Abstract
Few studies have assessed differences in the prevalence of and economic burden attributable to tobacco smoking, excess weight, physical inactivity, and alcohol use by gender. This article examines these gender differences in Canadians between the ages of 30 and 64 years. It also estimates the potential cost avoidance if the prevalence of the four risk factors (RFs) were reduced modestly in males. Data on the prevalence of the RFs and the relative risk of disease associated with each of the RFs were combined to calculate population-attributable fractions. A prevalence-based cost-of-illness approach was used to estimate the economic burden associated with the four RFs. Middle-aged Canadian males are more likely to smoke tobacco (26.4% vs. 20.2%), consume hazardous or harmful levels of alcohol (14.6% vs. 8.2%), and have excess weight (65.6% vs. 47.1%) than middle-aged Canadian females, resulting in an annual economic burden that is 27% higher in males than females. No significant differences were observed in the proportion of males who are physically inactive (48.4% vs. 49.4%). Modelling only a 1% annual relative reduction each year through to 2036 would result in a cumulative cost avoidance between 2013 and 2036 of $50.7 billion. The differences in RF prevalence between middle-aged males and females have an important effect on the population’s economic burden. A modest annual reduction in the four RFs in males can significantly affect population health and the economy over time.
Keywords: economic burden of disease, risk factors, smoking, alcohol use, obesity, overweight, physical inactivity
Introduction
When assessing the health of populations, gender matters (Salzman & Wender, 2006). Yet the historical approach to men’s health has tended to focus primarily on issues of the prostate and sexual function (Sadovsky & Levine, 2005). The world’s first Congress on Men’s Health was held in 2001 and focused on broader issues such as men’s shorter life expectancies and gender differences in accessing health information and seeking medical advice (Baker, 2001).
In Canada, male life expectancy is 79 years, compared with 83 years for females (Statistics Canada, 2012). The cause of death also varies substantially between males and females (Statistics Canada, 2015). For example, the age-standardized mortality rate for malignant neoplasms (ICD10 C00-C97) in Canadian males is 184 per 100,000 compared with 133 per 100,000 for Canadian females. Likewise, the mortality rate for major cardiovascular diseases (ICD10 I00-I78) is 159 per 100,000 for males compared with 97 per 100,000 for females (Statistics Canada, 2015). There is also evidence that the economic burden attributable to tobacco smoking, excess weight, and physical inactivity is higher in Canadian males than females (Krueger, Krueger, & Koot, 2015).
The Canadian Men’s Health Foundation (2015b) is a national, nonprofit organization founded in June of 2014. The goal of the foundation is
to raise social awareness of largely preventable health problems and to enable men, and their families to value men’s health by providing them with information and healthy lifestyle programs that will motivate them to truly hear, absorb and act on it. (Goldenberg, 2014)
The Canadian Men’s Health Foundation’s (2015a) Don’t Change Much campaign is an innovative health promotion campaign and website created specifically to encourage men to make small changes toward healthier habits, including increasing physical activity, reducing excess weight, limiting alcohol consumption, and quitting tobacco smoking.
The purpose of this study is to assess four important modifiable risk factors (RFs): physical inactivity, excess weight, alcohol use, and tobacco smoking in Canadian men between the ages of 30 and 64 years. In particular, the following questions were investigated: (a) How does the prevalence and economic burden attributable to these RFs differ by sex in Canada? (b) What would the potential cost avoidance be if the prevalence of these RFs in Canadian men were reduced by a relative 1% per year between 2013 and 2036?
Method
The details of the base model, together with an update, have been previously published (Krueger et al., 2015; Krueger, Turner, Krueger, & Ready, 2014; Krueger, Williams, Ready, Trenaman, & Turner, 2013). In short, an approach based on population attributable fraction (PAF) was used to estimate the economic burden associated with the four RFs. This involved the following steps: (a) estimation of the RF prevalence; (b) estimation of the causal relationship between the RF and comorbidities; (c) calculation of the PAF for all ages in the population; (d) estimation of the direct costs of treating the comorbidities associated with the RFs; (e) adjustment of the direct costs for overlapping RFs in a given individual; (f) estimation of indirect costs; (g) allocation of costs to the population aged 30 to 64 years; and (h) modelling of the potential cost avoidance associated with a modest 1% annual relative reduction (ARR) in the prevalence of the RFs between 2013 and 2036.
Prevalence of the Risk Factors
Prevalence rates for tobacco smoking, excess weight, physical inactivity, and alcohol use were drawn from the 2011/2012 Canadian Community Health Survey (CCHS; Statistics Canada, 2013). Individuals were considered overweight if their body mass index (BMI) was between 25 kg/m2 and 29.9 kg/m2 and obese if their BMI was equal to or greater than 30 kg/m2, calculated based on self-reported height and weight. Tobacco smokers were grouped as light (<10 cigarettes per day), moderate (10-19 cigarettes per day), and heavy (≥20 cigarettes per day) smokers based on the average number of cigarettes smoked per day. All current smokers who identified themselves as occasional smokers were included in the light smoking category. Physical inactivity rates were based on people categorized as “inactive” (leisure time energy expenditure of less than 1.5 kcal/kg/day) in the CCHS.
The prevalence of both chronic and binge alcohol use was estimated based on CCHS data adjusted for underreporting. Research has identified that it is common for alcohol use to be underreported, as individuals either report fewer drinks than are actually consumed or are unaware of the amount of alcohol present in their drinks (Kerr & Stockwell, 2012). Males were categorized as abstainer or very light (0-0.24 g/day), Category I—low (0.25-39.9 g/day), Category II—hazardous (40.0-59.9 g/day), and Category III—harmful (≥60.0 g/day). Females were categorized as abstainer or very light (0-0.24 g/day), Category I—low (0.25-19.9 g/day), Category II—hazardous (20.0-39.9 g/day), and Category III—harmful (≥40.0 g/day; Taylor et al., 2007). A female binge drinker was defined as a female who consumes at least four drinks (containing 13.6 g of ethanol) on one occasion at least once per month during the past 12 months. A male binge drinker was defined as a male who consumes at least five drinks on one occasion at least once per month during the past 12 months.
Estimating Relative Risks
The sources and values for the relative risks associated with excess weight (Pirie et al., 2013), tobacco smoking (Guh et al., 2009), and physical inactivity (Katzmarzyk & Janssen, 2004) remain the same as in the previously published model (Krueger et al., 2015). Relative risk values associated with alcohol use were assembled from a collection of studies that together describe the relative risk of all major comorbidities associated with both chronic and acute alcohol use (Bagnardi, Blangiardo, La Vecchia, & Corrao, 2001; Bagnardi et al., 2013; Baliunas et al., 2009; Fedirko et al., 2011; Islami et al., 2011; Lönnroth, Williams, Stadlin, Jaramillo, & Dye, 2008; Patra et al., 2010; Patra et al., 2011; Roerecke & Rehm, 2012; Samokhvalov, Irving, Mohapatra, & Rehm, 2010; Samokhvalov, Irving, & Rehm, 2010a, 2010b; Taylor et al., 2009; Taylor et al., 2010; Tramacere et al., 2010).
Calculating the Population Attributable Fraction
Sex-, RF-, and disease-specific PAFs were calculated for all ages combined in the population using the extension of Levin’s formula (Levin, 1953):
where i denotes a given exposure level, pi is the prevalence of that exposure level in the population, and RRi is the relative risk of a given disease for the given exposure level. Physical inactivity was regarded as a dichotomous exposure (no physical inactivity and physical inactivity), excess weight was regarded as a trichotomous exposure (no excess weight, overweight, and obesity), and tobacco smoking and alcohol use were regarded as tetrachotomous exposures (no smoking, light smoking, moderate smoking, and heavy smoking; abstaining, low alcohol use, hazardous alcohol use, and harmful alcohol use).
Estimating Costs
The economic burden (direct and indirect costs) associated with the RFs was estimated using a prevalence-based cost-of-illness approach. The cost estimates are expressed in 2013 Canadian dollars.
Direct Cost
Direct costs, including hospital care, physician services, other health care professionals (excluding dental services), drugs, health research, and “other” health care expenditures, were extracted from the National Health Expenditure Database (Canadian Institute for Health Information, 2013). Hospital care, physician care, and drug costs were allocated to each comorbidity, stratified by sex, based on 2008 data from the Economic Burden of Illness in Canada (EBIC) online tool (Public Health Agency of Canada, 2014).
EBIC 2008 does not allocate costs for other health care professionals (excluding dental services), health research, or “other” health care expenditures. These were estimated by allocating costs according to the same proportional distribution as hospital, physician, and drug costs.
These direct care costs were multiplied by the calculated RF-, sex-, and comorbidity-specific PAFs to calculate the direct care costs attributable to a given RF.
Adjusting Direct Costs in a Multifactorial System
To adjust for double counting, the combined PAF in a multifactorial system was calculated using the following formula (Krueger et al., 2013):
where PAFTS is the crude PAF of cost for tobacco smoking, PAFEW is the crude PAF of cost for excess weight, PAFPIA is the crude PAF of cost for physical inactivity, and PAFAU is the crude PAF of cost for alcohol use.
A disaggregation step was applied at the end of the direct costing process to assign an economic burden to each RF. This was achieved by dividing the crude cost for each RF by the sum of costs for all the RFs (i.e., the crude total cost for the combined system), thereby generating a ratio which was applied to the adjusted total cost.
Estimating Indirect Costs
Indirect costs were calculated following the method used in EBIC 1998 (a modified human-capital approach; Health Canada, 2002). The ratio of direct to indirect costs was determined for each diagnostic category within EBIC 1998, stratified by short-term disability, long-term disability, and premature mortality. Each ratio was applied to the previously identified direct costs within each diagnostic category attributable to individual RFs in order to generate the equivalent indirect cost data.
Distributing Costs Among Age Groups
Costs for individuals aged 30 to 64 years were calculated by distributing costs among age groups, proportional to the number of individuals in the population with each RF exposure level.
Modelling Cost Avoidance
A number of assumptions were made in modelling the economic benefits associated with future RF reduction (Krueger et al., 2014). First, population projections for the 24-year time frame from 2013 to 2036 by sex and 5-year age group were based on projections by Statistics Canada (2010). Second, the base model uses a 1% relative annual reduction in the RFs. Current trends of decreasing smoking prevalence and increasing weight and inactivity are not factored into the model. Third, constant 2013 dollars are used throughout the modelling process (i.e., no adjustments are made for projected inflation) to clearly identify changes in the economic burden associated with changing RF prevalence, rather than confusing these results with inflationary increases. Fourth, obese individuals who experience a reduction in excess weight move into the overweight category instead of immediately becoming a healthy weight. Last, the benefits associated with physical activity and healthy weights accrue within 1 year; however, the benefits of smoking cessation and reduced alcohol consumption accrue over time (Heckley, Jarl, Asamoah, & Ulf, 2011; Jarl & Gerdtham, 2012; Jarl, Gerdtham, Ludbrook, & Petrie, 2010; Kenfield, Stampfer, Rosner, & Colditz, 2008; Kiadaliri, Jarl, Gavriilidis, & Gerdtham, 2013).
Sensitivity Analysis
The point estimates for RR are used in the base model and a sensitivity analysis was performed using the lower and upper bounds of the 95% confidence interval (CI) for each RR value. The base model also assumes that there is no protective effect of low, chronic consumption of alcohol. This assumption was tested in the sensitivity analysis.
Results
A higher proportion of Canadian males aged 30 to 64 years smoke tobacco compared with females, with a major difference being the proportion of heavy smokers (10.1% of males vs. 4.6% of females, see Table 1). A higher proportion of males also use alcohol at every level of consumption, particularly at levels that are considered to be hazardous or harmful (14.6% of males vs. 8.2% of females), and of those who use alcohol, a higher proportion of males are binge drinkers (41.8% of males vs. 30.8% of females). A higher proportion of males also have excess weight (65.6% of males vs. 47.1% of females); however, there are a higher proportion of females than males with a BMI ≥40 (1.5% of males vs. 2.8% of females).
Table 1.
Prevalence of Tobacco Smoking, Excess Weight, Physical Inactivity, and Alcohol Use in Canada for Males and Females Ages 30 to 64, 2013.
| Females (%) | Males (%) | Absolute difference (%) | % Difference | p a | |
|---|---|---|---|---|---|
| Tobacco smoking | |||||
| Light | 8.6 | 8.4 | −0.3 | −3.2 | .886 |
| Moderate | 7.0 | 8.0 | 1.0 | 14.5 | .144 |
| Heavy | 4.6 | 10.1 | 5.5 | 121.5 | .002 |
| Subtotal: Tobacco smoking | 20.2 | 26.4 | 6.3 | 31.2 | .006 |
| Excess weight | |||||
| Overweight | 27.0 | 44.3 | 17.2 | 63.8 | <.001 |
| Obese Class I (BMI of 30-34.9) | 12.8 | 16.0 | 3.1 | 24.4 | .025 |
| Obese Class II (BMI of 35-39.9) | 4.5 | 3.9 | −0.6 | −12.6 | .217 |
| Obese Class III (BMI ≥ 40) | 2.8 | 1.5 | −1.3 | −47.1 | .003 |
| Subtotal: Obesity | 20.1 | 21.4 | 1.3 | 6.3 | .455 |
| Subtotal: Excess weight | 47.1 | 65.6 | 18.5 | 39.3 | <.001 |
| Physical inactivity | 49.4 | 48.4 | −1.1 | −2.2 | .378 |
| Alcohol use | |||||
| Category I: Low | 53.2 | 61.0 | 7.8 | 14.7 | <.001 |
| Category II: Hazardous | 5.6 | 7.6 | 2.0 | 35.7 | <.001 |
| Category III: Harmful | 2.6 | 7.0 | 4.4 | 170.1 | <.001 |
| Subtotal: Alcohol use | 61.4 | 75.6 | 14.3 | 23.2 | <.001 |
| Percentage of drinkers who binge | 30.8 | 41.8 | 11.0 | 35.7 | .010 |
Note. BMI = body mass index.
Two-tailed t test, α=0.05.
The total economic burden attributable to the four RFs in Canadian males aged 30 to 64 years is estimated at $22.8 (95% CI [$19.5, $25.9]) billion in 2013 (Table 2). This is $6.1 billion (27%) more than females in the same age group ($16.7 billion, 95% CI [$13.8, $19.6]).
Table 2.
Estimated Annual Economic Burden Attributable to Tobacco Smoking, Excess Weight, Physical Inactivity, and Alcohol Use in Canada for Males and Females Ages 30 to 64 Years, 2013.
| % Population with RF | No. of Individuals with RF | Direct cost per individual with RF, $ [95% CI] | Indirect cost per individual with RF, $ [95% CI] | Total cost per individual with RF, $ [95% CI] | Total direct cost of RF, million $ [95% CI] | Total indirect cost of RF, million $ [95% CI] | Total cost of RF, million $ [95% CI] | |
|---|---|---|---|---|---|---|---|---|
| Males | ||||||||
| Tobacco smoking | ||||||||
| Light | 8.4 | 711,906 | 800 [732, 867] | 1,561 [1,397, 1,725] | 2,361 [2,129, 2,592] | 570 [521, 617] | 1,111 [995, 1,228] | 1,681 [1,516, 1,845] |
| Moderate | 8.0 | 679,508 | 1,322 [1,271, 1,374] | 2,555 [2,463, 2,647] | 3,877 [3,734, 4,020] | 898 [864, 933] | 1,736 [1,674, 1,798] | 2634 [2,537, 2,732] |
| Heavy | 10.1 | 861,961 | 1,625 [1,540, 1,714] | 3,115 [2,957, 3,278] | 4,740 [4,497, 4,992] | 1,401 [1,328, 1,478] | 2,685 [2,549, 2,825] | 4,086 [3,876, 4,303] |
| Subtotal: Male tobacco smoking | 26.4 | 2,253,376 | 1,273 [1,204, 1,344] | 2,455 [2,315, 2,597] | 3,728 [3,519, 3,941] | 2,868 [2,713, 3,028] | 5,533 [5,217, 5,852] | 8,401 [7,930, 8,880] |
| Excess weight | ||||||||
| Overweight | 44.3 | 3,774,383 | 203 [146, 253] | 568 [417, 693] | 771 [563, 946] | 766 [550, 955] | 2,144 [1,574, 2,617] | 2,910 [2,125, 3,571] |
| Obese | 21.3 | 1,819,411 | 737 [570, 897] | 1,685 [1,285, 2,057] | 2,422 [1,855, 2,954] | 1,340 [1,037, 1,632] | 3,066 [2,338, 3,743] | 4,407 [3,374, 5,375] |
| Subtotal: Male excess weight | 65.6 | 5,593,794 | 366 [284, 462] | 908 [699, 1,137] | 1,308 [983, 1,599] | 2,107 [1,587, 2,586] | 5,210 [3,912, 6,360] | 7,316 [5,499, 8,946] |
| Physical inactivity | 48.4 | 4,122,237 | 221 [175, 265] | 394 [313, 474] | 614 [488, 739] | 910 [723, 1,093] | 1,623 [1,290, 1,953] | 2,533 [2,013, 3,046] |
| Alcohol use | ||||||||
| Category I: Low | 61.0 | 5,202,459 | 78 [67, 88] | 202 [173, 223] | 280 [239, 311] | 408 [347, 456] | 1,051 [898, 1,162] | 1,458 [1,246, 1,618] |
| Category II: Hazardous | 7.6 | 648,815 | 493 [426, 569] | 1,076 [956, 1,198] | 1,569 [1,382, 1,767] | 320 [276, 369] | 698 [620, 777] | 1,018 [896, 1,146] |
| Category III: Harmful | 7.0 | 597,660 | 1,246 [1,141, 1,341] | 2,254 [1,985, 2,524] | 3,500 [3,126, 3,865] | 744 [682, 801] | 1,347 [1,186, 1,509] | 2,092 [1,869, 2,310] |
| Subtotal: Male alcohol use | 75.6 | 6,448,935 | 228 [203, 252] | 480 [419, 535] | 708 [622, 787] | 1,472 [1,306, 1,627] | 3,096 [2,705, 3,448] | 4,568 [4,011, 5,074] |
| Subtotal: Males | 7,357 [6,329, 8,334] | 15,462 [13,124, 17,612] | 22,818 [19,453, 25,946] | |||||
| Females | ||||||||
| Tobacco smoking | ||||||||
| Light | 8.6 | 736,735 | 610 [558, 663] | 1,166 [1,053, 1,282] | 1,776 [1,610, 1,945] | 450 [411, 489] | 859 [776, 944] | 1,309 [1,186, 1,433] |
| Moderate | 7.0 | 594,802 | 1,054 [1,008, 1,102] | 2,037 [1,949, 2,128] | 3,091 [2,958, 3,230] | 627 [600, 656] | 1,212 [1,160, 1,266] | 1,838 [1,759, 1,921] |
| Heavy | 4.6 | 389,818 | 1,665 [1,581, 1,759] | 3,213 [3,056, 3,387] | 4,878 [4,636, 5,147] | 649 [616, 686] | 1,252 [1,191, 1,320] | 1,901 [1,807, 2,006] |
| Subtotal: Female tobacco smoking | 20.2 | 1,721,355 | 1,002 [945, 1,063] | 1,931 [1,816, 2,051] | 2,933 [2,761, 3,114] | 1,725 [1,626, 1,830] | 3,323 [3,126, 3,530] | 5,048 [4,753, 5,360] |
| Excess weight | ||||||||
| Overweight | 27.0 | 2,308,326 | 297 [207, 383] | 775 [583, 954] | 1,072 [790, 1,337] | 686 [477, 883] | 1,789 [1,346, 2,202] | 2,475 [1,823, 3,086] |
| Obesity | 20.1 | 1,715,699 | 902 [678, 1,120] | 1,963 [1,541, 2,371] | 2,864 [2,219, 3,492] | 1,547 [1,163, 1,922] | 3,367 [2,644, 4,069] | 4,914 [3,807, 5,991] |
| Subtotal: Female excess weight | 47.1 | 4,024,025 | 366 [407, 697] | 908 [991, 1,558] | 1,836 [1,399, 2,256] | 2,233 [1,640, 2,805] | 5,156 [3,990, 6,271] | 7,390 [5,629, 9,077] |
| Physical inactive | 49.4 | 4,223,445 | 187 [143, 228] | 432 [332, 525] | 619 [474, 752] | 789 [603, 962] | 1,826 [1,400, 2,216] | 2,615 [2,003, 3,177] |
| Alcohol use | ||||||||
| Category I: Low | 53.2 | 4,542,791 | 36 [25, 42] | 89 [73, 101] | 125 [98, 143] | 165 [114, 192] | 405 [331, 458] | 569 [445, 649] |
| Category II: Hazardous | 5.6 | 479,167 | 282 [273, 309] | 573 [545, 620] | 855 [818, 929] | 135 [131, 148] | 275 [261, 297] | 410 [392, 445] |
| Category III: Harmful | 2.6 | 221,605 | 1,163 [1,013, 1,405] | 1,981 [1,607, 2,467] | 3,144 [2,621, 3,873] | 258 [225, 311] | 439 [356, 547] | 697 [581, 858] |
| Subtotal: Female alcohol use | 61.4 | 5,243,564 | 106 [90, 124] | 213 [181, 248] | 320 [270, 372] | 557 [470, 651] | 1,118 [948, 1,301] | 1,676 [1,417, 1,953] |
| Subtotal: Females | 5,304 [4,339, 6,248] | 11,424 [9,464, 13,319] | 16,728 [13,803, 19,567] | |||||
Note. RF = risk factor; CI = confidence interval. Adjusted for multiple RFs in one individual.
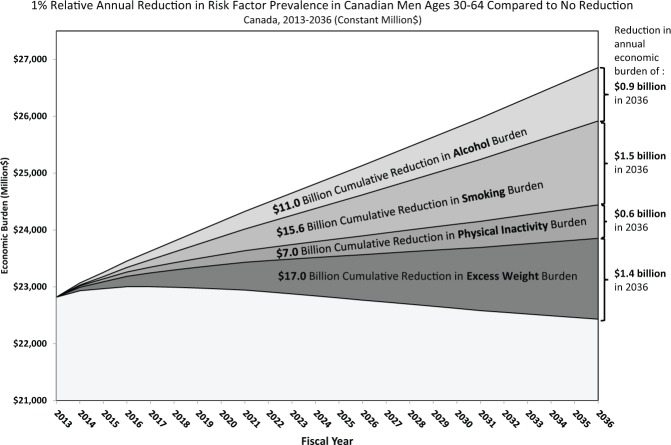
In estimating the cost avoidance, a 1% ARR was modelled each year through to 2036 (1% scenario). With no change in the prevalence of the RFs, the annual economic burden would increase from $22.8 billion in 2013 to $26.9 billion in 2036, due to projected population growth. Applying the 1% scenario would reduce the projected annual economic burden in 2036 from $26.9 to $22.4 billion (Figure 1). The cumulative cost avoidance between 2013 and 2036 would total $50.7 billion. Of this cumulative cost avoidance, approximately 33% ($16.6 billion) would be attributable to direct costs and 67% ($34.1 billion) to indirect costs. The highest proportion (34% or $17.0 billion) of the cumulative cost avoidance would be due to a reduction in excess weight, with 31% ($15.6 billion) due to a reduction in tobacco smoking, 22% ($11.0 billion) due to a reduction in alcohol use and 14% ($7.0 billion) due to a reduction in physical inactivity.
Figure 1.
Changes in economic burden of smoking excess weight, physical inactivity, and alcohol use.
Discussion
There are a number of key differences between middle-aged males and females in terms of tobacco smoking, excess weight, physical inactivity, and alcohol use in Canada, and these differences likely have an important effect on the health and economic burden in the population. Modelling a 1% relative annual risk reduction in middle-aged Canadian men suggests that there is the potential to reduce the projected annual economic burden in 2036 from $26.9 billion to $22.4 billion (17%), with a cumulative cost avoidance of $50.7 billion between 2013 and 2036.
Can this reduction reasonably be achieved? Between 2000 and 2013, the prevalence of tobacco smoking in Canadian men aged 30 to 64 years declined from 30.9% to 26.4%, an ARR of 1.2%. More important, the prevalence of heavy smoking declined by an ARR of 3.0%. The prevalence of physical inactivity has also declined from 55.4% in 2000 to 48.4% in 2013 (ARR of 1.0%). Unlike tobacco smoking and physical inactivity, however, the prevalence of obesity in Canadian males has increased from 17.7% in 2000 to 21.3% in 2013, an annual relative increase of 1.4%. The annual relative increase is 1.1% for those with a BMI of 30.0 to 34.9, 2.0% for a BMI of 35.0 to 39.9, and 4.5% for a BMI ≥40.0.
Trends in the prevalence of harmful or hazardous levels of alcohol consumption are more complicated than trends in the other three RFs. Between 2000 and 2008, the prevalence of harmful or hazardous levels of alcohol consumption increased from 12.5% to 15.9% (an annual relative increase of 3.1%) and then declined to 14.6% in 2009 and has remained relatively stable since then. The drop in prevalence coincides with the global recession in 2008/2009.
Recent trends in the prevalence of tobacco smoking and physical inactivity in middle-aged Canadian men have been positive and would simply need to continue to achieve the longer term results indicated in the 1% scenario. The negative trends in obesity, however, would need to be stopped and then reversed to be able to achieve results in the 1% scenario. The high relative annual increase in the prevalence of harmful or hazardous levels of alcohol consumption between 2000 and 2008 (3.1%) seems to have been reversed between 2009 and 2013. It is not clear why the observed reduction in 2009 occurred, followed by stability in prevalence between 2009 and 2013; however, it is possible that changes in the overall economy and a subsequent decrease in earning potential resulted in less disposable income for the purchase of alcoholic beverages. Nevertheless, the current trend would not only need to be maintained but would need to decline to achieve results in the 1% scenario.
In recent years, a debate has persisted over the evidence in favor and against the benefits of modest nonbinge alcohol use. Current evidence suggests that the observed protective effect may be exaggerated due to a number of methodological flaws in devising this association (Bergmann et al., 2013; Holmes et al., 2014; Stockwell, Greer, Fillmore, Chikritzhs, & Zeisser, 2012). As a result, the assumption in the base model is that there is neither increased nor decreased risk of those diseases for which some evidence suggests a protective effect. If the putative decreased risks in type 2 diabetes mellitus, ischemic heart disease, and ischemic stroke are included in the model, then the economic burden attributable to alcohol use in middle-aged Canadian males decreases from $4.6 billion to $4.0 billion (−12.7%) in 2013. Also note that the alcohol-attributable economic burden based on the model does not include increased costs associated with law enforcement or fire/traffic accident damage (Canadian Centre on Substance Abuse, 2006; Public Health Agency of Canada, 2016).
There are a number of limitations with this study. First, most studies categorize individuals with a BMI between 25 kg/m2 and 29.9 kg/m2 as overweight. This is also the approach taken in the current study. This range, especially the lower end, however, has been historically dynamic and some research has suggested that a more appropriate lower boundary with respect to negative health effects might be 27 kg/m2 (Hu et al., 2004). Second, the method of scaling up from direct to indirect costs depends on the assumption that the ratios of costs have not changed over time. Third, the source for the RRs associated with smoking and physical inactivity adjust for known confounding factors in generating disease-specific RRs. The meta-analyses for the RRs associated with overweight and obesity, however, did not include physical inactivity as a potentially confounding RF which may lead to an overestimate of the economic burden attributable to excess weight. On the other hand, RRs calculated in this meta-analysis are based on a combination of studies including both self-reported and objective measures of BMI while the model uses the prevalence of excess weight based on self-reported height and weight, which may lead to an underestimate of the economic burden attributable to excess weight. Fourth, calculating the prevalence of alcohol use by sex, age, and consumption category is particularly challenging, given current data availability and issues of underreporting. Despite the best efforts to adjust for underreporting, the actual prevalence of alcohol use may vary from the current estimates. Fifth, the inclusion of indirect costs in any economic analysis is controversial, given that a variety of approaches exist, all of which generate very different results. This study uses a modified human capital approach as this approach places an economic value on time lost due to disability and premature mortality.
Conclusion
There are a number of key differences between middle-aged males and females in terms of tobacco smoking, excess weight, physical inactivity, and alcohol use in Canada, and these differences likely have an important effect on the health and economic burden in the population. A modest annual reduction in the RFs can have an important public health impact over time.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: H. Krueger & Associates Inc. received funding from the Canadian Men’s Health Foundation for this research.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Bagnardi V., Blangiardo M., La Vecchia C., Corrao G. (2001). A meta-analysis of alcohol drinking and cancer risk. British Journal of Cancer, 85, 1700-1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagnardi V., Rota M., Botteri E., Tramacere I., Islami F., Fedirko V., . . . Pelucchi C. (2013). Light alcohol drinking and cancer: A meta-analysis. Annals of Oncology, 24, 301-308. [DOI] [PubMed] [Google Scholar]
- Baker P. (2001). Sex & gender matter—From boys to men: The future of men’s health. Proceedings of the 1st World Congress on Men’s Health Retrieved from http://citeseerx.ist.psu.edu/viewdoc/download;jsessionid=949F2769FCBCA4EB6B63484658A1B7CD?doi=10.1.1.195.2184&rep=rep1&type=pdf [Google Scholar]
- Baliunas D. O., Taylor B. J., Irving H., Roerecke M., Patra J., Mohapatra S., Rehm J. (2009). Alcohol as a risk factor for type 2 diabetes: A systematic review and meta-analysis. Diabetes Care, 32, 2123-2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergmann M. M., Rehm J., Klipstein-Grobusch K., Boeing H., Schütze M., Drogan D., Boutron-Ruault M. C. (2013). The association of pattern of lifetime alcohol use and cause of death in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. International Journal of Epidemiology, 42, 1772-1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Centre on Substance Abuse. (2006). The costs of substance abuse in Canada 2002. Retrieved from http://www.ccsa.ca/Resource%20Library/ccsa-011332-2006.pdf
- Canadian Institute for Health Information. (2013). National Health Expenditure Trends, 1975 to 2013. Retrieved from https://secure.cihi.ca/free_products/NHEXTrendsReport_EN.pdf
- Canadian Men’s Health Foundation. (2015a). Don’t Change Much. Retrieved from http://menshealthfoundation.ca/dont-change-much
- Canadian Men’s Health Foundation. (2015b). Home. Retrieved from http://menshealthfoundation.ca/
- Fedirko V., Tramacere I., Bagnardi V., Rota M., Scotti L., Islami F., . . . Boffetta P. (2011). Alcohol drinking and colorectal cancer risk: An overall and dose-response meta-analysis of published studies. Annals of Oncology, 22, 1958-1972. [DOI] [PubMed] [Google Scholar]
- Goldenberg S. L. (2014). Status of men’s health in Canada. Canadian Urological Association Journal, 8(7-8 Suppl. 5), S142-S144. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4145701/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guh D. P., Zhang W., Bansback N., Amarsi Z., Birmingham C. L., Anis A. H. (2009). The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health, 9(1), 88-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Canada. (2002). Economic Burden of Illness in Canada, 1998. Retrieved from http://publications.gc.ca/collections/Collection/H21-136-1998E.pdf
- Heckley G. A., Jarl J., Asamoah B. O., Ulf G. (2011). How the risk of liver cancer changes after alcohol cessation: A review and meta-analysis of the current literature. BMC Cancer, 11, 446. doi: 10.1186/1471-2407-11-446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes M. V., Dale C. E., Zuccolo L., Silverwood R. J., Guo Y., Ye Z., . . . Cavadino A. (2014). Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. British Medical Journal, 349, g4164. doi: 10.1136/bmj.g4164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu F. B., Willett W. C., Li T., Stampfer M. J., Colditz G. A., Manson J. E. (2004). Adiposity as compared with physical activity in predicting mortality among women. New England Journal of Medicine, 351, 2694-2703. [DOI] [PubMed] [Google Scholar]
- Islami F., Fedirko V., Tramacere I., Bagnardi V., Jenab M., Scotti L., . . . Straif K. (2011). Alcohol drinking and esophageal squamous cell carcinoma with focus on light-drinkers and never-smokers: A systematic review and meta-analysis. International Journal of Cancer, 129, 2473-2484. [DOI] [PubMed] [Google Scholar]
- Jarl J., Gerdtham U. G. (2012). Time pattern of reduction in risk of oesophageal cancer following alcohol cessation—A meta-analysis. Addiction, 107, 1234-1243. [DOI] [PubMed] [Google Scholar]
- Jarl J., Gerdtham U. G., Ludbrook A., Petrie D. (2010). On measurement of avoidable and unavoidable cost of alcohol: An application of method for estimating costs due to prior consumption. International Journal of Environmental Research and Public Health, 7, 2881-2895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzmarzyk P. T., Janssen I. (2004). The economic costs associated with physical inactivity and obesity in Canada: An update. Canadian Journal of Applied Physiology, 29, 90-115. [DOI] [PubMed] [Google Scholar]
- Kenfield S. A., Stampfer M. J., Rosner B. A., Colditz G. A. (2008). Smoking and smoking cessation in relation to mortality in women. Journal of the American Medical Association, 299, 2037-2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr W. C., Stockwell T. (2012). Understanding standard drinks and drinking guidelines. Drug and Alcohol Review, 31, 200-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiadaliri A. A., Jarl J., Gavriilidis G., Gerdtham U. G. (2013). Alcohol drinking cessation and the risk of laryngeal and pharyngeal cancers: A systematic review and meta-analysis. PLoS ONE, 8, e58158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger H., Krueger J., Koot J. (2015). Variation across Canada in the economic burden attributable to excess weight, tobacco smoking and physical inactivity. Canadian Journal of Public Health, 106, E171-E177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger H., Turner D., Krueger J., Ready A. E. (2014). The economic benefits of risk factor reduction in Canada: Tobacco smoking, excess weight and physical inactivity. Canadian Journal of Public Health, 105, E69-E78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger H., Williams D., Ready A. E., Trenaman L., Turner D. (2013). Improved estimation of the health and economic burden of chronic disease risk factors in Manitoba. Chronic Diseases and Injuries in Canada, 33, 236-246. [PubMed] [Google Scholar]
- Levin M. L. (1953). The occurrence of lung cancer in man. Acta-Unio Internationalis Contra Cancrum, 9, 531-541. [PubMed] [Google Scholar]
- Lönnroth K., Williams B. G., Stadlin S., Jaramillo E., Dye C. (2008). Alcohol use as a risk factor for tuberculosis—A systematic review. BMC Public Health, 8, 289. doi: 10.1186/1471-2458-8-289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patra J., Bakker R., Irving H., Jaddoe V. W., Malini S., Rehm J. (2011). Dose-response relationship between alcohol consumption before and during pregnancy and the risks of low birthweight, preterm birth and small for gestational age (SGA): A systematic review and meta-analyses. BJOG: An International Journal of Obstetrics and Gynaecology, 118, 1411-1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patra J., Taylor B., Irving H., Roerecke M., Baliunas D., Mohapatra S., Rehm J. (2010). Alcohol consumption and the risk of morbidity and mortality for different stroke types—A systematic review and meta-analysis. BMC Public Health, 10, 258. doi: 10.1186/1471-2458-10-258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirie K., Peto R., Reeves G. K., Green J., Beral V. Million Women Study Collaborators. (2013). The 21st century hazards of smoking and benefits of stopping: A prospective study of one million women in the UK. Lancet, 381, 133-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health Agency of Canada. (2014). Economic Burden of Illness in Canada, 2005-2008. Retrieved from http://www.phac-aspc.gc.ca/publicat/ebic-femc/2005-2008/assets/pdf/ebic-femc-2005-2008-eng.pdf
- Public Health Agency of Canada. (2016). The Chief Public Health Officer’s report on the state of public health in Canada, 2015: Alcohol consumption in Canada. Retrieved from http://healthycanadians.gc.ca/publications/department-ministere/state-public-health-alcohol-2015-etat-sante-publique-alcool/index-eng.php
- Roerecke M., Rehm J. (2012). The cardioprotective association of average alcohol consumption and ischaemic heart disease: A systematic review and meta-analysis. Addiction, 107, 1246-1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadovsky R., Levine L. (2005). Innovative practice men’s healthcare needs improvement: A recommendation for a midlife men’s health assessment visit. Journal of Men’s Health & Gender, 2, 375-381. [Google Scholar]
- Salzman B. E., Wender R. C. (2006). Male sex: A major health disparity. Primary Care, 33, 1-16. [DOI] [PubMed] [Google Scholar]
- Samokhvalov A. V., Irving H., Mohapatra S., Rehm J. (2010). Alcohol consumption, unprovoked seizures, and epilepsy: A systematic review and meta-analysis. Epilepsia, 51, 1177-1184. [DOI] [PubMed] [Google Scholar]
- Samokhvalov A. V., Irving H. M., Rehm J. (2010a). Alcohol consumption as a risk factor for atrial fibrillation: A systematic review and meta-analysis. European Journal of Cardiovascular Prevention & Rehabilitation, 17, 706-712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samokhvalov A. V., Irving H. M., Rehm J. (2010b). Alcohol consumption as a risk factor for pneumonia: A systematic review and meta-analysis. Epidemiology & Infection, 138, 1789-1795. [DOI] [PubMed] [Google Scholar]
- Statistics Canada. (2010). Population projections for Canada, provinces and territories: 2009 to 2036. Retrieved from http://www.statcan.gc.ca/pub/91-520-x/91-520-x2010001-eng.pdf
- Statistics Canada. (2012). Table 102-0512: Life expectancy at birth, by sex, by province. Retrieved from http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/health26-eng.htm
- Statistics Canada. (2013). Canadian Community Health Survey 2011/2012: Public use microdata file (Catalogue No. 82M0013X2013001). Ottawa, Ontario, Canada: Author. [Google Scholar]
- Statistics Canada. (2015). Table 102-0552: Deaths and mortality rate, by selected grouped causes and sex, Canada, provinces and territories: Annual. Retrieved from http://www5.statcan.gc.ca/cansim/a26?lang=eng&id=1020552
- Stockwell T., Greer A., Fillmore K., Chikritzhs T., Zeisser C. (2012). Health benefits of moderate alcohol consumption: How good is the science? British Medical Journal, 344, e2276. [DOI] [PubMed] [Google Scholar]
- Taylor B., Irving H. M., Baliunas D., Roerecke M., Patra J., Mohapatra S., Rehm J. (2009). Alcohol and hypertension: Gender differences in dose-response relationships determined through systematic review and meta-analysis. Addiction, 104, 1981-1990. [DOI] [PubMed] [Google Scholar]
- Taylor B., Irving H. M., Kanteres F., Room R., Borges G., Cherpitel C., Greenfield T., Rehm J. (2010). The more you drink, the harder you fall: A systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug and Alcohol Dependence, 110, 108-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor B., Rehm J., Patra J., Popova S., Baliunas D. (2007). Alcohol-attributable morbidity and resulting health care costs in Canada in 2002: Recommendations for policy and prevention. Journal of Studies on Alcohol and Drugs, 68, 36-47. [DOI] [PubMed] [Google Scholar]
- Tramacere I., Scotti L., Jenab M., Bagnardi V., Bellocco R., Rota M., . . . La Vecchia C. (2010). Alcohol drinking and pancreatic cancer risk: A meta-analysis of the dose-risk relation. International Journal of Cancer, 126, 1474-1486. [DOI] [PubMed] [Google Scholar]