Abstract
Introduction:
The use of syndromic surveillance has expanded from its initial purpose of bioterrorism detection. We present 6 use cases from New York City that demonstrate the value of syndromic surveillance for public health response and decision making across a broad range of health outcomes: synthetic cannabinoid drug use, heat-related illness, suspected meningococcal disease, medical needs after severe weather, asthma exacerbation after a building collapse, and Ebola-like illness in travelers returning from West Africa.
Materials and Methods:
The New York City syndromic surveillance system receives data on patient visits from all emergency departments (EDs) in the city. The data are used to assign syndrome categories based on the chief complaint and discharge diagnosis, and analytic methods are used to monitor geographic and temporal trends and detect clusters.
Results:
For all 6 use cases, syndromic surveillance using ED data provided actionable information. Syndromic surveillance helped detect a rise in synthetic cannabinoid-related ED visits, prompting a public health investigation and action. Surveillance of heat-related illness indicated increasing health effects of severe weather and led to more urgent public health messaging. Surveillance of meningitis-related ED visits helped identify unreported cases of culture-negative meningococcal disease. Syndromic surveillance also proved useful for assessing a surge of methadone-related ED visits after Superstorm Sandy, provided reassurance of no localized increases in asthma after a building collapse, and augmented traditional disease reporting during the West African Ebola outbreak.
Practice Implications:
Sharing syndromic surveillance use cases can foster new ideas and build capacity for public health preparedness and response.
Keywords: syndromic surveillance, emergency department, use cases
Syndromic surveillance, defined as the use of routinely collected electronic health data for public health surveillance and response, began in earnest in New York City the day after the 9/11 attacks on the World Trade Center towers.1 Although early detection of a bioterrorist attack was the initial intent of emergency department (ED) syndromic surveillance, it soon became apparent that tracking ED visits was most useful for monitoring seasonal disease trends, specifically influenza.2,3 During the past decade, several other advantageous uses of ED syndromic surveillance have emerged—namely, surveillance of noninfectious disease syndromes and situational awareness. As a result, several groups within the New York City Department of Health and Mental Hygiene (DOHMH) now routinely use syndromic surveillance data.
This article provides a brief sketch of 6 use cases for syndromic surveillance using ED data that span a broad range of programs and needs, including (1) synthetic cannabinoid drug use, (2) heat-related illness, (3) unreported cases of suspected meningococcal disease or unnecessary prophylaxis, (4) medical needs immediately after severe weather, (5) asthma exacerbation after a building collapse, and (6) Ebola-like illness in travelers returning from West Africa. Collectively, these 6 use cases illustrate the ways in which we have used ED data and the value of these data for detecting and responding to events of public health concern.
Materials and Methods
The New York City DOHMH syndromic surveillance system receives data on patient visits from all 53 hospital EDs in the city. Data are transmitted electronically daily in either flat files via file transfer protocol or through Health Level 7 messaging. Variables include date and time of patient visit, medical record number, reason for visit or chief complaint, mode of patient arrival, discharge diagnosis (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] and International Classification of Diseases, Tenth Revision, Clinical Modification [ICD-10-CM] codes), and patient demographic characteristics, including age, sex, and ZIP code. Patient records are assigned to syndrome categories using an in-house–designed text-processing algorithm that scans the chief complaint and discharge diagnosis variables.
Syndrome definitions vary depending on surveillance objectives and disease. Keywords may be highly specific (eg, meningitis or Ebola) or more general (eg, cough). Some syndromes have specific ICD-9-CM or ICD-10-CM codes (eg, ICD-10 T67.0 for heat stroke), whereas no codes are available for other syndromes (eg, synthetic cannabinoid use or tattoo complications4). The syndrome sensitivity and specificity can be adjusted by including or excluding keywords or phrases and ICD diagnosis codes. For example, if the goal is to identify every potential case of a rare syndrome (eg, Ebola), the keyword search can be broadened to include more terms (eg, countries with Ebola outbreaks), misspellings, and abbreviations, and a search can be made for the corresponding ICD diagnosis codes in the discharge diagnosis field. If the intent is to capture citywide population-level trends (eg, heat-related illness), less emphasis is placed on capturing every possible case. For example, only the most commonly used terms and codes (eg, heat, hot, T67) with necessary exclusions (eg, heater, hot food) would be considered.
The analytical methods we apply also vary by surveillance objective. For surveillance of heat-related illness, we use 2 Poisson generalized linear regression models to estimate expected heat-related illness—one adjusting for temporal trends and the other adjusting for temporal trends and weather. We then compare expected heat-related ED visit counts with observed counts for the previous day, in the context of the time of year and weather conditions. For daily surveillance of synthetic cannabinoids, we use a Poisson-based risk ratio to compare and test the previous day’s count with an expected count based on a 1-year baseline period, with P < .05 considered significant. This method alerts us to a significant increase on a single day. We also compare monthly aggregate counts to describe trends in synthetic cannabinoid-related ED visits. For postdisaster surveillance (eg, after severe weather or a building collapse), we use visual graphics to compare trends in the affected areas for the periods before, during, and after the event. Syndromes with counts that are too low for temporal or spatial analyses (eg, Ebola or meningitis) are presented in a line-list format for review by an analyst with syndromic surveillance expertise and a medical epidemiologist.
The 6 syndromes presented in this article all require previous knowledge or awareness of the disease or condition to design a definition to capture data on syndrome-related visits. For example, after Superstorm Sandy made landfall near New York City in October 2012, we recognized the need for a different approach to identifying health outcomes and community needs based on ED visits. We implemented a word analysis in 2013 to identify aberrations in the mentions of words in ED chief complaint data by comparing daily frequencies of unique words in the chief complaint with their average daily frequencies from the previous year. Words with a current frequency at least 4 times that of the previous year are listed in a report that is examined by a syndromic surveillance analyst to determine if further investigation is needed. This analysis can be adapted to run following special circumstances (eg, building collapse) or emergencies. The 6 use cases presented here were considered exempt from institutional review board review because the data were collected as part of routine public health surveillance, could not be linked to individuals, and were analyzed anonymously.
Results
We summarize the results of 6 use cases (Table).
Table.
Summary of 6 use cases of emergency department (ED) syndromic surveillance data and how they guided governmental response and decision making, New York City Department of Health and Mental Hygiene, 2012-2016
| Case | Syndrome Definition | Purpose | Analysis Method | Results | Outcome |
|---|---|---|---|---|---|
| Synthetic cannabinoid drug use | Mentions of synthetic marijuana, K2, K-2, K-TWO, K TWO, or other street names of synthetic cannabinoid drugs | To monitor citywide ED visit trends related to synthetic cannabinoid drug use as seen in other parts of the country | Compare daily counts with a 1-year baseline to detect unusual increases for a single day; compare monthly aggregates to understand trends | A 220% increase in the number of monthly synthetic cannabinoid-related ED visits from December 2013 (n = 14) to June 2014 (n = 45) | Prompted the immediate release of a health advisory and initiation of a public health investigation. Neighborhoods with higher synthetic cannabinoid-related ED visits were prioritized for removal of synthetic cannabinoid products |
| Heat-related illness | Mentions of words such as heat, hot, heat stroke, and T67 and excluding words such as heater or hot food | To monitor and report on heat-related illness during heat waves and to provide timely information to the city’s heat emergency steering committee | Generalized linear regression models controlling for temporal and meteorological variables and comparing increases with previous years | Enhanced situational awareness during extreme heat events by supplementing weather observations and forecasts with a timely indicator of public health impact | Prompted additional public health messaging |
| Unreported suspected meningococcal disease or unnecessary prophylaxis | Mentions of meningitis; visits with mentions of exposure, prophylaxis, or contact | To identify potentially unreported cases of meningococcal disease and misuse of prophylaxis | Create and disseminate line list daily | Identified 451 ED visits with mention of meningitis from May 1, 2015, through April 30, 2016. No unreported cases of meningococcal disease were found during the period. Followed up on 17 instances where chief complaint indicated an exposure to or prophylaxis for meningitis but no suspected cases had been reported | Hospital staff members were educated about the appropriate use of antibiotic prophylaxis |
| Medical needs after severe weather | Mentions of medication, methadone, dialysis, or oxygen need | To provide situational awareness in the worst affected areas immediately after Superstorm Sandy | Recognize community needs and monitor their trends for several weeks after the storm | ED visits for medical needs increased acutely after Superstorm Sandy and remained slightly elevated for the next 30 days | Identified new medical needs in specific locations and provided timely information to public health officials |
| Asthma after building collapse | Mentions of asthma, wheezing, or chronic obstructive pulmonary disease | To investigate potential increases in asthma after a building collapse and fire in a Manhattan neighborhood | Compare trends in affected vs nonaffected areas | No increase was found | Quickly addressed potential health impacts and provided reassurance to officials |
| Ebola virus disease | Mentions of Ebola, Guinea, Liberia, Mali, or Sierra Leone | To monitor for potentially unreported cases of Ebola | Create and disseminate line list when cases identified | 37 mentions of Ebola and 12 mentions of Ebola-affected countries | Prompted follow-up with ED for 3 questionable cases; none of the cases met the testing criteria |
Synthetic Cannabinoid Drug Use
Prompted by increasing morbidity observed in Wyoming and several other jurisdictions in 2012,5 we began daily surveillance of synthetic cannabinoid-related ED visits in late 2012. Syndrome keywords included common packaging names of synthetic cannabinoids (eg, K2 and spice). Through the word analysis, we identified a new keyword used by hospitals—K-TWO—that allowed us to further enhance the syndrome definition. We observed a 220% increase in monthly synthetic cannabinoid-related ED visits from December 2013 (n = 14) to June 2014 (n = 45) (Figure 1). The frequency of synthetic cannabinoid-related ED visits increased, with ≥1 visit every 2 to 3 days in 2014, compared with every 4 to 5 days in 2013. Men accounted for 159 of 191 (83%) synthetic cannabinoid-related ED visits. The median patient age was 37,6 and 99% of patients were aged ≥18.
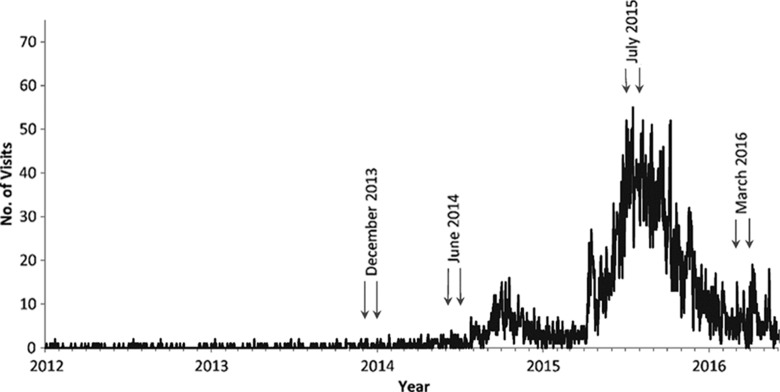
Figure 1.
Synthetic cannabinoid-related emergency department (ED) visit trends, New York City, January 2012 through May 2016. The periods highlighted with arrows indicate the initial detection of increases in cannabinoid-related ED visits (December 2013 to June 2014) and subsequent decreases in cannabinoid-related ED visits (July 2015–March 2016) after an intervention that included removal of synthetic cannabinoid products through a multiagency response.
The initial increase (December 2013 through June 2014) in synthetic cannabinoid-related ED visits prompted the immediate release of a health advisory7 and initiation of a public health investigation, including medical chart reviews that confirmed the patient’s reason for the visit. As synthetic cannabinoid-related ED visits continued to rise in 2015, neighborhoods with higher numbers of these visits were prioritized for removal of synthetic cannabinoid products through a multiagency response. After these efforts, ED syndromic surveillance detected an 85% reduction in synthetic cannabinoid-related ED visits from July 2015 through March 2016 (Figure 1).8
Heat-Related Illness
Heat-related illnesses are particularly dangerous for the very young and very old. New York City activates a heat emergency plan when the heat index is ≥95°F for ≥2 consecutive days or the predicted heat index is ≥100°F for ≥1 day. An interagency Heat Emergency Steering Committee conference call is held daily during declared heat emergencies to provide situational awareness, gather agency-specific data, and discuss other response options. Participating agencies include emergency services, public health, city utilities, and several others. Analysis of heat-related ED visits is conducted daily from May through September; the findings are summarized on the interagency call during a heat emergency.
Heat-related ED visits are expected during extreme heat events, but when increases are greater than expected and ongoing extreme heat is forecasted, syndromic surveillance provides information that supports additional or earlier public health actions.9 ED syndromic surveillance data could be especially useful during a heat wave complicated by another hazard, such as a widespread power outage.
Unreported Suspected Meningococcal Disease or Unnecessary Prophylaxis
On July 23, 2013, soon after implementing word analysis, we discovered a large single-day increase in the mention of the words meningitis (n = 33) and expose (n = 31) compared with a 365-day average of ≤1 mention daily. The line list identified 31 patients with chief complaints of “expose(d) to meningitis” presenting at 2 hospitals, with 30 of those patients presenting at the same ED within 1 hour of each other (Figure 2); however, no suspected case of meningococcal disease had been reported to the DOHMH. This occurrence highlighted the potential uses of syndromic data to identify reportable diseases such as meningitis.
Figure 2.
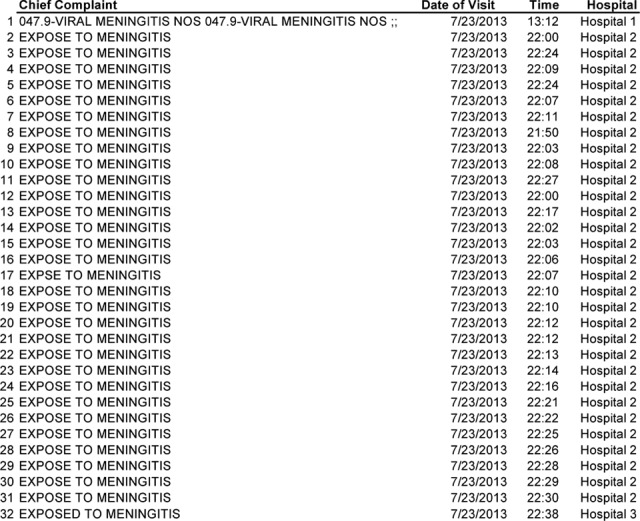
Partial emergency department (ED) line list of a cluster of patients exposed to meningitis on a single day, identified using the word analysis of the ED chief complaints, New York City, July 23, 2013. Abbreviations: HOSP, hospital; NOS, not otherwise specified.
Immediate reporting of suspected cases of meningococcal disease to the DOHMH by health care entities is required under the New York City Health Code. Culture-negative meningococcal disease is a common phenomenon. Therefore, when suspected cases are reported to the DOHMH, polymerase chain reaction testing is conducted. This test is not usually available in hospital laboratories. Antibiotic prophylaxis is indicated for close contacts of people with confirmed or suspected meningococcal disease to prevent secondary transmission.
Daily ED surveillance for meningitis was initiated in May 2015. A line list of all ED visits with a mention of MENING in their chief complaint is created daily, and those with mentions of exposure, contact, or prophylaxis are flagged. An investigator follows up on these visits with the hospital to determine if (1) the patient with known or suspected meningitis has been reported to the DOHMH or (2) the patient with a culture-negative laboratory test is still being considered as a suspected meningococcal disease case.
To quantify the burden of this surveillance effort, we conducted a retrospective study from May 1, 2015, through April 30, 2016. During this time period, we identified 451 ED visits with a mention of meningitis, of which 62 patients had a mention of exposure, contact, or prophylaxis. In 17 instances, further investigations were conducted and no cases of meningococcal disease that were not previously reported were found. However, instances of antibiotic prophylaxis overuse were identified, and hospital staff members were educated on appropriate use of meningococcal prophylaxis.
In June 2016, two patients identified through the daily line list were found, and further investigation connected them to a suspected meningococcal case that had not been reported. Hospital culture results were negative for the suspected case, and the DOHMH arranged for polymerase chain reaction testing, which confirmed meningococcal infection.
Medical Needs Immediately After Severe Weather
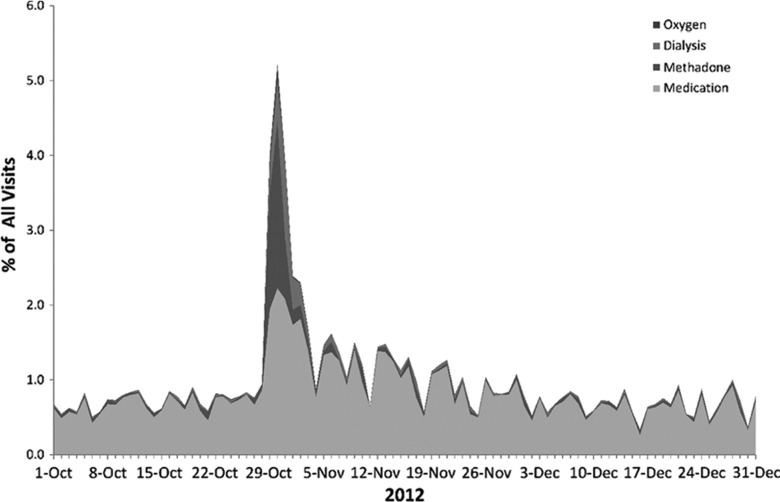
In October 2012, Superstorm Sandy, a category 2 hurricane, caused extensive damage in New York City, primarily from heavy winds and flooding. The storm underscored the need for timely situational awareness of storm-related health events, including drownings, electrocutions, mental health–related issues, and other injuries. We monitored the expected health events using our syndromic surveillance system and stratified the syndromes by impacted vs nonimpacted areas to compare trends. We also observed a surge in some unexpected health events, such as methadone-related ED visits in a highly affected area immediately after the storm. This observation prompted further investigation into ED visits for medications and other medical needs (eg, oxygen, dialysis). As part of surveillance efforts after Superstorm Sandy, time-series graphs were circulated daily to DOHMH analysts, subject matter experts, and public health officials. ED visits for medications and medical needs increased acutely during and immediately after the storm. After the storm, the daily number of medication-related visits (mean = 111, standard deviation [SD] = 39.7) and medical needs visits (mean = 7, SD = 10.1) remained elevated through November 2012 (Figure 3). During the 2-month period before the storm, the comparable number of medication-related visits (mean = 74, SD = 18.6) and medical needs visits (mean = 2, SD = 1.5) was substantially lower.
Figure 3.
Syndromic surveillance of medical needs trends of patients visiting New York City emergency departments (EDs) after Superstorm Sandy (October 28 and 29, 2012), as reported through ED chief complaint data, October 1 to December 31, 2012.
Superstorm Sandy also presented an opportunity to test the utility of the word analysis. Several months after the storm, we ran a retrospective analysis for all ED visits on the days of the storm (October 28-29, 2012). We noted increases in the words methadone, oxygen, O2, hypothermia, evacuation, dialysis, shelter, housing, refills, inhalation, smoke, prescriptions, carbon, monoxide, and opioids. In the immediate aftermath of Superstorm Sandy, we monitored syndromes that included some of these words (eg, hypothermia, carbon monoxide), but the word analysis will help us identify unexpected reasons for visits and expand syndrome definitions for future monitoring of severe weather events. This word analysis will increase the likelihood of identifying and addressing medical needs in affected communities.
Asthma After a Building Collapse
In March 2015, a gas leak caused an explosion, a 7-alarm fire, and the collapse of 3 mixed-use buildings in Manhattan’s East Village neighborhood. The size of the fire and subsequent release of building debris prompted concerns about potential localized increases in asthma-related ED visits because of higher levels of particulate matter air pollution. We monitored ED visits for asthma symptoms among residents of the East Village and asthma-related visits to hospitals near the explosion and found that the number of asthma-related visits did not increase. Syndromic surveillance helped to monitor the health impact of the event, inform the response, and provide reassurance to government leaders that the health of the community was not at risk.
Ebola During the West African Outbreak
During the 2014-2016 Ebola epidemic in West Africa, New York City hospitals were advised to report suspected cases of Ebola in people who had recently traveled to an affected country who presented for care with compatible symptoms. To augment passive Ebola surveillance and ensure no suspected cases were missed, we implemented a simple chief complaint keyword search for Ebola, Guinea, Liberia, Mali, or Sierra Leone. From January 1, 2014, through December 31, 2015, we identified 37 ED visits in the city’s hospitals with a mention of Ebola and 12 visits with a mention of 1 of the Ebola-affected countries. For identified visits with an ICD-9-CM discharge code unrelated to Ebola, we did not initiate an investigation. If the discharge code was not reported in the data feed from the hospital (which is common because of the lag involved in diagnosis code reporting), or if the Ebola response team had no previous knowledge of the ED visit, we contacted the hospital for additional details. In 3 instances, a person under investigation for Ebola virus disease was identified through syndromic surveillance but not through passive surveillance. None of the 3 patients met Ebola testing criteria.
Discussion
These 6 use cases for syndromic surveillance illustrate how syndromic surveillance has been used in New York City to advance public health goals. The cases show the important role that ED syndromic surveillance can play in providing timely situational awareness, identifying new and emerging trends, aiding in governmental decision making, helping frame public health messaging, and informing the public during a public health crisis. Although the original intent of ED syndromic surveillance data was to detect bioterrorism, these 6 cases demonstrate the broader utility of these data. Among the use cases presented here, the contribution of ED syndromic surveillance data to public health surveillance and investigations varied from being the only available data source (synthetic cannabinoids) to supplementing an established reporting system (Ebola). Few other data sources are comparable for understanding population-level health and health needs in near-real time.
Several previous studies have described the utility of ED syndromic surveillance data for bioterrorism-related early aberration detection,10 for routine surveillance of infectious2,11–13 and noninfectious14–17 diseases, and for surveillance during emergencies.18–21 As these studies found, ED syndromic surveillance data are a valuable resource for understanding a wide range of diseases, conditions, and patient needs. The challenge is to incorporate ED syndromic surveillance into regular protocols and governmental decision-making processes (eg, heat-related illness surveillance during heat waves). It is important to continually refine strategies and statistical methods during emergency situations, such as the building collapse, for application during future public health emergencies. Future investigations would benefit from using methodological approaches such as word analysis to aid in the identification of adverse health effects in populations. Insights gained through syndromic surveillance data can provide guidance on how the government should respond and provide timely information to the public.
Most published studies on syndromic surveillance focus on broad syndrome categories (eg, influenza-like illness or injuries). All of the syndromes described here, with the exception of asthma, used specific terms in the chief complaint (eg, meningitis or Ebola) rather than general terms (eg, fever or flu) and had relatively few cases. The small number of cases each day or intermittently allowed for a focused near–real-time public health response, such as educating hospital staff members on the misuse of meningitis prophylaxis or managing a patient with suspected Ebola virus disease. Although some actionable events might be missed because of gaps in the quality of data on chief complaints, the ability to quickly respond to cases identified by ED syndromic surveillance is beneficial to the prevention and control of public health concerns.
Limitations
Several challenges to ED syndromic surveillance should be noted. First, hospital chief complaint coding practices vary, and as a result, the quality and level of detail in the chief complaint field is not standardized. This variation makes it challenging to develop a uniform syndrome definition that is applicable to all hospitals. Some hospitals provide few words in the chief complaint field; therefore, creating syndromes with multiple symptoms (eg, fever, rash, and arthralgia for Zika virus) is not always useful. In certain situations (eg, Superstorm Sandy, building collapse), knowing which syndromes or keywords should be tracked may not be immediately evident. In such instances, the traditional approach of having a predetermined set of syndromes will have limitations.
To detect changes in patterns of ED use or unusual events, the word analysis provides an alert to sudden and unusual increases in words appearing in the chief complaint field. However, the DOHMH word analysis does not currently group misspellings, abbreviations, and synonyms and is most effective for rare words. We are exploring preprocessing the chief complaint and statistical approaches that detect both sudden and gradual increases to advance this technique beyond rare words. Based on our experience with surveillance of synthetic cannabinoid use, we are expanding the word analysis to alert analysts to new words being entered in the chief complaint field and to check for the increasing frequency of these words.
As demonstrated by the meningitis-related cluster identified via the word analysis, many clusters in ED data do not fall into an existing syndrome category. New approaches to cluster detection that do not require prespecifying syndromes are emerging to uncover such clusters.22,23 Such methods could reveal multiple clusters in a single day of ED visits without first requiring their categorization into a syndrome.24 Incorporating such an approach might enhance the utility of ED syndromic surveillance data; however, the burden of assessing and responding to an increased number of clusters must be weighed before this advancement can be incorporated into routine practice.
Practice Implications
Dozens of practical cases of ED syndromic surveillance data use are being developed and used by local and state health departments nationally and globally. These use cases are infrequently presented at conferences and are rarely published. An online collection of use cases of syndromic surveillance data could provide a searchable catalog of current practice and lessons learned. We developed a prototype website (https://sites.google.com/site/ssusecases) that is simple to use and facilitates new entries. A participatory community repository such as this would allow for timely documentation and sharing of syndrome definitions, statistical methods, alternative uses, and novel visualizations. Sharing use cases and methodologies among syndromic surveillance practitioners can benefit the surveillance community at large and help build capacity for public health preparedness and response.
Acknowledgments
We acknowledge the provision of details for and the review of the synthetic cannabinoid and heat-related illness sections by Michelle Nolan and Katie Lane of the New York City Department of Health and Mental Hygiene (DOHMH). We acknowledge the provision of details for the meningococcal use case by Mike Antwi, Paula Del Rosso, and Marie Dorsinville of the New York City DOHMH.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Heffernan R, Mostashari F, Das D, et al. Syndromic surveillance in public health practice, New York City. Emerg Infect Dis. 2004;10(5):858–864. [DOI] [PubMed] [Google Scholar]
- 2. Olson DR, Heffernan RT, Paladini M, et al. Monitoring the impact of influenza by age: emergency department fever and respiratory complaint surveillance in New York City. PLoS Med. 2007;4(8):e247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Buehler JW, Sonricker A, Paladini M, et al. Syndromic surveillance practice in the United States: findings from a survey of state, territorial, and selected local health departments. Adv Dis Surveill. 2008;6(3):1–20. [Google Scholar]
- 4. Kotzen M, Sell J, Mathes RW, et al. Using syndromic surveillance to investigate tattoo-related skin infections in New York City. PLoS One. 2015;10(6):e0130468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Murphy TD, Van Houten C, Gerona R, et al. Acute kidney injury associated with synthetic cannabinoid use—multiple states, 2012. MMWR Morb Mortal Wkly Rep. 2013;62(6):93–98. [PMC free article] [PubMed] [Google Scholar]
- 6. New York City Department of Health and Mental Hygiene. 2015. advisory #36: increase in synthetic cannabinoid (K2)–related adverse events and emergency department visits, New York City. 2015. https://www1.nyc.gov/assets/doh/downloads/pdf/ah/Synthetic%20cannabinoids-HAN-advisory_Summer%202015%20-penultimate8.pdf. Accessed May 16, 2016.
- 7. New York City Department of Health and Mental Hygiene. 2014. advisory #18: increase in synthetic cannabinoid-related adverse events and emergency department visits, New York City. 2014. https://www1.nyc.gov/assets/doh/downloads/pdf/ah/Synthetic%20cannabinoids-HAN-advisory-7%2027%2014%2011 AM.pdf. Accessed May 16, 2016.
- 8. City of New York, Office of the Mayor. Mayor de Blasio, Speaker Mark Viverito, and Health Commissioner Bassett announce 85 percent reduction in K2 related emergency visits. 2016. http://www1.nyc.gov/office-of-the-mayor/news/421-16/mayor-de-blasio-speaker-mark-viverito-health-commissioner-bassett-85-percent. Accessed May 16, 2016.
- 9. New York City Department of Health and Mental Hygiene. 2016. health alert #42: heat health advisory. 2016. https://a816-health30ssl.nyc.gov/sites/nychan/Lists/AlertUpdateAdvisoryDocuments/Heat%20Health%20Alert_20160908.pdf. Accessed January 13, 2017.
- 10. Buehler JW, Berkelman RL, Hartley DM, et al. Syndromic surveillance and bioterrorism-related epidemics. Emerg Infect Dis. 2003;9(10):1197–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Balter S, Weiss D, Hanson H, et al. Three years of emergency department gastrointestinal syndromic surveillance in New York City: what have we found? MMWR Morb Mortal Wkly Rep. 2005;54:175–180. [PubMed] [Google Scholar]
- 12. Westheimer E, Paladini M, Balter S, et al. Evaluating the New York City emergency department syndromic surveillance for monitoring influenza activity during the 2009-10 influenza season. PLoS Curr. 2012;4:e500563f3ea181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hsieh JL, Nguyen TQ, Matte T, et al. Drinking water turbidity and emergency department visits for gastrointestinal illness in New York City, 2002-2009. PLoS One. 2015;10(4):e0125071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mathes RW, Ito K, Matte T. Assessing syndromic surveillance of cardiovascular outcomes from emergency department chief complaint data in New York City. PLoS One. 2011;6(2):e14677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hughes HE, Morbey R, Hughes TC, et al. Using an emergency department syndromic surveillance system to investigate the impact of extreme cold weather events. Public Health. 2014;128(7):628–635. [DOI] [PubMed] [Google Scholar]
- 16. Seil K, Marcum J, Lall R, et al. Utility of a near real-time emergency department syndromic surveillance system to track injuries in New York City. Inj Epidemiol. 2015;2(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ising A, Proescholdbell S, Harmon KJ, et al. Use of syndromic surveillance data to monitor poisonings and drug overdoses in state and local public health agencies. Inj Prev. 2016;22(suppl 1):i43–i49. [DOI] [PubMed] [Google Scholar]
- 18. Marx MA, Rodriguez CV, Greenko J, et al. Diarrheal illness detected through syndromic surveillance after a massive power outage: New York City, August 2003. Am J Public Health. 2006;96(3):547–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Baer A, Elbert Y, Burkom HS, et al. Usefulness of syndromic data sources for investigating morbidity resulting from a severe weather event. Disaster Med Public Health Prep. 2011;5(1):37–45. [DOI] [PubMed] [Google Scholar]
- 20. Rappold AG, Stone SL, Cascio WE, et al. Peat bog wildfire smoke exposure in rural North Carolina is associated with cardiopulmonary emergency department visits assessed through syndromic surveillance. Environ Health Perspect. 2011;119(10):1415–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tsai S, Hamby T, Chu A, et al. Development and application of syndromic surveillance for severe weather events following Hurricane Sandy. Disaster Med Public Health Prep. 2016;10(3):463–471. [DOI] [PubMed] [Google Scholar]
- 22. Burkom H, Elbert Y, Piatko C, et al. A term-based approach to asyndromic determination of significant case clusters. Online J Public Health Inform. 2015;7(1):e11. [Google Scholar]
- 23. Faigen Z, Deyneka L, Ising A, et al. Cross-disciplinary consultancy to bridge public health technical needs and analytic developers: asyndromic surveillance use case. Online J Public Health Inform. 2015;7(3):e228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. International Society of Disease Surveillance. Technical conventions use cases: asyndromic cluster detection. 2015. http://www.syndromic.org/cop/analytic-solutions/technical-conventions-background/use-cases. Accessed January 13, 2017.