Abstract
A randomized controlled trial was conducted with homeless gay and bisexual men to assess the impact of two culturally sensitive intervention programs on reduction of drug use and risky sexual behavior. In this study, gay and bisexual men between 18 and 46 years of age were randomly assigned to one of two culturally sensitive behavioral intervention programs: a Nurse Case Management Plus Contingency Management (NCM + CM; n = 204) or a Standard Education Plus Contingency Management (SE + CM; n = 210) program. Regardless of group assignment, significant and clinically relevant reductions were observed in stimulant use over time. Multivariable predictors of stimulant use at 4- and 8-month follow-up evaluations were recent injection drug use, tested positive for HIV, or for use of amphetamine. Data revealed a significant linear decline over time for those who had sex with multiple partners. Furthermore, being HIV positive was associated with reporting multiple partners, while higher homophobia scores and having children were inversely related to reports of having sex with multiple partners at follow-up. Culturally sensitive approaches are needed to successfully reduce drug use and risky sexual activities among gay and bisexual populations.
Keywords: gay and bisexual homeless adults, nurse case management, contingency management, drug and sexual risk
Introduction
Gay and bisexual (G/B) men who engage in illicit drug use and unprotected sexual activity are at high risk for contracting human immunodeficiency virus (HIV; Koblin et al., 2007; Kral et al., 2005). In 2010, 63% of new HIV infections were reported among men who have sex with men (MSM; Centers for Disease Control and Prevention, 2013). High frequencies of homelessness over the last month have also been reported among bisexual men (90.7%) and MSM (72.5%; Bowers, Branson, Fletcher, & Reback, 2011). Findings from a national survey of service providers working with young lesbian, G/B, and transgender homeless adults revealed that 46% ran away from home because of family rejection of sexual orientation or identity and 43% were forced out by parents because of sexual orientation or gender identity (Durso & Gates, 2012).
Homelessness appears to be associated with drug use and risky sexual behaviors as well. Having a history of homelessness as well as currently being homeless were both strongly associated with high levels of exposure to both drug use and sexual risk (Clatts, Goldsamt, Yi, & Gwadz, 2005). A number of researchers have also revealed that experiencing homelessness (Elwood, Williams, Bell, & Richard, 1997) being of younger age (Elwood et al., 1997) and engaging in drug and alcohol use (Campsmith, Nakashima, & Jones, 2000) all related to exchanging sex for money, drugs, shelter, or food. While homelessness and lack of accessible drug treatment programs contribute to ongoing drug use in this vulnerable group (Reback et al., 2010), G/B adults in substance abuse treatment are less likely to complete treatment as compared with heterosexual counterparts (Senreich, 2009).
One strategy identified to be effective in reducing drug use among G/B and MSM includes contingency management (CM; Menza et al., 2010; Reback et al., 2010; Shoptaw et al., 2005; Shoptaw et al., 2008). One aspect of CM which incorporates and promotes positive reinforcement in the form of vouchers, goods, or services (Secades-Villa et al., 2013) was identified to be more effective in reducing methamphetamine use and unprotected receptive anal intercourse among G/B men in comparison with cognitive behavioral therapy (Shoptaw et al., 2005). After a 24-week program with homeless MSM, Reback et al. (2010) revealed that participants in CM were significantly more likely to be free of stimulant use in comparison with the control group.
Nurse case management (NCM)–delivered sessions, tailored to the needs of the client population, incorporate protective strategies, ways to improve coping, and provide linkage with community resources. Nyamathi and colleagues have successfully used nurse-delivered strategies to screen for HBV and HCV infections, reduce drug and alcohol use (Nyamathi et al., 2013; Nyamathi, Dixon, Wiley, Christiani, & Lowe, 2006) and increase the hepatitis vaccination completion rates and knowledge levels among homeless drug-using populations (Nyamathi et al., 2008; Nyamathi et al., 2009; Schumann, Nyamathi, & Stein, 2007).
While tailored interventions have been reported to be effective in reducing drug use and unprotected sex within the G/B community with CM (Reback et al., 2010; Shoptaw et al., 2005) or with nurse-led health-promoting behaviors (Nyamathi, Christiani, Nahid, Gregerson, & Leake, 2006; Nyamathi et al., 2008; Nyamathi et al., 2009; Nyamathi, Stein, Schumann, & Tyler, 2007; Schumann et al., 2007), these approaches have not been assessed for effectiveness when combined in targeting the dual risk of drug use and unprotected sexual behavior among stimulant-using homeless G/B men. The purpose of the current study was to assess the effectiveness of two approaches, the Nurse Case Management Plus Contingency Management (NCM + CM) versus the Standard Education Plus Contingency Management (SE + CM) programs in reducing drug use and unprotected risky sexual behavior among this vulnerable population at 4- and 8-month evaluation postintervention.
Method
Participants and Setting
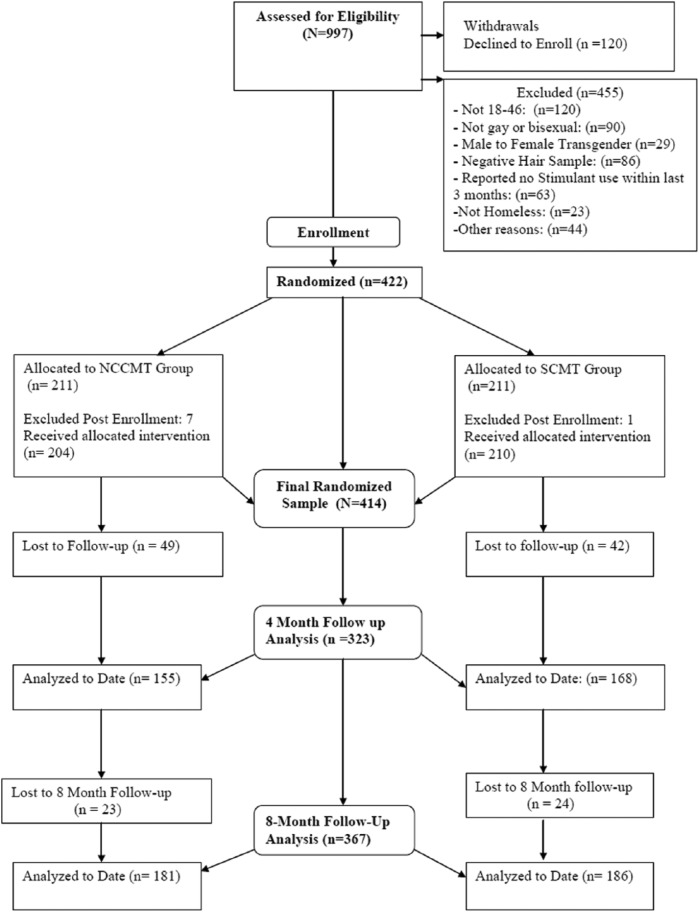
The inclusion criteria included (a) age 18 to 46 years, (b) self-reported being homeless, (c) G/B, (d) stimulant user within the past 3 months, and (e) no self-reported participation in substance abuse treatment in the past 30 days. In total, 451 stimulant-using (methamphetamine, amphetamine, and cocaine) participants were enrolled in the study. Among those enrolled, 29 identified as transgender women (male to female). Given the very distinct needs of this population, this small subgroup of participants was eliminated from this analysis. In addition, a total of eight participants were removed from the study post enrollment for providing incorrect information regarding their eligibility or tampering with urine specimens. Thus, the total sample was 414, for which 204 were enrolled in the NCM + CM group and 210 were enrolled in the SE + SM group. Follow-up rate at 4 months was 78% while the rate was 89% at 8-month follow-up. The 4-month follow-up period was limited to a 2-month period, while the 8-month follow-up was conducted over several months to find participants who were difficult to locate. Consort diagram is presented in Figure 1. Both the University of California, Los Angeles, and the Friends Research Institute Human Subjects Protection Committees approved the study.
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) diagram.
Data were collected in a community research site in Hollywood, California. This site is in the G/B sex-work district on the border of Hollywood and West Hollywood and offers substance-abuse prevention services for treatment seeking and out-of-treatment substance users.
Recruitment and Study Procedure
A convenience sample of participants was recruited by research staff who distributed flyers in Hollywood area community sites frequented by G/B homeless men. Once the study was described and questions answered in a private location, interested participants completed an informed consent for a 2-minute screening that assessed eligibility, and subsequently the baseline questionnaire. The screening assessed demographic characteristics, homeless status, and substance abuse or dependence using the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR). Stimulant use in the prior 3 months was verified by either urinalysis screening or by hair analysis if the urine screening could not detect a stimulant metabolite. Participants received $10 to complete the screening questionnaire, $20 to complete the baseline questionnaire, and $30 and $35 to complete the 4- and 8-month evaluations. There were no statistically significant differences between groups in numbers of participants who were followed over time.
Theoretical Foundation for Program Selection
The Comprehensive Health Seeking and Coping Paradigm (Nyamathi, 1989) served as the foundation for the programs selected. The Comprehensive Health Seeking and Coping Paradigm framework delineates a number of factors that are relevant to promote a positive health outcome among homeless G/B men. This includes situational and cognitive factors as well as social factors and coping strategies. Situational factors relate to the living situation of the participants, their history of drug and alcohol use, and risk for chronic illnesses. The intervention program (NCM + CM Program) was designed in a culturally sensitive manner to promote the health of the participants through needs assessment and referral by the nurses, both in terms of health issues and housing needs. Cognitive factors related to the critical knowledge transfer needed for the G/B men in terms of understanding the impact of risky behavior on the potential for HIV and hepatitis. The information delivery was made culturally sensitive by engaging peers as research staff who worked for years with the targeted community, and promoted risk reduction strategies designed for the population at risk. Furthermore, promoting social networking and positive coping strategies were also integrated in the intervention program as the peers met with the participants in group settings where the importance of networking and positive coping strategies were considered.
CM was selected as a component of both programs as it has been demonstrated to be effective in reducing methamphetamine use and unprotected sex among G/B men (Shoptaw et al., 2005). In fact, Reback et al. (2010) reported that substance-dependent homeless MSM who were provided a CM program provided significant more urine samples that were free of stimulant metabolites than the control group.
Nurse Case Management Plus Contingency Management Program
Participants were randomized into the NCM + CM or the SE + CM programs. Both programs were designed in culturally relevant approaches by engaging G/B community site attendees in the construction of the approved flyers for advertising the study, integrating community members in the design and implementation of the programs as peers employed and trained to deliver the content, and conducting the study in the community sites attended by G/B clientele. Integrating peers into the programs was a critical strategy to ensure cultural sensitivity.
Participants selected for the NCM + CM program were offered a total of eight 20-minute NCM and eight hepatitis health education sessions over the 16-week program. As the outcomes of the study related to reduction of drug use and risky sexual behaviors, the NCM sessions were delivered one-on-one and focused on the relationship between drug use and risky sexual behaviors and HIV, hepatitis B virus (HBV), hepatitis C virus (HCV), and other negative sequelae. Facts about transmission, signs, and symptoms of the disease and treatment for these diseases were also covered. Moreover, training in behavioral, self-management, and communications skills necessary for overcoming barriers to implementing behavior change were covered as well as strategies in enhancing the development of relationships and social networks conducive to achieving and maintaining reductions in risk behavior. Finally, the importance of completing the hepatitis A/B virus (HAV/HBV) vaccine was encouraged, as well as the importance of positive support and personal empowerment.
The sessions delivered by G/B community peers were about 20 to 30 minutes in length, conducted in either a group (4-5 per group) or individual format, and promoted strategies to reduce risk of hepatitis and HIV. Similarly, consistent with the outcome variables, and the culturally sensitive design of the program, a focus was placed on dangers of drug use and unprotected sexual activities on risk of HIV and hepatitis and ways to keep safe through negotiation with sexual partners. Nearly two thirds of the NCM + CM participants (total sample, n = 139; 63%) completed all eight NCM sessions while 65% (n = 144) completed all eight peer coaching sessions. All NCM + CM participants received CM described below.
Standard Education Plus Contingency Management Program
The brief SE component was delivered once over a 20-minute session by the health educator and focused on the importance of condom use and other means of protection against HIV, HBV, and HCV, including the importance of completing the HAV/HBV vaccination. Almost the entire sample of SE + CM participants (99%) completed the 20-minute education session.
Contingency Management Program
The same CM reinforcement and payout schedule was provided to participants in both programs. A progressive contingency schedule (Higgins et al., 1994) was provided wherein participants received a $2.50 voucher for the first urine sample that was negative for stimulant metabolites, with an incremental increase of $1.25 for each subsequent negative urine sample for stimulant metabolites. Thrice-a-week urine samples were required each week for the 16 weeks on Tuesdays, Thursdays, and Saturdays. Stimulant-free urines added voucher points that could be redeemed for merchandise selected by the participant. However, when positive tests for a stimulant metabolite was revealed, or for participants who did not submit a urine sample, voucher points were not accumulated and their subsequent voucher value was reduced to the initial $2.50. A rapid reset procedure enabled participants to return to their prepositive test result after three clean urine test results. The maximum value that participants could earn for all urines that tested negative was $444.
Measures
Sociodemographic Information
At baseline, a structured questionnaire was used to evaluate data on the following parameters: age, education, race/ethnicity, self-identification as G/B men, time period of homelessness, employment status, number of times incarcerated within 4 months and insurance status.
Health Status
A self-reported one-item measuring general health ranged from “excellent” to “poor.” Responses were dichotomized as “excellent” versus “very good” versus “poor” (Stewart, Hays, & Ware, 1988).
Visits to a Private Medical Doctor
Participants were asked whether they have visited a private medical doctor for their emotional health within the past 4 months.
HBV, HCV, and HIV Seropositivity
HBV and HCV status were evaluated using commercially available enzyme immunoassay kits to measure hepatitis B surface antibody and hepatitis C antibody, respectively. HIV status was assessed by a rapid HIV test, OraQuick ADVANCE Rapid HIV-1/2 Antibody test by OraSure, based in Bethlehem, Pennsylvania.
Social Support
Participant’s supporters were categorized as either users of drugs, nonusers, or both users and nonusers.
Depressive Symptomatology
A 10-item short form version of the Center for Epidemiologic Studies–Depression Scale (CES-D; Radloff, 1977) was used to assess depressive symptoms based on a 4-point continuum. Scores on this CES-D ranged from 0 to 30, with higher scores indicating greater depressive symptomatology. Cronbach’s alpha for CES-D scale was .82 in this homeless population.
Substance Use
The participants self-reported substance use over the past 30 days by means of the Addiction Severity Index (McLellan et al., 1992).
Injection Drugs
Use was assessed by asking participants whether they had ever injected any illegal drugs during the past month, 4 months, and lifetime. Injection drug use was one item used by the Behavioral Questionnaire–Amphetamine (Reback, Kamien, & Amass, 2007; Twitchell, Huber, Reback, & Shoptaw, 2002). This measure has been commonly used in addiction research.
Internalized Homophobia
A five-item assessment measured feelings about a man having sex with a man. Answers were scored on a 5-point Likert-type scale which ranged from disagree strongly (1) to agree strongly (5). The questions were summarized to yield a scale score of 1 to 25, with higher scores indicating a higher degree of internalized homophobia and lower scores indicating greater acceptance of being a G/B man. A summary score of more than 15 was considered to have a high level of internalized homophobia, which indicated that on an average, the participant had “agreed” or “agreed strongly” with the five internalized homophobia questions.
Drug Dependence
Status was determined by totaling the number of positive criteria from the DSM-IV-TR criteria for Dependence checklist (American Psychiatric Association, 2000). Scores higher than 3 indicated drug dependence.
Hepatitis B Knowledge and Attitudes
A modified 17-item instrument (Nyamathi et al., 2010) measured items on a 5-point scale ranging from definitely true (1) to don’t know (5). Cronbach’s reliability coefficient for the instrument was .88 in this population. With the range of 0 to 17, a person who answered at least 14 items correctly (the upper quartile score) was considered as having a high score of HBV knowledge.
HIV/AIDS Knowledge
A modified 21-item Centers for Disease Control and Prevention Scale measured knowledge and attitudes toward HIV/AIDS (National Center for Health Statistics, 1989). Range was 0 to 21. The Centers for Disease Control and Prevention instrument modifications have been described in other work (Leake, Nyamathi, & Gelberg, 1997). Cronbach’s alpha for the overall HIV knowledge and attitude scale was .86 in this homeless population. A person who answered at least 19 items correctly (the upper quartile score) was considered to have a high score of HIV/AIDS knowledge.
Multiple Partners
Status was determined by asking in the past 30 days, how many different men in total have you had sex with, including your primary male partner if you have a primary male partner. Responses were coded as 0 (0-1 partner) or 1 (2 or more partners).
Urinalysis Drug Testing Results
Participants were asked to provide urine specimens three times a week for the first 4 months, and then again at the time of the 4- and 8-month follow-up. The Phamatech QuickScreen™ test kit (San Diego, CA), a rapid, self-timed, qualitative immunoassay, was used to evaluate the urine samples for stimulant use. The cutoff concentrations for this five-panel Food and Drug Administration–approved urine test cup are as follows: methamphetamines 500 ng/mL, amphetamine 1,000 ng/mL, cocaine 300 ng/ml, opiates (2,000 ng/mL), and tetrahydrocannabinol (THC; 50 ng/mL). In this study, urine test results for the first 2 weeks of the intervention (six urine tests) were compiled to assign stimulant use status for the participant. If any of the first 6 tests were positive, the participants were scored as stimulant use positive = 1 for use of each stimulant. However, the participants were determined as stimulant use negative = 0, if they had at least 1 negative and no positive tests among the first 6 tests.
Data Analysis
Baseline balance between the two groups on sociodemographic characteristics and urinalysis test results was assessed using chi-square tests (categorical variables) and t and Wilcoxon two-sample tests (continuous variables). The authors also tested whether baseline variables that differed between the two groups were related to the two key outcomes of follow-up stimulant use and multiple partners. Logistic regression analysis was used to determine whether dropout differed between groups, controlling for potential confounders. Since no hint of a group difference in dropout was reported (p > .10), intention-to-treat analysis based on multiple imputed data was not performed.
Group differences in outcomes over time were assessed using repeated measures log-linear models for the dichotomous outcomes and multilevel linear regression models for the knowledge measures. Because results identified no significant group differences, contrasts were evaluated within each group for change over time.
For examining factors associated with stimulant outcomes, the authors used multiple logistic regression modeling for any positive urine test for a stimulant (methamphetamine, amphetamine, or cocaine) at either 4- or 8-month follow-up. The two follow-up periods were combined for the stimulant use outcome because the authors were concerned about any use of stimulants in a fairly short period of time and assessment of outcomes over time identified little change between 4- and 8-month follow-up. For multiple partners, multilevel logistic regression modeling for reporting multiple partners over the study period was used to identify factors associated with these outcomes. Group assignment was included in the models for both outcomes as a control variable. Other predictors in the models were selected if they were related to the outcomes at p < .15 in preliminary analyses. Multicollinearity was assessed and reported not to be a problem. Analysis was performed using SAS 9.3.
Parameter estimates are depicted in Tables 3 and 4 as the authors were primarily interested in detecting whether effects were significant, rather than amount of change in odds per unit change in independent variable, or amount of change in the logit of the dependent variable for unit change in independent variable. The parameter estimates give equivalent information as do odds ratios, but indicate the amount of change in the logit of the dependent variable for a unit change in independent variable. Furthermore, as SAS does not automatically give odds ratios in GEE or multilevel logistic models reporting multiple logistic regression and multilevel log regression in coefficients is generally done. Missing data were handled by imputation.
Table 3.
Multiple Logistic Regression Results for Any Stimulant Use at Follow-up (n = 273).
| Estimate | Standard error | p | |
|---|---|---|---|
| Intervention group | −0.409 | 0.27 | .126 |
| Age | 0.030 | 0.02 | .067 |
| Other race/ethnicitya | −1.360 | 0.66 | .039 |
| Birth countryb | −1.252 | 0.71 | .079 |
| Excellent healthc | 1.445 | 0.87 | .098 |
| HIV positived | 0.908 | 0.38 | .017 |
| Saw MD/RN for emotional problems, past 4 months | −0.899 | 0.34 | .008 |
| Injected drugs, past month | 0.932 | 0.30 | .002 |
| Amphetamine positivee | 0.694 | 0.27 | .011 |
Note. MD = medical doctor; RN = registered nurse.
Versus African American, White, Latino, and Mixed. bBorn in a country other than the United States and Mexico. cVersus very good, good, fair, and poor. dRapid HIV test at baseline. eUrine analysis at baseline.
Table 4.
Multilevel Logistic Regression Results for Multiple Partners (n = 359).
| Estimate | Standard error | p | |
|---|---|---|---|
| Group | −0.030 | 0.24 | .898 |
| Time | −0.580 | 0.14 | <.001 |
| Group × Time | −0.127 | 0.20 | .520 |
| Children | −0.468 | 0.21 | .028 |
| HIV positive | 0.601 | 0.25 | .016 |
| Internalized homophobia | −0.331 | 0.10 | .001 |
| Opiatesa | −0.807 | 0.43 | .062 |
Baseline urine sample tested positive for opiates.
In terms of power, the analysis sample was sufficient to detect small-to-medium effects with power = .80 and two-tailed α = .05 across primary analyses. For simple differences in proportions (e.g., positive stimulant urine test at a specific follow-up time point, the sample size would allow detection of a small-to-medium difference of approximately 16% between intervention groups; Cohen, 1988; Faul, Erdfelder, Lang, & Buchner, 2007). For examining differences between groups in change over time in risk behaviors, a small effect (approximately d = .28) was detectable, assuming a moderate correlation of .3 over time and adjusting for attrition (Hedeker, Gibbons, & Waternaux, 1999); a small within-group change (f = .11) was detectable. Small effects were detectable for assessing a specific predictor of multiple partners at follow-up using logistic regression, assuming that other predictors accounted for a moderate proportion of variance in outcome (about 0.30); small-to-medium effects were detectable for assessing predictors of stimulant use at follow-up.
Results
Sociodemographic Characteristics
As presented in Table 1, the sample was predominantly African American/Black and Caucasian/White, with fewer Hispanic/Latino participants and persons of other race/ethnicities. About one third reported having children. Almost two thirds (61%) had spent at least a week in the prior month living on the street. In terms of self-reported health, nearly three quarters reported good to excellent health, while 26% reported their health to be fair or poor. Just less than half (49.3%) were HBV antibody positive while 15% were HCV antibody positive.
Table 1.
Sample Characteristics by Program.
| NCMa + CMb (n = 211) |
SE + CMb (n = 211) |
Total (n = 422) |
||||
|---|---|---|---|---|---|---|
| Baseline measure | n | % | n | % | % | p c |
| Race/ethnicity | .66 | |||||
| African American | 73 | 34.60 | 77 | 36.49 | 35.55 | |
| White | 75 | 35.55 | 79 | 37.44 | 36.49 | |
| Hispanic | 30 | 14.00 | 32 | 15.17 | 14.69 | |
| Mixed | 20 | 9.48 | 12 | 5.69 | 7.58 | |
| Other | 13 | 6.16 | 11 | 5.21 | 5.69 | |
| Children | .868 | |||||
| Yes | 69 | 32.1 | 68 | 32.9 | 32.5 | |
| Homeless status | ||||||
| On street ≥1 weekd | 138 | 65.40 | 121 | 57.35 | 61.37 | .09 |
| In shelter ≥1 weekd | 24 | 11.37 | 35 | 16.59 | 13.98 | .12 |
| Health | .17 | |||||
| Excellent/very good/good | 150 | 71.42 | 163 | 77.25 | 74.34 | |
| Fair/poor | 60 | 28.57 | 48 | 22.75 | 25.66 | |
| Receiving health care | 59 | 28.10 | 43 | 20.38 | 24.23 | .07 |
| Discuss mental health with doctor | 49 | 22.8 | 37 | 17.9 | 20.4 | .279 |
| Positive for HBV | 108 | 51.18 | 100 | 47.39 | 49.29 | .44 |
| Positive for HCV | 63 | 29.86 | 66 | 31.28 | 30.57 | .75 |
| Positive for HIV | 32 | 15.38 | 29 | 14.15 | 14.77 | .77 |
| Positive urinalysise | ||||||
| Methamphetamine | 161 | 76.3 | 147 | 69.7 | 73.0 | .125 |
| Amphetamine | 105 | 49.8 | 99 | 46.9 | 48.3 | .559 |
| Cocaine | 67 | 31.8 | 76 | 36.0 | 33.9 | .355 |
| Opiates | 10 | 4.7 | 20 | 9.5 | 7.1 | .058 |
| Marijuana | 123 | 58.3 | 103 | 48.8 | 53.6 | .225 |
| Ever injected drugs | .68 | |||||
| Yes, past 30 days | 70 | 33.18 | 74 | 35.07 | 34.14 | |
| Social supportf | .51 | |||||
| Primarily users | 48 | 22.75 | 40 | 18.96 | 20.85 | |
| Primarily nonusers | 50 | 23.70 | 59 | 27.96 | 25.83 | |
| Both | 97 | 45.97 | 91 | 43.13 | 45.55 | |
| None | 16 | 7.58 | 21 | 9.95 | 8.72 | |
| Multiple partners | 76 | 36.0 | 78 | 37.0 | 36.5 | .923 |
| NCMa + CMb (n = 211) |
SE + CMb (n = 211) |
Total (n = 422) |
||||
| Baseline measure | Mean | SD | Mean | SD | Overall mean/SD (range) | P c |
| Age | 34.19 | 8.0 | 34.63 | 8.2 | 34.42/8.1 (18-46) | .58 |
| Education | 11.87 | 2.3 | 12.16 | 2.2 | 12.01/2.25 (2-21) | .19 |
| Depressive symptomsg | 12.41 | 6.5 | 13.33 | 6.6 | 12.87/6.50 (0-30) | .15 |
| Internalized homophobia (n = 418) | 12.69 | 4.932 | 12.62 | 4.99 | 12.66/4.955 (5-25) | .895 |
| HIV overall knowledge (n = 422) | 7.28 | 1.658 | 7.26 | 1.75 | 7.27/1.70 (1-10) | .887 |
| HIV cognitive knowledge (n = 420) | 5.23 | 1.607 | 5.19 | 1.70 | 5.21/1.65 (0-7) | .804 |
| HIV transmission knowledge (n = 420) | 1.84 | .457 | 1.85 | .430 | 1.85/0.44 (0-2) | .852 |
| HBV overall knowledge (n = 422) | 5.59 | 2.476 | 5.63 | 2.499 | 5.61/2.48 (0-9) | .891 |
| HBV cognitive knowledge (n = 376) | 3.84 | 1.969 | 4.11 | 1.810 | 3.97/1.90 (0-7) | .169 |
| HBV transmission knowledge (n = 378) | 1.76 | .520 | 1.71 | .551 | 1.73/0.54 (0-2) | .388 |
NCM + CM = Nurse Case Management + Contingency Management. bSE + CM = Standard Education + Case Management. cTwo-sample t or Wilcoxon test. dThe month before baseline. ePositive test for any stimulant drug (cocaine, methamphetamine, or amphetamine). fPrimary source of social support. gBased on the 10-item Center for Epidemiologic Studies–Depression Scale Questionnaire.
Methamphetamine was the most frequently used drug (73%) followed by marijuana (54%). Injection drug use in the past month was reported by about one third (34%). Almost half of the participants (45.4%) reported receiving social support by both drug users and nondrug users. The mean age of the sample was 34 years (SD]= 8.1) and the mean years of educational attainment was 12 years. No group differences were identified on sociodemographic variables.
Outcome Profiles Over Time as a Function of Group
Changes in the outcomes as measured by the number and percentages of positive urine drug screens at each point in the study are reported in Table 2. Results identified no significant group or group-by-time effects; thus, discussion and further analyses is focused on changes within each group. Reductions in positive drug tests and in reports of multiple partners were seen in both groups over time, along with increases in HIV/AIDS and HBV overall knowledge and in the subscales of cognitive knowledge and knowledge about transmission. Pairwise comparisons and contrasts (results not reported in Table 2) indicated that improvement in outcomes occurred primarily between baseline and 4-month follow-up; changes in outcomes between 4 and 8 months were not significant for all drugs except opiates, as well as for multiple partners and HIV/AIDS knowledge. The exception was positive urine tests for opiates, which changed significantly for the SE + CM from 4- to 8-month follow-up.
Table 2.
Program Comparisons for Drug Metabolite Positive Urine Samples, Multiple Sexual Partners, and Knowledge by Condition at Baseline, 4 and 8 Months.a
| Baseline | 4 months | 8 months | |||||
|---|---|---|---|---|---|---|---|
| Urine testing profile | n | % | n | % | n | % | p b |
| Marijuana | |||||||
| NCM + CM (n = 124) | 75 | 60.48 | 60 | 48.39 | 62 | 50.00 | .048 |
| SE + CM (n = 141) | 60 | 46.15 | 52 | 40.00 | 51 | 39.23 | .358 |
| Cocaine | |||||||
| NCM + CM (n = 124) | 40 | 32.26 | 7 | 5.65 | 14 | 11.29 | .001 |
| SE + CM (n = 130) | 44 | 33.85 | 10 | 7.69 | 9 | 6.92 | .001 |
| Methamphetamine | |||||||
| NCM + CM (n = 124) | 90 | 72.58 | 21 | 16.94 | 29 | 23.39 | .001 |
| SE + CM (n = 130) | 92 | 70.77 | 36 | 27.69 | 37 | 28.46 | .001 |
| Amphetamine | |||||||
| NCM + CM (n = 124) | 61 | 49.19 | 20 | 16.13 | 25 | 20.16 | .001 |
| SE + CM (n = 130) | 63 | 48.46 | 28 | 21.54 | 32 | 24.62 | .001 |
| Opiates | |||||||
| NCM + CM (n = 124) | 6 | 4.84 | 7 | 5.65 | 9 | 7.26 | .660 |
| SE + CM (n = 141) | 10 | 7.69 | 12 | 9.23 | 6 | 4.62 | .018 |
| Sexual activity profile | |||||||
| Multiple partners | |||||||
| NCM + CM (n = 148) | 55 | 37.16 | 30 | 20.27 | 22 | 14.86 | .001 |
| SE + CM (n = 163) | 57 | 34.97 | 28 | 17.18 | 30 | 18.40 | .001 |
| HIV/AIDS knowledge profilec | Mean | Mean | Mean | p b | |||
| Total knowledge (mean) | |||||||
| NCM + CM (n = 152) | 7.32 | 16.97 | 16.70 | .001 | |||
| SE + CM (n = 162) | 7.30 | 17.25 | 16.98 | .001 | |||
| Baseline mean | 4-month mean | 8-month mean | p b | ||||
| Cognitive knowledge | |||||||
| NCM+CM (n = 150) | 5.27 | 7.69 | 7.50 | .001 | |||
| SE+CM (n = 162) | 5.25 | 7.78 | 7.73 | .001 | |||
| Transmission knowledge | |||||||
| NCM + CM (n = 152) | 1.85 | 9.28 | 9.20 | .001 | |||
| SE + CM (n = 162) | 1.86 | 9.46 | 9.25 | .001 | |||
| HBV knowledge profile (mean) | |||||||
| NCM + CM (n = 152) | 5.58 | 10.40 | 10.19 | <.001 | |||
| SE + CM (n = 161) | 5.57 | 10.23 | 9.30 | <.001 | |||
| Cognitive knowledge profile (mean) | |||||||
| NCM + CM (n = 140) | 3.85 | 4.79 | 4.51 | .004 | |||
| SE + CM (n = 137) | 4.11 | 4.59 | 4.47 | .472 | |||
| Transmission (mean) | |||||||
| NCM + CM (n = 137) | 1.74 | 6.09 | 5.77 | <.001 | |||
| SE + CM (n = 145) | 1.74 | 5.74 | 5.14 | <.001 | |||
For participants with nonmissing outcome values at each time period. bFor change over time based on log-linear modeling chi-square test and on multilevel linear regression (for knowledge). cA person who answered at least 19 items correctly (the upper quartile score) was considered to have a high score of HIV/AIDS knowledge.
Multiple Logistic Regression Results for Any Stimulant Use at Follow-up
Use of stimulants at follow-up was coded as “yes” if there was a positive urine test for cocaine, methamphetamine, or amphetamines at either 4- or 8-month; it was coded as “no” if all tests were negative at both follow-up points (Table 3). Multiple logistic regression analysis for stimulant use at follow-up identified that recent injection drug use was the strongest baseline predictor; furthermore, being HIV antibody positive and testing positive for amphetamines at baseline also predicted follow-up stimulant use at 4- or 8-month follow-up. Having recently seen a health provider for emotional problems had a strong protective effect and “other” race/ethnicity was also inversely related to follow-up use of stimulants.
Multilevel Logistic Regression Results for Multiple Partners
Results of a multilevel logistic regression analysis for reporting multiple sexual partners at baseline, 4- and 8-month follow-up, controlling for group assignment are reported in Table 4. As reported, there was a significant linear decline in reporting multiple partners over time. Being HIV antibody positive was a strong predictor of reporting multiple partners, while higher baseline internalized homophobia scores and having children were inversely related to reports of multiple partners. When an interaction between group and time was added to the model, it was not significant, confirming that participants in the two groups had similar rates of decline in multiple partners.
Discussion
This randomized controlled trial evaluated two culturally sensitive, community-tailored behavioral intervention programs, the NCM + CM and the SE + CM programs on reducing drug use and risky behaviors among homeless, stimulant-using G/B men at 4- and 8-month follow-up evaluation. No significant group differences were reported between the NCM + CM and SE + CM. As a result, within-group differences were more heavily focused on.
Overall, significant reductions were observed in use of amphetamine, marijuana, cocaine, or methamphetamine use over time, regardless of group designation, suggesting the importance of encouraging at-risk populations to engage in the culturally sensitive behavioral intervention program as implemented in this study. Utilization of NCM in previous studies has been reported to improve outcomes on drug and/or sexual risk (Nyamathi, Flaskerud, Leake, Dixon, & Lu, 2001), as well as enhanced vaccine completion (Nyamathi et al., 2009; Nyamathi et al., 2009) among homeless and drug-using populations.
The fact that participants in both programs were successful in reducing the use of these drugs speaks also to the power of CM as has been reported in prior studies with MSM and G/B men. For example, previous studies have also reported that CM has decreased methamphetamine use among MSM (Shoptaw et al., 2006). A significant decrease was reported for opiate use for only the SE + CM from 4- to 8-month follow-up. This finding warrants further exploration to determine the nature of the impact and best strategies for sustainability.
While the NCM program was not reported to significantly improve outcomes, it is plausible that the CM component is adequate enough to promote a decrease in drug use and sexual risk alone and without an added benefit of NCM. However, as NCM-CM was generally health-related, it is possible that the additive benefit of the NCM program may well show strength in health-related outcomes if selected. Thus, the authors feel that the attention of NCM is critical among a population which is hard-to-reach and has a lack of access to health care. It is also important to note that while there was a significantly greater decrease in positive urines for opiate use for the SE + CM group as compared with the NCM-CM group, there were a low number of positive samples from baseline to 8 months.
Of particular note is the utility of methods which enabled the design of culturally sensitive programs. These include working within a community site which welcomed substance-using G/B men and transgender women, and developing and integrating intervention and control components with particular attention to the G/B homeless population. Furthermore, research staff were experienced in working with G/B men from the same community and were trained to administer the program.
Recent injection drug use was the strongest baseline predictor for follow-up stimulant use; furthermore, those who tested HIV antibody positive or positive for amphetamines at baseline also predicted ongoing stimulant use postintervention at either 4- or 8-month follow-up. This finding indicates that those who are amphetamine positive may need to be triaged related to drug use dependency and referred to inpatient treatment.
Inverse associations were identified with those who were able to see a health care provider and reported being of a race/ethnicity other than African American/Black, Latino or Caucasian/White. With respect to multiple sexual partners at 4- and 8-month follow-up, data likewise reveal there was a significant linear decline over time. The reduction of multiple sexual partners over time is a positive finding and targets the utility of a community-based, culturally sensitive targeted intervention. Being HIV positive was associated with reporting multiple partners. Unprotected sex with multiple partners increases the likelihood for HIV transmission (Kral et al., 2005).
Another finding was a negative association between internalized homophobia scores and multiple partners at follow-up which was contrary to findings of a relationship between increased sexual compulsivity and internalized homophobia (Dew & Chaney, 2005). Furthermore, having children was inversely related to ongoing reports of having sex with multiple sexual partners at follow-up which may indicate a protective effect of having children.
The current findings revealed that participants who injected drugs in the last month at baseline were more likely to test positive for stimulants at 4- or 8-month follow-up. Using needles to inject drugs often point to more severe form of drug use and dependence (Halkitis, Shrem, & Martin, 2005). Future research should identify those who are injection drug users and their need for additional supportive care.
The current data also identify that those who tested positive for amphetamine use at baseline were also more likely to test positive for stimulants at 4- or 8-month follow-up. It is important to note that those who tested positive for amphetamines at baseline or follow-up may be methamphetamine users as methamphetamine is metabolized to amphetamine in the body. Future study may consider the value for measuring use of amphetamine itself to differentiate from use of methamphetamine during a treatment intervention. Thus, the type of drug and method of administration by study participants may require different intervention strategies, such as inpatient drug treatment. It is also important to work with methamphetamine users to address safer types of sex and risk of ongoing drug use. In one study, 68.8% of G/B methamphetamine users in a large, urban city used methamphetamine to enhance sexual experiences as it prolonged sexual encounters, heightened sexual feelings, reduced anxiety, and increased openness about sex (Halkitis, Fischgrund, & Parsons, 2005).
These findings demonstrated that those who were HIV antibody positive were more likely to use stimulants at follow-up and to report having sex with multiple partners. This is an important finding as it may signify that those infected may have been those using stimulants for a longer time compared with those not HIV-infected. Reduction in substance use was also reported by other behavioral interventions conducted among people living with HIV/AIDS (Wong et al., 2008). However, it is especially critical to decrease stimulant use among this population as stimulant users may be the most challenged to take their HIV medication when high on stimulants (Royal et al., 2009).
In terms of sexual risk behavior, among one sample of HIV-positive MSM, those who used drugs before or during sex were more likely to engage in unprotected receptive anal intercourse with casual partners than those who used no drugs or used less drugs (Purcell, Parsons, Halkitis, Mizuno, & Woods, 2001). Given these findings, it is important that specific programs designed for stimulant-using G/B homeless men who are HIV antibody positive be developed which include stable housing, and substance use counselling and treatment in order to decrease stimulants use, along with access to antiretroviral medication. Equally important, those who were in the “other” race/ethnicity categories were less likely to use stimulants at follow-up. This finding is not easily justified and current literature relating to homeless G/B homeless populations currently do not provide any clues.
Interestingly, a protective effect was reported for those who had seen a medical provider for an emotional problem in the past 4 months, as these individuals were less likely to use stimulants at follow-up. Taking the step to see a medical provider is an important variable. When health care access is desired and attained, improvements can be seen in terms of stimulant use reduction and suggests involvement in a change process.
In addition, higher internalized homophobia scores were inversely related to self-report of engaging in sex with multiple partners. This finding is novel as some researchers note that internalized homophobia increases HIV/sexually transmitted infections risk behavior as feelings of decreased self-worth are generally prominent (Ross, Kajubi, Mandel, McFarland, & Raymond, 2013). Furthermore, personal discomfort and higher social discomfort with homosexuality were significantly associated with unprotected receptive anal intercourse in the past 6 months (Ross et al., 2013).
In this investigation, there are strengths which include the longitudinal design and the high rate of 4-month (78%) and 8-month follow-up data (89%), especially when working with a transient and hard-to-reach population. Despite the strengths, a number of limitations should be discussed. For instance, the current findings are based on a convenience sample from one large urban city which can limit generalizability for the study findings. Self-report for multiple partners are also prone to misclassification and may be biased as participants may self-report more or less total number of partners. Furthermore, even though PH monitors and vigilant research staff monitored accuracy of urine testing, research participants are savvy to know the limitations of urine testing to pick up drug use and may have altered their drug use behavior around the testing timelines. Finally, despite the significant training that the staff received, self-report for reporting multiple partners may also be underreported if participants felt that the interview staff were judging their behavior.
These findings emphasize the need to develop culturally sensitive and tailored programs which meet the specific needs of G/B, and substance use counseling and treatment programs should link their clients into such programs. Furthermore, it is critical that those who are unstably housed, HIV positive, and/or use injection drugs, are provided an additional set of resources as the degree of vulnerability to adverse events exponentially increases.
Conclusions
These findings highlight the success of integrating research strategies that engage the community in providing culturally sensitive intervention to reduce drug use and sexual risk behavior among a high-risk subgroup of homeless and drug-using G/B men. Findings also revealed the need for a multipronged approach which integrates strategies, such as CM, which draw and hold the target population in culturally sensitive programs, and deliver information and resources needed to improve overall health status, and bolster support networks.
Footnotes
Authors’ Note: This study is registered with the Clinical Trials Network NCT00926146.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the National Institute on Drug Abuse, Grant No. DA016147.
References
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- Bowers J. R., Branson C. M., Fletcher J., Reback C. J. (2011). Differences in substance use and sexual partnering between men who have sex with men, men who have sex with men and women and transgender women. Culture, Health & Sexuality, 13, 629-642. doi: 10.1080/13691058.2011.564301 [DOI] [PubMed] [Google Scholar]
- Campsmith M. L., Nakashima A. K., Jones J. L. (2000). Association between crack cocaine use and high-risk sexual behaviors after HIV diagnosis. Journal of Acquired Immune Deficiency Syndrome, 25, 192-198. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2013). HIV among gay, bisexual and other men who have sex with men. Atlanta, GA: Author; Retrieved from http://www.cdc.gov/hiv/pdf/risk_HIV_among_AA_Gay_other.pdf [Google Scholar]
- Clatts M. C., Goldsamt L., Yi H., Gwadz M. V. (2005). Homelessness and drug abuse among young men who have sex with men in New York City: A preliminary epidemiological trajectory. Journal of Adolescence, 28, 201-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum. [Google Scholar]
- Dew B. J., Chaney M. P. (2005). The relationship among sexual compulsivity, internalized homophobia, and HIV at-risk sexual behavior in gay and bisexual male users of internet chat rooms. Sexual Addiction & Compulsivity, 12, 259-273. doi: 10.1080/10720160500362306 [DOI] [Google Scholar]
- Durso L. E., Gates G. J. (2012). Serving our youth findings from a national survey of services providers working with lesbian, gay, bisexual and transgender youth who are homeless or at risk of becoming homeless. Retrieved from http://williamsinstitute.law.ucla.edu/wp-content/uploads/Durso-Gates-LGBT-Homeless-Youth-Survey-July-2012.pdf
- Elwood W. N., Williams M. L., Bell D. C., Richard A. J. (1997). Powerlessness and HIV prevention among people who trade sex for drugs (“strawberries”). AIDS Care, 9, 273-284. doi: 10.1080/713613155 [DOI] [PubMed] [Google Scholar]
- Faul F., Erdfelder E., Lang A. G., Buchner A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavioral Research Methods, 39, 175-191. [DOI] [PubMed] [Google Scholar]
- Halkitis P. N., Fischgrund B. N., Parsons J. T. (2005). Explanations for methamphetamine use among gay and bisexual men in New York City. Substance Use & Misuse, 40, 1331-1345. doi: 10.1081/JA-200066900 [DOI] [PubMed] [Google Scholar]
- Halkitis P. N., Shrem M. T., Martin F. W. (2005). Sexual behavior patterns of methamphetamine-using gay and bisexual men. Substance Use & Misuse, 40, 703-719. [DOI] [PubMed] [Google Scholar]
- Hedeker D., Gibbons R. D., Waternaux C. (1999). Sample size estimation for longitudinal designs with attrition. Journal of Education and Behavioral Statistics, 24, 70-93. [Google Scholar]
- Higgins S. T., Budney A. J., Bickel W. K., Foerg F. E., Donham R., Badger G. J. (1994). Incentives improve outcome in outpatient behavioral treatment of cocaine dependence. Archives of General Psychiatry, 51, 568-576. [DOI] [PubMed] [Google Scholar]
- Koblin B. A., Murrill C., Camacho M., Xu G., Liu K. L., Raj-Singh S., Torian L. (2007). Amphetamine use and sexual risk among men who have sex with men: Results from the National HIV Behavioral Surveillance study—New York City. Substance Use & Misuse, 42, 1613-1628. doi: 10.1080/10826080701212519 [DOI] [PubMed] [Google Scholar]
- Kral A. H., Lorvick J., Ciccarone D., Wenger L., Gee L., Martinez A., Edlin B. R. (2005). HIV prevalence and risk behaviors among men who have sex with men and inject drugs in San Francisco. Journal of Urban Health, 82(1 Suppl. 1), i43-i50. doi: 10.1093/jurban/jti023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leake B., Nyamathi A., Gelberg L. (1997). Reliability, validity, and composition of a subset of the Centers for Disease Control and Prevention acquired immunodeficiency syndrome knowledge questionnaire in a sample of homeless and impoverished adults. Medical Care, 35, 747-755. [DOI] [PubMed] [Google Scholar]
- McLellan A. T., Kushner H., Metzger D., Peters R., Smith I., Grissom G., . . . Argeriou M. (1992). The Fifth Edition of the Addiction Severity Index. Journal of Substance Abuse Treatment, 9, 199-213. [DOI] [PubMed] [Google Scholar]
- Menza T., Jameson D., Hughes J., Colfax G., Shoptaw S., Golden M. (2010). Contingency management to reduce methamphetamine use and sexual risk among men who have sex with men: A randomized controlled trial. BMC Public Health, 10, 774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. (1989). AIDS knowledge and attitudes of Black Americans. Hyattsville, MD: Centers for Disease Control. [Google Scholar]
- Nyamathi A. (1989). Comprehensive health seeking and coping paradigm. Journal of Advanced Nursing, 14, 281-290. [DOI] [PubMed] [Google Scholar]
- Nyamathi A., Flaskerud J. H., Leake B., Dixon E. L., Lu A. (2001). Evaluating the impact of peer, nurse case-managed, and standard HIV risk-reduction programs on psychosocial and health-promoting behavioral outcomes among homeless women. Research in Nursing & Health, 24, 410-422. doi: 10.1002/nur.1041 [DOI] [PubMed] [Google Scholar]
- Nyamathi A., Liu Y., Marfisee M., Shoptaw S., Gregerson P., Saab S., . . . Gelberg L. (2009). Effects of a nurse-managed program on hepatitis A and B vaccine completion among homeless adults. Nursing Research, 58, 13-22. doi: 10.1097/NNR.0b013e3181902b93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A., Nahid P., Berg J., Burrage J., Christiani A., Aqtash S., . . . Leake B. (2008). Efficacy of nurse case-managed intervention for latent tuberculosis among homeless subsamples. Nursing Research, 57, 33-39. doi: 10.1097/01.NNR.0000280660.26879.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A., Salem B., Reback C. J., Shoptaw S., Branson C. M., Idemundia F. E., . . . Liu Y. (2013). Correlates of hepatitis b virus and HIV knowledge among gay and bisexual homeless young adults in Hollywood. American Journal of Men’s Health, 7, 18-26. doi: 10.1177/1557988312456068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A., Stein J. A., Schumann A., Tyler D. (2007). Latent variable assessment of outcomes in a nurse-managed intervention to increase latent tuberculosis treatment completion in homeless adults. Health Psychology, 26, 68-76. doi: 10.1037/0278-6133.26.1.68 [DOI] [PubMed] [Google Scholar]
- Nyamathi A., Tyler D., Sinha K., Marfisee M., Cohen A., Greengold B. (2010). Predictors of hepatitis knowledge improvement among methadone maintained clients enrolled in a hepatitis intervention program. Journal of Community Health, 35, 423-432. doi: 10.1007/s10900-010-9266-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A. M., Christiani A., Nahid P., Gregerson P., Leake B. (2006). A randomized controlled trial of two treatment programs for homeless adults with latent tuberculosis infection. International Journal of Tuberculosis & Lung Disease, 10, 775-782. [PubMed] [Google Scholar]
- Nyamathi A. M., Dixon E. L., Wiley D., Christiani A., Lowe A. (2006). Hepatitis C virus infection among homeless men referred from a community clinic. Western Journal of Nursing Research, 28, 475-488. doi: 10.1177/0193945906286620 [DOI] [PubMed] [Google Scholar]
- Nyamathi A. M., Sinha K., Saab S., Marfisee M., Greengold B., Leake B., Tyler D. (2009). Feasibility of completing an accelerated vaccine series for homeless adults. Journal of Viral Hepatitis, 16, 666-673. doi: 10.1111/j.1365-2893.2009.01114.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purcell D. W., Parsons J. T., Halkitis P. N., Mizuno Y., Woods W. J. (2001). Substance use and sexual transmission risk behavior of HIV-positive men who have sex with men. Journal of Substance Abuse, 13, 185-200. [DOI] [PubMed] [Google Scholar]
- Radloff L. S. (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385-401. [Google Scholar]
- Reback C. J., Kamien J. B., Amass L. (2007). Characteristics and HIV risk behaviors of homeless, substance-using men who have sex with men. Addictive Behaviors, 32, 647-654. doi: 10.1016/j.addbeh.2006.06.008 [DOI] [PubMed] [Google Scholar]
- Reback C. J., Peck J. A., Dierst-Davies R., Nuno M., Kamien J. B., Amass L. (2010). Contingency management among homeless, out-of-treatment men who have sex with men. Journal of Substance Abuse Treatment, 39, 255-263. doi: 10.1016/j.jsat.2010.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross M. W., Kajubi P., Mandel J. S., McFarland W., Raymond H. F. (2013). Internalized homonegativity/homophobia is associated with HIV-risk behaviours among Ugandan gay and bisexual men. International Journal of STDs & AIDS, 24, 409-413. doi: 10.1177/0956462412472793 [DOI] [PubMed] [Google Scholar]
- Royal S. W., Kidder D. P., Patrabansh S., Wolitski R. J., Holtgrave D. R., Aidala A., . . . Stall R. (2009). Factors associated with adherence to highly active antiretroviral therapy in homeless or unstably housed adults living with HIV. AIDS Care, 21, 448-455. doi: 10.1080/09540120802270250 [DOI] [PubMed] [Google Scholar]
- Schumann A., Nyamathi A., Stein J. A. (2007). HIV risk reduction in a nurse case-managed TB and HIV intervention among homeless adults. Journal of Health Psychology, 12, 833-843. doi: 10.1177/1359105307080618 [DOI] [PubMed] [Google Scholar]
- Secades-Villa R., Garcia-Fernandez G., Pena-Suarez E., Garcia-Rodriguez O., Sanchez-Hervas E., Fernandez-Hermida J. R. (2013). Contingency management is effective across cocaine-dependent outpatients with different socioeconomic status. Journal of Substance Abuse Treatment, 44, 349-354. doi: 10.1016/j.jsat.2012.08.018 [DOI] [PubMed] [Google Scholar]
- Senreich E. (2009). A comparison of perceptions, reported abstinence, and completion rates of gay, lesbian, bisexual, and heterosexual clients in substance abuse treatment. Journal of Gay & Lesbian Mental Health, 13, 145-169. [Google Scholar]
- Shoptaw S., Klausner J. D., Reback C. J., Tierney S., Stansell J., Hare C. B., . . . Dang J. (2006). A public health response to the methamphetamine epidemic: The implementation of contingency management to treat methamphetamine dependence. BMC Public Health, 6, 214. doi: 10.1186/1471-2458-6-214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoptaw S., Reback C. J., Larkins S., Wang P. C., Rotheram-Fuller E., Dang J., Yang X. (2008). Outcomes using two tailored behavioral treatments for substance abuse in urban gay and bisexual men. Journal of Substance Abuse Treatment, 35, 285-293. doi: 10.1016/j.jsat.2007.11.004 [DOI] [PubMed] [Google Scholar]
- Shoptaw S., Reback C. J., Peck J. A., Yang X., Rotheram-Fuller E., Larkins S., . . . Hucks-Ortiz C. (2005). Behavioral treatment approaches for methamphetamine dependence and HIV-related sexual risk behaviors among urban gay and bisexual men. Drug & Alcohol Dependence, 78, 125-134. doi: 10.1016/j.drugalcdep.2004.10.004 [DOI] [PubMed] [Google Scholar]
- Stewart A. L., Hays R. D., Ware J. E., Jr. (1988). The MOS short-form general health survey. Reliability and validity in a patient population. Medical Care, 26, 724-735. [DOI] [PubMed] [Google Scholar]
- Twitchell G. R., Huber A., Reback C. J., Shoptaw S. (2002). Comparison of general and detailed HIV risk assessments among methamphetamine abusers. AIDS & Behavior, 6, 153-162. [Google Scholar]
- Wong F. L., Rotheram-Borus M.-J., Lightfoot M., Pequegnat W., Comulada W. S., Cumberland W., . . . Johnson M. (2008). Effects of behavioral intervention on substance use among people living with HIV: The Healthy Living Project randomized controlled study. Addiction, 103, 1206-1214. [DOI] [PMC free article] [PubMed] [Google Scholar]