Abstract
Acne is a chronic, immune-mediated, inflammatory disease with high prevalence among adolescents. By compromising face, thorax and back, with the risk of permanent scars, it has a negative impact on the quality of life. Effective, safe and early treatment is the key to remission, while decreasing the risk of physical and/or emotional sequelae. The Iberian-Latin American Group of Acne Studies joined professionals with expertise and developed a practical therapeutic algorithm, adapted to the reality of Latin American countries, Spain and Portugal. This article intends to disseminate it with an updated review on a rational, safe and effective acne treatment.
Keywords: Acne Vulgaris, Algorithms, Guideline
INTRODUCTION
Acne is one of the most common dermatological diseases seen by dermatologists in Latin America, Spain and Portugal, as well as in the rest of the world. It is a chronic inflammatory process that needs to be treated early and effectively to decrease the risk of physical and emotional sequelae. In this article, we present the result of the consensus among a group of dermatologists from Latin America, Spain and Portugal, based on the scientific evidence available in the literature and the experience of the members.
METHODS
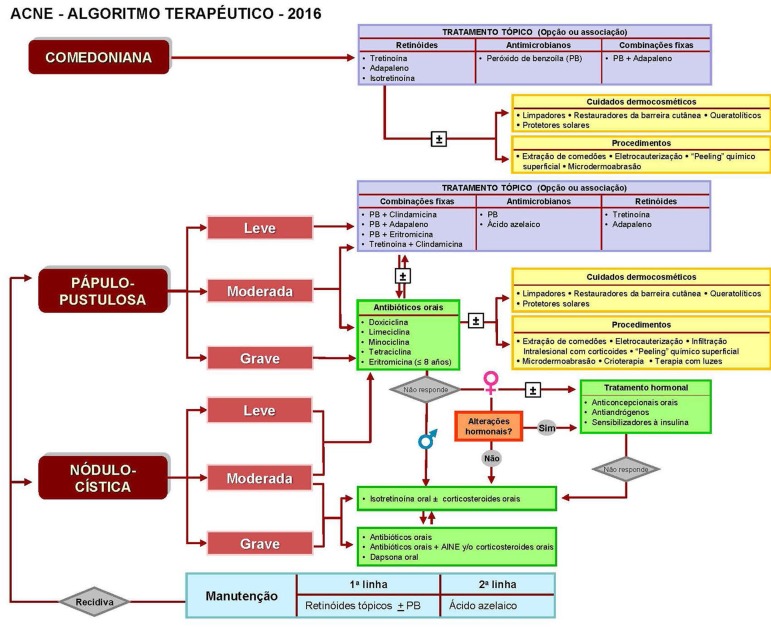
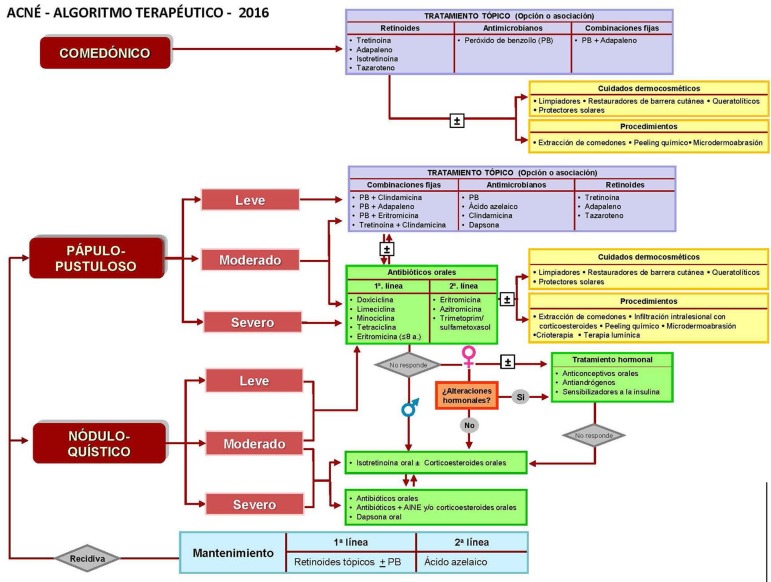
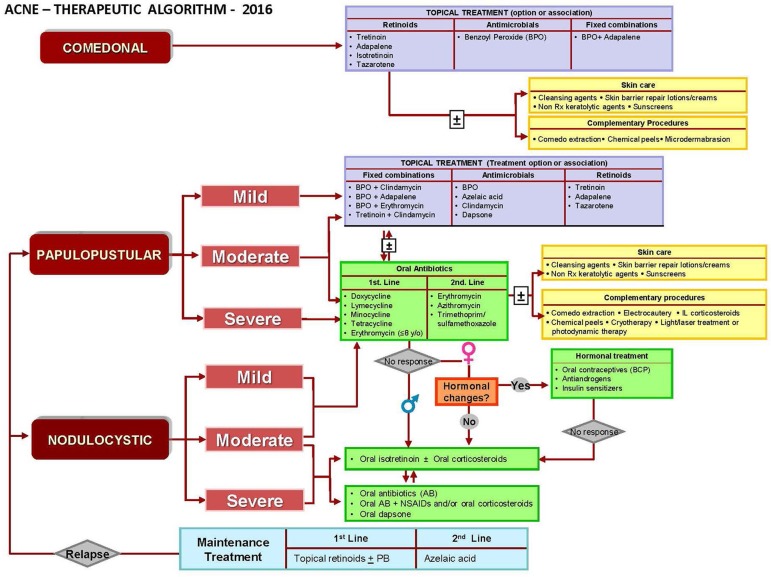
A group of 33 dermatologists, members of the Iberian-Latin American College of Dermatology - CILAD, and well-known acne specialists, created the Iberian-Latin American Group for the Study of Acne - GILEA. All the available scientific evidence was carefully chosen and several questions were developed in different face-to-face meetings to initially determine the classification and gradation of the disease and subsequently the guidelines for the treatment of acne or therapeutic algorithm. Through these meetings and others, conducted in electronic format (e.g. Skype, e-mail) between 2012 and 2016, questions based on scientific evidence and participants' experiences were circulated until a consensus was reached, which resulted in the therapeutic algorithm in Portuguese, Spanish and English adapted to the Iberian-Latin American conditions, that is presented in this paper (Figures 1, 2 and 3).
Figure 1.
Acne - Algoritmo Terapêutico 2016 - Português
Figure 2.
Acné - Algoritmo Terapéutico 2016 - Español
Figure 3.
Acne - Therapeutic Algorithm 2016 - English
TOPICAL TREATMENT
Topical treatment can be indicated as monotherapy or in combination with systemic antibiotics or hormonal treatment, depending on the type of acne. The majority of patients with comedonal acne respond to topical treatment associated or not with dermocosmetics.1
Retinoids
Considered the first-line therapy for comedonal acne, retinoids normalize infundibular keratinization, inhibit comedogenesis, have an anti-inflammatory action and also increase the penetration of other medications. They act by binding to cytoplasmic (CRAB) and nuclear receptors (retinoic acid receptors or RARs and X or RXRs) and regulate the expression of genes related to cell differentiation, lipid metabolism, apoptosis and cell cycle. The anti-inflammatory activity of retinoids is due to the modulation of the Toll-like receptors (TLR), the innate immunity, and the surface of sebocytes that bind to molecular patterns of the microorganisms, in this case, cell wall peptidoglycans of the Propionibacterium acnes (P. acnes), activating signaling pathways, such as NF-κB, with production of proinflammatory cytokines.2 Two groups are available: first generation, tretinoin or all-trans retinoic acid (concentrations of 0.025%, 0.05% and 0.1%) and isotretinoin or 13-cis-retinoic acid (sparingly used) and synthetic retinoids, adapalene and tazarotene, the latter not available in many countries. Tretinoin and adapalene are classified as Class C and Tazarotene as X by the Food and Drug Administration (FDA) - the United States regulatory agency. Recently the FDA removed the prescription need for adapalene 0.1%, based on a meta-analysis that showed no increase in the incidence of congenital malformations, abortion, low birth weight or prematurity in women who used adapalene during pregnancy. For tretinoin, the recommendation not to use during gestation was maintained.3 Irritant contact dermatitis (erythema, pruritus, desquamation), increased risk of photosensitivity and postinflammatory pigmentation are attenuated by the use of moisturizers and photoprotectors. They may be used alone or in combination with benzoyl peroxide (PB) and topical antibiotics.1,4
Benzoyl peroxide
PB is an antimicrobial agent with activity against P. acnes by the release of reactive oxygen species (ROS), and mild comedolytic effect. There is no description of PB-resistant strains; moreover, its use in combination with topical or systemic antibiotics prevents and treats bacterial resistance. Available concentrations, ranging from 2.5% to 10%, appear to have the same effectiveness; however, irritant contact dermatitis is more frequent with higher concentrations.1
Topical antibiotics
Topical antibiotics accumulate in the follicle and present anti-inflammatory and antimicrobial effect. Its use as monotherapy is not recommended, but combined with PB, it shows increased efficacy and decreased bacterial resistance.1
Fixed combinations
Fixed combinations have advantages over monotherapy because they act on several etiopathogenic factors. They have antimicrobial, anti-inflammatory and comedolytic activity while increasing PB penetration. They are the first choice for mild to moderate papular-pustular acne. The available options are: PB with clindamycin or erythromycin, tretinoin with clindamycin and PB with adapalene. There are two concentrations of adapalene combined with PB available in some countries: 0.1% for mild to moderate pustular acne and 0.3% approved in the United States and indicated for moderate to severe forms. Use of a single product increases adherence ensuring better results.5,6
Azelaic Acid (AA)
Azelaic acid is a saturated dicarboxylic acid that normalizes follicular hyperkeratinization by a cytostatic effect on keratinocytes. It decreases proliferation of P. acnes by inhibiting protein synthesis, and reduces inflammation by activating nuclear PPARγ receptors, inhibiting activation of NF-kB pathway and blocking the release of free radicals. It also has a bleaching action. AA is indicated for mild to moderate papular-pustular acne, particularly in patients with sensitive and darker skin, as well as in adult acne in women. AA is Category B for use in pregnancy.1,7
SYSTEMIC TREATMENT
Oral Antibiotics
The use of oral antibiotics (OABs) has been a mainstay of acne treatment for years.1 Their indication is papular-pustular and mild nodular-cystic acne. They are effective due to their antibacterial, immunosuppressive, but fundamentally by their anti-inflammatory actions. OABs should be used from 6 to 12 weeks. Their effect depends on gastrointestinal permeability, absorption, distribution and penetration into the skin. The more soluble and permeable ones are better absorbed and distributed, while the lipophilic ones penetrate better in the pilosebaceous follicle. P. acnes is the main bacteria involved in the etiopathogenesis of acne. It produces lipases that hydrolyze triglycerides, releasing pro-inflammatory fatty acids. P. acnes is recognized by TLR-2 and 4, activating the NF-κB pathways, with production of IL-6 and IL-8 by follicular keratinocytes and IL-8 and IL-12 by macrophages and AP-1, with production of matrix metalloproteinases (MMP) that degrade the dermal extracellular matrix causing scars. Doxycycline 100 mg/day, lymecycline 300mg/day, minocycline, 100mg/day and tetracycline 500mg twice daily, are the most used OABs. Erythromycin 1,000mg per day is recommended for pregnant women and infants. Dapsone is indicated for patients with nodular-cystic acne at doses of 50 to 100mg/day. Adverse events of OAB are gastrointestinal (epigastralgia, nausea and vomiting); photosensitivity and phototoxic reactions (doxycycline); hypersensitivity reactions, pigmentation and autoimmune phenomena (minocycline). Misuse of OABs may induce bacterial resistance due to several factors: monotherapy, prolonged use, indiscriminate use without strict adherence, dose below recommended, not association with the use of topical PB and/or retinoid and improper rotational use. Consequences are not limited to P. acnes, but to other bacteria, particularly Staphylococcus aureus in upper respiratory tract infections. It occurs more frequently with erythromycin (50%) than with tetracycline derivatives (20%).1,8
Isotretinoin
Isotretinoin is effective and safe in the treatment of severe acne, with prolonged remission or cure.1 It is a sebum-suppressive agent, reducing the sebum production, the comedogenesis and the size of the sebaceous gland. Inhibits terminal sebocyte differentiation and alters follicular microenvironment, decreasing colonization by P. acnes and reducing inflammation by modulating TLR-2 and 4.9 The bioavailability of the medication is increased by 25% with fat food reaching a plasma peak in 2 to 4 hours. It has low affinity for RARs. It is a prodrug with metabolite-dependent effects and metabolized in the liver by the P-450 system. Its approved indication is for severe nodular-cystic acne and papular-pustular acne that does not improve with conventional treatment or that present response, but with rapid relapse, tendency to leave scars and negative psychosocial impact. A daily dose of 0.5 to 1.0mg/kg and a total dose of 120 to 150mg/kg is recommended. In severe acne, prolonged treatment, higher dose of the medication or several cycles may be necessary. It should not be administered with other retinoids, vitamin A, tetracycline or derivative antibiotics, methotrexate, cyclosporine and imidazole antifungals. Common, controllable and dose-dependent adverse events are: cheilitis, xerosis cutis, facial dermatitis, nasal dryness, epistaxis, dry eyes, blepharoconjunctivitis and contact lens intolerance. Prevention and early treatment of these adverse events is important and should be done with lip and nasal balms, lubricant eye products, skin moisturizers and sunscreens. In patients with severe acne, exacerbation, with new inflammatory lesions, may occur three to four weeks after starting treatment, with a risk of scarring. To reduce this exacerbation the treatment should start with a daily low dose, combined with oral corticosteroids and antibiotics (except tetracyclines), until the lesions improve, when they are withdrawn and the dose of isotretinoin is increased. Other unpredictable events that are depending on dose and individual susceptibility are: elevation of liver enzymes and triglycerides, increase of serum cholesterol LDL fraction, and decreased HDL fraction as well as hematological changes. Laboratory monitoring is mandatory at baseline and after 1 to 2 months. If tests are abnormal, they should be repeated every month.10 Teratogenicity is the most serious and irreversible event. Pregnancy test is mandatory in women and must be performed every month before the next dose of the medication. The contraceptive period, with two contraceptive methods, should be one month before the beginning of the treatment, during and one month after the cessation of treatment without risk for future pregnancies.1 Some other adverse events, with very low or absent risk are: bone alterations (premature closure of the epiphysis, higher risk of keloids and hypertrophic scars, depression, suicidal ideation and suicide attempt - on the contrary, this medication improves quality of life -, and inflammatory bowel disease - demonstrated with tetracyclines and not confirmed in population-based, case-control studies).11-13 the recurrence of acne may occur within the first year after treatment. Also, 29% of patients require more than one cycle, 25% two cycles and 3% three cycles.1
Hormonal agents
For women, with or without hyperandrogenemia, hormonal blockade is useful because acne is an androgen-dependent disease. This is a safe and effective alternative, either alone or associated with topical treatments. The activity of the sebaceous gland - the production of sebum - depends on the activation of androgen receptors in the sebocytes by androgens produced by the gonads, adrenal and sebaceous gland. Treatment reduces plasma and peripheral concentration of androgens and production and qualitative changes in sebum, reduce colonization of P. acnes at pilosebaceous follicle. The most commonly used drugs that block receptors and inhibit ovarian production are cyproterone acetate and drospirenone, present in oral contraceptives in combination with ethinyl estradiol. Spironolactone (50 to 100mg/day) may be used to block androgen receptors. To inhibit the adrenal production, it is indicated the use of low doses of corticosteroids (prednisone 2.5 to 5mg/day).14
Meta-analysis comparing the efficacy of combined oral contraceptives (COCs) versus OABs concluded that both, compared with placebo, reduced acne lesions. OABs were superior after 3 months of treatment and COCs were equivalent at the sixth month, that is, COCs may represent the first-line for prolonged treatments in adult women. Their adverse events include nausea, headache, mastodynia, sporadic bleeding and decreased libido. Benefits include protection against ovarian and endometrial cancer, reduction of dysmenorrhea, iron deficiency anemia, and pelvic inflammatory disease. Incidence of venous thromboembolism in young women is low; however, there is an increase of 0.05% to 0.1% with COCs. They should be avoided in smokers, family history or risk of deep venous thrombosis and cardiovascular disease. Insulin sensitizers (e.g. metformin) are indicated only in polycystic ovary syndrome, improving hirsutism and acne.15
Corticosteroids
Corticosteroids are indicated in severe nodular-cystic acne, conglobata, fulminans, and severe acne at the beginning of the treatment with oral isotretinoin, as mentioned before, and in the adult woman with adrenal hyperandrogenism. The most commonly used are prednisone, prednisolone, deflazacort, dexamethasone and methylprednisolone.
ADJUNCTIVE THERAPY
Cosmetic procedures
Manual comedone extraction, unclogs follicular infundibulum, facilitates the penetration of topical products, providing a positive impact on the quality of life and avoiding improper manipulation of lesions by the patient and/or inexperienced people. The electrocauterization of closed macro-comedones should be superficial to decrease the risk of scars. It is useful to avoid the evolution to papular-pustular lesions and manipulation. The intralesional corticosteroid injection (triamcinolone acetonide) is used in isolated nodules, accelerating their regression and relieving pain, as well as in hypertrophic and keloid scars, with total or partial regression. Drainage of cysts and abscesses is done when there is fluctuation in lesions and should be associated with oral antibiotics. Superficial chemical peels (20% to 30% salicylic acid, Jessner's solution, 10% trichloroacetic acid or 20% aqueous solution, and 70% glycolic acid in gel, with partially buffered pH) are useful for comedonal and papular-pustular acne by their keratolytic action. All cause temporary burning, erythema and desquamation after 3 to 5 days to 7 to 15 days. Cryotherapy with liquid nitrogen is indicated to treat inflammatory nodules, hypertrophic scars and keloids, but its use is decreasing due to the risk of hypochromic sequelae. Microdermabrasion is a very superficial exfoliation method equivalent to superficial peeling, simple and safe.16
Light or LED - light emitting diode - blue or red exhibits photochemical, immunomodulatory and anti-inflammatory effects faster than drug treatment and can be associated in the early stages improving adherence to treatment. Photo-pneumatic therapy is a relatively new technology in the treatment of acne and appears to be effective in moderate cases combining photochemical effects with mechanical extrusion of comedones in addition to a light photothermal effect. Among the laser or light procedures, the most evidence is photodynamic therapy, which uses a photosensitizer, such as aminolevulinic acid, applied for 1 to 3 hours, during which it is absorbed by the sebocytes and later activated by a laser or light device, generating ROS that damage the sebaceous glands and reduce P. acnes. Although this treatment is promising, more controlled studies are needed to determine the ideal photosensitizer, incubation time, and light source.17
Dermocosmetics
In the mild and early forms of acne (comedonal, with hyperseborrhea), salicylic acid-based dermocosmetics, lipo-hydroxy-acids, retinol, glycolic acid (in low concentrations) and nicotinamide may be sufficient to control the disease. Moisturizers help to reduce adverse events of topical products and dryness due to oral isotretinoin, by improving the epidermal barrier that is essential to prevent and reduce inflammation. Sunscreens and nicotinamide prevent postinflammatory hyperpigmentation. Cleansing agents suitable for oily skin or sensitive skin, with ingredients that control sebaceous secretion, should be preferred. Camouflage with non-comedogenic makeup is useful for improving women's self-esteem.4
Proper and honest use of these products benefit drug treatment, reduce adverse events, decrease the need for topical antibiotics and improve adherence/compliance to the therapeutic plan.4
Treatment of acne scars is a different chapter and will be treated separately.
Footnotes
Conflict of interest: none.
Study conducted at the Colégio Ibero-Latino Americano de Dermatologia - Buenos Aires, Argentina.
Financial support: none.
REFERENCES
- 1.Zaenglein AL, Pathy AL, Schlosser BJ, Alikhan A, Baldwin HE, Berson DS, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74:945–973. doi: 10.1016/j.jaad.2015.12.037. e33. [DOI] [PubMed] [Google Scholar]
- 2.Hsu P, Litman GI, Brodell RT. Overview of the treatment of acne vulgaris with topical retinoids. Postgrad Med. 2011;123:153–161. doi: 10.3810/pgm.2011.05.2294. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan YC, Ozsarfati J, Etwel F, Nickel C, Nulman I, Koren G. Pregnancy outcomes following first-trimester exposure to topical retinoids: a systematic review and meta-analysis. Br J Dermatol. 2015;173:1132–1141. doi: 10.1111/bjd.14053. [DOI] [PubMed] [Google Scholar]
- 4.Araviiskaia E, Dréno B. The role of topical dermocosmetics in acne vulgaris. J Eur Acad Dermatol Venereol. 2016;30:926–935. doi: 10.1111/jdv.13579. [DOI] [PubMed] [Google Scholar]
- 5.Dréno B, Bettoli V, Ochsendorf F, Layton AM, Perez M, Dakovic R, et al. Efficacy and safety of clindamycin phosphate 1.2%/tretinoin 0.025% formulation for the treatment of acne vulgaris: pooled analysis of data from three randomised, double-blind, parallel-group, phase III studies. Eur J Dermatol. 2014;24:201–209. doi: 10.1684/ejd.2014.2293. [DOI] [PubMed] [Google Scholar]
- 6.Kim SY, Ochsendorf FR. New developments in acne treatment: role of combination adapalene-benzoyl peroxide. Ther Clin Risk Manag. 2016;12:1497–1506. doi: 10.2147/TCRM.S94062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thiboutot D. Versatility of azelaic acid 15% gel in treatment of inflammatory acne vulgaris. J Drugs Dermatol. 2008;7:13–16. [PubMed] [Google Scholar]
- 8.Dreno B, Thiboutot D, Gollnick H, Bettoli V, Kang S, Leyden JJ, et al. Antibiotic stewardship in dermatology: limiting antibiotic use in acne. Eur J Dermatol. 2014;24:330–334. doi: 10.1684/ejd.2014.2309. [DOI] [PubMed] [Google Scholar]
- 9.Dispenza MC, Wolpert EB, Gilliland KL, Dai JP, Cong Z, Nelson AM, et al. Systemic isotretinoin therapy normalizes exaggerated TLR-2 mediated innate immune responses in acne patients. J Invest Dermatol. 2012;132:2198–2205. doi: 10.1038/jid.2012.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tan J, Boyal S, Desai K, Knezevic S. Oral isotretinoin: new developments relevant to clinical practice. Dermatol Clin. 2016;34:175–184. doi: 10.1016/j.det.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 11.Wootton CI. Should isotretinoin be stopped prior to surgery? A Critically Appraised Topic. Br J Dermatol. 2014;170:239–244. doi: 10.1111/bjd.12761. [DOI] [PubMed] [Google Scholar]
- 12.Sundström A, Alfredsson L, Sjölin-Forsberg G, Gerdén B, Bergman U, Jokinen J. Association of suicide attempts with acne and treatment with isotretinoin: retrospective Swedish cohort study. BMJ. 2010;341:c5812. doi: 10.1136/bmj.c5812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stobaugh DJ, Deepak P, Ehrenpreis ED. Alleged isotretinoin-associated inflammatory bowel disease: Disproportionate reporting by attorneys to the Food and Drug Administration Adverse Event Reporting Syste. J Am Acad Dermatol. 2013;69:393–398. doi: 10.1016/j.jaad.2013.04.031. [DOI] [PubMed] [Google Scholar]
- 14.Bettoli V, Zauli S, Virgili A. Is hormonal treatment still an option in acne today? Br J Dermatol. 2015;172:37–46. doi: 10.1111/bjd.13681. [DOI] [PubMed] [Google Scholar]
- 15.Koo EB, Petersen TD, Kimball AB. Meta-analysis comparing efficacy of antibiotics versus oral contraceptives in acne. J Am Acad Dermatol. 2014;71:450–459. doi: 10.1016/j.jaad.2014.03.051. [DOI] [PubMed] [Google Scholar]
- 16.Florez-White M. Kaminsky A, Florez M. Acné, un enfoque global. 3rd ed. Vol. 16. Buenos Aires: CILAD; 2015. Procedimientos cosméticos complementários; pp. 225–230. e-book. [Google Scholar]
- 17.Momen S, Al-Niaimi F. Acne vulgaris and light-based therapies. J Cosmet Laser Ther. 2015;17:122–128. doi: 10.3109/14764172.2014.988727. [DOI] [PubMed] [Google Scholar]