Abstract
Nasal obstruction is one of the most common complaint that ENT surgeon faces in his day to day practice. Deviated nasal septum is the most common cause for the nasal obstruction. It causes altered airflow dynamics which leads to various histopathological changes in nasal mucosa.Histopathological changes like lymphocytic infiltration and squamous metaplasia were studied and comparison was done between convex and concave side. A prospective randomized study conducted on 42 patients of deviated nasal septum from January 2015 to December 2015 selected from inpatient department of Otorhinolaryngology, KLES Dr. Prabhakar Kore Hospital and Medical Research Center, Belagavi. This study determined significantly higher rate of squamous metaplasia and lymphocytic infiltration in septal mucosa on concave side when compared with convex side. Furthermore, there was increased lymphocytic infiltration and squamous metaplasia in lateral wall mucosa on concave side as compared to convex side but the difference was not statistically different. Deviated nasal septum predisposes the nasal epithelium to chronic inflammation and squamous metaplasia as a result of altered airflow. Due to changes in pathophysiology the patient is more susceptible to chronic rhinitis/rhinosinusitis.
Keywords: Nasal septum, Microscopy, Nasal mucosa, Squamous metaplasia, Chronic inflammation
Introduction
A deviated nasal septum (DNS) is the most common cause of nasal obstruction. It leads to mouth breathing, snoring and external nasal deformity. It also influences the airflow dynamics of the nasal cavity and improper aeration of paranasal sinuses leading to sinusitis. Due to airflow changes, compensatory hypertrophy of the nasal mucosa on concave side is often found [1–4]. Other changes which are seen due to altered air flow dynamics are disturbed mucociliary dysfunction, lymphocytic infiltration and squamous metaplasia. Although these changes are seen on both sides of nasal mucosa, but are more severe on concave side [5–9]. All these changes can be avoided by surgically correcting DNS.
With this background, we carried out a prospective randomised study to determine the influence of DNS on nasal epithelium.
Materials and Methods
This study was approved by the institutional research ethics committee and prior written informed consent was taken from all the patients.
The prospective randomized study was conducted on 42 patients (27 males and 15 females) between 16 and 60 years with symptomatic deviated nasal septum from the inpatient department of Otorhinolaryngology, KLES Dr. Prabhakar Kore Hospital and Medical Research Center, Belagavi.
Inclusion criteria were as follows:
Patients with symptomatic deviated nasal septum
Patients who are willing to undergo septoplasty
Exclusion criteria were as follows:
Patients having upper respiratory tract infection or sinusitis in previous 2 months
Patients clinically diagnosed with allergic rhinitis based on symptoms as skin prick test was not done
Patients with vasomotor rhinitis
Patients with previous history of having undergone endonasal surgery
Patients on medications such as nasal steroids, nasal sprays.
Patients with any other nasal ailments
All the patients fulfilling inclusion criteria were included in the study and mucosal biopsy samples were obtained from the following sites (prior to septoplasty):
Septum at the most deviated point on the convex side
The corresponding area on the concave side
Both inferior turbinates from anterior end
Both middle turbinates from anterior end
These biopsy samples were placed in formaldehyde. After fixing them on paraffin blocks they were cut into 3 µm slices and later stained with hematoxylin–eosin.
The slides were observed under a light microscope at 40× magnification power. The density of lymphocytic infiltration was noted and grading was done as follows:
Grade 0: No lymphocytes
Grade 1: 1–2 lymphocytes in the field
Grade 2: Sparse lymphocytes in all areas
Grade 3: Diffuse and intense lymphocytic infiltration (Fig. 1)
Fig. 1.
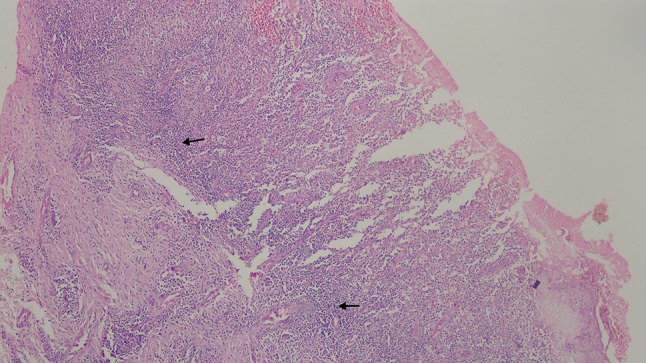
Microscopic picture of nasal mucosa. Epithelium is partly ulcerated, subepithelial tissue shows few mucosal glands and dense lymphocytic infiltration—Grade 3 (arrow)
Presence or absence of squamous metaplasia was also noted (Figs. 2, 3).
Fig. 2.
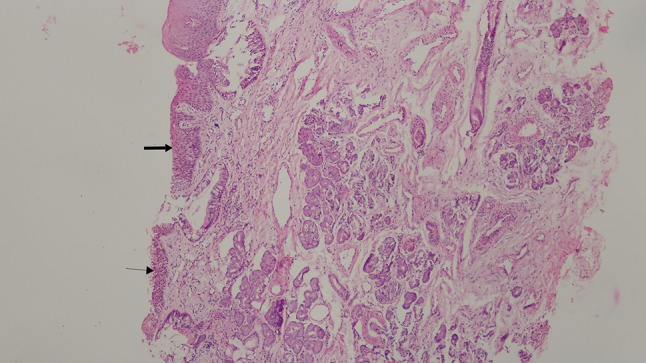
Microscopic picture showing nasal mucosa partly lined by ciliated columnar epithelium (thin arrow) and partly showing squamous metaplasia (thick arrow)
Fig. 3.
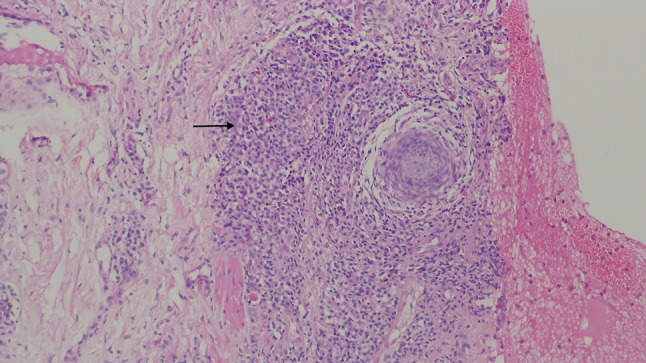
Microscopic picture of nasal mucosa. Epithelium is ulcerated, subepithelial tissue shows lymphocytic infiltration—Grade 2 with granuloma (arrow) (H&E, ×100)
Each case was numbered as Case 1 to Case 42 and blinding was done to prevent observer bias.
Statistical analysis was done using SPSS software version 16 for windows.
Results
All the 42 patients included in this study had septal deviation either on left or right side, i.e. 20 (47.6%) had deviation towards left, 22 (52.4%) patients had deviation towards right and none of the patients appeared with deviation on both sides.
In patients with Left side DNS:
Concave and convex sides showed statistically significant difference in the presence of squamous metaplasia in the septal mucosa with concave side affected more than the convex side (McNemar test, p = 0.004) (Tables 1, 2).
Presence of squamous metaplasia in lateral nasal wall (Inferior turbinate and Middle turbinate) mucosae between concave and convex side wasn’t significantly different (McNemar test, p = 1).
The intensity of lymphocytic infiltration in the septal mucosa on concave side was higher than on the convex side and the difference between the two was statistically significant (McNemar test, p < 0.001) (Tables 3, 4).
The intensity of lymphocytic infiltration in inferior turbinate mucosa on the convex side was not significantly different from that of inferior turbinate mucosa on concave side (McNemar test, p = 0.227).
The intensity of lymphocytic infiltration in middle turbinate mucosa on the convex side was not significantly different from that of middle turbinate mucosa on concave side (McNemar test, p = 0.065).
Table 1.
Finding of squamous metaplasia in nasal mucosa
| Squamous metaplasia | |
|---|---|
| Septal mucosa on convex side | 3 |
| Septal mucosa on concave side | 23 |
| Inferior turbinate mucosa on convex side | 1 |
| Inferior turbinate mucosa on concave side | 8 |
| Middle turbinate mucosa on convex side | 2 |
| Middle turbinate mucosa on concave side | 3 |
Table 2.
Comparison between presence of squamous metaplasia in septal mucosa on the convex side and concave side in patients with left side DNS (McNemar test)
| Left DNS | Septal mucosa on the convex side | ||
|---|---|---|---|
| Normal | Squamous metaplasia | ||
| Septal mucosa on concave side | |||
| Normal | 10 | 0 | |
| Squamous metaplasia | 9 | 1 | p = 0.004 |
| Total (n = 20) | 19 | 1 | |
Table 3.
Finding of lymphocytic infiltration in nasal mucosa
| Lymphocyte infiltration | ||||
|---|---|---|---|---|
| Grade 0 | Grade 1 | Grade 2 | Grade 3 | |
| Septal mucosa on convex side | 7 | 19 | 15 | 1 |
| Septal mucosa on concave side | 0 | 8 | 28 | 6 |
| Inferior turbinate mucosa on convex side | 8 | 19 | 13 | 2 |
| Inferior turbinate mucosa on concave side | 1 | 23 | 14 | 4 |
| Middle turbinate mucosa on convex side | 11 | 15 | 12 | 4 |
| Middle turbinate mucosa on concave side | 3 | 11 | 22 | 6 |
Table 4.
Comparison of intensity of lymphocytic infiltration between septal mucosa on the convex side and concave side in patients with left side DNS (McNemar test)
| Left DNS | Lymphocytic infiltration in septal mucosa on the convex sidea | ||
|---|---|---|---|
| Grade 0, 1 | Grade 2, 3 | ||
| Lymphocytic infiltration in septal mucosa on concave sidea | |||
| Grade 0, 1 | 4 | 0 | |
| Grade 2, 3 | 13 | 3 | p < 0.001 |
| Total (n = 20) | 17 | 3 | |
aThe statistical analysis was done by combining Grade 0 with Grade 1 and Grade 2 with Grade 3 as the numbers in cells were few
In patients with Right side DNS:
The presence of squamous metaplasia in the septal mucosa on concave side was higher than the convex side and the difference between the two was statistically significant (McNemar test, p = 0.001) (Table 5).
Squamous metaplasia in lateral nasal wall (Inferior turbinate and middle turbinate) mucosae on convex side was not significantly different from that on concave side (McNemar test, p = 1).
The intensity of lymphocytic infiltration in septal mucosa on the convex side was not significantly different from that of the septal mucosa on concave side (McNemar test, p = 0.227).
The intensity of lymphocytic infiltration in inferior turbinate mucosa on the convex side was not significantly different from that of inferior turbinate mucosa on concave side (McNemar test, p = 0.727).
The intensity of lymphocytic infiltration in middle turbinate mucosa on the convex side was not significantly different from that of middle turbinate mucosa on concave side (McNemar test, p = 0.180).
Table 5.
Comparison between presence of squamous metaplasia in septal mucosa on the convex side and concave side in patients with right side DNS (McNemar test)
| Right DNS | Septal mucosa on convex side | ||
|---|---|---|---|
| Normal | Squamous metaplasia | ||
| Septal mucosa on the concave side | |||
| Normal | 9 | 0 | |
| Squamous metaplasia | 11 | 2 | p = 0.001 |
| Total (n = 22) | 20 | 2 | |
Discussion
Septal deviation can cause symptoms such as nasal obstruction, mouth breathing with variable symptoms such as headache and olfactory disorders. Dynamic air flow in the nasal cavity is affected by the degree, localization and shape of deviation of the nasal septum.
The amount of, and resistance to, air flow in the nasal cavity of a patient with nasal septal deviation are different [10]. This leads to compensatory hypertrophy of the nasal mucosa on the concave side [1, 11]. Septal deviations play an important role in the aetiology of diseases of paranasal sinuses as incidences of sinusitis, osteomeatal complex obstruction and mucociliary dysfunction also increases [12–15].
In the present study, presence of squamous metaplasia was significantly higher in septal mucosa on concave side as compared to the convex side in both left and right sided DNS patients. Similar finding was seen in another study but the difference between convex and concave side was not statistically significant [9].
The presence of squamous metaplasia in lateral nasal wall (inferior and middle turbinate) mucosa on the convex side was not significantly different from the concave side. Similar result was seen in another study conducted by Kamani et al. [9].
In the present study, intensity of lymphocytic infiltration in patients with left sided DNS was more in the septal mucosa on the concave side and the difference was statistically significant. Whereas in patients with right side DNS lymphocytic infiltration was more in the septal mucosa on the concave side but the difference was not statistically significant. The exact mechanism for this for this occurrence is not understood, but it may be that a spontaneous inflammatory process not related to allergy or infection may be brought about in the more open nasal cavity by increased air flow.
In a similar study by Jang et al. [8] higher number of infiltrating inflammatory cells were seen in the concave side septal mucosa as compared to the convex side of septal mucosa and the difference was statistically significant. However, they obtained specimen 2 cm posterior to nostril and 1.5 cm inferior to nasal dorsum; in the present study specimen was taken from the most convex part of septum and its opposite side. Therefore, our specimen may more markedly show the effect of septal deviation on histopathology, compared to theirs.
In another study by Kamani et al. [9], they compared both sides of deviated septal mucosa in terms of lymphocytic infiltration and found increased lymphocytic infiltration in septal mucosa on concave side but this difference was not statistically significant. Similarly, Mariappan et al. [5] found more prominent infiltration of inflammatory cells in the concave side septal mucosa as compared to the convex side but was not statistically significant.
The intensity of lymphocytic infiltration in lateral nasal wall (inferior and middle turbinate) mucosa was higher on the concave side as compared to the convex side but the difference between the two was not statistically significant. Similar result was seen in another study conducted by Kamani et al. [9].
This study has its own limitation as this is not a case control study hence, further studies are required with larger sample size for better understanding of this entity.
Conclusion
The results of our study suggest that nasal septal deviation leads to histopathological changes in nasal mucosa in the form of lymphocytic infiltration and squamous metaplasia. These changes influence both sides of the nasal mucosa but have been found to be more severe on the concave sideas compared to convex side. Deviated nasal septum predisposes the nasal mucosa to chronic inflammation and squamous metaplasia, both of these changes may predispose a patient to increased incidence of chronic rhinitis/rhinosinusitis.
Funding
This study was not funded by any agency or body.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research ethics committee.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Illum P. Septoplasty and compensatory inferior turbinate hypertrophy: long-term results after randomized turbinoplasty. Eur Arch Otorhinolaryngol. 1997;254(Suppl. 1):89–92. doi: 10.1007/BF02439733. [DOI] [PubMed] [Google Scholar]
- 2.Berger G, Hammel I, Berger R, Avraham S, Ophir D. Histopathology of the inferior turbinate with compensatory hypertrophy in patients with deviated nasal septum. Laryngoscope. 2000;110:2100–2105. doi: 10.1097/00005537-200012000-00024. [DOI] [PubMed] [Google Scholar]
- 3.Berger G, Gass S, Ophir D. The histopathology of the hypertrophic inferior turbinate. Arch Otolaryngol Head Neck Surg. 2006;132:588–594. doi: 10.1001/archotol.132.6.588. [DOI] [PubMed] [Google Scholar]
- 4.Kang JW, Yoo JB, Kim CH, Lee JG. Structural changes of inferior turbinate in patients with septal deviation: surgical implication. J Rhinol. 2004;11:40–43. [Google Scholar]
- 5.Mariappan RG, Dhanalakshmi M, Mathaikutty DM, Shanmugam R, Shanmugam VU, Swaminathan B, et al. Clinico-pathological correlation and the effect of septal surgery on nasal mucociliary clearance. Sch J App Med Sci. 2014;2:1691–1695. [Google Scholar]
- 6.Yigit O, Akgul G, Alkan S, Uslu B, Dadas B. Changes occurring in the nasal mucociliary transport in patients with one-sided septum deviation. Rhinology. 2005;43:257–260. [PubMed] [Google Scholar]
- 7.Inagi K. Histological study of mucous membranes in the human nasal septum. Nippon JibiinkokaGakkaiKaiho. 1992;95:1174–1189. [PubMed] [Google Scholar]
- 8.Jang YJ, Myong NH, Park KH, Koo TW, Kim HG. Mucociliary transport and histologic characteristics of the mucosa of deviated nasal septum. Arch Otolaryngol Head Neck Surg. 2002;128:421–424. doi: 10.1001/archotol.128.4.421. [DOI] [PubMed] [Google Scholar]
- 9.Kamani T, Yilmaz T, Surucu S, Bajin MD, Gunaydin RO, Kuscu O. Histopathological changes in nasal mucosa with nasal septum deviation. Eur Arch Otorhinolaryngol. 2014;271:2969–2974. doi: 10.1007/s00405-014-2990-x. [DOI] [PubMed] [Google Scholar]
- 10.Cole P, Chavan R, Naito K, Oprysk D. The obstructive nasal septum: effect of stimulated deviations on nasal air flow. Arch Otolaryngol Head Neck Surg. 1988;114:410–412. doi: 10.1001/archotol.1988.01860160054020. [DOI] [PubMed] [Google Scholar]
- 11.Grymer LF, Illum P, Hilberg O. Septoplasty and inferior tubinate hypertrophy: a randomized study evaluated by acoustic rhinometry. J Laryngol Otol. 1993;107:413–417. doi: 10.1017/S0022215100123308. [DOI] [PubMed] [Google Scholar]
- 12.Ginzel A, Illum P. Nasal mucociliary clearance in patients with septal deviations. Rhinology. 1980;18(4):177–181. [PubMed] [Google Scholar]
- 13.Elahi MM, Frenkiel S, Fageeh N. Paranasal structural changes and chronic sinus disease in relation to the deviated septum. J Otolaryngol. 1997;26:236–240. [PubMed] [Google Scholar]
- 14.Tao Z, Zhong J, Yang Q. Differences of anatomic variations in osteomeatal complex between two sides of the deviated septum. Zhongua er Bi yan hou Ke Za Zhi. 2001;36(2):132–134. [PubMed] [Google Scholar]
- 15.Passali D, Ferri R, Becchini G, Passali GC, Bellusi L. Alternations of nasal mucociliary transport in patients with hypertrophy of the inferior turbinate, deviations of the nasal septum and chronic sinusitis. Eur Arch Otorhinolaryngol. 1999;256:335–337. doi: 10.1007/s004050050158. [DOI] [PubMed] [Google Scholar]


