Abstract
Rehabilitation and nutrition are included in general and family medicine. Rehabilitation nutrition care process includes rehabilitation nutrition assessment and diagnostic reasoning, rehabilitation nutrition diagnosis, rehabilitation nutrition goal setting, rehabilitation nutrition intervention, and rehabilitation nutrition monitoring. I expect that many general and family physicians are interested in rehabilitation nutrition, sarcopenia, and sarcopenic dysphagia and prevent iatrogenic sarcopenia.

Rehabilitation and nutrition are included in general and family medicine. Of the 368 articles identified in the Journal of General and Family Medicine on May 17, 2017, 15 (4.1%) and 21 (5.7%) were retrieved by a search using “rehabilitation” and “nutrition”, respectively. In addition, six (1.6%) were retrieved by a search using “rehabilitation nutrition”. 1, 2, 3, 4, 5, 6 In a super‐aged society like Japan, the number of older people with sarcopenia, malnutrition, frailty, and disability has increased. Therefore, the importance of rehabilitation and nutrition in general and family medicine has also increased.
Rehabilitation nutrition is defined as that (i) evaluates holistically by the International Classification of Functioning, Disability and Health, and the presence and causes of nutritional disorders, sarcopenia, and excess or deficiency of nutrient intake; (ii) conducts rehabilitation nutrition diagnosis and rehabilitation nutrition goal setting; and (iii) elicits the highest body functions, activities, participations, and QOL by improving nutritional status, sarcopenia, and frailty using “nutrition care management in consideration of rehabilitation” and “rehabilitation in consideration of nutrition” in people with a disability and frail older people. High‐quality rehabilitation nutrition is provided by a rehabilitation nutrition care process (Figure 1).
Figure 1.
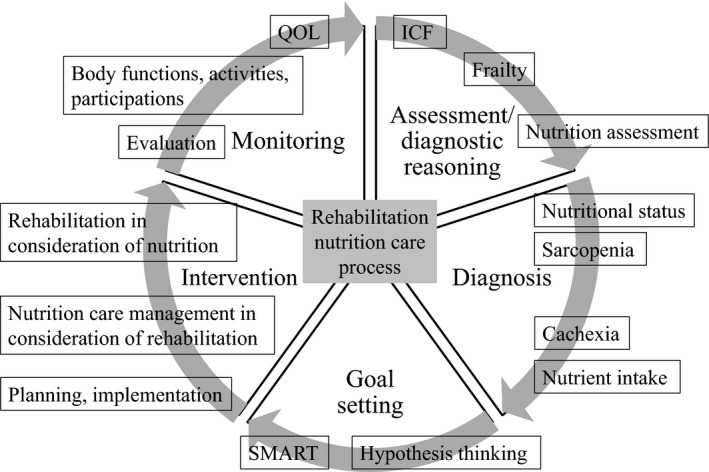
Rehabilitation nutrition care process. Rehabilitation nutrition care process includes rehabilitation nutrition assessment and diagnostic reasoning, rehabilitation nutrition diagnosis, rehabilitation nutrition goal setting, rehabilitation nutrition intervention, and rehabilitation nutrition monitoring. SMART means a goal that is specific, measurable, achievable, relevant, and time‐bound
Malnutrition is common in older hospitalized patients and affects poor outcome. Of 223 inpatients with hospital‐associated deconditioning, 202 patients (91%) were judged as being malnourished.1 In addition, patients with low hemoglobin level and low Onodera's prognostic nutritional index at referral to the department of rehabilitation medicine were more likely to have a poor rehabilitation outcome.1 In older patients with pneumonia, the number of days from the onset until the initiation of rehabilitation and nutritional status were independently associated with return to their activities of daily living.3 Of 177 patients admitted to a Japanese general medicine ward, 90 (51%) were malnourished assessed by the mini nutritional assessment short‐form, and those with malnutrition showed a high death rate and complication incidence rate.4 They were also difficult to early discharge from the hospital back to the patient's homes.4 Therefore, rehabilitation nutrition is recommended to improve clinical outcomes, including physical and swallowing function in older patients.6
Sarcopenia is characterized by a progressive and generalized loss of skeletal muscle mass and strength and is categorized into age‐, activity‐, nutrition‐, and disease‐related sarcopenia. Sarcopenia was included in the ICD‐10 in 2016 (Code; M62.84). Activity‐related sarcopenia results from prolonged bed rest, a sedentary lifestyle, or deconditioning. Nutrition‐related sarcopenia results from inadequate energy and/or protein intake. Disease‐related sarcopenia results from invasion (acute illness or injury) and/or cachexia (chronic illness). Age‐, activity‐, nutrition‐, and disease‐related sarcopenia can overlap in hospitalized patients that resulted in bedridden and sarcopenic dysphagia. Sarcopenic dysphagia is characterized by a loss of swallowing muscle mass and function associated with a generalized loss of skeletal muscle mass and function.
Iatrogenic sarcopenia is defined as sarcopenia caused by the activities of medical doctors, nurses, or other healthcare professionals in healthcare facilities. Iatrogenic sarcopenia includes activity‐related sarcopenia caused by unnecessary inactivity or bed rest, nutrition‐related sarcopenia caused by inappropriate nutritional care management, and disease‐related sarcopenia in cases of iatrogenic diseases. Iatrogenic sarcopenia due to activity‐ and nutrition‐related sarcopenia easily occurs in inpatients with aspiration pneumonia by tentative bed rest and nil per os at admission. However, iatrogenic sarcopenia due to unnecessary bed rest and noneating in hospitalized older people should be avoided, because swallowing function and activities of daily living deteriorated more by iatrogenic sarcopenia.
Sarcopenia should be treated by rehabilitation nutrition, because sarcopenia treatment differs depends on the etiology of sarcopenia. Rehabilitation and/or resistance training alone cannot treat nutrition‐related sarcopenia. Nutrition care management alone cannot treat activity‐related sarcopenia. Therefore, a comprehensive approach to treatment of sarcopenia and sarcopenic dysphagia should include rehabilitation such as resistance training, early ambulation, early oral intake, and nutrition care management. I expect that many general and family physicians are interested in rehabilitation nutrition, sarcopenia, and sarcopenic dysphagia and prevent iatrogenic sarcopenia.
CONFLICT OF INTEREST
The author have stated explicitly that there are no conflicts of interest in connection with this article.
REFERENCES
- 1. Wakabayashi H, Sashika H. Association of nutrition status and rehabilitation outcome in the disuse syndrome: a Retrospective Cohort Study. Gen Med 2011;12:69–74. [Google Scholar]
- 2. Murata K, Ishikawa S, Sugioka T. Investigation of dysphagia symptoms and their association with subjective symptoms in inhabitants of an Island. Gen Med 2013;14:32–9. [Google Scholar]
- 3. Goto R, Watanabe H, Tanaka N, Kanamori T, Yanagi H. Factors associated with recovery of activities of daily living in elderly pneumonia patients. Gen Med 2015;16:68–75. [Google Scholar]
- 4. Sato K. Mini Nutritional Assessment Short‐Form (MNA‐SF) predicts clinical outcomes: cohort study of small‐sized hospital in Japan. J Gen Fam Med 2016;17:90–8. [Google Scholar]
- 5. Tochino Y, Asai K, Shuto T, Hirata K. Asthma‐COPD overlap syndrome—Coexistence of chronic obstructive pulmonary disease and asthma in elderly patients and parameters for their differentiation. J Gen Fam Med 2017;18:5–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Momosaki R. Rehabilitative management for aspiration pneumonia in elderly patients. J Gen Fam Med 2017;18:12–5. [DOI] [PMC free article] [PubMed] [Google Scholar]


