Abstract
Many Australian young men (18-25 years) fail to meet recommendations in national dietary or physical activity (PA) guidelines. However, there is a lack of understanding of their perspectives on PA and diet to inform intervention design. This study examined young men’s motivators and barriers to healthy eating and PA, along with differences by demographic and behavioral factors. A cross-sectional online survey was completed by 282 men aged 18 to 25 years in Australia. Results identified the most common motivators for healthy eating included improving health (63.5%), body image (52.3%), and increasing energy (32.1%). Motivators for PA included improving body image (44.6%), fitness (44.2%), and health (41.0%). Common barriers to healthy eating were access to unhealthy foods (61.1%), time to cook/prepare healthy foods (55.0%), and motivation to cook healthy foods (50.7%). Barriers for PA included motivation (66.3%), time (57.8%), and cost of equipment/facilities (33.3%). Significant differences (p < .01) in motivators to healthy eating and/or PA were identified for BMI category, marital status, PA level, alcohol intake, and stress levels. Significant differences were identified for barriers to healthy eating and/or PA by BMI, PA level, stress, and fruit and vegetable intake, assessed using Pearson’s chi-square test. Findings suggest that promotion of benefits related to health, appearance/body image, increased energy and fitness, and addressing key barriers including motivation, time, financial restraints, and accessibility of unhealthy foods, could engage young men in improving lifestyle behaviors. Differences by demographic and behavioral factors suggest development of tailored programs to address diversity among young men may be required.
Keywords: young men, public health, exercise, nutrition
Introduction
Male life expectancy in Australia is 4 years less than females (80 vs. 84 years; Australian Institute of Health and Welfare, 2016). Improving longevity in men is likely to include lifestyle behavior changes, such as healthy eating and physical activity (PA). Making these changes during young adulthood can help prevent or delay progression to chronic conditions such as cardiovascular disease (CVD) and type 2 diabetes (Liu et al., 2012; Parker, Schmitz, Jacobs, Dengel, & Schreiner, 2007; Pereira et al., 2005). For example, the large prospective CARDIA study in the United States, reported higher levels of PA in young adulthood between the ages of 18 and 30 years was associated with a 5% significantly lower CVD risk profile (Liu et al., 2012) and a 15% reduction in risk of hypertension 20 years later in middle age (Parker et al., 2007), compared with young adults with lower levels of PA. Similarly, those with a healthier dietary pattern as a young adult, consistent with the Alternate Healthy Eating Index (McCullough & Willett, 2006), was significantly associated with a 6% lower CVD risk profile in middle age compared with those with a less healthy one (Liu et al., 2012).
Many young men fail to meet recommendations set out in national guidelines for PA and diet (Australian Bureau of Statistics, 2015b), but are underrepresented in programs that aim to improve these behaviors. Most programs include both sexes (Ashton, Hutchesson, Rollo, Morgan, & Collins, 2014) and all ages (Douketis, Macie, Thabane, & Williamson, 2005; Galani & Schneider, 2007) with the majority of participants middle aged and predominantly female (Pagoto et al., 2012). Using a “one-size-fits-all” approach to intervention design and delivery may not account for the psychological, social, and physical differences between sexes and age groups, highlighting the need for interventions to be sensitive to both gender and age (Oliffe & Greaves, 2012). A recent systematic review of health-related interventions exclusively in young males found few studies, with 10 identified for inclusion (Ashton, Morgan, et al., 2015). Although most demonstrated effectiveness up to 6 months, they commonly encountered difficulties in recruitment, retention, and engagement, or failed to report these (Ashton, Morgan, et al., 2015). None of the included interventions in the review were specifically tailored for young men. Instead, young men were recruited to ensure a homogenous sample or for convenience. The review expressed the need for more participatory research that included young men in program design, in order to personalize the program to their expressed needs, interests and barriers, and to improve understanding of how to successfully engage them in effective health behavior change interventions. A recent scoping review of 25 studies which explored factors to engaging men in chronic disease prevention and management programs identified that traditional programs were seen by men as feminine and a barrier to participation (Gavarkovs, Burke, & Petrella, 2015). Also, physical appearance, history of negative health events, and personal concern for health status were identified as facilitators to participation. However, the majority of responses were obtained from studies with middle-aged and older age groups of men, highlighting the need to obtain responses from young men.
Acquiring perspectives of young men’s motivators and barriers to addressing health behaviors is one example of what can be done within participatory research (Hagen et al., 2012). Some qualitative and quantitative studies have explored young men’s motivators and barriers to healthy eating and PA (Arzu, Tuzun, & Eker, 2006; Ashton, Hutchesson, et al., 2015; Hebden, Chan, Louie, Rangan, & Allman-Farinelli, 2015; Leyk et al., 2012; Walsh, White, & Greaney, 2009), to establish a foundation for young men’s perspectives. Common motivators to both healthy eating and PA include improvements of physical health, appearance, and sports performance (Ashton, Hutchesson, et al., 2015; Walsh et al., 2009). While common barriers to both healthy eating and PA include time restraints, financial implications, and peer influences (Arzu et al., 2006; Ashton, Hutchesson, et al., 2015; Greaney et al., 2009; Leyk et al., 2012; Walsh et al., 2009). Additional barriers that have been reported for healthy eating include taste and convenience of unhealthy foods (Ashton, Hutchesson, et al., 2015; Hebden et al., 2015; Walsh et al., 2009), while access to sports facilities and lack of enjoyment, energy, and support have been identified as additional barriers to PA (Arzu et al., 2006; Leyk et al., 2012). However, the few studies have predominantly been conducted in small university-based samples. This limits the generalizability of results and has prevented any explorations in perceptions by demographic and/or behavioral subgroups of young men.
Novel explorations are required to identify most prevalent responses in young men and explore views based on demographic and behavioral subgroups to identify the magnitude of any heterogeneity that may exist within a group of young men. Ultimately, this information can be used to inform development of targeted health programs for young men as a whole and/or tailored to different subgroups of young men. Therefore, the current study aims to report results of an online survey in young men aged 18 to 25 years to (1) identify the most prevalent motivators and barriers to adopting healthy eating habits and being physically active in order to inform development of a healthy lifestyle intervention for this group and (2) determine whether these responses differ based on body mass index (BMI), marital status, employment status, educational attainment, income, PA level, alcohol use, symptoms of stress, and fruit and vegetable intake.
Method
Study Design
A cross-sectional online survey was applied as a convenient method for the target respondents, allowing for broader reach (Ramo, Hall, & Prochaska, 2011). The online survey included a total of 67 questions, with 28 reported in this article. The remaining questions addressed preferences for intervention components and the delivery medium. The conduct and reporting of this survey adhered to the STROBE statement for cross-sectional studies (Vandenbroucke et al., 2007) and the Checklist for Reporting Results of Internet E-Surveys (Eysenbach, 2004).
Participants and Setting
Eligible participants were males aged 18 to 25 years who lived in Australia. Young men were selected using a purposive sampling technique and recruited via flyers distributed around the local university, technical colleges, and sports clubs. Young men were also recruited via advertisements on social media including Facebook and Twitter which were shared on pages of the student researcher, local university, technical college, Hunter Medical Research Institute, and local newspaper. Furthermore, recruitment entailed a media release to the community in the local newspaper and local and statewide radio stations. Eligible participants were also asked to share the survey link with other young men via e-mail and/or Facebook.
Links to the online survey were provided on all recruitment materials. An information statement outlining the study details was provided on the first page of the survey. Interested individuals who provided consent were then directed to the eligibility screen; those eligible were then directed to complete the online survey. Ineligible participants were informed via the survey, which then terminated.
On survey completion, participants had the option of entering a prize draw to win either an iPad mini or one of five gift vouchers valued at $150 each. The survey was available between July 6 and September 27, 2015. This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the University of Newcastle Human Research Ethics Committee (Approval number: H-2013-0344). Written informed consent was obtained from all subjects.
Data Collection
Data were collected using an online survey management system: www.surveymonkey.com.au. Survey questions were generated using a developmental model (Brancato et al., 2006) using five stages of questionnaire design and testing: (1) conceptualization, (2) design, (3) testing, (4) revision, and (5) data collection. In adhering to this model, the questions were informed by responses from previous qualitative research with young men (Ashton, Hutchesson, et al., 2015; Greaney et al., 2009; Walsh et al., 2009). An initial pilot survey was tested in 10 young men. This ensured questions were clearly understood and the survey length was appropriate. Revisions were then made based on the feedback provided, in order to reduce the number of questions and to improve clarity. The second draft was pilot tested in 20 young men to assess test–retest reliability of responses to questions, addressing motivators and barriers to healthy eating and PA. Items were mostly “adequate” or “poor,” therefore, questions were revised to reduce the number of response options, for example; the original three response options for influence of partner, family, or friends as barriers were combined into one as “social influences.” Also, the number of motivators and barriers to be ranked were reduced from five to three. Additionally, response options for all motivator and barrier questions were randomized to minimize response order bias and improve overall data quality. The final survey was then distributed online and included a total of 67 questions, of these 4 addressed consent and eligibility, with 28 concerning sociodemographics, weight status, fruit and vegetable intakes, alcohol use, PA levels, stress levels, and motivators and barriers to engaging in healthy eating and PA and of relevance to the current article. An IP check verified against date of birth data and responses was carried out to prevent multiple entries from the same user.
Sociodemographic Status
Sociodemographic data included date of birth, country of birth, languages spoken at home employment status, marital status, highest level of education, and income. The questions were consistent with the Australian Bureau of Statistics Census of Population and Housing (Australian Bureau of Statistics, 2011) to determine representativeness of the sample relative to the young Australian male population.
Weight Status
Young men self-reported height (cm) and weight (kg), with BMI calculated from these values (kg/m2), which was recently reported to provide a valid estimate of actual height and weight in young adults (Pursey, Burrows, Stanwell, & Collins, 2014). BMI categories were defined using widely accepted cut points, that is BMI <18.5 kg/m2 for underweight, 18.5 to 24.99 kg/m2 for healthy weight, 25.0 to 29.99 kg/m2 for overweight, and ≥30 kg/m2 for obese (World Health Organization, 2000).
Fruit and Vegetable Intake and Alcohol Use
Daily fruit and vegetable intake was assessed using questions modified from the Australian Health Survey (Australian Bureau of Statistics, 2013b). Participants were asked two separate questions for either fruit or vegetables: “How many serves of fruit/vegetables do you usually eat each day?” with responses ranging from do not eat fruit/vegetables to 6 or more per day. Images of typical servings of fruit or vegetables from the Australian Dietary Guidelines accompanied the questions to assist in establishing correct serving sizes. To determine “at-risk” drinking, young men were asked: “On a day that you drink alcohol, how many standard drinks do you usually have?” with an open response to report this.
Physical Activity Levels
The Godin Leisure-Time Exercise Questionnaire, previously validated in adults (Godin & Shephard, 1985), was used to assess exercise over the past 7 days. Participants were asked how many times per week and the average time per session of strenuous, moderate, and mild PA with culturally relevant examples to assist in correctly determining the intensity of exercise.
Stress
A single-item stress scale was used to measure stress symptoms. Participants were provided with a brief definition of stress and asked: “Do you feel that kind of stress these days?” with five response options ranging from not at all to very much. This measure has previously demonstrated satisfactory validity in adults (Elo, Leppänen, & Jahkola, 2003).
Motivators to Healthy Eating and Physical Activity
Young men were asked to rank their top three reasons for wanting to eat healthier and to participate in PA from a list of 11 predetermined motivators for healthy eating (improve overall health, improve body image, to have more energy, improve sporting performance, improve mental health and well-being, attract a partner, to live longer, achieve a healthy weight, improve sleeping patterns, social influences, expectations to eat well) and 13 predetermined motivator response options for PA (improve body image, improve fitness, improve overall health, improve muscle mass, for enjoyment, improve mental health and well-being, improve sporting performance, lose weight, attract a partner, to live longer, improve sleeping patterns, social influences, expectations to exercise) informed from previous qualitative research with young men (Ashton, Hutchesson, et al., 2015), with 1 = main motivator, 2 = second key motivator, and 3 = third key motivator. Key motivators reported are those that were selected most frequently as the first, second, or third main motivators by survey completers.
Barriers to Healthy Eating and Physical Activity
Per the motivator questions, the young men were asked to rank their top three barriers to eating healthier foods and to participating in PA from a list of 10 predetermined frequently mentioned barriers for healthy eating (ease of access of unhealthy foods, lack of time to cook/prepare healthy foods because of busy lifestyle, lack of motivation to cook healthy foods, high cost of healthy foods, lack of skills/knowledge to cook healthy foods, dislike taste of healthy foods, social influences, lack of variety, lack of information on healthy foods, eating healthy is not a masculine/bloke thing to do) and 11 response options for PA (lack of motivation to exercise, lack of time to exercise because of busy lifestyle, high cost of equipment/facilities, weather, injury, intimidation/embarrassment, lack of information on appropriate exercise routines, social influences, lack of skills/knowledge, lack of facilities, exercising is not a masculine/bloke thing to do) informed from previous qualitative research (Ashton, Hutchesson, et al., 2015). Key barriers reported are those that were selected most frequently as the first, second, or third main barriers by survey completers.
Study Sample Size
Similar research which has incorporated a cross-sectional survey design to assess either motivators or barriers to PA or healthy eating in young men achieved an overall mean of 237 completers (Arzu et al., 2006; Hebden et al., 2015; Leyk et al., 2012). Therefore, this was used as a guide and an initial sample size target of 300 young men was set.
Statistical Analysis
Data analysis was conducted using Stata Version 12 (StataCorp, 2011). Pearson’s chi-square (χ2) test was used to investigate motivators and barriers to healthy eating and PA and to explore differences across all subgroups which included BMI, marital status, education, income, employment, PA level, alcohol use, symptoms of stress, and fruit and vegetable intake. p Values less than .01 were considered statistically significant due to the multiple comparisons made, to reduce the likelihood of Type I error. Analysis was carried out on all completers of the survey.
For the subgroup analysis, BMI was categorized as underweight (BMI < 18.5 kg/m2), healthy weight (BMI 18.5 to 24.99 kg/m2), overweight (BMI 25.0 to 29.99 kg/m2), or obese (BMI ≥30 kg/m2) to align with WHO cutoffs (World Health Organization, 2000). There were small numbers underweight (n = 7) and so this group was excluded from further BMI analyses. Marital status was collapsed into two categories: married (married or de facto) or single (never married, separated, divorced, or widowed). Individual gross income was split into three categories: lower ($0-$299 per week), middle ($300-$999 per week), or higher ($1,000 or more per week) based on median weekly income of young men from National Census Data (Australian Bureau of Statistics, 2014b). Highest qualification level was collapsed into four categories: school certificate (Year 10 or equivalent), higher school certificate (Year 12 or equivalent), trade/apprenticeship/certificate/diploma or university degree/higher university. Employment status was collapsed into three categories: student (university, technical college, and school), employed (working part-/full-time paid employment), or unemployed/casual employment. PA was split into two categories based on whether respondents met national weekly recommendations, defined as 150 minutes of moderate intensity or ≥75 minutes of vigorous intensity PA per week (The Department of Health, 2014). Fruit and vegetable intake was split into two equal groups (≤3 serves per day or >3 serves per day) as few respondents (n=9) met the age- and sex-specific national fruit and vegetable intake recommendations (The Department of Health, 2015). Alcohol intake was split into two categories: ≤4 standard drinks on a single occasion or >4 standard drinks on a single occasion. This was done to align with the National Health and Medical Research Council single occasion risk guidelines (National Health and Medical Research Council, 2015). Finally, stress was collapsed into two groups based on symptoms of stress: “none/little/to some extent” or “rather much/very much.”
Results
Characteristics of Sample
Of the 419 people consenting to participate, 370 were eligible, of whom 282 completed the full survey and were included in final analysis (Figure 1). Demographic characteristics of the sample are summarized in Table 1. Mean age was 22.3 (SD = 2.1) years. Participants conveyed they were predominantly single (n = 223, 79.1%), studying at university (n = 165, 58.5%), and having the higher school certificate (n = 156, 55.3%) as their highest education level. A similar proportion of participants reported lower (n = 112, 41.5%) and middle (n = 115, 42.6%) incomes. Mean BMI was 24.7 (SD = 4.4) kg/m2 with most in the healthy weight range (n = 165, 58.5%), while 29.1% (n = 82) were overweight and 9.9% (n = 28) obese. Most participants reported they were sufficiently active, with 60.1% (n = 168) achieving national PA recommendations, but expressed low intakes of fruit and vegetables; with only 3.2% (n = 9) achieving national recommendations. For alcohol intake, 44.7% (n = 126) reported to have consumed more than four standard drinks on a single occasion, exceeding the risk guidelines (National Health and Medical Research Council, 2015). Symptoms of stress were prevalent in young men with most reporting experiencing these symptoms “to some extent” (n = 80, 28.4%).
Figure 1.
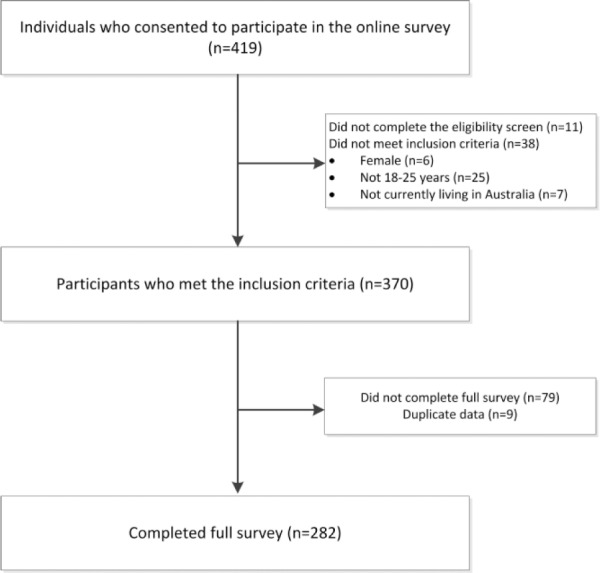
Participant recruitment and eligibility.
Table 1.
Characteristics of Young Men (n = 282) Who Completed the Online Survey and Met the Inclusion Criteria, Australia (Dates: July 6-September 27, 2015).
| M (SD) or % (n) | |
|---|---|
| Age (years) | 22.3 (2.1) |
| 18-21 | 45.0% (127) |
| 22-25 | 55.0% (155) |
| Country of birth | |
| Australia | 90.1% (254) |
| Languages spoken at home | |
| English only | 92.2% (260) |
| Other | 7.8% (22) |
| Marital status | |
| Single/separated/divorced/widowed | 80.5% (227) |
| Married/de facto | 19.5% (55) |
| Employment statusa | |
| Student (university/technical college/secondary school) | 64.5% (182) |
| Employed (working part-/full-time paid employment) | 28.1% (79) |
| Unemployed/casual employment | 7.4% (21) |
| Highest education level | |
| School certificate | 4.3% (12) |
| Higher school certificate | 55.3% (156) |
| Trade/apprenticeship/certificate/diploma | 14.9% (42) |
| University degree/higher university degree | 25.5% (72) |
| Individual income ($AU) | |
| Lower (0-299 per week) | 41.5% (112) |
| Middle (300-999 per week) | 42.6% (115) |
| Higher (1,000 or more per week) | 15.9% (43) |
| Weight status | |
| Current weight (kg) | 79.8 (16.3) |
| Current height (cm) | 179.5 (7.4) |
| BMI (kg/m2) | 24.7 (4.4) |
| BMI category (kg/m2) | |
| Underweight | 2.5% (7) |
| Healthy weight | 58.5% (165) |
| Overweight | 29.1% (82) |
| Obese | 9.9% (28) |
| Diet: Fruit and vegetables | |
| Fruit serves per day | 1.7 (1.2) |
| Vegetable serves per day | 2.4 (1.4) |
| ≤3 Serves of fruit and vegetables per day | 45.0% (127) |
| >3 Serves of fruit and vegetables per day | 55.0% (155) |
| Alcohol intake (at-risk drinking) | |
| More than four standard drinks on usual drinking day | 44.7% (126) |
| Physical activity | |
| Meeting recommendationsb | 61.1% (168) |
| Not meeting recommendations | 38.9% (114) |
| Stress | |
| Not at all/only a little/to some extent | 73.4% (207) |
| Rather much/very much | 26.6% (75) |
Participants could select multiple responses for the employment status. For the purpose of categorizing into appropriate groups, the following rules were applied to ensure participants were categorized into the “main” employment status: (1) If participant selected both student and working full-time paid employment, they were classed as “Employed.” (2) If participant selected both student and working part-time paid employment, they were classed as “Student.” (3) If participant selected both student and casual worker, they were classed as “Student.” (4) If participant selected both working part-time paid employment and casual worker, they were classed as Employed (part-time paid employment). b≥150 Minutes of moderate intensity physical activity or ≥75 minutes of vigorous intensity physical activity (The Department of Health, 2014).
Motivators to Healthy Eating
Over 60% of the sample rated to improve overall health (n = 176, 63.5%) as the most important reason for wanting to eat healthier (Table 2). This was followed by to improve body image (n = 145, 52.3%) and to have more energy (n = 89, 32.1%). Young men were least motivated by expectations to eat well with only 4.0% (n = 11) ranking it as a key motivator, followed by social influences (n = 15, 5.4%) and to improve sleeping patterns (n = 32, 11.6%).
Table 2.
Key Motivators for Healthy Eating and Physical Activity Reported by Australian Young Men (Aged 18-25 Years) From an Online Survey and Differences by Demographic and Behavioral Characteristics.a
| Ranked as key motivatorb |
Not ranked as key motivator |
BMI |
Marital status |
Highest qual |
Income |
Employ |
PA |
Alc |
Stress |
Fruit & veg |
|
|---|---|---|---|---|---|---|---|---|---|---|---|
| % (n) | p | ||||||||||
| Healthy eating motivators (n = 277) | |||||||||||
| Improve overall health | 63.5 (176) | 36.5 (101) | .431 | .990 | .349 | .329 | .344 | .672 | .129 | .011 | .606 |
| Improve body image | 52.3 (145) | 47.7 (132) | .274 | .946 | .119 | .601 | .982 | .909 | .029 | .457 | .622 |
| To have more energy | 32.1 (89) | 67.9 (188) | .064 | .278 | .659 | .993 | .618 | .994 | .521 | .518 | .901 |
| Improve sporting performance | 29.2 (81) | 70.8 (196) | .389 | .105 | .447 | .399 | .548 | .001c | .270 | .010 | .823 |
| Improve mental health and well-being | 28.2 (78) | 71.8 (199) | .440 | .574 | .084 | .893 | .035 | .450 | .045 | .001d | .691 |
| Attract a partner | 27.4 (76) | 72.6 (201) | .805 | .004e | .611 | .414 | .815 | .926 | .045 | .606 | .231 |
| To live longer | 25.3 (70) | 74.7 (207) | .908 | .960 | .453 | .797 | .934 | .167 | .057 | .075 | .748 |
| Achieve a healthy weight | 20.9 (58) | 79.1 (219) | <.001f | .424 | .903 | .937 | .666 | .041 | .283 | .615 | .480 |
| Improve sleeping patterns | 11.6 (32) | 88.5 (245) | .085 | .628 | .020 | .437 | .914 | .179 | .834 | .002g | .834 |
| Social influences (e.g., because your partner, family, or friends eat healthy) | 5.4 (15) | 94.6 (262) | .754 | .900 | .742 | .306 | .885 | .164 | .530 | .232 | .331 |
| Expectations to eat well | 4.0 (11) | 96.0 (266) | .320 | .461 | .563 | .649 | .311 | .660 | .216 | .966 | .217 |
| Physical activity motivators (n = 278) | |||||||||||
| Improve body image | 44.6 (124) | 55.4 (154) | .604 | .170 | .807 | .897 | .387 | .504 | .059 | .489 | .682 |
| Improve fitness | 44.2 (123) | 55.8 (155) | .294 | .003h | .259 | .805 | .268 | .643 | .163 | .747 | .237 |
| Improve overall health | 41.0 (114) | 59.0 (164) | .180 | .634 | .590 | .042 | .574 | .840 | .034 | .173 | .485 |
| Improve muscle mass | 27.0 (75) | 73.0 (203) | .268 | .463 | .051 | .459 | .771 | .034 | .103 | .058 | .138 |
| For enjoyment | 26.3 (73) | 73.7 (205) | .118 | .880 | .896 | .902 | .362 | .006i | .802 | .165 | .546 |
| Improve mental health and well-being | 23.7 (66) | 76.3 (212) | .077 | .467 | .944 | .074 | .329 | .902 | .005j | .004k | .468 |
| Improve sporting performance | 23.4 (65) | 76.6 (213) | .888 | .685 | .131 | .448 | .339 | .002l | .878 | .002m | .570 |
| Lose weight | 21.6 (60) | 78.4 (218) | <.001n | .679 | .656 | .734 | .365 | <.001o | .813 | .872 | .717 |
| Attract a partner | 21.6 (60) | 78.4 (218) | .379 | .004p | .271 | .236 | .262 | .781 | .002q | .027 | .342 |
| To live longer | 11.1 (31) | 88.9 (247) | .989 | .064 | .454 | .742 | .463 | .285 | .243 | .100 | .405 |
| Improve sleeping patterns | 6.8 (19) | 93.2 (259) | .215 | .100 | .562 | .166 | .037 | .082 | .770 | .103 | .227 |
| Social influences (e.g., because your partner, family, or friends are active) | 6.5 (18) | 93.5 (260) | .522 | .379 | .394 | .816 | .875 | .984 | .367 | .052 | .334 |
| Expectations to exercise | 2.2 (6) | 97.8 (272) | .081 | .846 | .516 | .918 | .010 | .005r | .551 | .169 | .272 |
Note. BMI = body mass index; highest qual = highest qualification level; employ = employment level, PA = physical activity level; Alc = alcohol use; stress = symptoms of stress; fruit & veg = fruit and vegetable intake. χ2 Tests were used for examining differences between motivations for healthy eating and physical activity and subgroups. p < .01 Indicates statistical significance. Motivators to healthy eating (survey completers: n = 282; completers after removal of anomalous results: n = 277; age group: n = 277; BMI category: n = 270; marital status: n = 277; highest qualification level: n = 277; income: n = 265; employment: n = 277; physical activity level: n = 271; alcohol level: n = 277; stress level: n = 277; fruit and vegetables intake: n = 277). Motivators to physical activity (survey completers: n = 282; completers after removal of anomalous results: n = 278; age group: n = 278; BMI category: n = 271; marital status: n = 278; highest qualification level: n = 278; income: n = 267; employment: n = 278; physical activity level: n = 271; alcohol level: n = 278; stress level: n = 278; fruit and vegetables intake: n = 278).
Recruitment dates from online survey: July 6 to September 27, 2015. bTo classify as “key motivator,” we calculated the percentage of those either ranking the motivator as first, second, or third main motivator. cMeeting PA recommendations: 36.4% ranked as key motivator vs. Not meeting PA recommendations: 17.9% ranked as key motivator. d“None/little/to some extent” stress symptoms: 22.7% ranked as key motivator vs. “rather much/very much”: 43.2% ranked as key motivator. eMarried/de facto: 11.5% ranked as key motivator vs. Single (never married, separated, divorced, or widowed): 31.1% ranked as key motivator. fHealthy weight: 11.7% ranked as key motivator vs. Overweight: 30.4% ranked as key motivator vs. Obese: 50.0% ranked as key motivator. g“None/little/to some extent” stress symptoms: 7.9% ranked as key motivator vs. “rather much/very much”: 21.6% ranked as key motivator. hMarried/de facto: 61.8% ranked as key motivator vs. Single (never married, separated, divorced, or widowed): 39.9% ranked as key motivator. iMeeting PA recommendations: 32.1% ranked as key motivator vs. Not meeting PA recommendations: 17.0% ranked as key motivator. jRisky drinking (>4 standard drinks on a single occasion): 15.9% ranked as key motivator vs. Nonrisky drinking (≤4 standard drinks on a single occasion): 30.3% ranked as key motivator. k“None/little/to some extent” stress symptoms: 19.2% ranked as key motivator vs. “rather much/very much”: 36.0% ranked as key motivator. lMeeting PA recommendations: 29.1% ranked as key motivator vs. Not meeting PA recommendations: 13.2% ranked as key motivator. m“None/little/to some extent” stress symptoms: 28.1% ranked as key motivator vs. “Rather much/very much”: 10.7% ranked as key motivator. nHealthy weight: 12.3% ranked as key motivator vs. Overweight: 30.9% ranked as key motivator vs. Obese: 46.4% ranked as key motivator. oMeeting PA recommendations: 14.5% ranked as key motivator vs. Not meeting PA recommendations: 33.9% ranked as key motivator. pMarried/de facto: 7.3% ranked as key motivator vs. Single (never married, separated, divorced, or widowed): 25.1% ranked as key motivator. qRisky drinking (>4 standard drinks on a single occasion): 30.2% ranked as key motivator vs. Nonrisky drinking (≤4 standard drinks on a single occasion): 14.5% ranked as key motivator. rMeeting PA recommendations: 0% ranked as key motivator vs. Not meeting PA recommendations: 4.7% ranked as key motivator.
Subgroup analysis revealed significant differences for some motivators by BMI, marital status, PA level, and symptoms of stress. Obese young men were significantly more likely (p < .001) to rank achieve a healthy weight as a key motivator (n = 14/28, 50.0%) when compared with overweight (n = 24/79, 30.4%) and healthy weight young men (n = 19/163, 11.7%). Single young men were more likely (p < .01) to rank attract a partner as a key motivator (n = 70/225, 31.1%) compared with those that were married (n = 6/52, 11.5%). Those meeting PA recommendations were more likely (p = .001) to rank to improve sports performance as a key motivator (n = 60/165, 36.4%) compared with those failing to meet recommendations (n = 19/106, 17.9%). Those reporting stress symptoms “rather much” or “very much” were more likely (p = .001) to rank improve mental health and well-being as a key motivator (n = 32/74, 43.2%) over those experiencing no symptoms, few symptoms, or “to some extent” (n = 46/203, 22.7%). They were also more likely (p < .01) to rank to improve sleeping patterns as a key motivator (n = 16/74, 21.6% vs. n = 16/203, 7.9%). See supplementary Tables 1 to 4 for common motivators to healthy eating based on subgroups of BMI, marital status, PA level, and symptoms of stress.
Motivators to Physical Activity
Greater than 40% of the sample either ranked to improve body image (n = 124, 44.6%), fitness (n = 123, 44.2%) or overall health (n = 114, 41.0%) as a key motivator (Table 2). Young men were least motivated by expectations to exercise with only 2.2% (n = 6) ranking it as a key motivator to undertaking PA, followed by social influences (n = 18, 6.5%) and to improve sleeping patterns (n = 19, 6.8%).
Differences were apparent for some motivators by BMI, marital status, PA level, alcohol use, and symptoms of stress. Obese young men were significantly more likely (p < .001) to rank lose weight as a key motivator (n = 13/28, 46.4%), compared with overweight (n = 25/81, 30.9%) and healthy weight young men (n = 20/162, 12.3%). Young men who were married or in a de facto relationship were more likely (p < .01) to rank improve fitness as a key motivator (n = 34/55, 61.8%) compared with single young men (n = 89/223, 39.9%). They were also less likely (p < .01) to rank attract a partner as a key motivator (n = 4/55, 7.3% vs. n = 56/223, 25.1%). Those not meeting PA recommendations were more likely (p < .001) to rank lose weight as a key motivator (n = 36/106, 33.9%) compared with those meeting recommendations (n = 24/165, 14.5%). They were also less likely to rank enjoyment (n = 18/106, 17.0% vs. n = 53/165, 32.1%, p < .01) or improve sporting performance (n = 14/106, 13.2% vs. n = 48/165, 29.1%, p < .01) as a key motivator and more likely to be motivated by expectations to exercise (n = 5/106, 4.7% vs. n = 0/165, 0%, p < .01). At-risk drinkers (>4 standard drinks on a single occasion) were less likely (p < .01) to rank improve mental health and well-being as a key motivator (n = 20/126, 15.9%) compared with those consuming four or less standard alcoholic drinks on a single occasion (n = 46/152, 30.3%). They were also more likely to rank attract a partner as a key motivator (n = 38/126, 30.2% vs. n = 22/152, 14.5%, p < .01). In addition, those reporting stress symptoms “rather much” or “very much” were more likely (p < .01) to rank improve mental health and well-being as a key motivator (n = 27/75, 36.0%) compared with those experiencing no symptoms, few symptoms, or “to some extent” (n = 39/203, 19.2%). They were also less likely to rank improve sporting performance as a key motivator (n = 8/75, 10.7% vs. n = 57/203, 28.1%, p < .01). See supplementary Tables 5 to 9 for prominent motivators to PA by the subgroups of BMI, marital status, PA level, alcohol intake, and symptoms of stress.
Barriers to Healthy Eating
Most common barriers to healthy eating included ease of access to unhealthy foods (n = 171, 61.1% ranked as a key barrier), lack of time to cook/prepare healthy foods (n = 154, 55.0%), and lack of motivation to cook healthy foods (n = 142, 50.7%; Table 3). The least influential barriers were eating healthy is not a masculine/bloke thing to do with only 2.5% (n = 7) ranking it as a key barrier, followed by lack of information on healthy foods (n = 22, 7.9%) and lack of variety (n = 39, 13.9%)
Table 3.
Key Barriers for Healthy Eating and Physical Activity Reported by Australian Young Men (Aged 18-25 Years) From an Online Survey and Differences by Demographic and Behavioral Characteristics.a
| Ranked as key barrierb |
Not ranked as key barrier |
BMI |
Marital status |
Highest qual |
Income |
Employ |
PA |
Alc |
Stress |
Fruit & veg |
|
|---|---|---|---|---|---|---|---|---|---|---|---|
| % (n) | p | ||||||||||
| Healthy eating barriers (n = 280) | |||||||||||
| Ease of access of unhealthy foods (e.g., take away) | 61.1 (171) | 38.9 (109) | .482 | .119 | .364 | .467 | .648 | .787 | .367 | .060 | .397 |
| Lack of time to cook/prepare healthy foods because of busy lifestyle | 55.0 (154) | 45.0 (126) | .165 | .190 | .106 | .208 | .013 | .322 | .365 | .067 | .492 |
| Lack of motivation to cook healthy foods | 50.7 (142) | 49.3 (138) | .263 | .053 | .078 | .490 | .051 | .027 | .386 | .992 | .011 |
| High cost of healthy foods | 42.5 (119) | 57.5 (161) | .911 | .748 | .249 | .615 | .438 | .713 | .316 | .162 | .147 |
| Lack of skills/knowledge to cook healthy foods | 25.7 (72) | 74.3 (208) | .226 | .759 | .065 | .927 | .759 | .434 | .049 | .691 | .712 |
| Dislike taste of healthy foods | 21.8 (61) | 78.2 (219) | <.001c | .779 | .373 | .045 | .517 | .077 | .420 | .231 | <.001d |
| Social influences (e.g., because your partner, family, or friends do NOT eat healthy) | 18.9 (53) | 81.1 (227) | .110 | .763 | .084 | .125 | .199 | .004e | .183 | .013 | <.001f |
| Lack of variety | 13.9 (39) | 86.1 (241) | .128 | .123 | .092 | .660 | .182 | .061 | .887 | .545 | .049 |
| Lack of information on healthy foods | 7.9 (22) | 92.1 (258) | .143 | .323 | .812 | .479 | .361 | .279 | .714 | .342 | .992 |
| Eating healthy is not a masculine/bloke thing to do | 2.5 (7) | 97.5 (273) | .643 | .190 | .173 | .587 | .554 | .584 | .149 | .914 | .094 |
| Physical activity barriers (n = 282) | |||||||||||
| Lack of motivation to exercise | 66.3 (187) | 33.7 (95) | .703 | .421 | .026 | .385 | .309 | .003g | .910 | .718 | .143 |
| Lack of time to exercise because of busy lifestyle | 57.8 (163) | 42.2 (119) | .319 | .396 | .240 | .284 | .036 | .018 | .312 | .712 | .409 |
| High cost of equipment/facilities (e.g., gym membership) | 33.3 (94) | 66.7 (188) | .255 | .671 | .615 | .633 | .635 | .464 | .309 | .253 | .554 |
| Weather (e.g., too hot or too cold to exercise) | 32.6 (92) | 67.4 (190) | .499 | .735 | .490 | .011 | .178 | .426 | .427 | .063 | .912 |
| Injury | 27.7 (78) | 72.3 (204) | .174 | .943 | .686 | .458 | .624 | .008h | .620 | .259 | .569 |
| Intimidation/embarrassment | 24.8 (70) | 75.2 (212) | .061 | .565 | .674 | .355 | .838 | .002i | .723 | <.001j | .673 |
| Lack of information on appropriate exercise routines | 16.0 (45) | 84.0 (237) | .865 | .362 | .839 | .374 | .806 | .767 | .109 | .372 | .810 |
| Social influences (e.g., because your partner, family, or friends are NOT active) | 15.6 (44) | 84.4 (238) | .606 | .317 | .760 | .994 | .153 | .170 | .078 | .353 | .294 |
| Lack of skills/knowledge | 14.2 (40) | 85.8 (242) | .991 | .606 | .722 | .924 | .997 | .001k | .324 | .168 | .040 |
| Lack of facilities | 11.0 (31) | 89.0 (251) | .916 | .143 | .753 | .058 | .185 | .145 | .745 | .122 | .023 |
| Exercising is not a masculine/bloke thing to do | 0.7 (2) | 99.3 (280) | .716 | .485 | .653 | .241 | .575 | .747 | .202 | .117 | .887 |
Note. BMI = body mass index; highest qual = highest qualification level; employ = employment level; PA = physical activity level; Alc = alcohol use; stress = symptoms of stress; fruit & veg = fruit and vegetable intake. χ2 Tests were used for examining differences between motivations for healthy eating and physical activity and subgroups. p < .01 Indicates statistical significance. Barriers to healthy eating (survey completers: n = 282; completers after removal of anomalous results: n = 280; age group: n = 280; BMI category: n = 273; marital status: n = 280; highest qualification level: n = 280; income: n = 268; employment: n = 280; physical activity level: n = 273; alcohol level: n = 280; stress level: n = 280; fruit and vegetables intake: n = 280). Barriers to physical activity (survey completers: n = 282; age group: n = 282; BMI category: n = 275; marital status: n = 282; highest qualification level: n = 282; income: n = 270; employment: n = 282; physical activity level: n = 275; alcohol level: n = 282; stress level: n = 282; fruit and vegetables intake: n = 282).
Recruitment dates from online survey: July 6 to September 27, 2015. bTo classify as “key barrier,” we calculated the percentage of those either ranking the barrier as first, second, or third main barrier. cHealthy weight: 19.4% ranked as key barrier vs. Overweight: 13.8% ranked as key barrier vs. Obese: 53.6% ranked as key barrier. d≤3 Serves of fruit and vegetables per day: 33.9% vs. >3 Serves of fruit and vegetables per day: 11.8%. eMeeting PA recommendations: 24.1% ranked as key barrier vs. Not meeting PA recommendations: 10.3% ranked as key barrier. f≤3 Serves of fruit and vegetables per day: 7.9% vs. >3 Serves of fruit and vegetables per day: 28.1%. gMeeting PA recommendations: 59.5% ranked as key barrier vs. Not meeting PA recommendations: 76.6% ranked as key barrier. hMeeting PA recommendations: 33.3% ranked as key barrier vs. Not meeting PA recommendations: 18.7% ranked as key barrier. iMeeting PA recommendations: 19.0% ranked as key barrier vs. Not meeting PA recommendations: 35.5% ranked as key barrier. j“None/little/to some extent” stress symptoms: 19.3% ranked as key motivator vs. “rather much/very much”: 40.0% ranked as key motivator. kMeeting PA recommendations: 8.9% ranked as key barrier vs. Not meeting PA recommendations: 23.4% ranked as key barrier.
Differences were evident for some barriers by BMI, PA level, and fruit and vegetable intake. Obese young men were more likely (p < .001) to report dislike taste of healthy foods as a key barrier (n = 15/28, 53.6%) compared with healthy weight (n = 32/165, 19.4%) and overweight young men (n = 11/80, 13.8%). Young men who met PA recommendations were more likely (p < .01) to rank social influences as a key barrier (n = 40/166, 24.1%) compared with those not meeting recommendations (n = 11/107, 10.3%). Furthermore, young men who consumed three or less serves of fruit and vegetables were more likely (p < .001) to rank dislike taste of healthy foods as a key barrier (n = 43/127, 33.9%), compared with those consuming more than three serves (n = 18/153, 11.8%). They were also less likely to report social influences (n = 10/127, 7.9% vs. n = 43/153, 28.1%, p < .001) as a key barrier to eating healthy. See supplementary Tables 10 to 12 for prominent barriers to PA by the subgroups of BMI, PA level, and fruit and vegetable intake.
Barriers to Physical Activity
The most frequently ranked barriers to PA were lack of motivation with 66.3% (n = 187) of the sample ranking this as a key barrier (Table 3). This was followed by lack of time to exercise (n = 163, 57.8%) and high cost of equipment/facilities (n = 94, 33.3%). The less prominent barriers included exercise is not a masculine/bloke thing to do with only 0.7% (n = 2) of the sample registering this as a key barrier. Next was lack of facilities (n = 31, 11.0%) and lack of skills/knowledge (n = 40, 14.2%).
Differences in subgroup analysis for barriers was by PA level and symptoms of stress. Young men not meeting PA recommendations were more likely (p < .01) to rank lack of motivation as a key barrier (n = 82/107, 76.6%) compared with those meeting recommendations (n = 100/168, 59.5%). They were also more likely to rank lack of skills/knowledge (n = 25/107, 23.4% vs. n = 15/168, 8.9%, p < .01) and intimidation/embarrassment (n = 38/107, 35.5% vs. n = 32/168, 19.0%, p < .01) as key barriers, but less likely to rank injury as a key barrier (n = 20/107, 18.7% vs. n = 56/168, 33.3%, p < .01). Those reporting stress symptoms “rather much” or “very much” were more likely (p < .001) to rank intimidation/embarrassment as a key barrier (n = 30/75, 40.0%) compared with those experiencing no symptoms, few symptoms, or “to some extent” (n = 40/207, 19.3%). See supplementary Tables 13 and 14 for prominent barriers to PA by the subgroups for PA level and symptoms of stress.
Discussion
This study aimed to provide in-depth insights into young men’s self-reported motivators and barriers to healthy eating and PA, and to explore differences by health behavior and demographic subgroups of young men. The most commonly ranked motivators for healthy eating included to improve overall health and body image and to have more energy. However, there were some differences in motivators by BMI, marital status, PA level, and symptoms of stress. There were some similarities in reported motivators for PA, with the most common being to improve body image, fitness, and overall health. Differences were evident by BMI, marital status, PA level, alcohol use, and symptoms of stress. Key barriers to eating healthily included ease of access to unhealthy foods, lack of time to cook/prepare healthy foods, and lack of motivation to cook healthy foods. Differences were apparent for some barrier responses by BMI, PA level, and fruit and vegetable intake. Finally, the most commonly ranked barriers to PA were lack of motivation, lack of time to exercise, and high cost of equipment/facilities with differences evident by PA level and symptoms of stress.
This is the first quantitative survey to explore young men’s key motivators and barriers to both PA and healthy eating. To the authors knowledge, there have only been three previous quantitative surveys related to this in young men, but the scope of these studies have been restricted to exploration of barriers to PA only (Arzu et al., 2006; Leyk et al., 2012) or influences on food selection behavior (Hebden et al., 2015). While further research is required in other population samples of young men to corroborate or refute the findings from the current survey, results are consistent with the few quantitative studies to date and confirm that key factors influencing healthy eating in young men are related to the cost (Hebden et al., 2015) and convenience/ease of access of foods (Hebden et al., 2015), with barriers to PA reported as lack of time (Arzu et al., 2006; Leyk et al., 2012). Surprisingly, social influences were not reported as major barriers, with only 14% ranking it as a key barrier to healthy eating and 16% for PA. This contrasts with other surveys in young men that reported a lack of social support can hinder PA (Arzu et al., 2006).
Sex (biological characteristics) and gender (socially constructed factors) both independently affect health and must be considered in the design, data collection, or analysis of health research (Oliffe & Greaves, 2012). Gendered social differences are evident, with healthy eating motivators unique to young men being to have more energy and unique PA motivators being to improve fitness, compared with young women (Egli, Bland, Melton, & Czech, 2011; Holley, Collins, Morgan, Callister, & Hutchesson, 2015; LaCaille, Dauner, Krambeer, & Pedersen, 2011). Moreover, young men appear to be highly motivated by the feeling of enjoyment with exercise, whereas this was considered less important in a similar study involving 1,182 young women in the United States (Egli et al., 2011). Despite this, appearance/body image appear to be key motivators in young women (Egli et al., 2011), which corroborates the responses in the current study and other similar studies in young men (Ashton, Hutchesson, et al., 2015; Walsh et al., 2009). It is not surprising that young men perceive this to be an important factor given that body image dissatisfaction in men has increased over the past few decades (Keel, Baxter, Heatherton, & Joiner Jr, 2007), with reports suggesting up to 45% of men are dissatisfied with their bodies (Victorian Government, 2009). However, recent research has revealed men typically desire a shape marked by a lean, well-toned muscular build, whereas women aim for thinner bodies and to lose weight (Bergeron & Tylka, 2007; Blashill, 2011; McCreary & Sasse, 2000; Ridgeway & Tylka, 2005).
It appears young men and young women share the same barriers to healthy eating and PA of lack of motivation, time constraints, and cost (Andajani-Sutjahjo, Ball, Warren, Inglis, & Crawford, 2004; Holley et al., 2015). The similarities in barriers may be due to age-related factors, as both sexes are experiencing similar transitional phases in their life such as starting tertiary education (Poobalan, Aucott, Precious, Crombie, & Smith, 2010; Stanwick, Lu, Rittie, & Circelli, 2014) and less financial stability compared with older adults, particularly for Australian young adults where full-time employment rates are at their lowest since 1986 (Stanwick et al., 2014). The age-related differences are apparent compared with similar studies in groups that were mostly middle-aged or older men (Gough & Conner, 2006; Hankey, Leslie, & Lean, 2002; Morgan, Warren, Lubans, Collins, & Callister, 2011; Sabinsky, Toft, Raben, & Holm, 2007). Unlike the responses in the current study, older men reported being less motivated by appearance (Hankey et al., 2002; Sabinsky et al., 2007) but being motivated to become more effective in their work role (Sabinsky et al., 2007). Lifestyle differences between young men and older men which influence socioeconomic status (e.g., occupational status, housing environment, family circumstances, and marital status) are likely to explain why older men were less likely to identify cost as a barrier (Gough & Conner, 2006; Morgan et al., 2011; Sabinsky et al., 2007).
Although the current findings have shown similarities in a number of motivators and barriers with other segments of the population (Andajani-Sutjahjo et al., 2004; Holley et al., 2015), it is important to view these factors through a sociocultural lens relating to young men in intervention design and delivery—as has been illustrated in a recent conceptual model developed by Morgan, Young, Smith, and Lubans (2016). Therefore, while there are common motivators and barriers that are apparent across population groups, such as improving health, lack of motivation, time constraints, and cost, these factors must still be uniquely targeted using socioculturally relevant content and strategies when presenting intervention messages to young men. For example, in addressing time and cost barriers to exercise, program components could consider including high intensity interval training as this uses short, intense periods of work with minimal or no equipment (Gibala & McGee, 2008). This has potential to engage young men given that strength and fitness hold particular salience in this group (Morgan et al., 2016). Previous research has demonstrated challenges of reaching, retaining, and/or engaging young men (LaRose, Tate, Gorin, & Wing, 2010; Tate et al., 2014; White et al., 2012), but health-related interventions which consider the intended population’s unique sociocultural factors in intervention design and delivery are more likely to achieve greater intervention engagement and improved outcomes (Morgan et al., 2016; Resnicow, Baranowski, Ahluwalia, & Braithwaite, 1998).
This is the first study to explore perceptions based on demographic or behavioral subgroups of young men. Although one study stratified results based on PA levels (Leyk et al., 2012), there were no other subgroup analyses performed. In the current study, data derived from the subgroup analysis highlight the differences within young men. These data can be used to inform development of tailored programs specifically for the individual demographics or behavioral characteristics of subgroups of young men. It can also be used by health professionals such as a dietitian, exercise physiologist, or general practitioner to provide appropriate counselling for behavior change. For example, the results in the supplementary tables highlight that those not meeting PA recommendations perceive the embarrassment of going to the gym as a major barrier to PA. Therefore, in designing a program for inactive young men, alternative ways to engage them in exercise such as home-based resistance training could be incorporated.
Previous surveys which have explored young men’s perceptions to either healthy eating or PA have been limited to university-based samples (Arzu et al., 2006; Hebden et al., 2015; Leyk et al., 2012). Therefore, the current study sought to obtain responses from a more diverse sample of young men. Comparisons with Australian census data indicate that the respondents were reasonably representative of young men in Australia. In particular, the national average income for young Australian men aged 15 to 24 years ($27,762 per annum; Australian Bureau of Statistics, 2013a) resembles that in the current sample (between $23,072 and $31,478 per annum). Additionally, the marital status of Australian young adults (82% single and 4% married; Australian Bureau of Statistics, 2009) is comparable to the current sample. There was some response bias in terms of overrepresentation of those enrolled in formal study (64.5% vs. 47.1%; Australian Bureau of Statistics, 2015a) and those with higher education levels: 25.5% of the current sample attained a university degree or above compared with 15.5% of Australian males aged 20 to 24 years (Australian Bureau of Statistics, 2014a). Comparisons with Australia Health Survey data (Australian Bureau of Statistics, 2015b) indicate higher proportions of healthy weight (58.5% vs. 49.6%) and overweight young men (29.1% vs. 26.9%) and an underrepresentation of those that are obese (9.9% vs. 17.3%). The proportion not meeting fruit and vegetable recommendations is almost identical to that of the average Australian male aged 18 to 24 years (96.9% vs. 98.2%). Direct comparisons also apply to those meeting PA recommendations (61.1% vs. 61.5%) or exceeding for alcohol consumption guidelines, classed as >2 standard drinks on a usual drinking day (64.9% vs. 69.4%). Despite the difference in measures of stress, the Australian Health Survey reported around 11.1% as having high/very high psychological distress, compared with 26.6% of this sample who experienced stress symptoms “rather much” or “very much.” Hence, the current sample can be considered relatively “stressed,” compared with Australian 18- to 24-year-old males (Australian Bureau of Statistics, 2015b).
Results from this research and Australian Health Survey data (Australian Bureau of Statistics, 2015b) highlight the unhealthy lifestyle behaviors that are prevalent in this demographic. Despite this, there is a considerable underrepresentation of lifestyle behavior interventions for young men (Ashton, Morgan, et al., 2015). Difficulties in reaching, engaging, and retaining young men may be a key factor. For example, a recent weight gain prevention study took 19 months to recruit 599 young adults and only 130 (22%) were young men, with a total expenditure of $139,543.72 USD for recruitment procedures (Tate et al., 2014). The difficulties in reaching young men are even more discernible in another weight gain prevention study for young adults, where only 2% of the sample recruited was young men (LaRose et al., 2010). Once young men have been recruited and enrolled into an intervention, retaining them throughout the entire program and for follow-up assessments has proven to be difficult, with only 53% of young men were retained at 5-month follow-up for a nutrition intervention (Uglem, Stea, Kjøllesdal, Frølich, & Wandel, 2013). Although the Premier League for Health campaign showed promise for reaching U.K. young men through sports clubs (2,134 of 3,779 recruited were aged 18-34 years), the study was affected by high attrition rates with only 29.5% of the sample retained at 12 weeks postintervention (White et al., 2012). Traditional “one-size-fits-all” approaches to intervention research may not be effective for young men. Alternative methods such as implementation of a participatory approach, where young men are actively involved in intervention design to account for their own individual preferences, needs, and barriers may help overcome the previous limitations. Participatory research has been particularly successful in terms of recruitment, retention, and outcome effects in other hard-to-reach population groups, such as racial and ethnic minorities (Las Nueces, Hacker, DiGirolamo, & Hicks, 2012) but it is yet to be explored in young adult men. Applying a participatory approach to program development and research in young men will add to the current gaps in the literature.
Strengths of the current study include perspectives from a relatively large sample (n = 282) of young men, who have previously been underrepresented in this type of research. Also, use of a development model and extensive pilot testing of survey questions in young men helped generate relatable and reliable questions. Limitations include the lack of reliability testing of the final survey after minor revisions were made to the pilot survey. The use of nonrandom sampling was implemented as it was more feasible to administer in this hard-to-reach population. However, the lack of generalizability can introduce bias as the sample may not be truly representative of the whole population in this demographic. In addition, all survey responses were self-reported and therefore subject to reporting bias. Despite this, comparisons with national census data and national health survey data indicate similarities between the current sample and that of the average Australian young male, except for an overrepresentation of those of healthy weight with higher education levels and in full-time study. Furthermore, the online survey combined multiple instruments to collectively obtain responses on a number of health behaviors. This may potentially have implications for the psychometric properties of some of the measures. The statistical analyses carried out in this study and other similar research have provided initial explorations of young men’s perspectives. Future research may consider the use of multivariate statistical analysis, such as structural equation modelling to consider the effect of the multiple factors and multiple simultaneous relationships on young men’s motivators and barriers to healthy eating and PA. Finally, there may be a mismatch between stated attitudes and beliefs and actual health behaviors in young men. To this extent, while it is good to explore the motivators and barriers identified when planning interventions, addressing these may still be limited in terms of the impact the intervention has on young men’s actual diet and exercise practices.
Conclusion
Findings from the current study provide insight into the personal, social, and environmental factors that young men report as facilitating or inhibiting their efforts to eat healthy and be physically active. Health-related interventions targeting PA and healthy eating for young men could include strategies to promote benefits relating to health, appearance/body image, increased energy and fitness, and address key barriers including lack of motivation, time, cost, and accessibility of unhealthy foods. This highlights the importance of designing interventions addressing these factors. The differences in motivators and barriers across the various subgroups based on BMI, marital status, PA, alcohol use, stress, and fruit and vegetable intake, confirm the social and behavioral diversity in young men and that a “one-size-fits-all” approach is not appropriate. Researchers and health professionals should tailor advice by providing recommendations specific to the needs of young men.
Supplementary Material
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research project was funded by a Hunter Medical Research Institute (14–30) project grant. L. M. Ashton undertook this research as part of a requirement for the degree of PhD (Nutrition and Dietetics), the University of Newcastle, Australia. L. M. Ashton is supported by an International Postgraduate Award Scholarship and the Greaves Family Medical Research Scholarship through Hunter Medical Research Institute. M. J. Hutchesson is supported by a Postdoctoral Research Fellowship from the National Heart Foundation of Australia (#100177).
Supplemental Material: The supplementary tables referenced in this article are available at http://journals.sagepub.com/doi/suppl/10.1177/1557988316680936
References
- Andajani-Sutjahjo S., Ball K., Warren N., Inglis V., Crawford D. (2004). Perceived personal, social and environmental barriers to weight maintenance among young women: A community survey. International Journal of Behavioral Nutrition and Physical Activity, 1(1), 15. doi: 10.1186/1479-5868-1-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arzu D., Tuzun E. H., Eker L. (2006). Perceived barriers to physical activity in university students. Journal of Sports Science & Medicine, 5, 615-620. [PMC free article] [PubMed] [Google Scholar]
- Ashton L. M., Hutchesson M. J., Rollo M. E., Morgan P. J., Collins C. E. (2014). A scoping review of risk behaviour interventions in young men. BMC Public Health, 14(1), 957. doi: 10.1186/1471-2458-14-957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashton L. M., Hutchesson M. J., Rollo M. E., Morgan P. J., Thompson D. I., Collins C. E. (2015). Young adult males’ motivators and perceived barriers towards eating healthily and being active: A qualitative study. International Journal of Behavioral Nutrition and Physical Activity, 12(1), 93. doi: 10.1186/s12966-015-0257-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashton L. M., Morgan P. J., Hutchesson M. J., Rollo M. E., Young M. D., Collins C. E. (2015). A systematic review of SNAPO (smoking, nutrition, alcohol, physical activity and obesity) randomized controlled trials in young adult men. Preventive Medicine, 81, 221-231. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics. (2009). 4102.0—Australian Social Trends, March 2009. Retrieved from http://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4102.0Main+Features20March%202009
- Australian Bureau of Statistics. (2011). Census of Population and Housing: Nature and content, Australia. Retrieved from http://www.abs.gov.au/ausstats/abs@.nsf/ViewContent?readform&view=productsbyCatalogue&Action=Expand&Num=2.1
- Australian Bureau of Statistics. (2013a). 5673.0.55.003—Wage and Salary Earner Statistics for small areas, time series, 2005-06 to 2010-11: 2B: Wage and salary earners, age by sex, statistical areas, 2010-11. Retrieved from http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/5673.0.55.0032005-06%20to%202010-11?OpenDocument
- Australian Bureau of Statistics. (2013b). National Health Survey 2011-12: Questionnaire. Retrieved from http://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/EF67D39400D52759CA257ACC000E3EF3/$File/national%20health%20survey%202011-12.pdf
- Australian Bureau of Statistics. (2014a). 4727.0.55.006—Australian Aboriginal and Torres Strait Islander Health Survey: Updated results, 2012–13. Retrieved from http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4727.0.55.0062012%E2%80%9313?OpenDocument
- Australian Bureau of Statistics. (2014b). 6310.0—Employee Earnings, Benefits and Trade Union Membership, Australia, August 2013. Retrieved from http://www.abs.gov.au/ausstats/abs@.nsf/mf/6310.0
- Australian Bureau of Statistics. (2015a). 6227.0—Education and work, Australia, May 2015. Retrieved from http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/6227.0May%202015?OpenDocument
- Australian Bureau of Statistics. (2015b). Australian Health Survey: First results, 2014-2015. Retrieved from http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4364.0.55.0012014-15?OpenDocument
- Australian Institute of Health and Welfare. (2016). Life expectancy. Retrieved from http://www.aihw.gov.au/deaths/life-expectancy/
- Bergeron D., Tylka T. L. (2007). Support for the uniqueness of body dissatisfaction from drive for muscularity among men. Body Image, 4, 288-295. [DOI] [PubMed] [Google Scholar]
- Blashill A. J. (2011). Gender roles, eating pathology, and body dissatisfaction in men: A meta-analysis. Body Image, 8, 1-11. [DOI] [PubMed] [Google Scholar]
- Brancato G., Macchia S., Murgia M., Signore M., Simeoni G., Blanke K., . . . Hoffmeyer-Zlotnik J. (2006). Handbook of recommended practices for questionnaire development and testing in the European statistical system. Retrieved from http://www.istat.it/en/files/2013/12/Handbook_questionnaire_development_2006.pdf
- The Department of Health. (2014). Australia’s Physical Activity and Sedentary Behaviour Guidelines. Retrieved from http://www.health.gov.au/internet/main/publishing.nsf/content/health-pubhlth-strateg-phys-act-guidelines
- The Department of Health. (2015). Recommended number of serves for adults. Retrieved from https://www.eatforhealth.gov.au/food-essentials/how-much-do-we-need-each-day/recommended-number-serves-adults
- Douketis J., Macie C., Thabane L., Williamson D. (2005). Systematic review of long-term weight loss studies in obese adults: Clinical significance and applicability to clinical practice. International Journal of Obesity, 29, 1153-1167. [DOI] [PubMed] [Google Scholar]
- Egli T., Bland H. W., Melton B. F., Czech D. R. (2011). Influence of age, sex, and race on college students’ exercise motivation of physical activity. Journal of American College Health, 59, 399-406. [DOI] [PubMed] [Google Scholar]
- Elo A.-L., Leppänen A., Jahkola A. (2003). Validity of a single-item measure of stress symptoms. Scandinavian Journal of Work, Environment & Health, 29, 444-451. [DOI] [PubMed] [Google Scholar]
- Eysenbach G. (2004). Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). Journal of Medical Internet Research, 6(3), e34. doi: 10.2196/jmir.6.3.e34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galani C., Schneider H. (2007). Prevention and treatment of obesity with lifestyle interventions: Review and meta-analysis. International Journal of Public Health, 52, 348-359. [DOI] [PubMed] [Google Scholar]
- Gavarkovs A. G., Burke S. M., Petrella R. J. (2015). Engaging men in chronic disease prevention and management programs: A scoping review. American Journal of Men’s Health. Advance online publication. doi: 10.1177/1557988315587549 [DOI] [PubMed] [Google Scholar]
- Gibala M. J., McGee S. L. (2008). Metabolic adaptations to short-term high-intensity interval training: A little pain for a lot of gain? Exercise and Sport Sciences Reviews, 36, 58-63. [DOI] [PubMed] [Google Scholar]
- Godin G., Shephard R. J. (1985). A simple method to assess exercise behavior in the community. Canadian Journal of Applied Sport Sciences. Journal Canadien des Sciences Appliquees au Sport, 10, 141-146. [PubMed] [Google Scholar]
- Gough B., Conner M. T. (2006). Barriers to healthy eating amongst men: A qualitative analysis. Social Science & Medicine, 62, 387-395. [DOI] [PubMed] [Google Scholar]
- Greaney M. L., Less F. D., White A. A., Dayton S. F., Riebe D., Blissmer B., . . . Greene G. W. (2009). College students’ barriers and enablers for healthful weight management: A qualitative study. Journal of Nutrition Education and Behavior, 41, 281-286. [DOI] [PubMed] [Google Scholar]
- Hagen P., Collin P., Metcalf A., Nicholas M., Rahilly K., Swainston N. (2012). Participatory design of evidence-based online youth mental health promotion, intervention and treatment. Melbourne, Victoria, Australia: Melbourne Young and Well Cooperative Research Centre. [Google Scholar]
- Hankey C. R., Leslie W. S., Lean M. E. (2002). Why lose weight? Reasons for seeking weight loss by overweight but otherwise healthy men. International Journal of Obesity and Related Metabolic Disorders, 26, 880-882. doi: 10.1038/sj.ijo.0801999 [DOI] [PubMed] [Google Scholar]
- Hebden L., Chan H., Louie J., Rangan A., Allman-Farinelli M. (2015). You are what you choose to eat: Factors influencing young adults’ food selection behaviour. Journal of Human Nutrition and Dietetics, 28, 401-408. [DOI] [PubMed] [Google Scholar]
- Holley T. J., Collins C. E., Morgan P. J., Callister R., Hutchesson M. J. (2015). Weight expectations, motivations for weight change and perceived factors influencing weight management in young Australian women: A cross-sectional study. Public Health Nutrition, 19, 275-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keel P. K., Baxter M. G., Heatherton T. F., Joiner T. E., Jr. (2007). A 20-year longitudinal study of body weight, dieting, and eating disorder symptoms. Journal of Abnormal Psychology, 116, 422-432. [DOI] [PubMed] [Google Scholar]
- LaCaille L. J., Dauner K. N., Krambeer R. J., Pedersen J. (2011). Psychosocial and environmental determinants of eating behaviors, physical activity, and weight change among college students: A qualitative analysis. Journal of American College Health, 59, 531-538. [DOI] [PubMed] [Google Scholar]
- LaRose J. G., Tate D. F., Gorin A. A., Wing R. R. (2010). Preventing weight gain in young adults: A randomized controlled pilot study. American Journal of Preventive Medicine, 39, 63-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Las Nueces D., Hacker K., DiGirolamo A., Hicks L. S. (2012). A systematic review of community-based participatory research to enhance clinical trials in racial and ethnic minority groups. Health Services Research, 47(3, Pt. 2), 1363-1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyk D., Witzki A., Sievert A., Rohde U., Moedl A., Rüther T., . . . Hackfort D. (2012). Importance of sports during youth and exercise barriers in 20- to 29-year-old male nonathletes differently motivated for regular physical activities. Journal of Strength and Conditioning Research, 26, S15-S22. [DOI] [PubMed] [Google Scholar]
- Liu K., Daviglus M. L., Loria C. M., Colangelo L. A., Spring B., Moller A. C., Lloyd-Jones D. M. (2012). Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: The Coronary Artery Risk Development in (Young) Adults (CARDIA) Study. Circulation, 125, 996-1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCreary D. R., Sasse D. K. (2000). An exploration of the drive for muscularity in adolescent boys and girls. Journal of American College Health, 48, 297-304. [DOI] [PubMed] [Google Scholar]
- McCullough M. L., Willett W. C. (2006). Evaluating adherence to recommended diets in adults: The Alternate Healthy Eating Index. Public Health Nutrition, 9(1A), 152-157. [DOI] [PubMed] [Google Scholar]
- Morgan P. J., Warren J. M., Lubans D. R., Collins C. E., Callister R. (2011). Engaging men in weight loss: Experiences of men who participated in the male only SHED-IT pilot study. Obesity Research & Clinical Practice, 5, e239-e248. [DOI] [PubMed] [Google Scholar]
- Morgan P. J., Young M. D., Smith J. J., Lubans D. R. (2016). Targeted health behavior interventions promoting physical activity: A conceptual model. Exercise and Sport Sciences Reviews, 44, 71-80. [DOI] [PubMed] [Google Scholar]
- National Health and Medical Research Council. (2015). Alcohol guidelines: Reducing the health risks. Retrieved from https://www.nhmrc.gov.au/health-topics/alcohol-guidelines
- Oliffe J. L., Greaves L. (2012). Designing and conducting gender, sex, and health research. Thousand Oak, CA: Sage. [Google Scholar]
- Pagoto S. L., Schneider K. L., Oleski J. L., Luciani J. M., Bodenlos J. S., Whited M. C. (2012). Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity, 20, 1234-1239. [DOI] [PubMed] [Google Scholar]
- Parker E. D., Schmitz K. H., Jacobs D. R., Jr., Dengel D. R., Schreiner P. J. (2007). Physical activity in young adults and incident hypertension over 15 years of follow-up: The CARDIA study. American Journal of Public Health, 97, 703-709. doi: 10.2105/AJPH.2004.055889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereira M. A., Kartashov A. I., Ebbeling C. B., Van Horn L., Slattery M. L., Jacobs D. R., Ludwig D. S. (2005). Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-Year prospective analysis. Lancet, 365, 36-42. [DOI] [PubMed] [Google Scholar]
- Poobalan A. S., Aucott L. S., Precious E., Crombie I. K., Smith W. C. (2010). Weight loss interventions in young people (18 to 25 year olds): A systematic review. Obesity Reviews, 11, 580-592. [DOI] [PubMed] [Google Scholar]
- Pursey K., Burrows T. L., Stanwell P., Collins C. E. (2014). How accurate is web-based self-reported height, weight, and body mass index in young adults? Journal of Medical Internet Research, 16(1), e4. doi: 10.2196/jmir.2909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramo D. E., Hall S. M., Prochaska J. J. (2011). Reliability and validity of self-reported smoking in an anonymous online survey with young adults. Health Psychology, 30, 693-701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnicow K., Baranowski T., Ahluwalia J., Braithwaite R. (1998). Cultural sensitivity in public health: Defined and demystified. Ethnicity & Disease, 9(1), 10-21. [PubMed] [Google Scholar]
- Ridgeway R. T., Tylka T. L. (2005). College men’s perceptions of ideal body composition and shape. Psychology of Men & Masculinity, 6, 209-220. [Google Scholar]
- Sabinsky M. S., Toft U., Raben A., Holm L. (2007). Overweight men’s motivations and perceived barriers towards weight loss. European Journal of Clinical Nutrition, 61, 526-531. doi: 10.1038/sj.ejcn.1602537 [DOI] [PubMed] [Google Scholar]
- Stanwick J., Lu T., Rittie T., Circelli M. (2014). How young people are faring in the transition from school to work. Retrieved from http://unlimitedpotential.fya.org.au/wp-content/uploads/2014/10/NVCER-report-FINAL-single-pages.pdf
- StataCorp. (2011) Stata (Version 12) [Statistical software]. College Station, TX: Author. [Google Scholar]
- Tate D. F., LaRose J. G., Griffin L. P., Erickson K. E., Robichaud E. F., Perdue L., . . . Wing R. R. (2014). Recruitment of young adults into a randomized controlled trial of weight gain prevention: Message development, methods, and cost. Trials, 15(1), 326. doi: 10.1186/1745-6215-15-326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uglem S., Stea T. H., Kjøllesdal M. K. R., Frølich W., Wandel M. (2013). A nutrition intervention with a main focus on vegetables and bread consumption among young men in the Norwegian National Guard. Food & Nutrition Research, 57. doi: 10.3402/fnr.v57i0.21036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandenbroucke J. P., Von Elm E., Altman D. G., Gøtzsche P. C., Mulrow C. D., Pocock S. J., . . . Egger M. (2007). Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Annals of Internal Medicine, 147(8), W-163-W-194. doi: 10.7326/0003-4819-147-8-200710160-00010-w1 [DOI] [PubMed] [Google Scholar]
- Victorian Government. (2009). Body image—Men. Retrieved from https://www.betterhealth.vic.gov.au/health/healthyliving/body-image-men
- Walsh J. R., White A. A., Greaney M. L. (2009). Using focus groups to identify factors affecting healthy weight maintenance in college men. Nutrition Research, 29, 371-378. [DOI] [PubMed] [Google Scholar]
- White A., Zwolinsky S., Pringle A., McKenna J., Daly-Smith A., Robertson S., Berry R. (2012). Premier League Health: A national programme of men’s health promotion delivered in/by professional football clubs: Final report 2012. Leeds, England: Leeds Metropolitan University. [Google Scholar]
- World Health Organization. (2000). Obesity: Preventing and managing the global epidemic. Retrieved from http://www.who.int/nutrition/publications/obesity/WHO_TRS_894/en/ [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


