Abstract
The Association of Public Health Epidemiologists in Ontario (APHEO) Core Indicators Work Group standardizes definitions and calculation methods for over 120 public health indicators to enhance accurate and standardized community health status reporting across public health units in Ontario. The Built Environment Subgroup is a multi-disciplinary group made up of planners, researchers, policy analysts, registered dietitians, geographic information systems (GIS) analysts and epidemiologists. The Subgroup selected and operationalized a suite of objective, standardized indicators intended to help public health units and regional health authorities assess their community retail food environments. The Subgroup proposed three indicators that use readily available data sources and GIS tools to characterize geographic access to various types of retail food outlets within neighbourhoods in urban settings. This article provides a status report on the development of these food environment indicators.
Keywords: measurement, food environment, urban environments, food retail, built environment
Highlights
Environmental factors (such as the unhealthy food retail that is easily accessible throughout communities) are gaining recognition as important determinants of food choice and diet-related health outcomes such as obesity.
There is a lack of consistency in food environment measures, which is problematic for the many jurisdictions across Canada interested in implementing policies to improve the food environment.
This paper provides a status report on recent work done to develop a set of standardized, objective indicators (i.e. measures) to aid public health units and regional health authorities assess their community food environments within urban settings.
Three indicators were selected to assess different dimensions of the community food environment: (1) intensity (i.e. density) of food outlets; (2) the relative density of less healthy food outlets; and (3) proximity of the population, living in specific geographic areas, to food outlets.
Introduction
Poor diet and excess body weight account for a significant share of disease burden in Canada and are among today’s most pressing public health challenges.1,2,3,4 The vast majority of Canadians do not consume a healthy diet5 and the prevalence of obesity has tripled over the past three decades.6 In 2011 to 2012, one in four or 6.3 million Canadians had obesity,7 and in 2012 to 2013, 62% of Canadian adults were overweight or had obesity based on measured height and weight data.8 Dietary patterns and body weight are complex issues influenced by biological, behavioural and contextual factors.9,10
The food environment is gaining recognition as a major determinant of food choices and diet-related outcomes such as obesity.10,11 Thus, a promising approach to improving population-level dietary patterns and associated health outcomes is to intervene in the environments in which food purchasing and consumption decisions are made.12,13,14,15,16
Food environment researchers acknowledge the complex psychosocial and environmental factors influencing dietary habits, and have investigated various aspects of the food environment in relation to food purchasing and consumption behaviours, and related health outcomes. 17-21 In Glanz and colleagues’ foundational paper on healthy nutrition environments,19 the food environment is conceptualized to consist of multiple dimensions, including the media environment, organizational environments (e.g. schools and workplaces), the community environment (i.e. type and location of stores and restaurants in neighbourhoods) and the consumer environment (i.e. availability, price and promotion of foods in stores and restaurants). Assessment of and interventions within the organizational food environment has been the focus of much research to date.22,23,24 The body of research on community and consumer environments has also grown considerably over the past decade, employing hundreds of different food environment measures.25 The use of inconsistent and diverse food environment measures has been regularly identified as a key limitation in this field of research.17,18,20 Measures of the consumer environment tend to be resource-intensive to implement (e.g. inventory-type measures to assess the availability and pricing of specific foods and beverages or the shelf space dedicated to fruits and vegetables). Therefore, the current report focusses on describing methods for the consistent assessment of community food environments across Ontario health units, using standardized measures that are feasible to implement.
Despite the growing interest over the past decade in the health impacts of food environments, the overall pattern of findings remains inconsistent.17,18,20 One reason for this may be the hundreds of different measures used to assess the food environment, 18,20,25,26,27 which challenge researchers’ ability to compare results of different studies across populations, social and economic contexts, geographic regions and trends over time.17,18,27,28,29 This lack of consistency in food environment measures is also problematic for the many jurisdictions across Canada interested in implementing policies to improve the food environment, but challenged by a lack of guidance on how best to assess their local food environments.30
This paper provides a status report on recent work done by the Association of Public Health Epidemiologists in Ontario (APHEO) to develop a set of standardized, objective indicators (i.e. measures) to aid public health units and health authorities in assessing their community food environments within urban settings. These indicators use readily available datasets and geographic information systems (GIS) methodology to characterize geographic access to various types of retail food outlets within neighbourhoods in urban settings.
APHEO Built Environment Subgroup
The Built Environment Subgroup* of the APHEO Core Indicators Work Group recognized the need of public health practitioners to assess their local food environments and identified the lack of consistent assessment tools as one of the largest practice gaps.
Indicator selection and adaptation
A nonsystematic scoping review of the literature was conducted for the Subgroup in 2014. PubMed, Web of Science and Scopus were searched for peer-reviewed articles published in English at any time up to and including May 2014. We used a variety of search terms including “food/ nutrition environment” and “retail food access” to identify studies that reported quantitative findings on some aspect of the retail food environment in relation to dietary or weight-related outcomes. Reviews, conceptual papers and commentaries were also included, as were studies of the school food environment. The quality of studies and the psychometric properties of food environment measures in the reviewed studies were not assessed. As selection and adaptation of the indicators unfolded, key empirical and review papers published after May 2014 were also reviewed by the Subgroup.
We reviewed article titles and abstracts, and selected 190 articles from the search results. Consistent with a number of previous systematic reviews of food environment studies,17,18,20,31,32 our literature scan found that of the different dimensions of the food environment,19 the community food environment (i.e. geographic access to local retail food outlets) has been studied most extensively, potentially due to the ease of obtaining the required retail food data and the growing availability of GIS-based tools.31,32 Given that the availability of reliable data and GIS tools are critical to public health for monitoring, surveillance and awareness building, objective measures of geographic access to food retail within communities were selected as the primary area of focus for our indicator selection.
Similar to findings from previous systematic reviews, we found that objective measures of geographic access to local stores and restaurants are commonly classified into three types of measures: density, proximity and variety.17,18,20,27,31 Density measures typically assess the concentration of outlets (i.e. number) per neighbourhood population or geographic area. Proximity is most commonly measured as the distance between a location (e.g. residential area or school) and the nearest outlet of a particular type (e.g. grocery or convenience store). Finally, variety measures attempt to reflect the relative mix of various types of outlets within a particular area. Such measures have been used in a number of recent investigations of the local food environment,33-36 and can be used in conjunction with other community food environment measures (such as in-store assessments) or layered with demographic information to provide a comprehensive understanding of the retail food environment at varying geographic scales (e.g. at the neighbourhood, municipal or regional levels).
Following our review of the existing literature, we chose three indicators reflecting different dimensions of the community food environment: (1) intensity (i.e. density) of food outlets; (2) the relative density of less healthy food outlets; and (3) proximity to food outlets. These indicators reflect the most commonly studied objective aspects of geographic food access in communities, and can be readily created in Ontario using a health unit’s existing food premise inspection database, standard geographic units from the Canadian census (or custom geographic units, if available), and the Ontario Road Network (or another road network file) in a GIS environment. All indicators measure the food environment within 1000 m (approximately a 10- to 15-minute walk) from residential areas, a distance that has been commonly used37,38,39 in previous studies to represent a neighbourhood environment easily accessible by walking.34,35,40
Indicator definitions
1. Density: population-weighted average number of food outlets of a given category within 1000 m† of dissemination block (DB) centroids per dissemination area (DA)‡ (or another geographic area of interest, such as the household vicinity).
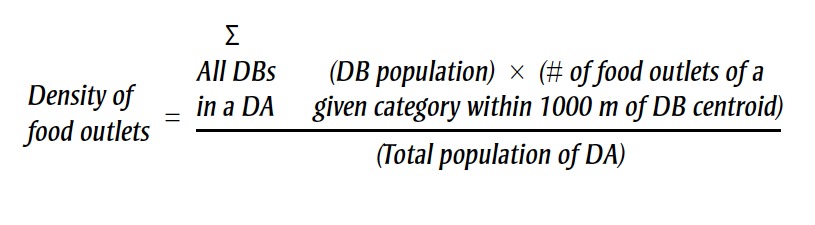 |
2. Relative density (also known as the Modified Retail Food Environment Index [mRFEI]): ratio of unhealthy food retailers to both healthy and unhealthy food retailers within 1000 m of DBs per DA (or another, larger geographic area of interest, such as census tracts, administrative division or neighbourhood).
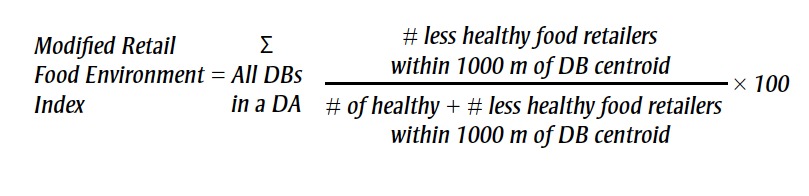 |
3. Proximity: Population-weighted mean network distance (metres) between dissemination block (DB) centroids and nearest food outlets of a given category per dissemination area (DA) (or geographic unit of interest).
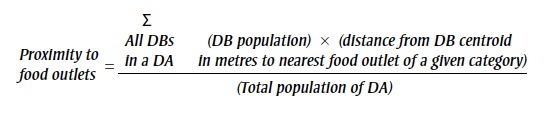 |
The APHEO Built Environment Subgroup is an interdisciplinary team of public health planners, researchers, policy analysts, public health nutritionists, GIS analysts and epidemiologists.
1000 metres is considered to be approximately a 15-minute walk for an adult in an urban setting.32
Statistics Canada defines a dissemination block as “…an area bounded on all sides by roads and/or boundaries of standard geographic areas. The dissemination block is the smallest geographic area for which population and dwelling counts are disseminated. Dissemination blocks cover all the territory of Canada.”41 A dissemination area is a “small area composed of one or more neighbouring dissemination blocks, with a population of 400 to 700 persons.”42
Classification of food retail types
Food retailers can be classified into different categories using Standard Industry Classification (SIC) codes or the newer system of North American Industry Classification System (NAICS) codes.43,§ These indicators of intensity and proximity can be calculated either for a specific outlet category (e.g. supermarket) or for a range of outlets classified as healthy or unhealthy, as indicated for the relative density indicator (i.e. a measure of the relative density of outlets offering unhealthy options).46,47,48 Previous studies have commonly classified supermarkets, grocery stores and fruit and vegetable markets as “healthy” food retail, while convenience stores and fast-food (i.e. limited-service) restaurants have been classified as “unhealthy” retail food outlets.44,49,50 While it is acknowledged that highly processed foods that are energy-dense and nutrientpoor can be purchased at “healthy” food retailers (e.g. supermarkets) and minimally processed nutrient-dense foods can be purchased at “unhealthy” food retailers (e.g. convenience stores or limited-service restaurants offering vegetables, fruit or less processed items), previous research has found that the consumer nutrition environment—food purchasing cues within stores and restaurants—varies by outlet type.49,51,52
We used the following NAICS codes to classify common types of stores and restaurants available within communities: supermarkets and other grocery stores (NAICS 445110); fruit and vegetable markets (NAICS 445230); convenience stores (NAICS 445120); gasoline stations with convenience stores (NAICS 447110); and limited-service eating places (NAICS 722512). This list of outlet types is by no means exhaustive and can be customized according to each public health unit’s needs. Examples of alternative lists of outlets may be found in the reference list for this article.44,45
Discussion
A retail food environment that promotes and supports access to and availability of healthy food choices is one aspect of a healthy neighbourhood design and built environment. Assessing geographic access to food retail either independently or alongside additional consumer nutrition environment measures (i.e. in-store or inrestaurant audits) can provide a method for health units to characterize the local retail food landscape and thus increase their understanding of how community design impacts the health and well-being of populations. Other methods, such as questionnaires, interviews and store and restaurant inventory measures, can be used to measure resident perceptions of the food environment or the availability and price of nutritious food.32,53
Strengths and limitations
The APHEO Core Indicators were developed in order to systematically define and operationalize a core set of health indicators due to a recognized need for consistency among health reports and to enable true comparisons across health units. They describe complex concepts in a concrete, clearly defined way using standardized definitions and methods and form the foundation for community health status reporting in public health in Ontario. The three indicators of the community food environment presented in this report (i.e. intensity, relative density and proximity) are the first set of core indicators on the food environment in Ontario and will allow health units to monitor their food environment and examine associations with various health outcomes or socioeconomic data. As municipalities across Canada and globally are increasingly considering or implementing different policies to affect the local food environment (e.g. zoning by-laws to restrict fast-food outlets in certain areas), these indicators will enable health units to monitor the impact of these policies on a variety of health outcomes. Moreover, these indicators are consistent with those recently proposed by the international INFORMAS framework to monitor and benchmark community food environments.27 As such, the use of indicators outlined in this paper can potentially contribute toward international efforts to monitor local food environments in a consistent way, which is critical for the development of effective policy interventions.27
While the three indicators of the community food environment outlined in this paper were created in part to reflect the legislative requirements set in the Ontario Public Health Standards,54 they can be used by other regional health authorities to characterize their food environments since the indicators were designed for use by public health practitioners. Additionally, in an attempt to leverage complementary work, the APHEO Built Environment Subgroup recently consulted with Health Canada during the development of a manual intended to guide communities across Canada in assessing their food environments. As a result of these consultations, the Health Canada manual and APHEO are recommending the same set of indicators to characterize the community food environment in urban settings.
Despite the strengths of these indicators, there are some limitations. The retail food environment is continuously changing in response to the changing nature of food retail business models. For example, fastfood outlets are increasingly offering healthier choices, while grocery stores continue to introduce many highly processed food choices, which pose challenges to the current “healthy” and “unhealthy” food retail classifications. The impact of these changes can in part be ameliorated by ensuring that the consumer (i.e. in-store or in-restaurant) nutrition environment assessments specific to Canadian contexts55 are included in the evaluation of the local food environment.
Another challenge to measuring the community food environment using the proposed indicators is the reliance on public health inspection databases. While these types of databases are accessible to health unit staff in Ontario and some other provinces (in Quebec and Newfoundland and Labrador such data are collected at the provincial level), it is important to note that they classify retail food outlets based on food safety risk and not for research or monitoring purposes. Therefore, food retail outlets may need to be recategorized (e.g. convenience stores and fruit and vegetable shops are commonly assigned to a single low-risk “food store” category in food inspection databases, but for research purposes should be categorized into distinct outlet types).
Finally, these indicators were developed for use within urban settings. Several studies have proposed different methods for assessing rural environments, citing the unique ways in which rural residents interact with their food environment and the need to consider the dispersed form and unique socio-spatial structure of the rural environment.56,57,58,59
Conclusion
Given the high prevalence of poor diet quality and excess body weight in Canada, public health agencies are increasingly looking at policies to reshape food environments to better support and promote healthy, active living. A promising means by which local health practitioners can assess their local food environment is through the use of standardized indicators that use readily available data. These assessments can serve as valuable local surveillance data for evaluating the impact of policy interventions. The use of standardized measures that can be applied across Ontario (and Canada) has the added benefit of enabling accurate between-region comparisons of how different policies are reshaping the food environment and impacting health outcomes.
Acknowledgements
The authors would like to acknowledge all the members of the Built Environment Subgroup of the APHEO Core Indicators work group. LMM gratefully acknowledges a Canadian Cancer Society Career Development Award in Prevention Research (grant #704744).
Conflicts of interest
The authors declare no conflicts of interest.
Authors' contributions
AM and JYP drafted the manuscript, and all authors made revisions and approved the final version of the manuscript.
References
- Institute for Health Metrics and Evaluation; (cited 2016 Oct 27) 2012 . Seattle (WA): Global burden of disease (GBD) profile: Canada (Internet). Available from: http:// www.healthdata.org/sites/default /files/files/country_profiles/GBD /ihme_gbd_country_report_canada .pdf . [Google Scholar]
- Dee A, Kearns K, O’Neill C, et al. The direct and indirect costs of both overweight and obesity: A systematic review. BMC Res Notes (Internet) 2014 Apr 16 (cited 2016 Oct 26);;7:242. doi: 10.1186/1756-0500-7-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hruby A, Hu FB. The epidemiology of obesity: a big picture. Pharmacoeconomics. 2015;33((7)):673–89. doi: 10.1007/s40273-014-0243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health Agency of Canada. Public Health Agency of Canada; (modified 2011 Jun. cited 2017 Jun 29) Ottawa (ON): 23. Obesity in Canada: health and economic implications (Internet). Available from: http:// www.phac-aspc.gc.ca/hp-ps/hl-mvs /oic-oac/econo-eng.php . [Google Scholar]
- Garriguet D. Diet quality in Canada. Health Rep. 2009;20((3)):41–52. [PubMed] [Google Scholar]
- Twells L, Gregory D, Reddigan J, Midodzi W. CMAJ Open. (1) Vol. 2. Erratum in: 2014. Current and predicted prevalence of obesity in Canada: a trend analysis. CMAJ Open. 2014; 2(1):E18-E26. p. E35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navaneelan T, Janz T. Statistics Canada; 2014 (Statistics Canada Catalogue No. Ottawa (ON): Health at a glance. Adjusting the scales: obesity in the Canadian population after correcting for respondent bias. pp. 82–624. [Google Scholar]
- Statistics Canada; (cited 2016 Oct 26) 2014 . Ottawa (ON): Canadian Health Measures Survey: household and physical measures data, 2012 to 2013 (Internet). Available at: http://www.statcan .gc.ca/daily-quotidien/141029 /dq141029c-eng.pdf . [Google Scholar]
- Hawkes C, Smith TG, Jewell J, et al. Smart food policies for obesity prevention. Lancet. 2015;385((9985)):2410–21. doi: 10.1016/S0140-6736(14)61745-1. [DOI] [PubMed] [Google Scholar]
- Roberto CA, Swinburn B, Hawkes C, et al. Patchy progress on obesity prevention: emerging examples, entrenched barriers, and new thinking. Lancet. 2015;385((9985)):2400–9. doi: 10.1016/S0140-6736(14)61744-X. [DOI] [PubMed] [Google Scholar]
- Swinburn BA, Sacks G, Hall KD, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378((9793)):804–14. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- Ding D, Sallis JF, Conway TL, et al. Interactive effects of built environment and psychosocial attributes on physical activity: a test of ecological models. Ann Behav Med. 2012;44((3)):365–74. doi: 10.1007/s12160-012-9394-1. [DOI] [PubMed] [Google Scholar]
- Lake A, Townshend T. Obesogenic environments: exploring the built and food environments. J Royal Soc Promot Health. 2006;126((6)):262–7. doi: 10.1177/1466424006070487. [DOI] [PubMed] [Google Scholar]
- Lipek T, Igel U, Gausche R, Kiess W, Grande G. Obesogenic environments: environmental approaches to obesity prevention. J Pediatr Endocrinol Metab. 2015;28((5-6)):485–95. doi: 10.1515/jpem-2015-0127. [DOI] [PubMed] [Google Scholar]
- Mackenbach J, Rutter H, Compernolle S, et al. Obesogenic environments: a systematic review of the association between the physical environment and adult weight status, the SPOTLIGHT project. BMC Public Health (Internet) 2014 (cited 2017 April 16);;14:233. doi: 10.1186/1471-2458-14-233. http://dx.doi.org/10.1186/1471-2458-14-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis JF, Floyd MF, Rodríguez DA, Saelens BE. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125((5)):729–37. doi: 10.1161/CIRCULATIONAHA.110.969022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: a systematic review. Health Place. 2012;18((5)):1172–87. doi: 10.1016/j.healthplace.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb LK, Appel LJ, Franco M, Jones- Smith JC, Nur A, erson CA. Erratum: The relationship of the local food environment with obesity: a systematic review of methods, study quality, and results. Obesity (Silver Spring) 2015;23((12)):2517–19. doi: 10.1002/oby.21363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Sallis JF, Saelens BE, Frank LD. Healthy nutrition environments: concepts and measures. Am J Health Promot. 2005;19((5)):330–3. doi: 10.4278/0890-1171-19.5.330. [DOI] [PubMed] [Google Scholar]
- Minaker LM, Shuh A, Olstad DL, Engler-Stringer R, Black JL, Mah CL. Retail food environments research in Canada: a scoping review. Can J Public Health. 2016;107((Suppl 1)):eS4–eS13. doi: 10.17269/CJPH.107.5344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minaker LM. Retail food environments in Canada: maximizing the impact of research, policy and practice. Can J Public Health. 2016;107((Suppl 1)):eS1–eS3. doi: 10.17269/CJPH.107.5632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driessen CE, Cameron AJ, Thornton LE, Lai SK, Barnett LM. Effect of changes to the school food environment on eating behaviours and/or body weight in children: a systematic review. Obes Rev. 2014;15((12)):968–82. doi: 10.1111/obr.12224. [DOI] [PubMed] [Google Scholar]
- Williams AJ, Henley WE, Williams CA, Hurst AJ, Logan S, Wyatt KM. Systematic review and meta-analysis of the association between childhood overweight and obesity and primary school diet and physical activity policies. Int J Behav Nutr Phys Act (Internet) 2013 (cited 2016 Oct 18);;10:101. doi: 10.1186/1479-5868-10-101. http://dx.doi.org/10.1186/1479-5868-10 -101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verweij LM, Coffeng J, van Mechelen W, Proper KI. Meta-analyses of workplace physical activity and dietary behaviour interventions on weight outcomes. Obes Rev. 2011;12((6)):406–29. doi: 10.1111/j.1467-789X.2010.00765.x. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. Measures of the food environment (Internet). Bethesda (MD): National Cancer Institute. (modified 2016 May. 6;cited 2016 Oct 18) Available from: http:// epi.grants.cancer.gov/mfe. . [Google Scholar]
- Gamba RJ, Schuchter J, Rutt C, Seto EYW. Measuring the food environment and its effects on obesity in the United States: a systematic review of methods and results. J Community Health. 2015;40((3)):464–75. doi: 10.1007/s10900-014-9958-z. [DOI] [PubMed] [Google Scholar]
- Ni Mhurchu C, Vandevijvere S, Waterlander W, et al. Monitoring the availability of healthy and unhealthy foods and non-alcoholic beverages in community and consumer retail food environments globally. Obes Rev. 2013;14((Suppl 1)):108–19. doi: 10.1111/obr.12080. [DOI] [PubMed] [Google Scholar]
- Glanz K, Sallis JF, Saelens BE. Advances in physical activity and nutrition environment assessment tools and applications: recommendations. Am J Prev Med. 2015;48((5)):615–9. doi: 10.1016/j.amepre.2015.01.023. [DOI] [PubMed] [Google Scholar]
- McKinnon RA, Reedy J, Morrissette MA, Lytle LA, Yaroch AL. Measures of the food environment. a compilation of the literature, 1990–2007. Am J Prev Med. 2009;36((4 Suppl)):S124–S133. doi: 10.1016/j.amepre.2009.01.012. [DOI] [PubMed] [Google Scholar]
- Mah CL, Cook BE, Rideout K, Minaker LM. Policy options for healthier retail food environments in city-regions. Can J Public Health. 2016;107((Suppl 1)):eS64–eS67. doi: 10.17269/CJPH.107.5343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Canada. Minister of Health; Ottawa (ON): 2013. Measuring the food environment in Canada. p. (Catalogue No. [Google Scholar]
- Lytle LA, Sokol RL. Measures of the food environment: a systematic review of the field, 2007–2015. Health Place. 2017;44:18–34. doi: 10.1016/j.healthplace.2016.12.007. [DOI] [PubMed] [Google Scholar]
- Kershaw T, Creighton T, Markham T. Saskatoon Health Region; Saskatoon (SK): 2010. Food access in Saskatoon: community report. p. 25 p. [Google Scholar]
- Cushon J, Creighton T, Kershaw T, Marko J, Markham T. Deprivation and food access and balance in Saskatoon, Saskatchewan. Chronic Dis Inj Can. 2013;33((3)):146–59. [PubMed] [Google Scholar]
- Larsen K, Gilliland J. Mapping the evolution of ‘food deserts’ in a Canadian city: supermarket accessibility in London, Ontario, 1961–2005. Int J Health Geogr (Internet) 2008 Apr 18 (cited 2016 Oct 18);;7:16. doi: 10.1186/1476-072X-7-16. http://dx.doi.org/10.1186/1476-072X-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polsky JY, Moineddin R, Glazier RH, Dunn, Booth GL. Relative and absolute availability of fast-food restaurants in relation to the development of diabetes: a population-based cohort study. Can J Public Health. 2016;107((Suppl 1)):eS27–eS33. doi: 10.17269/CJPH.107.5312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey R, Chaix B, Weber C, Schweitzer B, Charreire H, Salze P, et al. Spatial accessibility to physical activity facilities and to food outlets and overweight in French youth. Int J Obes (Lond) 2012;36((7)):914–19. doi: 10.1038/ijo.2012.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy MA, Gilliland JA. Quantifying the magnitude of environmental exposure misclassification when using imprecise address proxies in public health research. Spat Spatiotemporal Epidemiol. 2012;3((1)):55–67. doi: 10.1016/j.sste.2012.02.006. [DOI] [PubMed] [Google Scholar]
- Sadler RC, Gilliland JA, Arku G. Community development and the influence of new food retail sources on the price and availability of nutritious food. J Urban Aff. 2013;35((4)):471–91. [Google Scholar]
- Engler-Stringer R, Le H, Gerrard A, Muhajarine N. The community and consumer food environment and children’s diet: a systematic review. BMC Public Health. 2014;14:522. doi: 10.1186/1471-2458-14-522. http://dx.doi.org/10.1186/1471-2458-14-522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada. Statistics Canada; (modified 2015 Nov. cited 2016 Oct 27) Ottawa (ON): 27. Dissemination block (DB) (Internet). Available from: https://www12.statcan.gc.ca /census-recensement/2011/ref/dict /geo014-eng.cfm . [Google Scholar]
- Statistics Canada. Statistics Canada; (modified 2015 Nov. cited 2016 Oct 27) Ottawa (ON): 27. Dissemination area (DA) (Internet). Available from: https://www12.statcan.gc.ca /census-recensement/2011/ref/dict /geo021-eng.cfm . [Google Scholar]
- Statistics Canada. Statistics Canada; (modified 2017 May. cited 2016 Oct 26) Ottawa (ON): 8. North American Industry Classification System (NAICS) Canada 2012 (Internet). Available from: http://www.statcan.gc.ca/eng /subjects/standard/naics/2012/index . [Google Scholar]
- Clary C, Kestens Y. Field validation of secondary data sources: a novel measure of representativity applied to a Canadian food outlet database. Int J Behav Nutr Phys Act (Internet) 2013;10:77. doi: 10.1186/1479-5868-10-77. http://dx.doi.org/10.1186/1479-5868-10-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsyth A, editor. editor. Available from: http://designforhealth .net/wp-content/uploads/2012/12 /TREC_Protocol_V1_3_Nov2007.pdf . [Google Scholar]
- Truong K, Fernandes M, An R, Shier V, Sturm R. Measuring the physical food environment and its relationship with obesity: evidence from California. Public Health. 2010;124((2)):115–8. doi: 10.1016/j.puhe.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Centers for Disease Control (CDC). CDC; (cited 2016 Oct 27) 2011 . Atlanta (GA): Census tract level state maps of the Modified Retail Food Environment Index (mRFEI) (Internet). Available from: ftp://ftp.cdc.gov/pub /Publications/dnpao/census-tract -level-state-maps-mrfei_TAG508.pdf . [Google Scholar]
- California Center for Public Health Advocacy (CCPHA). CCPHA; (cited 2016 Oct 27) 2007 . Davis (CA): Searching for healthy food: the food landscape in Solano County. Available from: http://foodoasis.solanocounty. com/documents/SolanoFastFood.pdf . [Google Scholar]
- Minaker LM, Raine KD, Wild TC, Nykiforuk CIJ, Thompson ME, Frank LD. Construct validation of 4 food-environment assessment methods: adapting a multitrait-multimethod matrix approach for environmental measures. Am J Epidemiol. 2014;179((4)):519–28. doi: 10.1093/aje/kwt272. [DOI] [PubMed] [Google Scholar]
- Polsky JY, Moineddin R, Glazier RH, Dunn, Booth GL. Foodscapes of southern Ontario: neighbourhood deprivation and access to healthy and unhealthy food retail. Can J Public Health. 2014;105((5)):e369–e375. doi: 10.17269/cjph.105.4541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Sallis JF, Saelens BE, Frank LD. Nutrition Environment Measures Survey in Stores (NEMS-S): development and evaluation. Am J Prev Med. 2007;32((4)):282–9. doi: 10.1016/j.amepre.2006.12.019. [DOI] [PubMed] [Google Scholar]
- Saelens BE, Glanz K, Sallis JF, Frank LD. Nutrition Environment Measures Study in Restaurants (NEMS-R): development and evaluation. Am J Prev Med. 2007;32((4)):273–81. doi: 10.1016/j.amepre.2006.12.022. [DOI] [PubMed] [Google Scholar]
- Glanz K, Johnson L, Yaroch AL, Phillips M, Ayala G, Davis E. Measures of retail food store environments and sales: review and implications for healthy eating initiatives. J Nutr Educ Behav. 2016;48((4)):280–8. doi: 10.1016/j.jneb.2016.02.003. [DOI] [PubMed] [Google Scholar]
- Ontario Ministry of Health and Long- Term Care. Queen’s Printer for Ontario; 2016 (revised 2017 Mar; Toronto (ON): cited 2016 Jun 1). Ontario public health standards, 2008 (Internet). Available from: http://www .health.gov.on.ca/en/pro/programs /publichealth/oph_standards/docs /ophs_2008.pdf . [Google Scholar]
- Lo BKC, Minaker L, Chan ANT, Hrgetic J, Mah CL. Adaptation and validation of a Nutrition Environment Measures Survey for university grab-and-go establishments. Can J Diet Pract Res. 2016;77((1)):17–24. doi: 10.3148/cjdpr-2015-036. [DOI] [PubMed] [Google Scholar]
- Lebel A, Noreau D, Tremblay L, et al. Identifying rural food deserts: methodological considerations for food environment interventions. Can J Public Health. 2016;107((Suppl 1)):eS21–eS26. doi: 10.17269/CJPH.107.5353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutko P. Food deserts suffer persistent socioeconomic disadvantage. Choices (Internet) 2012 (cited 2016 Oct 18);;Quarter 3 Available from: http://www.choicesmagazine.org /choices-magazine/theme-articles/an -evaluation-of-food-deserts-in-america /food-deserts-suffer-persistent -socioeconomic-disadvantage . [Google Scholar]
- McEntee J, Agyeman J. Towards the development of a GIS method for identifying rural food deserts: geographic access in Vermont, USA. Appl Geogr. 2010;30((1)):165–76. [Google Scholar]
- Mulangu F, Clark J. Identifying and measuring food deserts in rural Ohio. J Ext (Internet) 2012 (cited 2016 Oct 18);;50((3)) Available from: https:// www.joe.org/joe/2012june/a6.php. [Google Scholar]


