Abstract
The few studies carried out on the effects of Ramadan fasting (RF) on spirometric values present contradictory conclusions. This study aimed at assessing whether RF affects healthy adults’ spirometric values. Twenty-nine nonsmoking healthy males (M ± standard error of mean [SEM] of age: 27 ± 1 years) who fasted during Ramadan (June 29-July 28, 2014) volunteered to the study. Three periods (before-Ramadan [June 23-25], mid-Ramadan [July 14-16] and after-Ramadan [August 11-14]) were selected for spirometry measurements that were consistently performed 5.5 to 3.5 hours (between 15:00 and 17:00 hours) before fasting break. Assessment sessions comprised following: weight (kg), forced vital capacity (FVC), first second expiratory volume (FEV1), FEV1/FVC, peak expiratory flow (PEF), maximal mid expiratory flow (MMEF), and forced expiratory flow rate at the x% of FVC to be exhaled (FEFx%). Spirometric data were expressed in percentages of reference values. Results were analyzed by applying repeated measures analysis of variance. The M ± SEM of weight (before-R: 81.6 ± 2.8 kg, mid-R: 80.8 ± 2.9 kg, after-R: 81.2 ± 2.9 kg), FEV1 (before-R: 99 ± 2%, mid-R: 98 ± 2%, after-R: 98 ± 2%), FVC (before-R: 103 ± 2%, mid-R: 101 ± 2%, after-R: 101 ± 2%), PEF (before-R: 112 ± 3%, mid-R: 113 ± 2%, after-R: 114 ± 3%), MMEF (before-R: 83 ± 3%, mid-R: 83 ± 3%, after-R: 82 ± 3%), FEF25% (before-R: 90 ± 5%, mid-R: 89 ± 6%, after-R: 87 ± 6%), FEF50% (before-R: 94 ± 4%, mid-R: 91 ± 4%, after-R: 93 ± 3%), and FEF75% (before-R: 108 ± 3%, mid-R: 111 ± 2%, after-R:111 ± 3%) were not significantly influenced by RF. To conclude, RF did not bring about any significant changes in the spirometric values of nonsmoking healthy adult males.
Keywords: Ramadan, fasting, adults, lung function, body mass
Introduction
Ramadan fasting (RF) is practiced by about 2.08 billion adult Muslims (Islamic population, n.d; http://www.islamicpopulation.com). It is not abstinence, for 1 month each year from dawn to sunset, only from all types of liquid and solid nutrient intake but also from medication use, smoking, and sexual activities (Bragazzi, 2015).
The evaluation of the effects of RF on human physiology has clinically applicable implications (Bragazzi, 2015; Mughal, 2014). In a globalized society, physicians may be consulted by Muslim patients with chronic diseases such as respiratory disorders who intend or insist on fasting during Ramadan (Al Wakeel et al., 2013). Nevertheless, in healthy subjects, while several studies have observed the effects of RF on body functions, such as weight, biological data (e. g., fluid and electrolyte balance, lipid levels, glucose metabolism, immunity system), sleep, and exercise (Husain, Duncan, Cheah, & Ch’ng, 1987; Margaria, Taglietti, & Agostoni, 1957; Mustafa, Mahmoud, Gumaa, & Gader, 1978; Shepard, Campbell, Martin, & Enns, 1957; Shephard, 2014; Trabelsi, Stannard, Shephard, Jamoussi, & Hakim, 2014), only a few studies have investigated its effects on spirometric data (Abdel-aziz & Ibraheem, 2008; Duncan, Husain, Raman, Cheah, & Ch’ng, 1990; Moosavi, Kabir, Moghimi, Chehrei, & Rad, 2007; Roy & Bandyopadhyay, 2016; Siddiqui, Sabir, & Subhan, 2005; Subhan, Siddiqui, Khan, & Sabir, 2006). The latter studies have some discrepancies in the findings concerning the effects of RF on pulmonary flows and/or volumes of healthy individuals. While some (Abdel-aziz & Ibraheem, 2008; Roy & Bandyopadhyay, 2016) reported that healthy males could tolerate fasting the month of Ramadan without significant alteration in their spirometric data, others (Duncan et al., 1990; Moosavi et al., 2007; Siddiqui et al., 2005; Subhan et al., 2006) reported significant changes in some lung volumes and/or flows. On one hand, some studies reported significant increases in some spirometric data values obtained at mid-Ramadan (mid-R) as compared to those obtained before-Ramadan (before-R; Moosavi et al., 2007) or after-Ramadan (after-R; Siddiqui et al., 2005). On the other, other studies (Duncan et al., 1990; Subhan et al., 2006) reported significant decreases in some forced expiratory flows values obtained at mid-R as compared to those obtained after-R.
The methodology of the above six studies included some issues concerning the study design and spirometric measurements (Ben Saad, 2016; Subhan, 2008). First, readers were faced with a variety of unknown information concerning Ramadan year (Duncan et al., 1990), ambient temperature and relative humidity at the time of spirometric tests (Moosavi et al., 2007; Siddiqui et al., 2005; Roy & Bandyopadhyay, 2016), and the elapsed time between dawn and sunset (Duncan et al., 1990; Moosavi et al., 2007; Roy & Bandyopadhyay, 2016; Siddiqui et al., 2005; Subhan et al., 2006). Second, some confusing factors were noted, such as the inclusion of both sexes (Moosavi et al., 2007) or of some smokers (Duncan et al., 1990). Third, it is unclear if several of the studies (Abdel-aziz & Ibraheem, 2008; Duncan et al., 1990; Siddiqui et al., 2005; Subhan et al., 2006) were adequately powered given the lack of reporting of sample size requirement targets to maximize study power. Fourth, there was a lack of information about previous experience of RF (Abdel-aziz & Ibraheem, 2008; Duncan et al., 1990; Moosavi et al., 2007; Roy & Bandyopadhyay, 2016; Siddiqui et al., 2005; Subhan et al., 2006) or about applied medical questionnaires (Abdel-aziz & Ibraheem, 2008; Duncan et al., 1990; Moosavi et al., 2007; Siddiqui et al., 2005; Subhan et al., 2006). Fifth, some studies failed to provide information on the calibration of spirometric measurements or on the applied spirometric guidelines (Duncan et al., 1990; Moosavi et al., 2007), while several others (Abdel-aziz & Ibraheem, 2008; Moosavi et al., 2007; Roy & Bandyopadhyay, 2016; Subhan et al., 2006) failed to adhere to the 2005 international recommendations for spirometry (Miller et al., 2005). Finally, some other limitations include the application of unknown spirometric norms (Abdel-aziz & Ibraheem, 2008; Moosavi et al., 2007; Roy & Bandyopadhyay, 2016; Siddiqui et al., 2005; Subhan et al., 2006), the absence of reports about the position of subjects during spirometry (Moosavi et al., 2007; Roy & Bandyopadhyay, 2016), and the application of different subject positions such as standing (Duncan et al., 1990) or sitting (Abdel-aziz & Ibraheem, 2008; Siddiqui et al., 2005; Subhan et al., 2006) positions. The factors mentioned above are known to affect respiratory mechanics performance and therefore lead to difficult comparisons of lung function data among published studies (Abdel-aziz & Ibraheem, 2008; Duncan et al., 1990; Moosavi et al., 2007; Roy & Bandyopadhyay, 2016; Siddiqui et al., 2005; Subhan et al., 2006).
In the light of the contradictory conclusions of the above studies (Abdel-aziz & Ibraheem, 2008; Duncan et al., 1990; Moosavi et al., 2007; Roy & Bandyopadhyay, 2016; Siddiqui et al., 2005; Subhan et al., 2006), the present study aims at examining the effects of RF on the spirometric data of healthy never-smoker adult males.
Population and Method
Study Design
The experimental study was performed in the summer of 2014 during the months of Shaaban, Shawwal, and Ramadan 1435 Hijri corresponding to 2014 Gregorian calendar. It was conducted at the Occupational Medicine Group Functional Exploration Laboratory, Sousse, Tunisia. Approval for the study (No. 2602/2014) was obtained from the ethical committee of the Farhat Hached hospital. Written consent was obtained from all study participants. The elapsed time from dawn to sunset was almost 17 hours at the beginning (June 29) and almost 16 hours at the end (July 28). The M ± SD fasting duration was 971 ± 12 minutes. The ambient temperature and humidity M ± SD during the 53-day study period was 33.2°C ± 3.3°C and 68% ± 1%, respectively.
Sample Size
The sample size was estimated according to the following formula (Whitley & Ball, 2002): N = (Zα/2)2 s2/d2, where s is the SD (=0.115 L) and “d” is the accuracy of estimate or how close it is to the true mean (=0.08 L). These two data were collected from a Malay study (Duncan et al., 1990), where the forced vital capacity (FVC) values were 3.82 ± 0.11 L and 3.90 ± 0.12 L, respectively, during mid-R and after-R sessions. Zα/2 (=3.29 at an error rate of 0.1%) is the normal deviate for a two-tailed alternative hypothesis at a level of significance. The estimated sample size gives a total sample of 22 participants (N = 3.292 × 0.1152/0.082 = 22). The assumption of 25% for absence during the second or the third sessions gives a corrected total sample of 29 participants, N = 22/(1.0-0.25).
Study Population
Participants were nonathletic healthy males aged 20 to 40 years. They were recruited among local medical school students and/or their parents or friends, and among friends of the staff involved in the study. At the beginning of the study, a letter of information, containing details about the study and visit dates, was given to the participants.
Exclusion criteria were as follows: history of RF for less than 5 years, any history of smoking, respiratory symptoms (e.g., chronic cough, wheezing, dyspnea), known cardiovascular or pulmonary or neuromuscular chronic diseases, diabetes mellitus, malignancy, vertebral column or thoracic cage abnormalities or chronic medication use, thoracic or abdominal surgery, or lack of cooperation during the spirometry test. In addition, body mass index (BMI) >35 kg/m2, absence during any testing session, and the discovery of an obstructive ventilatory defect were applied as exclusion criteria. Female subjects were not included because Muslim laws forbid them to fast during their menses and because lung function is somewhat lowered during menses (Cotes, Chinn, & Reed, 1997).
Experimental Design, Collected Data, and Applied Definitions
The experimental design consisted of three testing sessions: 1 week before-R (June 23-25), 3 days at mid-R (June 14-16), and 2 weeks after-R (August 11-14). During the before-R session, all participants underwent the modified short version of the American Thoracic Society Medical Questionnaire (Ferris, 1978). The following data were collected: practice of regular physical activity, personal medical or surgical histories, chronic medication use, and smoking history. Then, the following anthropometric data were collected/measured: decimal age (accuracy to 0.1 years); height (±0.01 m) and weight (±0.001 kg) measured with an electronic multifunction scale (Max 21 LCD, Cartagena, 245-2º 2ª. 08025 Barcelona-Spain) with the participants’ shoes removed, heels joined, and their back straight. The participants were in light clothes. The BMI was calculated, and the following definitions were adopted (Tsai & Wadden, 2013): underweight (BMI < 18.5 kg/m2), normal weight (18.5 kg/m2-24.9 kg/m2), overweight (25.0 kg/m2-29.9 kg/m2), and obese (BMI ≥ 30.0 kg/m2). After a 10-minute rest period, participants underwent the spirometry tests in a sitting position (Miller et al., 2005). To avoid the issues of variability due to diverse technicians and devices, only two qualified persons (authors CM and MZC) performed all tests in one spirometer (Micro Medical Limited, Kent, England). The turbine of the spirometer was calibrated daily with a 3-L syringe. The medium spirometry room temperature was ~25°C. The spirometric data—FVC (L), first second forced expiratory volume (FEV1, L), forced expiratory flow when x% of FVC has been exhaled (FEFx%; L/s), MMEF, L/s, PEF, L/s, and FEV1/FVC ratio (absolute value)—were expressed as “body temperature, barometric pressure saturated with water vapor” (Miller et al., 2005). The FVC maneuver has been previously described (Ben Saad et al., 2013). Briefly, at least three reproducible FVC measurements were obtained (Miller et al., 2005). FVC and FEV1, the best two out of the three selected tests, did not differ by more than 150 ml. The highest FVC and FEV1 were computed, even though the two parameters did not come from the same flow-volume curve (Miller et al., 2005). Local spirometric norms were applied (Ben Saad et al., 2013). An obstructive ventilatory defect was defined by a FEV1/FVC ratio <lower limit of normal (Affes, Rekik, & Ben Saad, 2015). During the mid-R and after-R sessions, only anthropometric and spirometric data were measured. All test sessions were performed at the same time of the day, approximately 5.5 to 3.5 hours before sunset (i.e., iftar), when participants could break their fast.
Statistical Analysis
Quantitative parameters were expressed as mean ± standard error of mean (SEM; 95% confidence interval). Comparisons of collected data were made between the before-R, mid-R, and after-R sessions. Results were obtained by applying repeated measures analysis of variance. When appropriate, significant differences between means were tested using the Tukey post hoc test. Analyses were carried out using Statistica software (Statistica Kernel Version 6; StatSoft, Paris, France). Significance was set at the .05 level.
Results
Among the 33 examined participants, only 29 completed all sessions. Reasons for dropout were obstructive ventilatory defect (n = 1) or absence during the second (n = 1) or the third (n = 2) testing sessions. The M ± SEM (95% confidence interval) of their Ramadan experience were 12 ± 1 (range = 11-14 years). Seven participants were normal weight, 15 overweight, and 7 obese. Ambient temperatures were similar during the three sessions (Table 1). However, humidity was significantly lower during the mid-R session compared to the before-R and after-R sessions (Table 1).
Table 1.
Ambient Temperature and Humidity Data and Anthropometric Data of the 29 Healthy Adult Males During the Three Sessions.
| Parameters | Before-R | Mid-R | After-R | p |
|---|---|---|---|---|
| Ambient temperature (°C) | 32.3 ± 5.5 | 32.0 ± 1.0 | 32.7 ± 0.6 | .96 |
| Humidity (%) | 72 ± 2 | 64.0 ± 3.0 | 74.0 ± 2.0 | .006*ac |
| Age (years) | 27.44 ± 1.06 [25.27, 29.61] | 27.50 ± 1.06 [25.33, 29.66] | 27.57 ± 1.06 [25.41, 29.74] | .99 |
| Height (m) | 1.73 ± 0.01 [1.71, 1.76] | 1.73 ± 0.01 [1.71, 1.76] | 1.73 ± 0.01 [1.71, 1.76] | NA |
| Weight (kg) | 81.6 ± 2.84 [75.8, 87.5] | 80.8 ± 2.9 [74.9, 86.7] | 81.2 ± 2.9 [75.3, 87.1] | .98 |
| Body mass index (kg/m2) | 27.1 ± 0.8 [25.5, 28.7] | 26.9 ± 0.8 [25.2, 28.5] | 27.0 ± 0.8 [25.4, 28.6] | .97 |
Note. R = Ramadan; SEM = standard error of mean. Ambient temperature and humidity data are M ± SD. Anthropometric data are M ± SEM [95% confidence interval].
p < .05: analysis of variance between the three sessions data.
p < .05 (Tukey post hoc test): before-R versus mid-R. cp < .05 (Tukey post hoc test): mid-R versus after-R.
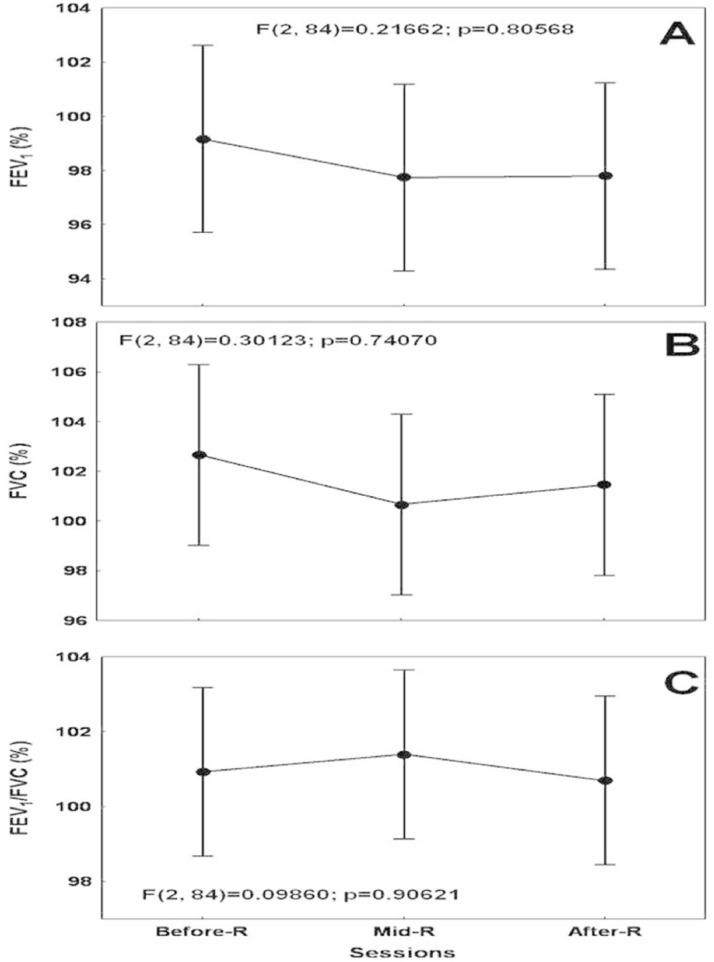
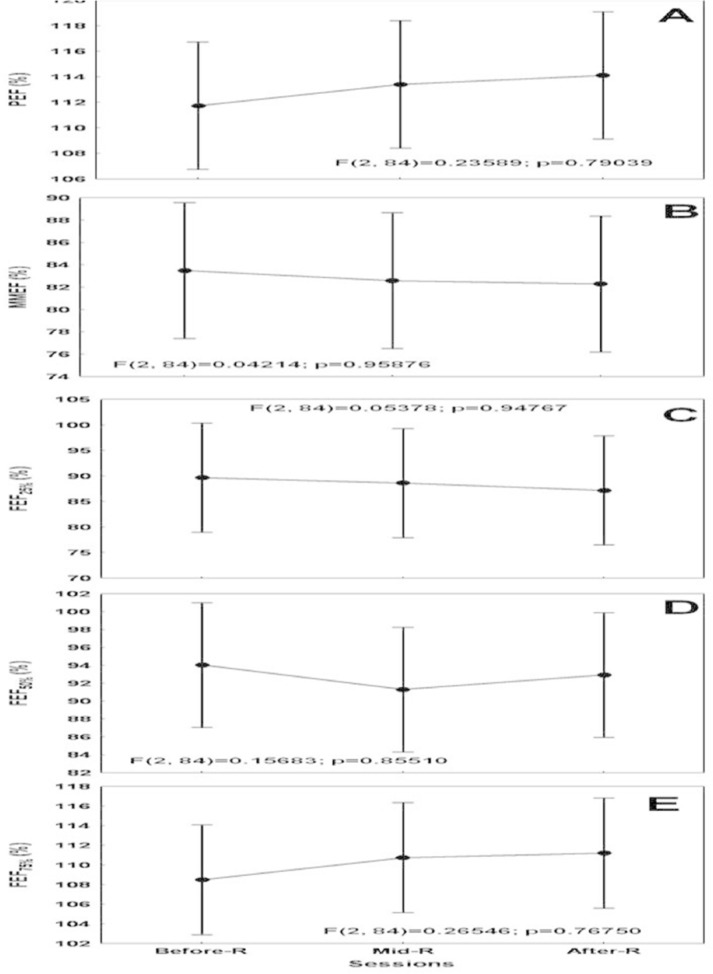
Table 1 presents the anthropometric data of the participants. There was no statistical significant effect of RF on weight (p = .98) or BMI (p = .97). Table 2 presents their spirometric data (expressed in absolute values). Its main conclusion was that RF had no effect on spirometric data. Figures 1 and 2 display their spirometric volumes, ratio, and flows (expressed as a percentage of predicted values). The M ± SEM of FEV1 (before-R: 99 ± 2%, mid-R: 98 ± 2%, after-R: 98 ± 2%), FVC (before-R: 103 ± 2%, mid-R: 101 ± 2%, after-R: 101 ± 2%), FEV1/FVC (before-R: 101 ± 6%, mid-R: 101 ± 6%, after-R: 101 ± 6%), PEF (before-R: 112 ± 3%, mid-R: 113 ± 2%, after-R: 114 ± 3%), MMEF (before-R: 83 ± 3%, mid-R: 83 ± 3%, after-R: 82 ± 3%), FEF25% (before-R: 90 ± 5%, mid-R: 89 ± 6%, after-R: 87 ± 6%), FEF50% (before-R: 94 ± 4%, mid-R: 91 ± 4%, after-R: 93 ± 3%) and FEF75% (before-R: 108 ± 3%, mid-R: 111 ± 2%, after-R: 111 ± 3%) were not significantly influenced by RF.
Table 2.
Spirometric Data (Expressed in Absolute Values) of the 29 Healthy Adult Males During the Three Sessions.
| Parameters | Before-R | Mid-R | After-R | p |
|---|---|---|---|---|
| FEV1 (L) | 4.51 ± 0.12 [4.27, 4.76] | 4.44 ± 0.12 [4.21, 4.68] | 4.44 ± 0.10 [4.23, 4.66] | .89 |
| FVC (L) | 5.40 ± 0.15 [5.10, 5.70] | 5.29 ± 0.14 [5.01, 5.58] | 5.33 ± 0.13 [5.07, 5.59] | .85 |
| FEV1/FVC (absolute value) | 83.79 ± 0.98 [81.79, 85.80] | 84.17 ± 1.01 [82.10, 86.25] | 83.59 ± 0.99 [81.56, 85.61] | .91 |
| PEF (L/s) | 9.86 ± 0.24 [9.37, 10.36] | 10.01 ± 0.21 [9.57, 10.44] | 10.06 ± 0.24 [9.57, 10.56] | .81 |
| MMEF (L/s) | 5.08 ± 0.20 [4.67, 5.49] | 5.02 ± 0.22 [4.57, 5.48] | 5.00 ± 0.22 [4.55, 5.45] | .96 |
| FEF25% (L/s) | 2.45 ± 0.14 [2.15, 2.74] | 2.42 ± 0.17 [2.06, 2.77] | 2.38 ± 0.16 [2.04, 2.71] | .95 |
| FEF50% (L/s) | 5.98 ± 0.26 [5.45, 6.51] | 5.80 ± 0.26 [5.27, 6.33] | 5.90 ± 0.24 [5.41, 6.38] | .88 |
| FEF75% (L/s) | 8.92 ± 0.27 [8.36, 9.47] | 9.10 ± 0.21[8.67, 9.54] | 9.14 ± 0.24 [8.65, 9.63] | .78 |
Note. R = Ramadan; FEV1 = first second forced expiratory volume; FVC = forced vital capacity; PEF= peak expiratory flow; MMEF = maximal mid expiratory flow; FEFx% = forced expiratory flow when x% of FVC has been exhaled; SEM = standard error of mean. Data are M ± SEM (95% confidence interval). p = analysis of variance between the three sessions data.
Figure 1.
The effects of Ramadan fasting on the spirometric volumes and ratio (expressed in percentages of predicted values) of the 29 healthy adult males: (A) FEV1 = first second forced expiratory volume; (B) FVC = forced vital capacity; (C) FEV1/FVC ratio.
Note. R = Ramadan. Data are mean (O) ± 95% confidence interval ( ). p = analysis of variance between the three session.
). p = analysis of variance between the three session.
Figure 2.
The effect of Ramadan fasting on the spirometric flows (expressed in percentages of predicted values) of the 29 healthy adult males: (A) PEF = peak expiratory flow; (B) MMEF = maximal mid expiratory flow; (C) FEF25% = forced expiratory flow when 25% of forced vital capacity (FVC) has been exhaled (FEF25%); (D) FEF50% = forced expiratory flow when 50% of FVC has been exhaled; (E) FEF75% = forced expiratory flow when 75% of FVC has been exhaled.
Note. R = Ramadan. Data are mean (O) ± 95% confidence interval ( ). p = analysis of variance between the three session.
). p = analysis of variance between the three session.
Discussion
RF did not bring about any significant changes in the spirometric data of adult males aged 20 to 40 years. To the best of the authors’ knowledge, only six studies, largely detailed in the Supplementary Data Tables 1 and 2 (available online at http://jmh.sagepub.com/supplemental), have examined the effects of RF on adults’ respiratory mechanics (Abdel-aziz & Ibraheem, 2008; Duncan et al., 1990; Moosavi et al., 2007; Roy & Bandyopadhyay, 2016; Siddiqui et al., 2005; Subhan et al., 2006).
RF Duration and Season
Ramadan, moving ahead ~11 days each year compared to the Gregorian calendar, can take place at any season (Fenneni et al., 2014; Fenneni et al., 2015). The present study was carried out during the summer 2014 when the mean elapsed time from sunrise to sundown was ~17 hours at the start and ~16 hours at the end of Ramadan, with an average ambient temperature and humidity around 32.3°C and 70%, respectively. These circumstances could be judged as relatively hard as temperature was quite hot and participants were expected to fast long hours prior to the spirometry test (13 hours to 14 hours), depending on the time they had their last allowed meal, either before dawn or just before going to bed (Fenneni et al., 2014; Fenneni et al., 2015).
Subjects’ Characteristics
All included adults had an RF history of minimum 5 years, were nonathletes (as reported by the participants themselves), and were never-smokers free from any obstructive ventilatory defect. It is possible, as seen in studies evaluating the effects of RF on exercise performance (Chtourou, Hammouda, Chaouachi, Chamari, & Souissi, 2012), that the participants’ RF history could influence their respiratory adaptations (Fenneni et al., 2015). In addition, the participants’ sports status may interfere with the independent effects of RF on ventilatory mechanics (Cheng et al., 2003). Information about previous experiences with RF or about the subjects’ physical activity status was omitted in previous related studies (Supplementary Data Table 1). Moreover, as seen in a previous study (Duncan et al., 1990), some subjects may have misrepresented their smoking status during eligibility screening.
Sessions Timing and Numbers
Three testing sessions were conducted at the same time of the day. In related studies, the number of testing sessions varied from two to eight, and the test timing was different across studies (Supplementary Data Table 1). These discrepancies make between-studies comparison difficult since time of the day could affect respiratory mechanics (Lewinsohn, Capel, & Smart, 1960).
Spirometric Measurements
Spirometry guidelines were deeply changed in 2005, and currently, it is recommended to apply the latest international recommendations (Miller et al., 2005). Moosavi et al. (2007) have expressed their spirometric data as a percentage of predicted values without reporting the applied spirometric norms. This could lead to a misinterpretation of spirometry data, especially if reference values established on different populations were used (Ben Saad et al., 2013). Currently, it is recommended (Miller et al., 2005) to perform spirometry in a sitting position (Siddiqui et al., 2005; Subhan et al., 2006). Indeed, the standing position, adopted in one study (Duncan et al., 1990), could overestimate spirometric data (Lalloo, Becklake, & Goldsmith, 1991).
In addition to the spirometric data measured in this study, related studies have explored the effect of RF on other lung function data frequently determined in daily practice, such as functional residual capacity, total lung capacity, residual volume, slow vital capacity (SVC), FEV1/SVC ratio, and other data rarely measured in laboratory such as expiratory reserve volume, anatomic dead space volume, maximal voluntary ventilation, FEF75%-85%, and tidal volume (Supplementary Data Table 1).
Effect of RF on Weight
Concerning the before-R and after-R data, there was no significant effect of RF on weight in this group of healthy young adults. Therefore, it seems unlikely that study subjects in this current study were dehydrated. In related studies, confusing results were noted for the effects of RF on weight (Supplementary Data Table 2). While some studies (Duncan et al., 1990; Roy & Bandyopadhyay, 2016) reported no significant change in weight during Ramadan, others identified a significant weight loss during mid-R compared to after-R or before-R periods (Siddiqui et al., 2005; Subhan et al., 2006). In a recent systematic review including 35 studies, it was concluded that RF could result in relatively small but significant weight loss (−1.24 kg; 95% confidence interval: [−1.60, −0.88 kg]) in both sexes, and most of the weight loss was regained within a few weeks after-R (Sadeghirad, Motaghipisheh, Kolahdooz, Zahedi, & Haghdoost, 2014). Additional discussion concerning the effects of RF on weight is added in the supplementary data section.
Effects of RF on Spirometric Data
Numerous animal samples have been designed to evaluate the longtime starvation effect on respiratory mechanic function (Harkema, Mauderly, Gregory, & Pickrell, 1984; Sahebjami & MacGee, 1985), but few human case studies have been conducted on sick (Aaron et al., 2004; Bener et al., 2006; Harkema et al., 1984; Norouzy et al., 2013; Sahebjami & MacGee, 1985; Stenius-Aarniala et al., 2000) or healthy (Abdel-aziz & Ibraheem, 2008; Duncan et al., 1990; Moosavi et al., 2007; Roy & Bandyopadhyay, 2016; Siddiqui et al., 2005; Soori, Mohaghegh, Hajain, & Moraadi, 2016; Subhan et al., 2006) subjects. In 1,590 asthmatic Muslim subjects, the FVC, FEV1, FEV1/FVC, MMEF, and PEF mean values did not identify any statistically significant differences between before-R, mid-R, and after-R sessions (Bener et al., 2006). Other studies have reported improvement in respiratory function following caloric restriction in asthmatics (Stenius-Aarniala et al., 2000) and obese (Aaron et al., 2004) subjects.
Tunisian healthy adult males could tolerate fasting the month of Ramadan without significant alteration of their respiratory system functions (Table 2). This result is similar to that of Egyptian and Indian studies (Abdel-aziz & Ibraheem, 2008; Roy & Bandyopadhyay, 2016), which report that RF did not modify the spirometric flows (PEF, MMEF, FEF75%-85%) or volumes (FEV1, FVC, tidal volume, SVC) or FEV1/FVC ratio (Supplementary Table 2). The four remaining studies performed on healthy subjects (Duncan et al., 1990; Moosavi et al., 2007; Siddiqui et al., 2005; Subhan et al., 2006) presented contradictory conclusions concerning the effects of RF on lung function data. Their results are largely described in Supplementary Table 2. The following sentences will describe changes in some spirometric flows (PEF, FEF75%, FEF75%-85%, FEF50%, and MMEF), volumes (FEV1, FVC), and FEV1/FVC ratio induced by RF.
While PEF was not modified by RF (Siddiqui et al., 2005), it significantly decreased during the second week of Ramadan when compared to the after-R period (Duncan et al., 1990) or increased during the first and the second weeks of Ramadan when compared to the before-R period (Moosavi et al., 2007). While FEF75% significantly decreased at mid-R when compared to the after-R period (Subhan et al., 2006), it significantly increased during the first or the second weeks of Ramadan when compared to the before-R or after-R periods (Moosavi et al., 2007). The study of Subhan et al.(2006) identified a decrease of FEF75% - 85% during mid-R when compared to the after-R period. While FEF50% was not modified by RF (Subhan et al., 2006), it increased during the first and the second weeks of Ramadan when compared to the before- or after-R periods (Moosavi et al., 2007). While MMEF was not modified by RF (Siddiqui et al., 2005), it increased during the first and the second weeks Ramadan when compared to the before-R or after-R periods (Moosavi et al., 2007).
While FEV1 was not modified by RF (Duncan et al., 1990; Siddiqui et al., 2005), it increased during the first and the second weeks of Ramadan when compared to the before-R period (Moosavi et al., 2007). While FVC was not modified by RF (Duncan et al., 1990; Moosavi et al., 2007), it decreased during MR when compared to the before-R and after-R periods (Siddiqui et al., 2005).
While FEV1/FVC ratio was not modified by RF (Duncan et al., 1990; Siddiqui et al., 2005), it increased during the first and the second weeks of Ramadan when compared to the before-R and after-R periods (Moosavi et al., 2007).
Study Limitations
Six limitations should be highlighted. First, the convenience sampling, largely detailed in the supplementary data section, is a major confounding factor (Sousa, Zauszniewski, & Musil, 2004). All subjects were conscious of the study goals, which might raise concern about religious prejudice and then might motivate fasting subjects to carry out harder work in spirometry tests. Second, the noninclusion of a control group could be considered a serious limitation because the internal validity of the findings from these studies and the changes in the variables assessed cannot be attributed solely to RF (Fenneni et al., 2015). In this regard, it has to be highlighted that obtaining nonfasting groups in Muslim majority countries is difficult (Fenneni et al., 2014; Fenneni et al., 2015). Third, the included subjects were free from chronic diseases, although 24% of them had moderate obesity with a BMI ranging from 30 to 35 kg/m2. Subjects with BMI >35 kg/m2 were not included because impaired respiratory function was reported to appear in cases of marked or extreme obesity without any proven pulmonary disease (Dore & Orvoen-Frija, 2002). In addition, 21% of Tunisian adults suffer from obesity (Maatoug et al., 2013), and the included group composition (24% of obese) reflects this “healthy” population as they exist in the real population. This increases the external validity of the study. Fourth, to better evaluate the effects of fasting the whole month of Ramadan, it was preferable to add an additional session, for example, during the last days of Ramadan (Moosavi et al., 2007). Finally, it was preferable to evaluate the hydration status and the dietary regime of included subjects. On one hand, hypohydration causes significant increase in respiratory flow rates because the loss of water from the bronchovascular sheath and airway mucosa potentially decrease the airway resistance (Subhan et al., 2006). On the other, dietary abnormalities adversely affect the lung structure and function, the neural control of breathing, and the functioning of the respiratory muscles (Riley & Thakker-Varia, 1995). To overcome these limitations and improve the quality of data, future research studies may use random sampling, should be conducted more rigorously by systematically including a session performed during the last week of Ramadan. They also should methodically include, whenever possible, a nonfasting control group, and some studies should focus on the effects of RF on the spirometric data of obese adults.
In conclusion, RF did not bring about any significant changes in the spirometric data of adult healthy nonathletic males aged 20 to 40 years fasting during Ramadan.
Supplementary Material
Acknowledgments
Authors wish to express their sincere gratitude to all participants for their cooperation and for the following professors from the Faculty of Medicine of Sousse: Nejib Mrizak, Abdelhamid Garrouch, Monia Zaouali, and Sonia Rouatbi. They also wish to thank Professor Béchir Saadaoui for his invaluable contribution in the improvement of the quality of the writing in the present article.
Footnotes
Authors’ Note: The present research data were previously presented as a poster at the European Respiratory Society International Congress (September 2015, Amsterdam, Holland). First author presenting such data: Imed Latiri. Imed Latiri and Siwar Sandid contributed equally as first authors to this study; Karim Chamari and Helmi Ben Saad contributed equally as senior authors to this study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplementary material is available for this article online.
References
- Aaron S. D., Fergusson D., Dent R., Chen Y., Vandemheen K. L., Dales R. E. (2004). Effect of weight reduction on respiratory function and airway reactivity in obese women. Chest, 125, 2046-2052. [DOI] [PubMed] [Google Scholar]
- Abdel-aziz I., Ibraheem A. (2008). Fasting during Ramadan: Does it alter pulmonary functions in healthy males? Al-Azhar Assiut Medical Journal, 6(3), 53-63. [Google Scholar]
- Affes Z., Rekik S., Ben Saad H. (2015). Defining obstructive ventilatory defect in 2015. Libyan Journal of Medicine, 10, 28946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Wakeel J., Mitwalli A. H., Alsuwaida A., Al Ghonaim M., Usama S., Hayat A., Shah I. H. (2013). Recommendations for fasting in Ramadan for patients on peritoneal dialysis. Peritoneal Dialysis International, 33(1), 86-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben Saad H. (2016). Pulmonary function of young Muslim males during the month of Ramadan: Some points to highlight. American Journal of Men’s Health. Advance online publication. doi: 10.1177/1557988316662840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben Saad H., El Attar M. N., Hadj Mabrouk K., Ben Abdelaziz A., Abdelghani A., Bousarssar M., . . . Rouatbi S. (2013). The recent multi-ethnic global lung initiative 2012 (GLI2012) reference values don’t reflect contemporary adult’s North African spirometry. Respiratory Medicine, 107, 2000-2008. [DOI] [PubMed] [Google Scholar]
- Bener A., Colakoglu B., Mobayed H., El Hakeem A., Al Mulla A. A., Sabbah A. (2006). Does hospitalization for asthma and allergic diseases occur more frequently in Ramadan fasting: A population based study (2000-2004). European Annals of Allergy and Clinical Immunology, 38, 109-112. [PubMed] [Google Scholar]
- Bragazzi N. L. (2015). Ramadan fasting and biological biomarkers: The new opportunities of systems biology and omics sciences. In Chtourou H. (Ed.), Effects of Ramadan fasting on health and athletic performance (pp. 86-90). Retrieved from http://www.esciencecentral.org/ebooks/effects-of-ramadan-fasting/biological-biomarkers.php
- Cheng Y. J., Macera C. A., Addy C. L., Sy F. S., Wieland D., Blair S. N. (2003). Effects of physical activity on exercise tests and respiratory function. British Journal of Sports Medicine, 37, 521-528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chtourou H., Hammouda O., Chaouachi A., Chamari K., Souissi N. (2012). The effect of time-of-day and Ramadan fasting on anaerobic performances. International Journal of Sports Medicine, 33, 142-147. [DOI] [PubMed] [Google Scholar]
- Cotes J. E., Chinn D. J., Reed J. W. (1997). Lung function testing: Methods and reference values for forced expiratory volume (FEV1) and transfer factor (TL). Occupational Environmental Medicine, 54, 457-465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dore M. F., Orvoen-Frija E. (2002). Respiratory function in the obese subject. Revue de Pneumologie Clinique, 58(2), 73-81. [PubMed] [Google Scholar]
- Duncan M. T., Husain R., Raman A., Cheah S. H., Ch’ng S. L. (1990). Ventilatory function in Malay Muslims during normal activity and the Ramadan fast. Singapore Medical Journal, 31, 543-547. [PubMed] [Google Scholar]
- Fenneni M. A., Latiri I., Aloui A., Rouatbi S., Chamari K., Ben Saad H. (2015). Critical analysis of the published literature about the effects of Ramadan intermittent fasting on healthy children’s physical capacities. Libyan Journal of Medicine, 10, 28351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenneni M. A., Latiri I., Aloui A., Rouatbi S., Saafi M. A., Bougmiza I., . . . Ben Saad H. (2014). Effects of Ramadan on physical capacities of North African boys fasting for the first time. Libyan Journal of Medicine, 9, 25391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferris B. G. (1978). Epidemiology Standardization Project (American Thoracic Society). American Review of Respiratory Disease, 118(6 Pt 2), 1-120. [PubMed] [Google Scholar]
- Harkema J. R., Mauderly J. L., Gregory R. E., Pickrell J. A. (1984). A comparison of starvation and elastase models of emphysema in the rat. American Review of Respiratory Disease, 129, 584-591. [PubMed] [Google Scholar]
- Husain R., Duncan M. T., Cheah S. H., Ch’ng S. L. (1987). Effects of fasting in Ramadan on tropical Asiatic Moslems. British Journal of Nutrition, 58(1), 41-48 [DOI] [PubMed] [Google Scholar]
- Lalloo U. G., Becklake M. R., Goldsmith C. M. (1991). Effect of standing versus sitting position on spirometric indices in healthy subjects. Respiration, 58, 122-125. [DOI] [PubMed] [Google Scholar]
- Lewinsohn H. C., Capel L. H., Smart J. (1960). Changes in forced expiratory volumes throughout the day. British Medical Journal, 1(5171), 462-464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maatoug J., Harrabi I., Hmad S., Belkacem M., Nouira A., Ghannem H. (2013) Advising obese adults about diet and physical activity in Sousse, Tunisia. International Scholarly Research Notices: Obesity, 21, 498527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margaria R., Taglietti A., Agostoni E. (1957). Indirect determination of respiratory dead space and mean alveolar air composition. Journal of Applied Physiology, 11, 235-240. [DOI] [PubMed] [Google Scholar]
- Miller M. R., Hankinson J., Brusasco V., Burgos F., Casaburi R., Coates A., . . . Wanger J. (2005). Standardisation of spirometry. European Respiratory Journal, 26, 319-338. [DOI] [PubMed] [Google Scholar]
- Moosavi S. A., Kabir A., Moghimi A., Chehrei A., Rad M. B. (2007). Evaluation of the effect of Islamic fasting on lung volumes and capacities in the healthy persons. Saudi Medical Journal, 28, 1666-1670. [PubMed] [Google Scholar]
- Mughal F. (2014). Ramadan: What it means for general practice. British Journal of General Practice, 64(624), 356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustafa K. Y., Mahmoud N. A., Gumaa K. A., Gader A. M. (1978). The effects of fasting in Ramadan. 2. Fluid and electrolyte balance. British Journal of Nutrition, 40, 583-589. [DOI] [PubMed] [Google Scholar]
- Norouzy A., Karimirad R., Sabety Baygi Z., Amini M., Attaran D., Mohajeri S. M. R., . . . Nematy M. (2013). Effects of Ramadan fasting on spirometric values and clinical symptoms in asthmatic patients. Journal of Fasting and Health, 1(1), 23-27. [Google Scholar]
- Riley D. J., Thakker-Varia S. (1995). Effect of diet on lung structure, connective tissue metabolism and gene expression. Journal of Nutrition, 125(6 Suppl.), 1657S-1660S. [DOI] [PubMed] [Google Scholar]
- Roy A., Bandyopadhyay A. (2016). Pulmonary function of young Muslim males during the month of Ramadan. American Journal of Men’s Health. Advance online publication. doi: 10.1177/1557988316643292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeghirad B., Motaghipisheh S., Kolahdooz F., Zahedi M. J., Haghdoost A. A. (2014). Islamic fasting and weight loss: A systematic review and meta-analysis. Public Health Nutrition, 17, 396-406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahebjami H., MacGee J. (1985). Effects of starvation on lung mechanics and biochemistry in young and old rats. Journal of Applied Physiology, 58, 778-784. [DOI] [PubMed] [Google Scholar]
- Shepard R. H., Campbell E. J., Martin H. B., Enns T. (1957). Factors affecting the pulmonary dead space as determined by single breath analysis. Journal of Applied Physiology, 11, 241-244. [DOI] [PubMed] [Google Scholar]
- Shephard R. J. (2014). Maintaining fluid balance during day fasting in the month of Ramadan. In Chtourou H. (Ed.), Effects of Ramadan fasting on health and athletic performance (pp. 117-126). Retrieved from http://www.esciencecentral.org/ebooks/effects-of-ramadan-fasting/maintaining-fluid-balance.php
- Siddiqui Q. A., Sabir S., Subhan M. M. (2005). The effect of Ramadan fasting on spirometry in healthy subjects. Respirology, 10, 525-528. [DOI] [PubMed] [Google Scholar]
- Soori M., Mohaghegh S., Hajain M., Moraadi B. (2016). Effects of Ramadan fasting on inspiratory muscle function. Asian Journal of Sports Medicine, 15, e35201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sousa V. D., Zauszniewski J. A., Musil C. M. (2004). How to determine whether a convenience sample represents the population. Applied Nursing Research, 17, 130-133. [PubMed] [Google Scholar]
- Stenius-Aarniala B., Poussa T., Kvarnstrom J., Gronlund E. L., Ylikahri M., Mustajoki P. (2000). Immediate and long term effects of weight reduction in obese people with asthma: Randomised controlled study. British Medical Journal, 320, 827-832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subhan M. M. (2008). Evaluation of the effect of Islamic fasting on lung volumes and capacities in healthy persons. Saudi Medical Journal, 29, 626. [PubMed] [Google Scholar]
- Subhan M. M., Siddiqui Q. A., Khan M. N., Sabir S. (2006). Does Ramadan fasting affect expiratory flow rates in healthy subjects? Saudi Medical Journal, 27, 1656-1660. [PubMed] [Google Scholar]
- Trabelsi K., Stannard S., Shephard R., Jamoussi K., Hakim A. (2014). Body composition, hematological and biochemical modifications during Ramadan fasting. In Chtourou H. (Ed.), Effects of Ramadan fasting on health and athletic performance (pp. 108-116). Retrieved from http://www.esciencecentral.org/ebooks/effects-of-ramadan-fasting/body-composition.php
- Tsai A. G., Wadden T. A. (2013). In the clinic: Obesity. Annals of Internal Medicine, 159(5), ITC3-1-ITC3-15. [DOI] [PubMed] [Google Scholar]
- Whitley E., Ball J. (2002). Statistics review 4: Sample size calculations. Critical Care, 6, 335-341. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.