Abstract
Mental disorders and alcohol/drug use worsen treatment outcomes for multidrug-resistant tuberculosis (TB), but data are lacking for extensively drug-resistant (XDR) TB. We investigated the association of baseline mental disorders and alcohol/drug use on XDR-TB treatment outcomes in a retrospective study of 53 XDR-TB Peruvian patients during 2010–2012. Logistic regression estimated the odds ratios for unfavourable XDR-TB treatment outcomes. Overall treatment success was 25%. Mental disorders and drug/alcohol use were found in respectively 22.4% and 20.4% of patients; neither were associated with unfavourable treatment outcomes. Future research should explore the relationship between mental health and drug/alcohol use in XDR-TB treatment outcomes.
Keywords: depression, anxiety, psychosis, alcohol, XDR-TB
Abstract
Les troubles mentaux et la consommation d'alcool/de drogue entravent le résultat du traitement de la tuberculose multirésistante (TB-MDR), mais on manque de données pour la TB ultrarésistante (TB-XDR). Nous avons examiné l'association de troubles mentaux préexistants et de consommation d'alcool/de drogue sur le résultat du traitement de la TB-XDR dans une étude rétrospective de 53 patients péruviens atteints de TB-XDR en 2010–2012. Une régression logistique a estimé les odds ratios de résultat défavorable du traitement de la TB-XDR. Le taux d'ensemble de succès du traitement a été de 25%. Des troubles mentaux et une consommation d'alcool/de drogue ont été constatés chez respectivement 22,4% et 20,4% des patients ; aucun n'a été associé à un résultat défavorable du traitement. Des recherches ultérieures devraient explorer la relation entre santé mentale et consommation de drogue/alcool et leur impact sur le traitement de la TB-XDR.
Abstract
Los trastornos mentales y el consumo de alcohol y de drogas agravan los desenlaces terapéuticos de la tuberculosis multidrogorresistente (TB-MDR), pero no existen datos en cuanto a la TB extremadamente resistente (TB-XDR). En un estudio retrospectivo en 53 pacientes peruianos que padecieron TB-XDR del 2010 al 2012, se investigó la asociación de la presencia inicial de trastornos mentales y consumo de alcohol o drogas con los desenlaces del tratamiento de la TB-XDR. Mediante un modelo de regresión logística se calcularon los cocientes de posibilidades de desenlaces terapéuticos desfavorables. La tasa global de éxito terapéutico fue de 25%. Se encontró que el 22,4% de los pacientes sufría trastornos mentales y el 20,4% consumía alcohol o drogas; ninguna de estas características se asoció con desenlaces desfavorables del tratamiento. Nuevas investigaciones tendrán que explorar la correlación que existe entre la salud mental y el consumo de alcohol o drogas y los desenlaces terapéuticos de la TB-XDR.
Adherence to antimicrobial regimens is critical for optimal tuberculosis (TB) treatment. Comorbid mental disorders, including depression, anxiety, psychosis and drug/alcohol use disorders—present in up to 70% of TB patients1—are associated with poorer outcomes.2 While some patients begin anti-tuberculosis treatment with pre-existing mental disorders, onset sometimes occurs due to added bio-psychosocial stressors during TB treatment, psychiatric side-effects of anti-tuberculosis drugs or drug interactions between antimicrobial and antipsychotic medications.1,3 Particularly for patients with multi-drug resistant (MDR) TB, where treatment can last for years, addressing comorbid mental disorders such as depression increases cure rates and patient wellbeing.4 A study from Peru was among the first to demonstrate the benefit of psychosocial support for MDR-TB patients with mental disorders, reporting a TB treatment non-completion rate of 3%.5 Nonetheless, integrated TB and mental health services are not the global norm.3 Moreover, only scant data exist on the prevalence of mental health comorbidities among MDR-TB patients, and we are unaware of any published data for extensively drug-resistant (XDR) TB, which requires longer, more toxic treatment regimens.
Peru, designated by the World Health Organization (WHO) as a high MDR-TB burden country, has an annual MDR-TB incidence rate of 10 per 10 000 population.6 This pilot study investigated the baseline prevalence of comorbid mental disorders and drug/alcohol use and their association with outcomes among a small sample of Peruvian XDR-TB patients.
ASPECT OF INTEREST
Methods
We conducted a retrospective case series analysing patients commencing their first XDR-TB treatment episode in Peru during 2010–2012. In accordance with Peru's National TB Programme (NTP) recommendations, XDR-TB patients receive a baseline clinical assessment from a psychologist or psychiatrist to screen for mental health conditions using the International Classification of Diseases 10th revision (ICD-10). Demographic and clinical data were abstracted from medical charts in the NTP's central archive onto paper forms during June–July 2015. The data were then single-entered and cleaned electronically using EpiData v3.1 (EpiData Association, Odense, Denmark), Excel 2011 (Microsoft Corp, Redmond, USA) and q (Ben-Attia Harel, Israel).
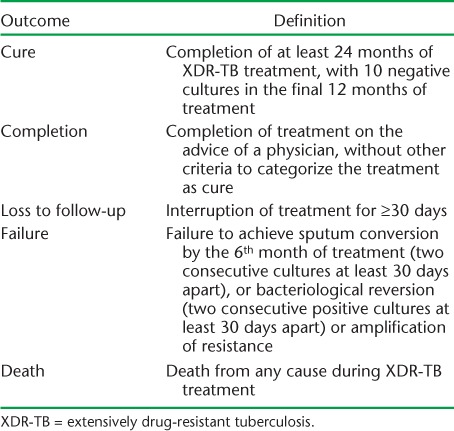
The prevalence of mental disorders—depression, anxiety, mixed anxiety-depressive disorder and psychosis—and alcohol and drug use was calculated. Using the Peruvian NTP definition for XDR-TB treatment outcomes (Table 1), we estimated the crude odds ratios (OR) for unfavourable (failure, loss to follow-up, death) outcomes for mental disorders and current drug/alcohol use using exact logistic regression using Stata 13.0 (StataCorp, College Station, TX, USA).
TABLE 1.
Definitions of XDR-TB treatment outcomes, Peru National Tuberculosis Programme
The study was approved by the Human Ethics Research Committees at the Universidad Peruana Cayetano Heredia (Lima, Peru) and London School of Hygiene & Tropical Medicine (London, UK).
RESULTS
We abstracted treatment data for 53 XDR-TB patients who were mostly males aged 19–66 years living in metropolitan Lima/Callao. One patient was a secondary XDR-TB case, while the remainder had a median of 2.35 years of previous anti-tuberculosis treatment (interquartile range [IQR] 9.6 months–3.75 years). Of the 53 patients, 49 had documented psychiatric evaluations, of whom 11/49 were diagnosed with a mental disorder: five with depression, three with anxiety, two with mixed anxiety-depressive disorder and one with psychosis. Overall treatment outcomes were: 12/49 favourable (seven cured, five completed) and 37/49 unfavourable (11 lost to follow-up, 11 failures and 15 deaths). Among those diagnosed with mental disorders, 9/11 had an unfavourable treatment outcome. Three of the four patients without psychiatric assessments had unfavourable outcomes (Table 2).
TABLE 2.
Prevalence of psychiatric conditions at baseline among 49 patients commencing XDR-TB treatment in Peru, 2010–2012
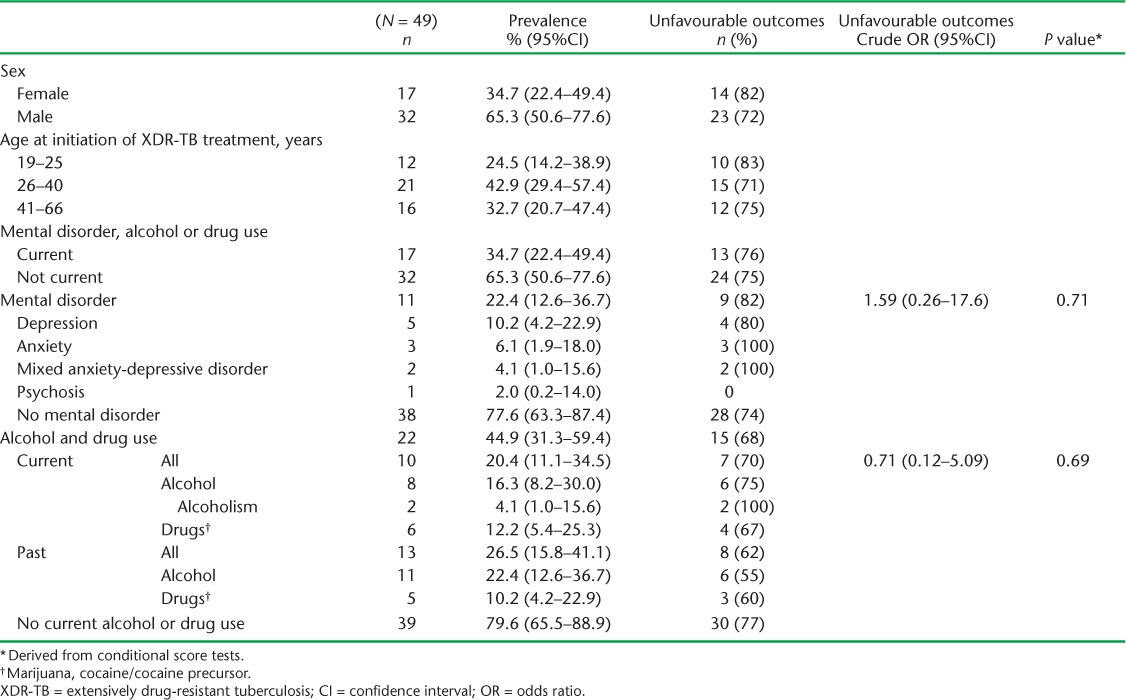
Regarding alcohol use, 8/49 patients were consuming alcohol at baseline, of whom two were diagnosed with alcoholism. A further 11/49 had a history of alcohol consumption. Six patients currently used drugs; five more had a history of drug use. Nearly half (22/49) had a current or prior history of alcohol/drug use; these patients tended to have unfavourable outcomes.
There was no statistical evidence that a diagnosis of mental disorder (OR 1.59, 95% confidence interval [CI] 0.26–7.6, P = 0.70) or current alcohol/drug use (OR 0.71, 95%CI 0.12–5.09, P = 0.69) were associated with increased odds of worse XDR-TB treatment outcomes.
DISCUSSION
To our knowledge, this retrospective series is the first to report on XDR-TB psychiatric comorbidity in Peru or elsewhere. The point prevalences of baseline depression and anxiety observed in this cohort of XDR-TB patients were greater than for the adult population of Lima/Callao (10.2% vs. 2.8% and 6.1% vs. 1.9%, respectively), while rates of psychosis and alcohol/drug use were comparable to the general population.7 Compared to the first 75 MDR-TB patients in Peru to receive individualised therapy (1996–1999), depression was less prevalent in the present study (10.2% vs. 52.2%), but the prevalence of anxiety was similar (6.1% vs. 8.7%).8 However, our results for all psychiatric conditions are comparable to a larger MDR-TB cohort in Peru (22.4% vs. 18.9%).2 Nonetheless, we found no association of psychiatric conditions or drug/alcohol use with unfavourable XDR-TB outcomes.
Prospective studies and qualitative inquiry would shed further light on these unexpected findings. It may be that patients with pre-existing (prior to XDR-TB treatment) mental disorders were less likely to present for care, or had died before they could, and were therefore underrepresented in our sample. Alternatively, patients may have been too gravely ill to be evaluated with appropriate instruments, thereby underestimating the true prevalence of psychiatric disorders. Patients who were not using alcohol/drugs at baseline may have restarted once treatment improved their TB symptomatology. As it is unlikely that psychiatric disorders are protective factors during XDR-TB treatment, NTPs should assume that mental health interventions would increase patient wellbeing and reduce loss to follow-up. Initiatives such as the WHO End TB strategy9 and Zero TB,10 which include mental health support as core components, offer promise; however, more data are needed on specific comorbid mental disorders with XDR-TB to develop the most successful interventions.
Due to the small sample size and missing data, such as patients' socio-economic status and whether diagnoses were made by psychiatrists or psychologists, key confounders cannot be ruled out. As the mental health evaluations were performed at treatment initiation, we could not assess the incidence of mental disorders.
CONCLUSION
Baseline psychiatric disorders and drug/alcohol use were not associated with poor XDR-TB outcomes; however, overall treatment success was low. Appropriately powered cohort studies are needed to better understand mental health issues affecting XDR-TB patients throughout treatment and develop interventions that improve patients' survival and quality of life.
Acknowledgments
The authors thank the Tuberculosis Prevention and Control Directorate of the Peruvian Ministry of Health (Lima, Peru) for allowing access to patient health records. We also thank A Sweetland for her review of the manuscript.
JTG received support from the Abundance Foundation Fellowship in Global Mental Health Implementation Science.
Footnotes
Conflicts of interest: none reported.
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- 1. Doherty A M, Kelly J, McDonald C, O'Dywer A M, Keane J, Cooney J.. A review of the interplay between tuberculosis and mental health. Gen Hosp Psychiatry 2013; 35: 398– 406. [DOI] [PubMed] [Google Scholar]
- 2. Franke M F, Appleton S C, Bayona J, . et al. Risk factors and mortality associated with default from multidrug-resistant tuberculosis treatment. Clin Infect Dis 2008; 46: 1844– 1851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Walker I F, Baral S C, Wei X, . et al. Multidrug-resistant tuberculosis treatment programmes insufficiently consider comorbid mental disorders. Int J Tuberc Lung Dis 2017; 21: 603– 609. [DOI] [PubMed] [Google Scholar]
- 4. Sweetland A, Oquendo M, Wickramaratne P, Weissman M, Wainberg M.. Depression: a silent driver of the global tuberculosis epidemic. World psychiatry 2014; 13: 325– 326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Acha J, Sweetland A, Guerra D, Chalco K, Castillo H, Palacios E.. Psychosocial support groups for patients with multidrug-resistant tuberculosis: five years of experience. Glob Public Health 2007; 2: 404– 417. [DOI] [PubMed] [Google Scholar]
- 6. World Health Organization. . Global tuberculosis report, 2016. WHO/HTM/TB/2016.13 Geneva, Switzerland: WHO, 2016. http://apps.who.int/iris/bitstream/10665/250441/1/9789241565394-eng.pdf?ua=1/ Accessed August, 2017. [Google Scholar]
- 7. Instituto Nacional de Salud Mental Honorio Delgado. . Estudio epidemiológico de salud mental en Lima Metropolitana y Callao - replicación 2012. Lima, Peru: Instituto Nacional de Salud Mental, 2013. http://www.insm.gob.pe/investigacion/archivos/estudios/2012%20ASM%20-EESM%20-LM.pdf Accessed July 2017. [Spanish] [Google Scholar]
- 8. Vega P, Sweetland A, Acha J, . et al. Psychiatric issues in the management of patients with multidrug-resistant tuberculosis. Int J Tuberc Lung Dis 2004; 8: 749– 759. [PubMed] [Google Scholar]
- 9. World Health Organization. . The WHO End TB Strategy. WHO/HTM/TB/2015.19 Geneva, Switzerland: WHO, 2015. http://www.who.int/tb/post2015_strategy/en/ Accessed August 2017. [Google Scholar]
- 10. Stop TB Partnership. . The ‘Zero TB Initiative’ sparks new action to end TB. Geneva, Switzerland: Stop TB Partnership, 2016. http://www.stoptb.org/news/stories/2016/ns16_034.asp Accessed August 2017. [Google Scholar]


