Abstract
Background
Assaultive violence events are associated with increased risk for adverse psychiatric outcomes, including post-traumatic stress (PTS), depression, and generalized anxiety. Prior research has indicated that economic, legal, and social stressors that could follow assaultive events may explain the increased risk for adverse psychiatric outcomes, yet longitudinal studies have not adequately examined this pathway. In the current study, we aimed to address this limitation.
Methods
Participants (N = 1360) were part of a longitudinal population-based study of adults living in Detroit. At three waves, participants indicated their exposure to assaultive violence and economic, legal, and social stressors, and completed inventories of PTS, depression, and generalized anxiety. Longitudinal mediation models were used to test the hypothesized pathway from assaultive violence to each psychiatric outcome.
Results
The hypothesized models evidenced good fit with the data and, in each, the paths from Wave 1 (W1) assaultive violence to W2 stressors, and from W2 stressors to W3 symptoms were significant (range of Standardized Estimates: 0.09–0.15, all p < 0.01). Additionally, the indirect paths from W1 assaultive violence to W3 symptoms were significant (range of Standardized Estimates: 0.01–0.02, all p < 0.05).
Conclusions
The findings illustrate that the economic, legal, and social stressors that could follow assaultive violence increase risk for a range of psychiatric symptoms. Although future research is needed, the results suggest that investment in interventions that prevent and mitigate assaultive violence survivors’ exposure to such stressors may be an effective way to prevent mental illness in the aftermath of violent assaults.
Keywords: Assaultive violence, depression, generalized anxiety, post-traumatic stress, stressful life events
Introduction
Experiences of assaultive violence, including physical and sexual assault, are fairly common. For example, in the National Comorbidity Survey, 11.1% of men and 6.9% of women reported lifetime exposure to physical attack, 3.2 and 4.8% to physical abuse, and 0.7 and 9.2% to rape, respectively (Kessler et al. 1995). Epidemiologic studies have documented that approximately half of residents of urban environments have experienced one or more lifetime assaultive violence events (Goldmann et al. 2011). Assaultive events have been found to be associated with a higher risk for post-traumatic stress disorder (PTSD) than non-assaultive traumatic events (McLaughlin et al. 2013). In addition, exposure to such events has been linked to other mental health symptoms, including depression and generalized anxiety (Cerdá et al. 2012). Although the link between assaultive violence and adverse psychiatric outcomes is clear, little is known about the pathways underlying this association. Examining the pathways from assaultive violence to mental health is critical to understanding the etiology of post-event mental illness, and for identifying opportunities for intervention.
One possible pathway from assaultive violence to psychiatric outcomes is through the increased incidence of stressful life events that seem to follow exposure to trauma. Indeed, a large body of literature focused on survivors of intimate partner violence (IPV) and sexual assault suggests three types of stressors can potentially occur after such events. First, IPV has been linked to a range of economic stressors, including financial strain, unemployment, and difficulty accessing services (Loya, 2014). Second, researchers have shown that IPV survivors experience legal stressors, including dissatisfaction with and lack of perceived control over the judiciary process, and a sense of ‘secondary victimization’ (Walsh & Bruce, 2011). Third, IPV and sexual assault have been associated with a range of social stressors, including difficulties maintaining intimate relationships and sexual dysfunction (Polusny & Follette, 1995; Bryne et al. 1999; Davis & Petretic-Jackson, 2000). Survivors have also described negative reactions from loved ones and service providers, including blame, stigmatization, or control (Campbell et al. 2001; Relyea & Ullman, 2015). Further research has provided evidence that the economic, legal, and social stressors that potentially follow IPV and sexual assault extend to victims of other forms of assaultive violence, including physical assault, as well (e.g. MacMillan, 2000; Herman, 2003; Mueller et al. 2008). These stressors, in turn, have been linked to an increased risk for adverse psychiatric outcomes among trauma survivors (Osenback et al. 2009; Hassija & Gray, 2012).
Therefore, research suggests a pathway from assaultive violence to psychiatric outcomes through economic, legal, and social stressors. However, only two studies to our knowledge have tested such a model using longitudinal data. First, Beeble et al. (2010) studied 160 women who were part of an IPV community-based advocacy intervention and, using hierarchical linear modeling and a Sobel test for mediation, found evidence that economic resource constraints mediated the relationship between changes in psychological abuse (but not changes in physical abuse) and changes in depression over time. Second, a five-wave study of 503 single mothers receiving welfare assistance from the Women’s Employment Study found significant indirect effects from more extensive IPV exposure over the course of the study to higher levels of depression and anxiety at Wave 5 (W5) through lower job stability between W4 and W5 (Adams et al. 2013). These studies represent significant advances in understanding the pathways through which IPV leads to adverse psychiatric outcomes, yet each suffers from notable limitations, including a non-representative sample and low statistical power in the former, and the lack of longitudinal data on mental health in the latter.
More generally, the extant literature is limited by the lack of a comprehensive approach to understanding the pathway from assaultive violence to mental health problems. For example, researchers have primarily focused on survivors of IPV and sexual assault, and findings might not generalize to those who have experienced other forms of assaultive violence. In a similar vein, no study to our knowledge has examined the cumulative influence of different forms of assaultive violence, and few have assessed stressors in more than one domain. It is possible that there is a dose–response relationship between assaultive violence and stressors, such that persons who experience more forms of violence are likely to experience a broader range of stressors. This relationship could perhaps account for the well-documented dose–response relationship between trauma exposure and mental health outcomes (Cerdá et al. 2012; McLaughlin et al. 2013). The extant research has also focused primarily on post-traumatic stress (PTS) and depression symptoms, whereas exposure to assaultive violence has been associated with a broader range of other psychiatric outcomes, including generalized anxiety (Cerdá et al. 2012).
Aiming to address these limitations in the literature, we explored the pathway from a range of assaultive violence events to PTS, depression, and generalized anxiety through economic, legal, and social stressors using data from a population-based study of Detroit residents. Based on the prior literature, we expected significant indirect paths from a greater number of assaultive violence events to more severe psychiatric symptoms via exposure to more economic, legal, and social stressors.
Methods
Participants and procedures
Data were from the Detroit Neighborhood Health Study (DNHS), a longitudinal study of predominantly Black adults (18 years or older) living in Detroit, Michigan. Participants were selected through a dual-frame probability design; telephone numbers were obtained from a list-assisted random-digit-dial frame and from the US Postal Service Sequence Files. Within eligible households, one adult was randomly selected to participate. Additional details regarding the sampling methodology can be found elsewhere (Uddin et al. 2010).
W1 of data collection was conducted between 2008 and 2009, and 1547 participants completed the W1 survey. Approximately a year after W1, 1054 participants completed the W2 survey (68.1% retention rate), and approximately a year after W2, 965 participants completed the W3 survey (62.5% retention rate). The current study focuses on participants who reported experiencing at least one traumatic event at W1 and who were therefore eligible to report on PTS at all three waves (N = 1360). A total of 847 participants completed all three waves, yielding an overall retention rate of 54.8%. At each wave, participants completed a structured telephone survey, lasting an average of 40 min and including measures of trauma, stressors, and psychiatric symptoms. Participants gave oral informed consent and were offered $25 for their participation for each interview. The Institutional Review Board of the University of Michigan approved the study.
Measures
Assaultive violence events
At W1, participants completed a 20-item inventory of lifetime traumatic events (Breslau et al. 1998). At W2 and W3, participants completed this inventory in reference to the time since the previous interview. In the current study, we included six items on the inventory that were indicative of assaultive violence: (1) been raped; (2) experienced another kind of sexual assault or unwanted sexual contact as a result of force, threat of harm, or manipulation; (3) been shot or stabbed; (4) been mugged, held up, or threatened with a weapon; (5) been held captive, tortured or kidnapped; and (6) been badly beaten up. The total number of events endorsed at each wave was included in the analysis.
Stressful life events
At each wave, participants completed a modified inventory of 11 stressful life events (Boardman et al. 2001; Boardman, 2004; Tracy et al. 2011). At W1, participants were asked if they experienced these events in reference to their lifetime, and at W2 and W3, in reference to the time since the prior interview. In the current study, we included seven items from this inventory there were indicative of economic stressors (four items, e.g. ‘lost your job’), legal stressors (one item: ‘experienced stressful legal problems – for example, being sued or suing someone else’), and social stressors (two items, e.g. ‘been through a divorce or “break-up”’). The total number of stressors endorsed was included in the analysis. The four excluded items (‘had a parent who had a problem with drugs or alcohol’, ‘had a family member other than a parent with a serious drug or alcohol problem’, ‘seen or heard physical fighting between your parents or caregivers’, and ‘experienced mental illness personally or the mental illness of someone close’) were conceptualized as not reflecting these domains. More specifically, although the first three items pertain to the participant’s social network, they are not consistent with the social stressors that have been documented in prior research with assaultive violence survivors (e.g. Polusny & Follette, 1995; Mueller et al. 2008; Relyea & Ullman, 2015). The fourth item, being that it in part assessed the participant’s mental health, was conceptualized as redundant with the psychiatric outcomes included in the current analysis.
Post-traumatic stress
PTS was assessed using the PTSD Checklist – Civilian Version (PCL-C; Weathers et al. 1993). The PCL-C includes 17 items, representing criterion B (re-experiencing: five items, e.g. ‘repeated, disturbing thoughts or memories about the event’), C (avoidance: two items, e.g. ‘avoiding activities or situations because they reminded you of the stressful experience’; and emotional numbing: five items, e.g. ‘loss of interest in things you used to enjoy’), and D (hyperarousal: five items, e.g. ‘trouble falling or staying asleep’) from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; APA, 1994). At each wave, participants responded based on the traumatic event they rated as the ‘worst’ at W1, and at W2 and W3, were reminded of the traumatic event they had reported. Respondents indicated how much they were bothered by each symptom from 1 = not at all to 5 = extremely. At W1, participants reported on how much they were ‘ever’ bothered by each symptom, and at W2 and W3, on how much they were bothered since their prior interview. Responses were summed to yield a symptom severity score from 17 to 85. The PCL-C has previously demonstrated excellent internal consistency and agreement with PTSD diagnosis and symptom ratings (Blanchard et al. 1996; Weathers & Ford, 1996). For the current study, clinical in-person interviews conducted at W1 with a random subsample of 51 DNHS participants supported the reliability and validity of the telephone-administered PCL-C, relative to the gold-standard Clinician-Administered PTSD Scale for DSM-IV [for additional information, see (masked for blind review)]. Cronbach’s α in the current study ranged from 0.94 to 0.95.
Depression
Past-year depressive symptoms were evaluated with the nine-item Patient Health Questionnaire (PHQ-9; Kroenke & Spitzer, 2002). Items (e.g. ‘feeling down, depressed, or hopeless’) were rated from 0 = not at all to 3 = nearly every day, with symptom severity scores ranging from 0 to 27. The PHQ-9 has excellent internal consistency, test–retest reliability, and construct validity (Martin et al. 2006) Cronbach’s α in the current study ranged from 0.89 to 0.90.
Generalized anxiety
Past-year generalized anxiety symptoms were evaluated by a seven-item questionnaire (GAD-7; Spitzer et al. 2006). Participants rated to what degree they experienced each anxiety symptom (e.g. ‘feeling nervous, anxious, or on edge’) from 0 = not at all to 3 = nearly every day, such that scores ranged from 0 to 21. The GAD-7 has been previously shown to have excellent internal consistency and test–retest reliability (Spitzer et al. 2006) Cronbach’s α in the current study ranged from 0.90 to 0.92.
Data analysis
Preliminary analyses were conducted in SAS version 9.3 (SAS, Cary, NC). First, descriptive statistics for all study variables were computed. Second, χ2 tests and one-way analysis of variance (ANOVA) examined demographic differences between the 1360 participants who reported at least one W1 lifetime trauma and the 187 who did not. Third, we assessed for differences between the 847 respondents who participated in all three waves and the 513 who did not on all variables in the analysis using one-way ANOVA.
Analyses to fulfill study aims were conducted in Mplus 7.1 (Muthén & Muthén, 1998–2012). We tested three cross-lagged panel models for longitudinal data (Selig & Preacher, 2009) in which assaultive trauma at each wave were predictive of stressors at the subsequent wave, and stressors at each wave were in turn predictive of PTS, depression, and generalized anxiety at the subsequent wave. Separate models were conducted for each outcome. Goodness of fit was evaluated using the Root Mean Square Error of Approximation (RMSEA) and its 90% confidence interval (CI), and the Comparative Fit Index (CFI). The following criteria were used to determine acceptable model fit (Hu & Bentler, 1999): RMSEA and its 90% CI upper limit close to or below 0.06, and CFI close to or above 0.95. Modification indices were inspected and additional paths were included if necessary to improve model fit. We also examined indirect effects from W1 assaultive trauma to W3 psychiatric outcomes via W2 stressors, which were computed as the product of the path from W1 assaultive trauma to W2 stressors, and the path from W2 stressors to W3 psychiatric outcomes. Maximum-likelihood (ML) estimation with robust standard errors, via the MLR estimator, was used to handle missing data and non-normality. Standardized estimates are listed in the results.
Online Supplementary analyses were then conducted. First, we ran models without the two direct paths comprising the hypothesized indirect effect, i.e., with these paths constrained to zero. Satorra–Bentler scaled χ2 difference tests were used to test whether constraining the paths to zero led to significantly worse model fit. Second, for each outcome, we ran separate models for economic, legal, and social stressors to discern whether one or more types of stressors accounted for the pattern of results.
Results
Preliminary analysis
The frequency of each assaultive violence and stressful life event at each wave, and descriptive statistics for all variables included in the analysis are shown in Table 1. Of the 1360 participants included in the study, the majority identified as female (57.4%) and non-Hispanic Black (84.4%); 9.9% identified as non-Hispanic White, and 1.8% as Hispanic. On average, participants were 50.60 years old (S.D. = 16.57; range 18–92). At W1, 28.2% reported their income as under $15 000 and 56.9% were unemployed. There were no demographic differences between the 1360 participants who reported at least one lifetime trauma at W1 and the 187 who did not. Respondents who participated in all three waves reported significantly fewer W1 lifetime assaultive events and stressors [F(1, 1358) = 10.42, p = 0.001 and F(1, 1358) = 4.91, p = 0.027, respectively], significantly fewer W2 stressors [F(1, 939) = 13.79, p < 0.001], significantly lower W1 PTS and generalized anxiety, [F(1, 1349) = 10.45, p = 0.001, and F(1, 1348) = 4.52, p = 0.034, respectively], and significantly lower W2 depression and generalized anxiety [F(1, 939) = 11.07, p = 0.001, and F(1, 938) = 9.54, p = 0.002, respectively], than those who did not.
Table 1.
Frequency of assaultive violence and stressful life events, and means and frequencies of variables in the analysis (N = 1360)
| Wave 1
|
Wave 2
|
Wave 3
|
||||
|---|---|---|---|---|---|---|
| n or M | % or S.D. | n or M | % or S.D. | n or M | % or S.D. | |
| Assaultive violence events | ||||||
| Been raped | 162 | 12.0% | 2 | 0.2% | 3 | 0.4% |
| Experienced another kind of sexual assault or unwanted sexual contact as a result of force, threat of harm, or manipulation | 212 | 15.7% | 11 | 1.2% | 12 | 1.4% |
| Been shot or stabbed | 177 | 13.0% | 2 | 0.2% | 1 | 0.1% |
| Been mugged, held up, or threatened with a weapon | 532 | 39.2% | 31 | 3.3% | 30 | 3.5% |
| Been held captive, tortured, or kidnapped | 76 | 5.6% | 1 | 0.1% | 0 | 0.0% |
| Been badly beaten up | 205 | 15.1% | 12 | 1.3% | 5 | 0.6% |
| Total number of events | 1.00 | 1.19 | 0.06 | 0.29 | 0.06 | 0.27 |
| Stressful life events | ||||||
| Lost your job (economic) | 586 | 43.1% | 122 | 13.0% | 77 | 9.0% |
| Been unemployed and seeking employment for at least 3 months (economic) | 681 | 50.2% | 219 | 23.3% | 160 | 18.9% |
| Had serious financial problems (economic) | 780 | 57.6% | 336 | 35.8% | 282 | 33.2% |
| Had problems getting access to adequate healthcare (economic) | 395 | 29.1% | 171 | 18.2% | 120 | 14.1% |
| Experienced stressful legal problems – for example, being sued or suing someone else (legal) | 403 | 29.6% | 95 | 10.1% | 77 | 9.0% |
| Been through a divorce or ‘break up’ with a partner or significant other (social) | 743 | 54.7% | 91 | 9.7% | 65 | 7.6% |
| Been emotionally mistreated – for example, shamed, embarrassed, ignored, or repeatedly told you were no good (social) | 454 | 33.4% | 99 | 10.5% | 66 | 7.8% |
| Total number of events | 2.97 | 2.09 | 1.20 | 1.50 | 0.99 | 1.36 |
| Psychiatric symptoms | ||||||
| Post-traumatic stress (PCL-C) | 33.29 | 15.35 | 27.43 | 11.92 | 28.48 | 12.49 |
| Depression (PHQ-9) | 5.62 | 6.28 | 4.16 | 5.39 | 3.85 | 5.34 |
| Generalized anxiety (GAD-7) | 4.29 | 5.24 | 3.06 | 4.80 | 2.87 | 4.64 |
PCL-C, Post-traumatic Stress Checklist – Civilian Version; PHQ-9, Patient Health Questionnaire-9; GAD-7, Generalized Anxiety Disorder-7.
Longitudinal cross-lagged panel models
Post-traumatic stress
The model for PTS showed evidence of good fit with the data: χ2(16) = 55.92 (p < 0.001), RMSEA = 0.04 (90% CI 0.04–0.06), CFI = 0.96 (Fig. 1). More W1 assaultive events were significantly associated with more W2 stressors [Standardized Estimate (Est.) = 0.09, Standard Error (S.E.) = 0.04, p = 0.009], which in turn were associated with higher W3 PTS (Est. = 0.14, S.E. = 0.04, p = 0.001). The indirect effect from W1 assaultive events to W3 PTS through W2 stressors was significant (Est. = 0.01, S.E. = 0.01 p = 0.049).
Fig. 1.
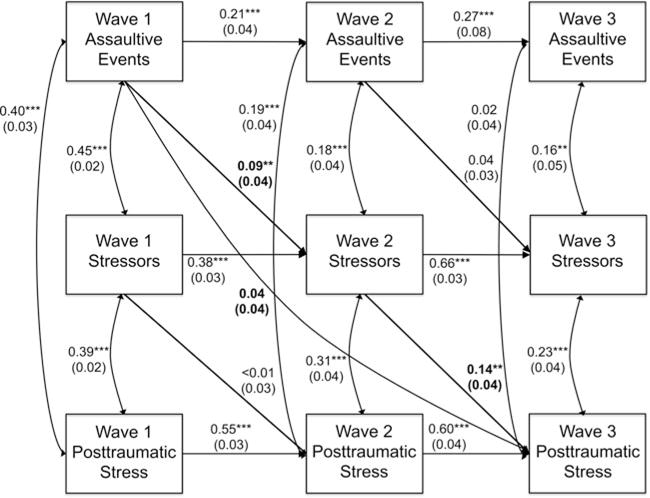
Results of model for post-traumatic stress symptoms. *p < 0.05, **p < 0.01, ***p < 0.001. For clarity, coefficients for the direct paths along the hypothesized indirect pathway, and the direct path from Wave 1 assaultive violence to Wave 3 post-traumatic stress are in bold. Standardized results are listed.
Depression
The initial model for depression did not meet criteria for acceptable model fit, χ2(16) = 95.38 (p < 0.001), RMSEA = 0.06 (90% CI:0.05–0.07), CFI = 0.93. Inspection of modification indices led to the addition of a path from W1 depression to W3 depression. The resulting model had acceptable fit with the data, χ2(15) = 52.92 (p < 0.001), RMSEA = 0.04 (90% CI 0.03–0.06), CFI = 0.97 (Fig. 2). More W1 assaultive events were significantly associated with more W2 stressors (Est. = 0.10, S.E. = 0.04, p = 0.006), which in turn were associated with higher W3 depression (Est. = 0.14, S.E. = 0.04, p < 0.001). The indirect effect from W1 assaultive events to W3 depression through W2 stressors was significant (Est. = 0.01, S.E. = 0.01, p = 0.040).
Fig. 2.
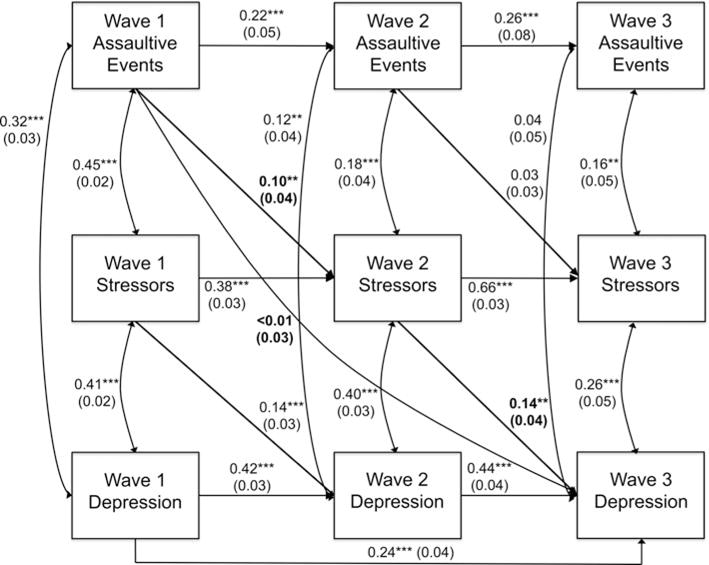
Results of model for depression symptoms. *p < 0.05, **p < 0.01, ***p < 0.001. For clarity, coefficients for the direct paths along the hypothesized indirect pathway, and the direct path from Wave 1 assaultive violence to Wave 3 depression are in bold. Standardized results are listed.
Generalized anxiety
The initial model for generalized anxiety did not meet criteria for acceptable model fit, χ2(16) = 83.84 (p < 0.001), RMSEA = 0.06 (90% CI 0.04–0.07), CFI = 0.93. Inspection of modification indices led to the addition of a path from W1 generalized anxiety to W3 generalized anxiety. The resulting model had acceptable fit with the data, χ2(15) = 56.99 (p < 0.001), RMSEA = 0.05 (90% CI 0.03–0.06), CFI = 0.96 (Fig. 3). More W1 assaultive events were significantly associated with more W2 stressors (Est. = 0.11, S.E. = 0.04, p = 0.002), which in turn were associated with higher W3 generalized anxiety (Est. = 0.15, S.E. = 0.04, p = 0.001). In addition, the indirect effect from W1 assaultive events to W3 generalized anxiety through W2 stressors was significant (Est. = 0.02, S.E. = 0.01, p = 0.032).
Fig. 3.
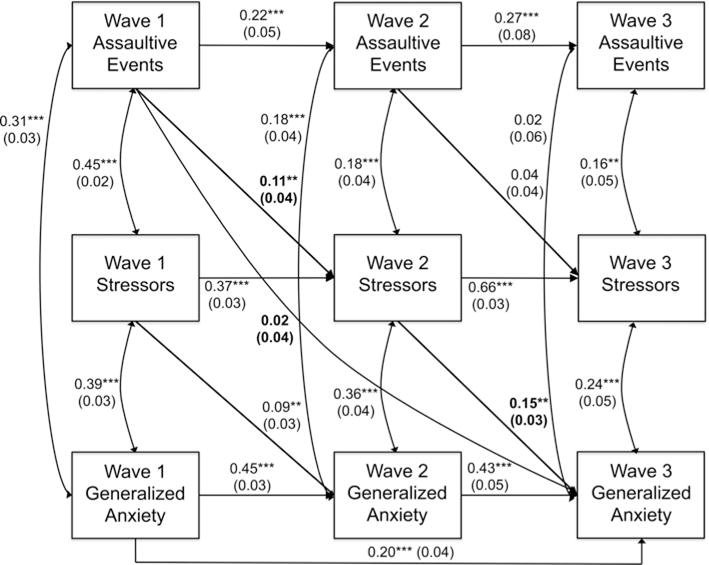
Results of model for generalized anxiety symptoms. *p < 0.05, **p < 0.01, ***p < 0.001. For clarity, coefficients for the direct paths along the hypothesized indirect pathway, and the direct path from Wave 1 assaultive violence to Wave 3 generalized anxiety are in bold. Standardized results are listed.
Supplementary analyses
Tests of alternative models
For each outcome, constraining the two direct paths comprising the indirect effect from W1 assaultive events to W3 symptoms through W2 stressors to zero resulted in significantly worse fit – PTS: χ2Δ(2) = 17.07, p < 0.001; depression: χ2Δ(2) = 19.75, p < 0.001; generalized anxiety: χ2Δ(2) = 21.63, p < 0.001.
Models for economic, legal, and social stressors
Table 2 lists standardized estimates for direct paths from W1 assaultive events to W2 stressors, and from W2 stressors to W3 symptoms, as well as the indirect path from W1 assaultive events to W3 symptoms through W2 stressors from separate models including economic, legal, and social stressors predicting each mental health outcome. As shown, all direct paths reached statistical significance with two exceptions: the path from W2 legal stressors to W3 depression, and the path from W2 social stressors to W3 PTS. None of the indirect effects reached statistical significance. Full results for these models are listed in Online Appendix A.
Table 2.
Direct and indirect pathways of interest for separate models testing economic, legal, and social stressors
| W1 assaultive events → W2 stressors
|
W2 stressors → W3 symptoms
|
Indirect effect
|
||||
|---|---|---|---|---|---|---|
| Est. | S.E. | Est. | S.E. | Est. | S.E. | |
| Economic stressors | ||||||
| PTS | 0.09* | 0.03 | 0.11** | 0.04 | 0.01 | 0.01 |
| Depression | 0.09* | 0.04 | 0.10** | 0.04 | 0.01 | 0.01 |
| Generalized anxiety | 0.10** | 0.03 | 0.11** | 0.04 | 0.01 | 0.01 |
| Legal stressors | ||||||
| PTS | 0.11** | 0.04 | 0.08* | 0.03 | 0.01 | 0.01 |
| Depression | 0.11** | 0.04 | 0.06 | 0.04 | 0.01 | 0.01 |
| Generalized anxiety | 0.12** | 0.04 | 0.07* | 0.03 | 0.01 | 0.01 |
| Social stressors | ||||||
| PTS | 0.08* | 0.04 | 0.06 | 0.05 | 0.01 | <0.01 |
| Depression | 0.08* | 0.04 | 0.10* | 0.04 | 0.01 | 0.01 |
| Generalized anxiety | 0.09* | 0.04 | 0.10* | 0.05 | 0.01 | 0.01 |
W1, Wave 1; Est., estimate; S.E., standard error; PTS, post-traumatic stress.
N = 1360.
Standardized results listed.
p < 0.05,
p < 0.01.
Discussion
This study found support for a model wherein exposure to assaultive violence is associated with three psychiatric outcomes – PTS, depression, and generalized anxiety symptoms – through economic, legal, and social stressors. Cross-lagged panel models with three waves of data from an epidemiologic sample of adults living in Detroit testing this pathway had good fit with the data. In each model, the paths from W1 assaultive violence to W2 stressors, and from W2 stressor to W3 psychiatric symptoms were significant in the hypothesized direction. In addition, the indirect effects from assaultive violence to psychiatric outcomes through stressors were significant.
The results are consistent with prior research focused on survivors of IPV and sexual assault suggesting this indirect pathway, including the two studies to our knowledge using longitudinal data (Beeble et al. 2010; Adams et al. 2013). The study adds to this literature by using a large epidemiologic sample from an urban environment, and participants who experienced a range of assaultive violence events. As such, the results suggest that the pathway to psychiatric outcomes through stressful life events might not be limited to IPV and sexual violence, but rather could possibly extend to other assaultive events, including physical assault and robbery, although we notably did not look at different types of assaultive violence separately due to their limited frequencies in the sample. Similarly, unlike the majority of previous studies investigating this pathway, our main analysis included a range of stressors that assaultive violence survivors are more likely to experience, rather than limited our assessment to stressors in a single domain.
Our use of longitudinal mediation models provided more robust support for the indirect pathway than has been documented previously. For example, unlike the study by Adams et al. (2013), we controlled for prior levels of psychiatric symptoms, permitting greater insight into how assaultive violence and stressors contributed to change in symptoms over the course of the study. The cross-lagged approach also more accurately reflects the temporal nature of the indirect pathway, with assaultive violent events preceding stressors, and stressors preceding psychiatric outcomes, than the hierarchical linear model approach employed by Beeble et al. (2010). Given the methodological advantages of our analytic strategy and the consistency of the results across psychiatric outcomes, the results bolster the implications of prior research that we can attenuate the adverse psychiatric consequences of assaultive violence by mitigating the stressors that follow.
The results also provide insight into the cumulative impact of a range of assaultive violence experiences and support prior research showing dose–response effects of trauma exposure (McLaughlin et al. 2013). This is in contrast to prior research on the indirect pathway, which has examined the influence of the severity of assaultive events (Beeble et al. 2010). Despite this divergence, the trends in the data were notably consistent with prior research, perhaps indicating that cumulative exposure is a marker of exposure severity, and vice versa. To examine this possibility, researchers could assess both the number and severity of exposures and examine the role of both in longitudinal models. This suggestion also applies to stressful life events, as researchers could more thoroughly assess their severity and relationships with outcomes in future research.
Whereas we sought to take a comprehensive approach in the current study, it would also be valuable for researchers to hone in on the different types of assaultive events and assess for variability in the extent to which they are linked to different psychiatric outcomes via stressors. Similarly, future work could assess whether the different domains of stressful life events differentially mediate relationships between assaultive violence and psychiatric outcomes. In our Online Supplementary analysis, we noted that the trends were similar for separate models including economic, legal, and social stressors, except that the direct paths from W2 legal stressors to W3 depression and from W2 social stressors to W3 PTS were non-significant, and none of the indirect paths reached statistical significance. The results suggest variability in the extent to which different types of stressors relate to symptoms over time, and that perhaps it is only the accumulation of multiple forms of stressful life events stemming from assaultive violence that contribute to the meditational pathway. However, these results should be interpreted with caution given the small number of items for each type of stressor. To address this issue, further research could more thoroughly assess and examine separately the three domains.
The results should also be interpreted in light of six additional limitations. First, the time frame for the assessment of all study variables differed across study waves and mental health measures. Assaultive violence events, stressors, and PTS were assessed in reference to the participant’s lifetime at W1, and in reference to the time since the participant’s prior interview at W2 and W3. The timing of the ‘worst’ trauma used as an anchor in the assessment of PTS symptoms and duration between interviews therefore varied across participants – for the latter, especially given some W3 participants did not complete the W2 assessment. In contrast, depression and generalized anxiety were assessed in reference to the prior year at each wave. This variability introduces error into our models, and limits our interpretations regarding mediation and our ability to make comparisons across models. In particular, although we did not assess the dates of each assaultive event, it is likely that there was both within- and between-participant variation in the time between W1 (lifetime) assaultive events and W2 (past-year) stressors. It is perhaps unlikely that W2 stressors mediated the influence of assaultive violence events experienced in childhood, for example. However, the inclusion of temporally remote events would likely lead to underestimations of indirect effects and therefore it is notable that our findings were significant despite this limitation. A related issue regarding temporality is that we did not assess the start and end dates of stressors, which could have been either acute or chronic. It is possible that some participants were experiencing chronic stressors that were present both before and after their assaultive violence exposures. Although this limitation is somewhat tempered by our inclusion of autoregressive paths from stressors at earlier to later waves, it nonetheless limits our conclusions regarding indirect pathways and demonstrates the need for further research that more thoroughly examines the nature and timing of exposure to assaultive violence and stressful life events. More generally, we did not assess participants’ perceptions of whether assaultive violence had contributed to the onset or severity of stressors, and it is important to emphasize that the pathways within our models are associations rather than indicators of causation.
Second, PTS was assessed in reference to the lifetime traumatic event that participants indicated as the ‘worst’ from an inventory of traumatic events that was not limited to assaultive violence. It was therefore possible that participants were reporting on PTS that was not directly related to their assaultive violence exposure. However, this method of PTS assessment was consistent with prior epidemiologic research (e.g. McLaughlin et al. 2013), and it is unclear how this limitation could influence the pattern of results. Third, we prioritized parsimony in our models and did not include all possible pathways among variables. We did not, for example, include paths from psychiatric symptoms to stressors and assaultive events, which have been demonstrated in prior research (Hammen, 2006; Cougle et al. 2009). However, a previous analysis of DNHS data found non-significant longitudinal pathways from PTS to assaultive events (Lowe et al. 2014), our models demonstrated good fit with the data despite the exclusion of these paths, examination of model fit indices did not suggest that adding them would substantially improve model fit, and our models were consistent with established guidelines for cross-lagged panel models (Selig & Preacher, 2009). Nevertheless, future studies could test models that perhaps more accurately reflect the complexity of relationships among these constructs. Fourth, the analysis did not control for potentially shared covariates of assaultive violence, stressful life events, and mental health symptoms, including genetic variants, physical health comorbidities, and mental health service access and utilization, which could have led to inflated estimates. Fifth, no efforts to our knowledge have been made to examine the psychometric properties of the inventories of traumatic and stressful life events used in the study. Finally, the results of the study might not generalize to non-urban areas, to other urban environments, or to populations with different demographic characteristics (e.g. that are not majority non-Hispanic Black). It is worth noting, however, that race is conceptualized as a social construct, that there is heterogeneity with respect to geographic origins within and across racial groups in the study, and therefore no scientific basis for the argument that the results observed here would be significantly different or in the opposite direction in any other urban population exposed to similar social and physical environments in the USA. Nonetheless, replication is needed. One potentially useful direction for future research would be to explore whether pathways from assaultive violence to mental health symptoms differ among different demographic groups. For example, given gender differences in assaultive violence exposures and post-trauma mental health (e.g. McLaughlin et al. 2013), further studies could investigate whether the pathways within our model differ for men and women. Replication is especially needed given significant differences between participants who completed all three waves v. those who did not.
Despite these limitations, the results add to the growing literature exploring the pathways through which exposure to assaultive violence influences mental health. Although future research is needed, the results suggest that efforts to address the economic, legal, and social stressors that assaultive violence survivors often encounter could potentially help prevent and mitigate psychiatric symptoms.
Supplementary Material
Acknowledgments
This research was supported by a grant from the National Institute on Drug Abuse (R01 DA022720).
Footnotes
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291717001143.
Declaration of Interest
None.
References
- Adams AE, Bybee D, Tolman RM, Sullivan CM, Kennedy AC. Does job stability mediate the relationship between intimate partner violence and mental health among low-income women. American Journal of Orthopsychiatry. 2013;83:600–608. doi: 10.1111/ajop.12053. [DOI] [PubMed] [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders. 4th. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Beeble ML, Bybee D, Sullivan CM. The impact of resource constraints on the psychological well-being of survivors of intimate partner violence over time. Journal of Community Psychology. 2010;38:943–958. doi: 10.1007/s10464-010-9398-6. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behavioral Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Boardman JD. Stress and physical health: the role of neighborhoods as mediating and moderating processes. Social Science & Medicine. 2004;58:2473–2483. doi: 10.1016/j.socscimed.2003.09.029. [DOI] [PubMed] [Google Scholar]
- Boardman JD, Finch BK, Ellison CG, Williams DS, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. Journal of Health and Social Behavior. 2001;42:151–165. [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit area survey of trauma. Archives of General Psychiatry. 1998;55:626–633. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Bryne CA, Resnick HS, Kilpatrick DG, Best CL, Saunders BE. The socioeconomic impact of interpersonal violence on women. Journal of Consulting and Clinical Psychology. 1999;67:362–366. doi: 10.1037//0022-006x.67.3.362. [DOI] [PubMed] [Google Scholar]
- Campbell R, Wasco SM, Ahrens CE, Sefl T, Barnes HE. Preventing the ‘second rape’: rape survivors’ experiences with community service providers. Journal of Interpersonal Violence. 2001;16:1239–1259. [Google Scholar]
- Cerdá M, DiGangi J, Galea S, Koenen K. Epidemiologic research on interpersonal violence and common psychiatric disorders: where do we go from here? Depression & Anxiety. 2012;29:359–385. doi: 10.1002/da.21947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cougle JR, Resnick H, Kilpatrick DG. Does prior exposure to interpersonal violence increase risk of PTSD following subsequent exposure? Behaviour Research and Therapy. 2009;47:1012–1017. doi: 10.1016/j.brat.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JL, Petretic-Jackson PA. The impact of child sexual abuse on adult interpersonal functioning: a review and synthesis of the empirical literature. Aggression and Violent Behavior. 2000;5:291–328. [Google Scholar]
- Goldmann E, Aiello A, Uddin M, Delva J, Koenen K, Gant LM, Galea S. Pervasive exposure to violence and posttraumatic stress disorder in a predominantly African American Urban Community: The Detroit Neighborhood Health Study. Journal of Traumatic Stress. 2011;24:747–751. doi: 10.1002/jts.20705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C. Stress generation in depression: reflection on its origins, research, and future directions. Journal of Clinical Psychology. 2006;62:1065–1082. doi: 10.1002/jclp.20293. [DOI] [PubMed] [Google Scholar]
- Hassija CM, Gray MJ. Negative social reactions to assault disclosure as a mediator between self-blame and posttraumatic stress symptoms among survivors of interpersonal assault. Journal of Interpersonal Violence. 2012;27:3425–3441. doi: 10.1177/0886260512445379. [DOI] [PubMed] [Google Scholar]
- Herman JL. The mental health of crime victims. Journal of Traumatic Stress. 2003;16:159–166. doi: 10.1023/A:1022847223135. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler P. Cutoff criteria for fit indexes in covariance structure: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer R. The PHQ-9: a new depression diagnostic and severity measure. Psychiatric Annals. 2002;32:1–9. [Google Scholar]
- Loya RM. The role of sexual violence in creating and maintaining economic insecurity among asset-poor women of color. Violence Against Women. 2014;20:1299–1310. doi: 10.1177/1077801214552912. [DOI] [PubMed] [Google Scholar]
- Lowe SR, Walsh K, Uddin M, Galea S, Koenen KC. Bidirectional relationships between trauma exposure and posttraumatic stress: a longitudinal study of Detroit residents. Journal of Abnormal Psychology. 2014;123:533–544. doi: 10.1037/a0037046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macmillan R. Adolescent victimization and income deficits in adulthood: rethinking the costs of criminal violence from a life-course perspective. Criminology. 2000;38:553–587. [Google Scholar]
- Martin A, Rief W, Klaiberg A, Braehler E. Validity of the brief Patient Health Questionnaire mood scale (PHQ-9) in the general population. General Hospital Psychiatry. 2006;28:71–77. doi: 10.1016/j.genhosppsych.2005.07.003. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Koenen KC, Hill ED, Petukhova M, Sampson NA, Zaslavsky AM, Kessler RC. Trauma exposure and posttraumatic stress disorder in a national sample of adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52:815–830. doi: 10.1016/j.jaac.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller J, Moergeli H, Maercker A. Disclosure and social acknowledgment as predictors of recovery from posttraumatic stress: a longitudinal study in crime victims. The Canadian Journal of Psychiatry. 2008;53:160–168. doi: 10.1177/070674370805300306. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7th. Muthén & Muthén; Los Angeles, CA: 1998–2012. [Google Scholar]
- Osenback JE, Stubbs J, Wang J, Russo J, Zatzick D. Legal events as predictors of posttraumatic stress in injured trauma survivors. Psychiatry. 2009;72:70–78. doi: 10.1521/psyc.2009.72.1.70. [DOI] [PubMed] [Google Scholar]
- Polusny MA, Follette VM. Long-term correlates of child sexual abuse: theory and review of the empirical literature. Applied and Preventive Psychology. 1995;4:143–166. [Google Scholar]
- Relyea M, Ullman SE. Unsupported or turned against: understanding how two types of negative social reactions to sexual assault relate to postassault outcomes. Psychology of Women Quarterly. 2015;39:37–52. doi: 10.1177/0361684313512610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selig JP, Preacher KJ. Mediation models for longitudinal data in developmental research. Research in Human Development. 2009;6:144–164. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, Lowe B. A brief measure for assessing Generalized Anxiety Disorder: The GAD-7. Archives of Internal Medicine. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tracy M, Norris FH, Galea S. Differences in the determinants of posttraumatic stress disorder and depression after a mass traumatic event. Depression and Anxiety. 2011;28:666–675. doi: 10.1002/da.20838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uddin M, Aiello A, Wildman DE, Koenen KC, Pawelec G, de los Santos R, Goldmann E, Galea S. Epigenetic and immune function profiles associated with posttraumatic stress disorder. Proceedings of the National Academy of Sciences. 2010;107:9470–9475. doi: 10.1073/pnas.0910794107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh RM, Bruce SE. The relationships between perceived levels of control, psychological distress, and legal system variables in a sample of sexual assault survivors. Violence against Women. 2011;17:603–618. doi: 10.1177/1077801211407427. [DOI] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. [Google Scholar]
- Weathers FW, Ford J. Psychometric properties of the PTSD Checklist (PCL-C, PCL-S, PCL-M, PCL-PR) In: Stamm BH, editor. Measurement of Stress, Trauma, and Adaptation. Sidran; Lutherville, MD: 1996. pp. 250–251. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


