Emergency medicine is a recognized specialty in the United Kingdom (UK), with formal training and accreditation conducted and governed by the Royal College of Emergency Medicine.1 Health care in the UK is publicly funded and provided by the National Health Service (NHS) through a residence-based (rather than insurance-based) system. Emergency care within emergency departments (EDs) is currently provided free at the point of delivery for everyone, including non-UK residents.
Although emergency care in the UK is under the control of a single-payer provider (the NHS), there is currently no single, clinically driven, standardized data set for emergency care in the UK. Each ED manages the collection and storage of data related to its patients, as required for their care, through locally developed processes for electronic data collection, format, and storage. These processes may still include the use of paper records during treatment, to be transcribed to an electronic patient record at a later date. Numerous electronic clinical information systems are currently in use, with many differences in data formats by location, even those running the same software.
In England, a subset of the data for each ED visit is collected nationally, to monitor activity and for payment purposes, in the Accident and Emergency Commissioning Data Set (hereinafter, CDS), currently type 010.2 Created in the 1980s3 and maintained by NHS Digital (as required by NHS and the UK Department of Health), the CDS is not collated centrally in real time. Each hospital submits data more or less monthly after a series of completion and validation processes. In certain circumstances, an anonymized extract of the CDS is made available through the NHS Secondary Uses Service4 for further reporting and analysis to support the delivery of NHS health care and for public health purposes.
Emergency Department Syndromic Surveillance in England
ED syndromic surveillance uses an anonymized feed of electronic records of ED visits to identify and monitor trends in human health at the more severe end of the disease spectrum (ie, those requiring acute hospital care). The Public Health England Emergency Department Syndromic Surveillance System (EDSSS) was originally developed as part of public health preparations for the London 2012 Olympic and Paralympic Games to meet the surveillance requirements of hosting such a large mass-gathering event.5
Although public health is listed as a purpose for the NHS Secondary Uses Service, there is no provision or potential for real-time surveillance usage, given the delay between patient visits and data submission to the CDS. This time delay limited the potential for developing real-time ED surveillance systems in the UK and required that the EDSSS be developed as a sentinel surveillance system, relying on the recruitment of individual EDs on an ad hoc basis. This approach required the agreement and clinical support of each ED, followed by a complex and often lengthy process of liaison with, and reassurance to, the information governance teams responsible for data security.
In collaboration with the Royal College of Emergency Medicine, the EDSSS was developed after identifying the types of clinical information that would be useful for syndromic surveillance (eg, nonidentifiable patient demographic characteristics, diagnoses based on coded information rather than free text, dates and times of visits, and the destinations of patients upon leaving the ED). Processes were developed to access, anonymize, and translate the information held in clinical software systems in individual EDs to a standardized format based on the Royal College of Emergency Medicine’s suggested minimum data set for emergency care.5 The resultant EDSSS process of secure data extraction and daily transfer to Public Health England is automated, with no additional resources required by participating EDs, resulting in a unique, anonymized data set that is collected, stored, and used solely for public health purposes.
The EDSSS provided a valuable contribution to overall surveillance during the London 2012 Olympic and Paralympic Games and continued to develop after the Olympics were over, remaining as a public health legacy of the Games, contributing to national surveillance programs and vaccine-impact studies, and supporting the response to public health incidents.6–10
By December 2016, 35 EDs in England and Northern Ireland were reporting to the EDSSS.11 Five additional EDs had reported previously; however, because of the bespoke nature of the EDSSS data transfer setup, whenever a software system in a reporting ED changes—resulting in differences in the local data set format and storage—the EDSSS data transfer setup for EDSSS is no longer valid, and the ED is lost from the EDSSS.
The Emergency Care Data Set Project: Emergency Care Evolution
The Emergency Care Data Set (ECDS) project is a collaborative project initiated by the Royal College of Emergency Medicine in early 2015, with representation from government and nongovernment bodies on the project board.3,12 The ECDS project aims to improve the collection, quality, and completeness of data in EDs in England through a single, mandated, standardized data format to be implemented during 2017-2018 in all EDs, across all software systems. The primary aim is to improve the quality of clinical data captured in EDs, thus improving the delivery of clinical care and treatment of patients. Furthermore, the ECDS project aims to make better use of information captured in the EDs, including streamlining local methods for forwarding information for individual patient care (eg, letters to general practitioners). Promoting completion of the patient care record in electronic systems in real time, through use of the ECDS, would also make information on capacity, demand for services, and workload in each department more accessible locally.
Some EDs already collect additional details on patient visits, such as injuries resulting from violence, to fulfill specific project needs or research interests. The ECDS project would standardize the capability for collecting additional detail across all EDs in England.
The next step in the ECDS project is to replace the existing CDS type 010, allowing collection of an updated and extended data set that would more accurately describe activity across EDs in England. This extended data set would also improve the availability of data for and amount of information included in the NHS Secondary Uses Service, enabling better provision for performance management, surveillance, and research, in addition to local commissioning of and payment for ED services delivered. There is also the potential to make CDS submission a contemporaneous process, making information available in near-real time, providing a national picture of supply and demand in a more timely manner than is currently possible. Implementation of the ECDS, which will be known as CDS type 011–ECDS,13 will be mandated in consultant-led (type 1 and type 2) EDs by October 2017 and in others (minor injury and walk-in centers: type 3 and type 4) by October 2018.3
How Syndromic Surveillance Helped the ECDS Project
Syndromic surveillance systems use electronic health data collected for patient care to provide information for public health action on a population level rather than an individual level. As described previously, each NHS ED currently has its own method for collecting patient information. The EDSSS has helped to identify similarities across existing ED systems, where details can be extracted in a standard format and transmitted securely in an anonymized daily feed. The EDSSS successfully provided proof of concept of this process without causing additional work within EDs. EDs have been passively providing more detail in the surveillance picture for infectious diseases (eg, influenza and respiratory syncytial virus surveillance6,10) and the impact of other events (eg, air pollution, heat waves, extreme cold weather7–9).
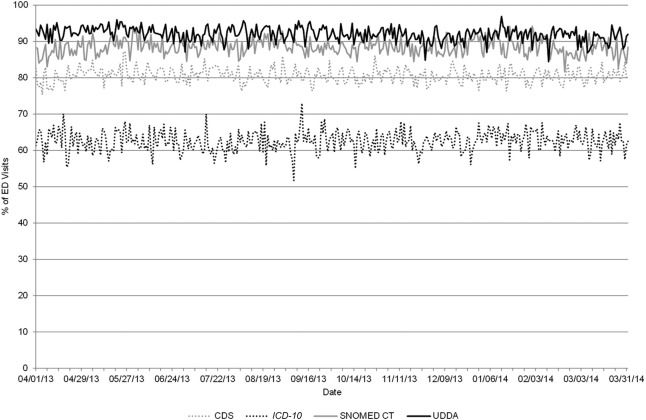
As part of this process, several EDs reporting to the EDSSS adopted a standard list of clinical diagnosis codes (the Unified Diagnostic Dataset)—a first step to make diagnosis recording easier in the ED—with the intention that patients with a condition such as croup should receive the same diagnosis code regardless of which ED or clinician treats them. Those EDs using the Unified Diagnostic Dataset to record diagnoses illustrated higher levels of coding when compared with other EDSSS EDs using existing diagnostic coding data sets (Figure).
Figure.
Daily percentage of emergency department (ED) visits reported to the Public Health England Emergency Department Syndromic Surveillance System for which a diagnosis code was recorded, April 1, 2013, to March 31, 2014. EDs grouped by diagnostic coding system used. Abbreviations: CDS, Commissioning Data Set; ICD-10, International Classification of Diseases, Tenth Revision; SNOMED CT, Systematized Nomenclature of Medicine, Clinical Terms; UDDA, Unified Diagnostic Dataset.
How a Standardized ED Data Set Could Help Syndromic Surveillance
The implementation of the ECDS would immediately remove the primary hurdle that has inhibited growth of the EDSSS: the lack of a standardized system to capture data in EDs. Additionally, proposed changes to the CDS reporting infrastructure would result in a single national ED data repository, which, if collected in near-real time, would potentially make all EDs in England available for recruitment to the EDSSS through a central resource, rather than individually. The expansion of the EDSSS to all EDs in England would increase the system’s ability to report on local public health incidents, improve data quality with regard to signal-to-noise ratio, and make the EDSSS a leading national ED syndromic surveillance system internationally.
The expansion of data recording to include simplified injury fields, as proposed by the ECDS project,13 would also allow the EDSSS to provide real-time information on accidental injuries and violence across the country and locally. Although many EDs may already collect data on injuries for local public health initiatives or research, these data are not currently accessible by the EDSSS.
The ECDS project is currently focused on EDs in England but is being watched closely by colleagues in devolved administrations (Scotland, Wales, and Northern Ireland). Northern Ireland already participates in the EDSSS, with 5 EDs reporting daily. Because implementation of the ECDS would likely allow the simple expansion of the EDSSS across more (if not all) EDs in England, it has the potential to become a standard throughout the UK. A single, formal, standardized ED data set, mandated by the NHS, would enable harmonization of surveillance activities across the UK. The publication of the ECDS structure and the EDSSS outputs also has the potential to harmonize surveillance efforts with other countries, into Europe, and further afield. The data need not be shared; however, a more easily understood format and structure would allow similarities to be identified, enable direct comparison across borders, and improve resilience to and provide information for action during large public health incidents (eg, influenza pandemics or volcanic ash clouds).
What’s New in This Approach
Mandated changes to national clinical emergency care data sets, such as the one proposed in the ECDS project, are infrequent but have been executed before (eg, in France14). The workload required to implement the ECDS is substantial, including needs and impact assessments, stakeholder consultations, and pilot trials of potential technological solutions. However, this process has allowed the ECDS to be developed in a novel way, including all stakeholders in emergency care, from ED clinicians and patient representatives to potential secondary users of the data, such as those in public health.
Patient care and NHS operational benefits are the driving factors for implementation of the ECDS: syndromic surveillance aims to have no impact on frontline staff members. In this instance, however, rather than remaining behind the scenes, syndromic surveillance has become part of a wider multidisciplinary conversation, demonstrating what is possible.
After introduction of the ECDS, the EDSSS could become a standard, mandated item in public health surveillance in England. Again, the requirement for ED data to be submitted nationally for syndromic surveillance purposes has been achieved elsewhere; participation in ED surveillance became mandatory in France in July 2013.14 However, we believe that the ECDS development process would be the first example of syndromic surveillance being included in the development of national ED data changes.
Improvements in the collection and delivery of more timely and better-quality data on ED visits will have a wider-reaching impact than syndromic surveillance and benefit other aspects of the public health system. The evolution of the emergency care electronic health record in England will result in a revolution in ED syndromic surveillance, delivering a national system that can provide an enhanced surveillance capability for years to come.
Acknowledgments
We acknowledge the ongoing work of the ECDS project board, the contribution of and support from ED clinicians and NHS Trust staff members to the EDSSS, the ongoing support of the Royal College of Emergency Medicine, and the technical support provided by EMIS Health and L2S2 Ltd in developing the EDSSS.
Authors’ Note: The views expressed are those of the authors and are not necessarily those of the National Health Service, the National Institute for Health Research, the Department of Health, or Public Health England.
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Thomas C. Hughes is employed as the clinical lead of the Emergency Care Data Set project but has no financial interest in its implementation.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Alex J. Elliot and Gillian E. Smith receive support from the National Institute for Health Research Health Protection Research Unit in Emergency Preparedness and Response. Helen E. Hughes receives support from the National Institute for Health Research Health Protection Research Unit in Gastrointestinal Infections.
References
- 1. The Royal College of Emergency Medicine. About the college. http://www.rcem.ac.uk/RCEM/About/RCEM/About_Us/About_the_College.aspx. Accessed March 8, 2017.
- 2. NHS Digital. CDS V6-2 type 010—accident and emergency commissioning data set. http://www.datadictionary.nhs.uk/data_dictionary/messages/cds_v6-2/data_sets/cds_v6-2_type_010_-_accident_and_emergency_cds.asp?shownav=1. Accessed March 8, 2017.
- 3. NHS England. Emergency care data set (ECDS). https://www.england.nhs.uk/ourwork/tsd/ec-data-set . Accessed March 8, 2017.
- 4. NHS Digital. Secondary uses service. http://www.datadictionary.nhs.uk/data_dictionary/nhs_business_definitions/s/secondary_uses_service_de.asp?shownav=1?query=%22sus%22&rank=100&. Accessed March 8, 2017.
- 5. Elliot AJ, Hughes HE, Hughes TC, et al. Establishing an emergency department syndromic surveillance system to support the London 2012 Olympic and Paralympic Games. Emerg Med J. 2012;29(12):954–960. [DOI] [PubMed] [Google Scholar]
- 6. Pebody RG, Green HK, Andrews N, et al. Uptake and impact of vaccinating school age children against influenza during a season with circulation of drifted influenza A and B strains, England, 2014/15. Euro Surveill. 2015;20(39):37–47. [DOI] [PubMed] [Google Scholar]
- 7. Smith S, Elliot AJ, Hajat S, et al. Estimating the burden of heat illness in England during the 2013 summer heatwave using syndromic surveillance. J Epidemiol Community Health. 2016;70(5):459–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Smith GE, Bawa Z, Macklin Y, et al. Using real-time syndromic surveillance systems to help explore the acute impact of the air pollution incident of March/April 2014 in England. Environ Res. 2015;136:500–504. [DOI] [PubMed] [Google Scholar]
- 9. Hughes HE, Morbey R, Hughes TC, et al. Using an emergency department syndromic surveillance system to investigate the impact of extreme cold weather events. Public Health. 2014;128(7):628–635. [DOI] [PubMed] [Google Scholar]
- 10. Hughes H, Morbey R, Hughes T, et al. Syndromic surveillance of respiratory pathogens using routine ED data in England. Online J Public Health Inform. 2015;7(1):e81. [Google Scholar]
- 11. Public Health England. Emergency Department Syndromic Surveillance System: England & Northern Ireland [weekly bulletin]. Week 49. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/587943/EDSSSBulletin2016wk49.pdf. Published 2016. Accessed March 8, 2017.
- 12. The Royal College of Emergency Medicine. Informatics: emergency care data set (ECDS). http://www.rcem.ac.uk/RCEM/Quality-Policy/Professional_Affairs/Informatics_ECDS.aspx?WebsiteKey=b3d6bb2a-abba-44ed-b758-467776a958cd&hkey=8b5437c1-d7a9-47b7-a8d6-acfca418606e&New_ContentCollectionOrganizerCommon=2#New_ContentCollectionOrganizerCommon. Accessed March 8, 2017.
- 13. NHS Digital. SCCI0092-2062. Commissioning data sets (CDS) version 6.2: addition of type 011. Emergency care data set (ECDS). http://www.content.digital.nhs.uk/isce/publication/SCCI0092-2062. Accessed March 8, 2017.
- 14. Pontais I, Bousquet V, Ruello M, et al. Factors influencing the stability and quality of the French ED surveillance system. Paper presented at: International Society for Disease Surveillance Conference; December 9-10, 2015; Denver, CO. [Google Scholar]