Abstract
Proper diagnosis is a first step in applying best available treatments, and prognosticating outcomes for clients. Currently, the majority of musculoskeletal diagnoses are classified according to pathoanatomy. However, the majority of physical therapy treatments are applied toward movement system impairments or pain. While advocated within the physical therapy profession for over thirty years, diagnostic classification within a movement system framework has not been uniformly developed or adopted. We propose a basic framework and rationale for application of a movement system diagnostic classification for atraumatic shoulder pain conditions, as a case for the broader development of movement system diagnostic labels. Shifting our diagnostic paradigm has potential to enhance communication, improve educational efficiency, facilitate research, directly link to function, improve clinical care, and accelerate preventive interventions.
Keywords: Diagnosis, Movement System, Physical Therapy
INTRODUCTION
As health care providers, we seek to provide the best possible care to clients who seek our counsel. To do so, we need to provide the “right treatment to the right patient at the right time”.1 Optimally, we evaluate our clients and use “best available evidence”2,3 to determine the “right” intervention. In musculoskeletal care, this process has traditionally relied upon pathoanatomic diagnostic labels. However, as physical therapists, we focus on treating movement impairments, consistent with our professional vision and identity in the movement system.4,5 Subsequently, there is a disconnect between our diagnostic and treatment process.6,7 This manuscript will advocate that in order to advance best possible care and preventive interventions, our diagnostic paradigm needs to shift to a movement system diagnostic classification approach.8 While a uniformly agreed upon and proven movement system diagnostic classification does not currently exist, we present a framework to develop and test such an approach using examples of clients presenting with atraumatic shoulder pain. Our proposal is not presented as the definitive “answer” to our collective diagnostic dilemma.8,9 We firmly believe development of the most effective movement based diagnostic classification will rely upon an interdisciplinary collaborative process, with ongoing refinement. We hope this manuscript will assist in advancing that process.
WHY CLASSIFY?
In considering such a diagnostic paradigm shift, we first must consider why we classify clients in the first place. Why not treat each client individually? There are many benefits to classifying signs and symptoms across individuals. These include best directing our interventions toward common patterns of clinical presentation; understanding the prognosis; communicating with clients, amongst the health care team, and with third parties; influencing reimbursement models; and creating homogenous groups for research investigations and clinical practice guidelines.6–8
There are many potential classification schemes for use in grouping clients. For instance, we can categorize by region of symptoms (e.g. shoulder, low back, or knee), duration of symptoms (acute, subacute, or chronic), or level of tissue irritability (high, moderate, low).10 A diagnostic classification is often presumed to provide utility in determining causation, guiding treatment decisions, and/or prognosticating about a condition.6,11 “Diagnosis may be defined as the determination of the cause or nature of an illness by evaluation of the signs, symptoms and supportive tests in an individual patient.” “Diagnostic criteria are a set of signs, symptoms, and tests for use in routine clinical care to guide the care of individual patients”.12 An ideal diagnostic classification would incorporate adequate, but not excessive specificity. As such, clinical interventions could be tested and clinical practice and prognostic guidelines could be developed and refined within homogenous groups. Some amount of treatment individualization will always need to occur with each unique client, while still allowing an overall treatment approach to be developed and tested from a set of diagnostic labels.
TRADITIONAL PATHOANATOMIC DIAGNOSTIC MODEL
The most common diagnostic labeling for musculoskeletal conditions attempts to identify a specific tissue pathology that is presumed to be the source or cause of the client's pain or dysfunction (i.e. pathoanatomy). For the shoulder, diagnostic terms such as rotator cuff tendinopathy, full thickness rotator cuff tears, or labral tears are frequently utilized. The gold standard for verifying these conditions is medical imaging (MRI, x-ray, etc.) and/or surgical confirmation.13,14 In typical clinical practice, however, practitioners often rely heavily on “special tests” or “pain provocation tests” to theoretically confirm the underlying presence of a tissue pathology, and that tissue's role as a pain generator or source of the symptoms. Some immediate challenges with a pathoanatomic model include the high cost of diagnostic imaging, limited validity and reliability of special tests,15–17 and the frequency with which pathoanatomy is found in asymptomatic patients.18–22
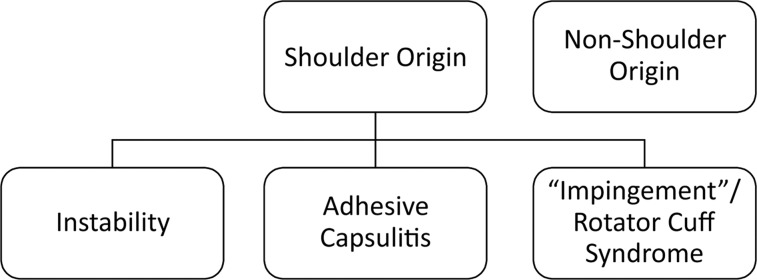
As a specific example of the pathoanatomic model, the three most common diagnostic labels for shoulder conditions are depicted in Figure 1. In particular, shoulder impingement or rotator cuff syndrome is the most commonly assigned diagnostic label in individuals presenting with shoulder pain, but may also be termed rotator cuff disease, subacromial impingement, or subacromial pain syndrome.23–27 The generally accepted clinical confirmation of shoulder impingement syndrome is pain with one or more impingement tests (Hawkins/Kennedy, Neer, etc.), a painful arc of motion when raising the arm, and pain or weakness with resisted external rotation.10,28,29
Figure 1.
The three most common diagnostic classifications of shoulder pain in the traditional pathoanatomic model, after ruling out conditions not of shoulder origin (e.g. cervical referred pain).
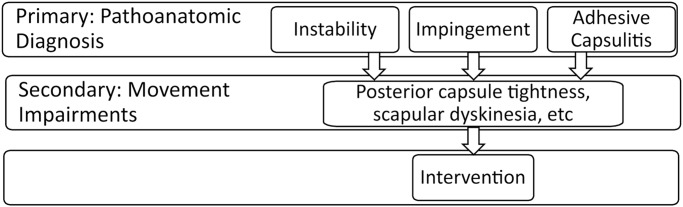
Additional challenges exist within this pathoanatomic diagnostic framework. First, many of the specific pathoanatomical findings co-exist. As such, distinguishing a labral tear from rotator cuff disease, or distinguishing rotator cuff tendinopathy from a partial thickness rotator cuff tear, for example, may not be possible, or even important with regard to treatment planning. Second, even presuming the clinician reaches a valid pathoanatomic diagnostic conclusion, these diagnostic labels have limited ability to direct selection of interventions.10 This is in part because rotator cuff disease, for example, is associated with multifactorial etiology and a wide variety of movement system impairments.30–32 Further, the presence of tissue pathology is often not the source of the client's pain. Consequently, it is not beneficial to look to the literature evidence for the “five best exercises” to most effectively treat rotator cuff tendinopathy. As physical therapists, even when we have a pathoanatomic diagnosis in hand, we still need to examine the patient for the associated movement impairments that may contribute to their condition and that are appropriate for physical therapy intervention (Figure 2).10,31 For example, one individual might have posterior shoulder tightness as a primary movement impairment leading to their rotator cuff tendinopathy,33,34 while another individual might have glenohumeral microinstability as their primary contributing movement impairment.35 These differing contributing factors require different treatments. The traditional pathoanatomic approach treats these movement impairments as secondary to the pathoanatomic diagnosis, when in fact the movement factors are most often the primary drivers of treatment decisions.31,36
Figure 2.
Depiction of the typical flow of the diagnostic process in the traditional pathoanatomic framework. First a pathoanatomic diagnosis would be determined or confirmed using clinical examination findings with or without additional diagnostic imaging. Subsequently, additional examination for associated movement impairments is still needed prior to identifying the best evidence intervention. The three most common pathoanatomic diagnostic categorizations are presented, as well as two examples of potentially related movement impairments.
But perhaps an even more important limitation with pathoanatomic diagnoses is that, when present, the pathoanatomy often results from “wear and tear” or “overuse” through repeated exposure to tissue stresses and microtrauma over time. For example, a recent meta-analysis suggests substantially increased incidence of shoulder pain at follow-up in asymptomatic overhead athletes prospectively identified with scapular dyskinesis.37 Clinical practitioners aim to target treatments to the cause of a condition as early as possible in its development to facilitate optimal healing and minimize further progression. The pathoanatomic model, which focuses on the effects of stresses on tissues rather than the causative factors, is therefore limited in its power for early detection or ideally prevention of a condition.
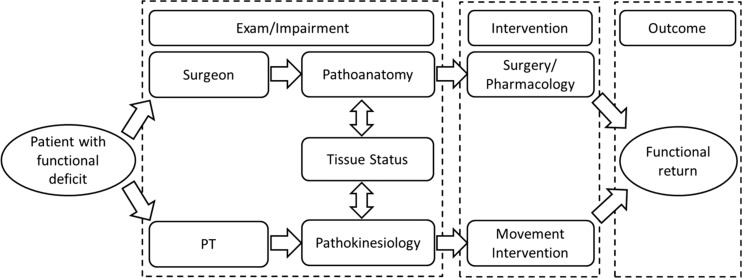
Despite these limitations, one of the most common arguments for retaining the pathoanatomic model as the diagnostic framework is that this is the existing physician model. Some argue creating a new and unfamiliar diagnostic framework will impair communication with physicians and other healthcare providers. However in the case of the most common shoulder diagnosis, “impingement”, surgical specialists are advocating for doing away with this diagnostic label.27,38,39 The rationale for this advocacy is that the use of the impingement label has become so broadly applied as to limit its ability to effectively direct treatment. In effect, the impingement diagnosis has become a diagnosis of exclusion of other primary related diagnoses (cervical radiating pain, adhesive capsulitis, glenohumeral instability).40 Once these other disorders are ruled out, nearly all patients with anterior/lateral shoulder pain complaints are diagnosed with “impingement” or related rotator cuff diagnostic labels.40 Further, the “impingement” label typically implies anatomic causation to surgeons (specifically anterior acromial), while the same diagnosis typically implies movement causation to physical therapists.39,41 (Figure 3). As such, we are using the same label but with different meaning, confounding rather than enhancing communication. We should seize the opportunity the proposed shift in labeling brings in order to also shift the underlying framework from which we make our diagnostic decisions.
Figure 3.
Depiction of similarities and differences in how an orthopaedic surgeon and a physical therapist may evaluate and treat the same client. Each provider's evaluation will focus on the respective area they are able to treat (surgeon - pathoanatomy; physical therapist – pathokinesiology). Both professions are interested in the presence or absence of various tissue pathologies, but from a differing perspective. Both professions are directed toward assisting the client to obtain the best possible functional outcome.
PATHOKINESIOLOGIC OR KINESIOPATHOLOGIC MODEL: MOVEMENT SYSTEM MODEL
An alternate framework to the pathoanatomic diagnostic classification is a pathokinesiologic or kinesiopathologic model.5,6 This model creates a diagnostic classification related to the characteristic movement impairments that are the cause of, or consequence of, the client's pain or dysfunction. This classification then leads directly to the intervention approach (i.e. treating these movement impairments), and can be considered a movement system model. A presumption with this movement system model is that there will be a stronger relationship to function and better integration with the International Classification of Functioning, Disability and Health (ICF) model as compared to the weaker relationships between function and pathoanatomy.7 This movement system model framework does not presume or preclude any specific tissue pathology. The movement system model continues to recognize the importance of pathoanatomy to our clinical decision-making, but instead treats it as a modifier rather than the overarching categorization of primary interest (Figure 3). The movement system framework also does not preclude psychosocial components to a condition. For example, if a client has reduced scapular upward rotation, glenohumeral subluxation, and shoulder pain secondary to a stroke, we treat the movement impairments, but are informed by the neurophysiologic and psychosocial impacts of the stroke.
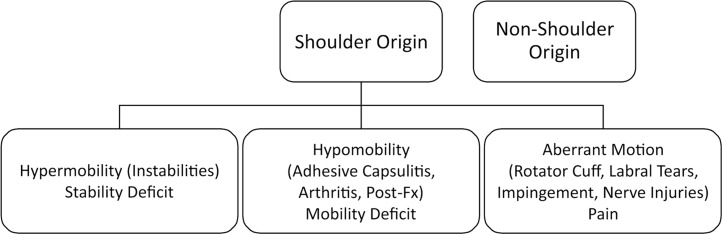
When referring back to the three most common shoulder diagnoses (Figure 1), these three categories can be renamed in the movement system framework as depicted in Figure 4. In essence, instability was really already a movement system based diagnosis. This category can be thought of as either a hypermobility or a stability deficit. Clients in this category are moving too much at the joint. Secondly, the distinguishing clinical characteristic of adhesive capsulitis is a primary equivalent loss of both active and passive glenohumeral joint motion. This category can be thought of as either a hypomobility, or a mobility deficit. Clients in this category are moving too little at the joint. Within a movement framework, we can also include other pathoanatomic conditions in this hypomobility category with the same characteristic motion loss, including glenohumeral osteoarthritis or post-fracture stiffness. Finally, clients in the “impingement” categorization can be labeled as moving abnormally, with some moving too much, some too little, and others with aberrant or discoordinated movement. As with the hypomobility category, we can expand the pathoanatomic conditions that might present in this motion category beyond just the rotator cuff to include long head biceps tendinopathy, subacromial bursitis, or labral tearing (Figure 4).
Figure 4.
Three proposed broad classifications of shoulder pain following a movement system diagnostic framework, after ruling out conditions not of shoulder origin.
At this stage of our classification (three main groups), many clients would end up in the same initial broad categorization based on clinical examination using either the pathoanatomic or the pathokinesiologic framework. However, there are a number of advantages to the movement system based framework. First, the overall treatment goals are derived directly from the diagnostic category: improve functional stability in clients in the hypermobility category; improve functional mobility in clients in the hypomobility category; and improve functional movement coordination or balance of mobility and stability in clients in the aberrant motion category. We would not apply treatments to gain mobility with a client with hypermobility and so forth. This framework further prioritizes the movement in the classification system, and also in the diagnostic process. A movement examination assessing both quality and quantity of movement follows directly from the patient history. Special tests to identify tissue pathology are best used more selectively to potentially modify the intervention approach and inform prognosis and/or coordination of care after identifying a movement classification. Because the movement system is the focus of the diagnosis, there are no issues with scope of practice,5–7 and no over reliance on expensive medical imaging.
PROPOSED SHOULDER MOVEMENT BASED CLASSIFICATION OF GREATER SPECIFICITY
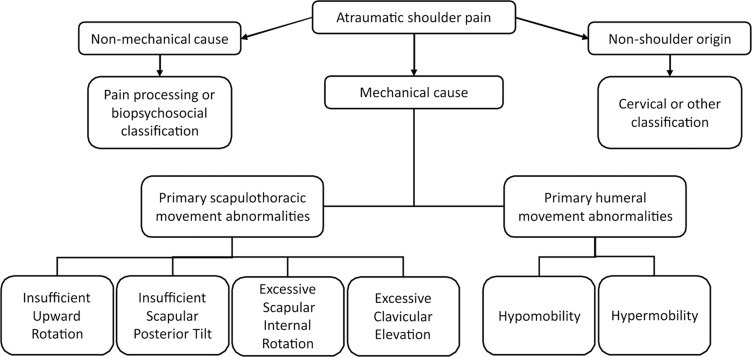
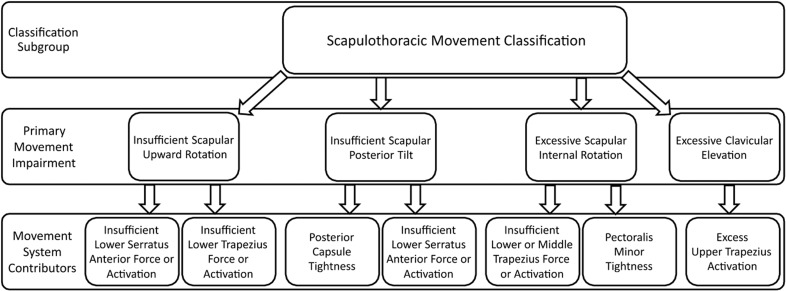
In either model, we still need to drill down from these broad overarching categories to a level of specificity that can more effectively direct treatment. However, doing so from the movement system framework results in a logical and consistent flow starting immediately from the initial diagnostic classification. First, the patient's chief complaint related to stability, mobility, or pain with movement provides a broad classification that begins to direct our treatment (Figure 4). Subsequently, a movement examination informed by the subjective reports results in pattern recognition related to a primary movement pattern contributing to the client's pain or dysfunction (Figure 5). In our proposed framework, non-mechanical or unrelated causes (cervicogenic, cardiac conditions) of shoulder pain are ruled out, and primary glenohumeral impairments are distinguished from scapulothoracic impairments. Subtypes of each primary movement impairment are then considered. From this primary movement impairment pattern, we proceed with additional tests and measures to determine primary movement system contributors such as tissue flexibility, muscle strength, coordination, etc (Figures 6 and 7). Finally, we assess for important pathoanatomic contributors, such as a tissue tear, nerve injury, or tissue restriction. In practice, this process will likely be non-linear, with the results of each step supporting or refuting the suspected diagnosis, and dynamically guiding the clinician's examination.
Figure 5.
Proposed classification of primary patterns of movement impairments. Clients may present with shoulder pain of non-mechanical or non-shoulder origin, requiring alternate classification. Within those with symptoms or dysfunction of mechanical origin, glenohumeral or scapulothoracic subtypes are distinguished. Further specificity is provided for the scapulothoracic subtypes. It is recognized that multiple movement impairments may be present and the classification is based on the movement impairment pattern believed most relevant to the client's presentation.
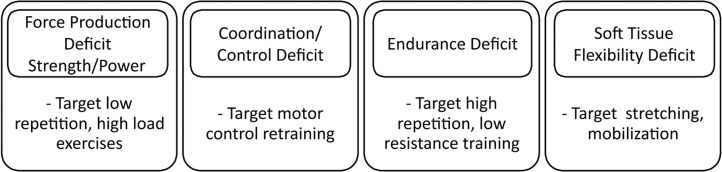
Figure 6.
Additional classification of potential movement impairment contributors to a condition, and subsequent targeted treatment approaches that may follow.
Figure 7.
Depiction of potential movement system impairments to be assessed following from identification of primary movement pattern abnormalities. These impairments if present would lead directly to treatment planning decisions.
With regard to the shoulder, Figure 5 presents common movement patterns recognized in a number of previously described classifications31,42,43 (Joe Godges, DPT, MA, OCS, personal communication). These patterns are not typically present in isolation. For instance, insufficient scapular upward rotation is often associated with glenohumeral hypermobility 44,45 and excess scapular internal rotation and insufficient scapular posterior tilt may occur in combination.32 A classification is not determined based on simply the presence of an isolated movement impairment, but instead on the collective history and physical examination, including assistance or symptom relief tests 6,31,46 as well as pain provocation tests. Clinical judgement is used to assimilate the collective examination findings in determining which classification is most representative of the client's movement system dysfunction. Figure 7 illustrates that from a movement classification, a clinician can further assess for the associated movement system impairments that would be the focus of a treatment intervention. These representations are not considered all-inclusive or complete, but provide a representation of a framework that can be further investigated and discussed. For the scapulothoracic deviations, these patterns can be thought of as representing movement dysfunction in each of the three planes (sagittal - scapular tilting; frontal - clavicle elevation or scapular downward rotation; transverse - scapular internal rotation). This consideration may help structure the evaluation process, as well as education of new clinicians in performing the evaluation (Joe Godges DPT, MA, OCS, personal communication).
LIMITATIONS OF THE MOVEMENT SYSTEM FRAMEWORK
The movement system framework is not without limitations that need to be addressed. It will require research investigation to determine and confirm reliable, valid, and useful categorizations within the movement system framework, and the necessary associated clinical diagnostic tests and measures. Investigation of utility should be broad ranging, including impact on client short- and long-term outcomes, cost-effectiveness, efficiency of the diagnostic and treatment process, and efficiency of the educational process. There will also need to be additional discussion surrounding the most appropriate labels for each diagnostic category. The American Physical Therapy Association (APTA) has endorsed the following criteria for use with a movement system diagnostic classification.47
1) Use recognized movement-related terms to describe the condition or syndrome of the movement system;
2) Include, if deemed necessary, the name of the pathology, disease, disorder, anatomical or physiological terms, and stage of recovery associated with the diagnosis.
3) Be as succinct and direct as possible to improve clinical usefulness.
4) Strive for movement system diagnoses that span all populations, health conditions, and the lifespan. Whenever possible, use similar movement-related terms to describe similar movements, regardless of pathology or other characteristics of the patient or client.
As this framework is developed, this type of nomenclature will require reworking the diagnostic and therapeutic algorithm for clinical practitioners and developing new curricula not only for those in practice, but also for those who educate the next generation of clinicians. However, the direct flow from movement diagnosis, to assessment of movement impairments, to targeted intervention (Figures 5 and 7) can improve the efficiency of the educational process and advancement toward clinical expertise.
This framework is presented with a musculoskeletal shoulder example, but other health conditions can be described in a similar manner. For instance, in a client who has experienced a stroke, classifying the movement presentation will inform the appropriate rehabilitation intervention more directly than classifying the location or size of the brain lesion. Furthermore, there will be a need for linkage to traditional pathoanatomic diagnoses since billing, historical research, and clinician communication are difficult to change. This idea is consistent with criteria #2 listed above. The issue is whether we emphasize the movement system impairments during these communications and how we choose to diagnose and treat our patients.
Lastly, this framework as presented focuses on mechanical pain and dysfunction. As noted in Figure 5, some clients may best fit a biopsychosocial or pain processing classification system in the absence of identifiable mechanical contributors. In addition, it is always important to consider psychosocial and pain processing factors when determining the most appropriate diagnostic classification and treatment approach, even with a primary mechanical contributor. Additional research is required to fully investigate relationships between movement impairments and pain and function.
IS THERE MULTI-DISCIPLINARY UTILITY IN A MOVEMENT SYSTEM DIAGNOSTIC CLASSIFICATION?
When originally envisioned, it was thought that a movement system diagnostic framework would be primarily utilized by physical therapists given their movement system identity and expertise. Figure 3 illustrates that in evaluating the same client, a surgeon may focus their exam more on the pathoanatomy, because surgical interventions can modify the pathoanatomy. Physical therapists focus their exam more on the pathokinesiology because rehabilitation interventions can modify the movement system impairments and movement stresses. Both are interested in tissue pathology but from different perspectives. Both are interested in the best functional outcomes for the patients, but each profession has unique treatment “tools”. As such, it might seem that surgeons would continue to use specific pathoanatomic classifications,27 while therapists might more frequently use a movement system diagnostic classification.
However, at least at the broad categorical level (Figure 4) there is likely substantial multi-disciplinary utility for musculoskeletal conditions. Considering if a condition is predominantly a joint hyper- or hypo-mobility helps to drive appropriate surgical procedure decisions as well as non-surgical rehabilitation. Further, if the origin of the presenting pathoanatomy is based on an abnormal movement causation, a movement classification can be particularly beneficial in treatment planning. Other non-surgical health care providers responsible for first line patient care (physiatrists, family practice physicians, nurse practitioners, physician's assistants, etc) may also have interest in a movement system diagnostic classification as it relates to appropriate referral and preventive interventions.
As mentioned earlier, clear communication between clinicians is paramount for best patient care. Even so, there remain examples where something as simple as the definition of the same diagnostic label (e.g. “impingement”) differs from profession to profession. Consequently, standardized diagnostic labels would facilitate communication between providers. As a result, we advocate that these movement system diagnostic labels be developed to enhance communication. When developed, they will benefit patients by making communication between all parties easier and more consistent.
CONCLUSION
In conclusion, we advocate that development of movement system based diagnostic classifications for health conditions will benefit health care provision, outcomes, education, communication, and preventive interventions. As a profession, we are slow in advancing the legacy first put forth over 30 years ago.6,8,9 With regard to utility of diagnostic classification, we believe improved classifications will evolve from rigorous scientific testing and the test of time - i.e. “the proof of the pudding is in the eating”. As such, it is time to work in earnest toward advancing a movement system diagnostic framework.
REFERENCES
- 1.Haldorsen EMH. The right treatment to the right patient at the right time. Occup Environ Med. 2003;60(4):235-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manske RC Lehecka BJ. Evidence - based medicine/practice in sports physical therapy. Int J Sports Phys Ther. 2012;7(5):461-473. [PMC free article] [PubMed] [Google Scholar]
- 3.Cleland JA Noteboom JT Whitman JM, et al. A primer on selected aspects of evidence-based practice relating to questions of treatment. Part 1: asking questions, finding evidence, and determining validity. J Orthop Sports Phys Ther. 2008;38(8):476-484. [DOI] [PubMed] [Google Scholar]
- 4.American Physical Therapy Association. Physical Therapist Practice and the Movement System. An American Physical Therapy Association White Paper. 2015 https://www.apta.org/MovementSystem/WhitePaper/. Published 2015.
- 5.Sahrmann S. The human movement system: our professional identity. Phys Ther. 2014;94(7):1034-1042. [DOI] [PubMed] [Google Scholar]
- 6.Sahrmann S. Diagnosis by the physical therapist-a prerequisite for treatment. A special communication. Phys Ther. 1988;68(11):1703-1706. [DOI] [PubMed] [Google Scholar]
- 7.Ludewig PM Lawrence RL Braman JP. What's in a name? Using movement system diagnoses versus pathoanatomic diagnoses. J Orthop Sports Phys Ther. 2013;43(5):280-283. [DOI] [PubMed] [Google Scholar]
- 8.Rose SJ. Description and classification--the cornerstones of pathokinesiological research. Phys Ther. 1986;66(3):379-381. [DOI] [PubMed] [Google Scholar]
- 9.Coffin-Zadai CA. Disabling our diagnostic dilemmas. Phys Ther. 2007;87(6):641-653. [DOI] [PubMed] [Google Scholar]
- 10.McClure PW Michener LA. Staged approach for rehabilitation classification: shoulder disorders (STAR-Shoulder). Phys Ther. 2014;95(5):791-800. [DOI] [PubMed] [Google Scholar]
- 11.Zimny NJ. Diagnostic classification and orthopaedic physical therapy practice: what we can learn from medicine. J Orthop Sports Phys Ther. 2004;34(3):105-115. [DOI] [PubMed] [Google Scholar]
- 12.Aggarwal R Ringold S Khanna D, et al. Distinctions between diagnostic and classification criteria? Arthritis Care Res (Hoboken). 2015;67(7):891-897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vlychou M Dailiana Z Fotiadou A, et al. Symptomatic partial rotator cuff tears: Diagnostic performance of ultrasound and magnetic resonance imaging with surgical correlation. Acta radiol. 2009;50(1):101-105. [DOI] [PubMed] [Google Scholar]
- 14.Anderson MW Brennan C Mittal A. Imaging evaluation of the rotator cuff. Clin Sports Med. 2012;31(4):605-631. [DOI] [PubMed] [Google Scholar]
- 15.Hanchard NCA Handoll HHG. Physical tests for shoulder impingements and local lesions of bursa, tendon or labrum that may accompany impingement. Cochrane Database Syst Rev. 2013;(4):CD007427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hegedus EJ Goode A Campbell S, et al. Physical examination tests of the shoulder: a systematic review with meta-analysis of individual tests. Br J Sports Med. 2008;42(2):80-92. [DOI] [PubMed] [Google Scholar]
- 17.Calvert E Chambers GK Regan W, et al. Special physical examination tests for superior labrum anterior posterior shoulder tears are clinically limited and invalid: a diagnostic systematic review. J Clin Epidemiol. 2009;62(5):558-563. [DOI] [PubMed] [Google Scholar]
- 18.Borenstein DG O’Mara JW Boden SD, et al. The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects: A seven-year follow-up study. J Bone Joint Surg Am. 2001;83-A(9):1306-1311. [DOI] [PubMed] [Google Scholar]
- 19.Connor PM Banks DM Tyson AB, et al. Magnetic resonance imaging of the asymptomatic shoulder of overhead athletes: a 5-year follow-up study. Am J Sports Med. 2003;31(5):724-727. [DOI] [PubMed] [Google Scholar]
- 20.Fukuta S Kuge A Korai F. Clinical significance of meniscal abnormalities on magnetic resonance imaging in an older population. Knee. 2009;16(3):187-190. [DOI] [PubMed] [Google Scholar]
- 21.Yamamoto A Takagishi K Kobayashi T, et al. Factors involved in the presence of symptoms associated with rotator cuff tears: A comparison of asymptomatic and symptomatic rotator cuff tears in the general population. J Shoulder Elb Surg. 2011;20(7):1133-1137. [DOI] [PubMed] [Google Scholar]
- 22.Nakashima H Yukawa Y Suda K, et al. Abnormal findings on magnetic resonance images of the cervical spines in 1211 asymptomatic subjects. Spine (Phila Pa 1976). 2015;40(6):392-398. [DOI] [PubMed] [Google Scholar]
- 23.van der Windt DA Koes BW de Jong BA, et al. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis. 1995;54(12):959-964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vecchio P Kavanagh R Hazleman BL, et al. Shoulder pain in a community-based rheumatology clinic. Rheumatology. 1995;34(5):440-442. [DOI] [PubMed] [Google Scholar]
- 25.Lewis JS. Rotator cuff tendinopathy/subacromial impingement syndrome: is it time for a new method of assessment? Br J Sports Med. 2009;43(4):259-264. [DOI] [PubMed] [Google Scholar]
- 26.Malavolta EA Gracitelli MEC Assunção JH, et al. Shoulder disorders in an outpatient clinic: an epidemiological study. Acta Ortop Bras. 2017;25(3):78-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Papadonikolakis A McKenna M Warme W, et al. Published evidence relevant to the diagnosis of impingement syndrome of the shoulder. J Bone Jt Surg Am. 2011;93(19):1827-1832. [DOI] [PubMed] [Google Scholar]
- 28.Park HB Yokota A Gill HS, et al. Diagnostic accuracy of clinical tests for the different degrees of subacromial impingement syndrome. J Bone Jt Surg Am. 2005;87(7):1446-1455. [DOI] [PubMed] [Google Scholar]
- 29.Michener LA Walsworth MK Doukas WC, et al. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil. 2009;90(11):1898-1903. [DOI] [PubMed] [Google Scholar]
- 30.Ludewig PM Reynolds JF. The Association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sport Phys Ther. 2009;39(2):90-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Caldwell C Sahrmann S Van Dillen L. Use of a movement system impairment diagnosis for physical therapy in the management of a patient with shoulder pain. J Orthop Sports Phys Ther. 2007;37(9):551-563. [DOI] [PubMed] [Google Scholar]
- 32.Seitz AL McClure PW Finucane S. Mechanisms of rotator cuff tendinopathy: Intrinsic, extrinsic, or both? Clin Biomech. 2011;26(1):1-12. [DOI] [PubMed] [Google Scholar]
- 33.Myers JB. Glenohumeral range of motion deficits and posterior shoulder tightness in throwers with pathologic internal impingement. Am J Sports Med. 2005;34(3):385-391. [DOI] [PubMed] [Google Scholar]
- 34.Tyler TF Nicholas SJ Lee SJ, et al. Correction of posterior shoulder tightness is associated with symptom resolution in patients with internal impingement. Am J Sports Med. 2010;38(1):114-119. [DOI] [PubMed] [Google Scholar]
- 35.Lawrence RL Braman JP Staker JL, et al. Comparison of 3-dimensional shoulder complex kinematics in individuals with and without shoulder pain, part 2: Glenohumeral joint. J Orthop Sport Phys Ther. 2014;44(9):646-655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Klintberg IH Cools AMJ Holmgren TM, et al. Consensus for physiotherapy for shoulder pain. Int Orthop. 2015;39(4):715-720. [DOI] [PubMed] [Google Scholar]
- 37.Hickey D Solvig V Cavalheri V, et al. Scapular dyskinesis increases the risk of future shoulder pain by 43 % in asymptomatic athletes: a systematic review and meta-analysis. Br J Sport Med. 2017;22:1-10. [DOI] [PubMed] [Google Scholar]
- 38.McFarland EG Maffulli N Del Buono A, et al. Impingement is not impingement: the case for calling it “Rotator Cuff Disease”. Muscles Ligaments Tendons J. 2013;3(3):196-200. [PMC free article] [PubMed] [Google Scholar]
- 39.de Witte PB de Groot JH van Zwet EW, et al. Communication breakdown: Clinicians disagree on subacromial impingement. Med Biol Eng Comput. 2014;52(3):221-231. [DOI] [PubMed] [Google Scholar]
- 40.Kibler WB Ludewig PM McClure PW, et al. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the “scapular summit.” Br J Sports Med. 2013;47(14):877-885. [DOI] [PubMed] [Google Scholar]
- 41.Braman JP Zhao KD Lawrence RL, et al. Shoulder impingement revisited: Evolution of diagnostic understanding in orthopedic surgery and physical therapy. Med Biol Eng Comput. 2014;52(3):211-219. [DOI] [PubMed] [Google Scholar]
- 42.Burkhart SS Morgan CD Kibler WB. The disabled throwing shoulder: Spectrum of pathology part III: The SICK scapula, #scapular |dyskinesis, the kinetic chain, and rehabilitation. Arthrosc - J Arthrosc Relat Surg. 2003;19(6):641-661. [DOI] [PubMed] [Google Scholar]
- 43.Uhl TL Kibler WB Gecewich B, et al. Evaluation of clinical assessment methods for scapular dyskinesis. Arthrosc J Arthrosc Relat Surg. 2009;25(11):1240-1248. [DOI] [PubMed] [Google Scholar]
- 44.Paletta GA Warner JJP Warren RF, et al. Shoulder kinematics with two-plane x-ray evaluation in patients with anterior instability or rotator cuff tearing. J shoulder Elb Surg. 1997;6(6):516-527. [DOI] [PubMed] [Google Scholar]
- 45.Ogston JB Ludewig PM. Differences in 3-dimensional shoulder kinematics between persons with multidirectional instability and asymptomatic controls. Am J Sports Med. 2007;35(8):1361-1370. [DOI] [PubMed] [Google Scholar]
- 46.Spoto MM Collins J. Physiotherapy diagnosis in clinical practice: A survey of orthopaedic certified specialists in the USA. Physiother Res Int. 2008;13(1):31-41. [DOI] [PubMed] [Google Scholar]
- 47.Association American Physical Therapy. Board of Directors Meeting Minutes. April 2017 26-29. http://www.apta.org/BOD/Meetings/Minutes/2017/4/26/.