Abstract
Objective
To review articles on the relationship of dietary and circulating micronutrients with sleep patterns, and to identify issues surrounding implications for future research and public health practice.
Design
A systematic review was conducted. PubMed, Embase and Scopus were searched through January 2016.
Setting
Both experimental and observational studies were included. However, studies that focused on secondary sleep impairment due to comorbidities were excluded.
Subjects
Individuals in different age groups, from infants to older adults.
Results
A total of twenty-six articles were selected. In the articles reviewed, researchers generally supported a potential role of micronutrients, particularly Fe and Mg, in the development of sleep stages among infants and in reversing age-related alterations in sleep architecture in older adults. Micronutrient status has also been linked to sleep duration, with sleep duration positively associated with Fe, Zn and Mg levels, and negatively associated with Cu, K and vitamin B12 levels. The mechanisms underlying these relationships include the impact of micronutrients on excitatory/inhibitory neurotransmitters and the expression of circadian genes.
Conclusions
Although the number of studies on the relationship between micronutrient status and sleep remains low, evidence has emerged that suggests a link between dietary/circulating micronutrients and sleep. Future research is needed to investigate the dose-dependent as well as the longitudinal relationships between micronutrient levels and human sleep across populations, test the interactions among micronutrients on sleep outcomes, and ultimately examine the clinical relevance of micronutrients on sleep health.
Keywords: Micronutrient, Mineral, Vitamin, Trace element, Sleep
An optimal sleep pattern has important implications for health maintenance and health promotion( 1 ). However, cross-sectional studies have suggested that between 14 and 40 % of the general population has impaired sleep, including insufficient sleep duration, long sleep-onset latency, frequent and long nocturnal awakenings, and other sleep disturbances( 2 – 6 ). Sleep deprivation and sleep impairment can affect cognitive performance in children( 7 ) and adults( 8 ). Over time, impaired sleep patterns have been linked to depression( 9 ), obesity( 10 ), metabolic( 11 ) and cardiovascular diseases( 12 ), cancer( 13 ) and increased risk of mortality( 14 ). The high prevalence and consequent negative impact of sleep impairment highlight the importance of understanding potentially modifiable factors.
As the relationship between insufficient sleep, weight gain and obesity has been observed in both children( 10 ) and adults( 15 ), increasing attention has been given to the potential links between sleep, dietary intake and nutrition. Whereas current findings consistently support the impact of sleep deprivation and sleep problems on dietary intake and metabolic outcomes( 15 – 17 ), recent studies have revealed a reverse relationship between dietary or serum nutrient levels and sleep problems( 18 – 20 ). Researchers have found that macronutrients, such as carbohydrates and amino acids (specifically tryptophan), can involve and influence the levels of neurotransmitters in the intrinsic sleep processes and affect sleep patterns( 21 , 22 ). For example, low proportion of carbohydrate intake was found to increase the percentage of slow-wave sleep (SWS; or deep sleep) and reduce the percentage of rapid-eye-movement (REM) sleep among healthy good sleepers( 18 ).
Micronutrient intake has not received as much attention as macronutrients as a modifiable factor for sleep deprivation and sleep problems. However, experimental studies indicate that micronutrients may impact important nerve-signalling chemicals or neurotransmitters of sleep regulation, including serotonin( 22 ), N-methyl-d-aspartate (NDMA) glutamate( 23 ) and melatonin secretion( 24 ). Several epidemiological studies and clinical trials have also provided evidence to support the relationship between micronutrient intake and sleep patterns. For example, randomized controlled trials in infants found longer night-time and total sleep duration in those receiving supplemental Zn or Fe compared with the placebo group( 25 ). To date, however, no study has critically reviewed the current literature on the association between micronutrients and sleep in a developmental perspective for sleep patterns.
The aim of the current review was twofold: (i) to examine empirical research on the relationship of dietary or biological micronutrient levels with sleep patterns; and (ii) to identify issues surrounding implications for future research and public health practice. As micronutrient deficiency and poor sleep are of particular concern in both developed and developing countries( 26 – 29 ), understanding the possible roles of micronutrients in sleep will inform future prevention and intervention programmes for the multifaceted and interrelated public health issues of nutrition and sleep; and shed light on the full extent of their consequences on health.
Method
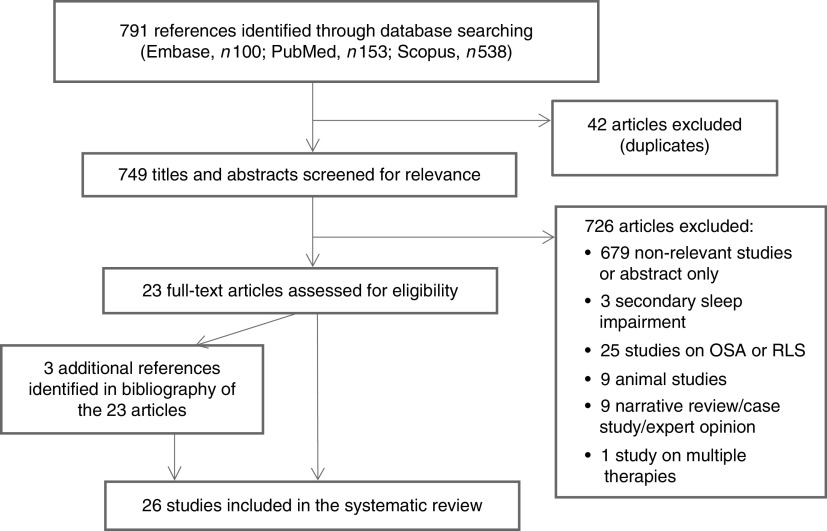
The current review was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement checklist( 30 ). We searched articles in PubMed, Embase and Scopus through January 2016. PubMed was searched using MeSH to identify articles with the medical subject headings ‘micronutrients’, ‘minerals’, ‘iron compounds’, ‘zinc’, ‘copper’, ‘cobalt’, ‘potassium’, ‘magnesium’, ‘calcium’, ‘sodium’, ‘phosphorus’, ‘manganese’ and ‘sleep’, and the keywords ‘vitamin*’, which yielded 153 articles. Embase was searched using EMTREE with ‘trace element’, ‘vitamin’, ‘mineral intake’, ‘mineral deficiency’, ‘mineral blood level’, ‘trace metal blood level’, ‘zinc deficiency’, ‘vitamin deficiency’, ‘sodium deficiency’, ‘selenium deficiency’, ‘potassium deficiency’, ‘phosphate deficiency’, ‘calcium deficiency’, ‘copper deficiency’, ‘iron deficiency’, ‘magnesium deficiency’, ‘cobalt’ and ‘sleep’, yielding 100 articles. Additionally, Scopus was searched using the keywords ‘micronutrient*’, ‘vitamin*’, ‘trace element’, ‘sleep’, ‘sleep pattern’ and ‘sleep quality’, identifying 538 results. As shown in Fig. 1 (PRISMA flow diagram of the article selection process), duplicates were identified and deleted in Refworks, yielding 749 potentially relevant articles. Twenty-three articles were identified for additional scrutiny after reviewing titles and abstracts. The reference lists of the twenty-three articles were then manually searched. Only articles published in English and Chinese and with full text available were considered. No year restriction was set in the literature search.
Fig. 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram of the article selection process (OSA, obstructive sleep apnoea; RLS, restless-leg syndrome)
Inclusion and exclusion criteria
Studies relevant to the research question were expected to focus on micronutrient intake or biological micronutrient levels and sleep patterns in human subjects. More specifically, the term ‘micronutrients’ refers to three types of nutrients: (i) vitamins; (ii) trace elements, such as Fe, Zn, Cu, Co, Se and Mn; and (iii) minerals, such as Ca, Mg and K( 31 ). The term ‘sleep pattern’ is used to denote frequently examined parameters in subjective and objective sleep studies, including sleep duration (the time one spends sleeping), sleep-onset latency (the amount of time from lights out, or bedtime, to the commencement of sleep), night awakenings (number of times waking up in the middle of the night), sleep stages (REM and four stages of non-REM (NREM) sleep scored according to standard polysomnographic criteria), as well as sleep phases in circadian sleep rhythm, indicated by habitual bedtime and wake time( 32 ). A total of seventy articles met the inclusion criteria. To examine the direct correlation between micronutrients and sleep patterns, articles were excluded if they met any of the following criteria: (i) the study focused on secondary sleep impairment due to comorbidities such as mood disorders, pain and treatment effects (n 3); (ii) the study investigated the relationship of micronutrient status with physiological sleep disorders, such as restless-leg syndrome or obstructive sleep apnoea (n 25); (iii) the study primarily examined the molecular or genetic pathways linking micronutrients and sleep patterns using animal models (n 9); (iv) the study was a narrative literature review, expert opinion or case study (n 9); (v) the study examined the effect of multiple treatments with micronutrient supplementation as one of the therapeutic elements (n 1).
Data extraction and analysis
Extracted data included research design, subjects (age, sex and sample size), the covariates that were adjusted for in observational studies, study site, micronutrient measurement, sleep measurement and key findings (see Tables 1 and 2). The methodological strengths and limitations of each study were also summarized in Tables 1 and 2. The research quality of each study was then further evaluated using the validity questions of the American Dietetic Association’s Quality Criteria Checklist for primary research( 33 ). Each study was classified as positive, neutral or negative according to the rating criteria of the Quality Criteria Checklist.
Table 1.
Observational studies on micronutrients and sleep patterns in human subjects
| Study | Methods | Samples/settings | Micronutrient measures | Sleep measures | Major findings | Strengths | Limitations |
|---|---|---|---|---|---|---|---|
| Luojus et al. (2015)( 43 ) | Cross-sectional study V: age, cumulative smoking history, alcohol consumption, Human Population Laboratory depression scale scores, physical activity, cardiometabolic syndrome, CVD history | Men aged 42–60 years (n 2570)/Eastern Finland | Serum Zn and Cu concentrations | Self-reported sleep duration | Sleep duration significantly associated with level of both serum Cu and hs-CRP in adjusted models. Zn no longer significantly associated with sleep duration after adjustment | 1. A large sample size 2. Biomarkers of Zn and Cu 3. Controlled for important confounders | 1. Self-reported sleep duration may lead to recall bias 2. Sleep duration was categorized into nine levels, which decreased statistical power 3. Only included men in the study, which may reduce its generalizability |
| Ji & Liu (2015)( 42 ) | Longitudinal study V: grade, sex, education level of mother and father | Followed children from 3–5 years to 11–15 years old (n 1295)/China | Serum Zn concentrations | Self-reported sleep patterns, Pittsburgh Sleep Quality Index | Cross-sectional analyses showed negative correlations of blood Zn concentrations with insufficient sleep duration, sleep disturbances and poor sleep quality in adolescence, but no association at pre-school age. Longitudinal analyses indicated that blood Zn concentrations at pre-school age predict poor sleep efficiency and poor sleep quality in adolescence | 1. Includes two-wave longitudinal data from a pre-school cohort 2. Large sample size 3. Used biomarker of Zn status | 1. Used only subjective sleep measures 2. Did not adjust for dietary nutrients, environmental influential factors |
| Massa et al. (2015)( 55 ) | Cross-sectional study V: age, clinic, season, comorbidities, BMI, physical and cognitive function | Men aged 68 years or older (n 3048)/USA | Total 25(OH)D combining 25(OH)D2 and 25(OH)D3 | Nightly total sleep time, sleep efficiency and WASO obtained using wrist actigraphy worn for an average of five consecutive 24 h periods | Low levels of total serum 25(OH)D are associated with poorer sleep including short sleep duration and lower sleep efficiency | 1. Objective sleep measures for an average of five consecutive 24 h periods 2. Used biomarkers of nutrient 3. Data were from a large cohort study | 1. Findings may not be generalizable to young men or women |
| Bertisch et al. (2014)( 20 ) | Cross-sectional study V: Model A adjusted for age, sex, race/ethnicity, examination site, waist circumference; Model B additionally adjusted for education, family income, physical activity, smoking status, alcohol intake; Model C additionally adjusted for antidepressant use, depression score, history of osteoarthritis, history of asthma, glomerular filtration rate | Adults with mean age of 68·2 years (n 1721)/USA | Serum 25(OH)D concentration | Sleep duration, efficiency and symptoms were measured by PSG, actigraphy and questionnaires | Vitamin D-deficient individuals slept shorter than sufficient individuals, with strongest associations shown in African Americans. Chinese Americans with vitamin D deficiency had higher AHI v. sufficient individuals | 1. Investigated ethnic disparity in sleep effect of vitamin D 2. Used both objective and subjective sleep measures 3. Used biomarker of nutrient 4. Rigorously controlled for multiple potential confounders | 1. Vitamin D measurement preceded the collection of sleep outcomes by average of 10·3 years 2. Did not adjust for season variation of vitamin D levels |
| Kim et al. (2014)( 54 ) | Cross-sectional study V: sex, age, cigarette smoking, alcohol consumption, self-reported daily sun exposure | Adults aged 60–80 years (n 1614)/South Korea | Serum 25(OH)D concentration | Self-reported sleep duration | Serum vitamin D level positively associated with self-reported daily sleep duration in elderly Korean individuals | 1. Used a nationally representative sample of older adults 2. Considered sun exposure as a vitamin D resource | 1. Did not adjusted for dietary intake, supplementation of vitamin D and season influence 2. Self-reported sleep duration and sun exposure may lead to recall bias |
| Beydoun et al. (2014)( 52 ) | Cross-sectional study V: age, sex, race/ethnicity, education, marital status, family income, BMI, smoking, physical activity, self-reported chronic conditions, antidepressant medication use, dietary intakes | US NHANES, 2005–2006 (aged 20–85 years, n 2459)/USA | Serum concentrations of key nutrients | Sleep questionnaire included items on sleep habits and disorders; and a subscale of the Functional Outcomes of Sleep Questionnaire | Independent inverse associations were found between serum vitamin B12 and sleep duration, between 25(OH)D and sleepiness (as well as insomnia), and between folate and sleep disturbance | 1. Used a nationally representative sample 2. Biomarkers of nutrients 3. Adjusted for important confounders | 1. Did not stratify age groups 2. Self-reported sleep may lead to recall bias |
| Shiue (2013)( 53 ) | Cross-sectional study V: sex, ethnicity, BMI, high blood pressure, active smoking, depressive symptoms | NHANES, 2005–2006 (aged 16 years or above, n 6139)/USA | Serum 25(OH)D concentrations | Self-reported sleeping hours, minutes to fall asleep and sleep complaints; sleep disorders diagnosed by doctors | No association between serum 25(OH)D concentrations and sleeping hours was observed, while a significant inverse association was found between serum 25(OH)D concentrations and minutes to fall asleep. Moreover, people with higher vitamin D levels could be more likely to complain about sleep problems, although the reason is unclear | 1. Used a nationally representative sample | 1. Did not stratify by age group 2. Did not adjust the status of other nutrients which may affect sleep patterns 3. Self-reported sleep duration and latency may lead to recall bias |
| Grandner et al. (2013)( 35 ) | Cross-sectional study V: total energy intake, total number of foods consumed, age, gender, income, education, BMI, exercise | Adults aged 18+years in NHANES 2007–2008 (n 5587)/USA | 24 h food recall | Self-reported sleep duration | After adjustment for overall diet, only decreased P, Mg, Fe, Zn and Se in the context of very short (<5 h) sleep and decreased P in the context of long sleep remained significant. Some of the effects of the vitamin for very short (<5 h) sleep remained including decreased thiamin, total folate, folic acid and folate DFE in fully adjusted analyses | 1. Sampling was performed to ensure generalizability to the US population 2. Effects of covariates were examined separately and totally | 1. Self-reported sleep duration and dietary intake may lead to recall bias 2. Did not differentiate sleep duration on weekdays and weekends |
| Song et al. (2012)( 41 ) | Cross-sectional study V: age, smoking status, occupation | Women aged 21–72 years (n 126)/South Korea | Zn, Cu and Zn:Cu in serum and hair | Self-reported questionnaire (7 d recall): average sleep hours separately on weekdays and weekends | Participants in the middle tertile of Zn and Zn:Cu ratio in serum had significantly longer sleep duration v. those in the lowest tertile. Increasing Zn:Cu in hair was associated with longer sleep hours, whereas sleep duration decreased significantly from the lowest to the highest tertile of hair Cu level | 1. Compared results from different micronutrient measures | 1. Results of the study may not generalize to men and other people 2. Self-reported sleep duration may lead to recall bias 3. Did not mention the method used to calculate mean hours of sleep based on weekday and weekend sleep hours |
| Sato-Mito et al. (2011)( 48 ) | Cross-sectional study V: current smoking status, supplement use, energy intake | Women aged 19–36 years (n 112)/Japan | Self-administered diet history questionnaire (1-month recall) | MEQ, preferred bedtime and rise time | Lower MEQ score showed significant associations with lower energy-adjusted intakes of protein, Ca, Mg, Zn, vitamins (D, riboflavin and B6) and vegetables, and with a higher intake of noodles. Furthermore, later midpoint of sleep showed significant associations with lower energy-adjusted intakes of protein, cholesterol, K, Ca, Mg, Zn, vitamins (D, riboflavin, B6 and B12), soya, fish and shellfish, and eggs, and with higher intakes of noodles, bread and confections | 1. Supplement use was addressed in data analyses | 1. Sample used may be limited in its generalizability 2. Self-reported dietary intake may lead to recall bias 3. Investigated preferred rather than actual sleep schedule 4. Did not consider known confounders such as SES, course load |
| Sato-Mito et al. (2011)( 40 ) | Cross-sectional study V: means of dietary intake, dietary behaviours (time at which meals began, eating duration, number of skipped meals, number of occasions when TV was watched during weekday meals), lifestyle variables, residential block, size of residential area and current smoking status | Female dietetics students aged 18–20 years (n 3304)/Japan | Self-administered diet history questionnaire (1-month recall) | Self-reported bedtimes and rise times on weekdays | Late midpoint of sleep was significantly negatively associated with the percentage of energy from protein and carbohydrates, and energy-adjusted intakes of cholesterol, K, Ca, Mg, Fe, Zn, vitamin A, vitamin D, thiamin, riboflavin, vitamin B6, folate, rice, vegetables, pulses, eggs, and milk and milk products | 1. Used large sample size 2. Important confounders were controlled for | 1. Sample used may be limited in its generalizability 2. Self-reported dietary intake may lead to recall bias 3. Did not consider sleep-latency-adjusted midpoint of sleep 4. Did not consider known confounders such as SES, course load 5. Investigated sleep schedule on weekdays only |
| Grandner et al. (2010)( 56 ) | Cross-sectional study V: age, income, education, total dietary amount, BMI, minutes of moderate–strenuous physical activity | Postmenopausal women (n 459)/USA | FFQ (3-month recall) | Objective sleep: 1 week of actigraphy. Subjective sleep: sleep diary | Later sleep acrophase, an indicator of sleep timing, was associated with more dietary vitamin D | 1. Used large sample size 2. Incorporated subjective and objective sleep measurement | 1. Sample used may be limited in its generalizability 2. Self-reported dietary intake may lead to recall bias 3. Did not differentiate weekdays from weekends for sleep schedule |
| Kordas et al. (2008)( 34 ) | Cross-sectional study V: age, sex, SES, breast-feeding, caste, malarial parasite count, Trichuris egg densities, illness in previous week, walking unassisted | Infants aged 6–18 months: Study 1 (n 174)/Pemban and Zanzibar Study 2 (n 770)/Pemban and Zanzibar Study 3 (n 326)/Nepal | Hb, serum Zn protoporphyrin | Sleep questionnaire (parental report) | IDA infants were associated with shorter night-time sleep duration and higher frequency of night waking | 1. Used large sample size. 2. Used biomarkers of micronutrient status 3. Compared results across three places | 1. Parental reports/recall may lead to measurement bias 2. Did not mention if infants with medication were excluded 3. Adjusted for different covariates in the studies, which inhibited the precision of the comparison across studies |
| Kordas et al. (2007)( 39 ) | Cross-sectional study V: anxiety, bedroom sharing, who decides when to get up and go to bed, age, sex, crowding in the home | Children aged 6–8 years (n 550)/Mexico | Serum Zn, SF, Hb | Sleep questionnaire (parental report) | Children with anaemia tended to have an earlier bedtime and be less likely to have long sleep-onset latency. Low SF was related to longer sleep-onset latency. Zn deficiency was not related to sleep, behaviour or activity | 1. Used large sample size 2. Used biomarkers of micronutrient status | 1. Parental recall may lead to measurement bias 2. Did not differentiate weekdays from weekends for sleep schedule 3. Did not classify the type of anaemia |
| Peirano et al. (2007)( 36 ) | Cross-sectional study V: age, gender, birth weight, weight-for-age Z-score, mother’s IQ | Otherwise healthy 6-month-old infants with IDA (n 26) and non-anaemic control infants (n 18)/Chile | Hb, SF | Sleep PSG (EEG activity) | IDA infants differed from control group by having sleep spindles with reduced density, lower frequency and longer inter-spindle intervals in NREM sleep stage 2 and SWS | 1. Used objective sleep measurement | 1. Did not evaluate the precise location of spindle waves which reflect different developmental paths 2. Did not tease apart the pharmacological effects |
| Peirano et al. (2007)( 37 ) | Longitudinal cohort study Exposure: IDA in infancy V: age, sex | Healthy 4-year-old children (n 55; former IDA, n 27, non-anaemic controls, n 28)/Chile | IDA in infancy | Sleep PSG (EEG activity) | Relative to controls, former IDA children showed: (i) longer duration of REM sleep episodes in the first third and shorter in the last third; (ii) more REM sleep episodes in the first third and fewer in the second third; and (iii) shorter latency to the first REM sleep episode and shorter NREM stage 2 and SWS episodes within the first sleep cycle | 1. Time–order relationship was generally clear 2. Used objective sleep measurement | 1. Only recorded a single night’s sleep in the laboratory 2. Did not assess daytime naps and could not determine whether disrupted night-time sleep was caused by a long daytime nap 3. Did not consider current Fe status |
| Lichstein et al. (2007)( 57 ) | Cross-sectional study V: age, ethnicity, sex | People ranging in age from 20 to 98 years (n 72)/USA | Self-reported vitamin use (1-month recall) | Sleep diaries and sleep questionnaires | For those individuals taking a multivitamin or multiple single vitamins, sleep diaries revealed poorer sleep v. non-vitamin users in the number and duration of awakenings during the night. After controlling for age, ethnicity and sex, the difference in the number of awakenings was still marginally significant | 1. Used large sample size | 1. Self-reported vitamin intake may lead to recall bias 2. Sleep diary may be not reliable 3. Did not stratify the type of vitamin use 4. Did not collect data on herbal supplements |
| Black et al. (2006)( 45 ) | Longitudinal cohort study Exposure: antenatal MgSO4 supplement V: N/A | Preterm infants (n 134): MgSO4 only (n 5) Steroids only (n 46) MgSO4 + steroids (n 45) Non-treatment (n 38)/USA | MgSO4 supplement | Sleep EEG | Infants exposed to MgSO4 had more active sleep without REM. MgSO4-only group had higher quiet sleep regularity scores and fewer state changes | 1. Time–order relationship was generally clear 2. Used objective sleep measurement | 1. Did not mention if confounders were controlled for in regression models 2. Dose or duration of MgSO4 treatment was not adjusted for 3. Sampling issues may limit the generalizability of these findings 4. Size of the MgSO4 only group is small |
| Dralle & Bodeker (1980)( 44 ) | Cross-sectional studyV: N/A | Full-term newborn infants between the 5th and 15th days of life (n 14)/Germany | Serum Mg | Sleep EEG, EMG from chin muscles, EOG and ECG | With increasing serum Mg, quiet sleep increased, whereas active sleep decreased | 1. Used objective sleep and micronutrient measures | 1. Used small sample size 2. Mg treatment was not controlled for in regression models |
V, variables adjusted for; TV, television; SES, socio-economic status; IQ, intelligence quotient; IDA, Fe-deficiency anaemia; N/A, not applicable; NHANES, National Health and Nutrition Examination Survey; 25(OH)D, 25-hydroxyvitamin D; 25(OH)D2, 25-hydroxyergocalciferol; 25(OH)D3, 25-hydroxycholecalciferol; SF, serum ferritin; WASO, wake time after sleep onset; PSG, polysomnography; MEQ, Morningness–Eveningness Questionnaire; EEG, electroencephalography; EOG, electro-oculogram; ECG, electrocardiography; hs-CRP, high-sensitivity C-reactive protein; AHI, apnaea–hypopnoea index; DFE, dietary folate equivalents; NREM, non-rapid eye movement; SWS, slow-wave sleep; REM, rapid eye movement.
Table 2.
Clinical trials on micronutrients and sleep patterns in human subjects
| Study | Methods | Samples/settings | Sleep measurement | Major findings | Strengths | Limitations |
|---|---|---|---|---|---|---|
| Kordas et al. (2009)( 25 ) | RCT with 2×2 factorial designG1: 12·5 mg elemental Fe + 50 µg FA for 12 monthsG2: 10 mg ZnG3: Fe–FA and ZnG4: placebo | Study 1: Pemban and Zanzibar infants (n 877)Study 2: Nepali infants (n 567) | Maternal reports of sleep patterns (napping frequency and duration, night-time sleep duration, frequency of night waking) | Serum Zn levels and Zn:Cu were lowest in those with ≤6 h sleep. Serum Cu levels were highest in those with ≥10 h sleep. Supplemental Fe was consistently associated with longer night-time and total sleep duration. There was also a positive main effect of Zn on total sleep duration | 1. Used large sample size and multiple study sites | 1. Maternal recall may lead to bias 2. It is also possible that micronutrient treatment increased daytime activity (reduced lethargy), in which case infants would be tired and require longer sleep 3. Side-effects were not assessed |
| Held et al. (2002)( 46 ) | RCT with crossover designTwo Mg2+ treatment intervals of 20 d duration separated by 2 weeks washout | Elderly subjects aged 60–80 years (n 12)/Germany | Sleep EEG | Mg2+ led to a significant increase in SWS delta power and sigma power | 1. Used objective sleep measures | 1. Used small sample size 2. Long-term effect was not assessed |
| Honma et al. (1992)( 24 ) | RCT with a crossover designVitamin B12 supplement was taken for 4 weeks | Healthy male subjects aged 20–28 years (n 9)/Japan | Sleep log, serum melatonin | No significant differences were observed between groups in the timing and duration of sleep | 1. RCT design allows for examination of causal effect 2. Explored the mediators of vitamin B12 and sleep | 1. Sample size is small 2. Side-effects were not assessed 3. Sleep log may not reveal the real sleep–wake cycle |
| Okawa et al. (1997)( 49 ) | RCTMethylcobalamin (3 mg/d) or placebo was administered for 4 weeks | Patients with DSPS aged 13–55 years (n 50; methylcobalamin group, n 27; control group, n 23)/Japan | Sleep log | No significant differences were observed between the two groups in drowsiness during daytime or night-time sleep duration | 1. RCT design allows for examination of causal effect | 1. Sleep duration from sleep log may be biased due to the lack of information on sleep latency 2. Side-effects were not assessed |
| Takahashi et al. (1999)( 50 ) | RCTMethylcobalamin (6 mg/d) or control (0·03 mg/d) for 8 weeks | Patient with DSPS, age N/A (methylcobalamin group, n 21; control group, n 27)/Japan | Sleep diary and questionnaire | Significant improvement of parameters of the sleep–wake cycle was observed in test group v. control group at end of the 4th week but not the 8th week of administration | 1. Examined the dose effect of vitamin B12 | 1. Sleep diary may not reveal the real sleep–wake cycle 2. Did not design a placebo group 3. Did not compare the baselines |
| Mayer et al. (1996)( 51 ) | Pre-test/post-test designG1: 3 mg cyanocobalamin (CB12) treatment for 14dG2: methylcobalamin (MB12) treatment for 14d | Healthy adults, mean age 35·17 years for women, 37·2 years for men) (CB12, n 9; MB12, n 10)/Germany | Wrist actigraph | Only MB12 had a positive psychotropic alerting effect with a distribution of the sleep–wake cycle towards sleep reduction | 1. Compared the effects of different forms of vitamin B12 | 1. Did not design a placebo group 2. The ceiling effect may exist due to the optimal pre-treatment scores in many participants 3. The comparison between groups was questioned due to the unequal baselines |
| Drennan et al. (1991)( 47 ) | RCT with a crossover design1 week of oral KCl supplements (96 meq/d) v. 1 week of identical placebo capsules | Healthy male volunteers aged 18–33 years (n 9)/USA | Sleep log and wrist actigraphy | K supplementation significantly delayed sleep-log-identified bedtime. K reduced sleeping interval for both sleep-log and wrist-actigraph data. K significantly increased actigraphic sleep efficiency due to a reduction in actigraphic WASO. No effect of K on actigraphic sleep phase was observed | 1. Compared findings from subjective and objective sleep measures 2. Side-effects were assessed | 1. Sample size is small 2. Experimental period is short (2 weeks) and long-term effects were not assessed |
RCT, randomized controlled trial; G, group; FA, folic acid; DSPS, delayed sleep phase syndrome; N/A, not available; EEG, electroencephalography; SWS, slow-wave sleep; WASO, wake after sleep onset.
Results
A final sample of twenty-six articles assessing the association between micronutrients and sleep was identified for review, including nineteen observational studies (Table 1) and seven clinical trials (Table 2). The reviewed articles covered a range of non-institutionalized samples from infants to older adults across several different countries. However, adolescents, who may experience significant developmental sleep alteration and metabolic changes, were rarely reported in the articles reviewed. Micronutrients studied in the existing literature included Fe, Zn, Cu and Mg, as well as vitamins D and B12. Studies with an observational design measured micronutrient status by 24 h dietary recall (one day only; n 1), generic FFQ (n 3), micronutrient intake recall (n 2) or laboratory indices of serum/hair concentrations (n 13). The seven clinical trials specifically examined the sleep effect of dietary supplements with various treatment periods, from 1 week to 12 months. The body of literature on sleep pattern variables associated with micronutrients is broadly categorized into sleep stage, sleep duration, sleep-onset latency, waking after sleep onset and circadian rhythm of sleep. Along with retrospective questionnaires and prospective sleep logs, objective measurements of actigraphy and polysomnography have been used to collect sleep data. Table 3 shows the scientific validity of each study.
Table 3.
Research validity assessment using the American Dietetic Association’s Quality Criteria Checklist( 33 )
| Study | 1. Clear research question | 2. Participant selection free of bias | 3. Comparable study groups* | 4. Withdrawals or response rate described | 5. Use of blinding | 6. Intervention protocol and/or data collection procedure described in detail | 7. Outcomes clearly defined and the measurements valid and reliable | 8. Appropriate statistical analysis | 9. Conclusion supported by results | 10. Unlikely funding bias | Overall quality rating† |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Observational studies | |||||||||||
| Luojus et al. (2015)( 43 ) | Y | Y | Y | N | Unclear | Y | Y | Y | Y | Y | + |
| Ji & Liu (2015)( 42 ) | Y | Y | Y | Y | Unclear | Y | Y | Y | Y | Y | + |
| Massa et al. (2015)( 55 ) | Y | Y | Y | Y | Unclear | Y | Y | Y | Y | Y | + |
| Bertisch et al. (2014)( 20 ) | Y | Y | Y | Y | Unclear | Y | Y | Y | Y | Y | + |
| Kim et al. (2014)( 54 ) | Y | Y | Y | N | Unclear | Y | Y | Y | Y | Y | + |
| Beydoun et al. (2014)( 52 ) | Y | Y | Y | Y | Unclear | Y | Y | Y | Y | Y | + |
| Shiue (2013)( 53 ) | Y | Y | Y | N | Unclear | N | Unclear | Y | Y | Unclear | Ø |
| Grandner et al. (2013)( 35 ) | Y | Y | Y | N | Unclear | Y | Y | Y | Y | Y | + |
| Song et al. (2012)( 41 ) | Y | Unclear | Y | N | Unclear | Y | Y | Y | Y | Y | Ø |
| Sato-Mito et al. (2011)( 48 ) | Y | Unclear | Unclear | N | Unclear | Y | Y | Y | Y | Y | Ø |
| Sato-Mito et al. (2011)( 40 ) | Y | Y | Y | Y | Unclear | Y | Y | Y | Y | Y | + |
| Grandner et al. (2010)( 56 ) | Y | Y | Y | N | Unclear | Y | Y | Y | Y | Unclear | + |
| Kordas et al. (2008)( 34 ) | Y | Y | Y | Y | Unclear | Y | Y | Y | Y | Unclear | + |
| Kordas et al. (2007)( 39 ) | Y | Y | Y | Y | Unclear | Y | Y | Y | Y | Unclear | + |
| Peirano et al. (2007)( 36 ) | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | + |
| Peirano et al. (2007)( 37 ) | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | + |
| Lichstein et al. (2007)( 57 ) | Y | Y | Y | Y | Unclear | Y | Y | Y | Y | Y | + |
| Black et al. (2006)( 45 ) | Y | Y | Y | N | Unclear | Y | Y | Y | Y | Unclear | + |
| Dralle & Bodeker (1980)( 44 ) | Y | Unclear | Unclear | N | Unclear | Y | Y | Y | Y | Unclear | Ø |
| Clinical trials | |||||||||||
| Kordas et al. (2009)( 25 ) | Y | Y | Y | N | Unclear | Y | Y | Y | Y | Y | + |
| Held et al. (2002)( 46 ) | Y | Unclear | Y | Y | Unclear | Y | Y | Y | Y | Unclear | |
| Honma et al. (1992)( 24 ) | Y | N | Y | Y | Unclear | Y | Y | Y | Y | Unclear | Ø |
| Okawa et al. (1997)( 49 ) | Y | Y | Y | Y | Y | Y | Y | Y | Y | Unclear | + |
| Takahashi et al. (1999)( 50 ) | Y | Y | N | N | Y | Y | Y | Y | Y | Unclear | Ø |
| Mayer et al. (1996)( 51 ) | Y | Unclear | N | N | Unclear | Y | Y | Y | Y | Unclear | Ø |
| Drennan et al. (1991)( 47 ) | Y | N | Y | N | Unclear | Y | Y | Y | Y | Unclear | Ø |
Y, yes; N, no; unclear, not clearly reported.
Randomized controlled trials, baseline comparison between groups; observational studies: were pre-existing differences accounted for by using appropriate adjustments?
Positive (+): if most (six or more) of the answers to the above validity questions are ‘Yes’ (including criteria 2, 3, 6 and 7), the report should be designated with a plus symbol (+) on the Evidence Worksheet. Neutral (Ø): if the answers to validity criteria questions 2, 3, 6 and 7 are ‘Yes’ but several other criteria indicate study weaknesses, the report should be designated with a neutral (Ø) symbol on the Evidence Worksheet. Negative (–): if most (six or more) of the answers to the above validity questions are ‘No’, the report should be designated with a minus (–) symbol on the Evidence Worksheet.
Trace elements and sleep patterns
Fe
The association between Fe and sleep duration has been consistently reported in infants and the general adult population. Based on results from a cross-sectional study and a clinical trial, iron-deficiency anaemia (IDA) may be associated with more night waking and shorter total sleep duration compared with better-nourished infants( 34 ), whereas Fe supplementation can decrease the length of daytime naps among IDA infants, and increase night-time and total sleep duration in infants regardless of their IDA status at baseline( 25 ). A recent observational study extended such associations to adults, showing an association between decreased Fe intake and very short sleep (<5 h) after controlling for overall diet( 35 ). Fe deficiency is also associated with altered characteristics of sleep stages. Compared with non-IDA infants, IDA infants showed more awake times, shorter quiet-sleep duration and delayed sleep-spindle patterns in NREM sleep at night( 36 ). Such alterations in the temporal organization of sleep architecture may be long lasting. A longitudinal study followed up children with and without IDA in infancy, indicating that former IDA infants exhibited altered distribution of NREM and REM sleep at 4 years old relative to the non-IDA controls( 37 ).
Zn and Cu
Although the association between Zn and sleep phase in circadian rhythm has been suggested in several studies( 38 , 39 ), no consensus has been reached on this effect. In a sample of children aged 6–8 years, researchers found no significant association between low serum Zn and bedtime or wake-up time( 39 , 40 ). In contrast, the study by Sato-Mito et al., which classified participants into quintiles (Q) by the midpoint of sleep (Q1/earliest=2:32am, Q2 =3:10 am, Q3=3:37 am, Q4=4:11 am, Q5/latest=5:31 am), reported a significant reduction of energy-adjusted Zn intake in women who had the latest midpoint of sleep( 40 ).
With regard to sleep duration, five studies provided evidence to support the association of Zn and Cu with sleep duration among different populations. The randomized controlled trials, using maternal reports of sleep patterns, found longer night-time and total sleep duration in infants who received supplemental Zn than in the placebo group( 25 ). This finding agrees with an observational study that found an association between decreased Zn and very short sleep in a general adult population( 35 ). In terms of nutritional biomarkers, researchers found that shorter sleep duration or increased odds of sleep insufficiency were associated with lower serum Zn levels in women( 41 ) and children in early adolescence( 42 ). Cu levels showed mixed effects in prior research. Whereas researchers reported a negative relationship between hair Cu levels and sleep duration in 126 women aged 21–72 years( 41 ), a study of 2570 men aged 42–60 years showed highest average levels of serum Cu in the group with the longest sleep duration( 43 ).
Minerals and sleep patterns
Mg
The involvement of Mg in sleep patterns has been investigated in infants and older adults. Researchers found that increased serum Mg was associated with increased quiet sleep and decreased active sleep in full-term infants( 44 ). In a longitudinal study, Black et al.( 45 ) reported that preterm infants whose mothers received prenatal MgSO4 treatment (whether or not they also received steroids) had more active sleep without REM, whereas the MgSO4-only group showed higher quiet-sleep regularity and fewer state changes. In older adults, a clinical trial also suggested that oral Mg supplementation may increase SWS delta power and sigma power measured by polysomnography( 46 ).
K
Using sleep log and actigraph data, the randomized controlled trial by Drennan et al.( 47 ) reported reduced sleep duration and wakefulness after sleep onset in young males following K supplements compared with controls. These researchers also identified a later bedtime after K supplementation, which is contrary to an observational study on female students aged 18–20 years that found a negative association between the midpoint of sleep and dietary K intake( 48 ).
Vitamins and sleep patterns
Vitamin B12
The results showed mixed effects of vitamin B12 on sleep patterns. No significant or definitive effect of vitamin B12 on sleep phase and sleep duration at night was reported in early human studies( 24 , 49 , 50 ), except the clinical trial by Mayer et al.( 51 ) that reported an alerting effect of vitamin B12 supplementation with a decrease in sleep duration. A recent study consistently found an independent inverse relationship between serum vitamin B12 concentrations and sleep duration in adults( 52 ). Additionally, one study investigated the relationship between vitamin B12 and sleep timing, measured as the midpoint of sleep. That study showed that young women with lower intakes of vitamin B12 were more likely to have a later sleep period( 48 ).
Vitamin D
Several studies have indicated a potential protective effect of vitamin D on sleep. Analyses of data from the National Health and Nutrition Examination Surveys (NHANES) 2005–2006 and found inverse correlations of serum vitamin D with sleep latency (minutes to fall asleep)( 53 ) and daytime sleepiness( 52 ), but not sleep duration( 53 ), in adults. While these relationships were found from heterogeneous populations including both young adults and older adults, studies specific to community-dwelling older adults reported a positive association between vitamin D levels in serum and sleep duration( 20 , 54 , 55 ). Current studies also examined the link between vitamin D and sleep phase but showed inconsistent findings. In a study on postmenopausal women, participants with higher intake of dietary vitamin D showed a later sleep acrophase (which refers to the peak of a fitted 24 h cosine wave that was an indicator of sleep timing measured by actigraphy; this is an indicator of mathematically modelled curve peak)( 56 ). In contrast, an inverse relationship was reported in another study conducted with female students aged 18–20 years in Japan( 40 ).
Possible interactions of micronutrients on sleep patterns
While the main effect of each micronutrient on sleep patterns has been reported in current research, such sleep effect may change depending on the level of another micronutrient, suggesting an interaction among micronutrients. For example, although Fe and Zn supplements alone reduced the length of naps as well as increased the duration of night-time sleep and total sleep in infants, infants receiving Fe together with Zn supplements did not exhibit such sleep effect( 25 ). Zn:Cu in serum and hair also significantly predicted sleep duration in women, with longer sleep duration associated with a medium tertile of Zn:Cu in serum or a high tertile of Zn:Cu in hair( 41 ). In combining effects of vitamins, researchers of a cross-sectional study reported negative effects from a multivitamin or multiple single-vitamin use on sleep patterns in the number and duration of night-time awakenings compared with non-vitamin users( 57 ). Considering the significant effects of vitamins mentioned, this finding suggested possible antagonistic effects between vitamins on sleep outcomes.
Discussion
Sleep stages in relation to micronutrient status
The reviewed studies consistently supported the hypothesis that micronutrient levels, particularly Fe and Mg, can predict the organization of sleep stages. However, researchers should interpret these findings from a developmental perspective for sleep patterns across the life span. Two distinct sleep states are defined on the basis of polysomnography: REM and NREM sleep, which are called active sleep and quiet sleep in infants, respectively( 1 ). Given that one of the main alterations in infant sleep is the transition from predominantly active sleep to increased quiet sleep by about 4 months of age( 36 ), decreased quiet sleep and delayed spindle patterns in NREM sleep from IDA( 36 ) indicate that Fe may be essential for the normal development of quiet sleep/NREM sleep in infants.
Prenatal exposure to Mg in preterm infants( 45 ) and postnatal serum Mg concentrations in full-term infants( 44 ) have consistently been associated with an increase in the duration of quiet sleep, suggesting a potentiating role of Mg in the maturity of quiet sleep during infancy. In contrast, preterm birth with prenatal exposure to MgSO4 was also associated with more active sleep without REM( 45 ). REM sleep in infants has been linked to the development of the neuromuscular and sensory system, as well as brain function( 58 ). As the amount of active sleep without REM often decreases over the preterm period( 59 ), increased active sleep without REM suggests delayed development of active sleep and a possible influence on brain development, thus raising a concern over Mg treatment for pregnant women and infants. The effects of Mg on infant sleep need to be interpreted cautiously due to the coexistence of acceleration in the development of quiet sleep and a delay in the maturity of active sleep.
The benefit of Mg supplements on increased SWS in the elderly is of particular interest. Whereas the most prominent alterations in elderly sleep are known to be reductions of SWS, REM sleep and sleep efficiency( 1 ), Mg may have beneficial effects on sleep patterns due to its action on reversing age-related sleep changes. Additionally, given that the delta power of SWS in electroencephalography reflects the restorative property of sleep( 60 ), Mg may improve the physiological function of sleep in older adults, which warrants future research on the clinical application of Mg supplementation for older adults.
Sleep duration in relation to micronutrient status
Most trace elements and minerals in the present review correlated significantly with sleep duration in different populations, despite the discrepancy in the direction of these relationships across micronutrients. Specifically, Fe, Zn and Mg may positively associate with sleep duration, whereas the relationship of sleep duration is inverse to the level of hair Cu, as well as K and vitamin B12 supplements. The relationship between vitamin D and sleep duration is controversial. Considering the negative correlation between the number of waking episodes and sleep duration at night( 34 ), together with associated sleep-onset latency( 39 ), the effect of Fe, Zn and Mg on sleep duration might be moderated or mediated by the number of awakenings after sleep onset and sleep latency at night. This hypothesis may not be supported by the study on K due to the coexistence of reduced sleep duration and wakefulness after sleep onset( 47 ). However, delayed sleep time reported by sleep logs in that study could explain such paradoxical findings.
Although micronutrient status could be a modifiable factor to improve sleep duration, micronutrient levels may not show a linear association with sleep, with the longest sleep duration found in the middle tertile level of Zn and Cu in women( 41 ). This finding, together with evidence that both short- and long-sleep duration have been documented to increase all-cause mortality (cardiovascular-related, cancer-related and all)( 14 ), indicates that optimal rather than high or low micronutrient levels are essential for healthy sleep.
Sleep phase in relation to micronutrient status
The published literature supported the presence of an association between sleep phase and micronutrient variables of Zn, K and vitamin D. However, the limited evidence and lack of consensus on such associations preclude the conclusion of causal links or concrete clinical recommendations. The different results could be attributed to the large night-to-night variation of the indicators for sleep phase: sleeping time and wake-up time. Sleep habits in human subjects vary greatly between weekdays and weekends( 61 ), and human chronotype is known to correlate better with the midpoint of sleep on free days than on work days in a non-experimental environment( 62 ). However, studies in the current review did not differentiate weekdays from weekends for bedtime and wake-up time, thus leading to substantial measurement error and biased findings.
The inconsistent results of micronutrients and sleep phase may also result from the variability of micronutrient and sleep measurements. Dietary intake may be positively associated with biological micronutrient levels in red blood cells and serum( 25 , 51 , 63 ). However, metabolic characteristics enable some micronutrients, such as vitamin B12, to maintain a normal range under a short period of dietary deficiency( 31 ), suggesting a possible discrepancy between dietary intake and biological levels of micronutrients. Similarly, sleep data were collected by different questionnaires, and thus it is possible that inconsistent patterns of statistical significance reflect different psychometrical properties rather than true differences in the associations. Besides, subjective sleep measurements do not highly correlate with estimates based on physiological measures( 64 ) and may lead to different results as compared with objective measurements. Therefore, standardized objective measures of micronutrient status and sleep should be incorporated into future studies.
Neurobiological mechanisms of current findings
Although the possible neurobiological mechanisms underlying the main effects of micronutrients on sleep patterns are not fully understood, researchers have suggested a number of causal pathways linking micronutrients with sleep in experimental studies. For example, micronutrients may be essential in the synthesis and transportation of neurotransmitters that are related to sleep homeostasis. Whereas Fe, Zn, Cu and Mg may be associated with antagonists of excitatory transmissions, including the NDMA receptor( 65 , 66 ) and dopaminergic neurons( 67 , 68 ), micronutrients can also potentiate inhibitory transmissions, such as γ-aminobutyric acid (GABAA) receptors( 69 , 70 ). In addition to the neurobiological pathways, researchers have documented that retinoic acid, a metabolite of vitamin A, significantly up-regulates the expression of clock/bmal (circadian locomotor output cycles kaput/brain and muscle arylhydrocarbon receptor nuclear translator)-dependent circadian genes, thus modulating the circadian-sleep regulatory process and affecting sleep phase, sleep duration, as well as the organization of sleep stages( 71 ). The mechanisms underlying the association between micronutrients and sleep regulation warrant future examination of the effect of micronutrient supplementation on sleep patterns.
The long-term effect of suboptimal levels of micronutrients, such as Fe deficiency, may be due to an irreversible impact on the brain. Several studies on rats have shown that Fe deficiency causes disturbances and damage to brain Fe distribution and sleep-related neurotransmitter systems, and such disturbances could not be completely normalized by Fe replenishment( 72 ). Current literature has also supported the interactions between micronutrients on sleep patterns, which possibly result from the antagonism between micronutrients in either metabolic absorption or the binding to receptors of neurotransmitters( 73 , 74 ). Specifically, a high intake of Zn may interfere with absorption of Fe and Cu( 73 ). Additionally, under physiological conditions, Zn ion would liberate Cu ion from the GABAA receptor and inhibit the effect of Cu on sleep regulation( 74 ). These interactions have made it hard to disentangle the direct effect of a single micronutrient on sleep outcomes from current findings.
Implications for future nutrition–sleep research
The results from the current review have important implications for future research. Due to the possibility of concentration-dependent effect and intertwined actions of micronutrients, further studies demonstrating the nature of the effects of micronutrient levels on sleep are warranted. In terms of studied populations, whereas articles involving human subjects have primarily focused on infants, young children, general adults, postmenopausal women and older adults, very few studies have specifically investigated children in adolescence when substantial developmental changes in sleep pattern occur. Additionally, many of the current studies were heterogeneous in age, including all young, middle-aged and older adults( 35 , 52 ). Given that the metabolic characteristics of micronutrients and the biological regulation of sleep may vary across the life span, researchers should take into account the developmental effect when interpreting results.
More than half of the human studies are observational studies and the degree of control for confounders varies across studies. Confounders that were typically adjusted for included age, sex, education, family income, BMI, energy intake, smoking status and race/ethnicity. There are only four studies involving covariates of depressive symptoms or antidepressant use( 20 , 43 , 52 , 53 ). Future research should take into account important covariates, such as a medical history of psychiatric disorder or medication usage known to affect micronutrient absorption or sleep, to uncover the nature of the associations. Furthermore, a majority of reviewed studies were cross-sectional or focused on the short-term effects of micronutrient supplements. Research with a longitudinal design is needed to investigate how micronutrient status early in life predicts later sleep patterns and how the trajectory of micronutrient profile over the parts of the life span are associated with age-related changes in sleep patterns.
Implications for public health practice
Both micronutrient deficiency and poor sleep are significant public health issues worldwide. Although the clinical relevance of micronutrients on sleep patterns needs further examination, health-care providers, particularly those practising in primary-care settings, should take into account several findings from the current literature in health-care practice for individuals and communities. First, health-care providers should be attentive about micronutrient levels in infants due to the irreversible influence on brain function and sleep organization, Fe status in particular. Second, when using Mg in prenatal settings, particular attention should be given to mixed effects on the development of active sleep and quiet sleep in infants. However, Mg may be beneficial for elderly sleep and brain function. Third, despite the indefinite recommendation of optimal doses at this moment, it is important to note that optimal intake rather than high or low intake of micronutrients is needed to maintain normal sleep patterns.
Limitations of the current review
The current review has several potential limitations. First, only articles focusing on a direct relationship between micronutrient variables and sleep pattern variables are included. Studies on physiological sleep disorders such as restless-leg syndrome and obstructive sleep apnoea, and health complaints such as pain, which were not reviewed here, may uncover other missed relationships between micronutrients and sleep patterns. Second, the review did not stratify findings by gender, race and cultural context due to the unavailability of relevant data, and thus it cannot disentangle the interplays between social factors and micronutrients on sleep patterns.
Conclusion
Although no definite clinical recommendations can be made at this point due to the limited evidence, current studies have linked trace elements, minerals and vitamins to sleep patterns in human subjects. In the articles reviewed, researchers have observed a beneficial effect of adequate serum Fe on the development of sleep stages in infants, and of Mg supplements on inhibiting age-related sleep changes in older adults. Published literature also supported an association between sleep duration and micronutrients, with sleep duration positively associated with Fe, Zn and Mg, and negatively associated with Cu, K and vitamin B12. However, the results of the associations between micronutrients and sleep phase were insufficient and inconsistent. Future research is needed to investigate the concentration-dependent as well as the longitudinal relationships between micronutrient levels and human sleep across populations, test the interactions among micronutrients on sleep outcomes, and ultimately examine the clinical relevance of micronutrients on sleep health.
Acknowledgements
Acknowledgements: The authors would like to thank Drs Maureen George, Jinyoung Kim and Tanja Kral for their helpful comments on the initial draft of this paper. Financial support: This study was funded by the Office of Nursing Research grant award issued by the School of Nursing, University of Pennsylvania. The funder had no role in the design, analysis or writing of this article. Conflict of interest: None of the authors declare any conflict of interest that may be relevant to the materials presented in this paper. Authorship: X.J. developed the idea for the study, performed the systematic searches and the article retrieval, analysed the data, and wrote and revised the article. J.L. mentored the review process, including conceptualizing the research question, the literature search and the interpretation of results, and critically revised the article. M.A.G. contributed to the conceptualization of the research question, the initial outline of the manuscript and article revision. Ethics of human subject participation: Not applicable.
References
- 1. Amlaner CJ & Fuller PM (2009) Basics of Sleep Guide, 2nd ed. Westchester, IL: Sleep Research Society. [Google Scholar]
- 2. Cho YW, Shin WC, Yun CH et al. (2009) Epidemiology of insomnia in Korean adults: prevalence and associated factors. J Clin Neurol 5, 20–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hossain JL & Shapiro CM (2002) The prevalence, cost implications, and management of sleep disorders: an overview. Sleep Breath 6, 85–102. [DOI] [PubMed] [Google Scholar]
- 4. Minowa M, Okawa M & Uchiyama M (2000) Prevalence of sleep disturbance and hypnotic medication use in relation to sociodemographic factors in the general Japanese adult population. J Epidemiol 10, 79–86. [DOI] [PubMed] [Google Scholar]
- 5. Sutton DA, Moldofsky H & Badley EM (2001) Insomnia and health problems in Canadians. Sleep 24, 665–670. [DOI] [PubMed] [Google Scholar]
- 6. Wong WS & Fielding R (2011) Prevalence of insomnia among Chinese adults in Hong Kong: a population-based study. J Sleep Res 20, 117–126. [DOI] [PubMed] [Google Scholar]
- 7. Liu J, Zhou G, Wang Y et al. (2012) Sleep problems, fatigue, and cognitive performance in Chinese kindergarten children. J Pediatr 161, 520.e2–525.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dinges D & Baynard RN (2005) Chronic sleep deprivation. In Principles and Practice of Sleep Medicine, 4th ed., pp. 67–76 [MH Kryger, T Roth and WC Dement, editors]. Philadelphia, PA: Elsevier/Saunders. [Google Scholar]
- 9. Riemann D, Berger M & Voderholzer U (2001) Sleep and depression – results from psychobiological studies: an overview. Biol Psychol 57, 67–103. [DOI] [PubMed] [Google Scholar]
- 10. Liu J, Zhang A & Li L (2012) Sleep duration and overweight/obesity in children: review and implications for pediatric nursing. J Spec Pediatr Nurs 17, 193–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vgontzas AN, Liao D, Pejovic S et al. (2009) Insomnia with objective short sleep duration is associated with type 2 diabetes: a population-based study. Diabetes Care 32, 1980–1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cappuccio FP, Cooper D, D’Elia L et al. (2011) Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J 32, 1484–1492. [DOI] [PubMed] [Google Scholar]
- 13. Qin Y, Zhou Y, Zhang X et al. (2014) Sleep duration and breast cancer risk: a meta-analysis of observational studies. Int J Cancer 134, 1166–1173. [DOI] [PubMed] [Google Scholar]
- 14. Gallicchio L & Kalesan B (2009) Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res 18, 148–158. [DOI] [PubMed] [Google Scholar]
- 15. Canuto R, Pattussi MP, Macagnan JBA et al. (2014) Sleep deprivation and obesity in shift workers in southern Brazil. Public Health Nutr 17, 2619–2623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Spiegel K, Tasali E, Penev P et al. (2004) Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med 141, 846–850. [DOI] [PubMed] [Google Scholar]
- 17. Burt J, Dube L, Thibault L et al. (2014) Sleep and eating in childhood: a potential behavioral mechanism underlying the relationship between poor sleep and obesity. Sleep Med 15, 71–75. [DOI] [PubMed] [Google Scholar]
- 18. Afaghi A, O’Connor H & Chow CM (2008) Acute effects of the very low carbohydrate diet on sleep indices. Nutr Neurosci 11, 146–154. [DOI] [PubMed] [Google Scholar]
- 19. Grandner MA, Jackson N, Gerstner JR et al. (2014) Sleep symptoms associated with intake of specific dietary nutrients. J Sleep Res 23, 22–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bertisch S, Sillau S, de Boer I et al. (2014) 25-Hydroxyvitamin D concentration and sleep duration and continuity: Multi-Ethnic Study of Atherosclerosis. Sleep 38, 1305–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Peuhkuri K, Sihvola N & Korpela R (2012) Diet promotes sleep duration and quality. Nutr Res 32, 309–319. [DOI] [PubMed] [Google Scholar]
- 22. Ursin R (2002) Serotonin and sleep. Sleep Med Rev 6, 55–67. [DOI] [PubMed] [Google Scholar]
- 23. Sowa-Kućma M, Legutko B, Szewczyk B et al. (2008) Antidepressant-like activity of zinc: further behavioral and molecular evidence. J Neural Transm 115, 1621–1628. [DOI] [PubMed] [Google Scholar]
- 24. Honma K, Kohsaka M, Fukuda N et al. (1992) Effects of vitamin B12 on plasma melatonin rhythm in humans: increased light sensitivity phase-advances the circadian clock? Experientia 48, 716–720. [DOI] [PubMed] [Google Scholar]
- 25. Kordas K, Siegel EH, Olney DK et al. (2009) The effects of iron and/or zinc supplementation on maternal reports of sleep in infants from Nepal and Zanzibar. J Dev Behav Pediatr 30, 131–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Diaz J, De las Cagigas A & Rodriguez R (2003) Micronutrient deficiencies in developing and affluent countries. Eur J Clin Nutr 57, Suppl. 1, S70–S72. [DOI] [PubMed] [Google Scholar]
- 27. Liu J, Ai Y-X, Hanlon A et al. (2011) Micronutrients deficiency and associated sociodemographic factors in Chinese children. World J Pediatr 7, 217–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Moore LL, Singer MR, Qureshi MM et al. (2012) Food group intake and micronutrient adequacy in adolescent girls. Nutrients 4, 1692–1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Qin Y, Melse-Boonstra A, Shi Z et al. (2009) Dietary intake of zinc in the population of Jiangsu Province, China. Asia Pac J Clin Nutr 18, 193–199. [PubMed] [Google Scholar]
- 30. Moher D, Liberati A, Tetzlaff J et al. (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151, 264–269. [DOI] [PubMed] [Google Scholar]
- 31. Katz DL (2014) Nutrition in Clinical Practice. Phildelphia, PA: Lippincott Williams & Wilkins. [Google Scholar]
- 32. Cortese S, Konofal E, Yateman N et al. (2006) Sleep and alertness in children with attention-deficit/hyperactivity disorder: a systematic review of the literature. Sleep 29, 504–511. [PubMed] [Google Scholar]
- 33. Academy of Nutrition and Dietetics (2012) Evidence Analysis Manual: steps in the ADA evidence analysis process. https://www.andeal.org/evidence-analysis-manual (accessed March 2016).
- 34. Kordas K, Siegel EH, Olney DK et al. (2008) Maternal reports of sleep in 6–18 month-old infants from Nepal and Zanzibar: association with iron deficiency anemia and stunting. Early Hum Dev 84, 389–398. [DOI] [PubMed] [Google Scholar]
- 35. Grandner MA, Jackson N, Gerstner JR et al. (2013) Dietary nutrients associated with short and long sleep duration. Data from a nationally representative sample. Appetite 64, 71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Peirano P, Algarín C, Garrido M et al. (2007) Iron-deficiency anemia is associated with altered characteristics of sleep spindles in NREM sleep in infancy. Neurochem Res 32, 1665–1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Peirano PD, Algarin CR, Garrido MI et al. (2007) Iron deficiency anemia in infancy is associated with altered temporal organization of sleep states in childhood. Pediatr Res 62, 715–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Golub MS, Takeuchi PT, Keen CL et al. (1996) Activity and attention in zinc-deprived adolescent monkeys. Am J Clin Nutr 64, 908–915. [DOI] [PubMed] [Google Scholar]
- 39. Kordas K, Casavantes KM, Mendoza C et al. (2007) The association between lead and micronutrient status, and children’s sleep, classroom behavior, and activity. Arch Environ Occup Health 62, 105–112. [DOI] [PubMed] [Google Scholar]
- 40. Sato-Mito N, Sasaki S, Murakami K et al. (2011) The midpoint of sleep is associated with dietary intake and dietary behavior among young Japanese women. Sleep Med 12, 289–294. [DOI] [PubMed] [Google Scholar]
- 41. Song CH, Kim YH & Jung KI (2012) Associations of zinc and copper levels in serum and hair with sleep duration in adult women. Biol Trace Elem Res 149, 16–21. [DOI] [PubMed] [Google Scholar]
- 42. Ji X & Liu J (2015) Associations between blood zinc concentrations and sleep quality in childhood: a cohort study. Nutrients 7, 5684–5696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Luojus MK, Lehto SM, Tolmunen T et al. (2015) Serum copper, zinc and high-sensitivity C-reactive protein in short and long sleep duration in ageing men. J Trace Elem Med Biol 32, 177–182. [DOI] [PubMed] [Google Scholar]
- 44. Dralle D & Bodeker RH (1980) Serum magnesium level and sleep behavior of newborn infants. Eur J Pediatr 134, 239–243. [DOI] [PubMed] [Google Scholar]
- 45. Black B, Holditch-Davis D, Schwartz T et al. (2006) Effects of antenatal magnesium sulfate and corticosteroid therapy on sleep states of preterm infants. Res Nurs Health 29, 269–280. [DOI] [PubMed] [Google Scholar]
- 46. Held K, Antonijevic I, Künzel H et al. (2002) Oral Mg2+ supplementation reverses age-related neuroendocrine and sleep EEG changes in humans. Pharmacopsychiatry 35, 135–143. [DOI] [PubMed] [Google Scholar]
- 47. Drennan MD, Kripke DF, Klemfuss HA et al. (1991) Potassium affects actigraph-identified sleep. Sleep 14, 357–360. [PubMed] [Google Scholar]
- 48. Sato-Mito N, Shibata S, Sasaki S et al. (2011) Dietary intake is associated with human chronotype as assessed by both morningness–eveningness score and preferred midpoint of sleep in young Japanese women. Int J Food Sci 62, 525–532. [DOI] [PubMed] [Google Scholar]
- 49. Okawa M, Mishima K, Nanami T et al. (1997) Vitamin B12 treatment for delayed phase syndrome: a multicenter double-blind study. Psychiatry Clin Neurosci 51, 275–279. [DOI] [PubMed] [Google Scholar]
- 50. Takahashi K, Okawa M, Matsumoto M et al. (1999) Double-blind test on the efficacy of methylcobalamin on sleep–wake rhythm disorders. Psychiatry Clin Neurosci 53, 211–213. [DOI] [PubMed] [Google Scholar]
- 51. Mayer G, Kroger M & Meier-Ewert K (1996) Effects of vitamin B12 on performance and circadian rhythm in normal subjects. Neuropsychopharmacology 15, 456–464. [DOI] [PubMed] [Google Scholar]
- 52. Beydoun MA, Gamaldo AA, Canas JA et al. (2014) Serum nutritional biomarkers and their associations with sleep among US adults in recent national surveys. PLoS One 9, e103490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Shiue I (2013) Low vitamin D levels in adults with longer time to fall asleep: US NHANES, 2005–2006. Int J Cardiol 168, 5074–5075. [DOI] [PubMed] [Google Scholar]
- 54. Kim JH, Chang JH, Kim DY et al. (2014) Association between self-reported sleep duration and serum vitamin D level in elderly Korean adults. J Am Geriatr Soc 62, 2327–2332. [DOI] [PubMed] [Google Scholar]
- 55. Massa J, Stone KL, Wei EK et al. (2015) Vitamin D and actigraphic sleep outcomes in older community-dwelling men: the MrOS sleep study. Sleep 38, 251–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Grandner MA, Kripke DF, Naidoo N et al. (2010) Relationships among dietary nutrients and subjective sleep, objective sleep, and napping in women. Sleep Med 11, 180–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lichstein KL, Payne KL, Soeffing JP et al. (2007) Vitamins and sleep: an exploratory study. Sleep Med 9, 27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Holditch-Davis D (2010) Development of sleep and sleep problems in preterm infants. http://www.child-encyclopedia.com/sleeping-behaviour/according-experts/development-sleep-and-sleep-problems-preterm-infants (accessed March 2016).
- 59. Holditch-Davis D, Scher M, Schwartz T et al. (2004) Sleeping and waking state development in preterm infants. Early Hum Dev 80, 43–64. [DOI] [PubMed] [Google Scholar]
- 60. Knyazev GG (2012) EEG delta oscillations as a correlate of basic homeostatic and motivational processes. Neurosci Biobehav Rev 36, 677–695. [DOI] [PubMed] [Google Scholar]
- 61. Liu X, Zhao Z, Jia C et al. (2008) Sleep patterns and problems among Chinese adolescents. Pediatrics 121, 1165–1173. [DOI] [PubMed] [Google Scholar]
- 62. Roenneberg T, Kuehnle T, Juda M et al. (2007) Epidemiology of the human circadian clock. Sleep Med Rev 11, 429–438. [DOI] [PubMed] [Google Scholar]
- 63. Chollet D, Franken P, Raffin Y et al. (2000) Blood and brain magnesium in inbred mice and their correlation with sleep quality. Am J Physiol Regul Integr Comp Physiol 279, R2173–R2178. [DOI] [PubMed] [Google Scholar]
- 64. Kurina LM, McClintock MK, Chen JH et al. (2013) Sleep duration and all-cause mortality: a critical review of measurement and associations. Ann Epidemiol 23, 361–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Marchetti C, Baranowska-Bosiacka I & Gavazzo P (2014) Multiple effects of copper on NMDA receptor currents. Brain Res 1542, 20–31. [DOI] [PubMed] [Google Scholar]
- 66. Takeda A, Minami A, Seki Y et al. (2004) Differential effects of zinc on glutamatergic and GABAergic neurotransmitter systems in the hippocampus. J Neurosci Res 75, 225–229. [DOI] [PubMed] [Google Scholar]
- 67. Beard JL, Erikson KM & Jones BC (2002) Neurobehavioral analysis of developmental iron deficiency in rats. Behav Brain Res 134, 517–524. [DOI] [PubMed] [Google Scholar]
- 68. Panossian LA & Veasey SC (2012) Daytime sleepiness in obesity: mechanisms beyond obstructive sleep apnea – a review. Sleep 35, 605–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Schwartz RD, Wagner JP, Yu X et al. (1994) Bidirectional modulation of GABA-gated chloride channels by divalent cations: inhibition by Ca2+ and enhancement by Mg2+ . J Neurochem 62, 916–922. [DOI] [PubMed] [Google Scholar]
- 70. Turgeon SM & Albin RL (1992) Zinc modulates GABAB binding in rat brain. Brain Res 596, 30–34. [DOI] [PubMed] [Google Scholar]
- 71. Navigatore-Fonzo LS, Delgado SM, Golini RS et al. (2014) Circadian rhythms of locomotor activity and hippocampal clock genes expression are dampened in vitamin A-deficient rats. Nutr Res 34, 326–335. [DOI] [PubMed] [Google Scholar]
- 72. Beard J (2003) Iron deficiency alters brain development and functioning. J Nutr 133, 5 Suppl. 1, 1468S–1472S. [DOI] [PubMed] [Google Scholar]
- 73. Singh M (2004) Role of micronutrients for physical growth and mental development. Indian J Pediatr 71, 59–62. [DOI] [PubMed] [Google Scholar]
- 74. Sharonova IN, Vorobjev VS & Haas HL (2000) Interaction between copper and zinc at GABAA receptors in acutely isolated cerebellar Purkinje cells of the rat. Br J Pharmacol 130, 851–856. [DOI] [PMC free article] [PubMed] [Google Scholar]