Abstract
Aims
The appropriate management of Medication-Related OsteoNecrosis of the Jaw (MRONJ) is still a challenge for dentists and oral surgeons and in these last years high-technology instruments have been proposed at the different steps of interventions, also combined with promoters of tissue repair.
The aim of this report is to show the advantages of a combined approach (laser and PRP) for the treatment of MRONJ.
Methods
It is described the case of a patient positive for MRONJ observed at the Odontostomatology and Maxillo-Facial Surgery Unit of the Hospital of Piacenza where surgical approach was performed by using different devices: Er:YAG laser (2940 nm) to remove and vaporize necrotic hard tissue until bleeding bone; Platelet-Rich Plasma (PRP) to stimulate hard and soft tissue healing; diode laser (808 nm) to biostimulate the surgical site.
Results
At the time of suture removal, wound closure was observed and the complete healing of the MRONJ site was observed for the 2 years follow up.
Conclusion
This case may suggest that this kind of combined approach during all the steps of MRONJ treatment allows to perform a faster and less invasive surgery with a more comfortable postoperative healing process and it represents an innovative approach in this severe adverse event.
Keywords: Medication-Related Osteonecrosis of the Jaws, Laser, Platelet-Rich Plasma, Photobiomodulation, Er:YAG laser
Introduction
Since 2003, Bisphosphonates-related Osteonecrosis of the Jaws (BRONJ) is a challenging disease for oral and maxillofacial surgeon and more recently American Association of Oral and Maxillofacial Surgeons (AAOMS) proposed for it the new definition “Medication-related Osteonecrosis of the Jaws (MRONJ)” due to the growing number of osteonecrosis developed in patients treated with other kind of antiresorptive and anti-angiogenic drugs (e.g. denosumab and sunitinib) 1).
Treatment of MRONJ is still discussed even if surgery with different degrees of invasive therapies (from curettage to wide resection) on the basis of the stage and/or of the size seems to have a key role 1, 2).
Literature about treatment of MRONJ describes lasers as useful devices thanks to the ability to perform the removal of necrotic bone; in particular, the tissue vaporization by Er:YAG laser (wavelength = 2940 nm) is very effective due to its affinity to the water and hydroxyapatite as well as to the biomodulation of both soft and hard tissues which is obtained by all the wavelengths in the range of visible and near infrared light 3,4).
Platelet-Rich Plasma (PRP) has been proposed for different bone diseases in maxilla-facial surgery and in other medical fields; in fact the presence in PRP of many growth factors as epidermal growth factor (EGF), fibroblast growth factor (FGF), insulin-like growth factor (IGF), keratinocyte growth factor (KGF), platelet-derived growth factor (PDGF), transforming growth factor-β (TGF-β) modulates and prevents excessive recruitment of inflammatory leukocytes and vascular endothelial growth factor (VEGF) 5–7).
Case report
Medical history
The patient here described was a 60 year-old man with a kidney cancer diagnosed 3 years before the first observation at our Unit. Due to his positivity to bone metastasis, he was treated with Zoledronate (4 mg every 4 weeks with infusion over a period of 15 min) and Sunitinib (50 mg taken every day for 4 weeks or 28 days, then stopped for 2 weeks or 14 days) during 30 months.
He had no comorbidity, he was not assuming any other drug and he did not undergo radiotherapy. Patient assumed as corticosteroid treatment prednisone 25 mg/day per os at the same time of Sunitinib treatment. He had no dental extraction previously our first observation.
Clinical examination
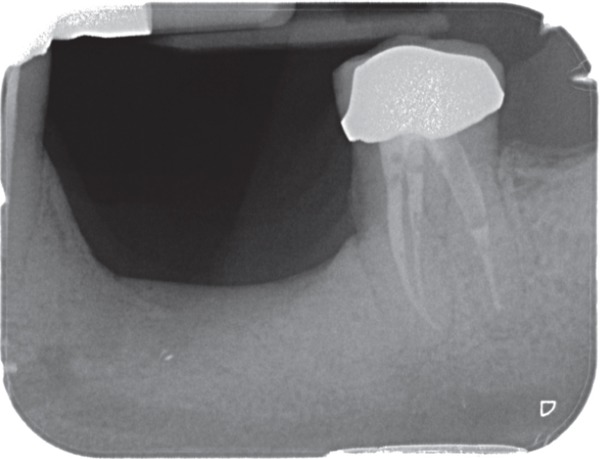
At the first oral examination patient showed a bone exposure (about 2 cm) at mandibular level in premolar left zone where two dental implants have been placed 10 years before; bone necrosis was evaluable also at radiographic view (Figure 1).
Figure 1:
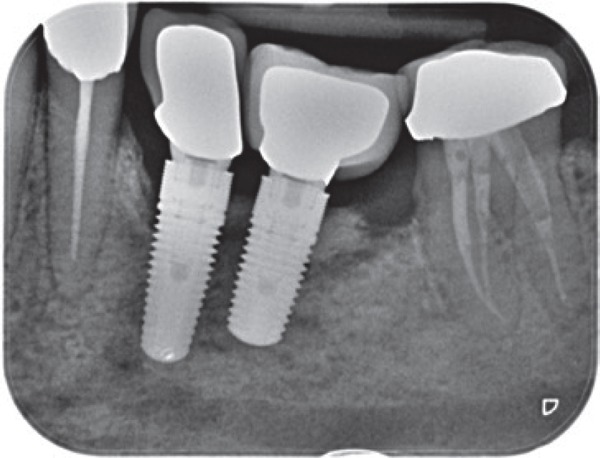
Radiographic view of bone necrosis in left mandible at dental implants level.
He complained of pain and bleeding, which appeared about 30 months after the beginning of bis-phosphonate and Sunitinib therapy: this case of Medication-Related Osteonecrosis of the Jaws (MRONJ) was classified as a Stage II accordingly to Ruggero staging system.
Treatment
Patient interrupted bisphosphonates and Sunitinib therapy at the time of first oral evaluation, according to his oncologists' approval, and he was treated with a medical approach consisting in amoxicillin 2 g/die per os and metronidazole 500 mg/die per os and mouthwashes with chlorhexidine and hydrogen peroxide.
Antibiotic therapy was started 3 days before surgery and continued for at least 2 weeks after surgery.
Surgical intervention was realized with Er:YAG laser device (2940 nm - Lightwalker - Fotona - Slovenia) to perform vaporization of necrotic bone until the observation of bleeding, considering that as sign of viable, non MRONJ affected bone. Er:YAG laser was used with a mirror handpiece for non-contact application (R02) at a distance of about 0.8 cm corresponding to the same incidence on tissue for laser light and air-water spray with an energy of 200 mJ and a frequency of 20 Hz in Medium Short Pulse (Fluence/pulse: 39.80 J/cm2) (Figures 2–3).
Figure 2:
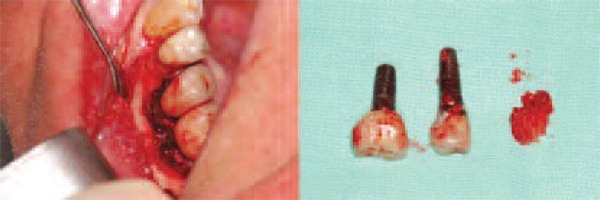
Removal of necrotic bone and implants.
Figure 3:
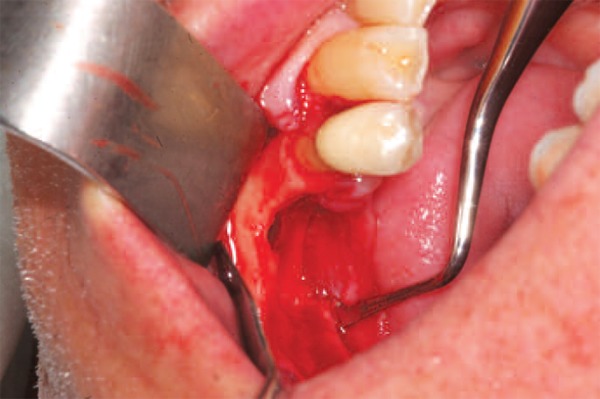
Mandibular aspect after removal of implants and necrotic bone and after Er.YAG laser vaporization.
A diode laser 808 nm was used to perform bio-modulating sessions in both intraoperative and postoperative time: first irradiation was started just after the suturing while the subsequent ones 2 times/week until the removal of suture on a completely closed surgical wound. Biomodulation was performed with a 600 µm diameter fiber on a scanning mode on the surgical site with 1 W power in continuous and non-contact mode during 1 minute for 5 times (Theorical fluence: 21231 J/cm2).
Autologous platelet gel was prepared at the Department of Immunohematology and Transfusion Medicine of the Hospital of Piacenza (Italy) during the planning of the surgery and stored until the day of the intervention. Multiple samples of whole blood were taken and collected in 10 ml vacutainers. Blood was then centrifuged at 180 rpm per 10′ in order to separate concentrated erythrocytes from platelet rich plasma (PRP) and then PRP was stored at −40°C.
The day of the surgery, PRP was maintained at room temperature until the use and just before that was added with thrombin, prepared by adding calcium gluconate, to activate platelets and accelerate the gelling process.
PRP gel was used directly in gel on the wound, absorbed on fibrin sponge and injected with a syringe after suture directly in the wound (Figure 4).
Figure 4:
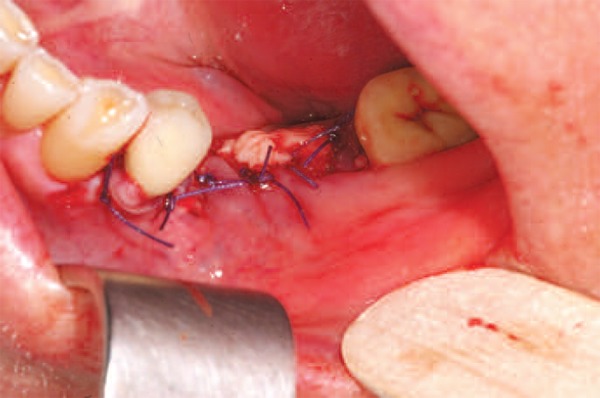
Surgical suture after the placement of PRP gel.
Patient underwent surgical treatment followed by curettage of the residual cavity to remove necrotic bone, under local anaesthesia. Suture was applied and maintained for two weeks.
At the time of suture removal, wound closure was observed and the complete healing of the MRONJ site was observed for the 2 years follow up (Figures 5–6–7).
Figure 5:

Aspect of the 3 months follow up.
Figure 6:
Rx of the 2 years follow up.
Figure 7:

Aspect of the 2 years follow up.
Discussion
The case we described in this paper is emblematic for the advantages we can obtain in MRONJ treatment thanks to the use of a combined approach.
Er:YAG laser surgery allows us to vaporize the necrotic bone with a good control of the surgical site thanks to the affinity of this wavelength (2940 nm) for the water and the superficial action avoiding, at the same time, thanks to the air-water spray and the wavelength properties, any temperature increase 3, 4). These aspects are related to a good comfort for the patient during and after surgery with a reduction of postsurgical morbility (with a reduction/elimination of pain and oedema) and a better and faster healing 3, 4). Aoki and colleagues reported as Er:YAG laser used for bone surgery even with high level irradiation may induce cell reactions, thanks to scattering phenomena surrounding the direct irradiated tissue, so stimulating bone regeneration 8–10). In the combined treatment performed on this patient the biostimulating effect, beyond to Er:YAG laser, was also enhanced by means of a diode laser (808 nm): this kind of approach, completely safe and comfortable for the patient, may help tissue healing through the stimulation of keratinocytes, osteoblast and endothelial cells 11, 12).
The Rationale for the use of PRP is the addition of growth factors (GFs) as epidermal growth factor (EGF), fibroblast growth factor (FGF), insulin-like growth factor (IGF), keratinocyte growth factor (KGF), platelet-derived growth factor (PDGF), transforming growth factor-β (TGF-β) and vascular endothelial growth factor (VEGF) in suffering environments as bone exposed to the action of bisphosphonates and monoclonal antibodies: in this way, after the surgical removal of necrotic bone and the decontamination of the surgical site, PRP may play a key role in induction of tissue healing by cells chemotaxis, proliferation and differentiation, angiogenesis and deposition of new extracellular matrix 6, 7).
Conclusion
The combined therapy consisting in the utilisation of Er:YAG laser, Diode laser and Platelet-Rich Plasma may be considered a good approach for the treatment of the Medication-Related Osteonecrosis of the Jaws.
References
- 1: Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, O'Ryan F. (2014): American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw—2014 update. J Oral Maxillofac Surg; 72:1938-56. [DOI] [PubMed] [Google Scholar]
- 2: Franco S, Miccoli S, Limongelli L, Tempesta A, (2014): New dimensional staging of bisphosphonate-related osteonecrosis of the jaw allowing a guided surgical treatment protocol: long-term follow-up of 266 lesions in neoplastic and osteoporotic patients from the University of Bari. International Journal of Dentistry, Article ID 935657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3: Vescovi P, Merigo E, Meleti M, Manfredi M, Guidotti R, et al. (2012): Bisphosphonates-related osteonecrosis of the jaws: a concise review of the literature and a report of a single-centre experience with 151 patients. J Oral Pathol Med; 41(3):214-21. [DOI] [PubMed] [Google Scholar]
- 4: Vescovi P, Merigo E, Meleti M, Manfredi M, Fornaini C, et al. (2014): Conservative surgical management of stage I bisphosphonate-related osteonecrosis of the jaw. Int J Dent. 2014:107690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5: Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, et al. (1998): Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. June;85(6):638-46. [DOI] [PubMed] [Google Scholar]
- 6: Oyama T, Nishimoto S, Tsugawa T, Shimizu F. (2004): Efficacy of platelet-rich plasma in alveolar bone grafting. J Oral Maxillofac Surg. May;62(5):555-8. [DOI] [PubMed] [Google Scholar]
- 7: Curi MM, Cossolin GS, Koga DH, Araújo SR, Feher O, dos Santos MO, Zardetto C. (2007): Treatment of avascular osteonecrosis of the mandible in cancer patients with a history of bisphosphonate therapy by combining bone resection and autologous platelet-rich plasma: Report of 3 cases. J Oral Maxillofac Surg. February;65(2):349-55. [DOI] [PubMed] [Google Scholar]
- 8: Aoki A, Mizutani K, Schwarz F, Sculean A, Yukna RA, Takasaki AA, Romanos GE, et al. (2015): Periodontal and peri-implant wound healing following lasertherapy. Periodontol 2000. June;68(1):217-69. [DOI] [PubMed] [Google Scholar]
- 9: Pourzarandian A, Watanabe H, Aoki A, Ichinose S, Sasaki KM, Nitta H, Ishikawa I. (2004): Histological and TEM examination of early stages of bone healing after Er:YAG laser irradiation. Photomed Laser Surg. August;22(4):342-50. [DOI] [PubMed] [Google Scholar]
- 10: Aleksic V, Aoki A, Iwasaki K, Takasaki AA, Wang CY, Abiko Y, Ishikawa I, Izumi Y. (2010): Low-level Er:YAG laser irradiation enhances osteoblast proliferation through activation of MAPK/ERK. Lasers Med Sci. July;25(4):559-69. [DOI] [PubMed] [Google Scholar]
- 11: Mergoni G, Vescovi P, Sala R, Merigo E, Passerini P, Maestri R, et al. (2016): The effect of laser therapy on the expression of osteocalcin and osteopontin after tooth extraction in rats treated with zoledronate and dexamethasone. Support Care Cancer. February;24(2):807-13. [DOI] [PubMed] [Google Scholar]
- 12: Vescovi P, Merigo E, Manfredi M, Meleti M, Fornaini C, et al. (2008): Nd:YAG laser biostimulation in the treatment of bisphosphonate-associated osteonecrosis of the jaw: clinical experience in 28 cases. Photomed Laser Surg. February;26(1):37-46. [DOI] [PubMed] [Google Scholar]


