Abstract
The Sexual Health in Faith Traditions Study evaluated the relationships between religiosity, spirituality, internalized homonegativity, and sexual risk behaviors among a sample of African American men who have sex with men living in the Deep South. Participants were recruited primarily from Black Gay Pride celebrations to complete a self-administered, paper-and-pencil survey. Structural equation modeling was used to determine relationships between key constructs and condom use for insertive (n = 285) and receptive (n = 263) anal intercourse in the past 3 months. Almost half of respondents reported using condoms “every time” when engaging in insertive (48.3%) or receptive (45.1%) anal intercourse. Religiosity and spirituality were differentially associated with dimensions of internalized homonegativity. While no significant direct relationships were reported between either religiosity or spirituality and condom use, dimensions of internalized homonegativity mediated significant indirect relationships. Findings suggest that religiosity and spirituality influence African American men who have sex with men’s internalized homonegativity and, subsequently, engagement in safer sex behaviors.
Keywords: religiosity, spirituality, internalized homonegativity, condom use, African American MSM
Introduction
African American men who have sex with men (AAMSM) are disproportionately affected by HIV. AAMSM are estimated to account for 9% of all men who have sex with men (MSM) in the United States, but represent 38% of new HIV infections among MSM (Black AIDS Institute, 2012). An estimated 15,855 African American men were diagnosed with HIV infection in 2013; of those, 76% were reported to have been infected through male-to-male sexual contact (Centers for Disease Control and Prevention, 2015). According to a six-city study conducted by the HIV Prevention Trials Network (2012), the rate of new HIV infections among AAMSM was 2.8% per year, a rate that is 50% higher than the infection rate for White MSM in the United States. The high reported incidence rates of HIV infection among AAMSM are comparable to HIV infection rates in developing countries (Mays, Cochran, & Zamudio, 2004).
Similarly, within the American South, rates of HIV infection were higher among AAMSM than the rates for White or Hispanic MSM (Lieb et al., 2011). While the HIV epidemic among AAMSM has been well-documented, less attention has been given to finding explanations for the high rates of HIV infection among AAMSM. Condomless anal intercourse is one of the most commonly cited factors associated with HIV infection among MSM (Beyrer et al., 2012; Koblin et al., 2006). Previous research has indicated that there are no significant differences between AAMSM and MSM of other racial/ethnic groups, and in some cases that AAMSM were comparatively less likely to engage in condomless anal intercourse or other high-risk sexual behaviors (Millett, Peterson, Wolitski, & Stall, 2006). The lack of race-based differences in HIV risk behaviors suggests that alternative explanations for the high rates of HIV infection among AAMSM as compared with other racial/ethnic MSM groups must exist. For example, the Black AIDS Institute (2012) outlined potential factors that may contribute to increased HIV burden among AAMSM including diminished access to health care and lower health service utilization; high prevalence of other sexually transmitted infections; sexual behavior patterns among young AAMSM, including earlier sexual debut and increased likelihood of having older sex partners; and social determinants of health, including poverty, unemployment, violence, homelessness, childhood sexual abuse, and incarceration. More attention should be given to the sociocultural contextual factors that may influence the sexual behaviors and subsequent HIV risk of AAMSM (Ayala, Bingham, Kim, Wheeler, & Millett, 2012; Malebranche, 2003; Millett, Flores, Peterson, & Bakeman, 2007). One such factor that warrants further investigation is the role of African American religiosity and spirituality on sexual health.
The Black Church in African American Communities
One of the oldest and most influential institutions in African American communities is the African American Christian faith community, commonly referred to as the “Black church.” The Black church is a foundation that links African American ethnicity, the American South, working-class socioeconomic status, and conservative sociopolitical ideology (Schulte & Battle, 2004). Lincoln and Mamiya (1990) argued that
the core values of black culture, like freedom, justice, equality, an African heritage, and racial parity at all levels of human intercourse, are raised to ultimate levels and legitimated in the black sacred cosmos . . . given birth and nurtured in the womb of the Black Church. (p. 7)
This notion of the Black church as the cultural nucleus of African American history and culture is also evidenced in the Black church’s role in the development of nonreligious organizations, such as the National Association for the Advancement of Colored People, that have advocated for civil rights and social justice (Calhoun-Brown, 2000).
According to Lugo et al. (2008), African Americans are the most likely racial or ethnic group to report a formal religious affiliation, with the vast majority (85%) identifying as Christian. African Americans also report frequent attendance at religious services, high rates of prayer and affective religious behaviors, and feel strongly that their religious beliefs guide their approach to life (Taylor, Chatters, & Brown, 2014). Even African Americans who are “unaffiliated” with a religious group still often report having been profoundly influenced by the religious ideology in which they were raised, and that these doctrines continue to influence their current beliefs (Dyson, 2003; Lugo et al., 2008).
African American religiosity has also been associated with positive health outcomes. For example, African Americans who frequently attended church experienced lower rates of mortality than those who did not attend frequently (Ellison, Hummer, Cormier, & Rogers, 2000). Similarly, another study reported that African American and Puerto Rican women living with HIV/AIDS cited spirituality as a key component of their ability to live healthy lives; however, they emphasized aspects of religious activity, specifically citing prayer, television ministries, and Bible reading as markers of their spirituality, indicating a strong relationship between religious activity and spirituality (Musgrave, Allen, & Allen, 2002).
The Black Church, AAMSM, and HIV
While positive associations between religiosity, spirituality, and health have been documented among African Americans, AAMSM may not experience the same benefits of involvement in African American religious life. Many Black churches espouse antihomosexual, or homonegative, messages and policies that can negatively affect AAMSM members (Ward, 2005). Some of these homonegative positions are based on Biblical interpretations of homosexuality as “sinful,” relying on a small number of passages in the Bible that reference homosexual behavior. These homonegative positions may also be based in historical realities and sociocultural stereotypes about African American sexuality. For example, many African American churches and communities have adopted conservative constructions of African American sexuality as a way to resist stereotypes of hypersexuality and “deviant” sexual proclivities that were often used to justify the mistreatment, abuse, and segregation of Black people in American society (Collins, 2004; Douglas, 1999). As a result, many African American faith communities have developed a negative view of homosexuality as a threat to the African American family and manhood (Collins, 2004; Douglas, 1999; Griffin, 2006).
Regardless of the origins of homonegativity in Black churches, its effects on AAMSM are pernicious. Homonegativity is manifested in Black churches to varying degrees, ranging from verbal hostility to silence (Ward, 2005). Pastors, preachers, or church leaders may publicly engage in verbal ridicule of homosexual men using derogatory terms and situating them as a threat to Black masculinity and survival of the race, with little to no resistance—and often, encouragement—from parishioners. Qualitative studies have indicated that many churches’ antihomosexual messages have contributed to a hierarchy of “sin,” or a perception that being a homosexual is more egregious than other transgressions, such as adultery or participation in the drug trade (Fullilove & Fullilove, 1999). Other churches adopt a culture of silence on homosexuality, privately encouraging AAMSM to participate in the religious community as long as no outward acknowledgments or expressions of their sexuality are displayed (Jeffries, Dodge, & Sandfort, 2008). This notion of private welcome in the face of public ridicule has been described as the “open closet,” or a phenomenon in which nonheterosexuals are encouraged to take part in the religious experience at the expense of their nonheterosexual identity (Fullilove & Fullilove, 1999).
Some researchers have suggested that homophobia among Black churches, and by extension African American communities, has contributed to the dramatic spread of HIV/AIDS among African Americans. Fullilove and Fullilove (1999) argued that, because discussion of HIV/AIDS is often linked to discussions about sexuality in general and homosexuality in particular, many churches have shied away from engagement in HIV prevention, testing, treatment, and care activities out of reluctance to acknowledge the existence of homosexuality in African American populations. Because of the widespread homonegative experiences often associated with participation in traditional African American religious organizations or communities, it may seem logical to believe that AAMSM would eschew religion and spirituality altogether. However, research suggests that AAMSM, despite the homonegative messages they may receive, maintain high levels of involvement in African American religious life (Griffin, 2006; Jeffries et al., 2008; Pitt, 2010; Woodyard, Peterson, & Stokes, 2000).
When faced with homonegative messages from the pulpit, many AAMSM have expressed feelings of guilt, condemnation, embarrassment, and alienation, to the point that they sometimes internalize those negative messages (Balaji et al., 2012; Woodyard et al., 2000). This phenomenon, referred to as internalized homonegativity, has been associated with depression, anxiety (Graham, Aronson, Nichols, Stephens, & Rhodes, 2011), and sexual risk behaviors that could lead to HIV infection among AAMSM (Amola & Grimmett, 2015; Stokes & Peterson, 1998). Griffin (2006) wrote that the homophobia sanctioned by the Black church has become internalized by many AAMSM, who begin to harbor beliefs that they are “inherently sinful because they are sexually attracted to the same sex” (p. 149). Internalized homonegativity has also discouraged AAMSM from accessing HIV prevention information (Voisin, Bird, Shiu, & Krieger, 2013).
Despite the potential negative effects of AAMSM religious participation, AAMSM have developed resilience and coping strategies to the negative messages they encounter through spirituality. Spirituality is defined as “the sense of meaning, purpose, and morality that individuals espouse regarding their lives” (Tan, 2005, p. 136). Spirituality is considered distinct from religiosity in that, whereas religiosity is considered an embrace of prescribed beliefs and practices, spirituality refers more to internal values and relationships (Mattis, 2000). Some AAMSM have indicated that a personal sense of spirituality provided them with the resilience to neutralize antigay messages and accept their sexual orientation, calling on affirming messages such as “God loves me,” “God made me this way,” or “Only God can judge me” as a coping mechanism (Jeffries et al., 2008; Miller, 2007; Woodyard et al., 2000). Greater spirituality has also been identified as a significant predictor of lower experiences of internalized homonegativity (Tan, 2005).
Although the disproportionate impact of HIV infection among AAMSM has been well-documented in the literature, little information is available about the underlying psychological and sociocultural factors that contribute to their increased risk. Furthermore, even less is known about the associations between these factors and the unique ways in which they manifest themselves among AAMSM.
Study Purpose
The purpose of this study was to better understand the relationships between religiosity, spirituality, and internalized homonegativity, and explore their connection to condom use among AAMSM. Specifically, the authors sought to address the following research questions:
Research Question 1: Is religiosity negatively associated with condom use among AAMSM?
Research Question 2: Is spirituality positively associated with condom use among AAMSM?
Research Question 3: Does internalized homonegativity mediate the associations between religiosity, spirituality, and sexual risk behaviors among AAMSM?
The results of this study can contribute to the development of more culturally-specific, contextually-based HIV prevention interventions for AAMSM.
Method
Sample and Recruitment
Data were collected between June 2011 and December 2011, from 348 participants enrolled in the Sexual Health in Faith Traditions (SHIFT) Study, a cross-sectional, quantitative study of AAMSM living in the Deep South. Participants were included in the study if they met the following criteria: (a) self-identifying as an African American man who had sex with a man at least once in the past 12 months, or self-identifying as gay or bisexual regardless of having had sex with a man in the past 12 months; (b) aged 18 years or older; and (c) residing in one of the states classified as the “Deep South”: Alabama, Georgia, Louisiana, Mississippi, North Carolina, or South Carolina. These states were selected because they share similar demographic profiles as well as similar patterns of HIV infection rates (Reif, Geonnotti, & Whetten, 2006).
Participants were recruited into the SHIFT Study using multiple strategies. A purposive convenience sample was recruited using a proactive recruitment strategy at Black Gay Pride celebrations in the following cities in the Deep South: Columbia, SC; Charlotte, NC; Raleigh, NC; Atlanta, GA; and Jackson, MS. More than four fifths (80.2%) of study participants were recruited at Black Gay Pride events. In two Southern cities that did not have Black Gay Pride celebrations (Greenville, SC and Greensboro, NC), small social gatherings, or “survey parties,” were held to recruit participants. For these “survey parties,” the principal investigator (PI) reached out to professional colleagues in both cities to request their assistance with recruitment. The “host” in each city secured the venue, provided food, and recruited attendees to participate in the study at a designated time by circulating the SHIFT Study flyer. These flyers, which contained basic information about the study purpose and its target population, were also distributed through community-based HIV prevention organizations, AIDS service organizations, lesbian, gay, bisexual, and transgender (LGBT)–serving organizations, LGBT-friendly businesses, and LGBT e-mail listservs. Finally, a Facebook page and Twitter account were developed as a means to recruit potential participants. All SHIFT Study protocols were approved by the Institutional Review Board at the University of South Carolina.
Data Collection
Data were collected using printed surveys administered by the PI or a trained member of the data collection team. Before administering the survey, the data collector provided a brief verbal summary of the survey’s purpose and an estimate of the time required to complete it (approximately 10 minutes). The data collector then provided the participant with a copy of the informed consent form, outlining the study’s purpose, potential risks, benefits, and the PI’s contact information. The participant then received a printed survey to complete. Data collectors were allowed to read aloud any items in which the participant had difficulty comprehending. The data collectors were instructed not to interpret items for the participant. After the survey was completed, the data collector placed the survey in a sealable file folder and provided the participant with $5 cash as an incentive for their participation.
For AAMSM in the PI’s local area who expressed an interest in participating, the PI met each contact in a mutually agreed-on location at a time that was convenient for the potential participant and followed the data collection protocols. On completion of the survey, the study participant was asked to share information about the study with at least three to five other members of the target population who might be interested in participating in the study. The PI provided each study participant with a phone number and e-mail address through which new potential participants could contact the PI for more information and to schedule a time to complete the survey.
Measures
Data for the SHIFT Study were collected using a cross-sectional survey which included measures of sociodemographic characteristics, religiosity, spirituality, internalized homonegativity, and condom use. Sociodemographic variables in the survey included age (in years), highest educational level attained, income, relationship status, sexual identity, HIV status, and degree of masculinity/femininity. Sexual identity was measured by one item, “How do you describe yourself?” Response options were “gay/homosexual,” “same-gender-loving,” “bisexual,” “straight/heterosexual,” and “other.” Those who chose “other” were given space to write their own description. HIV status was measured by one item, “Have you ever tested positive for HIV?” Response options were “yes,” “no,” and “I have never been tested for HIV.” Degree of the respondent’s masculinity/femininity was measured by one item, “Which statement best describes you?” Response options were “extremely masculine,” “masculine,” “equally masculine and feminine,” “feminine,” and “extremely feminine.” The degree of masculinity was measured because previous research has indicated that, among young AAMSM, perceptions of masculinity may influence perceptions of partner risk and condom use decision making (Fields et al., 2012).
Religiosity was measured using the Religious Commitment Inventory–10 (RCI-10), a 10-item measure, scored using a 5-point Likert-type scale, with responses ranging from 1 (“not at all true of me”) to 5 (“totally true of me”; Worthington et al., 2003). Religious commitment was defined as “the degree to which a person adheres to his or her religious values, beliefs, and practices and uses them in daily living” (Worthington et al., 2003, p. 85). The RCI-10 has demonstrated good internal consistency reliability (α = .93) and evidence of construct validity (Worthington et al., 2003). The Cronbach’s alpha for the RCI-10 in the present study is .94.
Spirituality was measured using the Daily Spiritual Experiences Scale (DSES). The DSES is a 16-item scale developed to address “reported ordinary experiences of spirituality such as awe, joy that lifts one out of the mundane, and a sense of deep inner peace” (Underwood & Teresi, 2002, p. 22). A total 15 of the 16 items in the DSES are scored using a modified 6-point Likert-type scale, in which responses range from “many times a day” to “never or almost never.” The final item, “In general, how close do you feel to God?” has four response options: “not close at all,” “somewhat close,” “very close,” and “as close as possible.” The items are then summed to create an overall score on the DSES (Underwood, 2006). Lower scores on the DSES indicate a higher occurrence of daily spiritual experiences; however, for the SHIFT Study, all items were reverse-coded so that higher scores indicated a higher occurrence of daily spiritual experiences. The DSES has exhibited high internal consistency reliability, with Cronbach’s alpha values around .94 (Underwood & Teresi, 2002); in the present study, the Cronbach’s alpha for the DSES is .96.
Internalized homonegativity was measured using the 23-item Internalized Homonegativity Inventory (IHNI). Responses were scored on a 6-point Likert-type scale (1 = “strongly disagree” to 6 = “strongly agree”). Mayfield (2001) reported an internal consistency reliability of .91 for the entire 23-item inventory and evidence of construct validity. The IHNI has been used in previous studies to assess levels of internalized homonegativity among AAMSM, with reliability coefficients ranging from .76 to .91 for the entire scale (Shoptaw et al., 2009; Young, Shoptaw, Weiss, Munjas, & Gorbach, 2011). While the original IHNI measured internalized homonegativity across three subscales (“Personal Homonegativity,” “Gay Affirmation,” “Morality of Homosexuality”), an exploratory factor analysis of SHIFT Study data provided evidence of a two-factor solution; in the exploratory factor analysis, one factor included all of the items from both the “Personal Homonegativity” and “Morality of Homosexuality” subscales, while the “Gay Affirmation” subscale remained intact. The “Gay Affirmation” label was retained, while the combined factor was reclassified as “Personal/Moral Homonegativity” (Smallwood, Spencer, Annang Ingram, Thrasher, & Thompson-Robinson, 2013). The two-dimensional conceptualization of internalized homonegativity was used in the present study. Cronbach’s alpha values in the present study for the entire IHNI (α = .93) and the identified subscales (Gay Affirmation subscale of the IHNI α = .83, Personal/Moral Homonegativity subscale of the IHNI α = .93) provide evidence of good internal consistency.
Condom use was assessed using two items adapted from the National Household Survey of Drug Abuse (U.S. Department of Health & Human Services, 2013). Participants were asked about their frequency of condom use for insertive anal intercourse (IAI) and receptive anal intercourse (RAI) with another man in the past 3 months, respectively. Response options were presented on a 4-point Likert-type scale (1 = “every time,” 2 = “most times,” 3 = “some times,” 4 = “never”), with an additional response option for those who reported that they had not had anal intercourse with another man in the past 3 months. Response options 1 to 4 were reverse-coded for analysis. Those who reported not engaging in anal intercourse in the past 3 months were excluded from analysis.
Data Analysis
Descriptive statistics were calculated for all study variables using SPSS version 20, including means and standard deviations for continuous variables and frequencies for categorical variables. Latent variable structural equation modeling was conducted using Mplus version 5.2 (Muthén & Muthén, 2008). Structural equation modeling is a statistical technique that uses both a measurement (confirmatory factor) model and a structural (path) model to evaluate the validity of a theoretical model using both observed and latent variables (Schumacker & Lomax, 2004). A full information maximum likelihood estimation method was used to address missing data (Little & Rubin, 2002). A full information maximum likelihood is different from other common methods of dealing with missing data (e.g., listwise or pairwise deletion) in that all available data are used in the process of parameter estimation, thus minimizing the number of cases that are excluded from analysis (Enders & Bandalos, 2001).
Structural equation models were generated separately for two outcome variables: frequency of condom use during IAI and RAI, respectively. In each model, the analytic sample was restricted only to those who had participated in either type of anal intercourse within the past 3 months (n = 285 for IAI; n = 263 for RAI). Note: Almost three fourths of the overall sample (71.0%) had engaged in both IAI and RAI in the previous 3 months.
Model fit was assessed using six indices. A chi-square difference test was used to assess absolute model fit, which is calculated based on the differences between the observed and reproduced covariance matrix. A chi-square statistic with an associated p value greater than .05 is indicative of good model fit. However, a significant chi-square statistic may not necessarily provide evidence for poor model fit, as the chi-square test is sensitive to sample size (Schumacker & Lomax, 2004). In addition to the chi-square test, the goodness-of-fit index (GFI; Bentler & Bonett, 1980), normed fit index (NFI; Bollen, 1989), Bentler comparative fit index (CFI; Bentler, 1980), the nonnormed fit index (NNFI), also known as the Tucker–Lewis Index (TLI; Tucker & Lewis, 1973), and the root mean square error of approximation (RMSEA; Brown & Cudek, 1993) were used to assess model fit. GFI values of .90 or greater, NFI, CFI, and TLI values of .95 or greater, and RMSEA values of .05 or lower are generally considered indicators of acceptable model fit; however, these cutoffs are considered as guidelines and are not absolute (Barrett, 2007; Lance, Butts, & Michels, 2006). Based on model complexity and sample size for this study, GFI values of .93 or greater, CFI values of .96 or greater, TLI values of .95 or greater, NFI values of .94 or greater, and RMSEA values of .05 or lower were used to evaluate model fit (Sivo, Fan, Witta, & Willse, 2006).
To allow for the possibility of different relationships among the variables of interest, the outcome variables—frequency of condom use for IAI and RAI in the past 3 months—were modeled separately. In the proposed models, religiosity and spirituality were considered exogenous variables. The two components of internalized homonegativity were endogenous variables and tested to determine whether they mediate the relationships between the exogenous variables and condom use. Religiosity, spirituality, and internalized homonegativity were treated as continuous latent variables.
Results
Participant Characteristics
The mean age of participants was 28.24 years (SD = 8.46) for the IAI analytic sample and 27.65 years (SD = 8.34) for the RAI analytic sample. As illustrated in Table 1, more than a third of the men in each analytic sample reported having some college education but no degree, and almost three-fourths reported an annual income of less than $40,000. The majority of men reported a “single” relationship status and a gay/homosexual identity. Most men classified themselves as being equally masculine and feminine or masculine. Almost one quarter of the participants reported having tested positive for HIV.
Table 1.
Sociodemographic Characteristics of Study Participants.
| As insertive partner (n = 285) |
As receptive partner (n = 263) |
|||
|---|---|---|---|---|
| N | % | N | % | |
| State of residence | ||||
| Georgia | 58 | 20.4 | 50 | 19.0 |
| Louisiana | 3 | 1.1 | 3 | 1.1 |
| Mississippi | 72 | 25.3 | 70 | 26.6 |
| North Carolina | 67 | 23.5 | 60 | 22.8 |
| South Carolina | 83 | 29.1 | 78 | 29.7 |
| Highest educational level completed | ||||
| High school diploma/GED or less | 55 | 19.3 | 56 | 21.3 |
| Some college but no degree | 102 | 35.8 | 97 | 36.9 |
| Associate’s or bachelor’s degree | 72 | 25.2 | 69 | 26.3 |
| Some graduate school or advance degree | 55 | 19.3 | 40 | 15.2 |
| Annual income | ||||
| Less than $10,000 | 64 | 22.5 | 63 | 24.0 |
| $10,000-$24,999 | 63 | 22.1 | 62 | 23.6 |
| $25,000-$39,999 | 77 | 27.0 | 72 | 27.4 |
| $40,000-$49,999 | 39 | 13.7 | 32 | 12.2 |
| $50,000 or more | 40 | 14.1 | 32 | 12.2 |
| Relationship status | ||||
| Single | 163 | 57.2 | 149 | 56.7 |
| Dating | 78 | 27.4 | 72 | 27.4 |
| Married/long-term relationship with man | 35 | 12.3 | 34 | 12.9 |
| Married/long-term relationship with woman | 2 | 0.7 | 2 | 0.8 |
| Separated | 4 | 1.4 | 4 | 1.5 |
| Sexual identity | ||||
| Gay/homosexual | 204 | 71.6 | 192 | 73.0 |
| Same-gender-loving | 20 | 7.0 | 16 | 6.1 |
| Bisexual | 41 | 14.4 | 36 | 13.7 |
| Straight/heterosexual | 2 | 0.7 | 2 | 0.8 |
| Other | 6 | 2.1 | 7 | 2.7 |
| Masculinity/femininity | ||||
| Extremely masculine/masculine | 119 | 41.8 | 99 | 37.7 |
| Equally masculine and feminine | 135 | 47.4 | 132 | 50.2 |
| Extremely feminine/feminine | 26 | 9.2 | 29 | 11.1 |
| Ever tested positive for HIV | ||||
| Yes | 65 | 22.8 | 63 | 24.0 |
| No | 210 | 73.7 | 189 | 71.9 |
| I have never been tested for HIV | 3 | 1.1 | 4 | 1.5 |
Note. GED = general educational development. The column totals may not sum to 100% due to missing values.
The data used for both IAI and RAI models were limited to those men who reported engaging in IAI and RAI, respectively, over the past 3 months. In the IAI model, significant differences were identified between included and excluded cases by HIV status, with seropositivity rates of 11% for excluded cases and 24% for included cases. In the RAI model, significant differences were identified between included and excluded cases on several sociodemographic variables. Those excluded from analysis were older, with a mean age of 30.04 years compared with 27.65 years in the included cases. Excluded cases also reported more educational experience, higher income, being more masculine, and a lower HIV seropositivity rate (10%, as opposed to 25% among included cases; data not reported).
Condom Use During Insertive Anal Intercourse
The chi-square difference test for condom use during IAI was significant (χ2 = 343.66, df = 6), p < .001, indicating inadequate model fit. However, other fit indices provided evidence of adequate fit (GFI = .95, NFI = .95, CFI = .98, TLI = .98, RMSEA = .04).
Bivariate correlations were calculated to determine the magnitude and direction of the relationships between certain variables. Religiosity and spirituality were significantly correlated (r = .38, p < .001), as were the two dimensions of internalized homonegativity, Personal/Moral Homonegativity and Gay Affirmation (r = −.11, p < .001).
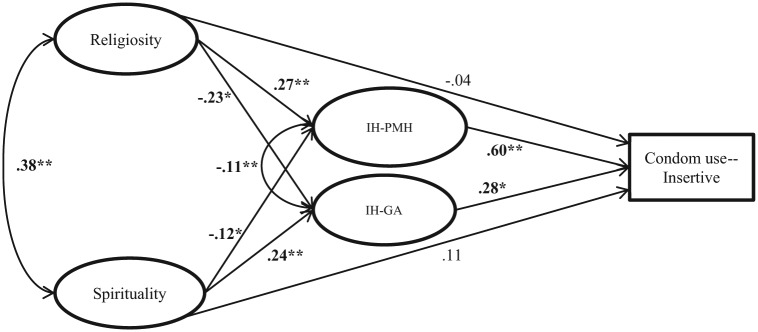
Figure 1 illustrates the structural model and corresponding path coefficients for predictors of condom use during IAI. Several paths in the model were statistically significant. Religiosity had a significant effect on both dimensions of internalized homonegativity: Personal/Moral Homonegativity (Β = .27, p < .001) and Gay Affirmation (Β = −.23, p = .01), indicating that higher levels of religiosity were associated with higher levels of Personal/Moral Homonegativity, and with lower levels of Gay Affirmation. Spirituality also had a significant effect on both Personal/Moral Homonegativity (Β = −.12, p = .02) and Gay Affirmation (Β = .24, p = .002). These results suggest that higher levels of spirituality were associated with higher levels of Gay Affirmation and lower levels of Personal/Moral Homonegativity. However, neither religiosity nor spirituality demonstrated a significant direct effect on the frequency of condom use during IAI in the past 3 months. Both Gay Affirmation (Β = .28, p = .03) and Personal/Moral Homonegativity (Β = .60, p = .001) had significant direct effects on condom use during IAI, indicating that higher levels of both Gay Affirmation and Personal/Moral Homonegativity were associated with increased frequency of condom use for IAI in the past 3 months.
Figure 1.
Structural model path diagram for frequency of condom use during insertive anal intercourse with unstandardized path coefficients (n = 285).
Note. IH-PMH = Personal/Moral Homonegativity subscale of the IHNI; IH-GA = Gay Affirmation subscale of the IHNI. *Denotes significance at p < .05, **denotes significance at p < .01.
A test of indirect effects was conducted to examine whether dimensions of internalized homonegativity mediated the relationships between religiosity, spirituality, and condom use during IAI. Assessment of the overall indirect pathways from religiosity and spirituality to condom use during IAI suggested Personal/Moral Homonegativity mediated the relationship between religiosity and frequency of condom use (Β = .11, p = .01). None of the indirect paths involving spirituality and dimensions of internalized homonegativity was significant.
Condom Use During Receptive Anal Intercourse
The chi-square difference test for condom use during RAI was significant (χ2 = 297.83, df = 6), p < .001, indicating less than ideal model fit. However, other fit indices provide evidence of adequate model fit (GFI = .94, NFI = .94, CFI = .98, TLI = .98, RMSEA = .04).
As in the model for IAI condom use, bivariate correlations were calculated to determine the magnitude and direction of relationships between religiosity and spirituality, and between Gay Affirmation and Personal/Moral Homonegativity. Religiosity and spirituality were significantly correlated (r = .39, p < .001), as were the two dimensions of internalized homonegativity, Gay Affirmation and Personal/Moral Homonegativity (r = −.10, p < .001). The model explained 5% of the variance in Gay Affirmation and 7% of the variance in Personal/ Moral Homonegativity.
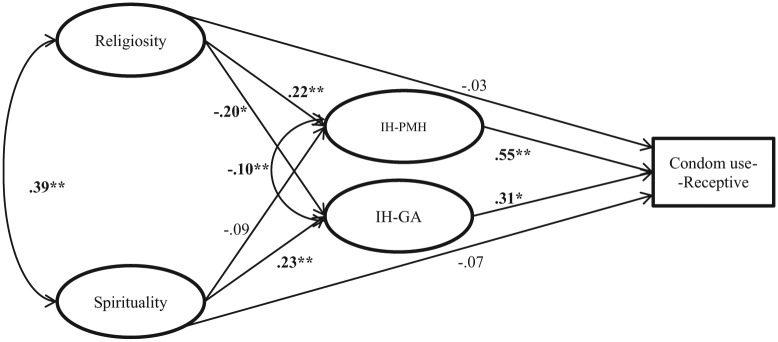
Figure 2 illustrates the structural model and corresponding path coefficients for predictors of condom use during RAI. Again, several paths within the model were statistically significant. Religiosity scores were associated with a significant direct effect on the two dimensions of internalized homonegativity, Gay Affirmation (Β = −.20, p = .03) and Personal/Moral Homonegativity (Β = .22, p = .001). This indicates that higher levels of religiosity were associated with higher levels of Personal/Moral Homonegativity, and lower levels of Gay Affirmation. Spirituality was associated with a significant direct effect on Gay Affirmation (Β = .22, p = .001), but not on Personal/Moral Homonegativity (Β = −.09, p = .07), indicating that higher levels of spirituality were associated with higher levels of Gay Affirmation. Neither religiosity nor spirituality had a significant direct effect on condom use during RAI in the past 3 months. However, both dimensions of internalized homonegativity, Gay Affirmation (Β = .31, p = .02) and Personal/Moral Homonegativity (Β = .55, p = .005) had a significant direct effect on condom use for RAI, such that higher levels of each were associated with greater frequency of condom use.
Figure 2.
Structural model path diagram for frequency of condom use during receptive anal intercourse with unstandardized path coefficients (n = 263).
Note. IH-PMH = Personal/Moral Homonegativity subscale of the IHNI; IH-GA = Gay Affirmation subscale of the IHNI. *Denotes significance at p < .05, **denotes significance at p < .01.
A test of indirect effects was conducted to determine whether the dimensions of internalized homonegativity mediated the relationships between religiosity, spirituality, and condom use for RAI. Two significant indirect paths were identified: Personal/Moral Homonegativity mediated the relationship between religiosity and condom use during RAI (Β = .08, p = .03), and Gay Affirmation mediated the relationship between spirituality and condom use during RAI (Β = .06, p = .04).
Discussion
Results from the current study indicate that, among AAMSM, religiosity and spirituality influence condom use for both IAI and RAI by means of their differential impact on two dimensions of internalized homonegativity. Higher religiosity was associated with higher reported Personal/Moral Homonegativity scores and lower Gay Affirmation scores in both of the models presented. This association suggests that religious involvement among AAMSM can be a source of sexuality related psychological distress, exacerbating negative personal feelings about sexuality. This connection between religiosity and internalized homonegativity is consistent with the findings of previous research, which have suggested that African American religious communities are often characterized by stigma toward homosexuality (Balaji et al., 2012; Wilkerson, Smolenski, Brady, & Rosser, 2012; Woodyard et al., 2000). Higher spirituality, on the other hand, was associated with higher Gay Affirmation. This association is consistent with the results of previous research, which suggest that spirituality was positively associated with self-esteem and that spirituality can be a source of empowerment for LGBT individuals (Foster, Arnold, Rebchook, & Kegeles, 2011; Tan, 2005). Spirituality was also significantly associated with Personal/Moral Homonegativity, but only in the model for condom use during IAI. These discordant findings suggest that religiosity and spirituality cannot be conceptualized as equivalent constructs, as they may, at times, operate in very different ways. As such, future intervention research should disaggregate religiosity from spirituality to determine whether this consideration enhances intervention effectiveness.
Internalized homonegativity was significantly associated with condom use during both IAI and RAI. However, the two dimensions of internalized homonegativity functioned in a way that was unexpected. Higher Gay Affirmation scores were associated with an increased frequency of condom use for both IAI and RAI, a finding consistent with previous research (Shoptaw et al., 2009). However, higher Personal/Moral Homonegativity scores were also associated with increased frequency of condom use during both IAI and RAI. The latter finding challenges the notion that negative feelings about one’s own homosexuality are associated with higher engagement in risky sexual behaviors (Peterson & Jones, 2009; Stokes & Peterson, 1998). One potential explanation for this finding might be related to stigma- or shame-avoidance strategies. Homosexuality carries a significant stigma among African Americans—a stigma that many AAMSM try to resist or avoid. HIV infection also carries a stigma that is not entirely related to homosexuality. It is possible that AAMSM who feel more homonegative might engage in more frequent condom use to protect themselves from HIV infection and its accompanying stigma. It is also possible that, as more Black churches engage in HIV prevention discourse and become sites of HIV prevention and care activities, the overarching messages of prevention may outweigh the homonegative messages that AAMSM may encounter in these religious spaces. Finally, it is possible that AAMSM have developed resilience that allows them to resist the homonegative messages they may experience. As noted in previous studies, AAMSM use a variety of coping strategies to circumvent the homonegative messages they receive from the church (Jeffries et al., 2008; Miller, 2007; Woodyard et al., 2000). Additional research is needed to understand the complexities of the relationships between internalized homonegativity and engagement in sexual risk behaviors among AAMSM, including whether interventions that consider this relationship are any more effective than interventions that do not.
The structural models presented in this study support the hypothesis that internalized homonegativity mediates the relationships between religiosity, spirituality, and condom use. Personal/Moral Homonegativity mediated the relationship between religiosity and condom use in both the IAI and RAI condom use models, and Gay Affirmation mediated the relationship between spirituality and condom use during RAI. These findings suggest that the African American religious experience, as a sociocultural contextual factor, has some influence on the individual sexual health behaviors of AAMSM by contributing to feelings of internalized homonegativity. As such, HIV prevention efforts should not focus solely on individual-level factors; rather, interventionists should use a more social–ecological approach to address the multilevel structures that exacerbate or ameliorate the likelihood that AAMSM may engage in risky sexual behaviors. Examples of this approach include training programs for clergy or opportunities for AAMSM to discuss their religious and spiritual experiences within the context of HIV prevention interventions.
This study is not without its limitations. The sample used was a convenience sample largely drawn from attendees at Black Gay Pride events. Such events may be more likely to attract participants who identify as gay, bisexual, or same-gender-loving; demonstrate more comfort with their sexuality; and thus be less likely to report higher levels of internalized homonegativity. Future research should aim to recruit a more diverse sample, including AAMSM who would not be as likely to attend a Black Gay Pride or self-identify in their social networks as gay, bisexual, or same-gender-loving. All participants in the study resided in the Deep South at the time of data collection, thus limiting the ability to generalize to the nationwide AAMSM population. This limitation is mitigated by the fact that most African American communities, including institutions such as the Black church, are rooted in the history and culture of the Deep South, so there may be more contextual similarities across regions than for other racial/ethnic groups. In addition, it is possible that there was a literacy bias due to the self-administered nature of the survey; specifically, participants who did not fully comprehend the questions might have been too uncomfortable to ask for clarification. Future studies should confirm that the literacy level of all instruments is appropriate prior to administration.
Because the study was cross-sectional, the causal direction of the pathways specified in the model cannot be determined. This causal model is based on an a priori theory- and evidence-based conceptual model, which supported the model specification. To further validate these conclusions, experimental or observational studies could examine longitudinal changes in the key pathways and outcomes that these models assess. The present study does not take into account the significant variation across African American religious communities. Black churches’ doctrines and policies related to issues of homosexuality vary greatly based on factors such as denomination, leadership, and geographic location (urban vs. rural). Given the promising findings of this study, future research should examine the perceived degree of LGBT affirmation within African American faith communities as a potential moderator of the relationships between religiosity, internalized homonegativity, and condom use.
Despite its limitations, the findings of this study provide insight for future investigation into the determinants of HIV risk for AAMSM. This study is the first to simultaneously examine the relationships between religiosity, spirituality, internalized homonegativity, and condom use among AAMSM. The results indicate that the sociocultural experiences of African American faith communities have the potential to influence AAMSM’s feelings toward their sexuality and, subsequently, their engagement in safer sex behaviors. As such, African American faith communities can be a powerful venue through which HIV prevention messages can be communicated to AAMSM. These results can be used to develop more culturally specific HIV prevention interventions that incorporate the power and value associated with highly regarded, highly influential institutions in African American communities, namely the Black church. Although the results of the present study provide a unique look into the experiences of AAMSM in the Deep South, there are many opportunities to build on this research in order to better understand the factors affecting HIV risk among this disproportionately affected population, and develop nuanced, evidence-based strategies to reduce risk and promote sexual health.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Amola O., Grimmett M. A. (2015). Sexual identity, mental health, HIV risk behaviors, and internalized homophobia among Black men who have sex with men. Journal of Counseling & Development, 93, 236-246. [Google Scholar]
- Ayala G., Bingham T., Kim J., Wheeler D. P., Millett G. A. (2012). Modeling the impact of social discrimination and financial hardship on the sexual risk of HIV among Latino and Black men who have sex with men. American Journal of Public Health, 102(Suppl. 2), S242-S249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balaji A. B., Oster A. M., Viall A. H., Heffelfinger J. D., Mena L. A., Toledo C. A. (2012). Role-flexing: How community, religion, and family shape the experiences of young Black men who have sex with men. AIDS Patient Care and STDs, 26, 730-737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett P. (2007). Structural equation modelling: Adjudging model fit. Personality and Individual Differences, 42, 815-824. [Google Scholar]
- Bentler P. M. (1980). Multivariate analysis with latent variables: Causal modeling. Annual Review of Psychology, 31, 419-456. [Google Scholar]
- Bentler P. M., Bonett D. G. (1980). Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin, 88, 588-606. [Google Scholar]
- Beyrer C., Baral S. D., van Griensven F., Goodreau S. M., Chariyalertsak S., Wirtz A. L., Brookmeyer R. (2012). Global epidemiology of HIV infection in men who have sex with men. Lancet, 380, 367-377. doi: 10.1016/S0140-6736(12)60821-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black AIDS Institute. (2012). Back of the line: The state of AIDS among Black gay men in America, 2012. Los Angeles, CA: Author. [Google Scholar]
- Bollen K. A. (1989). A new incremental fit index for general structural equation models. Sociological Methods & Research, 17, 303-316. [Google Scholar]
- Brown M., Cudek R. (1993). Alternative ways of assessing model fit. In Bollen K., Long J. (Eds.), Testing structural equation models (pp. 136-162). Newbury Park, CA: Sage. [Google Scholar]
- Calhoun-Brown A. (2000). Upon this rock: The Black church, nonviolence, and the civil rights movement. PS: Political Science & Politics, 33, 169-174. [Google Scholar]
- Centers for Disease Control and Prevention. (2015). HIV surveillance report: Diagnoses of HIV infection and AIDS in the United States and dependent areas (Vol. 25). Atlanta, GA: Author. [Google Scholar]
- Collins P. H. (2004). Black sexual politics: African Americans, gender, and the new racism. New York, NY: Routledge. [DOI] [PubMed] [Google Scholar]
- Douglas K. (1999). Sexuality and the Black church: A womanist perspective. Maryknoll, NY: Orbis Books. [Google Scholar]
- Dyson M. (2003). Open Mike: Reflections on philosophy, race, sex, culture and religion. New York, NY: Basic Books. [Google Scholar]
- Ellison C. G., Hummer R. A., Cormier S., Rogers R. G. (2000). Religious involvement and mortality risk among African American adults. Research on Aging, 22, 630-667. [Google Scholar]
- Enders C., Bandalos D. (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling, 8, 430-457. [Google Scholar]
- Fields E. L., Bogart L. M., Smith K. C., Malebranche D. J., Ellen J., Schuster M. A. (2012). HIV risk and perceptions of masculinity among young Black men who have sex with men. Journal of Adolescent Health, 50, 296-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster M. L., Arnold E., Rebchook G., Kegeles S. M. (2011). “It’s my inner strength”: Spirituality, religion and HIV in the lives of young African American men who have sex with men. Culture, Health & Sexuality, 13, 1103-1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullilove M., Fullilove R. (1999). Stigma as an obstacle to AIDS action: The case of the African-American community. American Behavioral Scientist, 42, 1117-1129. [Google Scholar]
- Graham L. F., Aronson R. E., Nichols T., Stephens C. F., Rhodes S. D. (2011). Factors influencing depression and anxiety among Black sexual minority men. Depression Research and Treatment, 2011, 9. doi: 10.1155/2011/587984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin H. (2006). Their own receive them not: African American lesbians and gays in Black churches. Cleveland, OH: Pilgrim Press. [Google Scholar]
- HIV Prevention Trials Network. (2012). HPTN 061 fact sheet. Retrieved from http://www.hptn.org/web%20documents/HPTN061/061FactSheetJan2014.pdf
- Jeffries W., Dodge B., Sandfort T. (2008). Religion and spirituality among bisexual Black men in the USA. Culture, Health & Sexuality, 10, 463-477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin B. A., Husnik M. J., Colfax G., Huang Y., Madison M., Mayer K., . . . Buchbinder S. (2006). Risk factors for HIV infection among men who have sex with men. AIDS, 20, 731-739. [DOI] [PubMed] [Google Scholar]
- Lance C. E., Butts M. M., Michels L. C. (2006). The sources of four commonly reported cutoff criteria: What did they really say? Organizational Research Methods, 9, 202-220. [Google Scholar]
- Lieb S., Prejean J., Thompson D., Fallon S., Cooper H., Gates G., . . . Mallow R. (2011). HIV prevalence rates among men who have sex with men in the southern United States: Population-based estimates by race/ethnicity. AIDS and Behavior, 15, 596-606. [DOI] [PubMed] [Google Scholar]
- Lincoln C., Mamiya L. (1990). The Black church in the African American experience. Durham, NC: Duke University Press. [Google Scholar]
- Little R., Rubin D. (2002). Statistical analysis with missing data (2nd ed.). New York, NY: Wiley-Interscience. [Google Scholar]
- Lugo L., Stencel S., Green J., Smith G., Cox D., Pond A., . . . Ralston M. (2008, February). US religious landscape survey: Religious affiliation: Diverse and dynamic. Paper presented at the Pew Forum on Religion & Public Life Retrieved from http://www.pewforum.org/files/2013/05/report-religious-landscape-study-full.pdf [Google Scholar]
- Malebranche D. (2003). Black men who have sex with men and the HIV epidemic: Next steps for public health. American Journal of Public Health, 93, 862-865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattis J. S. (2000). African American women’s definitions of spirituality and religiosity. Journal of Black Psychology, 26, 101-122. [Google Scholar]
- Mayfield W. (2001). The development of an Internalized Homonegativity Inventory for gay men. Journal of Homosexuality, 41, 53-76. doi: 10.1300/J082v41n02_04 [DOI] [PubMed] [Google Scholar]
- Mays V., Cochran S., Zamudio A. (2004). HIV prevention research: Are we meeting the needs of African American men who have sex with men? Journal of Black Psychology, 30, 78-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller R. L., Jr. (2007). Legacy denied: African American gay men, AIDS, and the Black church. Social Work, 52, 51-61. [DOI] [PubMed] [Google Scholar]
- Millett G., Flores S. A., Peterson J. L., Bakeman R. (2007). Explaining disparities in HIV infection among Black and White men who have sex with men: A meta-analysis of HIV risk behaviors. AIDS, 21, 2083-2091. [DOI] [PubMed] [Google Scholar]
- Millett G., Peterson J., Wolitski R., Stall R. (2006). Greater risk for HIV infection of Black men who have sex with men: A critical literature review. American Journal of Public Health, 96, 1007-1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musgrave C. F., Allen C. E., Allen G. J. (2002). Spirituality and health for women of color. American Journal of Public Health, 92, 557-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L., Muthén B. (2008). Mplus user’s guide. Los Angeles, CA: Author. [Google Scholar]
- Peterson J. L., Jones K. T. (2009). HIV prevention for Black men who have sex with men in the United States. American Journal of Public Health, 99, 976-980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitt R. N. (2010). “Killing the messenger”: Religious Black gay men’s neutralization of anti-gay religious messages. Journal for the Scientific Study of Religion, 49, 56-72. doi: 10.1111/j.1468-5906.2009.01492.x [DOI] [Google Scholar]
- Reif S., Geonnotti K. L., Whetten K. (2006). HIV infection and AIDS in the Deep South. American Journal of Public Health, 96, 970-973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulte L., Battle J. (2004). The relative importance of ethnicity and religion in predicting attitudes towards gays and lesbians. Journal of Homosexuality, 47, 127-142. [DOI] [PubMed] [Google Scholar]
- Schumacker R., Lomax R. (2004). A beginner’s guide to structural equation modeling. Mahwah, NJ: Lawrence Erlbaum. [Google Scholar]
- Shoptaw S., Weiss R., Munjas B., Hucks-Ortiz C., Young S., Larkins S., . . . Gorbach P. (2009). Homonegativity, substance use, sexual risk behaviors, and HIV status in poor and ethnic men who have sex with men in Los Angeles. Journal of Urban Health, 86, 77-92. doi: 10.1007/s11524-009-9372-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivo S. A., Fan X., Witta E. L., Willse J. T. (2006). The search for “optimal” cutoff properties: Fit index criteria in structural equation modeling. Journal of Experimental Education, 74, 267-288. [Google Scholar]
- Smallwood S. W., Spencer S. M., Annang Ingram L., Thrasher J. F., Thompson-Robinson M. V. (2013). Different dimensions: Internalized homonegativity among African American men who have sex with men. Manuscript submitted for publication. [DOI] [PubMed] [Google Scholar]
- Stokes J., Peterson J. (1998). Homophobia, self-esteem, and risk for HIV among African American men who have sex with men. AIDS Education and Prevention, 10, 278-292. [PubMed] [Google Scholar]
- Tan P. P. (2005). The importance of spirituality among gay and lesbian individuals. Journal of Homosexuality, 49, 135-144. [DOI] [PubMed] [Google Scholar]
- Taylor R., Chatters L. M., Brown R. K. (2014). African American religious participation. Review of Religious Research, 56, 513-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker L., Lewis C. (1973). A reliability coefficient for maximum likelihood factor analysis. Psychometrika, 38, 1-10. doi: 10.1007/BF02291170 [DOI] [Google Scholar]
- Underwood L. G. (2006). Ordinary spiritual experience: Qualitative research, interpretive guidelines, and population distribution for the Daily Spiritual Experience Scale. Archive for the Psychology of Religion, 28, 181-218. [Google Scholar]
- Underwood L. G., Teresi J. A. (2002). The Daily Spiritual Experience Scale: Development, theoretical description, reliability, exploratory factor analysis, and preliminary construct validity using health-related data. Annals of Behavioral Medicine, 24, 22-33. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health & Human Services. (2013). National household survey on drug abuse, 1996. Retrieved from http://www.icpsr.umich.edu/icpsrweb/SAMHDA/studies/2391
- Voisin D. R., Bird J. D., Shiu C.-S., Krieger C. (2013). “It’s crazy being a Black, gay youth.” Getting information about HIV prevention: A pilot study. Journal of Adolescence, 36, 111-119. [DOI] [PubMed] [Google Scholar]
- Ward E. (2005). Homophobia, hypermasculinity and the US black church. Culture, Health & Sexuality, 7, 493-504. [DOI] [PubMed] [Google Scholar]
- Wilkerson J. M., Smolenski D. J., Brady S. S., Rosser B. R. S. (2012). Religiosity, internalized homonegativity and outness in Christian men who have sex with men. Sexual and Relationship Therapy, 27, 122-132. doi: 10.1080/14681994.2012.698259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodyard J. L., Peterson J. L., Stokes J. P. (2000). “Let us go into the house of the Lord”: Participation in African American churches among young African American men who have sex with men. Journal of Pastoral Care, 54, 451-460. [DOI] [PubMed] [Google Scholar]
- Worthington E., Wade N., Hight T., Ripley J., McCullough M., Berry J., . . . O’Connor L. (2003). The Religious Commitment Inventory—10: Development, refinement, and validation of a brief scale for research and counseling. Journal of Counseling Psychology, 50, 84-96. [Google Scholar]
- Young S. D., Shoptaw S., Weiss R. E., Munjas B., Gorbach P. M. (2011). Predictors of unrecognized HIV infection among poor and ethnic men who have sex with men in Los Angeles. AIDS and Behavior, 15, 643-649. doi: 10.1007/s10461-009-9653-8 [DOI] [PMC free article] [PubMed] [Google Scholar]