Abstract
Managing patients with erectile dysfunction (ED) who failed to respond to phosphodiesterase type 5 inhibitors (PDE5is) is a challenging task. Recently, low-intensity extracorporeal shockwave therapy (LI-ESWT) was reported to improve ED by enhancing perfusion of the penis. The current study was performed to evaluate whether combined treatment with LI-ESWT and PDE5is can restore erectile function in patients who failed to respond to PDE5is alone. This was an open-label single-arm prospective study. ED patients with an erection hardness score (EHS) ≦2 under a maximal dosage of PDE5is were enrolled. Sociodemographic information and detailed medical history were recorded. LI-ESWT treatment consisted of 3,000 shockwaves once weekly for 12 weeks. All patients continued their regular PDE5is use. The EHS and the 5-item version of the International Index of Erectile Function (IIEF-5) were used to evaluate the change in erectile function 1 and 3 months after LI-ESWT. A total of 52 patients were enrolled. After LI-ESWT treatment, 35 of the 52 patients (67.3%) could achieve an erection hard enough for intercourse (EHS ≧ 3) under PDE5is use at the 1-month follow-up. Initial severity of ED was the only significant predictor of a successful response (EHS1: 35.7% vs. EHS2: 78.9%, p = .005). Thirty-three of the 35 (94.3%) subjects who responded to LI-ESWT could still maintain their erectile function at the 3-month follow-up. LI-ESWT can serve as a salvage therapy for ED patients who failed to respond to PDE5is. Initial severity of ED was an important predictor of a successful response.
Keywords: shockwave therapy, erectile dysfunction, phosphodiesterase type 5 inhibitor, erection hardness score
Erectile dysfunction (ED) is defined as a persistent inability to attain and maintain an erection sufficient to permit satisfactory sexual performance that often lasts for more than 6 months (NIH Consensus Conference, 1993). It is a common disorder in men older than 40 years, with the highest prevalence in Asian men, as reported in a global study (Laumann et al., 2005). In Taiwan, the prevalence of ED in men older than 40 years has been reported to be 26.0% to 54.3% (Hwang, Tsai, Lin, Chiang, & Chang, 2010; Liu et al., 2010; Wu et al., 2007). Although the pathophysiology of ED is usually multifactorial, the most common etiology is vasculogenic disorders (Dean, & Lue, 2005; Jackson et al., 2010; Shamloul, & Ghanem, 2013). Phosphodiesterase type 5 inhibitors (PDE5is), which result in increased arterial blood flow and penile erection, often serve as first-line treatment for patients with ED, due to their convenience and good efficacy (Hatzimouratidis et al., 2016; Porst et al., 2013). Up to 30% to 40% of patients with ED may not respond sufficiently to the maximum dose of PDE5is (Porst et al., 2013).
Traditional second-line treatments including intracavernosal injections, intraurethral injections, or use of vacuum constrictive devices could serve as salvage therapy for patients who failed to respond to PDE5is. If second-line treatments fail or are not preferred by the patients, penile prosthesis implantation is usually the last resort treatment for ED (Porst et al., 2013; Shamloul, & Ghanem, 2013). Although the above treatments are usually effective, they have many drawbacks, such as their invasiveness, inconvenience, or nonnatural status.
Low-intensity extracorporeal shock wave therapy (LI-ESWT), a noninvasive therapy, has been applied recently in the treatment of ED because it can induce neovascularization and increase blood flow in cavernosal tissues to improve erectile function (Chung, & Cartmill, 2015; Vardi, Appel, Jacob, Massarwi, & Gruenwald, 2010; Vardi, Appel, Kilchevsky, & Gruenwald, 2012). Although most of the published results report that LI-ESWT can be a useful treatment for patients with mild-to-moderate ED, especially those who respond to PDE5is (Srini, Reddy, Shultz, & Denes, 2015; Vardi et al., 2010, 2012), few studies have evaluated the role of LI-ESWT in patients with severe ED who were nonresponders to PDE5is, especially in Asia (Bechara, Casabe, De Bonis, & Nazar, 2015; Gruenwald, Appel, & Vardi, 2012; Kitrey et al., 2016). An initial report from Gruenwald et al. (2012) identified that only one third of patients with severe ED were able to recover an erection hard enough for sexual intercourse using LI-ESWT after a PDE5i washout. LI-ESWT was recently reported to improve erectile function independent of the nitric oxide (NO)/cyclic guanosine monophosphate (cGMP) pathway, and it could potentiate its effect in combination with PDE5i use in a type 2 diabetes mellitus rat model (Assaly-Kaddoum et al., 2016). It would be reasonable to combine LI-ESWT and PDE5i to maximize treatment effects in patients with severe ED (Bechara et al., 2015; Gruenwald et al, 2012; Kitrey et al., 2016). The aim of the current study was to evaluate whether combined treatment with LI-ESWT and PED5is could restore erectile function in Taiwanese patients who failed to respond to PDE5is alone.
Methods
This was an open-label single-arm prospective study. Patients who were not able to achieve an erection hard enough for vaginal penetration (erection hardness score, EHS ≦2) after taking a maximal dosage of PDE5is between April 2015 and December 2016 were enrolled from Kaohsiung Medical University–affiliated hospitals, Kaohsiung Municipal Ta-Tung Hospital, and Pingtung Hospital, which are all located in southwestern Taiwan. Eligible subjects were aged more than 20 years and in a stable relationship and had had ED at least 6 months with an insufficient response to any of the PDE5is at a maximal dosage and after adequate education. The PDE5is and dosages used were sildenafil (100 mg), tadalafil (20 mg), and vardenafil (20 mg) with a trial of at least four times, or tadalafil (5 mg) with a trial of at least 28 days (Porst et al., 2013). If unrecognized hypogonadism with serum total testosterone levels below 350 ng/dL was noted during initial screening, a testosterone replacement therapy (TRT) trial of at least 3 months was performed first to restore testosterone levels to a normal range (Aversa, Francomano, & Lenzi, 2015; Wang et al., 2009). Only those subjects who still failed to respond to PDE5is (EHS ≦2) after their hypogonadism was corrected were enrolled. Subjects were excluded if they had significant coagulopathy, penile anatomical abnormalities, neurological abnormalities, unstable psychiatric disorders, uncorrected hormone abnormalities, clinically significant medical diseases, or a history of extensive pelvic surgery or irradiation. The study protocol was approved by the Institutional Review Board of Kaohsiung Medical University Hospital. Each participant provided and signed informed consent.
Initial Screening
All participants were assessed using a structured questionnaire to collect their demographic information and detailed medical, surgical, and psychosexual history. The well-known risk factors for ED, including diabetes mellitus, hypertension, hyperlipidemia, cardiovascular disease, stroke, alcohol drinking, and cigarette smoking, were completely reviewed. Subjects were classified as alcohol drinkers or cigarette smokers if they had regularly consumed any alcoholic beverage ≥1 time per week, or had smoked ≥10 cigarettes per week, respectively, for at least 6 months. Current users were those who were still using any of these substances within 1 year before the interview (Liu et al., 2012, 2015). In addition to a detailed physical examination, 20-mL blood samples were drawn from all participants between 8:00 AM and 11:00 AM, after an overnight fasting of more than 8 hr, for analyses of serum glucose, lipid panels, routine biochemical profiles, and total testosterone levels. Erectile function of each participant under a maximal dosage of PDE5i was assessed using EHS and an abridged, 5-item version of the International Index of Erectile Function (IIEF-5).
Treatment Protocol
All participants received LI-ESWT (Duolith SD1 T-TOP, Storz, Switzerland) once weekly for 12 weeks in an outpatient setting, without local or systemic anesthesia. At each treatment session, a total of 3,000 shocks of LI-ESWT were applied at six sites (500 shocks per site at the bilateral distal and proximal parts of the corpus cavernosa and the bilateral crural areas) with an energy setting of 0.15 mJ/mm2 intensity at a frequency of 240 shocks/min. Since the penetration depth of LI-ESWT is enough to cover the bilateral corpus cavernosa, the level of application at bilateral sites differed to achieve maximal penile treatment. During the LI-ESWT treatment period, all patients remained on their regular high on-demand or once-daily PDE5i dosing schedules. In subjects with concomitant hypogonadism, TRT was also performed simultaneously, unless their condition had improved.
Outcome Measures of LI-ESWT
Erectile function of the participants was reassessed using EHS and IIEF-5 at 1 and 3 months after a complete course of LI-ESWT and with regular PDE5is use. The main outcome measure for efficacy of LI-ESWT was EHS. Success of treatment was defined as EHS 3 or greater, which indicated the regaining of an erection sufficient for vaginal penetration (Mulhall, Levine, & Junemann, 2006). During treatment, any adverse effect associated with LI-ESWT, like penile pain or ecchymosis, was recorded.
Statistical Analysis
Quantitative data were represented as mean ± standard deviation (SD) and median with interquartile range (IQR), unless otherwise indicated. Categorical data were represented by number (n) and percentage. To quantify the difference between subjects with and without response to LI-ESWT, qualitative variables were compared using the chi-square test and Fisher’s exact test, while quantitative variables were compared using Student’s t-test. For all statistical analyses, p < .05 was considered statistically significant. All statistical operations were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, U.S.A.).
Results
A total of 52 patients with a mean age of 60.1 ± 11.5 years (median: 63.0 years, IQR: 52.5–68.0, range: 33.0–79.0) were enrolled. The mean history of ED was 38.3 ± 26.9 months (median: 33.0 months, IQR: 18.0–60.0). More than half of the patients had been diagnosed as having hypertension (51.9%) and hyperlipidemia (59.6%). The prevalence of diabetes mellitus and cardiovascular disease was 26.3% and 13.5%, respectively. The mean serum total testosterone level was 501.4 ± 183.6 ng/dL (median: 476.5 ng/dL, IQR: 378.4–611.2). Nine of the 52 patients (17.3%) had serum total testosterone levels below 350 ng/dL (Table 1).
Table 1.
Baseline Characteristics of the Study Population (n = 52).
| Parameter | No (%) | Mean ± SD | Median | IQR |
|---|---|---|---|---|
| Age (years) | 60.1 ± 11.5 | 63.0 | 52.5–68.0 | |
| Body mass index (kg/m2) | 25.3 ± 2.3 | 25.1 | 23.5–26.2 | |
| Erectile dysfunction history (month) | 38.3 ± 26.9 | 33.0 | 18.0–60.0 | |
| Diabetes mellitus | 14 (26.3) | |||
| Hypertension | 27 (51.9) | |||
| Dyslipidemia | 31 (59.6) | |||
| Cardiovascular disease | 7 (13.5) | |||
| Stroke | 0 (0) | |||
| Current smoking | 11 (21.2) | |||
| Current alcohol drinking | 9 (17.3) | |||
| Laboratory data | ||||
| Testosterone (ng/dL) | 501.4 ± 183.6 | 476.5 | 378.4–611.2 | |
| Triglycerides (mg/dL) | 112.1 ± 57.4 | 90.5 | 73.8–154.8 | |
| Total cholesterol (mg/dL) | 191.1 ± 33.9 | 191.5 | 161.8–211.5 | |
| High-density lipoprotein (mg/dL) | 46.9 ± 13.6 | 45.3 | 35.4–55.3 | |
| Fasting sugar (mg/dL) | 114.2 ± 36.6 | 102.5 | 94.8–116.5 |
Note. IQR = interquartile range; SD = standard deviation.
With regard to medical treatment with an insufficient response (EHS ≦2) before LI-ESWT, 40 (76.9%), 11 (21.2%), and 2 (3.8%) patients failed to respond to a maximal dosage of sildenafil (100 mg), tadalafil (20 mg), and vardenafil (20 mg), individually, in a trial of at least four times. In addition, 28 (53.8%) patients also failed to respond to a tadalafil (5 mg) daily dosage in a trial of at least 28 days. Nearly half of the study population (48.1%) had tried different kinds of PDE5is before LI-ESWT, but still failed. In nine patients (17.3%) with serum total testosterone levels below 350 ng/dL, as noted in the initial screening, a TRT trial of at least 3 months was performed first, in addition to PDE5is use. The nine patients still had an insufficient response (EHS ≦2), even after serum total testosterone levels returned to normal. During LI-ESWT treatment, those subjects continued TRT in addition to PDE5is use (Table 2).
Table 2.
Medical Treatments With Insufficient Response (Erection Hardness Score ≦2) Before Shockwave Therapy.
| Phosphodiesterase type 5 inhibitors | N (%) | Adjuvant TRT (N) |
|---|---|---|
| Sildenafil (100 mg) | 19 (36.6) | 2 |
| Tadalafil (5 mg) daily use | 8 (15.4) | 0 |
| Sildenafil (100 mg) and vardenafil (20 mg) | 1 (1.9) | 1 |
| Sildenafil (100 mg) and tadalafil (20 mg) | 4 (7.7) | 1 |
| Sildenafil (100 mg) and tadalafil (5 mg) daily use | 12 (23.1) | 3 |
| Tadalafil (20 mg) and tadalafil (5 mg) daily use | 4 (7.7) | 1 |
| Sildenafil (100 mg), vardenafil (20 mg), and tadalafil (5 mg) daily use | 1 (1.9) | 0 |
| Sildenafil (100 mg), tadalafil (20 mg), and tadalafil (5 mg) daily use | 3 (5.8) | 1 |
| Total | 52 (100.0) | 9 |
Note. TRT = testosterone replacement therapy.
Changes in erectile function at the 1-month and 3-month follow-up after 12 weeks of LI-ESWT revealed the following. The mean value of the EHS score increased from 1.7 ± 0.4 to 2.8 ± 0.8, with a difference of 1.1 ± 0.7 (p < .001) at the 1-month follow-up. Thirty-five of 52 patients (67.3%) had a successful response to LI-ESWT, with 28 (53.8%) achieving EHS 3, and 7 (13.5%) achieving EHS 4, which indicated sufficient erections for vaginal penetration during sexual intercourse under PDE5is use. The mean value of the IIEF-5 increased from 9.6 ± 2.9 to 15.0 ± 5.0 points, with a difference of 5.4 ± 3.7 ( p < .001) at the 1-month follow-up. The improvement of EHS and IIEF-5 were persistent at the 3-month follow-up (Table 3). No adverse effect associated with LI-ESWT, like penile pain or ecchymosis, was reported in any of the patients.
Table 3.
Change of Erectile Function After Shockwave Therapy at the 1-Month and 3-Month Follow-up.
| Baseline | 1 month after treatment | Difference | 3 months after treatment | Difference | |
|---|---|---|---|---|---|
| Erectile hardness score | 1.7 ± 0.4 | 2.8 ± 0.8 | 1.1 ± 0.7a | 2.7±0.8 | 1.0 ± 0.7a |
| 1 | 14 (26.9) | 3 (5.8) | 3 (5.8) | ||
| 2 | 38 (73.1) | 14 (26.9) | 16 (30.8) | ||
| 3 | 0 (0) | 28 (53.8) | 27 (51.9) | ||
| 4 | 0 (0) | 7 (13.5) | 6 (11.5) | ||
| IIEF-5 score | 9.6 ± 2.9 | 15.0 ± 5.0 | 5.4 ± 3.7a | 15.4 ± 4.9 | 5.8 ± 3.4a |
Note. IIEF-5 = 5-item version of the International Index of Erectile Function.
p < .001.
Clinical characteristics and laboratory data of subjects with and without a response to LI-ESWT at the 1-month follow-up revealed no significant difference in age, body mass index (BMI), history of ED, comorbidities, current cigarette smoking and alcohol drinking, or laboratory data (Table 4). Subjects with more severe ED at baseline had a significantly low response rate to LI-ESWT (EHS1: 35.7% vs. EHS2: 78.9%, p = .005). IIEF-5 score at baseline was also significantly lower in subjects without response to LI-ESWT compared to those with response (8.1 ± 2.8 vs. 10.4 ± 2.7, p = .01). The result is still significant even after adjusting for age, BMI, history of ED, comorbidities, and current cigarette smoking and alcohol drinking (EHS1 vs. EHS2, adjusted odds ratio: .08, 95% CI[0.013, 0.520], p = .008).
Table 4.
Comparison of Clinical Characteristics and Laboratory Data Between Subjects With and Without Response to Shockwave Therapy.
| Parameter | Subjects without response (N = 17) |
Subjects with response (N = 35) |
p value |
|---|---|---|---|
| Age (years) | 61.4 ± 10.5 | 59.4 ± 12.1 | .57 |
| Body mass index (kg/m2) | 25.8 ± 2.9 | 25.1 ± 2.0 | .29 |
| Duration of erectile dysfunction (month) | 39.6 ± 24.1 | 37.6 ± 27.1 | .80 |
| Severity of erectile dysfunction, n (%) | |||
| Initial EHS1 | 9 (64.3) | 5 (35.7) | .005 |
| Initial EHS2 | 8 (21.1) | 30 (78.9) | |
| IIEF-5 | 8.1 ± 2.8 | 10.4 ± 2.7 | .01 |
| Diabetes mellitus, n (%) | 7 (50.0) | 7 (50.0) | .11 |
| Diabetes mellitus with insulin control, n (%) | 3 (60.0) | 2 (40.0) | .37 |
| Hypertension, n (%) | 8 (29.6) | 19 (70.4) | .63 |
| Dyslipidemia, n (%) | 11 (35.5) | 20 (64.5) | .60 |
| Cardiovascular disease, n (%) | 2 (28.6) | 5 (71.4) | .80 |
| Stroke, n (%) | 0 (0) | 0 (0) | |
| Hypogonadism, n (%) | 4 (44.4) | 5 (55.6) | .41 |
| Current smoking, n (%) | 3 (27.3) | 8 (72.7) | .19 |
| Current alcohol drinking, n (%) | 1 (11.1) | 8 (88.9) | .13 |
| Number of comorbidities | 2.0 ± 1.3 | 1.7 ± 1.2 | .29 |
| Laboratory data | |||
| Total testosterone (ng/dL) | 492.9 ± 198.3 | 505.6 ± 178.9 | .82 |
| Triglycerides (mg/dL) | 104.9 ± 56.4 | 115.9 ± 58.5 | .52 |
| Total cholesterol (mg/dL) | 189.0 ± 35.4 | 192.2 ± 33.6 | .76 |
| High-density lipoprotein (mg/dL) | 47.4 ± 17.4 | 46.6 ± 11.5 | .86 |
| Fasting blood sugar (mg/dL) | 132.4 ± 54.7 | 104.8 ± 16.9 | .058 |
Note. EHS = erection hardness score; IIEF-5 = 5-item version of the International Index of Erectile Function.
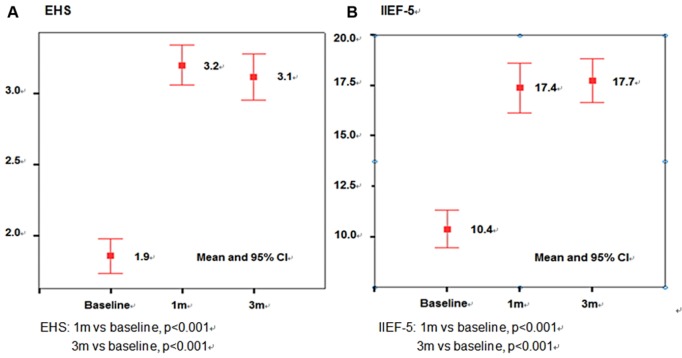
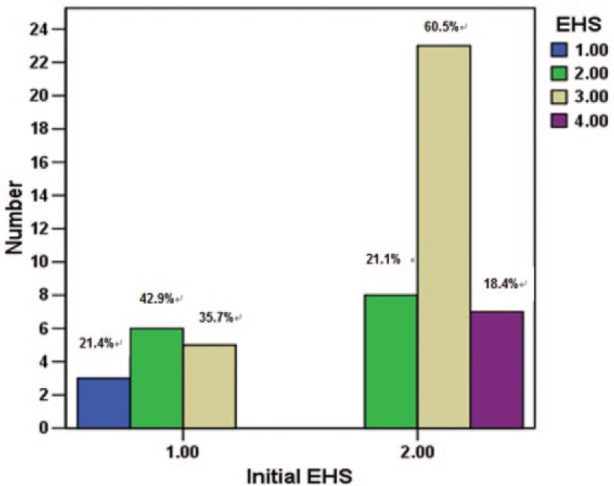
Figure 1 presents the improvement in erectile function 1 month after LI-ESWT in patients with different initial EHS scores. Of 38 subjects with an initial EHS 2, 23 (60.5%) achieved EHS 3 and 7 (18.4%) achieved EHS 4. However, only 5 of 14 subjects (35.7%) with an initial EHS 1 could achieve EHS 3, and none could achieve EHS 4 (Figure 1). In 35 subjects who responded to LI-ESWT, the mean value of the EHS score increased from 1.9 ± 0.4 to 3.2 ± 0.4 at the 1-month follow-up and 3.1 ± 0.5 at the 3-month follow-up, respectively (both p < .001). The mean value of the IIEF-5 also increased from 10.4 ± 2.7 to 17.4 ± 3.6 and 17.7 ± 3.2 points, respectively (both p < .001; Figure 2). Thirty-three of the 35 (94.3%) subjects who responded to LI-ESWT could still achieve EHS 3 or greater with PDE5is use at the 3-month follow-up (Table 3).
Figure 1.
Improvement of erectile function after shockwave therapy in patients with different initial erection hardness scores (EHSs).
Figure 2.
Improvement of erectile function in subjects who responded to shockwave therapy at the 1-month and 3-month follow-up (n = 35).
Note. EHS = erection hardness score; IIEF-5 = 5-item version of the International Index of Erectile Function.
Discussion
In the current study, nearly two thirds of the ED patients (67.3%) who failed to respond to PDE5is (EHS ≦2) could achieve an erection sufficient for vaginal penetration during sexual intercourse (EHS ≧3) after 12 weeks of LI-ESWT treatment; 94.3% of those subjects were able to maintain their erectile function (EHS ≧3) at the 3-month follow-up. In addition, no one reported any adverse effect associated with LI-ESWT.
PDE5is have been widely accepted as first-line treatment for ED that can facilitate erection by inhibiting the PDE5 enzyme. This enzyme is specifically responsible for the degradation of cGMP in the cavernous smooth muscles. Use of PDE5is can result in prolonged cGMP activity, which further decreases intracellular calcium concentrations and maintains smooth muscle relaxation, leading to rigid penile erection. Up to 30% to 40% of patients with ED may not sufficiently respond to a maximum dose of PDE5is (Porst et al., 2013). Adequate education for the optimization of PDE5i use, lifestyle modification, controlling of vascular and psychosocial risk factors, switching to another type or daily dosage of PDE5i, and additional TRT for unrecognized hypogonadism are common strategies for PDE5i nonresponders (Aversa, et al., 2015; Eardley, 2006; Lowe, & Bahnson, 2009; Porst et al., 2013), but their efficacy is usually unsatisfactory.
All of the patients in the current study had received adequate education for the optimization of their PDE5i use, and their hypogonadism was corrected by TRT. Nearly half (48.1%) had tried a different kind of PDE5i before enrolling in this study. Previous reports identified that only a small percentage (5%–12%) of nonresponders to one PDE5i could be satisfactorily rescued with another (Brisson, Broderick, Thiel, Heckman, & Pinkstaff, 2006; Porst et al., 2013). Although daily dosing of PDE5is has been reported to have a better rescue rate (Kim, Seftel, Goldfischer, Ni, & Burns, 2014; McMahon, 2004; Porst et al., 2013), more than half of the patients (53.8%) in the current study failed to respond to daily dosing of tadalafil (5 mg) in a trial of at least 28 days. The salvage rate of TRT in hypogonadal men who failed to respond to PDE5is have been reported with variable ranging from 32% to 100% (Isidori, Buvat, & Corona, 2014). In the meta-analysis from Corona et al. (2014), TRT was only reported to be positive on PDE5is outcome in uncontrolled studies, but not in placebo-controlled ones. Nine hypogonadal patients in the current study had still failed to respond to PDE5is use even after a TRT trial of at least 3 months to restore their testosterone levels to a normal range. Therefore, this study population represented true nonresponders to PDE5is, which is a significant challenge to manage in clinical practice.
LI-ESWT, a noninvasive treatment that can increase intracavernosal neovascularization, has become a novel, alternative treatment for ED. The mechanism by which LI-ESWT induces angiogenesis has been evaluated in a number of recent studies. Mariotto et al. (2005) demonstrated that extracorporeal shockwaves at a low energy density could enhance endothelial nitric oxide synthase (eNOS) activity and induce enzymatic NO production in human umbilical vein endothelial cells. Wang et al. (2003) identified that LI-ESWT stimulated the expression of angiogenesis-related growth factors and endothelial cell proliferation factors, including NOS, vascular endothelial growth factors (VEGF), and proliferating cell nuclear antigen (PCNA) in a rabbit model. It has been hypothesized that when appropriate energy from LI-ESWT accumulates within the targeted tissues, it will induce shear stress and intracellular microtrauma, and then stimulate eNOS and release of VEGF and PCNA, resulting in neovascularization. This hypothesis has been proven in several animal studies (Goertz et al., 2012, 2014; Tepeköylü et al., 2013). Another possible mechanism through which LI-ESWT can improve ED may be mediated by recruitment of endogenous mesenchymal stem cells. Qiu et al. (2013) reported that LI-ESWT could recruit endogenous mesenchymal stem cells to promote regeneration of neuronal nitric oxide synthase (nNOS)–positive nerves, endothelium, and smooth muscle in the penis, which further ameliorated ED in a diabetes mellitus rat model. Li et al. (2016) reported that LI-ESWT could recruit endogenous progenitor cells and activate Schwann cells to promote angiogenesis and tissue and nerve generation in a rat model of pelvic neurovascular injuries. Assaly-Kaddoum et al. (2016) suggested that the effects of LI-ESWT may not be mediated by a NO/cGMP-dependent mechanism in a rat model of type 2 diabetes. Further investigation is needed to evaluate the efficacy of LI-ESWT in patients with different etiologies of ED and to elucidate possible underlying mechanisms.
Although LI-ESWT has been widely used in urology for Peyronie’s disease and chronic pelvic pain (Fojecki, Tiessen, & Osther, 2017), Vardi et al. first reported the experience of using LI-ESWT in the treatment of ED in 2010 (Vardi et al., 2010). Since that, more and more studies on LI-ESWT have reported positive results in the improvement of ED. The results of the updated meta-analysis of Lu et al. (2017), which analyzed 14 studies (7 randomized controlled trials and 7 cohort studies, n = 833)suggested that LI-ESWT could significantly improve EHS and IIEF in ED patients, although variation in patient’s baseline characteristics, LI-ESWT’s setup parameters, and treatment protocols existed. Few studies have evaluated the role of LI-ESWT in the treatment of patients with ED who were nonresponders to PDE5is, especially in Asia. Only five studies with limited patient numbers were found in a literature review (Table 5; Bechara, Casabe, De Bonis, & Ciciclia, 2016; Chung, & Cartmill, 2015; Gruenwald et al., 2012; Kitrey et al., 2016; Ruffo et al., 2015), and only one study was a randomized controlled trial (Kitrey et al., 2016). Most of these patients had concomitant PDE5is use during and after LI-ESWT, and up to 50% to 72.4% of patients were converted to PDE5i responders (EHS ≧3) after LI-ESWT treatment. The improvement of IIEF-EF or IIEF-5 scores in those studies were all higher than 4 points that were suggested as the minimal clinically important differences (MCIDs) by Rosen et al. in the evaluation of treatment efficacy for ED patients (Rosen, Allen, Ni, & Araujo, 2011). In the current study, nearly two thirds of the patients (67.3%) were converted to PDE5i responders after 12 weeks of LI-ESWT treatment. The mean improvement of IIEF-5 score was 5.4 ± 3.7 at the 1-month follow-up. The current results are compatible with those of previous studies (Table 5). In addition, initial severity of ED was identified as the important predictor of successful response to LI-ESWT. In patients with initial EHS2, 78.9% were able to achieve EHS ≧3, compared to 35.7% of subjects with initial EHS1 (p = .005; Table 4). IIEF-5 score at baseline was also significantly higher in subjects with response to LI-ESWT compared to those without response (10.4 ± 2.7 vs. 8.1 ± 2.8, p = .01). No statistically significant difference in age, BMI, duration of ED, comorbidities, and personal habits was identified in the current study when comparing responders to nonresponders to LI-ESWT. Bechara et al. reported similar results in their 12-month follow-up of LI-ESWT in patients who were nonresponders to PDE5is (Bechara et al., 2016). Hisasue et al. (2016) reported that age and the number of comorbidities were negative predictive factors of therapeutic response to LI-ESWT in a population of ED patients composed of responders and nonresponders to PDE5is. Since different generators and protocols of LI-ESWT were used in those studies, further studies are needed to compare the efficacy of different generators of LI-ESWT and to determine an adequate therapeutic protocol and important predictors of successful response to LI-ESWT in patients with different etiologies of ED.
Table 5.
Literature Review of Studies About Li-ESWT in Patients With Erectile Dysfunction Who Were Nonresponders to PDE5i.
| Study |
Setup of LI-ESWT |
Protocol of LI-ESWT |
Combined PDE5i |
Outcomes |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Authors | Study design | Generator | Patient number | Follow-up (month) | Energy density (mJ/mm2) | No. of pulses each treatment | Frequency (shocks/min) | No. of treatments each week | No. of treatment sites | Total treatment courses (week) | Washout PDE5i before LI-ESWT | Concomitant PDE5i during LI-ESWT | Adjuvant PDE5i after LI-ESWT | EHS ≧3 | IIEF |
| Gruenwald et al., 2012 | Cohort study | Omnispec ED 1000 | 29 | 1, 2 | 0.09 | 1,500 | 120 | 2 | 5 | 9a | Yes | No | Yes | 34.5% without PDE5i (1month); 72.4% with PDE5i (2 months) | IIEF-EF: +3.5 without PDE5i (1 month); +10.0 with PDE5i (2 months) |
| Ruffo et al., 2015 | Cohort study | Renova NR | 31 | 1,3 | 0.09 | 3,600 | NA | 1 | 4 | 4 | Yes | No | NA | NA | IIEF-EF: +4.6 (1 month); +4.5 (3 months) |
| Chung et al., 2015 | Cohort study | Duolith SD1 | 30 | 1,4 | 0.25 | 3,000 | 360 | 2 | 4 | 6 | NA | NA | NA | 50% (6 weeks) | IIEF-5 improvement ≧5: 60% (6 weeks) |
| Kitrey et al., 2015 | RCT | Omnispec ED 1000 | 53 | 1 | 0.09 | 1,500 | 120 | 2 | 5 | 9a | No | Yes | Yes | 54.1% (1 month) | IIEF-EF: +6 (1 month) |
| Bechara et al., 2016 | Cohort study | Renova NR | 40 | 3, 6, 9, 12 | 0.09 | 3,600 | NA | 1 | 4 | 4 | No | Yes | Yes | 60% (3 months) | Responders: IIEF-EF: +9.3 (3 month); +9.1 (12 months) |
| Our study | Cohort study | Duolith SD1 | 52 | 1, 3 | 0.15 | 3,000 | 240 | 1 | 6 | 12 | No | Yes | Yes | 67.3% (1 month) 63.4% (3 months) |
IIEF-5 improvement: +5.4 (1 month); +5.8( 3 months) |
Note. EHS = erection hardness score; IIEF-EF = International Index of Erectile Function-Erectile Function; IIEF-5 = 5-item version of the International Index of Erectile Function; LI-ESWT = low-intensity extracorporeal shock wave therapy; NA = not available; PDE5i = phosphodiesterase type 5 inhibitor; RCT = randomized controlled trial.
Include a 3-week interval without treatment.
In the meta-analysis from Lu et al. (Lu et al., 2017), the therapeutic efficacy of LI-ESWT in ED patients seems to last at least 3 months. In the literature review of LI-ESWT in the treatment of patients who were nonresponders to PDE5is, most of the studies reported similar results (Table 5). In the current study, 33 of the 35 (94.3%) subjects who responded to LI-ESWT could still maintain EHS3 or greater with PDE5is use at the 3-month follow-up (Table 3). The improvement of IIEF-5 score was also persistent at the 3-month follow-up (Figure 2). Recently, Bechara et al. reported that 91.7% of responders to LI-ESWT, who were nonresponders to PDE5is before, could still maintain their responses after the 12-month follow-up (Bechara et al, 2016). Further large studies, especially randomized controlled trials, are needed to elucidate the long-term efficacy and cost-effectiveness of LI-ESWT in the treatment of ED patients.
There are several limitations to the current study. First, this study design is a single-arm prospective study without controls or comparison group with other form of therapy. Second, the patient number was limited, so it is difficult to compare the efficacy of LI-ESWT in different etiologies of ED. Third, the follow-up period was only 3 months, so the long-term efficacy of LI-ESWT could not be evaluated. Further large and long-term studies are needed to clarify these questions.
In conclusion, LI-ESWT can serve as a salvage therapy in ED patients who failed to response to PDE5is. Nearly two thirds of the patients in the current study could be converted to PDE5i responders (EHS ≧3) and 94.3% could maintain their erectile function at the 3-month follow-up. Initial severity of ED was the only significant predictor of successful response to LI-ESWT. Further studies are needed to compare the efficacy of different generators of LI-ESWT and to determine an adequate therapeutic protocol and important predictors in patients with different etiologies of ED.
Acknowledgments
The authors thank Superintendent Yuh-Min Cheng for his support to introduce LI-ESWT into Pingtung Hospital and perform this study.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported in part by grants from the Ministry of Science and Technology, Taiwan (MOST 103-2314-B-037-066-MY2; MOST 105-2314-B-037-015-; MOST 106-2314-B-037-065-MY3), Kaohsiung Municipal Ta-Tung Hospital, Kaohsiung, Taiwan (KMTTH104-3R23), Kaohsiung Medical University Hospital, Kaohsiung, Taiwan (KMUH104-4R46; KMUH105-5R43), and Research Center for Environmental Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan (KMU-TP104A08; KMU-TP105A09). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- Assaly-Kaddoum R., Giuliano F., Laurin M., Gorny D., Kergoat M., Bernabé J., . . . Behr-Roussel D. (2016). Low intensity extracorporeal shock wave therapy improves erectile function in a model of type II diabetes independently of NO/cGMP pathway. Journal of Urology, 196(3), 950–956. [DOI] [PubMed] [Google Scholar]
- Aversa A., Francomano D., Lenzi A. (2015). Does testosterone supplementation increase PDE5-inhibitor responses in difficult-to-treat erectile dysfunction patients? Expert Opinion on Pharmacotherapy, 16(5), 625–628. [DOI] [PubMed] [Google Scholar]
- Bechara A., Casabe A., De Bonis W., Ciciclia P. G. (2016). Twelve-month efficacy and safety of low-intensity shockwave therapy for erectile dysfunction in patients who do not respond to phosphodiesterase type 5 inhibitors. Sexual Medicine, 4(4), e225–e232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bechara A., Casabe A., De Bonis W., Nazar J. (2015). Effectiveness of low-intensity extracorporeal shock wave therapy on patients with erectile dysfunction (ED) who have failed to respond to PDE5i therapy. A pilot study. Archivos Españoles de Urología, 68(2), 152–160. [PubMed] [Google Scholar]
- Brisson T. E., Broderick G. A., Thiel D. D., Heckman M. G., Pinkstaff D. M. (2006). Vardenafil rescue rates of sildenafil nonresponders: Objective assessment of 327 patients with erectile dysfunction. Urology, 68(2), 397–401. [DOI] [PubMed] [Google Scholar]
- Chung E., Cartmill R. (2015). Evaluation of clinical efficacy, safety and patient satisfaction rate after low-intensity extracorporeal shockwave therapy for the treatment of male erectile dysfunction: An Australian first open-label single-arm prospective clinical trial. BJU International, 115(5), 46–49. [DOI] [PubMed] [Google Scholar]
- Corona G., Isidori A. M., Buvat J., Aversa A., Rastrelli G., Hackett G., . . . Maggi M. (2014). Testosterone supplementation and sexual function: A meta-analysis study. Journal of Sexual Medicine, 11(6), 1577–1592. [DOI] [PubMed] [Google Scholar]
- Dean R. C., Lue T. F. (2005). Physiology of penile erection and pathophysiology of erectile dysfunction. Urologic Clinics of North America, 32(4), 379–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eardley I. (2006). Optimisation of PDE5 inhibitor therapy in men with erectile dysfunction: Converting “non-responders” into “responders”. European Urology, 50(1), 31–33. [DOI] [PubMed] [Google Scholar]
- Fojecki G. L., Tiessen S., Osther P. J. (2017). Extracorporeal shock wave therapy (ESWT) in urology: A systematic review of outcome in Peyronie’s disease, erectile dysfunction and chronic pelvic pain. World Journal of Urology, 35(1), 1–9. [DOI] [PubMed] [Google Scholar]
- Goertz O., Lauer H., Hirsch T., Ring A., Lehnhardt M., Langer S., . . . Hauser J. (2012). Extracorporeal shock waves improve angiogenesis after full thickness burn. Burns, 38(7), 1010–1018. [DOI] [PubMed] [Google Scholar]
- Goertz O., von der Lohe L., Lauer H., Khosrawipour T., Ring A., Daigeler A., . . . Kolbenschlag J. (2014). Repetitive extracorporeal shock wave applications are superior in inducing angiogenesis after full thickness burn compared to single application. Burns, 40(7), 1365–1374. [DOI] [PubMed] [Google Scholar]
- Gruenwald I., Appel B., Vardi Y. (2012). Low-intensity extracorporeal shock wave therapy–A novel effective treatment for erectile dysfunction in severe ED patients who respond poorly to PDE5 inhibitor therapy. Journal of Sexual Medicine, 9(1), 259–264. [DOI] [PubMed] [Google Scholar]
- Hatzimouratidis K., Salonia A., Adaikan G., Buvat J., Carrier S., El-Meliegy A., . . . Khera M. (2016). Pharmacotherapy for erectile dysfunction: Recommendations from the fourth International Consultation for Sexual Medicine (ICSM 2015). Journal of Sexual Medicine, 13(4), 465–488. [DOI] [PubMed] [Google Scholar]
- Hisasue S., China T., Horiuchi A., Kimura M., Saito K., Isotani S., . . . Horie S. (2016). Impact of aging and comorbidity on the efficacy of low-intensity shock wave therapy for erectile dysfunction. International Journal of Urology, 23(1),80–84. [DOI] [PubMed] [Google Scholar]
- Hwang T. I., Tsai T. F., Lin Y. C., Chiang H. S., Chang L. S. (2010). A survey of erectile dysfunction in Taiwan: Use of the erection hardness score and quality of erection questionnaire. Journal of Sexual Medicine, 7(8), 2817–2824. [DOI] [PubMed] [Google Scholar]
- Isidori A. M., Buvat J., Corona G. (2014). A critical analysis of the role of testosterone in erectile function: From pathophysiology to treatment-a systematic review. European Urology, 65(1), 99–112. [DOI] [PubMed] [Google Scholar]
- Jackson G., Montorsi P., Adams M. A., Anis T., El-Sakka A., Miner M., . . . Kim E. (2010). Cardiovascular aspects of sexual medicine. Journal of Sexual Medicine, 7(4 Pt 2), 1608–1626. [DOI] [PubMed] [Google Scholar]
- Kim E. D., Seftel A. D., Goldfischer E. R., Ni X., Burns P. R. (2014). A return to normal erectile function with tadalafil once daily after an incomplete response to as-needed PDE5 inhibitor therapy. Journal of Sexual Medicine, 11(3), 820–830. [DOI] [PubMed] [Google Scholar]
- Kitrey N. D., Gruenwald I., Appel B., Shechter A., Massarwa O., Vardi Y. (2016). Penile low intensity shock wave treatment is able to shift PDE5i nonresponders to responders: A double-blind, sham controlled study. Journal of Urology, 195(5), 1550–1555. [DOI] [PubMed] [Google Scholar]
- Laumann E. O., Nicolosi A., Glasser D. B., Paik A., Gingell C., Moreira E,. . . . GSSAB Investigators’ Group. (2005). Sexual problems among women and men aged 40-80 y: Prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. International Journal of Impotence Research, 17(1), 39–57. [DOI] [PubMed] [Google Scholar]
- Li H., Matheu M. P., Sun F., Wang L., Sanford M. T., Ning H., . . . Lue T. F. (2016). Low-energy shock wave therapy ameliorates erectile dysfunction in a pelvic neurovascular injuries rat model. Journal of Sexual Medicine, 13(1), 22–32. [DOI] [PubMed] [Google Scholar]
- Liu C. C., Juan H. C., Lee Y. C., Wu W. J., Wang C. J., Ke H. L., . . . Huang S. P. (2010). The impact of physical health and socioeconomic factors on sexual activity in middle-aged and elderly Taiwanese men. Aging Male, 13(2), 148–153. [DOI] [PubMed] [Google Scholar]
- Liu C. C., Lee Y. C., Tsai V. F., Cheng K. H., Wu W. J., Bao B. Y., . . . Huang S. P. (2015). The interaction of serum testosterone levels and androgen receptor CAG repeat polymorphism on the risk of erectile dysfunction in aging Taiwanese men. Andrology, 3(5), 902–908. [DOI] [PubMed] [Google Scholar]
- Liu C. C., Lee Y. C., Wang C. J., Yeh H. C., Li W. M., Wu W. J., . . . Huang S. P. (2012). The impact of androgen receptor CAG repeat polymorphism on andropausal symptoms in different serum testosterone levels. Journal of Sexual Medicine, 9(9), 2429–2437. [DOI] [PubMed] [Google Scholar]
- Lowe G., Bahnson R. (2009). Non-invasive management of primary phosphodiesterase type 5 inhibitor failure in patients with erectile dysfunction. Therapeutic Advances in Urology, 1(5), 235–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Z., Lin G., Reed-Maldonado A., Wang C., Lee Y. C., Lue T. F. (2017). Low-intensity extracorporeal shock wave treatment improves erectile function: A systematic review and meta-analysis. European Urology, 71(2), 223–233. [DOI] [PubMed] [Google Scholar]
- Mariotto S., Cavalieri E., Amelio E., Ciampa A. R., de Prati A. C., Marlinghaus E., . . . Suzuki H. (2005). Extracorporeal shock waves: From lithotripsy to anti-inflammatory action by NO production. Nitric Oxide, 12(2), 89–96. [DOI] [PubMed] [Google Scholar]
- McMahon C. (2004). Efficacy and safety of daily tadalafil in men with erectile dysfunction previously unresponsive to on-demand tadalafil. Journal of Sexual Medicine, 1(3), 292–300. [DOI] [PubMed] [Google Scholar]
- Mulhall J. P., Levine L. A., Junemann K. P. (2006). Erection hardness: A unifying factor for defining response in the treatment of erectile dysfunction. Urology, 68(3), 17–25. [DOI] [PubMed] [Google Scholar]
- NIH Consensus Conference. (1993). Impotence. NIH Consensus Development Panel on Impotence. JAMA, 270(1), 83–90. [PubMed] [Google Scholar]
- Porst H., Burnett A., Brock G., Ghanem H., Giuliano F., Glina S., . . . ISSM Standards Committee for Sexual Medicine. (2013). SOP conservative (medical and mechanical) treatment of erectile dysfunction. Journal of Sexual Medicine, 10(1), 130–171. [DOI] [PubMed] [Google Scholar]
- Qiu X., Lin G., Xin Z., Ferretti L., Zhang H., Lue T. F., Lin C. S. (2013). Effects of low-energy shockwave therapy on the erectile function and tissue of a diabetic rat model. Journal of Sexual Medicine, 10(3), 738–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen R. C., Allen K. R., Ni X., Araujo A. B. (2011). Minimal clinically important differences in the erectile function domain of the International Index of Erectile Function scale. European Urology, 60(5), 1010–1016. [DOI] [PubMed] [Google Scholar]
- Ruffo A., Capece M., Prezioso D., Romeo G., Illiano E., Romis L., . . . Iacono F. (2015). Safety and efficacy of low intensity shockwave (LISW) treatment in patients with erectile dysfunction. International Brazilian Journal Of Urology, 41(5), 967–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamloul R., Ghanem H. (2013). Erectile dysfunction. Lancet, 381(9861), 153–165. [DOI] [PubMed] [Google Scholar]
- Srini V. S., Reddy R. K., Shultz T., Denes B. (2015). Low intensity extracorporeal shockwave therapy for erectile dysfunction: A study in an Indian population. The Canadian Journal of Urology, 22(1), 7614–7622. [PubMed] [Google Scholar]
- Tepeköylü C., Wang F. S., Kozaryn R., Albrecht-Schgoer K., Theurl M., Schaden W., . . . Holfeld J. (2013). Shock wave treatment induces angiogenesis and mobilizes endogenous CD31/CD34-positive endothelial cells in a hindlimb ischemia model: Implications for angiogenesis and vasculogenesis. Journal of Thoracic and Cardiovascular Surgery, 146(4), 971–978. [DOI] [PubMed] [Google Scholar]
- Vardi Y., Appel B., Jacob G., Massarwi O., Gruenwald I. (2010). Can low-intensity extracorporeal shockwave therapy improve erectile function? A 6-month follow-up pilot study in patients with organic erectile dysfunction. European Urology, 58(2), 243–248. [DOI] [PubMed] [Google Scholar]
- Vardi Y., Appel B., Kilchevsky A., Gruenwald I. (2012). Does low intensity extracorporeal shock wave therapy have a physiological effect on erectile function? Short-term results of a randomized, double-blind, sham controlled study. Journal of Urology, 187(5), 1769–1775. [DOI] [PubMed] [Google Scholar]
- Wang C. J., Wang F. S., Yang K. D., Weng L. H., Hsu C. C., Huang C. S., . . . Yang L. C. (2003). Shock wave therapy induces neovascularization at the tendon-bone junction. A study in rabbits. Journal of Orthopaedic Research, 21(6), 984–989 [DOI] [PubMed] [Google Scholar]
- Wang C., Nieschlag E., Swerdloff R., Behre H. M., Hellstrom W. J., Gooren L. J., . . . Wu F. C. (2009). Investigation, treatment, and monitoring of late-onset hypogonadism in males: ISA, ISSAM, EAU, EAA, and ASA recommendations. European Urology, 55(1), 121–130. [DOI] [PubMed] [Google Scholar]
- Wu C. J., Hsieh J. T., Lin J. S., Hwang T. I., Jiann B. P., Huang S. T., . . . Lin H. D. (2007). Comparison of prevalence between self-reported erectile dysfunction and erectile dysfunction as defined by five-item International Index of Erectile Function in Taiwanese men older than 40 years. Urology, 69(4), 743–747. [DOI] [PubMed] [Google Scholar]