Abstract
Introduction
Surgical site infection (SSI) can cause devastating reconstructive failure in implant-based breast reconstructions. Many large national database studies have offered insights into complication rates, but only capture early outcomes within 30-days post-operatively. This study evaluates both early and late SSI in immediate implant-based reconstruction and identifies predictors.
Methods
As part of the Mastectomy Reconstruction Outcomes Consortium Study (MROC), 1662 implant-based breast reconstructions in 1024 patients were evaluated for early vs. late SSI. Early SSI was defined as infection occurring within 30 days post-operatively and late SSI as infection occurring 31 days to 1 year. Minor infection required oral antibiotics only, and major infection required hospitalization and/or surgical treatment. Direct-to-implant (DTI) patients had one-year follow-up, and tissue-expander (TE) patients had one-year post-exchange follow-up.
Results
Among 1491 TE and 171 DTI reconstructions, overall SSI rate for TE was 5.7% (85/1491) after first-stage, 2.5% (31/1266) after second-stage, and 9.9% (17/171) for DTI. Over 47–71% of SSI complications occurred as late SSI. Multivariate analysis identified radiotherapy and BMI as significant predictors of late SSI. No significant difference between DTI and TE group in the occurrence of early, late, or overall SSI was found.
Conclusions
The majority of SSI complications in immediate implant-based breast reconstructions are late infections occurring more than 30 days following both first-stage and second-stage procedures. Radiotherapy and obesity are significantly associated with late-onset SSI. Current studies limited to early complications do not present an accurate or complete assessment of infection complications associated with implant-based breast reconstructions or their long-term clinical outcomes.
Introduction
Implant-based breast reconstruction is currently the most popular method of immediate breast reconstruction given its simplicity and lack of donor-site. It can be achieved either as a two-stage surgery with a tissue expander (TE) that is later exchanged to an implant, or as a single-stage surgery utilizing a direct-to-implant (DTI) approach.1–3 Advantages of implant-based breast reconstruction compared to autologous breast reconstruction include shorter procedure time, decreased length of hospital stay, and quicker overall recovery.4–5 However, the risk of surgical site infection (SSI) is a major concern as it can lead to reconstructive failure, ultimately requiring removal of the breast TE or implant.6
The SSI rate following implant-based breast reconstructions has been reported as approximately 2.5–3.4% and can have potentially devastating complications.7–18 Management often involves tissue expander or implant removal and systemic antibiotic therapy for up to two weeks for common infections.19 Re-implantation following removal can be attempted within 3–6 months, although this may not be possible in cases involving chest wall radiotherapy.20 In order to attempt salvage of prosthetic reconstruction, systemic antibiotics without implant removal may be successful in a subset of patients with mild SSIs.21–22 Such management frequently requires long-term antibiotic treatment and can lead to delay or disruption of oncologic therapy. Previous studies have reviewed single surgeon or institutional outcomes following TE or DTI reconstructions in attempts to ascertain infection and reconstructive failure rates and identify associated risk factors.7–9
Recently, larger population studies have been performed on a broader scale employing national databases such as the National Surgical Quality Improvement Program (NSQIP) and Tracking Operations and Outcomes for Plastic Surgeons (TOPS).1,10–24 These studies have offered important insights into surgical complication rates and suggested co-morbidities that portend failure of implant-based breast reconstruction on a population level. However, these databases only capture up to 30-day outcomes following a procedure and do not allow for any long-term clinical outcome assessment. Thus, many recently published SSI complication rates in implant-based breast reconstructions are solely limited to early infections.
Although it has generally been assumed that the vast majority of SSI complications occur within 30 days following a procedure, late infections are frequently observed several months or even years following implant-based breast reconstruction.25 The consequences of late SSI are just as serious as early SSI and the treatment is not any easier. Despite this fact, the rate of late SSI is unknown and the associated risk factors for late SSI are unclear. The goal of the present study was to evaluate the rates of both early (</=30days) and late (>30days to 1 year) SSIs in immediate implant-based breast reconstruction and to identify predictors using a post hoc analysis of data from a large prospective multi-center trial.
Methods
Patients were recruited as part of the Mastectomy Reconstruction Outcomes Consortium (MROC) Study, a five-year prospective, multicenter cohort study of mastectomy reconstruction patients funded by the National Cancer Institute. Women 18 years or older undergoing first-time, unilateral or bilateral mastectomy breast reconstruction were eligible for participation. Fifty-seven plastic surgeons from 11 centers in the USA (Michigan, New York, Illinois, Ohio, Massachusetts, Washington, D.C., Georgia and Texas) and Canada (British Columbia and Manitoba) contributed patients to the study, which began in February 2012. Appropriate Institutional Review Board (IRB) approval was obtained from all participating sites. From the study, 1662 implant-based breast reconstructions in 1024 patients were evaluated for early vs. late SSI.
Early SSI was defined as infection occurring within 30 days after surgery, and late SSI was defined as infection occurring between 31 days to 1 year after surgery. DTI patients had minimum one-year follow-up, and TE patients had two-year follow-up including minimum one-year follow-up data from the second-stage exchange procedure. Minor infection was defined as SSI successfully treated with outpatient oral antibiotics, and major infection was defined as SSI requiring inpatient hospitalization and/or operative treatment.
Clinical and demographic characteristics of the cohort were summarized by those with no SSI, with early SSI and with late SSI. Occurrence of SSI was expressed as percentages by timing (early versus late) and type (major versus minor) and was also summarized by DTI and TE procedures. All analyses were done with breast as the analytical unit, except for the demographic characteristics, which were summarized at patient level. A mixed-effects logistic regression model was employed at breast level to further identify potential predictors for late SSI. The model included BMI, reconstructive procedure type (DTI vs. TE), indication for mastectomy (prophylactic vs. cancer), ADM usage, smoking status and radiation therapy as independent variables. The model also included random intercepts for hospitals and for patients nested within hospitals to account for between-center and between-patient variability. We reported adjusted odds ratios (OR), 95% confidence intervals (CI) and corresponding p-values based on the model. All statistical analyses were performed in SAS 9.4 (SAS Institute, Cary, NC), and statistical significance was set at 0.05.
Results
Demographic Data
A total of 1662 breast reconstructions in 1024 patients were included in the study. Among these, 1491 reconstructions were two-stage procedures performed with immediate tissue expander placement and 171 reconstructions were performed as single-stage surgery utilizing a direct-to-implant approach. Demographic data (Table 1) demonstrated a mean age of 48 years (±10.6 SD). Mean body mass index (BMI) was 25.8 (±5.6). 2.1% of patients were smokers at the time of reconstruction and 3.5% had diabetes. 90.4% of patients had one medical co-morbid condition or none.
Table 1.
Demographic Characteristics for Patients (N = 1024) and by Surgical Site Infection (SSI) Status and Timing
| SSI Status | |||||
|---|---|---|---|---|---|
|
|
|||||
| All Patients | No SSI | Early SSI | Late1 SSI | ||
| ≤30 days | ≥31 days | ||||
| N = 1024 | N = 910 | N2 = 48 | N2 = 68 | ||
| % = 88.87 | % = 4.69 | % = 6.64 | |||
| Age, mean (SD) | 48.42 (10.57) | 48.24 (10.71) | 49.25 (8.42) | 49.99 (10.05) | |
| BMI, mean (SD) | 25.84 (5.58) | 25.61 (5.28) | 26.12 (6.06) | 28.71 (7.91) | |
| Smoking | |||||
| Current smoker | 21 (2.07) | 17 (80.95) | 3 (14.29) | 1 (4.76) | |
| Previous smoker | 300 (29.59) | 263 (87.67) | 13 (4.33) | 25 (8.33) | |
| Non smoker | 693 (68.34) | 621 (89.61) | 32 (4.62) | 41 (5.92) | |
| Number of comorbid conditions3 | |||||
| 0 | 83 (8.11) | 76 (91.57) | 4 (4.82) | 3 (3.61) | |
| 1 | 843 (82.32) | 750 (88.97) | 38 (4.51) | 57 (6.76) | |
| >=2 | 98 (9.57) | 84 (85.71) | 6 (6.12) | 8 (8.16) | |
| Diabetes | 36 (3.52) | 29 (80.56) | 2 (5.56) | 5 (13.89) | |
Abbreviation: BMI is body mass index.
Cell values are n (%), unless otherwise specified. % are column percentages for "All Patients" column, and are row percentages for the rest columns.
Late SSI is defined as 31–365 days for direct to implant patients, 31 days to 365 days or up to exchange procedure for tissue expander patients, and 31–365 days after exchange for tissue expander post-exchange patients.
Includes two patients who experienced both early SSI and late SSI.
Based on Charlson index, including diabetes.
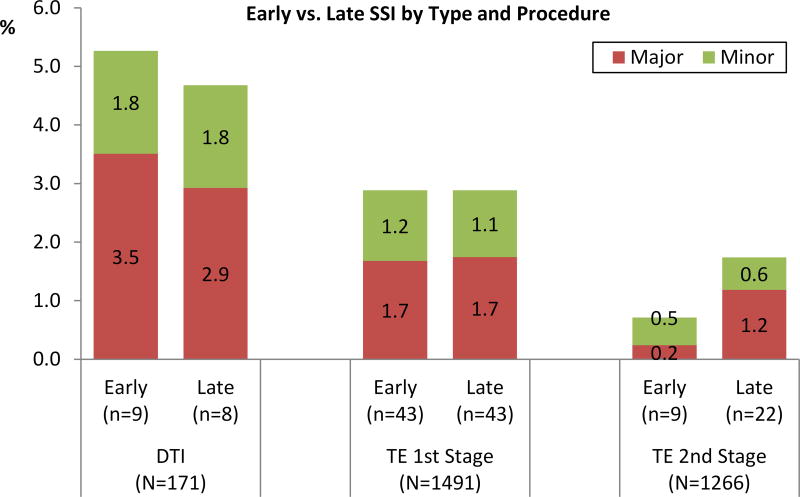
Overall SSI rate was 9.9% (17/171) in the DTI group and 7.7% (114/1491) in the TE group. Of note, 47.1% of SSI in the DTI group and 56.0% of SSI in the TE group were late SSI occurring 30+ days after the initial reconstruction (8/17 in DTI; 65/116 in TE) (Table 2). The major infection rate was 6.4% (11/171) in the DTI group with 45% (5/11) occurring as late SSI, and the major infection rate was 3.4% (51/1491) in the first-stage TE group with 51% (26/51) occurring as late SSI. The minor infection rate was 3.5% (6/171) in the DTI group with 50% (3/6) occurring as late SSI, and the minor infection rate was 2.3% (35/1491) in the first-stage TE group with 49% (17/35) occurring as late SSI (Figure 1). There was no significant difference between DTI and TE groups in the rates of early, late, or overall SSI.
Table 2.
Procedural and Clinical Characteristics for Reconstructed Breasts (N = 1662) and by Surgical Site Infection (SSI) Status and Timing
| SSI Status | ||||
|---|---|---|---|---|
|
|
||||
| All Breasts | No SSI | Early SSI | Late1 SSI | |
| ≤30 days | ≥31 days | |||
| N = 1662 | N = 1531 | N2 = 60 | N2 = 73 | |
| % = 92.12 | % = 3.61 | % = 4.39 | ||
| Reconstruction Types | ||||
| Direct to implant (DTI) | 171 (10.29) | 154 (90.06) | 9 (5.26) | 8 (4.68) |
| Tissue expander (TE) | 1491 (89.71) | 1377 (92.35) | 51 (3.42) | 65 (4.36) |
| Clinical Characteristics | ||||
| Prophylactic | 666 (40.07) | 619 (92.94) | 25 (3.75) | 23 (3.45) |
| ADM used | 937 (56.38) | 858 (91.57) | 35 (3.74) | 46 (4.91) |
| No chemo | 976 (58.72) | 899 (92.11) | 39 (4.00) | 40 (4.10) |
| Neo-adjuvant chemo | 218 (13.12) | 206 (94.50) | 4 (1.83) | 8 (3.67) |
| Adjuvant chemo | 468 (28.16) | 426 (91.03) | 17 (3.63) | 25 (5.34) |
| Radiation pre-reconstruction | 101 (6.08) | 86 (85.15) | 8 (7.92) | 7 (6.93) |
| Radiation post-TE placement3 | 262 (15.76) | 234 (89.31) | 5 (1.91) | 23 (8.78) |
| Radiation post-implant placement | 85 (5.11) | 79 (92.94) | 2 (2.35) | 4 (4.71) |
| No radiation | 1214 (73.04) | 1132 (93.25) | 45 (3.71) | 39 (3.21) |
Abbreviation: ADM is acellular dermal matrix.
Cell values are n (%). % are column percentages for "All Breasts" column, and are row percentages for the rest columns.
Late SSI is defined as 31–365 days for direct to implant patients, 31 days to 365 days or up to exchange procedure for tissue expander patients, and 31–365 days after exchange for tissue expander post-exchange patients.
Includes two patients who experienced both early SSI and late SSI.
Applicable for tissue expander patients only.
Figure 1.
Among 1491 TE and 171 DTI reconstructions, overall SSI rate for TE was 5.7% for first-stage, 2.5% for second-stage, and 9.9% for DTI. 47–71% of all SSI complications occurred as late SSI.
A total of 1266 TE reconstructions underwent second-stage exchange to implants. Of note, the second-stage procedures were found to be significantly more prone to late SSI than early SSI. The overall SSI rate for second-stage procedures was 2.5% (31/1266) with 71% (22/31) occurring as late SSI 30+ days following the exchange procedure (Figure 1).
A significant percentage of late SSI cases resulted in explantation of the prosthesis (Table 3). 43.8 % (32/73) of late SSI cases required ultimate explantation while 26.2 % (16/61) of early SSI cases led to explantation due to infection. Among the DTI group, 23.5 % (4/17) of overall SSI cases required removal of the implant with 50% of the explant cases being due to late SSI. In the first-stage TE group, 42.4% (36/85) of overall SSI cases required removal of the TE with 64% of the explant cases being due to late SSI. In the second-stage TE exchange group, 22.6% (7/31) of overall SSI cases required explantation of the implant with 100% of the explant cases being due to late SSI.
Table 3.
Number of Surgical Site Infection Resulting in Explantation by Type of Procedure and by Timing of Infection
| Total SSI | Early SSI | Late1 SSI | |
|---|---|---|---|
| ≤30 days | ≥31 days | ||
| N=133 | N=61 | N=73 | |
| Direct to Implant (N=17) | 4 | 2 | 2 |
| Tissue Expander Pre-Exchange (N=85) | 36 | 14 | 23 |
| Tissue Expander Post-Exchange (N=31) | 7 | 0 | 7 |
|
| |||
| Total | 47 | 16 | 32 |
Late SSI is defined as 31–365 days for direct to implant patients, 31 days to 365 days or up to exchange procedure for tissue expander patients, and 31–365 days after exchange for tissue expander post-exchange patients.
Multivariate analysis identified two predictors of late SSI following implant-based breast reconstruction. These predictors included radiation therapy following first-stage TE placement (OR:2.93, p=0.001) and increased BMI (OR:1.08, p=0.000) as significant predictors of late SSI (Table 4). Use of acellular dermal matrix, pre-reconstruction radiotherapy, radiotherapy following implant placement, and therapeutic versus prophylactic mastectomy were not associated with late SSI.
Table 4.
Mixed Effects Logistic Regression Model for Late SSI1
| OR | 95% CI | p-Value | ||
|---|---|---|---|---|
| BMI | 1.08 | (1.036, 1.117) | 0.000 | |
| Procedure type | ||||
| Tissue expander (TE) | -Reference- | |||
| Direct to implant (DTI) | 1.02 | (0.411, 2.550) | 0.959 | |
| Indication | ||||
| Prophylactic | -Reference- | |||
| Cancer | 1.36 | (0.803, 2.319) | 0.250 | |
| ADM used | 1.11 | (0.614, 2.012) | 0.728 | |
| Smoking | ||||
| Non smoker | -Reference- | |||
| Current smoker | 0.57 | (0.070, 4.654) | 0.601 | |
| Previous smoker | 1.47 | (0.865, 2.501) | 0.154 | |
| Radiation | ||||
| No radiation | -Reference- | |||
| Radiation pre-reconstruction | 2.10 | (0.843, 5.250) | 0.111 | |
| Radiation post-TE placement | 2.93 | (1.591, 5.395) | 0.001 | |
| Radiation post-implant placement | 1.34 | (0.427, 4.202) | 0.617 | |
Late SSI is defined as 31–365 days for direct to implant patients, 31 days to 365 days or up to exchange procedure for tissue expander patients, and 31–365 days after exchange for tissue expander post-exchange patients.
Figure 2 illustrates a clinical case example of late SSI that occurred 10 months after a second stage TE-to-implant exchange procedure. The patient had cancer affecting the left breast and underwent bilateral mastectomy and immediate breast reconstruction using TE and acellular dermal matrix followed by left chest wall radiotherapy. Although good cosmetic outcome was maintained through radiotherapy and for months following the second-stage exchange procedure, late SSI developed 10 months following the second-stage procedure leading ultimately to significant capsular contracture and compromise of reconstructive outcome.
Figure 2.
Patient is a 39 year-old female who was diagnosed with left breast cancer. Patient is seen following bilateral mastectomy with ADM and TE reconstruction, followed by post-mastectomy radiation therapy of the left chest during expansion. Patient is seen 2 months following TE exchange to implant (A). At 10 months post-operative from a TE to implant exchange procedure, mild cellulitis can be visualized overlying the left chest (B). Following IV antibiotic treatment and resolution of cellulitis, the patient now has capsular contracture and obvious asymmetry (C).
Discussion
Reported infection rates following prosthetic breast reconstruction for mastectomy defects range from 1–35%.26,27 SSI is highly predictive of subsequent implant failure.7 Prophylactic and perioperative antibiotics are known to decrease SSI rates, whereas postoperative hematomas and seromas increase the overall rate.28 Most early SSIs and implant failures are associated with endogenous skin flora that colonize the nipple, including staphylococcus aureus, streptococci and lactobacilli species, and propionibacterium acnes.29,30 Although most SSIs are generally thought to occur within months, some are observed to occur even after many years.26 The Center for Disease Control and Prevention (CDC) defines deep incisional SSI to be infection occurring within one year after the operation when implant is in place.31 However, up to this point, the true rate of late infections in implant-based breast reconstruction has been unknown.
The present study demonstrates that the majority of SSI complications in immediate implant-based breast reconstructions are late infections occurring later than 30 days post-operatively following either first-stage or second-stage procedures. Our data show that 47–71% of total SSI complications occur as late infections. This finding is of particular concern because of the recent popularity of large database studies utilizing national registries such as NSQIP and TOPS.32 Although such studies generate study populations of impressive size and appear to allow more robust analysis of complications and outcomes, their data collection is limited to a 30-day period following surgery and therefore is limited to short-term complications and outcomes. A small descriptive study by Luce and Pierce evaluating a cohort of tissue expander breast reconstructions suggested that greater numbers of tissue expander explants occur beyond the 30-day postoperative window and questioned the appropriateness of utilizing the NSQIP database to examine this patient.33 Similarly, Cohen et al. determined median time to explanation, following implant based breast procedures, to be 41 days and commented that only 50% of SSIs occurred within the one month time-point.34 Our current study confirms that a majority of SSI cases in this patient population occur later than 30 days following surgery and suggests that recent national database studies significantly underestimate the risk of actual SSI in implant-based breast reconstructions.
Although the etiologic mechanisms of late infection remain unclear, early colonization may result in the formation of a biofilm and subsequent subacute infection which only manifests in delayed fashion after many months.35 Late SSI may also be associated with capsular contracture.36–38 Recent studies suggest that late onset capsular contracture may simply be a manifestation of chronic infection and biofilm formation.39 In patients with implants removed for capsular contractures, 33–41% were associated with colonization by skin flora.39,40 The relationship between biofilm and capsular contracture remains unclear and warrants further research.41
In the present study, radiation therapy was identified as one of the significant independent risk factors for late SSI, particularly following second-stage tissue expander exchange procedure. This finding is consistent with prior studies reporting chest wall irradiation as a significant risk factor for overall breast SSI.42–44 In a recent study, radiation therapy increased the rate of permanent implant infection and removal by approximately 5-fold compared to non-radiated breasts, similar to the odds ratio of 4 that our study observed.45 In a separate study with a longer follow-up period, 9% of post-mastectomy irradiation patients suffered implant loss, as compared to 0.5% in the control population.46 Radiation therapy also reduces the likelihood of implant salvage following infection or prosthesis exposure.47 Many of these studies are limited by short-term follow-up, and outcomes specifically following the second-stage procedure are lacking. To the authors’ knowledge, the current study reports SSI outcomes from the largest population of second-stage exchange procedures (N=1266) with minimum of one-year follow-up to date. Moreover, strict use of CDC definitions of SSI in the data set results in the most complete and accurate assessment of SSI rate to date.
Although two-stage breast reconstruction using a tissue expander exchange to implant procedure is generally considered to be a simple and benign surgery with minimal complication risk, our study results show that the rate of late infection may have been vastly underappreciated in this patient population, with up to 71% of SSIs occurring as late infections. Moreover, post-mastectomy radiotherapy may produce tissue changes, including progressive soft tissue fibrosis and vascular compromise that is likely to contribute to the overall increased risk of late onset SSI complications, even following second-stage exchange procedures.
Our study also identified higher body mass index (BMI) as a significant predictor for late SSI. This is not a novel concept in surgical literature and many previous studies have reported obesity as a significant risk factor for SSI in general.48,49 Obesity is frequently associated with macromastia. Large preoperative breast volume results in significant dead space following mastectomy, and placement of a substantial foreign body burden (implant or TE) in the setting of already tenuous soft tissue envelope coverage can lead to infection. Postoperative seroma is also commonly encountered with obesity, and this can be especially challenging to detect in obese patients. Residual seroma after initial surgical drain removal may be a trigger for late onset infections. Although most reconstructive surgeons certainly understand obesity as a well-established risk factor for not only surgical complications but also poor aesthetic outcome in implant-based breast reconstruction, this patient group unfortunately has increased risk of surgical complications even with autologous breast reconstructions.50 The present study identified that the risk for late SSI increased by 8% per each point increase in BMI. It may therefore be wise to counsel obese patients regarding the late onset infection complications and reconstruction failure risks and to consider delayed breast reconstruction approach.
Although the present study provides valuable data from a large prospective multicenter cohort from the MROC study, it does have a number of limitations. Although the early, late, and overall SSI rates are well documented, our analysis is limited by the absence of additional data points, such as culture results, duration of antibiotic treatment, drain use, and duration of neoadjuvant or adjuvant therapy. Additionally, given the nature of a multicenter cohort design, there may be variations in the SSI evaluation and treatment protocol among the participating institutions, including the criteria for inpatient hospitalization and intravenous antibiotics, explantation versus salvage, as well as radiotherapy protocol. Nonetheless, the results illustrate the remarkable underestimation of the rate of surgical site infections in implant-based breast reconstruction and identify important predictors for late infections which can play a significant role in patient counseling. Finally, the number of patients undergoing DTI reconstruction was relatively small, which limits the power of our study to make conclusions regarding this patient group. Future research directions should incorporate an even longer follow-up period with evaluation of associations between incidences of SSIs and post-operative time period.
Conclusion
The majority of SSI complications following immediate implant-based breast reconstructions are late infections that present greater than 30 days after surgery following either the first or second stage of surgical treatment. Radiotherapy and higher BMI are significantly associated with late onset SSI. The NSQIP database captures data limited to 30 days after surgery and may under-report SSI complications in this patient population. Recent studies using NSQIP and other large national registries therefore may not present an accurate or complete assessment of infection complications associated with implant-based breast reconstructions nor their long-term clinical outcomes. Preoperative counseling when considering implant-based breast reconstruction should incorporate discussions regarding the risk of late SSIs and its specific risk factors--radiotherapy and obesity.
Acknowledgments
The study was supported by a grant from the National Cancer Institute (1RO1CA152192). The authors gratefully acknowledge the contributions of our colleagues at the following centers who contributed their expertise to this multicenter trial: University of Michigan Health System, Ann Arbor, MI; Memorial Sloan-Kettering Cancer Center, New York City, NY; St. Joseph Mercy Hospital, Ypsilanti, MI; Northwestern Memorial Hospital, Chicago, IL; Ohio State Medical Center, Columbus, OH; Brigham and Women’s Hospital, Boston, MA; Georgetown University Medical Center, Washington, D.C.; Georgia Institute of Plastic Surgery, Savannah, GA; M.D. Anderson Cancer Center, Houston, TX; University of Manitoba, Winnipeg, MB; University of British Columbia, Vancouver, BC.
Footnotes
Disclosures: The authors have no conflicts of interest or disclosures. This work has not been previously presented and is not in consideration for publication at any other journals
References
- 1.Fischer JP, Nelson JA, Serletti JM, Wu JZ. Peri-operative risk factors associated with early tissue expander loss following immediate breast reconstruction: A review of 9305 patients from the 2005–2010 ACS-NSQIP datasets. J Plast Recon Aesthet Surg. 2013;66:15014–12. doi: 10.1016/j.bjps.2013.06.030. [DOI] [PubMed] [Google Scholar]
- 2.Albornoz CR, Bach PB, Mehrara BJ, et al. A paradigm shift in US breast reconstruction: increasing implant rates. J Plast Reconstr Surg. 2013;131:15–23. doi: 10.1097/PRS.0b013e3182729cde. [DOI] [PubMed] [Google Scholar]
- 3.Cemal Y, Albornoz CR, Disa JJ, et al. A paradign shift in US breast reconstruction: part 2. The influence of changing mastectomy patters on reconstructive rate and method. J Plast Reconstr Surg. 2013;131:320e–6e. doi: 10.1097/PRS.0b013e31827cf576. [DOI] [PubMed] [Google Scholar]
- 4.Argenta LC. Reconstruction of the breast by tissue expansion. Clin Surg. 1984;11:257–64. [PubMed] [Google Scholar]
- 5.Shaikh-Naidu N, Preminger B, Rogers K, et al. Determinants of aesthetic satisfaction following TRAM and implant based breast reconstruction. Ann Plast Surg. 2004;52:465–70. doi: 10.1097/01.sap.0000123901.06133.b7. [DOI] [PubMed] [Google Scholar]
- 6.McCullough MC, Chu CK, Duggal CS, et al. Antibiotic prophylaxis and resistance in surgical site infection in immediate tissue expander reconstruction of the breast. Ann Plast Surg. 2014;73:1–5. doi: 10.1097/SAP.0000000000000275. [DOI] [PubMed] [Google Scholar]
- 7.Disa JJ, Ad-El DD, Cohen SM, et al. The premature removal of tissue expanders in breast reconstruction. Plast Reconstr Surg. 1999;104:1662–5. doi: 10.1097/00006534-199911000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Reish RG, Damjanovic B, Austen WG, Jr, et al. Infection following implant-based reconstruction in 1952 consecutive breast reconstructions: Salvage rates and predictors of success. Plast Reconstr Surg. 2013;131:1223–30. doi: 10.1097/PRS.0b013e31828bd377. [DOI] [PubMed] [Google Scholar]
- 9.Nahabedian MY, Tsangaris T, Momen B, Manson PN. Infectious complications following breast reconstruction with expanders and implants. Plast Reconstr Surg. 2003;112:467–76. doi: 10.1097/01.PRS.0000070727.02992.54. [DOI] [PubMed] [Google Scholar]
- 10.Fischer JP, Wes AM, Tuggle CT, et al. Mastectomy with or without immediate implant reconstruction has similar 30-day perioperative outcomes. J Plast Reconstr Aesthet Surg. 2014;67:1515–22. doi: 10.1016/j.bjps.2014.07.021. [DOI] [PubMed] [Google Scholar]
- 11.Fischer JP, Wes AM, Tuggle CT, et al. Risk analysis of early implant loss after immediate breast reconstruction: a review of 14,585 patients. J Am Coll Surg. 2013;217:983–90. doi: 10.1016/j.jamcollsurg.2013.07.389. [DOI] [PubMed] [Google Scholar]
- 12.Fischer JP, Nelson JA, Kovach SJ, et al. Impact of obesity on outcomes in breast reconstruction: analysis of 15,937 patients from the ACS-NSQIP datasets. J Am Coll Surg. 2013;217:656–64. doi: 10.1016/j.jamcollsurg.2013.03.031. [DOI] [PubMed] [Google Scholar]
- 13.Fischer JP, Nelson JA, Au A, et al. Complications and morbidity following breast reconstruction--a review of 16,063 cases from the 2005–2010 NSQIP datasets. J Plast Surg Hand Surg. 2014;48:104–14. doi: 10.3109/2000656X.2013.819003. [DOI] [PubMed] [Google Scholar]
- 14.Fischer JP, Nelson JA, Serletti JM, Wu LC. Peri-operative risk factors associated with early tissue expander (TE) loss following immediate breast reconstruction (IBR): a review of 9305 patients from the 2005–2010 ACS-NSQIP datasets. J Plast Reconstr Aesthet Surg. 2013;66:1504–12. doi: 10.1016/j.bjps.2013.06.030. [DOI] [PubMed] [Google Scholar]
- 15.Wink JD, Fischer JP, Nelson JA, et al. Direct-to-implant breast reconstruction: An analysis of 1612 cases from the ACS-NSQIP surgical outcomes database. J Plast Surg Hand Surg. 2014;48:375–81. doi: 10.3109/2000656X.2014.899240. [DOI] [PubMed] [Google Scholar]
- 16.Khavanin N, Gutowski KA, Hume KM, et al. The use of patient registries in breast surgery: a comparison of the tracking operations and outcomes for plastic surgeons and national surgical quality improvement program data sets. Ann Plast Surg. 2015;74:157–62. doi: 10.1097/SAP.0000000000000383. [DOI] [PubMed] [Google Scholar]
- 17.Alderman AK, Wilkins EG, Kim HM, Lowery JC. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2002;109:2265–74. doi: 10.1097/00006534-200206000-00015. [DOI] [PubMed] [Google Scholar]
- 18.Winocour S, Martinez-Jorge J, Habermann E, et al. Early Surgical Site Infection Following Tissue Expander Breast Reconstruction with or without Acellular Dermal Matrix: National Benchmarking Using National Surgical Quality Improvement Program. Archive Plast Surg. 2015;42(2):194–200. doi: 10.5999/aps.2015.42.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Macadam S, Mehling B, Fanning A, et al. Nontuberculosis mycobacterial breast implant infections. Plast Reconst Surg. 2007;119:337–44. doi: 10.1097/01.prs.0000244924.61968.d2. [DOI] [PubMed] [Google Scholar]
- 20.Pittet B, Montandon D, Pitted D. Infection in breast implants. Lancet Infect Dis. 2005;5:94–106. doi: 10.1016/S1473-3099(05)01281-8. [DOI] [PubMed] [Google Scholar]
- 21.Spear S, Howard M, Boehmler J, et al. The infected or exposed breast implant: management and treatment strategies. Plast Reconstr Surg. 2004;113:1634–44. doi: 10.1097/01.prs.0000117194.21748.02. [DOI] [PubMed] [Google Scholar]
- 22.Halvorson E, Disa J, Behrara B, et al. Outcome following remocal of infected tissue expanders in breast reconstruction: a 10-year experience. Ann Plast Surg. 2007;59:131–6. doi: 10.1097/01.sap.0000252716.73356.68. [DOI] [PubMed] [Google Scholar]
- 23.Gart MS, Smetona JT, Hanwright PJ, et al. Autologous options for postmastectomy breast reconstruction: a comparison of outcomes based on the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2013;216:229–38. doi: 10.1016/j.jamcollsurg.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 24.National Collaborating Centre for Women's and Children's Health. Surgical site infection: prevention and treatment of surgical site infection. London (UK): National Institute for Health and Clinical Excellence (NICE); 2008. Oct, [Google Scholar]
- 25.Horan TC, Gaynes RP, Martone WJ, et al. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infection Control and Hospital Epidemiology. 1992;13:606–8. [PubMed] [Google Scholar]
- 26.Washer LL, Gutowski K. Breast implant infections. Infect Dis Clin North Am. 2012;26:111–25. doi: 10.1016/j.idc.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 27.Saha D, Davila AA, Ver Halen JP, et al. Post-mastectomy reconstruction: a risk-stratified comparative analysis of outcomes. Breast. 2013;22:1072–80. doi: 10.1016/j.breast.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 28.Olsen MA, Lefta M, Dietz JR, et al. Risk factors for surgical site infection after major breast operation. J Am Coll Surg. 2008;207:326–35. doi: 10.1016/j.jamcollsurg.2008.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thornton J, Argenta L, McClatchey K, et al. Studies on the endogenous flora of the human breast. Ann Plast Surg. 1988;20:39–42. doi: 10.1097/00000637-198801000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Feldman E, Kontoyiannis D, Sharabi S, et al. Breast implant infections: is cefazolin enough? Plast Reconstr Surg. 2010;126:779–85. doi: 10.1097/PRS.0b013e3181e5f7ff. [DOI] [PubMed] [Google Scholar]
- 31.http://www.cdc.gov/nhsn/PDFs/pscManual/9pscSSIcurrent.pdf, Accessed 2/1/2016
- 32.Chow I, Hanwright PJ, Hansen NM, et al. Predictors of 30-day readmission after mastectomy: A multi-institutional analysis of 21,271 patients. Breast Dis. 2015;35(4):221–31. doi: 10.3233/BD-150412. [DOI] [PubMed] [Google Scholar]
- 33.Luce EA, Pierce CE. Lack of validity of the American College of Surgeons National Surgical Quality Improvement Program Database for alloplastic immediate postmastectomy reconstruction. Plast Reconstr Surg. 2015;136:296e–300. doi: 10.1097/PRS.0000000000001515. [DOI] [PubMed] [Google Scholar]
- 34.Cohen JB, Carroll C, Tenenbaum MM, Myckatyn TM. Breast implant-associated infections: the role of the National Surgical Improvement program and the local microbiome. Plast Reconstr Surg. 2015;136:921–9. doi: 10.1097/PRS.0000000000001682. [DOI] [PubMed] [Google Scholar]
- 35.Wolcott R, Costerton JW, Raoult D, Cutler SJ. The polymicrobial nature of biofilm infection. Clin Microbiol Infect. 2013;19:107–12. doi: 10.1111/j.1469-0691.2012.04001.x. [DOI] [PubMed] [Google Scholar]
- 36.Pajkos A, Deva AK, Vickery K, et al. Detection of subclinical infection in significant breast implant capsules. Plast Reconstr Surg. 2003;111:1605–11. doi: 10.1097/01.PRS.0000054768.14922.44. [DOI] [PubMed] [Google Scholar]
- 37.Del Pozo JL, Tran NV, Petty PM, et al. Pilot study of association of bacteria on breast implants with capsular contracture. J Clin Microbiol. 2009;47:1333–7. doi: 10.1128/JCM.00096-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spear SL, Rottman SJ, Glicksman C, et al. Late seromas after breast implants: theory and practice. Plast Reconstr Surg. 2012;130:423–35. doi: 10.1097/PRS.0b013e3182589ea9. [DOI] [PubMed] [Google Scholar]
- 39.Arad E, Navon-Venezia S, Gur E, et al. Novel rat model of methicillin-resistant Staphylococcus aureus-infected silicone breast implants: a study of biofilm pathogenesis. Plast Reconstr Surg. 2013;131:205–14. doi: 10.1097/PRS.0b013e3182778590. [DOI] [PubMed] [Google Scholar]
- 40.Rieger U, Pierer G, Luscher M, et al. Sonification of removed breast implants for improved detection of subclinical infection. Aesthetic Plast Surg. 2009;33:404–8. doi: 10.1007/s00266-009-9333-0. [DOI] [PubMed] [Google Scholar]
- 41.Arciola CR, Campoccia D, Speziale P, et al. Biofilm formation in Staphylococcus implant infections. A review of molecular mechanisms and implications for biofilm-resistant materials. Biomaterials. 2012;33:5967–82. doi: 10.1016/j.biomaterials.2012.05.031. [DOI] [PubMed] [Google Scholar]
- 42.Reish RG, Lin A, Phillips NA, et al. Breast reconstruction outcomes after nipple-sparing mastectomy and radiation therapy. Plast Reconstr Surg. 2015;135:959–66. doi: 10.1097/PRS.0000000000001129. [DOI] [PubMed] [Google Scholar]
- 43.Momoh AO, Ahmed R, Kelley BP, et al. A systematic review of complications of implant-based breast reconstruction with prereconstruction and postreconstruction radiotherapy. Ann Surg Oncol. 2014;21:118–24. doi: 10.1245/s10434-013-3284-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carnevale A, Scaringi C, Scalabrino G, et al. Radiation therapy after breast reconstruction: outcomes, complications, and patient satisfaction. Radiol Med. 2013;118:1240–50. doi: 10.1007/s11547-013-0947-6. [DOI] [PubMed] [Google Scholar]
- 45.Lentz R, Ng R, Higgins SA, et al. Radiation therapy and expander-implant breast reconstruction: an analysis of timing and comparison of complications. Ann Plast Surg. 2013;71:269–73. doi: 10.1097/SAP.0b013e3182834b63. [DOI] [PubMed] [Google Scholar]
- 46.McCullough MC, Chu CK, Duggal CS, et al. Antibiotic prophylaxis and resistance after immediate tissue expander reconstruction of the breast. Ann Plast Surg. 2014;73:1–5. doi: 10.1097/SAP.0000000000000275. [DOI] [PubMed] [Google Scholar]
- 47.Spear S, Seruya M. Management of the infected or exposed breast prosthesis: a single surgeons’s 15 year experience with 69 patients. Plast Reconstr Surg. 2012;125:1074–84. doi: 10.1097/PRS.0b013e3181d17fff. [DOI] [PubMed] [Google Scholar]
- 48.Ota D, Fukuuchi A, Iwahira Y, et al. Identification of complications in mastectomy with immediate reconstruction using tissue expanders and permanent implants for breast cancer patients. Breast Cancer. 2014 doi: 10.1007/s12282-014-0577-4. ePub ahead of print. [DOI] [PubMed] [Google Scholar]
- 49.Hanwright PJ, Davila AA, Hirsch EM, et al. The differential effect of BMI on prosthetic versus autogenous breast reconstruction: a multivariate analysis of 12,986 patients. Breast. 2013;22:938–45. doi: 10.1016/j.breast.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 50.Chun YS, Sinha I, Turko A, et al. Outcomes and patient satisfaction following breast reconstruction with bilateral pedicled TRAM flaps in 105 consecutive patients. Plast Reconstr Surg. 2010;125:1–9. doi: 10.1097/PRS.0b013e3181c2a620. [DOI] [PubMed] [Google Scholar]