Abstract
In 2016, gay, bisexual, and other men who have sex with men (MSM) comprise more than half of all new HIV diagnoses in the United States, with the primary mode of infection being condomless anal sex (CAS). While studies report an association between use of Internet-based social networking sites and increased CAS, the research on the relationship between cell phone mobile applications (e.g., Grindr, Scruff, Jack’d) and CAS is much less developed. The present study examines whether the manner in which gay, bisexual, and other MSM find sexual partners predicts an increase in likelihood of engaging in CAS in an urban, noncoastal U.S. city. Conducting a secondary data analysis of the 2011 National HIV Behavioral Surveillance survey for Denver (N = 546), the authors performed binary logistic regression analyses to assess the models that predict how MSM find sexual partners, and the odds of engaging in CAS. While the results suggest that age and race are associated with the mode of finding sexual partners, using the Internet or a mobile app to find sexual partners was not predictive of CAS (ZWald = .41, p = .52; ZWald = .80, p = .37). In terms of HIV prevention, these findings suggest a need for intervention to address HIV prevention on multiple levels (e.g., individual, group, community).
Keywords: HIV/AIDS, gay health issues, sexual health, sexuality, health promotion and disease prevention
HIV Prevalence Among MSM
In the United States, there are an estimated 1.2 million individuals living with the human immunodeficiency virus (HIV; Centers for Disease Control and Prevention [CDC], 2015). In 2014, there were approximately 44,073 new HIV infections (CDC, 2015). The HIV epidemic in the United States is considered a concentrated epidemic in which some populations of people are highly affected, and other populations are much less likely to be diagnosed with the virus. In the United States, those most often affected by HIV include gay, bisexual, and other men who have sex with men (MSM), persons who inject drugs, and high-risk heterosexuals (CDC, 2013).
MSM comprise the largest population of people affected by HIV/AIDS in the United States. While MSM represent about 4% of the adult U.S. population, MSM accounted for 67% of all new HIV diagnoses in 2014 (CDC, 2015). MSM diagnoses account for much of HIV diagnoses among all men living with HIV, comprising 83% of all newly diagnosed men in 2014 (CDC, 2015), and MSM account for most of the prevalence of HIV in the United States. In 2013, of those living with HIV, 57% were MSM (CDC, 2015). HIV transmission risks do not, however, accrue evenly across subpopulations within the MSM community, as new HIV diagnoses occur disproportionately in racial/ethnic minority groups. Between 2005 and 2014, HIV diagnoses among African American MSM rose by 22% and diagnoses among Latino/Hispanic MSM increased by 24% (CDC, 2015).
Colorado’s HIV epidemic mirrors that of the national HIV epidemiological profile. In 2013, there were 328 new HIV diagnoses in the state, of which 217 (66.2%) were individuals who were classified as MSM (Colorado Department of Public Health and Environment [CDPHE], 2015). Like national trends, Black and Hispanic MSM have disproportionate HIV diagnoses rates in Colorado (CDPHE, 2015). Black MSM comprised 11% of new HIV diagnoses from 2009 to 2013 but 4% of the population in the state, and Hispanic MSM comprised 28% of new diagnoses yet made up 21% of the population (CDPHE, 2015).
Risk Factors for HIV Among MSM
As described above, HIV diagnoses are highest among MSM in the United States. Several risk factors are associated with the overrepresentation of MSM who are HIV infected. First, it is estimated that half of all new HIV diagnoses are transmitted by persons unaware they are HIV positive (Hall, Holtgrave, & Maulsby, 2012), and approximately one quarter of all HIV-positive MSM have an undiagnosed infection (CDC, 2012). Behaviorally, the greatest HIV transmission risk for MSM is condomless receptive anal sex with an estimated transmission rate of 138 per 10,000 exposures (Patel et al., 2014), followed by condomless insertive anal sex with an estimated transmission rate of 11 per 10,000 exposures (Patel et al., 2014). Having a sexually transmitted infection (STI) also increases the likelihood of acquiring or transmitting HIV. Results of the 2014 National HIV Behavioral Surveillance (NHBS) survey reported 14% of HIV-positive-unaware MSM had syphilis (CDC, 2016b). Moreover, drug and alcohol use have been associated with risky sexual behavior among MSM (Vosburgh, Hansergh, Sullivan, & Purcell, 2012). While 46% of HIV-positive-unaware individuals reported binge drinking and 10% of HIV-positive-unaware MSM reported noninjection methamphetamine use (CDC, 2016b).
MSM and Internet Usage
With the increased popularity of the Internet and its use as a mechanism for finding relationship and sexual partners, it is not surprising than many MSM use the Internet in various forms to find potential sexual and romantic partners. A 2006 meta-analysis reported that 40% of MSM find their sexual partners using the Internet (Liau, Millett, & Marks, 2006), and among young MSM (YMSM), aged 18 to 24 years, 68% used the Internet in an attempt to find a sexual partner and 48% had actually met for sex with someone they met on the Internet (Garofalo, Herrick, Mustanski, & Donenberg, 2007). Different Internet sites are used for different types of interactions, and sexual partners may even be found on sites that are not expressly focused on dating or hookups (Mustanski, Lyons, & Garcia, 2011). While many YMSM attempt to find longer term relationship partners online, many are concerned that they will only be able to find short-term sexual partners through the Internet (Kubicek, Carpineto, McDavitt, Weiss, & Kipke, 2011).
As use of the Internet to find sexual partners has increased, researchers concerned with HIV and STI transmission and sexual risk taking have increased their focus on the Internet and its role in shaping sexual behaviors. Findings indicate that many Internet users are meeting their partners online (Bull & McFarlane, 2000), and a significant proportion of these individuals are demonstrating high-risk behaviors, such as choosing not to use condoms with their sexual partners when they meet up for real-time interactions (Benotsch, Kalichman, & Cage, 2002; McFarlane, Bull, & Rietmeijer, 2002). While some users are using the Internet to look for sexual partners in general, others are specifically using the Internet to find sexual partners who are interested in engaging in condomless anal sex (CAS), oftentimes referred to as “barebacking” (Carballo-Diéguez & Bauermeister, 2004; Halkitis & Parsons, 2003; Wilson et al., 2009).
Reports on risk-taking behaviors with sexual partners found through the Internet are mixed. While Klein (2009) found similar small proportions of men expressing unwillingness to ever use a condom or to allow their sexual partners to do so when comparing gay men (3.0%) and bisexual men (3.5%) who use the Internet to find sexual partners, the study also reported high rates of gay men and bisexual men willing to engage in receptive CAS (70.9% and 59.9%, respectively) and seeking to find receptive partners to engage in CAS (78.0% and 80.0%, respectively). Among YMSM who used the Internet to find sexual partners, while 48.0% actually met up for sex with someone they met online, only 53.0% reporting using condoms on consistent basis (Garofalo et al., 2007).
The number of sexual partners met online also appears to vary widely with one study finding that participants reported having had between 0 and 40 sexual partners that they had met via the Internet over the previous 3 months (Mustanski et al., 2011). While the type of sexual behavior being engaged in is critical to consider in terms of assessing risk, having large numbers of sexual partners is often considered one risk factor for HIV infection among MSM (Mustanski et al., 2011). Discussion of safer sexual practices has also been examined in a couple of research studies. Findings suggest that relatively few MSM hookup ads (8.8%) mention safe sex in the ad itself (Cheeseman, Goodlin-Fahncke, & Tewksbury, 2012) and condom use is seldom discussed during the online portion of communication (Mustanski et al., 2011). When it is discussed, it is most often done so after meeting in person (Mustanski et al., 2011).
Self-perceptions of risk do not always align with actual risky behaviors. Klein and Tilley (2012) reported that there was no correlation between gay and bisexual men’s self-assessment of their risk level for contracting HIV and the overall proportion of the time that they actually chose to practice safer sex. This same study reported that of those who considered their chance of contracting HIV to be low, moderate, or high, only 33.8%, 20.4%, and 18.9% consistently used condoms during anal sex with Internet partners, respectively (Klein & Tilley, 2012).
MSM Mobile Application Usage
The use of cell phones as the main mode of communication among American adults has grown significantly in the past decade. On average, over 93.0% of adults own a cell phone and of those, 67.0% of them use a smartphone or feature phone (Duggan & Brenner, 2013). These devices allow individuals to access the Internet and global positioning satellite technology to communicate with others nearby. In a study of smartphone ownership, the Pew Center reported that more than half of all smartphone owners use messaging applications or “apps” to communicate (Duggan, 2015).
Concomitantly, with the increased reliance on smartphones as a means of communication, there has been an increase in the use of these devices to find social and sexual partners, including among MSM (Grov, Breslow, Newcomb, Rosenberger, & Bauermeister, 2014). Grindr is one example of a geosocial networking application (GSN) that allows MSM to find other MSM near their current location to facilitate sexual relationships (PR Newswire, 2012). In the first 6 years since its establishment, Grindr has had more than 4 million users in 192 nations (PR Newswire, 2012). While Grindr may be one of the better known GSN apps used by MSM to facilitate connection with other MSM, a quick search finds numerous others that exist including Growlr, Scruff, Daddyhunt, Jack’d, Adam4Adam, Bro, Surge, Hornet, Hookd, and Recon. Many GSN apps focus on specific subpopulations among MSM. For example, Recon focuses on the fetish community, while Growlr targets the bear community.
While the body of literature on how the use of GSN apps facilitate sexual relationships and risky sexual behavior is still evolving, it is an emerging literature with important implications for HIV prevention. In a meta-analysis of technology utilization among MSM, Grov et al. (2014) reported that across several studies between 45% and 70% of MSM reported having sex with a partner they met using a mobile GSN application. There is a concern that because of the ease of locating a sexual partner using GSN apps, MSM may be more likely to engage in risky sexual behavior, similar to findings from studies of MSM and the utilization of the Internet to find sexual partners and the association with increased likelihood of CAS (Chng & Geliga-Vargas, 2000; Grosskopf, Harris, Wallace, & Nanin, 2011). Findings of frequent use of GSN to find sexual partners among MSM are fairly consistent with approximately half of respondents in numerous samples indicating having done so (YMSM, 46.1%, Landovitz et al., 2013; YMSM, 50.0%, Rice et al., 2012; MSM in New York, 45.0%, Phillips et al., 2014). The proportion engaging in CAS with a sexual partner found using a GSN vary from 28.0% (Phillips et al., 2014) to 70.0% (Landovitz et al., 2013). Comparing MSM who use GSN apps to find partners with MSM who found partners in other venues, Rice et al. (2012) reported participants who met using GSNs were actually more likely to use condoms than their counterparts who found partners in other ways. The discrepancy in findings and the unclear link between mobile GSN app usage to find sexual partners and CAS among MSM suggests the need for more research in this area to understand the impact of GSN apps on risky sexual behavior.
Research Question
While research has illustrated the prevalence of CAS among MSM using both the Internet and mobile applications, few comparative studies have demonstrated whether individuals are more or less likely to have CAS depending on the method through which MSM found a sexual partner. This study seeks to contribute to the literature by comparing modes of finding sexual partners and the prevalence of CAS. While much of the research on HIV among MSM in the United States has focused on the largest metropolitan areas, particularly those located on the East and West Coasts, less is known about HIV risks among MSM in noncoastal U.S. cities and in urban areas that are not among the largest 10 metropolitan areas. As such, this study contributes to the literature by examining these relationships in a less commonly explored urban context. In addition, the study seeks to determine which demographic and psychosocial factors predict increased likelihood of using Internet to find sexual partners, increased likelihood of using GSN apps to find sexual partners, and which predictors are associated with increased likelihood of engaging in CAS using any mode of finding sexual partners.
Method
National HIV Behavioral Surveillance
The NHBS is a CDC-funded behavioral surveillance system that conducts annual surveillance activities on a rotating cycle for three populations at high risk for acquiring HIV: MSM, people who inject drugs, and heterosexuals at increased risk for HIV infection. NHBS is conducted in 20 sites across the United States with high-HIV prevalence. The results from the survey are used to monitor prevalence and trends in HIV-related risks, testing behaviors, and access to HIV prevention services (Gallagher, Sullivan, Lansky, & Onorato, 2007). NHBS uses venue-based, time-space sampling following the national NHBS protocol, which identifies specific venues, times, and methods to recruit MSM. Listing all of the venues MSM attend, frequency of attendance, and time of attendance creates a venue universe. After construction of the venue universe, a systematic random selection occurs to structure when research staff will recruit and at which venue (Gallagher et al., 2007).
The Denver NHBS data was collected during the third MSM cycle, which occurred, between August and November 2011. During the data collection process, program staff approached men at venues to screen for eligibility and enroll individuals in the study. The inclusion criteria for NHBS includes being a resident of the Denver metropolitan area, being assigned a male sex at birth, being at least 18 years old, not having completed the interview in the current cycle, and having had sexual activity with another man during the past 12 months. The survey was available in both English and Spanish. After consenting to participate in the study, participants were enrolled in the study and offered HIV testing following the survey. Venues included bars, dance clubs, bathhouses, parks, and local grocery stores. The survey instrument was interviewer administered using a computer-assisted personal interview on handheld tablets. The behavioral survey included questions about sexual behavior, substance use, STI history, and HIV testing (Al-Tayyib et al., 2014).
Local Questions
In addition to the standardized behavioral survey administered across all participating NHBS sites, each individual site had the option to include supplemental questions. In the MSM cycle three, the local supplemental questionnaire included questions about preexposure prophylaxis (PrEP), a local syphilis prevention campaign, HIV testing, sexual partner characteristics, and using the Internet and/or mobile GSN applications to find sexual partners. The local questions about Internet and/or mobile GSN application usage to find sexual partners were used for this study to assess the risk behaviors of MSM who use the Internet and mobile applications to find sexual partners, which has become a prevalent mode of finding sexual partners for MSM (Grov et al., 2014; Liau et al., 2006).
In the questions used to assess usage of the Internet to find sexual partners and condom usage with those partners, participants were asked “Have you ever logged on the Internet to look for sexual partners?” and “Think about the most recent person you had sex with after meeting on the Internet. Did you use a condom for anal sex with that person?” In addition to the questions about the Internet, participants were asked to report their experiences using mobile GSN applications to find sexual partners. Participants were asked “Have you ever used a mobile application on a cell phone or smart phone that is primarily used to find romantic or sexual partners (e.g., Grindr, Scuff)?” and “Think about the most recent person you had sex with after meeting on a mobile application. Did you use a condom for anal sex with that person?” The response categories for questions about using either the Internet or mobile applications to look for sexual partners were dichotomous (yes/no) with the option for individuals to opt out of the question (refuse to answer). Similarly, a dichotomous response category (yes/no) was assigned to the question about having CAS with partners they met using either Internet or a mobile application, a response for opting out of the question (refuse to answer) and an additional option for individuals who did not have anal sex with the person they met for sex (did not have anal sex).
Analyses
Prior to inferential analysis, descriptive analysis was conducted. Logistic regressions were used to evaluate the relationships between (a) using the Internet to find sexual partners and engagement in CAS and (b) using a mobile application to find sexual partners and engagement in CAS. Multiple logistic regression models were also used to examine factors suggested by the literature to be predictors of HIV risk for MSM (i.e., race, alcohol use, drug use, use of PrEP, and HIV status) in three models to determine their relationship to (a) using the Internet to find a sexual partner, (b) using a mobile application to find sexual partners, and (c) the practice of CAS among MSM. Statistical analyses were conducted in SPSS (Version 23; IBM Corp. IBM SPSS Statistics for Windows, Armonk, NY). The study was approved by the institutional review board at the University of Denver.
Results
Descriptive Statistics
For cycle three of NHBS with MSM, 673 men were screened for the study. Of those, 546 (81.1%) men were eligible and completed both the core and local questionnaires. After excluding men who did not report having oral and/or anal sex with another man in the previous 12 months, the total sample size was 545 individuals. Of the total sample, 298 (54%) of the participants were White, 114 (20%) identified as Hispanic/Latino, 58 (10%) as Black/African American, 45 (8.3%) as Multiracial, 13 (2.4%) as American Indian/Alaskan Native, 12 (2%) as Asian, and 6 (0.2%) as Native Hawaiian/Pacific Islander. Because of sample sizes, in the analysis racial groups were recoded as Black, White, Latino, Multiracial, and other racial groups (which comprises American Indian/Alaskan Native, Asian, and Native Hawaiian/Pacific Islander).
The average age of participants was 36.81 years (SD = 12.37). A total of 403 (73.9%) participants had at least some postsecondary education, 320 (58.5%) were employed full-time, and 301 (57.25%) reported their relationship status as single. The largest percentage of participants fell into having a household income of $30000 to $40000, and over $75000 annually; however, 291 (53.4%) individuals in the sample earned less than $40000 per year. More than half, 428 (78.5%) of participants reported their HIV status as HIV-negative, with 71 (13%) MSM reporting their HIV status as HIV-positive; 302 (68.9%) of those who reported being HIV-negative reported they had been tested in the past 12 months. Less than a tenth, 46 (8.5%) participants had an unknown HIV status; which included individuals who did not obtain their HIV results, tested indeterminate, or refused to respond to the question. Most participants, 405 (74.3%) MSM reported having anal sex in the past 12 months (Table 1).
Table 1.
Demographic Characteristics of Men Enrolled in NHBS Study.
| Sample demographics (N = 546) | n | % |
|---|---|---|
| Race | ||
| African American/Black | 58 | 10.6 |
| Asian/Pacific Islander | 12 | 2.2 |
| Hispanic | 114 | 20.9 |
| American Indian | 13 | 2.4 |
| White | 298 | 54.6 |
| Multiracial | 45 | 8.2 |
| Age, years | ||
| 18-24 | 88 | 16.1 |
| 25-44 | 318 | 58.2 |
| 45-54 | 85 | 15.6 |
| 55-64 | 37 | 6.8 |
| 65 and older | 18 | 3.3 |
| Education | ||
| Less than 12 years | 17 | 3.1 |
| High school or GED | 125 | 22.9 |
| Some college | 193 | 35.3 |
| College graduate | 146 | 26.7 |
| Postgraduate degree | 64 | 11.7 |
| Relationship status | ||
| In a monogamous relationship | 127 | 23.3 |
| In an open relationship | 63 | 11.5 |
| Causally dating | 55 | 10.1 |
| Single | 301 | 55.1 |
| Income | ||
| Under $10,000 | 67 | 12.3 |
| $10,000 to $19,999 | 67 | 12.3 |
| $20,000 to $29,999 | 73 | 13.4 |
| $30,000 to $39,999 | 84 | 15.4 |
| $40,000 to $49,999 | 51 | 9.3 |
| $50,000 to $59,999 | 47 | 8.6 |
| $60,000 to $75,000 | 43 | 7.9 |
| Over $75,000 | 84 | 15.4 |
| HIV status | ||
| Negative | 428 | 78.5 |
| Positive | 71 | 13 |
| Do not know or unaware | 46 | 8.4 |
| HIV test in the past 12 months | ||
| Yes | 302 | 68.9 |
| No | 131 | 29.9 |
| Unknown HIV status | 5 | 1.1 |
| Ever used preexposure prophylaxis | ||
| Yes | 2 | 0.4 |
| No | 468 | 85.9 |
| Unknown | 75 | 13.8 |
| Internet use to find sex partner | ||
| Yes | 294 | 53.9 |
| No | 232 | 42.6 |
| Mobile app use to find sex partner | ||
| Yes | 171 | 31.4 |
| No | 355 | 65.1 |
| Used both Internet/mobile app to find sex partner | ||
| Yes | 145 | 26.6 |
| No | 381 | 69.9 |
Note. NHBS = National HIV Behavioral Surveillance.
Internet and CAS
More than half, 294 (53.9%) MSM reported using the Internet to look for a sex partner. Of those individuals, 149 (50.7%) MSM used only the Internet to look for sex. While previous literature suggests that using the Internet is associated with an increased likelihood of engagement in CAS among MSM, in this study, using the Internet to find a sexual partner was not a statistically significant predictor of CAS at the bivariate level (Wald = 0.41, p = .52). In evaluating the demographical and psychosocial factors associated with using the Internet to find a sexual partner, age, age-squared, and race (Multiracial and Hispanic/Latino) were statistically significant predictors of using the Internet to find a sexual partner. Initial investigation of the data suggested that the relationship between age and likelihood of CAS was quadratic and, as such, the squared term was included to capture the nonlinear relationship. As age increased, participants through age 40 were 1.1 times more likely to report using the Internet to find a sexual partner for each year increase (Wald = 6.04, p = .01) after which likelihood decreases significantly. The quadratic relationship between age and use of Internet to find sexual partners is illustrated in Figure 1.
Figure 1.
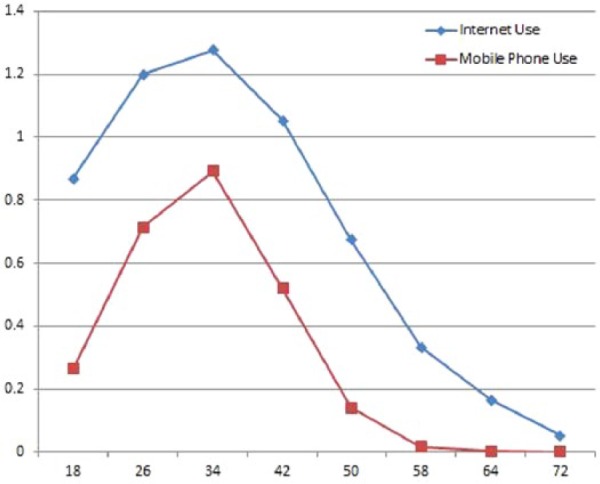
Curvilinear relationship between age and likelihood of using Internet or GSN mobile phone app to identify sexual/romantic partners among MSM in [Locale].
Note. GSN = geosocial networking application; MSM = men who have sex with men.
Racially, both Multiracial and Hispanic/Latino participants were statistically less likely to use the Internet to find sexual partners than White participants. Multiracial participants were 0.43 times and Hispanic/Latino participants were 0.56 times less likely to report using the Internet to find sexual partners (Wald = 4.83, p = .03 and Wald = 0.504, p = .03, respectively). There were no statistically significant relationships between alcohol use, drug use, using PrEP, and HIV status and likelihood of using the Internet to find a sexual partner.
Mobile Applications and CAS
Roughly, one third, 171 (31.4%) MSM reported using a mobile application to find a sex partner. Of those who used a mobile application to find a sex partner, 26 (15.2%) MSM only used a mobile application to find a sex partner. Like the results of the relationship between Internet usage and CAS, using a mobile application to find a sexual partner was not a statistically significant predictor of CAS at the bivariate level (Wald = 0.80, p = .37). Examining the demographical and psychosocial factors associated with likelihood of using a mobile application to find sexual partners, there were statistically significant relationships between age, age squared, and alcohol use, and the likelihood of using a mobile application to find a sexual partner. As age increased, individuals through age 40 were 1.4 times more likely to use a mobile app to find a sexual partner for each year increase (Wald = 17.30, p < .001) after which likelihood of using a mobile application to find a sexual partner decreased (Wald = 19.52, p <.001). The quadratic relationship is illustrated in Figure 1.
Individuals who reported alcohol use were 0.40 times less likely to use a mobile application to find a sexual partner (Wald = 4.33, p = .04) than those that did not report alcohol use (Table 2). There were no statistically significant relationships between drug use, using PrEP and HIV status, and using a mobile app to find a sexual partner.
Table 2.
Multivariate Logistic Regression for Predictors of Using the Internet or GSN App to Find Sexual Partners.
| Internet |
GSN app |
|||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Age | 1.14* | [1.03, 1.26] | 1.47*** | [1.23, 1.77] |
| Age squared | 1.0** | [0.99, 1.00] | 0.99*** | [0.992, 0.997] |
| Black | 0.66 | [0.34, 1.27] | 0.64 | [0.30, 1.35] |
| Multiracial | 0.43* | [0.20, 0.91] | 0.81 | [0.35, 1.84] |
| Latino | 0.56* | [0.33, 0.93] | 0.75 | [0.43, 1.30] |
| Other race | 1.37 | [0.49, 3.84] | 1.75 | [0.60, 5.10] |
| Alcohol | 0.49 | [0.22, 1.10] | 0.40* | [0.17, 0.95] |
| Drug use | 0.99 | [0.65, 1.50] | 0.30 | [0.50, 1.24] |
| HIV-positive | 0.68 | [0.14, 3.20] | 1.20 | [0.21, 6.70] |
Note. GSN = geosocial networking application; OR = odds ratio; CI = confidence interval.
p < .05. **p < .01. ***p < .001.
Predictors of CAS
In the final model, we examine whether demographical and psychosocial factors, using the Internet to find sexual partners, and using a mobile application to find sexual partners were predictive of engagement in CAS. In the multivariate context, only racial identity (Hispanic/Latino and other race) was statistically significant in predicting CAS among MSM. Hispanic/Latino MSM were 0.46 times less likely to engage in CAS than their White counterparts (Wald = 6.44, p < .05). Individuals who fell into the “other” racial group (American Indian/Alaskan Native, Asian, and Native Hawaiian/Pacific Islander) were 0.35 times less likely to report engagement in CAS (Wald = 5.94, p < .05) than White MSM. Age, age squared, alcohol use, drug use, PrEP use, and HIV status were not statistically significant factors associated with CAS among MSM in this study (Table 3). Additionally, neither use of the Internet nor use of a mobile application to find sexual partners were associated with increased or decreased likelihood of engaging in CAS compared with using other venues for finding sexual partners.
Table 3.
Multivariate Logistic Regression for Predictors of Condomless Anal Sex Among MSM.
| OR | 95% CI | |
|---|---|---|
| Age | 1.02 | [0.90, 1.15] |
| Age squared | 1.00 | [0.99, 1.00] |
| Black | 0.88 | [0.41, 1.87] |
| Multiracial | 0.99 | [0.39, 2.49] |
| Latino | 0.46* | [0.25, 0.84] |
| Other race | 0.27* | [0.09, 0.81] |
| Alcohol | 1.60 | [0.60, 4.19] |
| Drug use | 1.15 | [0.70, 1.90] |
| Mobile app | 0.65 | [0.37, 1.14] |
| Internet | 1.10 | [0.65, 1.86] |
Note. MSM = men who have sex with men; OR = odds ratio; CI = confidence interval.
p < .05. **p < .01. ***p < .001.
Discussion and Implications
As virtual modes of communication have become prominent avenues for MSM to meet other MSM for social and sexual interactions, this study sought to investigate whether method of finding sexual partners was associated with likelihood of engagement in CAS among MSM. The current study, one of the first studies to comparatively examine risky sexual behavior among MSM across virtual platforms in Denver, asked individuals to report their utilization of the Internet and GSN apps to find sexual partners, and their sexual practices when engagement in anal sex with partners they met using each method.
The sample consisted of MSM throughout the metro area and was conducted with face-to-face interaction instead of recruiting participants using the Internet or GSN apps. The participants in the study tended to be middle aged, identified as White, and were well educated. These characteristics are representative of the population of MSM in Denver. The findings are consistent with previous studies, which have investigated the role of Internet or GSN usage for meeting potential sexual partners, with a similar percentage of MSM reporting using the Internet or a GSN to find a sexual partner (Garofalo et al., 2007; Grosskopf, LeVasseur, & Glaser., 2014; Grov et al., 2014; Landovitz et al., 2013). The current study found that over half (53.9%) of the participants reported the use of the Internet to find potential sexual partners, and one third (31.4%) reported the use of a mobile GSN app to find a potential sexual partner. Utilization of the Internet and GSN apps to find sexual partners were more prevalent among younger MSM (up to age 40) and those who identified racially as White.
Some scholars have suggested that because the Internet and GSN apps provide MSM with more efficient ways to find sexual partners in a closer proximity than traditional methods of finding sexual partners (i.e., bars and public spaces), it is more likely to facilitate higher risk sexual behavior (Benotsch et al., 2002; Garofalo et al., 2007; Grosskopf et al., 2014; Grov et al., 2014; Landovitz et al., 2013). A majority of participants reported utilization of condoms for anal sex with partners they met using the Internet (58.2%) and GSN apps (59.1%). In fact, the current study’s findings indicate that the mode which an individual used to find a sexual partner was not a statistically significant predictor of condom use. These findings are similar to recent findings about mobile app utilization by MSM in other locations (Phillips et al., 2014; Rice et al., 2012).
These findings suggest that although MSM may use Internet and GSN apps expressly to seek sexual partners, there may be few differences in the level of sexual risk taken using these mediums compared with using traditional methods of finding sexual partners. Virtual forms of communication may provide greater access to potential sexual partners, and these results suggest that Internet and mobile GSN app social networking may simply be an extension of traditional forms of finding sexual partners, and not present greater challenges for HIV prevention with regard to risk-taking behavior among MSM. Moreover, the findings suggest a potential direction for HIV prevention that capitalizes on modern forms of communication. The rapid advancements in technology and an increase in MSM using these newer modes of communication to seek potential sexual partners necessitate the need for HIV prevention interventions to adopt Internet and mobile app messages.
Research and Intervention Implications
One challenge with much of the research examining sexual risk is that questions regarding the participant’s latest partners may ask about safer sex, how they met, and whether they were casual or significant, but do not go any further in depth. A person may have a casual partner with whom they are monogamous, or have met partner (casual or significant) on the Internet or an app months or even years previously. Additionally, those in polyamorous or consensually nonmonogamous relationships may have different guidelines around choices for safer sex, testing, and search for partners. Future research should include more nuanced questions regarding relationship status of each recent partner to more deeply understand these experiences.
One challenge in discussing HIV prevention/interventions as part of the online sexual and dating website context is the disparity between the views of the website users and the website owners, as well as between HIV/STD clinic directors and the website owners. While both HIV/STD clinic directors and website users support inclusion of seven different potential interventions as part of MSM-specific dating and/or hook up websites, the owners of the websites themselves do not support including these interventions (Wohlfeiler et al., 2013). Conversely, the same study reported that the three interventions that garnered support from the website owners had little enthusiasm in the response from the website users, indicating an incongruence in the views of these two groups. Given that 88.0% of YMSM are using the Internet to find information on HIV/AIDS (Mustanski et al., 2011), the incongruence between view of users and website owners remains a barrier to effective prevention efforts.
Another constraint with current HIV prevention efforts to interface with MSM using the Internet or GSN apps is low utilization of standalone HIV prevention websites and HIV GSN apps (Grov et al., 2014; Holloway et al., 2014). Future research should examine the feasibility of partnership with social networking platforms to reach MSM using existing Internet social networking websites and GSN apps to engage in HIV prevention interventions. Utilization of technology continues to be an avenue that is dominated by younger individuals. The recent increase of HIV infections among 13- to 25-year-old YMSM suggest that this avenue may also be a consideration for HIV preventions efforts to reach a younger group of MSM. Research should focus on the design of appropriate studies to assess the need for HIV prevention programming that targets younger MSM using technological advances, as well as evaluate the capacity and cost effectiveness of such programs to reduce HIV infections among this age group. The use of the Internet and mobile applications varies by subgroups of MSM racially; therefore, future research should investigate the racial difference in the utilization and risky sexual behavior by racial identity for MSM. Subsequently, research is needed to determine the necessity and acceptability for prevention interventions that address the differences in these factors, especially because HIV incidence MSM varies by racial identity as a way to reduce HIV incidence among racial/ethnic minority groups of MSM.
Limitations
The current study supports existing research that suggest the mode in which MSM find potential sexual partners is not associated with riskier sexual behavior. However, there are some limitations. One weakness of the study is the sampling strategy and data collection methodology. NHBS uses venue-based, time-space sampling which creates sampling bias. Participants were recruited in venues that target gay and bisexual men who openly identify as gay or bisexual. This bias reduces the likelihood of including individuals who may engage in high-risk MSM behavior but do not identify as MSM. In addition, the sample is limited to individuals who access these venues at the specific time recruitment is occurring, therefore depending on the designated time frame, the sample may not be reflective of the larger population of MSM because it only includes MSM who access the venues identified or access to venues during the times data collection occurred. While the demographics of the sample appear similar to the demographics of the MSM population in Denver, it may not represent the overall demographic of MSM at greatest risk for HIV infection using epidemiological data. The data for this study were drawn from one geographic area and may not be representative or generalizable to the larger MSM community in the United States. In addition, the data collection did not include transgender MSM, and there is a need for future research that includes this population.
Another limitation of the study is the use of an interviewer-administered computer-assisted personal interview, which introduces the potential for social desirability bias among the respondents because the primary data were collected by the Denver Health Department. Future studies should consider using a self-administered questionnaire, as research suggests MSM are more accurate in responding to questions about sexual behavior when this data collection protocol is used (Daley, McDermott, McCormack Brown, & Kittleson, 2003). Finally, this sample only included cisgender (nontransgender) MSM. Given that transgender people of all genders are at higher risk for HIV (CDC, 2016a), and transgender MSM are at an increased risk for becoming infected with HIV (Rowniak, Chesla, Rose, & Holzemer, 2011), future studies should include this group.
Conclusion
The findings from this study suggest that age and race are both associated with mode of finding sexual partners, while using the Internet or GSN applications to find a sexual partner was not significantly associated with engaging in CAS. These results support previous research indicating that mode of sexual partner selection is not correlated with having CAS. Given these results, there is a call for further research regarding racial differences in HIV predictors of risk, and a demonstrated need for interventions that not only make use of the Internet and mobile applications regarding HIV prevention and dialogue but specifically interventions that address multiple risk factors for HIV infection among MSM. Interventions should be tailored to meet the needs for specific risk groups including men who are younger, who engage in using mobile apps, and men who may not use traditional methods of obtaining information.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Al-Tayyib A., Thurn M. W., Haukoos J. S., Walls N. E. (2014). Knowledge of pre-exposure prophylaxis (PrEP) for HIV prevention among men who have sex with men in Denver, Colorado. AIDS and Behavior, 18(3 Suppl.), 340-347. doi: 10.1007/s10461-013-0553-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benotsch E. G., Kalichman S., Cage M. (2002). Men who have met sex partners via the Internet: Prevalence, predictors, and implications for HIV prevention. Archives of Sexual Behavior, 31, 177-183. doi: 10.1023/A:1014739203657 [DOI] [PubMed] [Google Scholar]
- Bull S. S., McFarlane M. (2000). Soliciting sex on the Internet: What are the risks for sexually transmitted diseases and HIV? Sexually Transmitted Diseases, 27, 545-550. [DOI] [PubMed] [Google Scholar]
- Carballo-Diéguez A., Bauermeister J. (2004). “Barebacking”: Intentional condomless anal sex in HIV-risk contexts: Reasons for and against it. Journal of Homosexuality, 47(1), 1-16. doi: 10.1300/J082v47n01_01 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2012). Diagnoses of HIV infection and AIDS among adolescents and young adults in the United States and 5 U.S. dependent areas, 2006–2009. HIV Surveillance Supplemental Report, 17(2). [Google Scholar]
- Centers for Disease Control and Prevention. (2013). Rates of diagnoses of HIV infection among adults and adolescents, by area of residence, 2011—United States and 6 dependent areas. HIV Surveillance Report, 23. [Google Scholar]
- Centers for Disease Control and Prevention. (2015). Diagnoses of HIV infection in the United States and dependent areas, 2014. HIV Surveillance Report, 26 Retrieved from https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-us.pdf [Google Scholar]
- Centers for Disease Control and Prevention. (2016. a). HIV among transgender people. Retrieved from https://www.cdc.gov/hiv/group/gender/transgender/
- Centers for Disease Control and Prevention. (2016. b). HIV infection risk, prevention, and testing behaviors among men who have sex with men: National HIV Behavioral Surveillance, 20 US cities, 2014. HIV Surveillance Special Report, 15 Retrieved from https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-hssr-nhbs-msm-2014.pdf [Google Scholar]
- Cheeseman K., Goodlin-Fahncke W., Tewksbury R. (2012). “Looking for a married hookup”: An examination of personal ads posted by men seeking sex with married men. Journal of Men’s Studies, 20, 144-157. doi: 10.3149/jms.2002.144 [DOI] [Google Scholar]
- Chng C. L., Geliga-Vargas J. (2000). Ethnic identity, gay identity, sexual sensation seeking and HIV risk taking among multiethnic men who have sex with men. AIDS Education and Prevention, 12, 326-329. [PubMed] [Google Scholar]
- Colorado Department of Public Health and Environment. (2015). HIV and AIDS in Colorado: HIV/AIDS epidemiology annual report for cases diagnosed through December 2013. Denver, CO: Author. [Google Scholar]
- Daley E. M., McDermott R. J., McCormack Brown K. R., Kittleson M. J. (2003). Conducting Web-based survey research: A lesson in Internet designs. American Journal of Health Behavior, 27, 116-124. doi: 10.5993/AJHB.27.2.3 [DOI] [PubMed] [Google Scholar]
- Duggan M. (2015). Mobile messaging and social media 2015. Washington, DC: Pew Research Center. [Google Scholar]
- Duggan M., Brenner N. (2013). The demographics of social media users: 2012. Washington, DC: Pew Research Center. [Google Scholar]
- Gallagher K. M., Sullivan P. S., Lansky A., Onorato I. M. (2007). Behavioral surveillance among people at risk for HIV infection in the U.S.: The National HIV Behavioral Surveillance System. Public Health Reports, 122(Suppl. 1), 32-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R., Herrick A., Mustanski B. S., Donenberg G. R. (2007). Tip of the iceberg: Young men who have sex with men, the Internet, and HIV risk. American Journal of Public Health, 97, 1113-1117. doi: 10.2105/AJPH.2005.075630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosskopf N. A., Harris J. K., Wallace B. C., Nanin J. E. (2011). Online sex-seeking behaviors of men who have sex with men in New York City. American Journal of Men’s Health, 5, 378-385. [DOI] [PubMed] [Google Scholar]
- Grosskopf N. A., LeVasseur M. T., Glaser D. B. (2014). Use of the Internet and mobile-based “apps” for sex-seeking among men who have sex with men in New York City. American Journal of Men’s Health, 8, 510-520. doi: 10.1177/1557988314527311 [DOI] [PubMed] [Google Scholar]
- Grov C., Breslow A. S., Newcomb M. G., Rosenberger J. G., Bauermeister J. A. (2014). Gay and bisexual men’s use of the Internet: Research from the 1990s through 2013. Journal of Sex Research, 51, 390-409. doi: 10.1080/00224499.2013.871626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis P. N., Parsons J. T. (2003). Intentional unsafe sex (barebacking) among HIV-positive gay men who seek sexual partners on the Internet. AIDS Care, 15, 367-378. [DOI] [PubMed] [Google Scholar]
- Hall H. I., Holtgrave D. R., Maulsby C. (2012). HIV transmission rates from persons living with HIV who are aware and unaware of their infection. AIDS, 26, 893-896. [DOI] [PubMed] [Google Scholar]
- Holloway I., Dunlap S., del Pino H. E., Hermanstyne K., Pulsipher C., Landovitz R. (2014). Online social networking, sexual risk and protective behaviors: Considerations for clinicians and researchers. Current Addictions Report, 1, 220-228. doi: 10.1007/s40429-014-0029-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein H. (2009). Differences in HIV risk practices sought by self-identified gay and bisexual men who use Internet websites to identify potential sexual partners. Journal of Bisexuality, 9, 125-140. doi: 10.1080/15299710902881533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein H., Tilley D. L. (2012). Perceptions of HIV risk among Internet-using, HIV-negative barebacking men. American Journal of Men’s Health, 6, 280-293. doi: 10.1177/1557988311434825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubicek K., Carpineto J., McDavitt B., Weiss G., Kipke M. D. (2011). Use and perceptions of the Internet for sexual information and partners: A study of young men who have sex with men. Archives of Sexual Behavior, 40, 803-816. doi: 10.1007/s10508-010-9666-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landovitz R. J., Tseng C. H., Weissman M., Haymer M., Mendenhall B., Rogers K., … Shoptaw S. (2013). Epidemiology, sexual risk behavior, and HIV prevention practices of men who have sex with men using GRINDR in Los Angeles, California. Journal of Urban Health, 90(4), 729-739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liau A., Millett G., Marks G. (2006). Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sexually Transmitted Diseases, 33, 576-584. doi: 10.1097/01.olq.0000204710.35332.c5 [DOI] [PubMed] [Google Scholar]
- McFarlane M., Bull S. S., Rietmeijer C. A. (2002). Young adults on the Internet: Risk behaviors for sexually transmitted diseases and HIV. Journal of Adolescent Health, 31, 11-16. doi: 10.1016/S1054-139X(02)00373-7 [DOI] [PubMed] [Google Scholar]
- Mustanski B., Lyons T., Garcia S. C. (2011). Internet use and sexual health of young men who have sex with men: A mixed-methods study. Archives of Sexual Behavior, 40, 289-300. doi: 10.1007/s10508-009-9596-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel P., Borkowf C. B., Brooks J. T., Lasry A., Lansky A., Mermin J. (2014). Estimating per-act HIV transmission risk: A systematic review. AIDS, 28, 1509-1519. doi: 10.1097/QAD.0000000000000298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips G., Magnus M., Kuo I., Rawls A., Peterson J., Jia Y., . . . Greenberg A. E. (2014). Use of geosocial networking (GSN) mobile phone applications to find men for sex by men who have sex with men (MSM) in Washington, DC. AIDS Behavior, 18, 1630-1637. doi: 10.1007/s10461-014-0760-9 [DOI] [PubMed] [Google Scholar]
- PR Newswire. (2012). Happy birthday, Grindr! 3 years: 3.5 Million users. 192 countries, and growing. Retrieved from http://www.prnewswire.com/news-releases/happy-birthday-grindr-3-years-35-million-users-192-countries-and-growing-144262325.html
- Rice E., Holloway I., Winetrobe H., Rhoades H., Barman-Adhikari A., Gibbs J., . . . Dunlap S. (2012). Sex risk among young men who have sex with men who use Grindr, a smartphone geosocial networking application. Journal of AIDS & Clinical Research, 3(Suppl. 4), 005. doi: 10.4172/2155-6113.S4-005 [DOI] [Google Scholar]
- Rowniak S., Chesla C., Rose C. D., Holzemer W. L. (2011). Transmen: The HIV risk of gay identity. AIDS Education and Prevention, 23, 508-520. doi: 10.1521/aeap.2011.23.6.508 [DOI] [PubMed] [Google Scholar]
- Vosburgh H. W., Hansergh G., Sullivan P. S., Purcell D. W. (2012). A review of the literature on event-level substance use and sexual risk behavior among men who have sex with me. AIDS Behavior, 16, 1394-1410. [DOI] [PubMed] [Google Scholar]
- Wilson P. A., Valera P., Ventuneac A., Balan I., Rowe M., Carballo-Diéguez A. (2009). Race-based sexual stereotyping and sexual partnering among men who use the Internet to identify other men for bareback sex. Journal of Sex Research, 46, 399-413. doi: 10.1080/00224490902846479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wohlfeiler D., Hecht J., Volk J., Raymond H. F., Kennedy T., McFarland W. (2013). How can we improve online HIV and STD prevention for men who have sex with men? Perspectives of hook-up website owners, website users, and HIV/STD directors. AIDS and Behavior, 17, 3024-3033. doi: 10.1007/s10508-010-9666-4 [DOI] [PMC free article] [PubMed] [Google Scholar]


