Abstract
Despite the importance of healthy settings for health promotion, little is known about how neighborhood characteristics affect men’s health. The present study aims to explore the associations between perceptions of home and workplace neighborhoods with diverse health outcomes, and to examine mediating mechanisms. A sample of 669 men members of labor unions in Quebec, Canada, completed a questionnaire assessing social and physical aspects of their work and home neighborhoods (the Health-Promoting Neighborhood Questionnaire) as well as subjective and objective health outcomes (perceived health, positive mental health, body mass index) and potential mediators (health behaviors, self-efficacy). Structural equation modeling (path analysis) revealed that the Health-Promoting Neighborhood Questionnaire was associated with all three health outcomes, either directly or indirectly through health behaviors and self-efficacy. Both home and workplace neighborhoods were associated with men’s health, home neighborhood being more strongly associated. The findings suggest that physical and social aspects of neighborhood might contribute to men’s health. The study highlights positive environmental levers for urban planners, policy makers, and health professionals to promote men’s health.
Keywords: neighborhood, workplace, positive mental health, health behaviors, health self-efficacy
Men are a population with documented health challenges (Gough, 2013; Robertson, Galdas, McCreary, Oliffe, & Tremblay, 2009). Studies report that men have lower life expectancy (Statistics Canada, 2012b), higher suicide rates (Nock et al., 2008), lower probability of consulting a general practitioner (Y. Wang, Hunt, Nazareth, Freemantle, & Petersen, 2013), less healthy lifestyles (Von Bothmer & Fridlund, 2005), and lower subjective well-being (Inglehart, 2002). Since 2000, men’s health has received increasing attention (Courtenay, 2011). Many studies have examined the association between neighborhood characteristics and health or well-being with mixed-gender samples (Bond et al., 2012; Eriksson & Emmelin, 2013; Gale, Dennison, Cooper, & Sayer, 2011; Meijer, Röhl, Bloomfield, & Grittner, 2012). However, gender specificities concerning those associations are understudied (Stafford, Cummins, Macintyre, Ellaway, & Marmot, 2005). Studies with men are needed to enable urban planners and policy makers to design environments that support men’s health.
Association Between Neighborhood Characteristics and Health
First, the distinction between subjective and objective aspects of neighborhood environment is important to consider. According to Marans (2003), the true quality of a setting should not be judged by its objective characteristics, but rather by the users’ perceptions. Measures of environmental perceptions are more closely linked to health than objective environmental characteristics (Weden, Carpiano, & Robert, 2008). Numerous efforts have been made to identity and classify the perceived characteristics of one’s neighborhood that influence health. In a qualitative research with 28 participants in Northern Sweden (Eriksson & Emmelin, 2013), the following themes emerged as positively influencing health: support between neighbors, good location, greenness, and proximity to essential places. Men also named sense of belonging and countryside lifestyle, the latter considered by participants to promote outdoor activity and socialization. Eriksson and Emmelin’s (2013) results align with those of a review of studies conducted in the past 30 years on environmental qualities (Bonaiuto & Alves, 2012). According to this review, residents’ perceptions of their neighborhood can be regrouped in four main areas: space (e.g., aesthetics, green areas), people (e.g., security, sociability), services (e.g., shops, transport), and context (e.g., pace of life, upkeep).
Findings on the association between neighborhood characteristics and men’s health are mixed. Several studies support the conclusion that, in comparison with women, men are more influenced by the physical aspects of neighborhood environment (e.g., quality of outdoor air, solid waste, or trash disposal) and less by social quality (e.g., crime, access to health care, homelessness; Berke, Gottlieb, Moudon, & Larson, 2007; Molinari, Ahern, & Hendryx, 1998; Mullings, McCaw-Binns, Archer, & Wilks, 2013). Other studies highlight the importance of social components of neighborhood even for men (Saarloos, Alfonso, Giles-Corti, Middleton, & Almeida, 2011). In a qualitative study, no overall difference was identified between men and women participants on ratings of the importance of social and physical neighborhood conditions for mental well-being (Burke, O’Campo, Salmon, & Walker, 2009).
The majority of research on the association between health and neighborhood has focused on the home area. Research on workplace neighborhood is scarce. Although people spend approximately two thirds of their time at home, they also spend much of the last third at work (European Communities, 2004). Workplace area is thus one of the few primary settings in one’s life. A study with a sample of school teachers, including a minority of men (21%), has reported an association between work neighborhood socioeconomic status and alcohol consumption after controlling for the status of their residential neighborhood (Virtanen et al., 2007). Another study with a mixed-gender sample (49% men) examined home and workplace neighborhoods (K. Moore et al., 2013), underlining that features of both environments were associated with body mass index (BMI). To our knowledge, no study on men’s health has ever looked at the association with workplace neighborhood. Exploring this question would be important, especially since men spend more time in the workplace than women (European Communities, 2004).
Finally, most studies concerning neighborhood and health have focused on environmental disorder and neighborhood contribution to health problems. Yet, according to the World Health Organization (1946, p. 1), health is “not merely the absence of disease or infirmity.” Keyes (2002) proposed a complete model of mental health that goes beyond the absence of psychopathology, including indicators of positive mental health such as emotional, psychological, and social well-being. This perspective can be extended to incorporate positive physical functioning indicators (e.g., physical status) and biological variables (e.g., BMI; Grzywacz & Keyes, 2004; Seligman, 2008). A multidimensional approach encompassing both positive and negative aspects of mental and physical well-being is needed.
Potential Mediators of Neighborhood Association With Health
As noted by Galster (2012), there is no empirical consensus on the causal paths between neighborhood and individual outcomes. Several studies on neighborhood and health, with samples including both men and women, have considered individual health behaviors (e.g., healthy diet, physical activity, nurturing of interpersonal relationships) as key mediators (Diez Roux & Mair, 2010). However, results are inconsistent. Poortinga (2006) reported only limited support for a mediating role of health behaviors in the association between community social capital and self-rated health. In contrast, Auchincloss, Diez Roux, Brown, Erdmann, and Bertoni (2008) identified that resources for physical activities and healthy food in the neighborhood were associated with lower insulin resistance, an effect partly mediated by physical activity and diet. Kruger, Reischl, and Gee (2007) provided empirical evidence that neighborhood deterioration is associated with well-being, an association mediated by level of social contact. Each of these studies has considered only one or a limited number of health behaviors, rendering it difficult to test the mediating role of health behaviors from a global perspective.
Health self-efficacy is another possible mediator. According to Ajzen’s (1991) theory of planned behavior, one’s behavior depends not only on the intention to perform a behavior but also on perceived control. This derives from having the necessary opportunities and resources. Scores on health efficacy scales have been associated with health behaviors and better health outcomes (Dempster & Donnelly, 2008; Jackson, Tucker, & Herman, 2007). It is plausible that health-promoting neighborhoods favor a sense of control over health by providing opportunities for healthy behaviors. Such reasoning has been supported for a few health behaviors (e.g., Bromell, 2011; Erinosho et al., 2012; McNeill, Wyrwich, Brownson, Clark, & Kreuter, 2006). However, it has never been studied with a focus on men’s health.
Objectives
The goal of the present study is to explore the associations between neighborhood and men’s health. Two objectives are pursued: (1) to examine the associations between home and workplace neighborhoods and men’s health (perceived health, positive mental health, BMI) and (2) to explore cognitive and behavioral health processes mediating these associations. It is hypothesized that, after accounting for individual (age, poverty, health comorbidity) and objective neighborhood characteristics (deprivation and level of rurality), (1) a perception of more health-promoting characteristics in home and workplace neighborhoods would be associated with better perceived health and positive mental health, as well as with lower BMI and (2) these associations would be mediated by health self-efficacy and health behaviors.
Method
Procedure
The project received ethics approval from an institutional review board. Male participants were recruited among active workers from four central labor unions in Quebec (Canada) in the fields of construction, metallurgy, aerospace industry, transportation, and police services. A random selection of 3,234 male union members older than the age of 18 years received a personalized invitation by mail including the questionnaire (in French) to be completed and mailed back in a prepaid envelope. They could also fill out the questionnaire on a secure website.
Measures
Health-Promoting Neighborhood Questionnaire
The Health-Promoting Neighborhood Questionnaire (HPNQ) was developed for the present study since, to our knowledge, no published measurement scale focuses on perceived health-promoting aspects of both home and work neighborhoods. The eight items (see the appendix) were designed to measure perceptions of the physical and social environmental qualities that support a healthy lifestyle (health behaviors from the list established by Walker, Sechrist, & Pender, 1987). The HPNQ focused on physical activity (e.g., availability of bicycle and pedestrian paths), nutrition (e.g., availability of fresh fruits/vegetables within walking distance), stress management (e.g., presence of green spaces where it is possible to relax), interpersonal relations (e.g., friendliness of the population), maintenance/aesthetics, and safety (Bonaiuto & Alves, 2012; Burke et al., 2009). The items were affirmative statements assessed on a 4-point Likert-type scale, from 1 (strongly disagree) to 4 (strongly agree). Participants answered each item twice, once for their home neighborhood and once for their workplace neighborhood. Neighborhood was defined as the overall area within an approximate 10- to 15-minute walking distance from home or work. Although there is considerable debate concerning delimitation, neighborhoods are usually defined as more or less large areas surrounding one place and nested in a larger community (Amérigo & Aragonés, 1997; Sampson, Morenoff, & Gannon-Rowley, 2002).
A two-step factor analysis approach was used to examine the structure validity of the questionnaire. A principal component analysis was performed on the HPNQ items using SPSS v22. Once a satisfying factorial structure was found, it was retested using a confirmatory factor analysis in Mplus v7.2. Results of the two analyses are presented in the appendix. All items from the home version loaded significantly on one factor (HPNQ–home), and all items from the work version loaded significantly on another factor (HPNQ–workplace). Reliability was satisfactory for both subscales (α = .80 for HPNQ–home; .84 for HPNQ–workplace).
Health Outcomes
Perceived health was measured using a single item from Statistics Canada’s (2008) Canadian Community Health Survey, inviting respondents to rate their health on a scale from 0 (poor) to 5 (excellent). The Mental Health Continuum (Short Form; Keyes, 2009) was used to measure positive mental health. The instrument includes 14 items that measure the frequency with which participants had experienced components of well-being in the previous month on a scale from 0 (never) to 5 (every day). The French version from Statistics Canada’s (2012a) Canadian Community Health Survey (Mental Health) was used. Scores were aggregated, and internal consistency was adequate (α = .89). BMI was computed using self-reported height and weight. BMI is the most frequently used indirect indicator of obesity, with correlations between .6 and .8 with percentage of body fat (see Kuczmarski, 2007).
Potential Mediators
Health behaviors were measured using the Health Promoting Lifestyle Profile II (Walker, Sechrist, & Pender, 1995), translated from English to French following back-translation guidelines (Guillemin, Bombardier, & Beaton, 1993). The instrument asks participants to report the frequency of 52 different health behaviors on a scale from 0 (never) to 3 (very often). The behaviors pertain to the following dimensions of a health-promoting lifestyle: health responsibility, physical activity, nutrition, interpersonal relations, stress management, and spirituality. Scores were averaged, yielding a single total score for the entire scale (α = .92). Health self-efficacy was measured with the Perceived Health Competence Scale comprising eight statements on perceived ability to achieve one’s health goal (Smith, Wallston, & Smith, 1995). Participants answered on a 6-point agreement scale. Negative statements were reverse-coded and scores were aggregated for all items. Internal consistency was high (α = .80).
Individual and Environmental Covariates
Age was calculated using self-reported month and year of birth. Perceived poverty was measured with a question from provincial surveys conducted in Quebec (e.g., Quebec Statistics Institute, 2001) inviting participants to assess their economic situation compared with that of other people of their age, on a scale from 1 (financially comfortable) to 4 (very poor). Finally, following the Functional Comorbidity Index (Groll, To, Bombardier, & Wright, 2005), a health comorbidity index was created, with participants indicating whether they had ever suffered from any of 19 conditions (e.g., arthritis, asthma, stroke, depression, anxiety, human immunodeficiency virus). The index referred to the number of conditions checked off by the participant.
Three objective characteristics of neighborhood were considered: material deprivation, social deprivation, and level of rurality. All three were obtained from the Public Health Institute of Quebec (2010) using participants’ residential postal codes. The deprivation indices reflect the socioeconomic composition of small geographic units, based on data from the Canada 2006 Census (Pampalon, Hamel, Gamache, & Raymond, 2009). For each index, the score (transformed into quintiles) rises with the level of deprivation. Levels of rurality ranged from 1 (large metropolitan area) to 4 (rural areas).
Statistical Analysis
Correlations were used to examine univariate relationships between HPNQ and health variables. Using Mplus v7.2, structural equation modeling (path analysis) was performed to test the hypotheses. Compared with other approaches for mediation testing, structural equation modeling allows simultaneous consideration of multiple mediators and outcomes (Cheung & Lau, 2008). Structural equation modeling also allows for bootstrap iterations, making it possible to calculate confidence intervals (Mallinckrodt, Abraham, Wei, & Russell, 2006).
Results
Participants’ Description
The sample consisted of 669 men who were on average 47.1 years old (SD = 11.1), with ages ranging from 19 to 71 years. They were mainly born in Canada (641; 95.8%). Three quarters were married or in a relationship (506; 75.6%). About the same proportion had children (475; 71.0%). Most had either a college or trade school diploma (404; 60.4%). Of the participants, 61 (9.1%) reported being poor or very poor. The majority of participants (389; 58.1 %) lived in metropolitan areas, about a quarter (171; 25.6%) in rural areas, and the others (74; 11.1%) in intermediate regions. Table 1 depicts a more detailed portrait of the sample composition in terms of demographic, clinical, and environmental characteristics.
Table 1.
Sociodemographic Composition of the Sample.
| Variables | n (%) |
|---|---|
| Age (years) | |
| 18-29 | 54 (8.1) |
| 30-39 | 130 (19.4) |
| 40-49 | 157 (23.5) |
| 50-59 | 258 (38.6) |
| 60 and more | 65 (9.7) |
| Education level | |
| Less than high school diploma | 68 (10.2) |
| High school diploma | 139 (20.8) |
| Trade school diploma | 191 (28.6) |
| College diploma | 213 (31.8) |
| University diploma | 52 (7.8) |
| Perceived economic situation | |
| Sufficient income or financially comfortable | 601 (89.8) |
| Poor or very poor | 61 (9.1) |
| Born in Canada | |
| Yes | 641 (95.8) |
| No | 25 (3.7) |
| Marital status | |
| Married or in a relationship | 506 (75.6) |
| Widowed, separated, or divorced | 52 (7.8) |
| Single | 104 (15.5) |
| Paternity | |
| Yes | 475 (71.0) |
| No | 187 (28.0) |
| Body mass index | |
| Underweight | 6 (0.9) |
| Normal | 175 (26.2) |
| Overweight | 327 (48.9) |
| Obesity | 143 (21.4) |
| Number of health comorbidities | |
| 0 or 1 | 470 (70.3) |
| 2 or 3 | 150 (22.4) |
| 4 and more | 39 (5.8) |
| Unions | |
| Construction | 117 (17.5) |
| Metallurgy | 100 (14.9) |
| Police services | 114 (17.0) |
| Aerospace and transportation | 189 (28.3) |
| Other | 121 (22.3) |
| Material deprivation quintile | |
| 1 (least deprived) | 107 (16.0) |
| 2 | 160 (23.9) |
| 3 | 131 (19.6) |
| 4 | 134 (20.0) |
| 5 (most deprived) | 84 (12.6) |
| Social deprivation quintile | |
| 1 (least deprived) | 157 (23.5) |
| 2 | 137 (20.5) |
| 3 | 133 (19.9) |
| 4 | 104 (15.5) |
| 5 (most deprived) | 85 (12.7) |
| Level of rurality | |
| Rural area | 171 (25.6) |
| Metropolitan area | 389 (58.1) |
| Intermediate region | 74 (11.1) |
Note. For any variable, a sum less than the total N = 669 (100%) is due to missing values.
Univariate Correlations
Univariate correlations between the main study variables are presented in Table 2. HPNQ–home was positively associated with positive mental health and perceived health, and negatively related to BMI. HPNQ–workplace was positively associated with positive mental health and perceived health, but not associated with BMI. Health behaviors and health self-efficacy were correlated with each other, and both were positively correlated with the two HPNQ subscales. Health behavior and health self-efficacy were also positively associated with positive mental health and perceived health, and negatively associated with BMI.
Table 2.
Correlations Between Main Study Variables and Descriptive Statistics (n = 596-666).
| Measure | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. HPNQ–home | — | ||||||
| 2. HPNQ–workplace | .30** | — | |||||
| 3. Positive mental health | .28** | .23** | — | ||||
| 4. Perceived health | .24** | .14** | .39** | — | |||
| 5. BMI | −.13** | −.02 | −.01 | −.25** | — | ||
| 6. Health behaviors | .27** | .16** | .55** | .43** | −.11* | — | |
| 7. Health self-efficacy | .24** | .19** | .44** | .60** | −.19** | .49** | — |
| M | 3.21 | 2.67 | 3.31 | 3.43 | 27.32 | 1.43 | 4.46 |
| SD | 0.54 | 0.68 | 0.85 | 0.91 | 4.27 | 0.37 | 0.81 |
| Skewness | −0.47 | −0.06 | −0.51 | −0.27 | 0.99 | 0.15 | −0.32 |
| Kurtosis | −0.20 | −0.53 | 0.01 | −0.04 | 2.41 | −0.20 | −0.22 |
Note. HPNQ = Health-Promoting Neighborhood Questionnaire; BMI = body mass index.
p ≤ .01. **p ≤ .001.
Path Analysis
The proposed model included the following pathways: (1) HPNQ–home and HPNQ–workplace on perceived health, BMI, and positive mental health; (2) HPNQ–home and HPNQ–workplace on health self-efficacy and health behaviors; (3) health self-efficacy and health behaviors on perceived health, BMI, and positive mental health; and (4) health self-efficacy on health behaviors. To control for possible covariates, the associations of age, poverty, and health comorbidity with the three health outcomes were also included, as well as the associations of the objective home neighborhood characteristics with HPNQ−home. The percentage of missing values was low (<2.7%), except for objective characteristics (between 5.2 and 7.9%), which were not available for some participants, and for HPNQ–workplace, where 10.0% of values were missing. A maximum likelihood (ML) algorithm implemented in Mplus was used as a robust approach for dealing with these missing values (Newman, 2014).
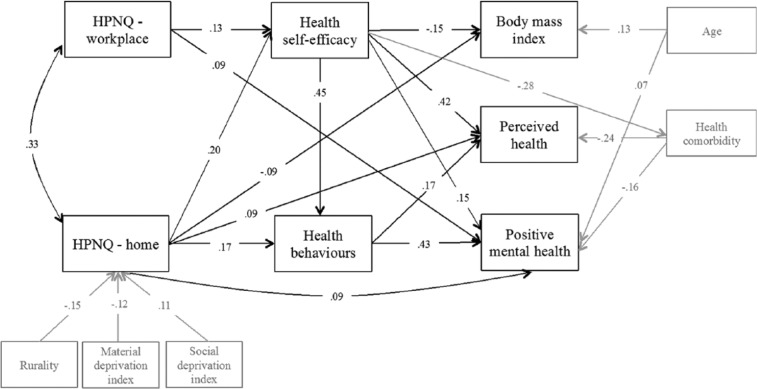
The model (N = 669) obtained an inadequate fit, χ2(22) = 145.238, p ≤ .001; Tucker–Lewis index = 0.755; comparative fit index = 0.894; root mean square error of approximation = 0.092; standardized root mean square residual = 0.059. Following an iterative process, changes were made based on the estimates and modification indices. The modified model was tested and additional changes were performed until fit was adequate. During this process, nonsignificant pathways were removed. Based on modification indices, correlations between the error terms for HPNQ–home and HPNQ–workplace, as well as between the error terms for health comorbidity and health self-efficacy were added. The final model (Figure 1) had excellent fit: χ2(26) = 28.647, p > .05; Tucker–Lewis index = 0.996; comparative fit index = 0.998; root mean square error of approximation = 0.012; standardized root mean square residual = 0.019. In the model, level of rurality and material deprivation were negatively associated with HPNQ–home. Social deprivation was positively associated with HPNQ–home. HPNQ–home and HPNQ–workplace both had a direct positive link with health self-efficacy, and positive mental health. HPNQ–home was also positively associated with health behaviors and perceived health, while negatively associated with BMI. The model also obtained a positive association of health self-efficacy with health behaviors, perceived health, and positive mental health, and a negative association with BMI. Health behaviors were positively associated with perceived health and positive mental health. Table 3 reports the estimates and the bootstrap (N = 2,000) bias-corrected confidence intervals for total, indirect, and direct effects. The positive association of HPNQ–home with positive mental health and perceived health was partially mediated by health behaviors and health self-efficacy. Health self-efficacy had a direct association with positive mental health and perceived health, as well an indirect association through health behaviors. Although the association was small in magnitude, HPNQ–home was negatively associated with BMI, partly mediated by a direct effect of health self-efficacy. Regarding HPNQ–workplace, higher scores were associated with more positive mental health. That association was partly mediated by health self-efficacy, which had both a direct association with positive mental health and an indirect one through health behaviors. HPNQ–workplace had a positive association with perceived health, which was completely mediated by health self-efficacy. Self-efficacy was both directly and indirectly (through health behaviors) related to perceived health. Finally, HPNQ–workplace had a negative, small but significant association with BMI, completely mediated by health self-efficacy.
Figure 1.
Path analysis with standardized estimates for relationships between HPNQ–home and HPNQ–workplace, health outcomes, and mediating variables (N = 669).
Note. HPNQ = Health-Promoting Neighborhood Questionnaire. All associations are statistically significant. Variables and arrows in gray consist of covariates.
Table 3.
Bootstrap Estimates and 95% Bias-Corrected Confidence Intervals for Direct and Indirect Effects of HPNQ–Home and HPNQ–Workplace on Three Health Outcomes (N = 669).
| DV: Positive mental health |
DV: Perceived health |
DV: BMI |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| B (β) | Low | High | B (β) | Low | High | B (β) | Low | High | |
| IV: HPNQ–home | |||||||||
| Total effect | 0.365 (0.231) | 0.240 | 0.484 | 0.360 (0.213) | 0.236 | 0.480 | −0.974 (−0.122) | −1.587 | −0.352 |
| Indirect effect of IV | 0.217 (0.137) | 0.149 | 0.291 | 0.216 (0.128) | 0.139 | 0.298 | −0.243 (−0.031) | −0.459 | −0.089 |
| Through health behaviors | 0.112 (0.071) | 0.065 | 0.162 | 0.048 (0.028) | 0.022 | 0.083 | — | — | — |
| Through health self-efficacy | 0.045 (0.029) | 0.019 | 0.082 | 0.142 (0.084) | 0.080 | 0.209 | −0.243 (−0.031) | −0.459 | −0.089 |
| Through health self-efficacy mediated by health behaviors | 0.060 (0.038) | 0.035 | 0.090 | 0.026 (0.015) | 0.012 | 0.044 | — | — | — |
| Direct effect | 0.148 (0.094) | 0.037 | 0.254 | 0.144 (0.085) | 0.034 | 0.242 | −0.731 (−0.092) | −1.373 | −0.075 |
| IV: HPNQ–workplace | |||||||||
| Total effect | 0.166 (0.133) | 0.078 | 0.253 | 0.085 (0.064) | 0.022 | 0.142 | −0.122 (−0.019) | −0.281 | −0.031 |
| Indirect effect of IV | 0.053 (0.043) | 0.014 | 0.094 | 0.085 (0.064) | 0.022 | 0.142 | −0.122 (−0.019) | −0.281 | −0.031 |
| Through health behaviors | — | — | — | — | — | — | — | — | — |
| Through health self-efficacy | 0.023 (0.018) | 0.006 | 0.049 | 0.072 (0.054) | 0.020 | 0.125 | −0.122 (−0.019) | −0.281 | −0.031 |
| Through health self-efficacy mediated by health behaviors | 0.030 (0.024) | 0.009 | 0.054 | 0.013 (0.010) | 0.004 | 0.027 | — | — | — |
| Direct effect | 0.113 (0.091) | 0.029 | 0.198 | — | — | — | — | — | — |
Note. HPNQ = Health-Promoting Neighborhood Questionnaire; IV = independent variable; DV = dependent variable; BMI = body mass index. Results obtained with N = 2,000 bootstraps. Although other variables were included in the model (see Figure 1), only the effects of IV on the three main health outcomes are presented in the table. All effects in the table are statistically significant (bootstrap confidence interval excludes zero).
Discussion
The present study is one of few rare empirical investigations of the relationships between health-promoting neighborhood and health outcomes with a specific focus on men. Confirming the first hypothesis, the study reported an association of a global measure of neighborhood health-promoting characteristics with several facets of health, including positive ones. The HPNQ aggregates perceptions concerning a wide array of neighborhood characteristics, both physical and social in nature: bicycle and pedestrian paths, sport facilities, availability of fresh fruits/vegetables, presence of green spaces, maintenance/aesthetics, socialization areas, friendliness of the population, and safety. Findings using this global scale suggest that both physical and social aspects of environment might contribute to men’s health, thereby confirming findings from previous studies (Burke et al., 2009; Saarloos et al., 2011). They are contrary to the results of Molinari et al. (1998), however, which reported no evidence of the influence of social aspects of neighborhood on men’s health. Due to evolving masculinity norms (Bridges & Pascoe, 2014), men from the present study’s sample might rely on social environment more than did the men in Molinari et al.’s study, which was published about two decades ago. It is also possible that social aspects might not have been associated with men’s health if they had been considered separately from physical aspects. In this regard, as a supplementary analysis (not presented in details here) the univariate correlations between health outcomes and individuals items from the HPNQ were examined. Both the physical and social items significantly correlated in the expected direction with one or more of the outcomes.
Another contribution of this study is the joint exploration of individuals’ perceptions of both home and workplace neighborhoods, showing stronger associations of perceived home neighborhood with health outcomes. In all likelihood, men spend most of their time in the workplace area working, rather than taking advantage of resources in the neighborhood. This result is in line with K. Moore et al.’s (2013) finding that the density of recreational facilities around the workplace was less strongly associated with BMI than was the density of facilities around the home.
In line with Taylor, Repetti, and Seeman (1997), findings from the present study suggest that environment gets “under the skin.” However, this holds true only to a limited extent when considering perceived health-promoting neighborhood characteristics and men’s BMI. This is consistent with studies that have identified only a relatively small effect size for the association between perceived environment factors and BMI (Christian, Giles-Corti, Knuiman, Timperio, & Foster, 2011; Saelens, Sallis, Black, & Chen, 2003). In contrast, positive mental health was most strongly associated with high HPNQ scores. A method effect (Maul, 2013) due to the fact that HPNQ and positive mental health are both self-reported subjective indicators might contribute to this result. Some people might be predisposed to have more positive perceptions no matter the object or the topic. For example, high optimism has been associated with positive scores on both perceived neighborhood and positive mental health scales (Gallagher & Lopez, 2009; Greenberg & Schneider, 1997). Although subjective neighborhood measures are prone to such bias, the significant associations between HPNQ and the objective home neighborhood characteristics (level of rurality, material, and social deprivation) considered in the study suggest that men’s perceptions of their neighborhood are anchored in their objective environmental reality. An additional mediation analysis (not presented here) suggests that these objective environmental characteristics had a significant indirect effect on positive mental health through men’s perceptions of the health-promoting neighborhood characteristics (HPNQ–home), supporting the mediator role of environmental perceptions as reported by other researchers before (Weden et al., 2008).
This study also contributes to identifying behavioral and cognitive processes underlying the associations between perceived neighborhood environment and health. It is one of the few times multiple mediators have been studied together, taking into account both health behaviors and self-efficacy. On the whole, the final model confirms the mediating role of health behaviors and self-efficacy proposed in the second hypothesis. The model suggests that health-promoting home neighborhood characteristics might lead to more frequent healthy behaviors, which in turn might lead to more positive mental health and perceived health. This expands results from previous studies that had focused on specific health behaviors (Kruger et al., 2007; L. V. Moore, Diez Roux, Nettleton, Jacobs, & Franco, 2009). In line with Ajzen’s (1991) theory, more perceived health-promoting characteristics of home and workplace neighborhoods might lead to more perceived control (i.e., self-efficacy) over one’s health, which in turn might promote health (in terms of positive mental health, perceived health, and lower BMI), either directly or by conducting to more frequent health behaviors.
Mediation effects completely explained the associations of perceived health and BMI with perceived workplace neighborhood. However, after controlling for the mediators, positive mental health was still directly associated with perceptions of home and workplace neighborhoods, and perceived health and BMI were still associated with perceptions of home neighborhood. Thus, overall, beyond the associations with the mediators, there seems to be something that remains unexplained in the relationship of perceived health-promoting neighborhood with health outcomes. Further research is needed to explore other mediators that could account for this remaining direct effect. For example, community variables should be given more attention. One of those variables is sense of community, which has recently been associated to neighborhood perceptions (Wood, Frank, & Giles-Corti, 2010) and could have a stress-buffering effect on men’s well-being (Kutek, Turnbull, & Fairweather-Schmidt, 2011).
Limitations of the Study
The present study has some limitations. First, a specific definition of neighborhood (i.e., as a zone which is accessible within a 10- to 15-minute walk) was chosen for the HPNQ. An ego-centered definition was chosen (Voigtländer, Razum, & Berger, 2013) so that the neighborhood would be individually anchored around each participant’s home or workplace and would be personally relevant. However, people in more rural areas had lower scores on the HPNQ. In rural areas, several health-promoting resources (e.g., sport installations, healthy food, etc.) are probably located more than a 10- to 15-minute walk away. The results might have differed if areas were delimited otherwise, such as by distance walked or travelled by car, depending on usual means of transport.
Second, despite several efforts to maximize response rate, the obtained rate (21%) possibly limits generalizability. The labor unions that collaborated to the study did not provide the characteristics of their members. Thus, it is impossible to estimate the comparability of the participants with the whole group of 3,234 members who were randomly invited to take part in the study. This makes it difficult to conclude with precision on the extent of generalizability of the findings to the whole population of workers.
Third, there were relatively many missing values for the items of the HPNQ–workplace (between 9.9% and 12.7%). The space in the questionnaire where participants had to answer the workplace version of each item was placed to the right of where they had to answer the home version. Participants might not have understood that they had to answer each item a second time with respect to their workplace area. Participants might also have purposely left the spaces blank, for example, those that work in the same neighborhood as the one in which they live. Another possibility is that some men recruited from the construction labor union have thought inappropriate to answer the workplace items given that their workplace changes throughout the year. Collecting information about workplace location (e.g., stable or changing, postal code, etc.) would help in controlling these issues. Suggested as an optimal approach for dealing with data missingness (Enders & Bandalos, 2001), the ML estimation algorithm was used with the intention of producing adequate estimates despite missing values. Although the results involving workplace neighborhood need to be interpreted with more caution, they represent one of the first attempts to explore its relationships with health outcomes. Compared with home neighborhood, the study of workplace area in relation to health is still in its infancy (K. Moore et al., 2013), and the present results, although rudimentary, are important for stimulating further research. The objective neighborhood characteristics (level of rurality, material, and social deprivation indices) based on Canada 2006 Census (Pampalon et al., 2009) were also missing for a considerable number of cases (between 5.2% and 7.9%). It was impossible to assign some participants’ postal codes to a dissemination area of the census. Although the ML estimators provided a certain degree of robustness despite missing values (Newman, 2014), supplementary models were tested not including the objective covariates. These models yielded similar patterns of association concerning the variables of interest (HPNQ and health outcomes).
Fourth, exploratory and confirmatory factor analyses to validate the HPNQ were performed on the same data set. This does not provide as much evidence for the validation of the factor structure as if the analyses were performed on two data sets (L. Wang, Watts, Anderson, & Little, 2013). However, replicating the structure with the same sample was a necessary first step because if “agreement cannot be found between the two approaches [exploratory and confirmatory] in the same sample, then it is very unlikely that confirmation would be found in a new sample” (L. Wang et al., 2013, p. 742).
Finally, the cross-sectional nature of the data collected prevented conclusions concerning the causal chain of effects between HPNQ, health outcomes, and mediators.
Conclusion
Macdonald (2006, p. 457) proposed that for addressing men’s health problems, “the professional response should be to work towards providing health-supporting work and social environments.” This study provided a unique comprehensive perspective on the health-promoting characteristics of home and workplace neighborhoods and their associations with working men’s health. The associations of the HPNQ with multiple health outcomes and mediating health processes highlight the importance of considering environmental influences in men’s health promotion. Men face numerous health challenges (Gough, 2013). Results highlight positive environmental levers to take into account for promoting their health, rather than focusing solely on individual determinants, which incurs the risk of blaming men for their difficulties (see Bilsker, Goldenberg, & Davidson, 2010). Based on the HPNQ, positive environmental levers include providing men with sport facilities and bicycle or pedestrian lanes, offering access to green spaces to relax and be physically active, and facilitating access to fruits and vegetables within walking distance. Other possible avenues are to plan spaces for men to socialize and have friendly interactions with neighbors, and to ensure the safety, maintenance, and aesthetics of neighborhoods. Programs integrated into community settings offer promising opportunities to implement some of these health promotion avenues (e.g., Premier League Health program delivered in English football clubs; Pringle et al., 2013). Urban planners, policy makers, and health professionals should be allies. Together they can improve men’s health by creating environments that increase health self-efficacy and the adoption of healthy behaviors. The HPNQ can be a useful tool to monitor men’s perceptions of their home and workplace neighborhoods.
Acknowledgments
We wish to thank Catherine Purenne, the research coordinator, as well as the research assistants: Benoit Martel, Catherine Guillou-Ouellette, Stéphanie Robert, Stephanie Radziszewski, and Jocelyne Gagné. We also thank the unions that collaborated in recruiting participants: CSD and CSD Construction, Metallos, Fédération des policiers municipaux du Québec, and TCA-Québec.
Appendix
Appendix.
Principal Component and Confirmatory Factor Analysis of Items From the Health-Promoting Neighborhood Questionnaire (HPNQ).
| Item | Principal component analysis (n = 548) |
Confirmatory factor analysis (n = 658) |
||||
|---|---|---|---|---|---|---|
| Factor loadings |
Communalities |
Standardized loadings (standard error) |
||||
| Home | Workplace | Home | Workplace | HPNQ–home | HPNQ–workplace | |
| 1. Bicycle and pedestrian lanes allow safe circulation. | .66 | .61 | .44 | .37 | .55 (.04) | .57 (.03) |
| 2. Fresh fruits and vegetables are available within walking distance. | .60 | .69 | .37 | .48 | .54 (.04) | .65 (.03) |
| 3. Population of the neighborhood is friendly (e.g., people smile or greet when they meet, help each other, etc.). | .51 | .63 | .29 | .40 | .32 (.04) | .50 (.04) |
| 4. The neighborhood is well maintained and looks nice (e.g., cleanliness, presence of trees, interesting buildings, or attractive shops). | .61 | .66 | .38 | .46 | .36 (.04) | .57 (.04) |
| 5. Sports facilities are available (e.g., swimming pools, fitness centers, soccer or tennis courts). | .74 | .75 | .56 | .57 | .77 (.03) | .73 (.03) |
| 6. The neighborhood offers green spaces that promote relaxation or the practice of sports. | .76 | .79 | .58 | .64 | .76 (.03) | .80 (.02) |
| 7. The neighborhood is safe enough so that I feel comfortable to walk alone. | .54 | .50 | .30 | .26 | .41 (.04) | .45 (.04) |
| 8. There are places for socializing (e.g., benches, picnic tables, outdoor terraces, community halls). | .70 | .81 | .51 | .67 | .69 (.03) | .79 (.03) |
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the Canadian Institutes of Health Research.
References
- Ajzen I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179-211. doi: 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- Amérigo M., Aragonés J. I. (1997). A theoretical and methodological approach to the study of residential satisfaction. Journal of Environmental Psychology, 17, 47-57. doi: 10.1006/jevp.1996.0038 [DOI] [Google Scholar]
- Auchincloss A. H., Diez Roux A. V., Brown D. G., Erdmann C. A., Bertoni A. G. (2008). Neighborhood resources for physical activity and healthy foods and their association with insulin resistance. Epidemiology, 19, 146-157. doi: 10.1097/EDE.0b013e31815c480 [DOI] [PubMed] [Google Scholar]
- Berke E. M., Gottlieb L. M., Moudon A. V., Larson E. B. (2007). Protective association between neighborhood walkability and depression in older men. Journal of American Geriatrics Society, 55, 526-533. doi: 10.1111/j.1532-5415.2007.01108.x [DOI] [PubMed] [Google Scholar]
- Bilsker D., Goldenberg L., Davison J. (2010). A roadmap to men’s health: Current status, research, policy & practice. Vancouver, Canada: Men’s Health Initiative of British Columbia; Retrieved from http://www.sfu.ca/content/dam/sfu/carmha/resources/mens-health/A-Roadmap-to-Mens-Health-May-17-2010.pdf [Google Scholar]
- Bonaiuto M., Alves S. (2012). Residential places and neighborhoods: Toward healthy life, social integration, and reputable residence. In Clayton S. (Ed.), The Oxford handbook of environmental and conservation psychology (pp. 221-247). New York, NY: Oxford University Press. doi: 10.1093/oxfordhb/9780199733026.013.0013 [DOI] [Google Scholar]
- Bond L., Kearns A., Mason P., Tannahill C., Egan M., Whitely E. (2012). Exploring the relationships between housing, neighborhoods and mental wellbeing for residents of deprived areas. BMC Public Health, 12, 48. doi: 10.1186/1471-2458-12-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bridges T., Pascoe C. J. (2014). Hybrid masculinities: New directions in the sociology of men and masculinities. Sociology Compass, 8, 246-258. doi: 10.1111/soc4.12134 [DOI] [Google Scholar]
- Bromell L. R. (2011). Neighborhood influences on health among black and white adults (Unpublished doctoral dissertation). Duke University, Durham, NC. [Google Scholar]
- Burke J., O’Campo P., Salmon C., Walker R. (2009). Pathways connecting neighborhood influences and mental well-being: Socioeconomic position and gender differences. Social Science & Medicine, 68, 1294-1304. doi: 10.1016/j.socscimed.2009.01.015 [DOI] [PubMed] [Google Scholar]
- Cheung G. W., Lau R. S. (2008). Testing mediation and suppression effects of latent variables: Bootstrapping with structural equation models. Organizational Research Methods, 11, 296-325. doi: 10.1177/1094428107300343 [DOI] [Google Scholar]
- Christian H., Giles-Corti B., Knuiman M., Timperio A., Foster S. (2011). The influence of the built environment, social environment and health behaviors on body mass index: Results from RESIDE. Preventive Medicine, 53, 57-60. doi: 10.1016/j.ypmed.2011.05.004 [DOI] [PubMed] [Google Scholar]
- Courtenay W. (2011). Dying to be men: Psychosocial, environmental, and biobehavioral directions in promoting the health of men and boys. New York, NY: Routledge. [Google Scholar]
- Dempster M., Donnelly M. (2008). Validity of the Perceived Health Competence Scale in a UK primary care setting. Psychology, Health & Medicine, 13, 123-127. doi: 10.1080/13548500701351984 [DOI] [PubMed] [Google Scholar]
- Diez Roux A. V., Mair C. (2010). Neighborhoods and health. Annals of the New York Academy of Sciences, 1186, 125-145. doi: 10.1111/j.1749-6632.2009.05333.x [DOI] [PubMed] [Google Scholar]
- Enders C. K., Bandalos D. L. (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling, 8, 430-457. doi: 10.1207/S15328007SEM0803_5 [DOI] [Google Scholar]
- Eriksson M., Emmelin M. (2013). What constitutes a health-enabling neighborhood? A grounded theory situational analysis addressing the significance of social capital and gender. Social Science & Medicine, 97, 112-123. doi: 10.1016/j.socscimed.2013.08.008 [DOI] [PubMed] [Google Scholar]
- Erinosho T. O., Oh A. Y., Moser R. P., Davis K. L., Nebeling L. C., Yaroch A. L. (2012). Association between perceived food environment and self-efficacy for fruit and vegetable consumption among US adults, 2007. Preventing Chronic Disease, 9. doi: 10.5888/pcd9.100291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Communities. (2004). How Europeans spend their time: Everyday life of women and men. Luxembourg: Office for Official Publications of the European Communities. [Google Scholar]
- Gale C. R., Dennison E. M., Cooper C., Sayer A. A. (2011). Neighborhood environment and positive mental health in older people: The Hertfordshire Cohort Study. Health Place, 17, 867-874. doi: 10.1016/j.healthplace.2011.05.003 [DOI] [PubMed] [Google Scholar]
- Gallagher M. W., Lopez S. J. (2009). Positive expectancies and mental health: Identifying the unique contributions of hope and optimism. Journal of Positive Psychology, 4, 548-556. doi: 10.1080/17439760903157166 [DOI] [Google Scholar]
- Galster G. C. (2012). The mechanism(s) of neighborhood effects: Theory, evidence, and policy implications. In van Ham M., Manley D., Bailey N., Simpson L., Maclennan D. (Eds.), Neighborhood effects research: New perspectives (pp. 23-56). Dordrecht, Netherlands: Springer. doi: 10.1007/978-94-007-2309-2_2 [DOI] [Google Scholar]
- Gough B. (2013). The psychology of men’s health: Maximizing masculine capital introduction. Health Psychology, 32, 1-4. doi: 10.1037/a0030424 [DOI] [PubMed] [Google Scholar]
- Greenberg M., Schneider D. (1997). Neighborhood quality, environmental hazards, personality traits, and resident actions. Risk Analysis, 17, 169-175. doi: 10.1111/j.1539-6924.1997.tb00856.x [DOI] [PubMed] [Google Scholar]
- Groll D. L., To T., Bombardier C., Wright J. G. (2005). The development of a comorbidity index with physical function as the outcome. Journal of Clinical Epidemiology, 58, 595-602. doi: 10.1016/j.jclinepi.2004.10.018 [DOI] [PubMed] [Google Scholar]
- Grzywacz J. G., Keyes C. L. M. (2004). Toward health promotion: Physical and social behaviors in complete health. American Journal of Health Behavior, 28, 99-111. doi: 10.5993/AJHB.28.2.1 [DOI] [PubMed] [Google Scholar]
- Guillemin F., Bombardier C., Beaton D. (1993). Cross-cultural adaptation of health-related quality of life measures: Literature review and proposed guidelines. Journal of Clinical Epidemiology, 46, 1417-1432. doi: 10.1016/0895-4356(93)90142-N [DOI] [PubMed] [Google Scholar]
- Inglehart R. (2002). Gender, aging, and subjective well-being. International Journal of Comparative Sociology, 43, 391-408. doi: 10.1177/002071520204300309 [DOI] [Google Scholar]
- Jackson E. S., Tucker C. M., Herman K. C. (2007). Health value, perceived social support, and health self-efficacy as factors in a health-promoting lifestyle. Journal of American College Health, 56, 69-74. doi: 10.3200/JACH.56.1.69-74 [DOI] [PubMed] [Google Scholar]
- Keyes C. L. M. (2002). The mental health continuum: From languishing to flourishing in life. Journal of Health and Social Behavior, 43, 207-222. doi: 10.2307/3090197 [DOI] [PubMed] [Google Scholar]
- Keyes C. L. M. (2009). Brief description of the Mental Health Continuum Short Form (MHC-SF). Atlanta, GA: Author. [Google Scholar]
- Kruger D. J., Reischl T. M., Gee G. C. (2007). Neighborhood social conditions mediate the association between physical deterioration and mental health. American Journal of Community Psychology, 40, 261-271. doi: 10.1007/s10464-007-9139-7 [DOI] [PubMed] [Google Scholar]
- Kuczmarski R. J. (2007). What is obesity? Definitions matter. In Kumanyika S., Brownson R. S. (Eds.), Handbook of obesity prevention: A resource for health professional (pp. 25-44). New York, NY: Springer. doi: 10.1007/978-0-387-47860-9_2 [DOI] [Google Scholar]
- Kutek S. M., Turnbull D., Fairweather-Schmidt A. K. (2011). Rural men’s subjective well-being and the role of social support and sense of community: Evidence for the potential benefit of enhancing informal networks. Australian Journal of Rural Health, 19, 20-26. doi: 10.1111/j.1440-1584.2010.01172.x [DOI] [PubMed] [Google Scholar]
- Macdonald J. J. (2006). Shifting paradigms: A social-determinants approach to solving problems in men’s health policy and practice. Medical Journal of Australia, 185, 456-458. [DOI] [PubMed] [Google Scholar]
- Mallinckrodt B., Abraham W. T., Wei M., Russell D. W. (2006). Advances in testing the statistical significance of mediation effects. Journal of Counseling Psychology, 53, 372-378. doi: 10.1037/0022-0167.53.3.372 [DOI] [Google Scholar]
- Marans R. W. (2003). Understanding environmental quality through quality of life studies: The 2001 DAS and its use of subjective and objective indicators. Landscape and Urban Planning, 65, 73-84. doi: 10.1016/S0169-2046(02)00239-6 [DOI] [Google Scholar]
- Maul A. (2013). Method effects and the meaning of measurement. Frontiers in Psychology, 4. doi: 10.3389/fpsyg.2013.00169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeill L. H., Wyrwich K. W., Brownson R. C., Clark E. M., Kreuter M. W. (2006). Individual, social environmental, and physical environmental influences on physical activity among black and white adults: A structural equation analysis. Annals of Behavioral Medicine, 31, 36-44. doi: 10.1207/s15324796abm3101_7 [DOI] [PubMed] [Google Scholar]
- Meijer M., Röhl J., Bloomfield K., Grittner U. (2012). Do neighborhoods affect individual mortality? A systematic review and meta-analysis of multilevel studies. Social Science & Medicine, 74, 1204-1212. doi: 10.1016/j.socscimed.2011.11.034 [DOI] [PubMed] [Google Scholar]
- Molinari C., Ahern M., Hendryx M. (1998). The relationship of community quality to the health of women and men. Social Science & Medicine, 47, 1113-1120. doi: 10.1016/S0277-9536(98)00114-2 [DOI] [PubMed] [Google Scholar]
- Moore K., Diez Roux A. V., Auchincloss A., Evenson K. R., Kaufman J., Mujahid M., Williams K. (2013). Home and work neighborhood environments in relation to body mass index: The Multi-Ethnic Study of Atherosclerosis (MESA). Journal of Epidemiological Community Health, 67, 846-853. doi: 10.1136/jech-2013-202682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore L. V., Diez Roux A., Nettleton J. A., Jacobs D. R., Franco M. (2009). Fast-food consumption, diet quality, and neighborhood exposure to fast food: The multi-ethnic study of atherosclerosis. American Journal of Epidemiology, 170, 29-36. doi: 10.1093/aje/kwp090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullings J. A., McCaw-Binns A. M., Archer C., Wilks R. (2013). Gender differences in the effects of urban neighborhood on depressive symptoms in Jamaica. Revista Panamericana de Salud Pública, 34, 385-392. [PubMed] [Google Scholar]
- Newman D. A. (2014). Missing data: Five practical guidelines. Organizational Research Methods, 17, 372-411. doi: 10.1177/1094428114548590 [DOI] [Google Scholar]
- Nock M. K., Borges G., Bromet E. J., Cha C. B., Kessler R. C., Lee S. (2008). Suicide and suicidal behavior. Epidemiologic Reviews, 30, 133-154. doi: 10.1093/epirev/mxn002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pampalon R., Hamel D., Gamache P., Raymond G. (2009). A deprivation index for health planning in Canada. Chronic Diseases in Canada, 29, 178-191. [PubMed] [Google Scholar]
- Poortinga W. (2006). Do health behaviors mediate the association between social capital and health? Preventive Medicine, 43, 488-493. doi: 10.1016/j.ypmed.2006.06.004 [DOI] [PubMed] [Google Scholar]
- Pringle A., Zwolinsky S., McKenna J., Daly-Smith A., Robertson S., White A. (2013). Delivering men’s health interventions in English Premier League football clubs: Key design characteristics. Public Health, 127, 716-726. doi: 10.1016/j.puhe.2013.04.011 [DOI] [PubMed] [Google Scholar]
- Public Health Institute of Quebec. (2010). SAS assignment of the Canadian deprivation index 2006. Montreal, Quebec, Canada: Author. [Google Scholar]
- Quebec Statistics Institute. (2001). Enquête sociale et de santé 1998 [1998 Health and Social Survey]. Québec City, Quebec, Canada: Author. [Google Scholar]
- Robertson S., Galdas P. M., McCreary D. R., Oliffe J. L., Tremblay G. (2009). Men’s health promotion in Canada: Current context and future direction. Health Education Journal, 68, 266-272. doi: 10.1177/0017896909348785 [DOI] [Google Scholar]
- Saarloos D., Alfonso H., Giles-Corti B., Middleton N., Almeida O. P. (2011). The built environment and depression in later life: The Health in Men Study. American Journal of Geriatric Psychiatry, 19, 461-470. doi: 10.1097/JGP.0b013e3181e9b9bf [DOI] [PubMed] [Google Scholar]
- Saelens B. E., Sallis J. F., Black J. B., Chen D. (2003). Neighborhood-based differences in physical activity: An environment scale evaluation. American Journal of Public Health, 93, 1552-1558. doi: 10.2105/AJPH.93.9.1552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson R. J., Morenoff J. D., Gannon-Rowley T. (2002). Assessing “neighborhood effects”: Social processes and new directions in research. Annual Review of Sociology, 28, 443-478. doi: 10.1146/annurev.soc.28.110601.141114 [DOI] [Google Scholar]
- Seligman M. E. P. (2008). Positive health. Applied Psychology, 57, 3-18. doi: 10.1111/j.1464-0597.2008.00351.x [DOI] [Google Scholar]
- Smith M. S., Wallston K. A., Smith C. A. (1995). The development and validation of the Perceived Health Competence Scale. Health Education Research, 10, 51-64. doi: 10.1093/her/10.1.51 [DOI] [PubMed] [Google Scholar]
- Stafford M., Cummins S., Macintyre S., Ellaway E., Marmot M. (2005). Gender differences in the associations between health and neighborhood environment. Social Science & Medicine, 60, 1681-1692. doi: 10.1016/j.socscimed.2004.08.028 [DOI] [PubMed] [Google Scholar]
- Statistics Canada. (2008). Canadian Community Health Survey—2008 Questionnaire. Ottawa, Ontario, Canada: Author. [Google Scholar]
- Statistics Canada. (2012. a). Canadian Community Health Survey—Mental Health (CCHS_MH). Ottawa, Ontario, Canada: Author. [Google Scholar]
- Statistics Canada. (2012. b). Life expectancy, at birth and at age 65, by sex, Canada, provinces and territories, annual (years). Ottawa, Ontario, Canada: Author. [Google Scholar]
- Taylor S. E., Repetti R. L., Seeman T. (1997). Health psychology: What is an unhealthy environment and how does it get under the skin? Annual Review of Psychology, 48, 411-447. doi: 10.1146/annurev.psych.48.1.411 [DOI] [PubMed] [Google Scholar]
- Virtanen M., Kivimäki M., Elovainio M., Linna A., Pentti J., Vahtera J. (2007). Neighborhood socioeconomic status, health and working conditions of school teachers. Journal of Epidemiological Community Health, 61, 326-330. doi: 10.1136/jech.2006.052878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voigtländer S., Razum O., Berger U. (2013). Methods to measure neighborhoods and analyse their impact on health: An overview. In Stock C., Ellaway A. (Eds.), Neighborhood structure and health promotion (pp. 93-115). New York, NY: Springer. doi: 10.1007/978-1-4614-6672-7_6 [DOI] [Google Scholar]
- Von Bothmer M. I. K., Fridlund B. (2005). Gender differences in health habits and in motivation for a healthy lifestyle among Swedish university students. Nursing & Health Sciences, 7, 107-118. doi: 10.1111/j.1442-2018.2005.00227.x [DOI] [PubMed] [Google Scholar]
- Walker S. N., Sechrist K. R., Pender N. J. (1987). The Health-Promoting Lifestyle Profile: Development and psychometric characteristics. Nursing Research, 36, 76-81. [PubMed] [Google Scholar]
- Walker S. N., Sechrist K. R., Pender N. J. (1995). Health promotion model—Instruments to measure health promoting lifestyle: Health-Promoting Lifestyle Profile [HPLP II] (Adult Version). Retrieved from http://deepblue.lib.umich.edu/handle/2027.42/85349
- Wang L., Watts A., Anderson R. A., Little T. (2013). Common fallacies in quantitative research. In Little T. D. (Ed.), Oxford handbook of quantitative methods (pp. 718-758). New York, NY: Guilford. doi: 10.1093/oxfordhb/9780199934898.013.0031 [DOI] [Google Scholar]
- Wang Y., Hunt K., Nazareth I., Freemantle N., Petersen I. (2013). Do men consult less than women? An analysis of routinely collected UK general practice data. BMJ Open, 3, 8. doi: 10.1136/bmjopen-2013-003320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weden M. M., Carpiano R., Robert S. A. (2008). Subjective and objective neighborhood characteristics and adult health. Social Science & Medicine, 66, 1256-1270. doi: 10.1016/j.socscimed.2007.11.041 [DOI] [PubMed] [Google Scholar]
- Wood L., Frank L. D., Giles-Corti B. (2010). Sense of community and its relationship with walking and neighborhood design. Social Science & Medicine, 70, 1381-1390. doi: 10.1016/j.socscimed.2010.01.021 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (1946). Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference. New York, NY: Author. [Google Scholar]