
- 20.de Lima Barros MB, Schubach TM, Galhardo MC, de Oliveira Schubach A, Monteiro PC, Reis RS, et al. Sporotrichosis: an emergent zoonosis in Rio de Janeiro. Mem Inst Oswaldo Cruz. 2001;96:777–779. doi: 10.1590/s0074-02762001000600006. [DOI] [PubMed] [Google Scholar]
- 21.Barros MB, Schubach A de O, do Valle AC, Gutierrez Galhardo MC, Conceição-Silva F, Schubach TM, et al. Cat-transmited sporotrichosis epidemic in Rio de Janeiro, Brazil: description of a series of cases. Clin Infect Dis. 2004;38:529–535. doi: 10.1086/381200. [DOI] [PubMed] [Google Scholar]
- 22.Barros MB, Schubach AO, Schubach TM, Wanke B, Lambert-Passos SR. An epidemic of sporotrichosis in Rio de Janeiro, Brazil: epidemiological aspects of a series of cases. Epidemiol Infect. 2008;136:1192–1196. doi: 10.1017/S0950268807009727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Freitas DF, Valle AC, da Silva MB, Campos DP, Lyra MR, de Souza RV, et al. Sporotrichosis: an emerging neglected opportunistic infection in HIV-infected patients in Rio de Janeiro, Brazil. PLoS Negl Trop Dis. 2014;8:e3110. doi: 10.1371/journal.pntd.0003110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gutierrez-Galhardo MC, Freitas DFS, do Valle ACF, Almeida-Paes R, Oliveira MME, Zancope-Oliveira RM, et al. Epidemiological aspects of sporotrichosis epidemic in Brazil. Curr Fungal Infect Rep. 2015;9:238–245. [Google Scholar]
- 25.Chakrabarti A, Bonifaz A, Gutierrez-Galhardo MC, Mochizuki T, Li S. Global epidemiology of sporotrichosis. Med Mycol. 2015;53:3–14. doi: 10.1093/mmy/myu062. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Y, Hagen F, Stielow B, Rodrigues AM, Samerpitak K, Zhou X, et al. Phylogeography and evolutionary patterns in Sporothrix spanning more than 14,000 human and animal case reports. Persoonia. 2015;35:1–20. doi: 10.3767/003158515X687416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moussa TAA, Kadasa NMS, Al Zahrani HS, Ahmed SA, Feng P, Gerrits van den Ende AHG, et al. Origin and distribution of Sporothrix globosa causing sapronoses in Asia. J Med Microbiol. 2017;66:560–569. doi: 10.1099/jmm.0.000451. [DOI] [PubMed] [Google Scholar]
- 28.Rodrigues AM, de Melo Teixeira M, de Hoog GS, Schubach TM, Pereira SA, Fernandes GF, et al. Phylogenetic analysis reveals a high prevalence of Sporothrix brasiliensis in feline sporotrichosis outbreaks. PLoS Negl Trop Dis. 2013;7:e2281. doi: 10.1371/journal.pntd.0002281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rodrigues AM, de Hoog G, Zhang Y, de Camargo ZP. Emerging sporotrichosis is driven by clonal and recombinant Sporothrix species. Emerg Microbes Infect. 2014;3:e32. doi: 10.1038/emi.2014.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marimon R, Gené J, Cano J, Trilles L, Dos Santos Lazéra M, Guarro J. Molecular phylogeny of Sporothrix schenkii. J Clin Microbiol. 2006;44:3251–3256. doi: 10.1128/JCM.00081-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou X, Rodrigues AM, Feng P, Hoog GS. Global ITS diversity in the Sporothrix schenckii complex. Fungal Divers. 2014;66:153–165. [Google Scholar]
- 32.de Beer ZW, Duong TA, Wingfield MJ. The divorce of Sporothrix and Ophiostoma: solution to a problematic relationship. Stud Mycol. 2016;83:165–191. doi: 10.1016/j.simyco.2016.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marimon R, Cano J, Gené J, Sutton DA, Kawasaki M, Guarro J. Sporothrix brasiliensis, S. globosa, and S. mexicana, three new Sporothrix species of clinical interest. J Clin Microbiol. 2007;45:3198–3206. doi: 10.1128/JCM.00808-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rodrigues AM, Bagagli E, de Camargo ZP, Bosco S de M. Sporothrix schenckii sensu stricto isolated from soil in an armadillo's burrow. Mycopathologia. 2014;177:199–206. doi: 10.1007/s11046-014-9734-8. [DOI] [PubMed] [Google Scholar]
- 35.Montenegro H, Rodrigues AM, Dias MA, da Silva EA, Bernardi F, de Camargo ZP. Feline sporotrichosis due to Sporothrix brasiliensis: an emerging animal infection in São Paulo, Brazil. BMC Vet Res. 2014;10:269–269. doi: 10.1186/s12917-014-0269-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ajello L, Kaplan W. A new variant of Sporothrix Schenckii. Mykosen. 1969;12:633–644. doi: 10.1111/j.1439-0507.1969.tb03423.x. [DOI] [PubMed] [Google Scholar]
- 37.Marimon R, Gené J, Cano J, Guarro J. Sporothrix luriei: a rare fungus from clinical origin. Med Mycol. 2008;46:621–625. doi: 10.1080/13693780801992837. [DOI] [PubMed] [Google Scholar]
- 38.Rodrigues AM, Cruz Choappa R, Fernandes GF, de Hoog GS, de Camargo ZP. Sporothrix chilensis sp. nov. (Ascomycota: Ophiostomatales), a soil-borne agent of human sporotrichosis with mild-pathogenic potential to mammals. Fungal Biol. 2016;120(2):246–264. doi: 10.1016/j.funbio.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 39.Rodrigues AM, de Hoog S, de Camargo ZP. Emergence of pathogenicity in the Sporothrix schenckii complex. Med Mycol. 2013;51:405–412. doi: 10.3109/13693786.2012.719648. [DOI] [PubMed] [Google Scholar]
- 40.Morrison AS, Lockhart SR, Bromley JG, Kim JY, Burd EM. An environmental Sporothrix as a cause of corneal ulcer. Med Mycol Case Rep. 2013;2:88–90. doi: 10.1016/j.mmcr.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mariat F, Escudié A, Gaxotte P. Isolation of Ceratocystis strains sp. conidial forms Sporotrichum, from human scalp and from tails of rats. Comparison with the pathogenic species Sporotrichum schenckii. C R Acad Sci Hebd Seances Acad Sci D. 1968;267:974–976. [PubMed] [Google Scholar]
- 42.Arrillaga-Moncrieff I, Capilla J, Mayayo E, Marimon R, Mariné M, Gené J, et al. Different virulence levels of the species of Sporothrix in a murine model. Clin Microbiol Infect. 2009;15:651–655. doi: 10.1111/j.1469-0691.2009.02824.x. [DOI] [PubMed] [Google Scholar]
- 43.Howard DH. Dimorphism of Sporotrichum schenckii. J Bacteriol. 1961;81:464–469. doi: 10.1128/jb.81.3.464-469.1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rodrigues AM, de Hoog GS, de Camargo ZP. Sporothrix species causing outbreaks in animals and humans driven by animal-animal transmission. PLoS Pathog. 2016;12:e1005638. doi: 10.1371/journal.ppat.1005638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mario DA, Santos RC, Denardi LB, Vaucher R de A, Santurio JM, Alves SH. Interference of melanin in the susceptibility profile of Sporothrix species to amphotericin B. Rev Iberoam Micol. 2016;33:21–25. doi: 10.1016/j.riam.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 46.Almeida-Paes R, Figueiredo-Carvalho MH, Brito-Santos F, Almeida-Silva F, Oliveira MM, Zancopé-Oliveira RM. Melanins protect Sporothrix brasiliensis and Sporothrix schenckii from the antifungal effects of terbinafine. PLoS One. 2016;11:e0152796. doi: 10.1371/journal.pone.0152796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Castro RA, Kubitschek-Barreira PH, Teixeira PA, Sanches GF, Teixeira MM, Quintella LP, et al. Differences in cell morphometry, cell wall topography and Gp70 expression correlate with the virulence of Sporothrix brasiliensis clinical isolates. PLoS One. 2013;8:e75656. doi: 10.1371/journal.pone.0075656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fernandes GF, dos Santos PO, Rodrigues AM, Sasaki AA, Burger E, de Camargo ZP. Characterization of virulence profile, protein secretion and immunogenicity of different Sporothrix schenckii sensu stricto isolates compared with S. globosa and S. brasiliensis species. Virulence. 2013;4:241–249. doi: 10.4161/viru.23112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Almeida-Paes R, de Oliveira LC, Oliveira MM, Gutierrez-Galhardo MC, Nosanchuk JD, Zancopé-Oliveira RM. Phenotypic characteristics associated with virulence of clinical isolates from the Sporothrix complex. Biomed Res Int. 2015;2015:212308. doi: 10.1155/2015/212308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alba-Fierro CA, Pérez-Torres A, Toriello C, Romo-Lozano Y, López-Romero E, Ruiz-Baca E. Molecular components of the Sporothrix schenckii complex that induce immune response. Curr Microbiol. 2016;73:292–300. doi: 10.1007/s00284-016-1045-5. [DOI] [PubMed] [Google Scholar]
- 51.Freitas DF, De Siqueira Hoagland B, do Valle AC, Fraga BB, de Barros MB, de Oliveira Schubach A, et al. Sporotrichosis in HIV-infected patients: report of 21 cases of endemic sporotrichosis in Rio de Janeiro, Brazil. Med Mycol. 2012;50(2):170–178. doi: 10.3109/13693786.2011.596288. [DOI] [PubMed] [Google Scholar]
- 52.Lopes-Bezerra LM, Schubach A, Costa RO. Sporothrix schenckii and sporotrichosis. An Acad Bras Cienc. 2006;78:293–308. doi: 10.1590/s0001-37652006000200009. [DOI] [PubMed] [Google Scholar]
- 53.Kurosawa A, Pollock SC, Collins MP, Kraff CR, Tso MO. Sporothrix schenckii endophthalmitis in a patient with human immunodeficiency virus infection. Arch Ophthalmol. 1988;106:376–380. doi: 10.1001/archopht.1988.01060130402030. [DOI] [PubMed] [Google Scholar]
- 54.Sena CM, Dias D, Oréfice F, Tanuri MA. Uveíte anterior granulomatosa causada por Sporothrix schenckii. Rev Bras Oftalmol. 1995;54:27–30. [Google Scholar]
- 55.Curi AL, Félix S, Azevedo KM, Estrela R, Villar EG, Saraça G. Retinal granuloma caused by Sporothrix schenckii. Am J Ophthalmol. 2003;136:205–207. doi: 10.1016/s0002-9394(03)00083-7. [DOI] [PubMed] [Google Scholar]
- 56.Freitas DF, Lima IA, Curi CL, Jordão L, Zancopé-Oliveira RM, Valle AC, Galhardo MC, et al. Acute dacryocystitis: another clinical manifestation of sporotrichosis. Mem Inst Oswaldo Cruz. 2014;109:262–264. doi: 10.1590/0074-0276130304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.de Macedo PM, Sztajnbok DC, Camargo ZP, Rodrigues AM, Lopes-Bezerra LM, Bernardes-Engemann AR, et al. Dacryocystitis due to Sporothrix brasiliensis: a case report of a successful clinical and serological outcome with low-dose potassium iodide treatment and oculoplastic surgery. Br J Dermatol. 2015;172:1116–1119. doi: 10.1111/bjd.13378. [DOI] [PubMed] [Google Scholar]
- 58.Ferreira CP, Nery JA, de Almeida AC, Ferreira LC, Corte-Real S, Conceição-Silva F. Parinaud's oculoglandular syndrome associated with Sporothrix schenckii. IDCases. 2014;1:38–39. doi: 10.1016/j.idcr.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Costa RO, de Mesquita KC, Damasco PS, Bernardes-Engemann AR, Dias CM, Silva IC, et al. Infectious arthritis as the single manifestation of sporotrichosis: serology from serum and synovial fluid samples as an aid to diagnosis. Rev Iberoam Micol. 2008;25:54–56. doi: 10.1016/s1130-1406(08)70014-7. [DOI] [PubMed] [Google Scholar]
- 60.Ribeiro BN, Ribeiro RN, Penna CR, Frota AC. Bone involvement by Sporothrix schenckii in an immunocompetent child. Pediatr Radiol. 2015;45:1427–1430. doi: 10.1007/s00247-015-3299-7. [DOI] [PubMed] [Google Scholar]
- 61.England DM, Hochholzer L. Sporothrix infection of the lung without cutaneous disease. Primary pulmonary sporotrichosis. Arch Pathol Lab Med. 1987;111:298–300. [PubMed] [Google Scholar]
- 62.Padhye AA, Kaufman L, Durry E, Banerjee CK, Jindal SK, Talwar P, et al. Fatal pulmonary sporotrichosis caused by Sporothrix schenckii var. luriei in India. J Clin Microbiol. 1992;30:2492–2494. [Google Scholar]
- 63.Singhai M, Rawat V, Verma P, Jha PK, Shree D, Goyal R, et al. Primary pulmonary sporotrichosis in a sub-Himalayan patient. J Lab Physicians. 2012;4:48–49. doi: 10.4103/0974-2727.98674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Orofino-Costa R, Unterstell N, Carlos Gripp A, de Macedo PM, Brota A, Dias E, et al. Pulmonary cavitation and skin lesions mimicking tuberculosis in a HIV negative patient caused by Sporothrix brasiliensis. Med Mycol Case Rep. 2013;2:65–71. doi: 10.1016/j.mmcr.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Aung AK, Spelman DW, Thompson PJ. Pulmonary Sporotrichosis: An Evolving Clinical Paradigm. Semin Respir Crit Care Med. 2015;36:756–766. doi: 10.1055/s-0035-1562901. [DOI] [PubMed] [Google Scholar]
- 66.Vilela R, Souza GF, Fernandes Cota G, Mendoza L. Cutaneous and meningeal sporotrichosis in a HIV patient. Rev Iberoam Micol. 2007;24:161–163. doi: 10.1016/s1130-1406(07)70035-9. [DOI] [PubMed] [Google Scholar]
- 67.Orofino-Costa R, Bóia MN, Magalhães GA, Damasco PS, Bernardes-Engemann AR, Benvenuto F, et al. Arthritis as a hypersensitivity reaction in a case of sporotrichosis transmitted by a sick cat: clinical and serological follow up of 13 months. Mycoses. 2010;53:81–83. doi: 10.1111/j.1439-0507.2008.01661.x. [DOI] [PubMed] [Google Scholar]
- 68.Freitas DF, Valle AC, Cuzzi T, Brandão LG, Zancope-Oliveira RM, Galhardo MC. Sweet syndrome associated with sporotrichosis. Br J Dermatol. 2012;166:212–213. doi: 10.1111/j.1365-2133.2011.10496.x. [DOI] [PubMed] [Google Scholar]
- 69.Zhang Y, Pyla V. Sweet's syndrome-like sporotrichosis. Int J Dermatol. 2014;53:e324–e325. doi: 10.1111/ijd.12424. [DOI] [PubMed] [Google Scholar]
- 70.Orofino-Costa R, de Macedo PM, Bernardes-Engemann AR. Hyperendemia of Sporotrichosis in the Brazilian Southeast: Learning From Clinics and Therapeutics. Curr Fungal Infect Rep. 2015;9:220–228. [Google Scholar]
- 71.Bernardes-Engemann AR, de Lima Barros M, Zeitune T, Russi DC, Orofino-Costa R, Lopes-Bezerra LM. Validation of a serodiagnostic test for sporotrichosis: a follow-up study of patients related to the Rio de Janeiro zoonotic outbreak. Med Mycol. 2015;53:28–33. doi: 10.1093/mmy/myu058. [DOI] [PubMed] [Google Scholar]
- 72.Kauffman CA, Bustamante B, Chapman SW, Pappas PG, Infectious Diseases Society of America Clinical practice guidelines for the management of sporotrichosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45:1255–1265. doi: 10.1086/522765. [DOI] [PubMed] [Google Scholar]
- 73.Hessler C, Kauffman CA, Chow FC. The Upside of Bias: A Case of Chronic Meningitis Due to Sporothrix schenckii in an Immunocompetent Host. Neurohospitalist. 2017;7:30–34. doi: 10.1177/1941874416641468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.de Hoog GS, Guarro J. Atlas of Clinical Fungi. Baarn: Centralbureau voor Schimmelcultures; 1995. [Google Scholar]
- 75.Mahajan VK. Sporotrichosis: an overview and therapeutic options. Dermatol Res Pract. 2014;2014:272376. doi: 10.1155/2014/272376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Oyarce JA, García C, Alave J, Bustamante B. Epidemiological clinical and laboratory characterization of sporotrichosis in patients of a tertiary care hospital in Lima, Peru, from 1991 to 2014. Rev Chilena Infectol. 2016;33:315–321. doi: 10.4067/S0716-10182016000300012. [DOI] [PubMed] [Google Scholar]
- 77.Jessica N, Sonia RL, Rodrigo C, Isabella DF, Tânia MP, Jeferson C, et al. Diagnostic accuracy assessment of cytopathological examination of feline sporotrichosis. Med Mycol. 2015;53:880–884. doi: 10.1093/mmy/myv038. [DOI] [PubMed] [Google Scholar]
- 78.Pappas PG, Tellez I, Deep AE, Nolasco D, Holgado W, Bustamante B. Sporotrichosis in Peru: description of an area of hyperendemicity. Clin Infect Dis. 2000;30:65–70. doi: 10.1086/313607. [DOI] [PubMed] [Google Scholar]
- 79.Zhao MD, Zhou X, Liu TT, Yang ZB. Morphological and physiological comparison of taxa comprising the Sporothrix schenckii complex. J Zhejiang Univ Sci B. 2015;16:940–947. doi: 10.1631/jzus.B1500055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Agarwal S Gopal K, Umesh Kumar B. Sporotrichosis in Uttarakhand (India): a report of nine cases. Int J Dermatol. 2008;47:367–371. doi: 10.1111/j.1365-4632.2008.03538.x. [DOI] [PubMed] [Google Scholar]
- 81.Quintella LP, Passos SR, do Vale AC, Galhardo MC, Barros MB, Cuzzi T, et al. Histopathology of cutaneous sporotrichosis in Rio de Janeiro: a series of 119 consecutive cases. J Cutan Pathol. 2011;38:25–32. doi: 10.1111/j.1600-0560.2010.01626.x. [DOI] [PubMed] [Google Scholar]
- 82.Zhang YQ, Xu XG, Zhang M, Jiang P, Zhou XY, Li ZZ, Zhang MF, et al. Sporotrichosis: clinical and histopathological manifestations. Am J Dermatopathol. 2011;33:296–302. doi: 10.1097/DAD.0b013e3181f5b622. [DOI] [PubMed] [Google Scholar]
- 83.Casserone S, Conti-Díaz IA, Zanetta E, Peña de Pereira ME. Serology of cutaneous sporotrichosis. Sabouraudia. 1983;21:317–321. [PubMed] [Google Scholar]
- 84.de Albornoz MB, Villanueva E, de Torres ED. of immunoprecipitation techniques to the diagnosis of cutaneous and extracutaneousforms of sporotrichosis. Mycopathologia. 1984;85:177–183. doi: 10.1007/BF00440950. [DOI] [PubMed] [Google Scholar]
- 85.Bernardes-Engemann AR, Costa RC, Miguens BR, Penha CV, Neves E, Pereira BA, et al. Development of an enzyme-linked immunosorbent assay for the serodiagnosis of several clinical forms of sporotrichosis. Med Mycol. 2005;43:487–493. doi: 10.1080/13693780400019909. [DOI] [PubMed] [Google Scholar]
- 86.Almeida-Paes R, Pimenta MA, Pizzini CV, Monteiro PC, Peralta JM, Nosanchuk JD, et al. Use of mycelial-phase Sporothrix schenckii exoantigens in an enzyme-linked immunosorbent assay for diagnosis of sporotrichosis by antibody detection. Clin Vaccine Immunol. 2007;14:244–249. doi: 10.1128/CVI.00430-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Almeida-Paes R, Bailão AM, Pizzini CV, Reis RS, Soares CM, Peralta JM, et al. Cell-free antigens of Sporothrix brasiliensis: antigenic diversity and application in an immunoblot assay. Mycoses. 2012;55:467–475. doi: 10.1111/j.1439-0507.2012.02175.x. [DOI] [PubMed] [Google Scholar]
- 88.Penha CV, Bezerra LM. Concanavalin A-binding cell wall antigens of Sporothrix schenckii: a serological study. Med Mycol. 2000;38:1–7. [PubMed] [Google Scholar]
- 89.Fernandes GF, Lopes-Bezerra LM, Bernardes-Engemann AR, Schubach TM, Dias MA, Pereira SA, et al. Serodiagnosis of sporotrichosis infection in cats by enzyme-linked immunosorbent assay using a specific antigen, SsCBF, and crude exoantigens. Vet Microbiol. 2011;147:445–449. doi: 10.1016/j.vetmic.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Alba-Fierro CA, Pérez-Torres A, Toriello C, Pulido-Camarillo E, López-Romero E, Romo-Lozano Y, et al. Immune response induced by an immunodominant 60 kDa glycoprotein of the cell wall of Sporothrix schenckii in two mice strains with experimental sporotrichosis. J Immunol Res. 2016;2016:6525831. doi: 10.1155/2016/6525831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Nascimento RC, Espíndola NM, Castro RA, Teixeira PA, Loureiro y Penha CV, Lopes-Bezerra LM, et al. Passive immunization with monoclonal antibody against a 70-kDa putative adhesin of Sporothrix schenckii induces protection in murine sporotrichosis. Eur J Immunol. 2008;38:3080–3089. doi: 10.1002/eji.200838513. [DOI] [PubMed] [Google Scholar]
- 92.Teixeira PA, de Castro RA, Nascimento RC, Tronchin G, Torres AP, Lazéra M, et al. Cell surface expression of adhesins for fibronectin correlates with virulence in Sporothrix schenckii. Microbiology. 2009;155:3730–3738. doi: 10.1099/mic.0.029439-0. [DOI] [PubMed] [Google Scholar]
- 93.Alba-Fierro CA, Pérez-Torres A, López-Romero E, Cuéllar-Cruz M, Ruiz-Baca E. Cell wall proteins of Sporothrix schenckii as immunoprotective agents. Rev Iberoam Micol. 2014 Jan-Mar;31(1):86–89. doi: 10.1016/j.riam.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 94.Almeida SR. Therapeutic monoclonal antibody for sporotrichosis. Front Microbiol. 2012;3:409–409. doi: 10.3389/fmicb.2012.00409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Oliveira MM, Almeida-Paes R, Muniz MM, Gutierrez-Galhardo MC, Zancope-Oliveira RM. Phenotypic and molecular identification of Sporothrix isolates from an epidemic area of sporotrichosis in Brazil. Mycopathologia. 2011;172:257–267. doi: 10.1007/s11046-011-9437-3. [DOI] [PubMed] [Google Scholar]
- 96.Ottonelli Stopiglia CD, Magagnin CM, Castrillón MR, Mendes SD, Heidrich D, Valente P, et al. Antifungal susceptibilities and identification of species of the Sporothrix schenckii complex isolated in Brazil. Med Mycol. 2014;52:56–64. doi: 10.3109/13693786.2013.818726. [DOI] [PubMed] [Google Scholar]
- 97.Camacho E, León-Navarro I, Rodríguez-Brito S, Mendoza M, Niño-Vega GA. Molecular epidemiology of human sporotrichosis in Venezuela reveals high frequency of Sporothrix globosa. BMC Infect Dis. 2015 Feb 25;15:94–94. doi: 10.1186/s12879-015-0839-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Madrid H, Cano J, Gené J, Bonifaz A, Toriello C, Guarro J. Sporothrix globosa, a pathogenic fungus with widespread geographical distribution. Rev Iberoam Micol. 2009;26:218–222. doi: 10.1016/j.riam.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 99.Romeo O, Scordino F, Criseo G. New insight into molecular phylogeny and epidemiology of Sporothrix schenckii species complex based on calmodulin-encoding gene analysis of Italian isolates. Mycopathologia. 2011;172:179–186. doi: 10.1007/s11046-011-9420-z. [DOI] [PubMed] [Google Scholar]
- 100.Yu X, Wan Z, Zhang Z, Li F, Li R, Liu X. Phenotypic and molecular identification of Sporothrix isolates of clinical origin in Northeast China. Mycopathologia. 2013;176:67–74. doi: 10.1007/s11046-013-9668-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kano R, Okubo M, Siew HH, Kamata H, Hasegawa A. Molecular typing of Sporothrix schenckii isolates from cats in Malaysia. Mycoses. 2015;58:220–224. doi: 10.1111/myc.12302. [DOI] [PubMed] [Google Scholar]
- 102.Rodrigues AM, de Hoog GS, de Camargo ZP. Genotyping species of the Sporothrix schenckii complex by PCR-RFLP of calmodulin. Diagn Microbiol Infect Dis. 2014;78:383–387. doi: 10.1016/j.diagmicrobio.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 103.Rodrigues AM, de Hoog GS, de Camargo ZP. Molecular diagnosis of pathogenic Sporothrix species. PLoS Negl Trop Dis. 2015;9:e0004190. doi: 10.1371/journal.pntd.0004190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rodrigues AM, Najafzadeh MJ, de Hoog GS, de Camargo ZP. Rapid identification of emerging human-pathogenic Sporothrix species with rolling circle amplification. Front Microbiol. 2015 Dec 08;6:1385–1385. doi: 10.3389/fmicb.2015.01385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Fire A, Xu SQ. Rolling replication of short DNA circles. Proc Natl Acad Sci U S A. 1995;92:4641–4645. doi: 10.1073/pnas.92.10.4641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.de Lima Barros MB, Schubach AO, de Vasconcellos Carvalhaes de Oliveira R, Martins EB, Teixeira JL, Wanke B. Treatment of cutaneous sporotrichosis with itraconazol-study of 645 patients. Clin Infect Dis. 2011;52:e200–e206. doi: 10.1093/cid/cir245. [DOI] [PubMed] [Google Scholar]
- 107.Song Y, Zhong SX, Yao L, Cai Q, Zhou JF, Liu YY, et al. Efficacy and safety of itraconazole pulses vs. continuous regimen in cutaneous sporotrichosis. J Eur Acad Dermatol Venereol. 2011;25:302–305. doi: 10.1111/j.1468-3083.2010.03785.x. [DOI] [PubMed] [Google Scholar]
- 108.Paul V, Rawal H. Cardiotoxicity with Itraconazole. BMJ Case Rep. 2017 Apr 10;2017 doi: 10.1136/bcr-2017-219376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sterling JB, Heymann WR. Potassium iodide in dermatology: a 19th century drug for the 21st century-uses, pharmacology, adverse effects, and contraindications. J Am Acad Dermatol. 2000;43:691–697. doi: 10.1067/mjd.2000.107247. [DOI] [PubMed] [Google Scholar]
- 110.Xue SL, Li L. Oral potassium iodide for the treatment of sporotrichosis. Mycopathologia. 2009;167:355–356. doi: 10.1007/s11046-008-9178-0. [DOI] [PubMed] [Google Scholar]
- 111.Costa RO, Macedo PM, Carvalhal A, Bernardes-Engemann AR. Use of potassium iodide in dermatology: updates on an old drug. An Bras Dermatol. 2013 May-Jun;88:396–402. doi: 10.1590/abd1806-4841.20132377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Macedo PM, Lopes-Bezerra LM, Bernardes-Engemann AR, Orofino-Costa R. New posology of potassium iodide for the treatment of cutaneous soporotrichosis: study of efficacy and safety in 102 patients. J Eur Acad Dermatol Venereol. 2015;29:719–724. doi: 10.1111/jdv.12667. [DOI] [PubMed] [Google Scholar]
- 113.Antunes Tde A, Nobre M de O, Faria RO, Meinerz AR, Martins AA, Cleff MB, et al. Experimental cutaneous sporotrichosis: In vivo evaluation of itraconazol and terbinafine. Rev Soc Bras Med Trop. 2009;42:706–710. doi: 10.1590/s0037-86822009000600018. [DOI] [PubMed] [Google Scholar]
- 114.Francesconi G, Valle AC, Passos S, Reis R, Galhardo MC. Terbinafine (250 mg/d): An effective and safe treatment of cutaneous sporotrichosis. J Eur Acad Dermatol Venereol. 2009;23:1273–1276. doi: 10.1111/j.1468-3083.2009.03306.x. [DOI] [PubMed] [Google Scholar]
- 115.Costa RO, Bernardes-Engemann AR, Azulay-Abulafia L, Benvenuto F, Neves Mde L, Lopes-Bezerra LM. Sporotrichosis in pregnancy: case reports of 5 patients in a zoonotic epidemic in Rio de Janeiro, Brasil. An Bras Dermatol. 2011;86:995–998. doi: 10.1590/s0365-05962011000500020. [DOI] [PubMed] [Google Scholar]
- 116.Bonifaz A, Vásquez-Gonzáles D. Diagnosis and treatment of cutaneous sporotrichosis: what are the options? Curr Fungal Infect Rep. 2013;7:252–259. [Google Scholar]
- 117.Gilaberte Y, Aspiroz C, Alejandre MC, Andres-Ciriano E, Fortuño B, Charlez L, et al. Cutaneous sporotrichosis treated with photodynamic therapy: An in vivo and in vitro study. Photomed Laser Surg. 2014;32:54–57. doi: 10.1089/pho.2013.3590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Oliveira DC, Lopes PG, Spader TB, Mahl CD, Tronco-Alves GR, Lara VM, et al. Antifungal susceptibilities of Sporothrix albicans, S. brasiliensis and S. luriei of the S. schenckii complex identified in Brazil. J Clin Microbiol. 2011;49:3047–3049. doi: 10.1128/JCM.00255-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Borba-Santos LP, Rodrigues AM, Gagini TB, Fernandes GF, Castro R, de Camargo ZP, et al. Susceptibility of Sporothrix brasiliensis isolates to amphotericin B, azoles, and terbinafine. Med Mycol. 2015;53:178–188. doi: 10.1093/mmy/myu056. [DOI] [PubMed] [Google Scholar]
- 120.Reis EG, Gremião ID, Kitada AA, Rocha RF, Castro VS, Barros MB, et al. Potassium iodide capsule treatment of feline sporotrichosis. J Feline Med Surg. 2012;14:399–404. doi: 10.1177/1098612X12441317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Gupta M, Narang T, Kaur RJ, Manhas A, Saikia UN, Dogra S. A prospective case series evaluating efficacy and safety of combination of itraconazole and potassium iodide in rhinofacial conidiobolomycosis. Int J Dermatol. 2016;55:208–214. doi: 10.1111/ijd.12966. [DOI] [PubMed] [Google Scholar]
- 122.Marimon R, Serena C, Gené J, Cano J, Guarro J. In vitro antifungal susceptibilities of five species of Sporothrix. Antimicrob Agents Chemother. 2008;52:732–734. doi: 10.1128/AAC.01012-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Rodrigues AM, de Hoog GS, de Cássia Pires D, Brihante RS, Sidrim JJ, Gadelha MF, et al. Genetic diversity and antifungal susceptibility profiles in causative agents of sporotrichosis. BMC Infect Dis. 2014;14:219–219. doi: 10.1186/1471-2334-14-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Gremião ID, Miranda LH, Reis EG, Rodrigues AM, Pereira SA. Zoonotic epidemic of sporotrichosis: Cat to human transmission. PLoS Pathog. 2017;13:e1006077. doi: 10.1371/journal.ppat.1006077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Taylor LH, Latham SM, Woolhouse ME. Risk factors for human disease emergence. Philos Trans R Soc Lond B Biol Sci. 2001;356:983–989. doi: 10.1098/rstb.2001.0888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ruiz-Baca E, Toriello C, Perez-Torres A, Sabanero-Lopez M, Villagomez-Castro JC, Lopez-Romero E. Isolation and some properties of a glycoprotein of 70 kDa (Gp70) from the cell wall of Sporothrix schenckii involved in fungal adherence to dermal extracellular matrix. Med Mycol. 2009;47:185–196. doi: 10.1080/13693780802165789. [DOI] [PubMed] [Google Scholar]
- 127.Borba-Santos LP, Gagini T, Ishida K, de Souza W, Rozental S. Miltefosine is active against Sporothrix brasiliensis isolates with in vitro low susceptibility to amphotericin B or itraconazole. J Med Microbiol. 2015;64:415–422. doi: 10.1099/jmm.0.000041. [DOI] [PubMed] [Google Scholar]
- 128.Brilhante RS, Silva NF, Marques FJ, Castelo-Branco Dde S, de Lima RA, Malaquias AD, et al. In vitro inhibitory activity of terpenic derivatives against clinical and environmental strains of the Sporothrix schenkii complex. Med Mycol. 2015;53:93–98. doi: 10.1093/mmy/myu085. [DOI] [PubMed] [Google Scholar]
- 129.Brilhante RS, Malaquias AD, Caetano EP, Castelo-Branco Dde S, Lima RA, Marques FJ, et al. In vitro inhibitory effect of miltefosine against strains of Histoplasma capsulatum var. capsulatum and Sporothrix spp. Med Mycol. 2014;52:320–325. doi: 10.1093/mmy/myt027. [DOI] [PubMed] [Google Scholar]
- 130.Borba-Santos LP, Ishida K, Calogeropoulou T, Wd Souza, Rozental S. Adamantylidene-substituted alkylphosphocholine TCAN26 is more active against Sporothrix schenckii than miltefosine. Mem Inst Oswaldo Cruz. 2016;111:523–527. doi: 10.1590/0074-02760160088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Borba-Santos LP, Visbal G, Gagini T, Rodrigues AM, de Camargo ZP, Lopes-Bezerra LM, et al. ∆24-sterol methyltransferase plays an important role in the growth and development of Sporothrix schenckii and Sporothrix brasiliensis. Front Microbiol. 2016;7:311–311. doi: 10.3389/fmicb.2016.00311. [DOI] [PMC free article] [PubMed] [Google Scholar]