ABSTRACT
Background: Sleep quality in hospitalized medicine patients is poor, with environmental factors among the most frequently cited reasons.
Objective: We tested the efficacy of a non-pharmacologic intervention on the sleep quality of medicine inpatients.
Design/Methods: A controlled study to evaluate our non-pharmacologic multidisciplinary ‘TUCK-in’ protocol (which includes timed lights-off periods, minimizing night-time noise, distribution of earplugs at bedtime, cued toileting before bedtime, and identification and reduction of modifiable interruptions) was deployed on two of five identical medicine wards. Randomization was at the level of the ward.
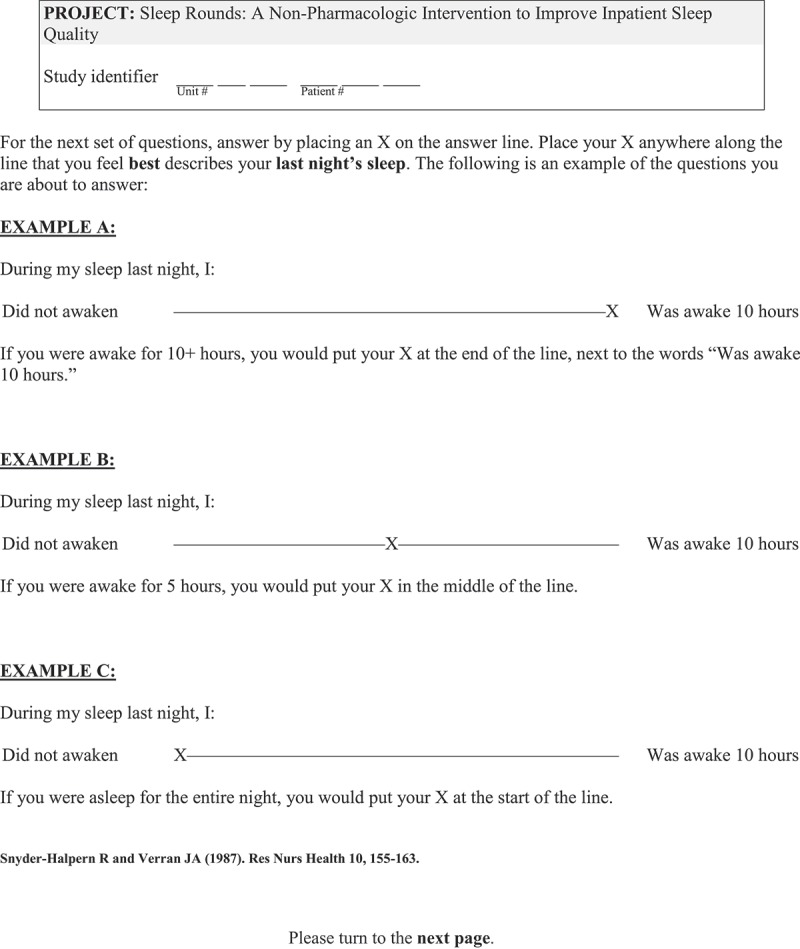
The main outcome measure was self-reported duration of night-time sleep within 48 hours prior to discharge. Additional outcome measures included the Verran–Snyder-Halpern (VSH) Sleep Score and inpatient sleep pharmaceutical use.
Results: Self-reported duration of night-time sleep (median 5.0 vs. 5.0 hours, p = 0.29) and daytime sleep (1.0 versus 0.5 hours, p = 0.43) did not differ between the 40 intervention patients and the 41 control patients (p = 0.13 on multivariate analysis). Cumulative VSH sleep disturbance (median 420 versus 359, p = 0.19), efficacy (median 169 versus 192, p = 0.29), or supplementation (median 97 versus 100, p = 0.51) scales were also not different between study arms.
Conclusions: Although staff reported the protocol to be achievable and worthwhile, there were no significant differences in any of the outcomes between intervention and control patients.
KEYWORDS: Sleep quality, inpatient sleep, non-pharmacologic interventions, sleep hygiene, factors affecting sleep
1. Introduction
Insomnia is associated with negative outcomes, such as depression, anxiety, and poor memory [1]. Poor sleep is common in hospitals [2,3]. Environmental factors most frequently contributing to poor sleep include noise and night-time disruptions, inappropriate lighting, and lack of daytime stimulation leading to loss of a normal sleep–wake cycle. [4]
Sleep hygiene protocols can improve sleep quality [5]. While this is well-studied in outpatient settings, the inpatient literature is predominately in critical care units, where evidence suggests non-pharmacologic protocols decrease delirium and improve subjective sleep quality [6]. Similar studies in non-critical care settings exist but have inconsistent results and include costly and time-consuming interventions, such as white-light lamps or nursing-led relaxation techniques [7]. One previous study introduced a protocol that aimed to reduce interruptions and had outcome measures of quality of sleep and use of as-needed sleep medications. Their sleep quality data was unusable as the majority of patients felt too ill to complete the questionnaires. However, they did show a significant decrease in use of as-needed sleep medication [8].
Our goal was to test the efficacy of a multidisciplinary non-pharmacologic intervention on the sleep quality of hospitalized patients on general medical wards. Our protocol included scheduled lights-off, minimized night-time noise, distribution of earplugs, cued toileting, and identification then elimination of modifiable interruptions. We used the mnemonic ‘TUCK-in’ (Figure 1) to represent our sleep hygiene protocol.
Figure 1.
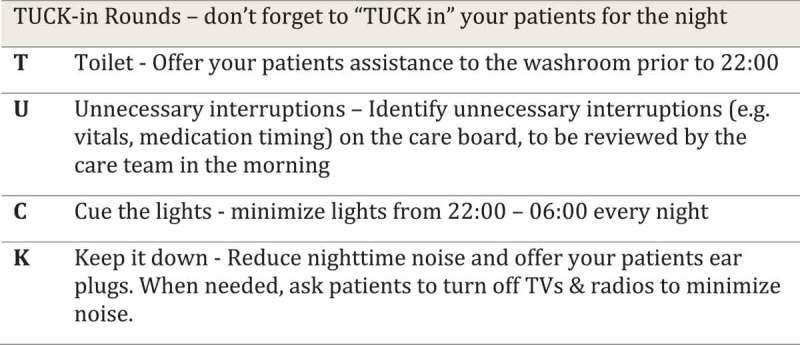
Mnemonic provided to nursing staff for the non-pharmacologic sleep intervention protocol.
2. Methods
2.1. Design
This was a controlled study performed at an 880-bed quaternary centre in Edmonton, Alberta, Canada. Two of the five general internal medicine (GIM) wards were assigned to be intervention wards and the other three control wards. Approval was obtained from the University of Alberta Research Ethics Board (Pro00059588). Written informed consent was obtained from participants prior to participation. Our target sample size, calculated using a one-tailed t-test with α 0.05, β 0.10, and assumed effect size of 1.5 hours based on previously published data [4], was 80 (40 per group).
2.2. Patients
To participate, patients had to be admitted to one of the five GIM wards during the three week data collection period, be 18 years or older, able to communicate in English, and willing/able to consent and complete the outcome questionnaires. Patients were excluded if they had a life expectancy of less than three months, significant cognitive impairment (score of less than 5 on the Short Portable Mental Status Questionnaire) [9], or were previously enrolled in the study. Discharge location and history of pre-existing sleep disorders were not exclusion criteria.
2.3. Intervention
Two of the five wards implemented our ‘TUCK-in’ protocol, and three units continued standard-of-care. All five units have a similar layout, comprised of private and semiprivate (2–4 person) rooms. Our intervention included a night-time lights-off and minimal-sound policy (from 10.00pm to 6.00am), bedtime cuing prior to 10.00pm with suggested timed toileting, and offering disposable earplugs. Night-shift staff were encouraged to identify interruptions felt to be potentially unnecessary on a daily communications board, to be reconsidered and potentially discontinued by the care team each morning. Educational sessions were held with physicians and nursing staff, and the protocol was implemented one week prior to data collection. Informational posters were also placed in staff areas. The wards to which patients were admitted were allocated by first availability, and patient populations were expected to be similar between intervention and standard units. Patients were not explicitly told if they were on an intervention or control unit.
2.4. Data collection
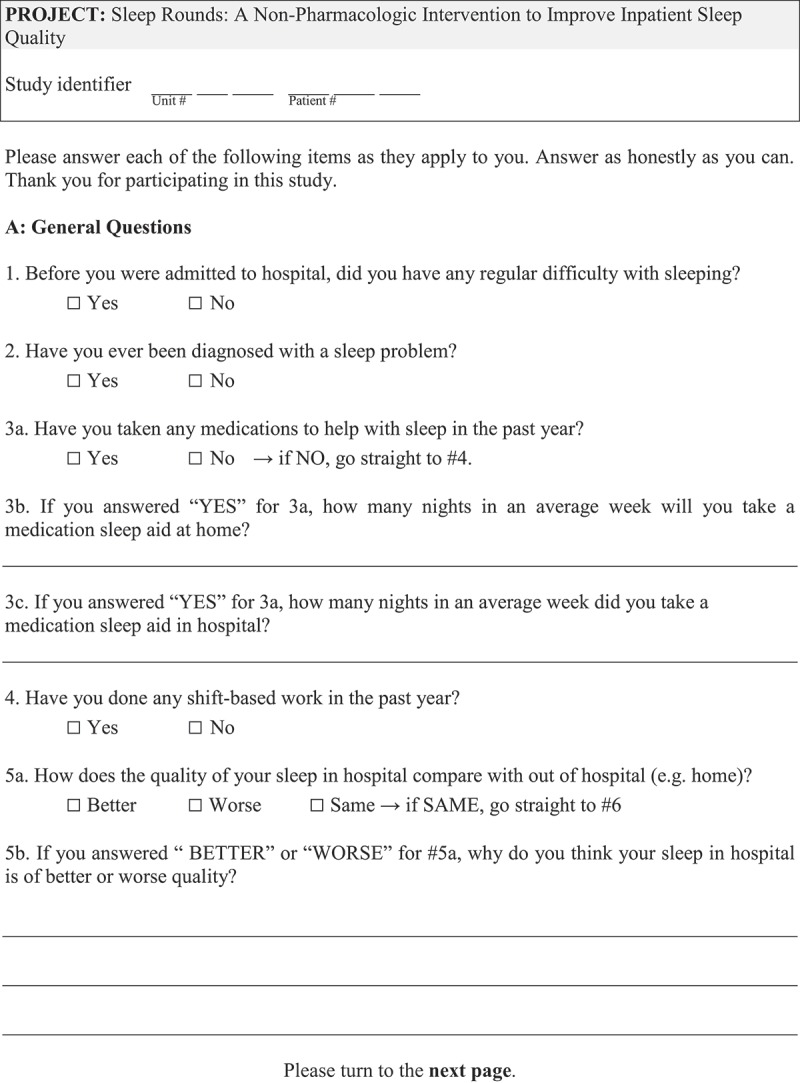
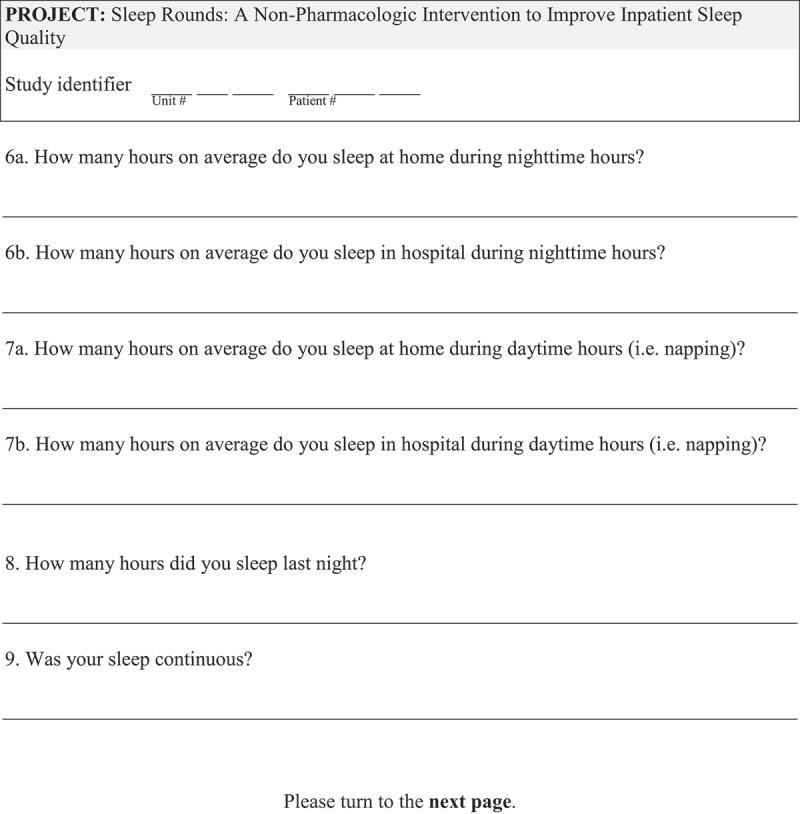
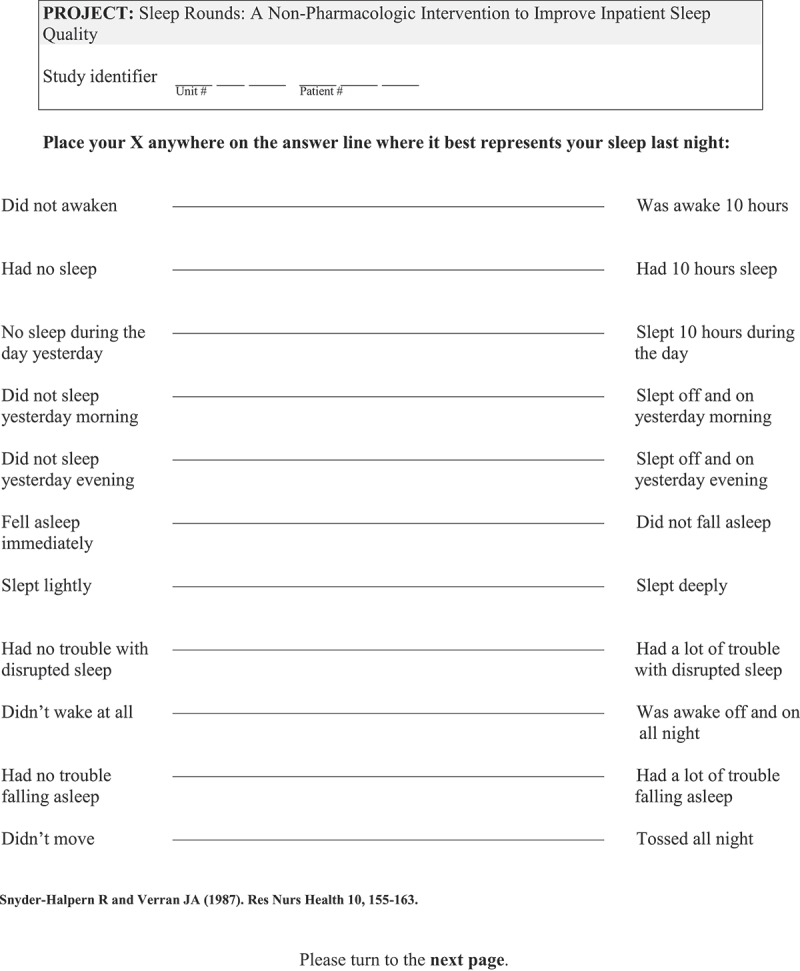
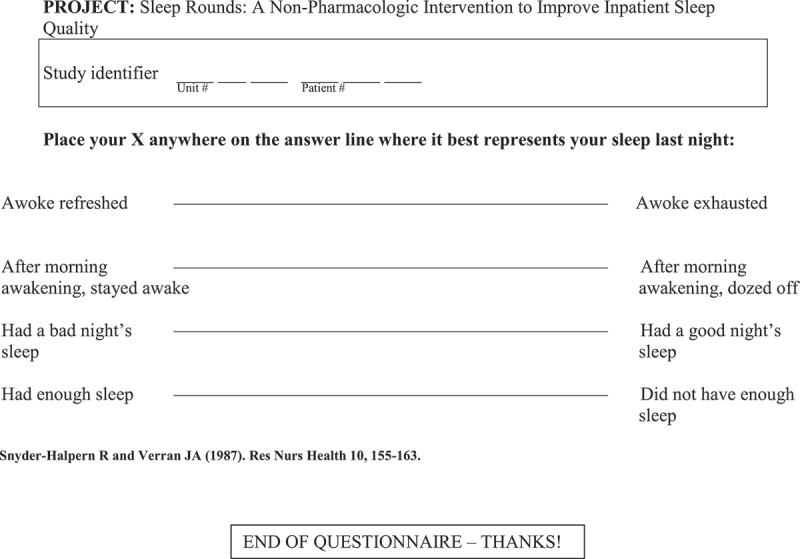
Patients were approached within 48 hours of expected discharge. Eligible participants completed an English-language questionnaire (Appendix A) on perceived sleep quality and factors affecting sleep quality. Participants also completed the Verran and Snyder-Halpern (VSH) sleep scale, a validated, 15-item visual analogue scale to measure the previous night’s sleep quality [10]. Each item on the scale is scored from 0–100 mm. There are three subscales to reflect sleep disturbance, effectiveness and supplementation. A high score indicates worse sleep for the sleep disturbance and supplementation subscales and better sleep for the sleep effectiveness subscale. A chart review was performed for concurrent illnesses, primary reason for hospitalization, and sleep pharmaceutical use at home and in hospital.
2.5. Statistics
All data were analysed using SAS version 9.4 (Cary, NC) and statistical significance was defined as p < 0.05. Multivariate models included age, sex, variables under p-value ≤0.10 threshold difference between populations, and variables previously identified as significant [4].
3. Results
We screened 128 patients for study eligibility. Of these, 10 failed cognitive screening, 12 were unable to communicate in English, 17 declined participation, 3 were excluded for limited life expectancy, and 5 did not fully complete the questionnaires. Patient characteristics were similar between intervention and control units, although participants from the intervention wards were less likely to have performed shift work in the past year but were more likely to have a self-reported diagnosis of a sleep disorder or pulmonary disease (Table 1) – all of these factors were considered in the multivariate analysis.
Table 1.
Patient characteristics.
| Characteristic | Control N = 41 | Intervention N = 40 | Total N = 81 | p-value |
|---|---|---|---|---|
| Age, years | 58.6 (19.5) | 61.4 (20.6) | 60.0 (20.0) | 0.537 |
| Female | 14 (34.1) | 17 (42.5) | 31 (38.3) | 0.439 |
| Total number of comorbidities | 2.7 (1.6) | 3.1 (1.3) | 2.9 (1.4) | 0.285 |
| Comorbidities | ||||
| Alcohol or recreational drug use | 11 (26.8) | 11 (27.5) | 22 (27.2) | 0.946 |
| Depression | 8 (19.5) | 8 (20.0) | 16 (19.8) | 0.956 |
| Insomnia or chronic outpatient sleep aid use | 1 (2.4) | 2 (5.0) | 3 (3.7) | 0.542 |
| Rheumatologic | 3 (7.3) | 5 (12.5) | 8 (9.9) | 0.434 |
| Pulmonary | 7 (17.1) | 15 (37.5) | 22 (27.2) | 0.039 |
| GI | 12 (29.3) | 12 (30.0) | 24 (29.6) | 0.943 |
| Endocrine | 16 (39.0) | 22 (55.0) | 38 (46.9) | 0.150 |
| Cardiovascular | 22 (53.7) | 20 (50.0) | 42 (51.9) | 0.742 |
| Cancer | 12 (29.3) | 6 (15.0) | 18 (22.2) | 0.123 |
| Shift work in past year | 15 (36.6) | 5 (12.5) | 20 (24.7) | 0.012 |
| Self-reported previous diagnosis of sleep disorder | 7 (17.1) | 14 (35.0) | 21 (25.9) | 0.066 |
| Sleep pharmaceutic use at home in past year | 19 (46.3) | 19 (47.5) | 38 (46.9) | 0.917 |
| Any sleep pharmaceutic use in hospital | 12 (29.3) | 12 (30.0) | 24 (29.6) | 0.943 |
| Single patient room | 7 (17.1) | 8 (20.0) | 15 (18.5) | 0.735 |
| Frequency of scheduled vitals | 0.438 | |||
| < 4x/day | 13 (31.7) | 19 (47.5) | 32 (39.5) | |
| ≥ 4x/day | 28 (68.3) | 21 (52.5) | 49 (60.5) | |
| Length of stay, days | 5.8 (3.9) | 6.8 (5.6) | 6.3 (4.8) | 0.378 |
| Any exposure to ICU/CCU | 3 (7.3) | 4 (10.0) | 7 (8.6) | 0.668 |
| Most responsible diagnosis | ||||
| DM | 2 (4.9) | 0 (0.0) | 2 (2.5) | 0.132 |
| Delirium | 1 (2.4) | 2 (5.0) | 3 (3.7) | |
| HF | 3 (7.3) | 5 (12.5) | 8 (9.9) | |
| Infection | 14 (34.1) | 17 (42.5) | 31 (38.3) | |
| Substance | 9 (22.0) | 4 (10.0) | 13 (16.0) | |
| VTE | 4 (9.8) | 0 (0.0) | 4 (4.9) | |
| Other | 8 (19.5) | 12 (30.0) | 20 (24.7) |
Numbers are displayed as n (%) for categorical variables and mean (SD) for continuous variables. p-values calculated using Chi-square test (categorical) or t-test (continuous)
3.1. Sleep outcome measures
No significant differences were found in self-reported duration of night-time sleep in hospital (median 5.0 versus 5.0 hours, p = 0.29) or daytime sleep in hospital (median 1.0 versus 0.5 hours, p = 0.43) between the intervention and control patients, respectively. There was also no significant difference between intervention and control patients by VSH subscales, or cumulative sleep disturbance (median 420 versus 359, p = 0.19), efficacy (median 169 versus 192, p = 0.29), or supplementation (median 97 versus 100, p = 0.51) scales. No significant differences between individual units were found when analysed separately.
Multivariate regression analysis was performed for self-reported average night-time sleep in hospital (Table 2). Only sex was significantly associated with duration of sleep (females reported longer sleep duration); intervention group was not significantly associated with sleep duration, nor were history of sleep disorder, single versus multi-patient rooms, or shift work.
Table 2.
Multivariable regression model for self-reported average night-time sleep in hospital.
| Variable | Average night-time sleep in hospital | |
|---|---|---|
| Adjusted regression coefficient (95% CI) | p-value | |
| Intervention (vs. control group) | −1.11 (−2.55, 0.32) | 0.127 |
| Age | 0.03 (−0.01, 0.07) | 0.141 |
| Female | 1.48 (0.11, 2.85) | 0.035 |
| Self-reported previous diagnosis of sleep disorder | −0.37 (−1.85, 1.11) | 0.618 |
| Single patient room | −0.90 (−2.57, 0.77) | 0.285 |
| Any time in ICU/CCU | −1.66 (−4.03, 0.71) | 0.166 |
| Comorbidity – Cancer | 0.04 (−1.67, 1.75) | 0.965 |
| Comorbidity – Pulmonary | −1.37 (−2.91, 0.16) | 0.079 |
| Shift-work in past year | −1.35 (−3.13, 0.44) | 0.137 |
3.2. Sleep aid usage
Sleep aid use was similar between the intervention and control units (30% versus 29.3%, p = 0.943). Zopiclone was the most commonly prescribed sleep aid, received by 17% of patients, followed by benzodiazepines (6%), antipsychotics (6%), antidepressants (4%), and melatonin (2%).
3.3. Qualitative data
Reasons for poor sleep given by patients were similar to previous studies. Noise was cited by 48% of intervention patients and 44% of control patients (p = 0.75). Other common environmental factors included care interruptions such as for vital signs or intravenous medications (20% versus 22%, p = 0.83), uncomfortable beds (20% versus 17%, p = 0.73), lighting (7.5% versus 12%, p = 0.48), and unfamiliarity of surroundings (18% versus 17%, p = 0.96) for intervention and control patients, respectively. Disease-related factors were infrequently cited (<10%) and included pain, anxiety, and cough. Other infrequently cited factors included intravenous lines, temperature, odours, and decreased daytime activity.
4. Discussion
Sleep quality, by self-reported duration of sleep and by VSH sleep scores, did not change significantly with the ‘TUCK-in’ protocol. Although intervention ward staff reported good implementation of the protocol, patients in intervention wards identified the same barriers to good sleep as patients on control units, including factors that our protocol was designed to address.
This study may have been influenced by a lack of true blinding. Patients were not purposefully made aware of their unit type, but many on the intervention units were cued by their care and/or the posters. This may have biased them to hold higher expectations. We also note that our study was conducted during a time of increased overcapacity utilization (i.e., rooms designed for 2 patients accommodating 3) compared with our pilot study in 2015 [4]. During these higher volume times, there are often more admissions during the night. These factors may have created additional challenges to sleep quality that our intervention was unable to address. Sleep quality for both the intervention and control groups was worse by self-reported measures and VSH scales when compared to our previous data on the same wards.
Encouragingly, multidisciplinary staff, particularly nursing, felt the protocol was beneficial to patient care, and have continued the protocol months after study period completion, suggesting there may be benefits not captured by our study outcomes.
5. Conclusions
Optimization of the hospital environment, including night-time sound and light minimization, limiting unnecessary interruptions, and bedtime cuing, to support inpatient sleep is attainable with multidisciplinary support. However, it remains unclear whether this translates into improved quality and/or quantity of sleep or improvements in inpatient outcomes.
Acknowledgments
We sincerely thank nursing staff and nursing management team for their support of this project. We would also like to thank Erik Youngson for statistical assistance. Funding for this study was provided by Alberta Health Services.
Appendix
Funding Statement
This work was supported by Alberta Health Services.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1]. Bonnet MH, Arand DL.. Consequences of insomnia. Sleep Med Clin. 2006;1:351–358. [Google Scholar]
- [2]. Knauert MP, Malik V, Kamdar BB. Sleep and sleep disordered breathing in hospitalized patients. Semin Resp Crit Care Med. 2014;35:582–592. [DOI] [PubMed] [Google Scholar]
- [3]. Gay PC. Sleep and sleep-disordered breathing in the hospitalized patient. Resp Care. 2010;55:1240–1254. [PubMed] [Google Scholar]
- [4]. Dobing S, Frolova N, McAlister F, et al. Sleep quality and factors influencing self-reported sleep duration and quality in the general internal medicine inpatient population. PLOS One. 2016;11:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. Stepanski EJ, Wyatt JK. Use of sleep hygiene in the treatment of insomnia. Sleep Med Rev. 2003;7:215–225. [DOI] [PubMed] [Google Scholar]
- [6]. Hu R, Jiang X, Chen J, et al. Non-pharmacological interventions for sleep promotion in the intensive care unit. Cochrane Database Syst Rev. 2015;10:1–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. Tamrat R, Huynh-Le M, Goyal M. Non-pharmacologic interventions to improve the sleep of hospitalized patients: A systematic review. J Gen Intern Med. 2014;29:788–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8]. Bartick MC, Thai X, Schmidt T, et al. Decrease in as needed sedative use by limiting nighttime sleep disruptions from hospital staff. J Hosp Med. 2010;5:E20–E24. [DOI] [PubMed] [Google Scholar]
- [9]. Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. [DOI] [PubMed] [Google Scholar]
- [10]. Snyder-Halpern R, Verran JA. Instrumentation to describe subjective sleep characteristics in healthy subjects. Res Nurs Health. 1987;10:155–163. [DOI] [PubMed] [Google Scholar]


