Abstract
BACKGROUND:
Acute appendicitis is the most common surgical condition presented in emergency departments worldwide. Clinical scoring systems, such as the Alvarado and modified Alvarado scoring systems, were developed with the goal of reducing the negative appendectomy rate to 5%–10%. The Raja Isteri Pengiran Anak Saleha Appendicitis (RIPASA) scoring system was established in 2008 specifically for Asian populations. The aim of this study was to compare the modified Alvarado with the RIPASA scoring system in Kuwait population.
METHODS:
This study included 180 patients who underwent appendectomies and were documented as having “acute appendicitis” or “abdominal pain” in the operating theatre logbook (unit B) from November 2014 to March 2016. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), diagnostic accuracy, predicted negative appendectomy and receiver operating characteristic (ROC) curve of the modified Alvarado and RIPASA scoring systems were derived using SPSS statistical software.
RESULTS:
A total of 136 patients were included in this study according to our criteria. The cut-off threshold point of the modified Alvarado score was set at 7.0, which yielded a sensitivity of 82.8% and a specificity of 56%. The PPV was 89.3% and the NPV was 42.4%. The cut-off threshold point of the RIPASA score was set at 7.5, which yielded a 94.5% sensitivity and an 88% specificity. The PPV was 97.2% and the NPV was 78.5%. The predicted negative appendectomy rates were 10.7% and 2.2% for the modified Alvarado and RIPASA scoring systems, respectively. The negative appendectomy rate decreased significantly, from 18.4% to 10.7% for the modified Alvarado, and to 2.2% for the RIPASA scoring system, which was a significant difference (P<0.001) for both scoring systems.
CONCLUSION:
Based on the results of this study, the RIPASA score is a simple scoring system with better sensitivity and specificity than the modified Alvarado scoring system in Asian populations. It consists of 14 clinical parameters that can be obtained from a good patient history, clinical examination and laboratory investigations. The RIPASA scoring system is more accurate and specific than the modified Alvarado scoring system for Kuwait population.
KEY WORDS: Acute appendicitis, Modified Alvarado score, RIPASA score
INTRODUCTION
Acute appendicitis is the most common surgical condition presented in emergency departments worldwide.[1] It is also the most common cause of abdominal pain requiring surgery, with a lifetime risk of 7%.[1] The diagnosis of acute appendicitis remains an ongoing challenge for most surgeons, because acute appendicitis presents with atypical symptoms in 50% of the cases.[1] The diagnosis of acute appendicitis is based on the patient’s medical history, a clinical examination and laboratory investigations. A negative appendectomy rate of 20%–30% has been previously accepted worldwide.[2]
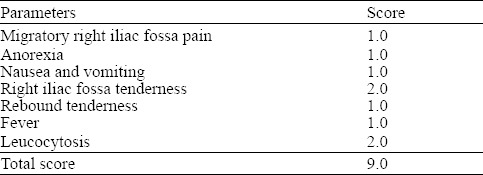
Clinical scoring systems were developed to reduce the negative appendectomy rate to 5%–10%. The most popular scoring system among surgeons is the Alvarado score, which was developed in 1986 as the simple addition of points related to eight clinical parameters (Table 1). The modified Alvarado score omitted the last point of the original score (shift to the left Neutrophils) (Table 2).[3,4] It has been shown that there were no significant differences between the outcomes of the two scores.[3,4]
Table 1.
Alvarado score
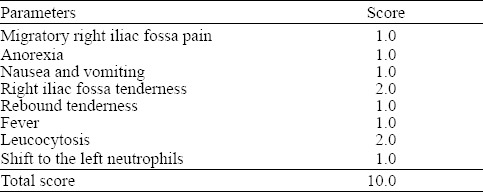
Table 2.
Modified Alvarado score
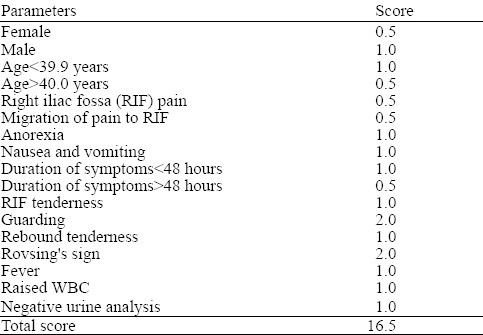
More recently, a new clinical scoring system was established, called the Raja Isteri Pengiran Anak Saleha Appendicitis (RIPASA) score,[5] and it was developed in 2008 at the Department of Surgery, Raja Isteri Pengiran Anak Saleha Hospital, Brunei Darussalam.[5] This score includes 14 clinical parameters (Table 3), and has a higher sensitivity, specificity and diagnostic accuracy than the Alvarado scoring system, especially in Asian populations.[1,5] Based on this background information, the objective of this study was to compare the modified Alvarado and RIPASA scoring systems with regard to the sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), diagnostic accuracy, predicated negative appendectomy and receiver operating characteristic (ROC) curve in Kuwait population. It is worth noting that the state of Kuwait consists of mixed ethnicities due to labour immigration.
Table 3.
RIPASA score
METHODS
This is a retrospective study consisted of 180 patients who underwent appendectomies (operating theatre logbook unit B) from November 2014 to March 2016. The inclusion criteria were as follows: any patient (from any age group) admitted for surgery with a diagnosis of acute appendicitis or abdominal pain, undergoing a diagnostic laparoscopy or open appendectomy, and a traceable approved histopathology report from a consulting pathologist. The exclusion criteria were as follows: untraceable medical records, insufficient clinical data documentation and/or an untraceable histopathology report. A total of 44 patients were excluded from the study according to our exclusion criteria. A total of 136 patients were included, with a study sample population consisting of the following nationalities: 41 (30.1%) Egyptians, 29 (21.3%) Kuwaitis, 15 (11.0%) Indians, 12 (8.8%) Filipinos, 8 (5.9%) Jordanians, 7 (5.1%) Syrians, 6 (4.4%) Sri Lankans, 4 (2.9%) Bangladeshis, 3 (2.2%) Persians, 3 (2.2%) Lebanese and 8 (5.9%) others.
The National Registration Identity Card (NRIC) is an additional parameter of the RIPASA scoring system, which is only applicable in Singapore. Therefore, this parameter was excluded because none of the patients in our study were from Singapore. The data were collected from the patients’ electronic health records in the hospital’s computer system. The histopathology reports were used as a standard confirmation of an acute appendicitis diagnosis.
Statistical analysis
The results of the various parameters were expressed as the mean±standard deviation (SD), assessed within a 95% confidence interval. The sensitivity, specificity, PPV, NPV, diagnostic accuracy and negative appendectomy rate for both scoring systems were calculated and analysed comparatively with a chi-squared test (SPSS software; SPSS Inc., Chicago, IL, USA). ROC curves were plotted for both scoring systems, and the two scoring systems were compared using the area under the curve (AUC).
RESULTS
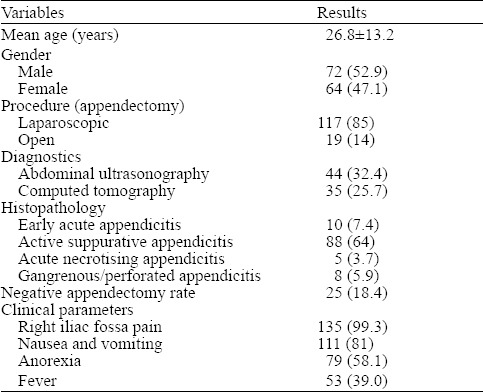
The age in our study population was 26.8±13.2 years old, with a gender distribution of 64 (47.1%) females and 72 (52.9%) males. The distribution of the clinical parameters collected for the studied sample was as follows: right iliac fossa pain 135 (99.3%), nausea and vomiting 111 (81%), anorexia 79 (58.1%) and fever 53 (39.0%).
The study population of 136 patients underwent either a laparoscopic appendectomy (n=117, 86%) or open appendectomy (n=19, 14%). The negative appendectomy rate was 25 (18.4%). The histopathological findings included early acute appendicitis in 10 (7.4%), acute suppurative appendicitis in 88 (64%), acute necrotising appendicitis in 5 (3.7%) and perforated/gangrenous appendicitis in 8 (5.9%) (Table 4).
Table 4.
Demographics of the study sample (n, %)
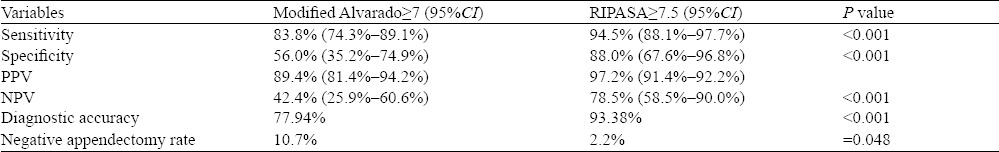
The cut-off threshold point of the modified Alvarado score was set at 7.0. This cut-off point yielded a sensitivity of 82.8% and a specificity of 56%, with a PPV of 89.3% and an NPV of 42.4%. The diagnostic accuracy of the modified Alvarado score was 77.94%. The cut-off threshold point for the RIPASA score was set at 7.5. It yielded a sensitivity of 94.5%, a specificity of 88.0%, a PPV of 97.2% and an NPV of 78.5%. The diagnostic accuracy of the RIPASA score was 93.38%. The predicted negative appendectomy rates were 10.7% and 2.2% for the modified Alvarado and RIPASA scoring systems, respectively, which was statistically significant (P=0.048). The negative appendectomy rate decreased significantly from 18.4% to 10.7% for the modified Alvarado and to 2.2% for the RIPASA scoring system, which was a significant difference (P<0.001) for both scoring systems (Table 5).
Table 5.
Comparison between the modified Alvarado and RIPASA scores
ROC curves were calculated for the modified Alvarado and RIPASA scoring systems (Figure 1). The AUC was 0.686 (68.6%) for the modified Alvarado and 0.876 (87.6%) for the RIPASA score. The difference in the AUCs (18.9%) was significant between the scoring systems (P<0.001), which was equal to 26 patients from our sample population being correctly diagnosed using the RIPASA score and misdiagnosed using the modified Alvarado score.
Figure 1.
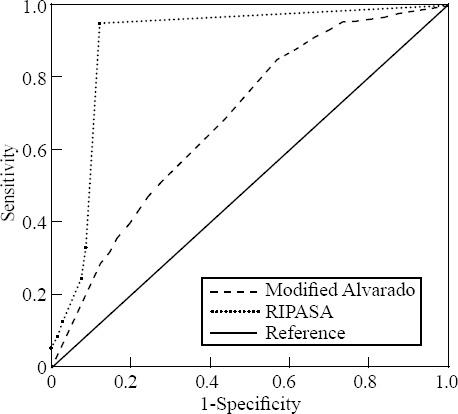
ROC plots for the modified Alvarado and RIPASA scoring systems.
DISCUSSION
Acute appendicitis can be challenging for surgeons because of appendectomy delays and problems with diagnostic accuracy.[6] A delay in performing an appendectomy may increase the risk of appendicular perforation or an appendicular inflammatory mass. Moreover, the rate of negative appendectomies is 20%–30%.[6] Several studies consider this rate to be unacceptable.[6,7] Improving diagnostic accuracy and reducing the negative appendectomy rate can be achieved through the use of several diagnostic investigations, such as computed tomography (CT) and ultrasonography, although these can increase the overall healthcare costs. In addition, several diagnostic scoring systems have been developed. The most popular scoring systems are the Alvarado score and the modified Alvarado score.[8,9] These scoring systems have good sensitivity and specificity when used in Western populations,[8,9] but they have less sensitivity and specificity for Asian populations. Therefore, a new scoring system, the RIPASA, was developed with better sensitivity and specificity than the Alvarado scores, especially in Asian populations.[1,5,10] The RIPASA scoring system is a simple system consisting of 14 fixed parameters (Table 3). These clinical parameters can be obtained from a good patient history, a clinical examination and laboratory investigations. Scores of 0.5, 1.0 and 2.0 are allocated to each clinical parameter, weighing their probability in diagnosing acute appendicitis.[11]
In the present study, the modified Alvarado score cut-off point was set at 7.0. This cut-off point yielded a sensitivity of 82.8%, a specificity of 56%, a PPV of 89.3% and an NPV of 42.4%. The diagnostic accuracy was 77.94%. Previous studies by Chong et al[12] have utilised Alvarado scores in which the sensitivity, specificity, PPV, NPV and diagnostic accuracy were 68.3%, 87.9%, 86.3%, 71.4% and 86.5%, respectively.
In our study, the RIPASA score results showed a sensitivity of 94.5%, a specificity of 88.0%, a PPV of 97.2%, an NPV of 78.5% and a diagnostic accuracy of 93.38%. Chong et al[12] detailed sensitivity, specificity, PPV, NPV and diagnostic accuracy rates of 98.0%, 81.3%, 85.3%, 97.4% and 91.8%, respectively, using the RIPASA score. In addition, Rathod et al[1] produced a sensitivity of 82.61% and a specificity of 88.89% using the RIPASA score, as well as a PPV of 96.61%, an NPV of 57.14% and a diagnostic accuracy of 83.91%.
The comparison of the modified Alvarado score and RIPASA score in our study is shown in Table 5. Overall, the sensitivity and specificity were better with the RIPASA than with the modified Alvarado score. Regarding the NPV and diagnostic accuracy, the RIPASA score was also better. The predicted negative appendectomy rates were better with RIPASA than the modified Alvarado scoring systems; however, the statistically significant was weak (P=0.048). The total negative appendectomy rate in our study was 18.4%, a rate comparable to those of Chong et al[5] and Rathod et al,[1] who documented rates of 22.9% and 20.69%, respectively.
CT scans have been reported as having a high sensitivity (94%) and specificity (95%) for diagnosing acute appendicitis.[13] Therefore, performing a CT scan would improve the diagnosis of acute appendicitis, but it would increase the healthcare costs. Unfortunately, the sensitivity, specificity and diagnostic accuracy of the modified Alvarado and RIPASA scores in our study were lower than those of a CT scan.[13]
The Appendicitis Inflammatory Response (AIR) score has a better sensitivity and specificity than the Alvarado and the modified Alvarado scoring systems.[14] It is similar to the modified Alvarado and RIPASA in that the AIR score can be calculated from the clinical parameters and two important laboratory investigations (leucocytosis and C-reactive protein).[14,15] The AIR score has a minimum value of five and a maximum value of 12, and it is presumed to assess the severity of acute appendicitis in relation to leucocytosis, the C-reactive protein and segmented neutrophils.[15] In addition, the AIR score has shown better results than the Alvarado score,[16] which yielded a value greater than four and a sensitivity and specificity of 97% and 77%, respectively,[16] whereas the AIR score had a value greater than 8 and yielded a sensitivity and specificity of 12% and 100%, respectively.[16]
Study limitations and weaknesses
This was a retrospective study that depended on the accuracy of the clinical documentation in our medical records. The establishment of the diagnosis of acute appendicitis in our sample population was based on the clinical judgment of the surgical specialist registrar on duty. Furthermore, different diagnostic modalities (CT or abdominal ultrasonography) were used in selected patients in our emergency medicine department (Table 4); therefore, the negative appendectomy rate in our study was higher than that of other studies.
CONCLUSION
The RIPASA score is a simple system with better sensitivity and specificity than the modified Alvarado score. It consists of 14 clinical parameters that can be obtained from a good patient history, a clinical examination and laboratory investigations. Our results showed that the RIPASA score had a better sensitivity, specificity, NPV and diagnostic accuracy than the modified Alvarado score in general. However, further studies are needed to confirm this impression.
Footnotes
Funding: None.
Ethical approval: The study was approved by the Institutional Review Board.
Conflicts of interest: The authors declare that there are no conflicts of interest regarding the publication of this paper.
Contributors: Shuaib A proposed the study, analyzed the data and wrote the first drafts. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
- 1.Rathod S, Ali I, Bawa AP, Singh G, Mishra S, Nongmaithem M. Development of the RIPASA score:a new appendicitis scoring system for the diagnosis of acute appendicitis. Singapore Med J. 2010;51(3):220–5. [PubMed] [Google Scholar]
- 2.Wani MM, Yousaf MN, Khan MA, Abdul B, Durrani M, Shafi M. Usefulness of the Alvarado scoring system with respect to age, sex and time of presentation, with regression analysis of individual parameters. Internet J Surg. 2007;11:562–9. [Google Scholar]
- 3.Kalan M, Talbot D, Cunliffe WJ, Rich AJ. Evaluation of the modified Alvarado score in the diagnosis of acute appendicitis:a prospective study. Ann R Coll Surg Engl. 1994;76(6):418–9. [PMC free article] [PubMed] [Google Scholar]
- 4.Kanumba ES, Mabula JB, Rambai P, Chalya PL. Modified Alvarado Scoring System as a diagnostic tool for acute appendicitis at Bugando Medical Centre, Mwanza, Tanzania. BMC Surg. 2011;11:4. doi: 10.1186/1471-2482-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chong CF, Thien A, Mackie AJ, Tin AS, Tripathi S, Ahmad MA, et al. Evaluation of the RIPASA score:A new scoring system for the diagnosis of acute appendicitis. Singapore Med J. 2010;51(3):220–5. [PubMed] [Google Scholar]
- 6.Gilmore OJ, Browett JP, Griffin PH, Ross IK, Brodribb AJ, Cooke TJ, et al. Appendicitis and mimicking conditions. Lancet. 1975;2(7932):421–4. doi: 10.1016/s0140-6736(75)90841-7. [DOI] [PubMed] [Google Scholar]
- 7.Antel J, Rivera L, Landenberg B, Halm G, Fatava MA, Brown CVR. Clinical diagnostic pathway for acute appendicitis:prospective validation. JAM Coll Surg. 2006;203(6):849–56. doi: 10.1016/j.jamcollsurg.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 8.Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15:557–65. doi: 10.1016/s0196-0644(86)80993-3. [DOI] [PubMed] [Google Scholar]
- 9.Owen TD, Williams H, Stiff G, Jenkinson LR, Rees BI. Evaluation of the Alvarado score in acute appendicitis. JR Soc Med. 1992;85:87–88. doi: 10.1177/014107689208500211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.N N, Mohammed A, Shanbhag V, Ashfaque K, S A P. A comparative study of RIPASA Score and ALVARADO Score in the diagnosis of acute appendicitis. J Clin Diagn Res. 2014;8(11):NC03–5. doi: 10.7860/JCDR/2014/9055.5170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ünlüer EE, Urnal R, Eser U, Bilgin S, Hacıyanlı M, Oyar O, et al. Application of scoring systems with point-of-care ultrasonography for bedside diagnosis of appendicitis. World J Emerg Med. 2016;7(2):124–9. doi: 10.5847/wjem.j.1920-8642.2016.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chong CF, Thien A, Mackie AJ, Tin AS, Tripathi S, Ahmad MA, et al. Comparison of RIPASA and Alvarado scores for the diagnosis of acute appendicitis. Singapore Med J. 2011;52(5):340–5. [PubMed] [Google Scholar]
- 13.Terasawa T, Blackmore CC, Bent S, Kohlwes RJ. Systematic review:Computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents. Ann Intern Med. 2004;141:537–46. doi: 10.7326/0003-4819-141-7-200410050-00011. [DOI] [PubMed] [Google Scholar]
- 14.Andersson M, Andersson RE. The appendicitis inflammatory response score:a tool for the diagnosis of acute appendicitis that outperforms the Alvarado score. World J Surg. 2008;32:1843–9. doi: 10.1007/s00268-008-9649-y. [DOI] [PubMed] [Google Scholar]
- 15.Von-Mühlen B, Franzon O, Beduschi M, Kruel N, Lupselo D. Air score assessment for acute appendicities. ABCD Arq Bras Cir Dig. 2015;28(3):171–173. doi: 10.1590/S0102-67202015000300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Malyar AA, Singh B, Dar HM, Ahmad MM, Bhat SB. A comparative study of appendicitis inflammatory response (AIR) score with Alvarado score in diagnosis of acute appendicitis. BMMR. 2015;18(3):72–76. [Google Scholar]


