Abstract
Introduction:
Mass gatherings that attract a large international presence may cause or amplify point-source outbreaks of emerging infectious disease. The Los Angeles County Department of Public Health customized its syndromic surveillance system to detect increased syndrome-specific utilization of emergency departments (EDs) and other medical encounters coincident to the 2015 Special Olympics World Games.
Materials and Methods:
We queried live databases containing data on ED visits, California Poison Control System calls, and Los Angeles County coroner-investigated deaths for increases in daily counts from July 19 to August 6, 2015. We chose syndrome categories based on the potential for disease outbreaks common to international travel and dormitory settings, morbidity amplified by high temperatures, and bioterrorism threats inherent to mass gatherings. We performed line-list reviews and trend analyses of total, syndrome-specific, and region-specific daily counts, using cumulative sum-based signals. We also piloted a novel strategy of requesting that ED registrars proactively tag Special Olympics attendees in chief complaint data fields.
Results:
The syndromic surveillance system showed that the 2015 Special Olympics did not generate large-scale acute morbidities leading to detectable stress on local EDs. We recruited 10 hospitals for proactive patient tagging, from which 16 Special Olympics attendees were detected; these patients reported various symptoms, such as injury, vomiting, and syncope.
Practice Implications:
As an enhancement to traditional syndromic surveillance, proactive patient tagging can illuminate potential epidemiologic links among patients in challenging syndromic surveillance applications, such as mass gatherings. Syndromic surveillance has the potential to enhance ED patient polling and reporting of exposure, symptom, and other epidemiologic case definition criteria to public health agencies in near-real time.
Keywords: syndromic surveillance, mass gathering, Special Olympics, patient tagging
The 2015 Special Olympics World Games in Los Angeles, California, attracted 500 000 spectators, 30 000 volunteers, 6500 athletes, and 2000 coaches in the year’s largest sporting event in the world.1 The opening ceremonies were held on July 25, 2015, and kicked off 9 days of 25 athletic events at 27 venues. The athletes and their delegations arrived from 165 countries—an even larger international representation than the 1984 Summer Olympics hosted in Los Angeles.2
The Special Olympics presented unique challenges for public health surveillance because of the high number of attendees, the duration of the Games, the geographic complexity involving several venues, and the influx of international visitors. In preparation, Los Angeles County’s (LA County’s) syndromic surveillance team participated in a planning meeting and subsequent communications with Special Olympics organizers, area hospital representatives, and local emergency management and public health authorities. Sick or injured athletes were to be treated at medical stations located at each venue and then transported to 1 of 2 polyclinics or to local emergency departments (EDs) for more intensive care if needed. The Special Olympics organizing committee was to track athlete medical encounters by equipping medical personnel with a smartphone application called RaceSafe3; however, medical encounters for spectators and volunteers were not tracked. Therefore, LA County’s syndromic surveillance system served an important complementary role in providing enhanced near–real-time surveillance during the Special Olympics in populations that were otherwise unmonitored.
The mainstay of LA County’s syndromic surveillance system is its ED data feeds, which draw near–real-time data from >65% of ED patients in LA County. Keyword searches are performed on data fields containing chief complaints, triage notes, and diagnosis information. In addition, California Poison Control System calls and death data investigated by the LA County Department of Medical Examiner-Coroner are transmitted daily and assessed through keyword searches in the caller complaint and death description data fields.
We created a syndromic surveillance strategy for the 2015 Special Olympics based on anticipated areas of public health concern. Most documented illnesses at previous mass gatherings resulted from noncommunicable causes, such as heat-related illness, cardiovascular ischemia, and physical injuries.4 Although communicable disease outbreaks are much less common, gastrointestinal and respiratory-transmitted illnesses, such as salmonellosis and measles, have been reported at previous international mass-gathering sporting events.5 However, since a 2002 influenza outbreak, no infectious disease outbreaks have been documented at summer or winter Olympic Games.6 For the 2015 Special Olympics, we expected a potential increase in heat-related morbidity, as well as fatigue caused by the stress of crowded environments and competition. Vaccine-preventable disease was also a concern because of the large influx of international athletes and their delegations, who were not required to provide proof of vaccination. Special Olympics athletes were also to be housed in dormitory settings for 9 days—ideal environments for the spread of highly contagious diseases, such as meningitis and norovirus.7
Using syndromic surveillance to monitor health events at mass gatherings is not new; syndromic surveillance was used during the 2002 Olympic Winter Games in Salt Lake City, Utah, and for the 2012 Olympic Summer Games in London.8,9 We aimed to enhance the effectiveness of traditional syndromic surveillance by piloting proactive patient tagging, a polling technique used to identify ED visits associated with Hurricane Irene in 2011.10 We describe how LA County’s syndromic surveillance system was customized to address various public health concerns, detect emerging health events congruent to the 2015 Special Olympics Games, and gauge the potential added value of proactive patient tagging.
Materials and Methods
Identifying Special Olympics Attendees
Two weeks before the start of the Special Olympics, nurse liaisons from the hospital outreach unit of LA County’s Acute Communicable Disease Control Program emailed a letter to infection preventionists at all participating syndromic hospitals, requesting that ED staff members proactively tag patient records of known attendees with “Special Olympics” in their chief complaint data field. We offered hospitals that responded to the outreach letter assistance with validating test patients and accommodated alternative data fields for keyword entry upon request. Hospital information technology staff members provided screenshots pinpointing where in the ED patient registration software keywords could be entered to be successfully captured in the syndromic feed. These screenshots were then distributed by our hospital outreach unit liaisons back to the hospitals’ ED registration staff members for use as visual aids. We created a syndrome category to flag patients tagged with the “Special Olympics” phrase and provided positive feedback to hospital staff members upon detection.
Implementation of Proactive Patient Tagging
Representatives from 6 medical groups at 13 hospitals responded to the letters and requested additional technical assistance. Screening each medical group for eligibility took 1 to 2 days. The most successful implementers had completed syndromic data-feed upgrades within the past year, eliminating our need to search for information technology representatives with working knowledge of their hospital’s unique data-feed configurations. Two medical groups from 3 hospitals could not make necessary modifications in time. Of these, 1 medical group was ineligible because its ED patient registration software used drop-down selections rather than free-text chief complaint data fields. The other medical group could only populate data fields that were not captured within its syndromic data feeds.
Four medical groups from 10 hospitals achieved total compliance (ie, information technology staff members performed test-patient validation before the start of the Games and provided screenshots identifying where the “Special Olympics” phrase should be entered into the ED patient registration software). Achieving total compliance took each group 4 to 5 days and required collaboration with hospital information technology staff members and infection control practitioners. Of the compliant groups, 1 group asked to use a different keyword abbreviation. Another group requested that an additional data field be accommodated, which required recoding the processing of the hospital’s raw data feed.
Syndrome Category Selection
Multiple syndrome categories were previously in place for routine daily surveillance, such as gastrointestinal, neurologic, rash, respiratory, influenza-like illness, and heat-related illness. All other syndrome categories were created on the basis of anticipated areas of public health concern specific to the Special Olympics (Table). We queried ED visits for health conditions potentially exacerbated by crowded environments, such as syncope and seizures, and addressed the potential for bioterrorism by including categories for ricin and category A bioterrorism agents.11 We also attempted to capture international patients by searching for references to Los Angeles International Airport or recent travel. Last, we searched for mentions of the Special Olympics venues as an additional surrogate measure of attendance. We ran data queries each morning in automated processes during the surveillance period of July 19 to August 6, 2015. Depending on the syndrome category, we analyzed data for case detection, increases in temporal trends, or both. We managed and queried all syndromic surveillance databases with SAS version 9.3.12
Table.
Syndrome categories used to monitor health impacts during the Special Olympics, Los Angeles County, California, July 19 to August 6, 2015
| Public Health Concern or Exposure | Syndrome Categorya | Data Source |
|---|---|---|
| Surge in ED visits at local hospitals | Total volume per hospital, total volume per Special Olympics region | ED visits |
| Hot weather | Heat-related | ED visits |
| Physical or emotional fatigue | Syncope, seizure | ED visits |
| GI disease outbreaks | GI symptoms, such as vomiting and diarrhea | ED visits, coroner-investigated deaths, poison control calls |
| Respiratory illness | Respiratory symptoms, such as cough and sore throat | ED visits, coroner-investigated deaths, poison control calls |
| Vaccine-preventable diseases | Measles, rash | ED visits |
| Dormitory housing | Meningitis, measles, neurological | ED visits, coroner-investigated deaths, poison control calls |
| Bioterrorism | Anthrax, botulism, plague, ricin, smallpox, tularemia, viral hemorrhagic fever | ED visits, coroner-investigated deaths, poison control calls |
| International visitors (with any chief complaint) | Mention of recent international travel, Los Angeles International Airport | ED visits |
| Special Olympics attendees (with any chief complaint) | Mention of Special Olympics, specific Special Olympics venues | ED visits, coroner-investigated deaths, poison control calls |
Abbreviations: ED, emergency department; GI, gastrointestinal.
aSome syndrome categories may address >1 public health concern. Syndrome category duplicates are not listed. For example, the syncope syndrome category may apply for monitoring ED visits potentially related to hot weather and fatigue from crowded environments.
Case Detection
We focused on case detection to identify Special Olympics attendees as well as patients with reportable health conditions from meningitis, measles, ricin, and category A bioterrorism agents. We geared keyword searches toward maximizing detection and, at the cost of increasing false positives, used all available reason-for-visit information, such as patient-stated and patient-coded chief complaints, preliminary and coded diagnoses, and triage notes. The syndromic team received automated email alerts with line lists of flagged patients, which we reviewed for plausibility and syndrome misclassification. Patient medical records were to be obtained by hospital outreach unit liaisons for further verification. Existing LA County Acute Communicable Disease Control Program outbreak investigation protocol was then applied for following up on potential outbreak clusters of patients or patients with a suspected reportable disease detected by the syndromic surveillance system.
Patients flagged for Special Olympics attendance were similarly evaluated. We assessed line lists for commonalities in reported symptoms, EDs visited, arrival dates and times, type of participation in the Special Olympics, if noted, and countries of origin. Any large influxes of Special Olympics attendees or patients with unusual symptoms were to be investigated via the aforementioned signal-investigation protocols.
Temporal Trend Analysis
Syndrome categories that we assessed for trend analysis included gastrointestinal, neurologic, rash, respiratory, influenza-like illness, and heat-related illness. To minimize syndrome misclassification, we limited keyword searches to chief complaints and diagnoses—data fields less likely to contain extraneous information, such as history of medical conditions. We assessed temporal trends for increases over baselines based on Early Aberration Reporting System cumulative sum algorithms.13 We compared daily counts against C1, C2, and C3 algorithm-derived thresholds, which were modified by increasing standard deviation multiples by 1 and with the addition of fixed minimum thresholds. We visualized signals with 120-day trend graphs, as well as summary tables with daily threshold and count information. We also compared heat-related illness trends against daily high temperatures obtained from the Weather Underground website.14
Defining Targeted Special Olympics Surveillance Regions
In addition to analyzing temporal trends across all participating syndromic EDs, we chose 5 geographic surveillance regions corresponding to concentrations of Special Olympics competition venues, athlete dormitories, and polyclinics (Figure 1). By only including hospitals that Specials Olympics attendees would be most likely to visit, we attempted to maximize the capture of Special Olympics attendees while reducing background noise from other ED patients. We retrospectively queried 30 days of ED visits to determine, for each region, 2 to 5 hospitals that cumulatively attracted the top 90% of total ED visits made by LA County residents. Our selections included at least 2 of the 3 closest syndromic hospitals, as well as all syndromic hospitals with trauma wards within a 5-mile radius of the Special Olympics venues in each region. We performed region-specific trend analyses on gastrointestinal, neurologic, rash, respiratory, seizure, syncope, heat-related illness, and measles syndrome categories.
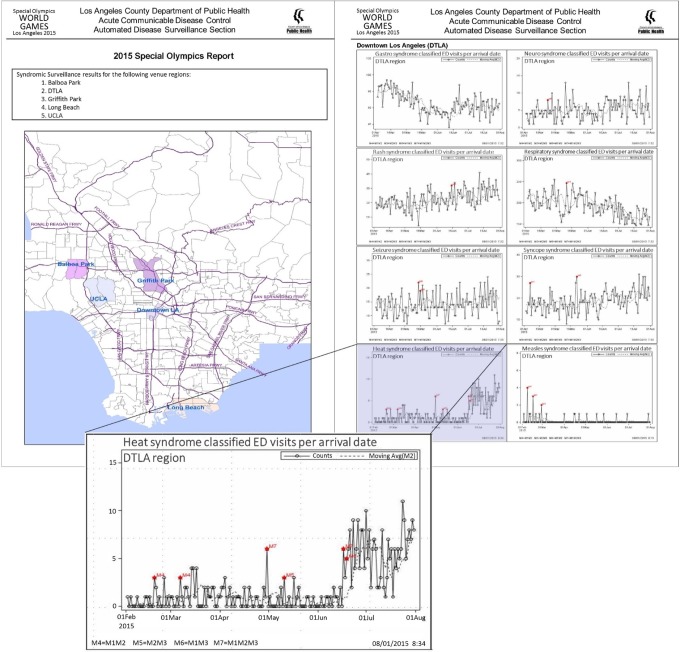
Figure 1.
Excerpts from the 2015 Special Olympics daily report, Los Angeles County, California, July 19 to August 6, 2015. Excerpts feature a map of the 5 surveillance regions (top left, shaded areas on map), as well as trend graphs for the downtown Los Angeles region (top right), for the following syndrome categories: gastrointestinal, neurologic, rash, respiratory, seizure, syncope, heat, and measles. Heat-trend graph enlarged for detail (bottom). Abbreviations: DTLA, downtown Los Angeles; ED, emergency department; UCLA, University of California, Los Angeles.
Spatial Analysis and Mapping
Because sick or injured Special Olympics attendees may have visited multiple EDs at various time points, we used SaTScan15 version 8.0 to prospectively detect spatial temporal clusters. We configured the software to detect daily clusters occurring within circular boundaries ranging from 0 to 6 km in diameter and with longevity from 1 to 7 days, within the past 30 days. We performed cluster analysis for all ED visits in the gastrointestinal, neurologic, rash, and respiratory syndrome categories. However, because the analysis used location information, only LA County residents were included. We visualized the resulting clusters in thematic maps produced in ArcMap16 version 10.2.2 and automated them using Python17 version 2.7 scripting. We reviewed line lists for relation to the Special Olympics and commonalities in patient demographic characteristics, chief complaints, and diagnoses.
Analysis of Poison Control and Coroner-Investigated Death Data
We assessed data from the California Poison Control System and the LA County coroner for gastrointestinal, neurologic, rash, respiratory, category A and B bioterrorism agents, and ricin-related calls and deaths. We created additional syndrome categories to capture references to Special Olympics attendance as well as the names of Special Olympics athletic venues and sporting events. We analyzed all data with a focus on case detection, temporal trend analysis, or both. We generated automated email alerts for detections in syndrome categories that required immediate follow-up, with additional information available from data providers upon request.
Reporting and Corroborating Results From Multiple Data Streams
For gastrointestinal, neurologic, rash, respiratory, and influenza-like illness syndrome categories, trend graphs and thematic maps were displayed in an internal website where daily analysis results from ED, poison control, and coroner data could be visualized side by side. All surveillance results important to and specially customized for Special Olympics surveillance were consolidated into a custom daily summary report created in Microsoft Word. The report included manually reported short summaries of case-detection results, as well as trend graphs and signal summary tables that automatically updated as the source files were output by SAS (Figure 1). Each day, the syndromic team reviewed signals and trend graphs for corroboration across data streams and surveillance regions.
Results
Case Detection Query Results
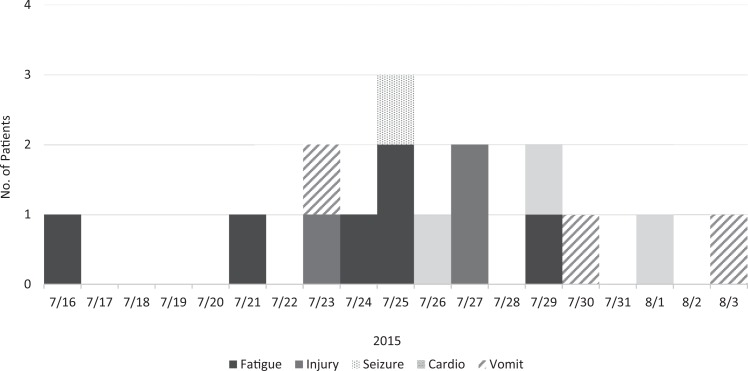
Sixteen proactively tagged Special Olympics attendees were detected—all from 3 total compliance hospitals—with arrival dates between July 16 and August 3, 2015 (Figure 2). Line lists indicated that 1 patient was a Special Olympics athlete, 2 were employees, 1 was a spectator, and 12 were unknown. Five patients reported symptoms of fatigue (eg, dizziness, giddiness, syncope), 4 had physical injuries, 3 had chest pain or a cardiovascular event, 3 reported gastrointestinal symptoms, and 1 had a seizure. Eight patients were from Southern California, 3 were from out of state, 1 was from another country, and 4 were of unknown origin.
Figure 2.
Distribution of reported symptoms (fatigue, injury, seizure, cardiovascular events, and vomiting) for 16 patients whose emergency department records were tagged for Special Olympics attendance, Los Angeles County, California, July 16 to August 3, 2015.
Thirty-seven ED patients referenced meningitis; none were related to the Special Olympics. No patients were flagged in any other case detection-focused queries, such as measles, ricin, category A bioterrorism agents, recent international travel, or mention of Special Olympics venues. No coroner-investigated deaths or poison control calls indicating Special Olympics attendance or bioterrorism agents were detected during the surveillance period.
Temporal Trend Signals
Eleven signals occurred, indicating increases in temporal trends: 1 gastrointestinal signal was detected across all ED visits, 1 gastrointestinal signal was localized to a single hospital, and 9 other syndrome-specific signals were detected across 3 Special Olympics surveillance regions. None of the signals were sustained for >1 day, and peaks were similar in magnitude to other peaks occurring within the past 120 days. Maximum daily temperatures averaged 85°F across the 5 Special Olympics surveillance regions during the surveillance period; the warmest region averaged 91°F. Two of 5 surveillance regions had moderate seasonal increases in heat-related ED visits; however, no increases above seasonal baselines were detected during the Special Olympics. No other increases in total daily ED volume per hospital or per surveillance region were detected. Neither the poison control nor coroner data generated any temporal trend signals during the surveillance period.
Spatial Temporal Clustering
One gastrointestinal, 1 neurologic, and 3 rash clusters were detected during the surveillance period. Only the gastrointestinal cluster was substantial for >1 day but did not persist for >2 days. A line-list review of patient visits contributing to the cluster showed no apparent relation to the Special Olympics or commonalities in reasons for visits, diagnoses, or demographic characteristics. All other clusters appeared to be similarly unrelated and occurred in different areas of LA County. None of the clusters coincided with signals occurring in any other ED, coroner, or poison control database analysis.
Discussion
Challenges of Mass-Gathering Surveillance
The benefits of LA County’s near–real-time syndromic surveillance system are clear: data are timely, and syndrome categories can be quickly improvised, complete with baseline information. However, some characteristics of mass gatherings create a poor fit for traditional syndromic surveillance. For instance, syndromic surveillance performs best when health conditions monitored (1) feature unique symptoms, (2) are acute, and (3) draw in a large number of ED visitors during a short period. Although these conditions may be met, for instance, during extreme climates, stampedes, or acts of terrorism, such scenarios are unlikely during the typical course of mass-gathering events. The 2015 Special Olympics in particular may have been less amenable to syndromic surveillance monitoring because athletes received Special Olympics–organized primary medical care; only the acutely ill would have visited local EDs. Temperatures were also high in some regions but not excessively so.
Attendees of multievent, multilocation mass gatherings may have a range of health conditions and exposures. Because only a small subset of an individual’s chief complaints may appear in syndromic data, ED influxes by multiple patients who have attended the same event may be diluted across several syndrome categories and over time. If health conditions with specific or immediately manifested acute symptoms are excluded, it is likely that only large-scale morbidities among mass-gathering attendees would generate discernable peaks in daily counts. Event names and locations are also not typically recorded in reason-for-visit data fields, which is perhaps the greatest hindrance in using syndromic surveillance to associate patients with mass-gathering exposures.
Added Value of Proactive Patient Tagging
Traditional syndromic surveillance results provided reassurance that a large or severe public health crisis corresponding to the 2015 Special Olympics did not occur. However, proactive patient tagging yielded a sample of ED patients from 3 hospitals that would not otherwise have been associated with the Special Olympics. These patients reported a variety of symptoms and were spread out over time; the greatest total number observed in 1 day was only 3 patients. Without proactive patient tagging, any increases involving such small numbers would have been indistinguishable from the day-to-day variability in background (non–Special Olympics) ED visits, even with queries narrowed down to a single syndrome category for a single hospital.
Practice Implications
We have discussed the merits of proactive patient tagging in the context of mass-gathering surveillance, for which traditional syndromic surveillance methods may not be ideal. However, proactive patient tagging can theoretically supplement the surveillance efforts for any emerging public health situation. Hospital registrars may poll ED patients for elements of epidemiologic case definitions, such as exposures or travel histories that are otherwise missing from traditionally recorded syndromic surveillance data. As a manual effort, however, the effectiveness of proactive patient tagging is dependent on hospital registrar staff members to accurately screen ED patients and record keywords in the correct data fields. The latter may be improved by providing software screenshots to registrar staff members. However, without a validation study, we cannot quantitatively assess how many patients may be missed or inappropriately tagged; analyses based on tagged-patient counts must then assume an unknown misclassification error rate. Criteria for tagging patients should therefore be as clear and as objective as possible to minimize misclassification and bias; the ability to create suitable criteria should be a central consideration for deciding whether to implement proactive patient tagging at all.
Given time constraints, hospitals may be recruited and tested for total compliance before an event, as long as ED patient registration software and data-feed configurations remain unchanged. Screening hospitals ahead of time may permit more time-consuming customizations, such as those requiring SAS code or hospital database adjustments. We would also recommend strategizing the recruitment of selected hospitals. For mass-gathering events, we would target hospitals serving the regions where venues are concentrated. For health conditions with delayed onsets, however, it may be necessary to broaden hospital selection, because patients may disperse and seek emergency care far from exposure sites.
To improve hospital recruitment, outreach letters should focus primarily on soliciting participation, specifying start and end dates for tagging efforts, and outlining the overall process. We found that specific implementation strategies can vary substantially among hospitals, and individualized instructions should be developed during test-patient validation. We were fortunate to be assisted by hospital outreach unit liaisons of LA County’s Acute Communicable Disease Control Program, who maintain strong relationships with hospital infection preventionists. Having preexisting partnerships with hospital information technology teams also reduced the time for initial screening, as well as testing and validation to achieve total compliance.
The syndromic surveillance system can be customized quickly and flexibly to produce many indicators for medical encounters during mass-gathering events where alternative methods of surveillance may otherwise be unavailable, time-consuming, or too expensive to implement. We detected no substantial increases coincident to the Special Olympics across multiple data streams that we monitored, providing quantitative, near–real-time reassurance that a large increase in acute illness did not occur. In addition to using classic methods, we attempted a novel enhancement to syndromic surveillance, implementing proactive patient tagging in a subset of hospitals. Although hospital recruitment for proactive patient tagging was time-consuming, we demonstrated its potential added value for traditionally challenging applications of syndromic surveillance such as mass gatherings. Using syndromic surveillance as a complementary surveillance tool, possibly enhanced with proactive patient tagging, can improve patient detection, expedite outbreak investigations, and reduce the impact of communicable diseases and other health conditions of public health interest.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Special Olympics. First Lady Michelle Obama to attend Opening Ceremony of the 2015 Special Olympics World Games [news release]. http://www.specialolympics.org/Press/2015/First_Lady_Michelle_Obama_to_Attend_Opening_Ceremony_of_the_2015_Special_Olympics_World_Games.aspx. Accessed May 23, 2016.
- 2. Knoll C. Young athletes get star treatment as final preparations for Special Olympics get underway. Los Angeles Times. http://www.latimes.com/sports/olympics/la-me-ln-special-olympics-20150724-story.html. Published 2015. Accessed May 24, 2016.
- 3. Sportzpeak, Inc. RaceSafe Version 1.6.9. San Francisco, CA: Sportzpeak, Inc; 2015. [Google Scholar]
- 4. Steffen R, Bouchama A, Johansson A, et al. Non-communicable health risks during mass gatherings. Lancet Infect Dis. 2012;12(2):142–149. [DOI] [PubMed] [Google Scholar]
- 5. Gautret P, Steffen R. Communicable diseases as health risks at mass gatherings other than Hajj: what is the evidence? Int J Infect Dis. 2016;47:46–52. [DOI] [PubMed] [Google Scholar]
- 6. McCloskey B, Endericks T, Catchpole M, et al. London 2012 Olympic and Paralympic Games: public health surveillance and epidemiology. Lancet. 2014;383(9934):2083–2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bruce MG, Rosenstein NE, Capparella JM, Shutt KA, Perkins BA, Collins M. Risk factors for meningococcal disease in college students. JAMA. 2001;286(6):688–693. [DOI] [PubMed] [Google Scholar]
- 8. Gesteland PH, Gardner RM, Tsui FC, et al. Automated syndromic surveillance for the 2002 Winter Olympics. J Am Med Inform Assoc. 2003;10(6):547–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Smith GE, Elliot AJ, Ibbotson S, et al. Novel public health risk assessment process developed to support syndromic surveillance for the 2012 Olympic and Paralympic Games [published online July 22, 2016]. J Public Health (Oxf). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McHugh L, Tsai S, Bradford L, Walsh A, Lifshitz E. Syndromic surveillance using emergency department chief complaints during and post–Hurricane Irene in New Jersey. Poster presented at: 2012 Council of State and Territorial Epidemiologists Annual Conference; June 3-7, 2012; Omaha, NE. [Google Scholar]
- 11. National Institute of Allergy and Infectious Diseases. NIAID emerging infectious diseases/pathogens. https://www.niaid.nih.gov/research/emerging-infectious-diseases-pathogens. Updated 2016. Accessed January 9, 2017.
- 12. SAS Institute, Inc. SAS Version 9.3. Cary, NC: SAS Institute, Inc; 2012. [Google Scholar]
- 13. Hutwagner LC, Thompson WW, Seeman GM, Treadwell T. A simulation model for assessing aberration detection methods used in public health surveillance for systems with limited baselines. Stat Med. 2005;24(4):543–550. [DOI] [PubMed] [Google Scholar]
- 14. Weather Underground. Los Angeles, CA. https://www.wunderground.com/us/ca/los-angeles. Accessed June 16, 2016.
- 15. Kulldorff M. SaTScan Version 8.0. Rockville, MD: Information Management Services, Inc; 2009. [Google Scholar]
- 16. ESRI, Inc. ArcGIS Release 10.2.2. Redlands, CA: Environmental Systems Research Institute; 2014. [Google Scholar]
- 17. Python Software Foundation. Python Language Reference Version 2.7. Wilmington, DE: Python Software Foundation; 2010. [Google Scholar]