Abstract
Yellow dots are follicular ostium filled with keratin and/or sebum. Initially, they were exclusively associated with alopecia areata. Currently they have also been described in androgenetic alopecia, chronic cutaneous (discoid) lupus erythematosus, and dissecting cellulitis. Due to the growing importance of trichoscopy and its findings in the evaluation of the scalp, this article describes the main diseases in which yellow dots are a common trichoscopic finding, highlighting its characteristics in each dermatosis.
Keywords: Alopecia, Dermoscopy, Hair diseases
INTRODUCTION
Yellow dots are trichoscopic findings that correspond to dilated follicular infundibulum filled with keratotic material and/or sebum.1,2 They are seen as rounded or polycyclic structures of distinct sizes, with color ranging from pinkish-yellow to brownish-yellow, usually devoid of hair shafts in their interior.2,3 However, in rare cases, it is possible to observe miniaturized or dystrophic vellus hair in the center of the ostium.2
First described in 2006 by Ross et al., yellow dots were initially considered pathognomonic signs of alopecia areata.4,5 However, it is now known that these structures can also be found in other diseases of the scalp, such as chronic cutaneous lupus erythematosus (CCLE), androgenetic alopecia, dissecting cellulitis and, less frequently, trichotillomania, featuring distinct characteristics in each of them.1,2,6 Their presence also depends on the age and skin phototype of the patient, being more visible in Caucasian and Asian patients, and rarely observed in prepubescent patients.7 Thus, this article summarizes the various peculiarities of the yellow dots in the dermatoses in which they are found, emphasizing their importance in the differential diagnosis among the multiple causes of alopecia.
DISCUSSION
Alopecia areata
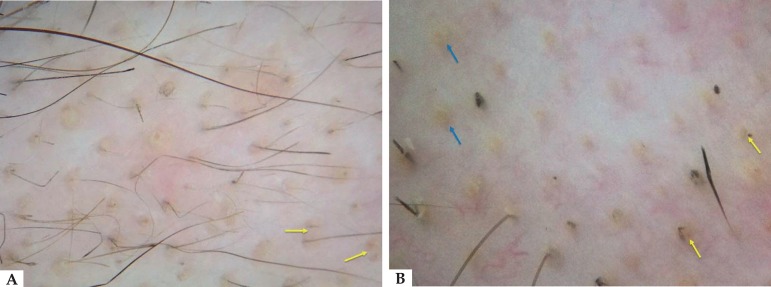
The observation of yellow dots is of great diagnostic value in the evaluation of hair loss.4 In relation to alopecia areata, they show great sensitivity and are observed in more than 60% of the patients.2,7 According to Inui et al. (2008), although yellow dots are associated with poor prognosis, their presence does not necessarily correlate with disease activity.4 They are generally numerous, pinkish-yellow in color, vary little in diameter (average of 210µm), and have a regular distribution in groups of two to three along the alopecia plaque (Figure 1).2
Figure 1.
Trichoscopy in alopecia areata. A: Presence of numerous yellow dots, some grouped in pairs (yellow arrows), with regular distribution along the lesion. B: Note multiple pinkish-yellow dots of uniform size and color (blue arrows), some with central dystrophic hairs (yellow arrows). Dermoscopy performed with 3Gen DermLite® II Hybrid M; X10 magnification
Androgenetic Alopecia
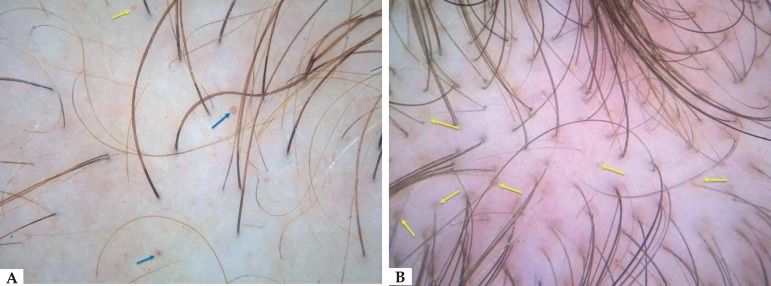
In androgenetic alopecia, in turn, yellow dots are seen in more advanced stages of the disease with a sebaceous component predominance over keratotic elements, differing from the other dermatosis, in which keratinocytic materials are predominant.1,7 It is believed that, in this condition, yellow dots result from the presence of engorged sebaceous glands that remain functioning despite the progress of the miniaturization process of the follicles, leading to the formation of intraepidermal sebaceous lakes.8 Such findings are observed in both male and female forms of the disease. They occur predominantly in the frontal region in relation to the occipital region, have irregular size and distribution, and are less numerous when compared to the amount found in alopecia areata (Figure 2).2 Moreover, their occurrence is so important in female pattern alopecia that the existence of four or more yellow dots on four trichoscopic fields in the frontal region is one of the major trichoscopic criteria for the diagnosis of the disease. In this way, the presence of yellow dots contributes not only to the correct detection of this dermatosis, but also sometimes reduces the need for more invasive diagnostic methods.8
Figure 2.
Trichoscopy in androgenetic alopecia. A: Frontal region revealing the presence of yellow dots of different sizes and color, ranging from pale yellow (yellow arrow) to brownish-yellow (blue arrows). Note the irregular distribution of these structures along the affected area. B: Vertex showing multiple yellow dots of varying sizes and colors, some associated with miniaturized hairs. Dermoscopy performed with 3Gen DermLite® II Hybrid M; X10 magnification
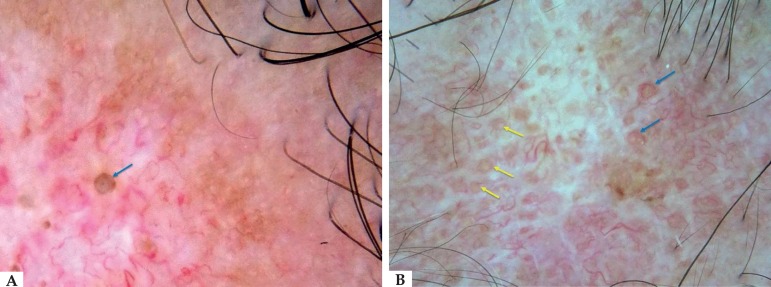
CCLE
Yellow dots in CCLE are larger, well delimited and sparse, corresponding to hyperkeratosis and follicular caps observed on histopathological examinations (Figure 3).9 They are typical of the active phase of the disease and are brownish-yellow in color, with double contour and large dimensions (mean diameter 650 µm).2,9 As the disease progresses to late stages, these structures become paler and poorly demarcated.2 The presence of thin arborizing vessels emerging radially from a large yellow dot constitutes the "red spider in a yellow dot" pattern and is considered peculiar of pre-fibrotic stages of lupus (Figure 3).1,2,9
Figure 3.
Trichoscopy in chronic cutaneous lupus erythematosus. A: Presence of a large brownish-yellow dot with a double contour in the center of the atrophic area (blue arrow). B: Yellow dots with double contour and irregular dimensions (yellow arrows). Observe the presence of fine arborizing vessels emerging from some yellow dots – “red spider in a yellow dot” – typical of pre-fibrotic stages of the disease (blue arrows). Dermoscopy performed with 3Gen DermLite® II Hybrid M; X10 magnification
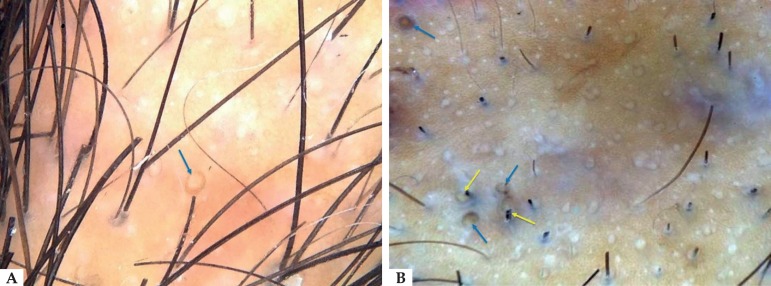
Dissecting Cellulitis
Another dermatosis that also may present with yellow dots is dissecting cellulitis. In this case, as in lupus, they present themselves as large structures observed in trichoscopy. However, the characteristic yellow dots observed in dissecting cellulitis have a three-dimensional appearance, resembling soap bubbles, with or without hair shafts (Figure 4).1,2 Such structures are strongly suggestive of this clinical condition and are not observed in other cicatricial or non-cicatricial forms of alopecia. This pattern is observed in almost all patients during the active phase of the disease.2,9
Figure 4.
Trichoscopy in dissecting cellulitis. A: Occipital region showing a large single yellow dot, of three-dimensional appearance, resembling a soap bubble (blue arrow). B: Three-dimensional brownish-yellow dots with irregular distribution along the plaque (blue arrows). Observe the presence of dystrophic hairs inside some yellow dots (yellow arrows). Dermoscopy performed with 3Gen DermLite® II Hybrid M; X10 magnification
Other disorders of the scalp
In addition to the aforementioned dermatosis, yellow dots may also occur in other conditions, such as congenital hypotrichosis, tinea capitis, seborrheic dermatitis and trichotillomania.6,7 In the latter, yellow dots are considered rare findings4,6 and were observed in only 7% of the patients studied by Rakowksa et al.10 In most cases, yellow dots contained a black dot in their central part or fine black hair residues, which corresponded to the remains of the intentionally removed capillary shafts.4,6,10 In addition, they are small in number and have irregular distribution along the affected area, features that aid in the differential trichoscopic diagnosis of alopecia areata.6,10
FINAL CONSIDERATIONS
The visualization of yellow dots by trichoscopy is of great relevance to diagnostic conclusion, definition of disease activity and determination of prognostic factors. Such structures are present in several dermatological conditions, having distinct characteristics in each of them. Therefore, it is fundamental for the dermatologist to recognize these peculiarities in the context of each dermatosis in order to reach the correct diagnosis and conduct each case appropriately.
Footnotes
Conflict of interest: none.
Work performed at Hospital Naval Marcílio Dias (HNMD) - Rio de Janeiro (RJ), Brazil
Financial support: None.
REFERENCES
- 1.Rudnicka L, Olszewska M, Rakowska A, Slowinska M. Trichoscopy update 2011. J Dermatol Case Rep. 2011;5:82–88. doi: 10.3315/jdcr.2011.1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rudnicka L, Olszewska M, Rakowska A. Atlas of trichoscopy - Dermoscopy in hair and scalp disease. London: Springer; 2012. [Google Scholar]
- 3.Jain N, Doshi B, Khopkar U. Trichoscopy in alopecias: diagnosis simplified. Int J Trichology. 2013;5:170–178. doi: 10.4103/0974-7753.130385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Inui S, Nakajima T, Nakagawa K, Itami S. Clinical significance of dermoscopy in alopecia areata: analysis of 300 cases. Int J Dermatol. 2008;47:688–693. doi: 10.1111/j.1365-4632.2008.03692.x. [DOI] [PubMed] [Google Scholar]
- 5.Park J, Kim JI, Kim HU, Yun SK, Kim SJ. Trichoscopic findings of hair loss in korean. Ann Dermatol. 2015;27:539–550. doi: 10.5021/ad.2015.27.5.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abraham LS, Torres FN, Azulay-Abulafia L. Pistas dermatoscópicas para diferenciar a tricotilomania da alopecia areata em placas. An Bras Dermatol. 2010;85:723–726. doi: 10.1590/s0365-05962010000500022. [DOI] [PubMed] [Google Scholar]
- 7.Miteva M, Tosti A. Hair and scalp dermatoscopy. J Am Acad Dermatol. 2012;67:1040–1048. doi: 10.1016/j.jaad.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 8.Rakowska A, Slowinska M, Kowalska-Oledzka E, Olszewska M, Rudnicka L. Dermoscopy in Female Androgenic Alopecia: Method Standardization and Diagnostic Criteria. Int J Trichology. 2009;1:123–130. doi: 10.4103/0974-7753.58555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rakowska A, Slowinska M, Kowalska-Oledzka E, Warszawik O, Czuwara J, Olszewska M, et al. Trichoscopy of cicatricial alopecia. J Drugs Dermatol. 2012;11:753–758. [PubMed] [Google Scholar]
- 10.Rakowska A, Slowinska M, Olszewska M, Rudnicka L. New trichoscopy findings in trichotillomania: flame-hairs, v-signs, hook hairs, hair powder, tulip hair. Acta Derm Venereol. 2014;94:303–306. doi: 10.2340/00015555-1674. [DOI] [PubMed] [Google Scholar]