Abstract
Setting: Programmes that integrate mental health care into primary care settings could reduce the global burden of mental disorders by increasing treatment availability in resource-limited settings, including Rwanda.
Objective: We describe patient demographics, service use and retention of patients in care at health centres (HC) participating in an innovative primary care integration programme, compared to patients using existing district hospital-based specialised out-patient care.
Design: This was a retrospective cohort study using routinely collected data from six health centres and one district hospital from October 2014 to March 2015.
Results: Of 709 patients, 607 were cared for at HCs; HCs accounted for 88% of the total visits for mental disorders. Patients with psychosis used HC services more frequently, while patients with affective disorders were seen more frequently at the district hospital. Of the 68% of patients who returned to care within 90 days of their first visit, 76% had a third visit within a further 90 days. There were no significant differences in follow-up rates between clinical settings.
Conclusion: This study suggests that a programme of mentorship for primary care nurses can facilitate the decentralisation of out-patient mental health care from specialised district hospital mental health services to HCs in rural Rwanda.
Keywords: mental disorders, task-sharing, mentorship, operational research
Abstract
Contexte : Les programmes qui intègrent les soins de santé mentale dans les structures de soins de santé primaires pourraient réduire le fardeau mondial des troubles mentaux en augmentant la disponibilité du traitement dans des contextes de ressources limitées, notamment au Rwanda.
Objectif : Nous décrivons les caractéristiques démographiques des patients, leur utilisation des services et la rétention des patients en traitement dans les centres de santé (HC) participant à un programme innovant d'intégration dans les soins de santé primaires, comparés aux patients recourant aux consultations spécialisées existantes, basées dans les hôpitaux de district.
Schéma : Une étude rétrospective de cohorte basée sur des données recueillies en routine dans six centres de santé et dans un hôpital de district, entre octobre 2014 et mars 2015.
Résultats : De 709 patients, 607 ont été soignés dans les HC et les HC ont totalisé 88% de l'ensemble des consultations pour troubles mentaux. Les patients atteints de psychose ont plus souvent utilisé les services des HC, tandis que les patients atteints de troubles affectifs ont été plus souvent vus à l'hôpital de district. De 68% des patients qui sont revenus dans les 90 jours suivant leur première consultation, 76% ont eu une troisième consultation au cours des 90 jours suivants. Il n'y a pas eu de différences significatives en termes de taux de suivi entre les deux contextes cliniques.
Conclusion : Cette étude suggère qu'un programme de tutorat destiné aux infirmiers de soins de santé primaires peut faciliter la décentralisation de la prise en charge de la santé mentale en consultation externe des services de santé mentale des hôpitaux spécialisés de district vers les HC dans le Rwanda rural.
Abstract
Marco de referencia: Los programas que integran la atención de la salud mental al entorno de la atención primaria podrían reducir la carga mundial de morbilidad por trastornos mentales, al aumentar la disponibilidad del tratamiento en los medios con escasos recursos, por ejemplo en Rwanda.
Objetivo: Se describen las características demográficas, la utilización de los servicios y la retención en la atención, de los pacientes atendidos en los centros de salud que participan en un programa innovador de atención primaria y se comparan con los pacientes que acuden a la consulta ambulatoria especializada que se presta en un hospital distrital.
Método: Fue este un estudio de cohortes retrospectivo a partir de los datos recogidos de manera sistemática en seis centros de salud y un hospital distrital, de octubre del 2014 a marzo del 2015.
Resultados: De los 709 pacientes, se atendieron 607 en los centros de salud y estos centros realizaron el 88% del total de consultas por trastornos mentales. Los pacientes con trastornos psicóticos utilizaban con mayor frecuencia los servicios en los centros de salud, pero los pacientes con trastornos del afecto se atendían con mayor frecuencia en el hospital distrital. El 68% de los pacientes regresaron al servicio de atención en los 90 días que siguieron a su primera consulta y el 76% de ellos acudió a una tercera consulta en los siguientes 90 días. No se observaron diferencias significativas en las tasas de seguimiento en los diferentes entornos clínicos.
Conclusión: Los resultados del presente estudio ponen de manifiesto que un programa tutorial dirigido al personal de enfermería de los centros de atención primaria puede facilitar la descentralización de la atención ambulatoria de los pacientes con trastornos de salud mental, desde el hospital distrital con servicios especializados hacia los centros de salud en zonas rurales de Rwanda.
Neuropsychiatric disorders account for 14% of the estimated global burden of disease, of which 75% is in low- and middle-income countries (LMICs).1 Although there is significant evidence supporting the efficacy of treatment for mental disorders, the treatment gap is estimated to be almost 90% across LMICs.2 There are many reasons for this, including shortages in adequately trained specialist providers, limited funding for services and a paucity of leadership and management support dedicated to mental health (MH).1,2
Rwanda, located in eastern sub-Saharan Africa, is one of the few LMICs to have a national plan to address the burden of mental disorders. The devastating impact of the 1994 genocide against the Tutsi population led the government to create a division for MH within the Ministry of Health (MoH) during the post-genocide reconstruction of the health system.3,4 Rwanda's national mental health policy aims to reduce the treatment gap by placing mental health services within public district health systems and decentralising care from national referral centres into district continuums of care.5 The MoH has been successful in placing at least one psychologist and one psychiatric nurse at each district hospital in the country to provide both out-patient and in-patient level specialty services within general medical settings.3,5,6
The number of specialised MH care providers at district hospitals in Rwanda does not yet meet the tremendous burden of disease; however, Rwanda's national MH policy also articulates the importance of improving access to treatment by integrating MH care into rural primary care health centres.5,7 Partners In Health (PIH), an international non-governmental organisation known locally as Inshuti Mu Buzima (IMB), has been working to support the public health system in three rural districts in Rwanda since 2005. Beginning in 2012, IMB has collaborated with the MoH to design an approach to support the integration of MH care into primary care, called the Mentoring and Enhanced Supervision at Health Centres for Mental Health (MESH MH) programme. MESH MH utilises task sharing—delegating responsibilities from specialised mental health clinicians to less specialised health workers—by capacitating primary care nurses to treat patients with mental disorders through a structured programme of supported mentorship and supervision by MoH psychiatric nurses and systems-level quality improvement initatives.8 The model is based on an existing primary care strengthening programme designed to improve the quality of care in a variety of clinical domains in IMB-supported districts.9 Since the inception of MESH MH, IMB has supported the programme's implementation at government health centres in one rural district of Rwanda (Burera District), with the goal of articulating a model that could potentially inform the scale-up of MH services at primary care centres throughout the country.
As MH care is progressively shared from the district hospital out-patient speciality clinic to primary care health centres in Burera District, it is critical to document and understand MH service provision trends. In this study, we examined patient demographics, service use and retention of patients in care at primary care health centre (HC) clinics participating in the MESH MH programme, in comparison to existing out-patient speciality MH services available at the district hospital.
METHODS
Study design
This was a descriptive cohort study that used routinely collected clinical data from patients seen at six primary care HC clinics in one rural district of Rwanda supported by the MESH MH programme, and at the district hospital's out-patient MH clinic.
Study setting
The study took place in Burera District (BD), northern Rwanda. Rwanda is classified as a low-income country, and more than 80% of the population live in rural areas and rely on subsistence farming.10 BD has a population of about 340 000 and is served by the 150-bed public Butaro District Hospital (BDH). The hospital is the primary referral centre for 19 HCs within the district. MH service provision in BD is supported by the IMB MH team, which, at the time of the study, included one programme manager, one community coordinator, one research coordinator, and several data officers. The IMB MH team is further supported by an expatriate psychiatrist, the Pagenel Fellow in Global Mental Health Delivery (Harvard Medical School, Boston, MA, USA, http://ghsm.hms.harvard.edu/education/fellowships#pagenel). The IMB team and the Pagenel Fellow are supported in turn by a PIH cross-site mental health team, which includes several psychiatrists with extensive experience in MH care delivery, global MH and public health.
District mental health services
Prior to the implementation of the MESH MH programme, out-patient MH care in BD was provided almost entirely by the hospital-based out-patient speciality clinic. The BDH out-patient MH clinic is run by one psychologist and four psychiatric nurses, with periodic supervision provided by visiting MoH psychiatric nurses. The clinic provides out-patient mental health services 5 days per week, including problem-based counselling and psychotropic medication management for patients with mental disorders and epilepsy. Patients with acute MH needs are admitted to BDH for treatment or are transferred to the national psychiatric referral centre if further specialised treatment is required.
The MESH MH programme
The MESH MH programme consists of a 5-day training course for HC primary care nurses, and is based on guidelines provided by the MoH and the World Health Organization's Mental Health Gap Action Programme (mhGAP) for non-specialist providers, as well as other PIH curriculum.5,11 The training is designed to capacitate primary care nurses to treat patients with severe mental disorders, particularly psychosis, depression, bipolar disorder and epilepsy, at the HC level. The training is followed by a programme of regular weekly structured supervision of the primary care nurses by MoH psychiatric nurse-mentors, as well as systems-based quality improvement efforts with nurses and health centre directors. Through the programme, primary care nurses are equipped to perform basic patient assessments, provide treatment including basic medication management and psycho-education, coordinate community support and manage follow-up care. Complicated cases or patients requiring acute MH care are referred to BDH for specialised care. The MESH MH programme was initially established at three district HCs in August 2012 and three additional HCs in August 2013, with plans for scale-up to the remaining district HCs over the subsequent years, with support from a proof-of-concept grant from Grand Challenges Canada (Toronto, ON, Canada).
Study population
All patients diagnosed with any mental disorder or epilepsy who had at least one MH visit at either the BDH out-patient MH clinic or one of the established six HCs supported by the MESH MH programme between 1 October 2014 and 31 March 2015 were included in the analysis. Patients being treated as in-patients at BDH and patients who did not have a visit date recorded were excluded from the analysis.
Data collection and analysis
Patient data were recorded in MH-specific paper registers at each participating HC and the BDH clinic. Collected variables included: sex, age, location of appointment, distance from home to the appointment location, primary diagnosis and the dates of individual patients' appointments over the study period. The IMB-supported district data team abstracted disaggregated patient variables from the MH registers into a centralised Microsoft Access database (Microsoft Corp, Redmond, Washington, USA).
Primary diagnosis was defined as the diagnosis made by the assessing clinician at the patient's first visit. Less common diagnoses (anxiety disorders, somatoform disorders, post-traumatic stress disorder, substance abuse and uncertain diagnoses) were combined into one category, labelled ‘other’. Service use was assessed by calculating the total number of unique patients and total number of patient visits for MH care per facility (BDH and all HCs combined) for each month of the study. Retention in care was based on follow-up visits; patients who had a second visit to any MH clinic within 90 days of their visit were considered to be retained in care. The number of patients with a second visit who then returned for a third visit within 90 days of their second visit was also calculated. Numbers and percentages were reported for categorical variables, and a two-tailed Fisher's exact test with a 5% significance level was used to compare variables for associations. Odds ratios (OR) and 95% confidence intervals (95%CI) were reported to measure associations between retention rates by diagnosis. The data were analysed using Stata v.13.1 (Stata Corp, College Station, TX, USA).
Ethics
Ethics approval was obtained from the Rwanda National Ethics Committee (Kigali, Rwanda, protocol #736/RNEC/2016) and the PIH/IMB research committee (Kigali, Rwanda). The study met the Médecins Sans Frontières Ethics Review Board (Geneva, Switzerland) approved criteria for studies of routinely collected data. As the study was completed using de-identified routinely collected programme data, informed consent was not required.
RESULTS
Of a total of 709 unique patients who received MH care in participating BD facilities from 1 October 2014 to 31 March 2015, 607 (85.6%) patients received care at the HCs and 102 (14.4%) patients received care at the BDH MH out-patient clinic. Table 1 shows the demographics of patients seen at the HCs and the BDH clinic. There were no significant differences in the ages or sex of the patients. However, 53.6% of the patients seen at BDH travelled ⩾5 km from their home to reach the facility, compared with 14.5% of those seen at the HCs (P < 0.001).
TABLE 1.
Characteristics of patients attending mental health services at six select health centres and the hospital-based clinic in Burera District, Rwanda, October 2014–March 2015 (N = 709)
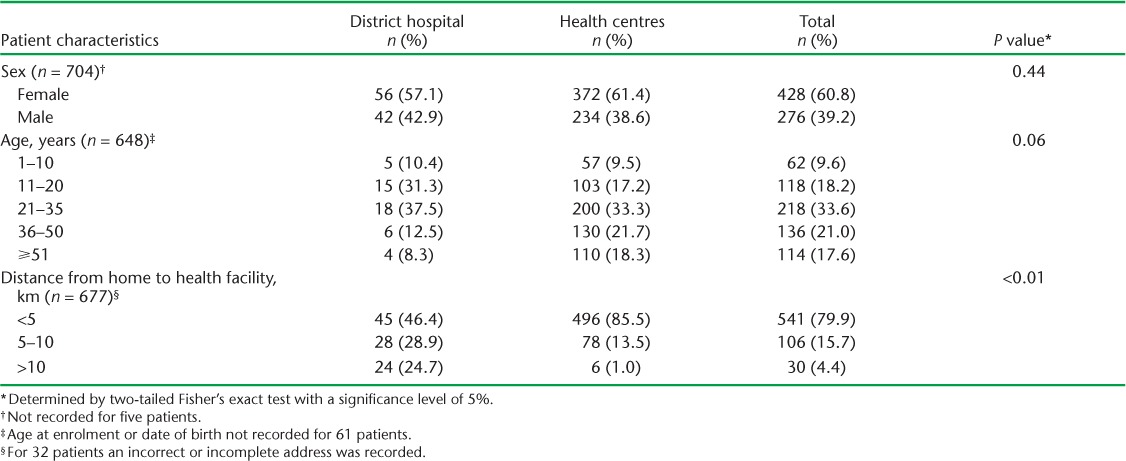
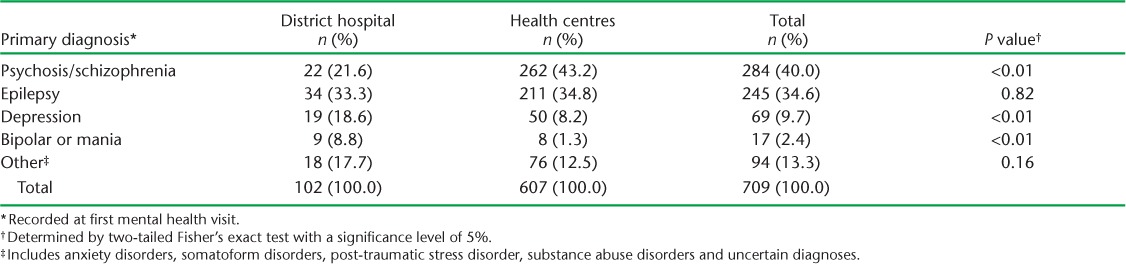
Table 2 shows the primary diagnoses at the BDH clinic compared with the HCs. Significantly more patients using MH services with psychotic disorders were seen at the HCs than at the BDH clinic (43.2% vs. 21.6%, P < 0.01). The BDH clinic saw a significantly higher percentage of patients with depression (18.6% vs. 8.2%, P < 0.01) and bipolar disorder (8.8% vs. 1.3%, P < 0.01) than the HCs. Overall, the total number of patients with epilepsy and psychotic disorders was proportionally much higher than the number of patients with affective disorders at all of the included sites.
TABLE 2.
Diagnosis of patients attending mental health services by health facility type, Burera District, Rwanda, October 2014–March 2015
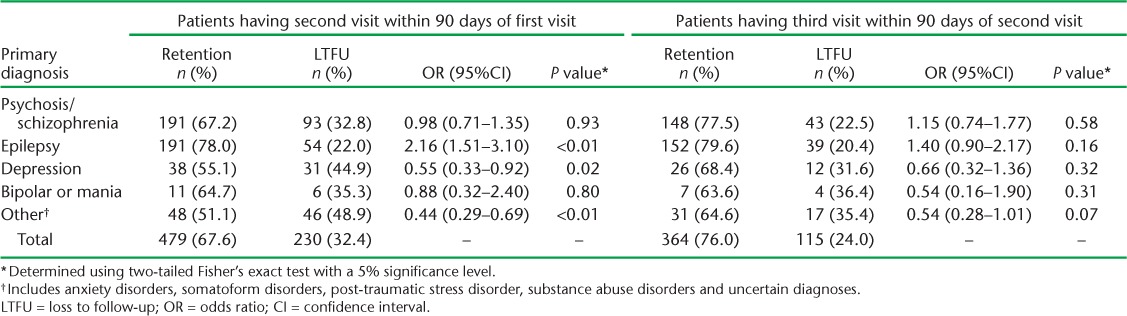
The total number of MH visits over the 6-month study period was 1934, of which 1707 (88.3%) occurred at the HCs and 227 (11.7%) at BDH (Table 3). The number of visits at the HCs and the BDH clinic was relatively steady over the study period. Table 4 shows the patient follow-up rates; of the 709 individual patients seen, 67.5% returned within 90 days for a second visit and 76.0% of these also returned for a third visit within 90 days of their second visit. Overall, across both types of facilities, 51.3% of individual patients returned for both a second and a third visit in the 6 months following their initial visit. There was no significant difference in return rates for a second and third visit by health facility type. Table 5 shows that the patients with epilepsy were more likely to return for care within 90 days of their first visit than the patients with any diagnosis of a mental disorder (OR 2.16, 95%CI 1.51–3.10). Patients with depression were the least likely to return to care following their initial visit for mental health care, relative to patients with all other diagnoses (OR 0.55, 95%CI 0.33–0.92).
TABLE 3.
Total number of mental health visits per facility type by month, Burera District, Rwanda, October 2014–March 2015
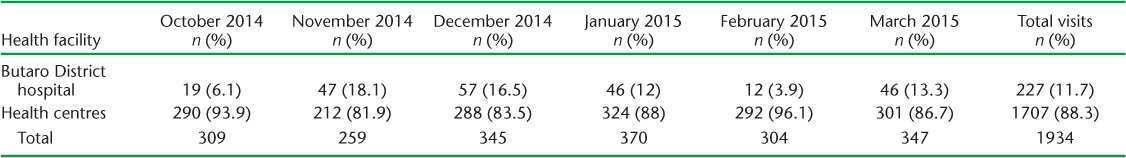
TABLE 4.
Retention rates by health facility type, Burera District, Rwanda, October 2014–March 2015
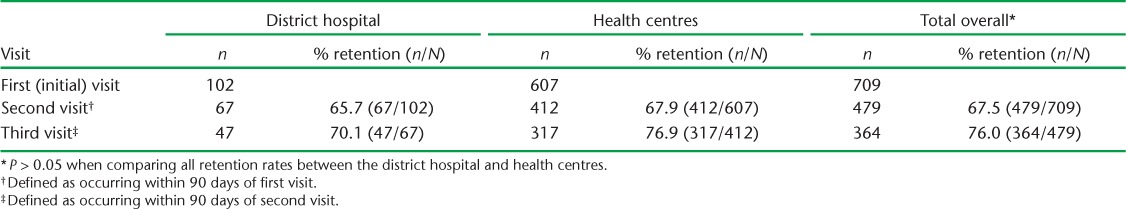
TABLE 5.
Diagnosis of patients attending mental health services by retention rate, Burera District, Rwanda, October 2014–March 2015
DISCUSSION
Globally, although the call to decentralise MH care and integrate it into primary care settings has been strong, there is little information available about service delivery trends from places where this has been attempted. To our knowledge, this is the first study undertaken in rural Rwanda, and one of the first in rural Africa, to compare patient demographics and service use of a district hospital-based speciality out-patient MH clinic with the characteristics of patients seen at district primary care HCs newly offering MH services via a programme of supported supervision, mentorship and systems-based quality improvement.
Our data demonstrate some important service use trends about MH care as it was decentralised within the district. Throughout our study period, the majority of patients with mental disorders seeking care within the district did so at primary care settings newly offering MH services. The service uptake at primary care clinics was relatively rapid and consistent, considering that the MESH MH programme had been implemented for less than 24 months at the participating HCs. Location may have contributed to this uptake; there is ample evidence that one of the greatest challenges for people living in rural areas to access health care is the distance to the nearest facility.12 In our population, patients seen for an MH visit at HCs travelled significantly less distance on average to access services than patients seen at BDH. Offering integrated MH services at HCs appears to have increased the accessibility of MH care within the district, although we do not have data on the proportion of patients who were entirely new to care or the coverage rates for specific disorders. In addition to the distance to services, the patients' perceived acceptability of using primary care HCs to provide MH care may be a contributing factor for the uptake and consistency of HC MH service use. Further research is needed to understand why mental health care is pursued at specialised vs. primary care clinics, and to measure the experienced acceptability for patients of receiving MH care at primary care HCs.
The top three leading diagnostic categories at the BDH clinic and the HCs were psychosis/schizophrenia, epilepsy and depression. These data are generally aligned with published data on the burden of mental and neurological disorders across LMICs; depression and schizophrenia are in the top 10 leading causes of disability across the globe, and LMICs are reported to carry 80% of the global epilepsy burden.13
The distribution of diagnoses across service levels reveals some important differences. For example, patients with psychosis were more likely to use services at the HCs than at BDH. This may reflect the challenges for patients and families with severe mental disorders to seek care if it is a significant distance from their home. It is also possible that HCs, as the health service level closest to the community, are generally better able to coordinate with available community-based resources to facilitate treatment for psychotic disorders. Surprisingly, patients with mood disorders (depression and bipolar disorder) as well as other disorders, were more likely to receive care at BDH. This may reflect a perception that services for mood disorders are more comprehensive at the speciaised clinic, which offers problem-based counselling, psycho-education and community-based support. However, the absolute number of patients with mood disorders seen at both BDH and the HCs was lower than what might be expected based on disease prevalence data in Rwanda.4,14 This may indicate a need for improved screening, community education, increased outreach and collaboration with community-based interventions, to reach people with depression who may not otherwise present to MH services.
We found no significant differences in retention rates between the BDH clinic and the HCs. Similarity in retention rates may indicate that generalist nurses staffing the HCs are able to provide care to patients that is equally as satisfactory as care provided at specialised MH clinics. Overall, the retention rate was 67% for a first follow-up visit, and 51% had a first- and second follow-up visit and remained in care after 6 months. These data are comparable to studies on out-patient follow-up for mental disorders in more resource-rich systems, but are not as high as anticipated during MESH MH programme development, given that proximity to care for patients increased with the MESH MH programme implementation.15,16 There were also some differences in retention rate by diagnosis: people with epilepsy were more than twice as likely to return to care, and people with depression were only about half as likely to return to care compared to people with other diagnoses, although these distinctions were no longer significant for the second follow-up visit. Possible reasons for loss to follow-up include differing perceptions on mental disorders among users of MH services, severity of illness, socio-economic barriers and stigma. For example, follow-up for epilepsy may be facilitated by community awareness; following a 2005 study of sociocultural perceptions of epilepsy in Rwanda, numerous actions were taken by the MoH and other organisations to increase awareness about epilepsy and reduce stigma.17 More research is needed to understand reasons for return to care and loss to follow-up for patients seen at both specialised and primary care MH clinics.
The primary limitation of this study is that it is a retrospective review of routinely collected data. The use of routine data does not allow us to draw causal inferences about programme implementation and service use changes, and includes challenges such as missing information, variations in data clarity and the manual labour required to collect data from paper registers. Our study was also limited to 6 months, largely due to delays in timely data collection for a newly implemented programme at HCs. Despite the limitations, our study represents one of the first descriptions of patient demographics and service use patterns in a rural, low-resource district that is decentralising care from a hospital-based specialised MH clinic to primary care settings through an innovative programme of supported supervision, mentorship and systems-based quality improvement, to improve access to MH care and reduce the burden of mental illness across the district.
CONCLUSION
This study suggests that MH care can be decentralised from specialised services at a district hospital to non-specialist nurses at primary care HCs, while maintaining considerable service demand and equivalent rates of retention. Challenges remain with providing adequate coverage for mental disorders and retention in care, even when care is provided closer to a patient's home. Our results can be used to inform the gaps in MH care that exist in rural Rwanda, and can be applied to other, similar contexts. Further research is needed to validate these findings and analyse patient-level clinical outcomes and experiences of care before scale-up is considered.
Acknowledgments
The integration of mental health care into primary care settings (MESH MH program) reported in this paper was funded from 2014 to 2016 by Grand Challenges Canada. The data collection and research that resulted in this publication was supported by the Inshuti Mu Buzima (IMB) Mental Health Team (Kigali, Rwanda), the Partners In Health cross-site mental health team, the IMB Research Department, the MESH Quality Improvement Program team, the IMB Monitoring and Evaluation team, as well as all Burera District mental health clinicians, the Burera District primary care nurses, and the Ministry of Health and leadership who manage Butaro District hospital and the health centers. We especially thank the Mental Health Division of the Rwanda Biomedical Center, led by Dr Yvonne Kayiteshonga, for its strategic vision for this work. This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO/TDR, Geneva, Switzerland). The training model is based on a course developed jointly by the International Union Against Tuberculosis and Lung Disease (The Union, Paris, France) and Médecins Sans Frontières (MSF, Geneva, Switzerland). The specific SORT IT programme that resulted in this publication was implemented by: MSF, Brussels Operational Centre (Luxembourg) and the Centre for Operational Research, The Union. Mentorship and the coordination/facilitation of these SORT IT workshops were provided through the Centre for Operational Research, The Union, the MSF Operational Research Unit (LuxOR), Academic Model Providing Access to Healthcare (AMPATH, Eldoret, Kenya); Institute of Tropical Medicine (Antwerp, Belgium); University of Gondar (Gondar, Ethiopia); School of Public Health, Johns Hopkins University (Baltimore, MD, USA); Luke International (Malawi Office, Mzuzu, Malawi); Centre for International Health, University of Bergen (Bergen,Norway); and the Northern State Medical University (Arkhangelsk, Russian Federation). The SORT IT programme was funded by the Department for International Development (London, UK), The Union, MSF and La Fondation Veuve Emile Metz-Tesch (Luxembourg). La Fondation Veuve Emile Metz-Tesch supported the open access publication costs. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflicts of interest: none declared.
In accordance with WHO's open-access publication policy for all work funded by WHO or authored/co-authored by WHO staff members, the WHO retains the copyright of this publication through a Creative Commons Attribution IGO licence (http://creativecommons.org/licenses/by/3.0/igo/legalcode) that permits unrestricted use, distribution and reproduction in any medium provided the original work is properly cited.
References
- 1. Prince M, Patel V, Saxena S, . et al. No health without mental health. Lancet 2007; 370: 859– 877. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization. . Investing in mental health: evidence for action. Geneva, Switzerland: WHO, 2003. http://apps.who.int/iris/bitstream/10665/87232/1/9789241564618_eng.pdf Accessed July 2017. [Google Scholar]
- 3. Mohand A A, Kayiteshonga Y.. The set-up of a national mental health programme in Rwanda. Basel, Switzerland: 9th European Congress on Tropical Medicine and International Health, 6–10 September, 2015. [Google Scholar]
- 4. Munyandamutsa N, Nkubamugisha P M, Gex-Fabry M, Eytan A.. Mental and physical health in Rwanda 14 years after the genocide. Soc Psychiatry Psychiatr Epidemiol 2012; 47: 1753– 1761. [DOI] [PubMed] [Google Scholar]
- 5. Republic of Rwanda Ministry of Health. . National Mental Health Policy in Rwanda. Kigali, Rwanda: MOH, 2011. http://www.moh.gov.rw/fileadmin/templates/Docs/Posted-National-Mental-health-Policy-1.pdf Accessed July 2017. [Google Scholar]
- 6. Katchanov J, Birbeck G L.. Epilepsy care guidelines for low- and middle-income countries: from WHO mental health GAP to national programmes. BMC Med 2012; 10: 107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shekar S, Graham T, Martin K, Harvey W.. Resources for mental health: scarcity, inequity, and inefficiency. Lancet 2007; 370: 878– 889. [DOI] [PubMed] [Google Scholar]
- 8. Smith S L, Kayiteshonga Y, Misago C N, . et al. Integrating mental health care into primary care: the case of one rural district in Rwanda. Intervention 2017; 15: 136– 150. [Google Scholar]
- 9. Manzi A, Hema M, Vanessa R, . et al. Nurse mentorship to improve the quality of health care delivery in rural Rwanda. Nurs Outlook 2013; 61: 137– 144. [DOI] [PubMed] [Google Scholar]
- 10. National Institute of Statistics of Rwanda, Ministry of Health, ICF International. . Rwanda Demographic and Health Survey 2014–15. Rockville, Maryland, USA: NISR, MOH, ICF International, 2015. https://dhsprogram.com/pubs/pdf/FR316/FR316.pdf Accessed July 2017. [Google Scholar]
- 11. World Health Organization. . mhGAP intervention guide for mental, neurological and substance use disorders in non-specialized health settings. Version 1.0. Geneva, Switzerland: WHO, 2010. http://www.who.int/mental_health/publications/mhGAP_intervention_guide/en/ Accessed July 2017. [PubMed] [Google Scholar]
- 12. Thomas A A, Wilbert M G, John S P, Jill S, Spencer J, Perin J.. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv Res 2005; 40: 135– 155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kassebaum N J, Arora M, Barber R M, . et al. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388: 1603– 1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bolton P, Neugebauer R, Ndogoni L.. Prevalence of depression in rural Rwanda based on symptom and functional criteria. J Nerv Ment Dis 2002; 190: 631– 637. [DOI] [PubMed] [Google Scholar]
- 15. Olfson M, Mojtabai R, Sampson N A, . et al. Dropout from out-patient mental health care in the United States. Psychiatr Serv 2009; 60: 898– 907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McIvor R, Ek E, Carson J.. Non-attendance rates among patients attending different grades of psychiatrist and a clinical psychologist within a community mental health clinic. BJ Psych Bulletin 2004; 28: 5– 7. [Google Scholar]
- 17. Sebera F, Munyandamutsa N, Teuwen D E, . et al. Addressing the treatment gap and societal impact of epilepsy in Rwanda - results of a survey conducted in 2005 and subsequent actions. Epilepsy Behav 2015; 46: 126– 132. [DOI] [PMC free article] [PubMed] [Google Scholar]


