Abstract
Currently, 1% of the United States population holds a diagnosis for celiac disease (CD), however, a more recently recognized and possibly related condition, “non-celiac gluten sensitivity” (NCGS) has been suggested to affect up to 6% of the United States public. While reliable clinical tests for CD exist, diagnosing individuals affected by NCGS is still complicated by the lack of reliable biomarkers and reliance upon a broad set of intestinal and extra intestinal symptoms possibly provoked by gluten. NCGS has been proposed to exhibit an innate immune response activated by gluten and several other wheat proteins. At present, an enormous food industry has developed to supply gluten-free products (GFP) with GFP sales in 2014 approaching $1 billion, with estimations projecting sales to reach $2 billion in the year 2020. The enormous demand for GFP also reflects a popular misconception among consumers that gluten avoidance is part of a healthy lifestyle choice. Features of NCGS and other gluten related disorders (e.g., irritable bowel syndrome) call for a review of current distinctive diagnostic criteria that distinguish each, and identification of biomarkers selective or specific for NCGS. The aim of this paper is to review our current understanding of NCGS, highlighting the remaining challenges and questions which may improve its diagnosis and treatment.
Keywords: Non-celiac gluten sensitivity, Celiac disease, Gluten, Wheat, Gluten related disorder, Gluten free diet
Core tip: Non-celiac gluten sensitivity, a less known clinical entity has been estimated to have a prevalence of up to 6% in the United States. This review identifies the pathophysiology of the disease delineating clearly the important components of wheat which play a role in its innate immune response. The updated guidelines on the diagnosis of this disease is discussed here with a bridge to other management strategies apart from the gluten free diet that are now being investigated.
INTRODUCTION
In the past decade, the consumption of gluten free food has become increasingly popular in the Western world. A Gallup poll conducted in July 2015 showed that 20% of Americans opt for a gluten free diet (GFD) while 17% say they avoid gluten free foods[1]. Estimates by the nutrition industry indicate that sales of gluten-free products (GFPs) had a compound annual growth rate of 34% over the five year period ending in 2014, with annual sales totaling close to $1 billion[2]. Current market projections predict sales will again soar to approach $2 billion in the year 2020[3]. Market research by the Mintel group gives a liberal estimation of the sales of products in the gluten-free industry to be $11.6 billion in the year ending 2015, an estimated 136% increase from 2013[4]. The significant increase in the retail sales of GFPs is alarming. However, currently only approxiately 1% of the United States population is diagnosed with celiac disease[5]. Despite this, gluten-free food consumption is clearly on an exponential rise. This enormous allocation of resources reflects self-diagnosis for gluten sensitivity and may reflect an additional condition described as non-celiac gluten sensitivity (NCGS).
The first comprehensively documented case of “gluten sensitivity” (in a non-celiac disease/wheat allergy patient) was reported in 1980[6]. That report described eight adult women suffering from incapacitating abdominal pain and chronic diarrhea which rapidly remitted when a gluten-free diet was initiated, with symptomatic relapse after re-exposure to a gluten containing diet (GCD). Jejunal biopsies performed on these patients, however, failed to identify CD-like histopathology, leading to a consensus description of these patients as having “gluten-sensitive diarrhea without evidence of celiac disease”. This was the beginning of the current era of what we now consider NCGS. Since then, many subsequent studies have attempted more extensive descriptions of NCGS to create effective diagnostic criteria and management strategies.
In 2011, an international consensus on NCGS reached an agreement on the definition of NCGS, defining it as a “non-allergic and non-autoimmune condition in which the consumption of gluten can lead to symptoms similar to those seen in CD.” NCGS is defined as gluten sensitivity because symptoms are relieved by gluten withdrawal, and re-appear upon introduction to gluten[7]. At least part of the difficulty in handling NCGS patients is that essentially, it is often a diagnosis by exclusion. First, CD and WA need to be excluded as possible diagnoses. Beyond this, NCGS often carries an extensive and relatively broad set of symptoms which affects diverse organ systems[8]. Symptoms of NCGS could be very disabling presenting as gastrointestinal and/or extra-intestinal symptoms[9]. The onset of NCGS symptoms after gluten consumption can also range widely, appearing hours to even days following exposure to a GCD; the timing of resolution in NCGS symptoms may also vary widely.
Given that NCGS presentation could resemble CD or WA, further research into highlighting their hallmark findings is necessary. It is essential now that individuals with gluten-related disorders are identified accurately and managed appropriately. This is important in order to curtail the significant rise in the retail sales of GFPs in the food industry as millions of dollars could be salvaged given the appropriate diagnosis amongst other important reasons. This current review discusses our present understanding of NCGS, its differences and similarities to CD and other gluten-related disorders, etiopathogenesis and management strategies. It is important to recognize that NCGS is a distinct disorder from CD and it is imperative that it is accurately distinguished.
EPIDEMIOLOGY
Despite becoming a more common diagnosis, there is currently a paucity of information on NCGS especially regarding its actual prevalence in the general population. This lack of information reflects the decision of many patients to start GFD after self-diagnosis without any formal clinical testing or management recommendation by their physician. As a result of this ambiguity, the prevalence of NCGS has been reported to vary enormously from 0.6%-6% in Western populations[10-12]. It is unclear how much of the rise in consumption of gluten free foods actually reflect a higher prevalence of NCGS in the population or the choice to adhere to a GFD based on patient’s preferences.
Despite the lack of accurate epidemiologic measurements of the actual US prevalence of NCGS, data in 2009-2010 from the National Health and Nutrition Examination Survey (NHANES) showed that of the 7762 NHANES participants who were free of celiac disease, 49 individuals reported a strict adherence to a GFD. This reflects a weighted prevalence of NCGS of only 0.55%[11]. Another more recent evaluation of the NHANES participants from 2009-2012 separated patients into those with CD and those without CD consuming a GFD. This study estimated a prevalence of NCGS of 0.8% in patients without CD who were consuming a GFD[10]. The prevalence in these NHANES studies were estimated based on the assessment that the individuals without CD avoiding gluten fall under the classification of NCGS.
During the period 2004 and 2010, 5896 patients were seen at the Center for Celiac Research at the University of Maryland. Of these, 347 participants met the criteria for diagnosis of “Gluten Sensitivity” reflecting about 6% of the patients seen[12]. These gluten triggered symptoms included abdominal pain (68%), eczema and/or rash (40%); headache (35%); “foggy mind” or difficulty focusing (34%); fatigue (33%); diarrhea (33%); depression (22%); anemia (20%); numbness in the legs, arms or fingers (20%); and joint pain (11%)[12]. The proportion of patients with NCGS in this study extrapolated to the general population estimated an enormous prevalence of NCGS compared with that previously seen in prior studies. Based on our review, the estimation of the prevalence of NCGS ranges widely from 0.6% to 6%, a ten-fold difference. As identified, the prevalence of NCGS in the general population may exceed that of CD - now estimated at 1%[5]. However this appears to be a high estimate based solely on symptomatology.
As NCGS is a relatively “new” entity compared to CD, it is also unclear whether or to what extent genetic or environmental risks might predispose individuals to this disorder. Studies have suggested gender contributions with the female to male prevalence ratio between 3:1[13,14] to 5.4:1[15], indicating a female predominance in NCGS. This may however reflect the observation that female patients are more prone to reporting gluten-related symptoms thus leading to referrals for further work-up as seen in a United Kingdom study in 2014[16]. There has also been a heightened interest in the association of NCGS with other medical conditions. An overlap between irritable bowel syndrome (IBS) and NCGS has been suggested since most of the gastrointestinal symptoms in NCGS resemble IBS (similar Rome III criteria), including abdominal pain/discomfort, bloating, diarrhea and constipation[15]. There is also a debate as to whether a GFD can help symptom resolution in IBS after excluding CD, as clinical trials have shown that GFD can reduce symptoms in patients with diarrhea-predominant IBS (IBS-D)[17]. Although recent research has suggested that a low fermentable oligo-, di-, mono-saccharides and polyols (FODMAPs) diet, regardless of gluten content, improves symptoms in IBS[18]. Given the close symptomatic resemblance between NCGS and IBS, prevalence estimates may be unclear as patients with NCGS could be mislabeled as IBS.
PATHOGENESIS
The pathobiology of NCGS is poorly understood, hotly debated and under intense research (Figure 1). NCGS potentially involves many triggers as are seen in CD and IBS. The initiating event in NCGS mainly involves exposure of gut epithelium to gluten containing foods leading to immune-mediated and/or non-immune mediated responses. Whereas CD shows increased gut permeability, NCGS shows a decreased gut solute permeability with increased epithelial barrier and elevated expression of the tight junctional component claudin-4[19-21]. Due to the lack of evidence for T-cell involvement and the apparent contribution from toll-like receptors (e.g., TLR-2, TLR-1)[21], NCGS may be more of an innate rather than adaptive immune response. Since specific triggers are not clear in NCGS, this could make NCGS a relatively different pathobiological entity from other gluten related conditions like CD and WA[20,22]. Changes in the gut microbiome (dysbiosis) produced by gluten consumption[23] may also influence NCGS. This predominantly innate TLR based systemic response potentially incited by changes in microbiota was further supported by the increased levels of LBP (lipopolysaccharide binding protein) and soluble CD14 proteins[24]. Additionally there is evidence for NCGS developing in individuals with some genetic predispositions (e.g., HLA-DR4, HLA-DR2)[21], which is higher than general population but lower than patients with CD who have a strong genetic component. However, currently this association does not appear to be as clear[21,22].
Figure 1.
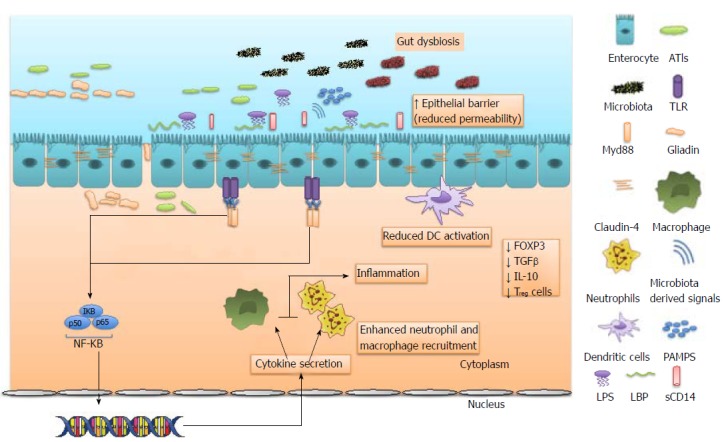
Toll like receptors act as primary sensors to gliadin and non-gluten proteins like alpha amylase/trypsin inhibitors, and microbiota derived signals in non-celiac gluten sensitivity. Dysregulated microbiota also release lipopolysaccharide (LPS) in circulation which result in production of LPS-binding protein (LBP) from gastrointestinal and hepatic epithelial cells and soluble CD14 (sCD14) from monocytes/macrophages. This leads to activation of transcription factor nuclear factor-kappaB (NF-κB), which controls the expression of an array of inflammatory cytokine genes resulting in recruitment of neutrophils and macrophages. In contrast to CD, there is limited dendritic cell activation, resulting in reduced expression of Treg cells, reduced FOXP3, TGFβ, IL-10. All these factors with increased expression of claudin-4 culminate in reduced intestinal permeability and increased epithelial barrier. Gut dysbiosis can also promote inflammation through expansion of pro-inflammatory pathobionts. TLRs: Toll like receptors.
Gluten, the main inciting agent in CD also has a significant role in NCGS pathology[25]. In addition to gluten, several other food-derived stimuli have been shown to also be important in the etiopathogenesis of NCGS include alpha amylase/trypsin inhibitors (ATIs)[26], FODMAPS[18] and other short chain fructans. Gliadin is the alcohol soluble fraction of gluten, and contains the bulk of the “immunogenic” components[27]. Gliadin has the ability to promote an inflammatory response primarily in the upper gastrointestinal tract. Gliadin has shown to trigger both innate and adaptive response via recruitment of CD4+ T cells and increasing expression of interleukin-15 by enterocytes[28]. The effects of gliadin-induced enteric responses are not however completely seen in NCGS with innate immune response apparently playing a bigger role than adaptive response[21,29]. The heterogeneous behavior of NCGS in comparison to CD can be explained by different motifs of gliadin protein exerting different responses with alpha gliadin peptides having a significant role in innate adaptive response, and probably expressed more in NCGS individuals[30]. NCGS individuals also have increased levels of TLR2 and to a lesser extent TLR1 expression, increased number of α and β intraepithelial lymphocytes, and reduced number of T-regulatory cells[21]. Solute barrier function remains largely unchanged in NCGS, which is consistent with fairly normal adaptive immune response, normal intestinal permeability and expression of tight junction proteins[14,21]. Gluten’s opioid like effect on the intestinal transit time and nocebo effect has also been studied and may have an important role on the overall pathology and clinical presentation of the disease[31].
In the recent years, other non-gluten components of wheat have also been shown to play a major role. ATIs in particular, have been implicated in NCGS pathology. The role of ATIs in mounting an immunological response has been shown in animal and human research models and is believed to be an important oral antigen both in CD as well as in NCGS[26]. This predominantly innate immune response involves macrophages, neutrophils and intestinal dendritic cells via activation of the toll like receptor complexes[21,26]. Their less tendency to affect the overall gut morphology falls well in line with NCGS pathology.
The gut microbiota has been shown to play a significant role in the pathogenesis of CD, in which gut dysbiosis precedes the activation of inflammatory and immune mediated pathways[32]. The role of gut dysbiosis has also recently been emphasized in NCGS pathobiology and might help to explain both intestinal and non-intestinal manifestations in the disease by upregulating gut and systemic inflammation[33].
CLINICAL PRESENTATION
The symptoms of NCGS can occur within hours to days following exposure to gluten-containing diet and can then dissipate upon withdrawal of gluten. Most of the presentation resembles CD, the main similarities and differences are presented in Table 1. Frequent symptoms reported in NCGS include bloating (87%), abdominal pain (83%), epigastric pain (52%), diarrhea (50%), and constipation (24%)[8]. Extra-intestinal manifestations are also reported which include; lack of well-being (68%), tiredness (64%), headache (54%), anxiety (39%), “foggy mind” or difficulty focusing (38%)[8].
Table 1.
| NCGS | CD | IBS | WA | |
| Colonic manifestations | Diarrhea | Diarrhea | Diarrhea | Diarrhea |
| Abdominal pain | Abdominal pain | Abdominal pain | Abdominal pain | |
| Bloating | Bloating | Bloating | Bloating | |
| Constipation | Constipation | Constipation | Constipation | |
| Nausea | Nausea | Mucous Discharge | Nausea | |
| Vomiting | Vomiting | Dyspepsia | Vomiting | |
| Early satiety | ||||
| Extra-colonic manifestations | Headache | Anemia | Major depression | Hives |
| Migraine | Osteoporosis | Anxiety | Angioedema | |
| Foggy mind | Neurological disturbances | Somatoform disorder | Asthma | |
| Fatigue | Pubertal delay | Fibromyalgia | Cough | |
| Eczema like rash | Dermatitis herpetiformis | Temporomandibular disorder | Post Nasal Drip | |
| Myositis | Foggy mind | Dyspareunia | Eczema | |
| Numbness | Lymphoma | |||
| Psychological changes | ||||
| Symptom Onset | Hours to Days | Hours to months | Unclear relation to gluten ingestion | Minutes to Hours |
| Cytomorphology | Small bowel intraepithelial lymphocytosis (Marsh 0-1) | Villous atrophy with crypt hyperplasia | Normal | Normal |
| Biomarkers | IgG-AGA | IL-17(A) | TNF- α | IgE antibodies to wheat protein |
| Zonulin | TCR-γδ IELs | IL-6 | ||
| LBP | IgA tTGA | IL-8 | ||
| sCD14 | IgA EMA | |||
| CD3 + IELS | ||||
| Zonulin | ||||
| Immunophenotype | HLA- DQ2 and DQ8 genotypes in 50% patients | HLA- DQ2 and DQ8 genotypes in 80% patients | Increase in: | Transforming growth factor-b (TGFb) mutations have been associated with higher rates of allergic disease |
| B cells expressing IgG or co-stimulatory molecules CD80 or CD86 | ||||
| T cells expressing b7 + HLADR+ and CD69+ | ||||
| Diagnosis | See figure 2 | 1Serologic testing followed by small bowel biopsy | Rome III diagnostic criteria | Skin prick test |
| Presence of serum IGE antibodies to wheat protein | ||||
| Management | GFD | GFD | Symptomatic treatment and elimination of stressors | GFD |
| Probiotics | Subcutaneous epinephrine for any acute episodes | |||
| AN-PEP | ||||
| ICD codes | K90.41 | K90.0 | K58 | K52.29 |
4 out of 5 of the following: Typical symptoms of CD, Serum CD IgA class auto antibodies at high titer, HLA-DQ2 and/or HLA-DQ8 genotypes, Celiac enteropathy found on small bowel biopsy, Response to a GFD(14).
Some of the other less commonly reported symptoms include weight loss, depression and skin rash[8]. Unlike CD, nutrient deficiencies such as iron, vitamin D and vitamin B 12 deficiencies are not significantly seen in NCGS[34]. NCGS also has a lesser association with autoimmune disorders when compared with CD[14,35].
DIAGNOSIS
NCGS should be considered in patients with the history and physical examination indicative of a gluten related disorder. The clinical presentation of NCGS, as outlined earlier, should include the remission of symptoms upon withdrawal of gluten. The proposed diagnostic work-up includes 3 vital steps.
The 1st step in an NCGS diagnosis is the exclusion of CD and WA. The patient needs to be on a GCD for a period of 6-wk. Several tests should be performed during this period to exclude WA; wheat specific IgE and skin prick test, and CD; IgA-tTG, IgG-DGP and IgA-EMA. If highly suspicious of CD, the physician can proceed with upper endoscopy for duodenal biopsy, although this should not be routine testing for every patient. If the biopsy results indicate less CD probability (Marsh 0-1) then the clinician can proceed to the next step[5]. Of note, these tests can be tailored by the clinician based on the patients’ presenting symptoms. The physician can bypass testing of CD or WA and proceed with the work-up for NCGS if patients’ history and physical is not suggestive of the condition.
The 2nd step consists of starting the patient on a GFD for a period of at least 6 wk and monitoring for symptom response. This symptom response is evaluated using the gastrointestinal symptom rating scale (GSRS) and a numerical rating scale (NRS). GSRS is used to identify the symptoms while the NRS is used to quantify the symptoms, weekly from week 0 (baseline) till week 6[36]. A symptomatic response to the GFD is defined as a decrease in 30% of the baseline score with no worsening of other symptoms in at least 50% of the observation time (3 wk)[36]. If the patient fails to show an improvement in symptoms in 6 wk upon resumption of GFD, the diagnosis of NCGS is ruled out and other diagnoses such as IBS and other functional bowel disorders need to be explored.
The 3rd step required to confirm the diagnosis of NCGS in patients who respond to treatment with the GFD involves the re-introduction of the GCD. This is performed because a potential nocebo effect (test subjects believe there is a side effect and they experience them as a result of this) secondary to the exposure to gluten in step 1 cannot be ruled out[37]. In this step, the patient is randomly assigned into test group x or y. The patient is exposed to either GFD + placebo (x) or GFD + gluten (y) for a week. A 1-week washout period of strict GFD is observed, followed by the crossover to GFD + gluten (x) or GFD + placebo (y)[36]. A variation of a 30% symptomatic improvement on introduction of the diet free from gluten in test group y or a variation of 30% symptomatic appearance on introduction of the GCD in test group x (assessed by the modified GSRS and NRS scales) indicates a positive result. Below this 30% value is considered a negative result[36]. This 30% mark is not a scientific estimate but is rather a fair estimate of an appropriate response[36]. This threshold although used in the Salerno experts’ criteria needs scientific validation.
In step 3, the placebo added should be gluten-free and must look very similar to the gluten content so that both the clinician and the patient are unaware of the difference between the gluten and the placebo. The dose of gluten to be used for the challenge should be close to the average daily intake of gluten (10-15 g)[38]. The dose should also be easy to mix with the gluten carrying package. The package carrying gluten can be in any form; bread, muffin. This package should also consist of ATIs as well. The suggested prepared package should contain 10-15 g of gluten and at least 0.3 g of ATIs. The package must also be free of FODMAPs[36]. The proposed diagnostic algorithm for NCGS is shown in (Figure 2).
Figure 2.
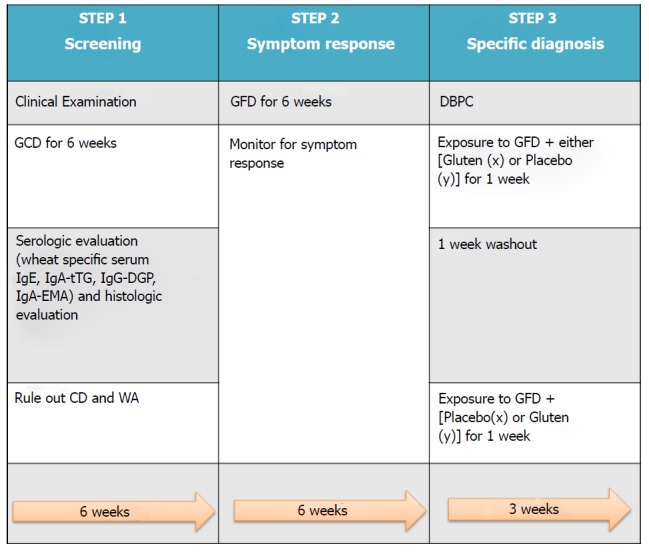
Proposed diagnostic algorithm for non-celiac gluten sensitivity. GCD: Gluten containing diet; GFD: Gluten free diet; CD: Celiac disease.
MANAGEMENT
Currently, the management of NCGS involves a multi-disciplinary approach. The patient is started on a GFD with the help of a registered dietician[14]. A gluten free diet usually helps resolve the intestinal and extra-intestinal symptoms of NCGS. The recommendation is to continue adherence to GFD for lifetime. There have been few if any studies showing whether or not reintroduction of gluten into the diet after a prolonged period of being asymptomatic will cause reversion into previous symptoms[39].
The importance of gluten has been outlined in recent research. Gluten consumption has been associated with a decreased risk of developing type 2 diabetes Mellitus and also a decreased risk of coronary heart disease[40,41]. Understanding these benefits of gluten beyond nutrition reflects the need for caution in the use of GFDs in patients without a proven diagnosis of NCGS. Although GFD seems to be the most important management strategy, it should be suggested only after careful examination and a definite diagnosis of NCGS.
Several ongoing clinical trials are now examining other possible treatment methods for NCGS besides the GFD. One study looks at the use of probiotics for alleviation of NCGS symptoms while maintaining a gluten free diet with introduction of gluten in a controlled environment. This randomized DBPC study evaluates NCGS patients’ response to a gluten source (two slices of bread each day for 7 d) whilst getting probiotics (Bifidobacterium longum ES1 - a patented probiotic bacterial strain) or a placebo during that time[42]. Theoretically the use of probiotics could result in resolving gut dysbiosis by reintroducing gut flora, with reduction in both gut and systemic inflammation but this needs to be clinically examined. Probiotic use has long been a source of debate amongst the medical community regarding its exact role as far as therapeutic option, it’s essential to see if it can be proven to have an ultimate benefit.
Another treatment option under investigation is the use of the enzyme Aspergillus niger prolyl endoprotease (AN-PEP). It has been reported in previous studies that the AN-PEP enzyme significantly enhanced gluten digestion in the stomach of healthy volunteers[43]. A randomized placebo controlled clinical trial is ongoing looking at the effect of AN-PEP on gluten degradation in our target population; gluten sensitive individuals[44]. If we can apply AN-PEP as a means of degrading gluten before it can affect the human gut, it would achieve a major goal as patients can enjoy foods without worrying about diet restriction, worrisome symptoms or soaring food costs.
The use of ancient diploid wheat species (e.g., Triticum monococcum ssp.) as compared with common wheat as a new treatment strategy is gaining ground[45]. Gianfrani et al[45]. demonstrated the low toxicity of these wheat proteins in celiac disease patients following in vitro gastrointestinal digestion. Newer studies have shown the distinction between these older wheat variants and modern wheat[46]. Older wheat variants were shown to have lower bioactivity and a lower concentration of ATIs in comparison with modern wheat[46]. Mechanistically, the modern wheats were observed to have high levels of TLR-4-activating ATIs which are highly resistant to intestinal proteolysis[46]. The application of these studies to favor the use of ancient wheat variants in the NCGS population would be a major step in the advancement of treatment strategies in this disease.
Mayer and Tillisch highlighted the role of the brain-gut axis in abdominal pain syndromes[47]. Recent literature has attempted to further describe how various clinical manifestations seen in IBS and also syndromes like NCGS could be viewed as a dysregulation in the signaling pathway that involves the gut, the enteric nervous system and the central nervous system[33,47,48]. Newer therapeutic options currently being hypothesized in NCGS include the use of vagus nerve stimulation and corticotropin releasing factor (CRF) antagonists to normalize any possible gut brain dysregulation[33,48]. The use of vagus nerve stimulation is based on its positive effects on many inflammatory diseases of vagus-innervated organs (including the GI tract) which thus suggest a case for its application in NCGS[33]. The use of CRF antagonists (seen to induce significant signal reductions in emotional control centers of the brain[23]) is based on the theory that NCGS often has a chronic anxiety or stress related component associated with the anticipation of abdominal pain. Consequently controlling the emotional impact of NCGS may improve its symptoms. The several on-going studies/theories in this area hopefully can shed light on the neuropsychiatric therapeutic components of NCGS.
With the release of the updated ICD 10 coding system, NCGS, along with WA, IBS and CD each have their own codes despite lingering ambiguities about NCGS diagnosis/management. NCGS’s code is K90.41 and it falls under the categories “enteropathy” (code K63.9) and gluten sensitivity (Code K90.41). Although treatment strategies in NCGS are still evolving, it is important to note that NCGS is a specific and billable diagnosis for reimbursement purposes[49].
CONCLUSION
A recent study involving gastroenterologists showed that although most of these specialist physicians were able to “identify” NCGS and prescribe GFD for its treatment, 44% of them were unable to define or agree on a uniform definition[50]. This highlights the difficulty in making the diagnosis of NCGS based on a specific clinical criterion. NCGS warrants further investigation and updated diagnostic and therapeutic strategies.
As we currently stand, the NCGS diagnostic process is arduous for the patient, requiring them to be on a GCD diet through several parts of the process. This could cause distress by eliciting unpleasant symptoms. Thus, an alternative diagnostic approach without subjecting the patient to the stressor would be a significant clinical advancement. Some biomarkers identified to aid in the diagnosis of NCGS are IgG-AGA[15] and Zonulin[51]. However these markers are evidently increased in CD as well[15,51]. Establishing NCGS specific biomarkers is imminent to also monitor for both the resolution of the disease and compliance of the patient to the GFD. Whether NCGS is a transient disease or a chronic disease warranting lifetime diet restriction still needs to be investigated.
The lack of information with regards to the prevalence of NCGS in the developing world is outstanding. Most of the studies being done on this condition are focused on the population, which includes the affluent communities of Europe and North America. Adhering to the GFD is expensive and not easily affordable, the likelihood of a low-income patient self-diagnosing as NCGS and going on a GFD is very minimal. This warrants the question as to if NCGS is really a condition more prevalent in the affluent as they are much more conscious of their diet intake as well as informed.
New and evolving science around gluten related disorders has led to better understanding of the disease process, making it easier for the clinicians to set specific management guidelines. Prospective clinical trials in a diverse population is warranted to better investigate the etiology and progression of this disease. There is still a role of further research to better understand NCGS as a medical condition.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: The authors declare no conflict of interest for this article.
Peer-review started: June 7, 2017
First decision: July 27, 2017
Article in press: September 5, 2017
P- Reviewer: Christodoulou DK, Pan W, Saniabadi AR, Sivandzadeh GR, Garcia-Olmo D S- Editor: Ma YJ L- Editor: A
E- Editor: Ma YJ
Contributor Information
Samuel O Igbinedion, Department of Internal Medicine, Louisiana State University Health Sciences Center, Shreveport, LA 71103, United States.
Junaid Ansari, Department of Molecular and Cellular Physiology, Louisiana State University, School of Medicine, Shreveport, LA 71103, United States.
Anush Vasikaran, Department of Internal Medicine, Louisiana State University Health Sciences Center, Shreveport, LA 71103, United States.
Felicity N Gavins, Department of Molecular and Cellular Physiology, Louisiana State University, School of Medicine, Shreveport, LA 71103, United States.
Paul Jordan, Department of Gastroenterology and Hepatology, Louisiana State University Health Sciences Center, Shreveport, LA 71103, United States.
Moheb Boktor, Department of Gastroenterology and Hepatology, Louisiana State University Health Sciences Center, Shreveport, LA 71103, United States.
Jonathan S Alexander, Department of Molecular and Cellular Physiology, Louisiana State University, School of Medicine, Shreveport, LA 71103, United States. jalexa@lsuhsc.edu.
References
- 1.Riffkin R. One in Five Americans Include Gluten-Free Foods in Diet. 2017. Available from: https://prezi.com/fuws7phgltkb/one-in-five-americans-include-gluten-free-foods-in-diet/ [Google Scholar]
- 2.3rd Edition: Market Research Report. Packaged Facts. 2011. Available from: http://https://www.researchandmarkets.com/reports/2860404/gluten-free-foods-and-beverages-in-the-u-s-3rd.pdf.
- 3. Available from: https://www.reportlinker.com/p02051931/Food-Formulation-Trends-Ingredients-Consumers-Avoid.html.
- 4.Half of Americans think gluten-free diets are a fad while 25% eat gluten-free foods Mintel com. 2017. Available from: http://www.mintel.com/press-centre/food-and-drink/half-of-americans-think-gluten-free-diets-are-a-fad-while-25-eat-gluten-free-foods.
- 5.Gujral N, Freeman HJ, Thomson AB. Celiac disease: prevalence, diagnosis, pathogenesis and treatment. World J Gastroenterol. 2012;18:6036–6059. doi: 10.3748/wjg.v18.i42.6036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cooper BT, Holmes GK, Ferguson R, Thompson RA, Allan RN, Cooke WT. Gluten-sensitive diarrhea without evidence of celiac disease. Gastroenterology. 1980;79:801–806. [PubMed] [Google Scholar]
- 7.Volta U, Tovoli F, Cicola R, Parisi C, Fabbri A, Piscaglia M, Fiorini E, Caio G. Serological tests in gluten sensitivity (nonceliac gluten intolerance) J Clin Gastroenterol. 2012;46:680–685. doi: 10.1097/MCG.0b013e3182372541. [DOI] [PubMed] [Google Scholar]
- 8.Volta U, Bardella MT, Calabrò A, Troncone R, Corazza GR; Study Group for Non-Celiac Gluten Sensitivity. An Italian prospective multicenter survey on patients suspected of having non-celiac gluten sensitivity. BMC Med. 2014;12:85. doi: 10.1186/1741-7015-12-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rostami K, Hogg-Kollars S. A Patient’s Journey. Non-coeliac gluten sensitivity. BMJ. 2012;345:e7982. doi: 10.1136/bmj.e7982. [DOI] [PubMed] [Google Scholar]
- 10.DiGiacomo DV, Tennyson CA, Green PH, Demmer RT. Prevalence of gluten-free diet adherence among individuals without celiac disease in the USA: results from the Continuous National Health and Nutrition Examination Survey 2009-2010. Scand J Gastroenterol. 2013;48:921–925. doi: 10.3109/00365521.2013.809598. [DOI] [PubMed] [Google Scholar]
- 11.Choung RS, Ditah IC, Nadeau AM, Rubio-Tapia A, Marietta EV, Brantner TL, Camilleri MJ, Rajkumar SV, Landgren O, Everhart JE, et al. Trends and racial/ethnic disparities in gluten-sensitive problems in the United States: findings from the National Health and Nutrition Examination Surveys from 1988 to 2012. Am J Gastroenterol. 2015;110:455–461. doi: 10.1038/ajg.2015.8. [DOI] [PubMed] [Google Scholar]
- 12.Sapone A, Bai JC, Ciacci C, Dolinsek J, Green PH, Hadjivassiliou M, Kaukinen K, Rostami K, Sanders DS, Schumann M, et al. Spectrum of gluten-related disorders: consensus on new nomenclature and classification. BMC Med. 2012;10:13. doi: 10.1186/1741-7015-10-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caio G, Riegler G, Patturelli M, Facchiano A, DE Magistris L, Sapone A. Pathophysiology of non-celiac gluten sensitivity: where are we now? Minerva Gastroenterol Dietol. 2017;63:16–21. doi: 10.23736/S1121-421X.16.02346-1. [DOI] [PubMed] [Google Scholar]
- 14.Fasano A, Sapone A, Zevallos V, Schuppan D. Nonceliac gluten sensitivity. Gastroenterology. 2015;148:1195–1204. doi: 10.1053/j.gastro.2014.12.049. [DOI] [PubMed] [Google Scholar]
- 15.Volta U, Caio G, De Giorgio R, Henriksen C, Skodje G, Lundin KE. Non-celiac gluten sensitivity: a work-in-progress entity in the spectrum of wheat-related disorders. Best Pract Res Clin Gastroenterol. 2015;29:477–491. doi: 10.1016/j.bpg.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 16.Aziz I, Lewis NR, Hadjivassiliou M, Winfield SN, Rugg N, Kelsall A, Newrick L, Sanders DS. A UK study assessing the population prevalence of self-reported gluten sensitivity and referral characteristics to secondary care. Eur J Gastroenterol Hepatol. 2014;26:33–39. doi: 10.1097/01.meg.0000435546.87251.f7. [DOI] [PubMed] [Google Scholar]
- 17.Aziz I, Hadjivassiliou M, Sanders DS. The spectrum of noncoeliac gluten sensitivity. Nat Rev Gastroenterol Hepatol. 2015;12:516–526. doi: 10.1038/nrgastro.2015.107. [DOI] [PubMed] [Google Scholar]
- 18.Biesiekierski JR, Peters SL, Newnham ED, Rosella O, Muir JG, Gibson PR. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology. 2013;145:320–328.e1-3. doi: 10.1053/j.gastro.2013.04.051. [DOI] [PubMed] [Google Scholar]
- 19.Vazquez-Roque MI, Camilleri M, Smyrk T, Murray JA, Marietta E, O’Neill J, Carlson P, Lamsam J, Janzow D, Eckert D, et al. A controlled trial of gluten-free diet in patients with irritable bowel syndrome-diarrhea: effects on bowel frequency and intestinal function. Gastroenterology. 2013;144:903–911.e3. doi: 10.1053/j.gastro.2013.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hollon J, Puppa EL, Greenwald B, Goldberg E, Guerrerio A, Fasano A. Effect of gliadin on permeability of intestinal biopsy explants from celiac disease patients and patients with non-celiac gluten sensitivity. Nutrients. 2015;7:1565–1576. doi: 10.3390/nu7031565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sapone A, Lammers KM, Casolaro V, Cammarota M, Giuliano MT, De Rosa M, Stefanile R, Mazzarella G, Tolone C, Russo MI, et al. Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: celiac disease and gluten sensitivity. BMC Med. 2011;9:23. doi: 10.1186/1741-7015-9-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brottveit M, Beitnes AC, Tollefsen S, Bratlie JE, Jahnsen FL, Johansen FE, Sollid LM, Lundin KE. Mucosal cytokine response after short-term gluten challenge in celiac disease and non-celiac gluten sensitivity. Am J Gastroenterol. 2013;108:842–850. doi: 10.1038/ajg.2013.91. [DOI] [PubMed] [Google Scholar]
- 23.Volta U, Caio G, Karunaratne TB, Alaedini A, De Giorgio R. Non-coeliac gluten/wheat sensitivity: advances in knowledge and relevant questions. Expert Rev Gastroenterol Hepatol. 2017;11:9–18. doi: 10.1080/17474124.2017.1260003. [DOI] [PubMed] [Google Scholar]
- 24.Uhde M, Ajamian M, Caio G, De Giorgio R, Indart A, Green PH, Verna EC, Volta U, Alaedini A. Intestinal cell damage and systemic immune activation in individuals reporting sensitivity to wheat in the absence of coeliac disease. Gut. 2016;65:1930–1937. doi: 10.1136/gutjnl-2016-311964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kabbani TA, Vanga RR, Leffler DA, Villafuerte-Galvez J, Pallav K, Hansen J, Mukherjee R, Dennis M, Kelly CP. Celiac disease or non-celiac gluten sensitivity? An approach to clinical differential diagnosis. Am J Gastroenterol. 2014;109:741–746; quiz 747. doi: 10.1038/ajg.2014.41. [DOI] [PubMed] [Google Scholar]
- 26.Junker Y, Zeissig S, Kim SJ, Barisani D, Wieser H, Leffler DA, Zevallos V, Libermann TA, Dillon S, Freitag TL, et al. Wheat amylase trypsin inhibitors drive intestinal inflammation via activation of toll-like receptor 4. J Exp Med. 2012;209:2395–2408. doi: 10.1084/jem.20102660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ciccocioppo R, Di Sabatino A, Corazza GR. The immune recognition of gluten in coeliac disease. Clin Exp Immunol. 2005;140:408–416. doi: 10.1111/j.1365-2249.2005.02783.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Green PH, Cellier C. Celiac disease. N Engl J Med. 2007;357:1731–1743. doi: 10.1056/NEJMra071600. [DOI] [PubMed] [Google Scholar]
- 29.Sapone A, Lammers KM, Mazzarella G, Mikhailenko I, Cartenì M, Casolaro V, Fasano A. Differential mucosal IL-17 expression in two gliadin-induced disorders: gluten sensitivity and the autoimmune enteropathy celiac disease. Int Arch Allergy Immunol. 2010;152:75–80. doi: 10.1159/000260087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dubois B, Bertin P, Mingeot D. Molecular diversity of α-gliadin expressed genes in genetically contrasted spelt (<i>Triticum aestivum</i> ssp. <i>spelta</i>) accessions and comparison with bread wheat (<i>T. aestivum</i> ssp. <i>aestivum</i>) and related diploid <i>Triticum</i> and <i>Aegilops</i> species. Mol Breed. 2016;36:152. doi: 10.1007/s11032-016-0569-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pruimboom L, de Punder K. The opioid effects of gluten exorphins: asymptomatic celiac disease. J Health Popul Nutr. 2015;33:24. doi: 10.1186/s41043-015-0032-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sanz Y. Microbiome and Gluten. Ann Nutr Metab. 2015;67 Suppl 2:28–41. doi: 10.1159/000440991. [DOI] [PubMed] [Google Scholar]
- 33.Daulatzai MA. Non-celiac gluten sensitivity triggers gut dysbiosis, neuroinflammation, gut-brain axis dysfunction, and vulnerability for dementia. CNS Neurol Disord Drug Targets. 2015;14:110–131. doi: 10.2174/1871527314666150202152436. [DOI] [PubMed] [Google Scholar]
- 34.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 35.Narciso-Schiavon JL, Schiavon LL. To screen or not to screen? Celiac antibodies in liver diseases. World J Gastroenterol. 2017;23:776–791. doi: 10.3748/wjg.v23.i5.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Catassi C, Elli L, Bonaz B, Bouma G, Carroccio A, Castillejo G, Cellier C, Cristofori F, de Magistris L, Dolinsek J, et al. Diagnosis of Non-Celiac Gluten Sensitivity (NCGS): The Salerno Experts’ Criteria. Nutrients. 2015;7:4966–4977. doi: 10.3390/nu7064966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Molina-Infante J, Carroccio A. Suspected Nonceliac Gluten Sensitivity Confirmed in Few Patients After Gluten Challenge in Double-Blind, Placebo-Controlled Trials. Clin Gastroenterol Hepatol. 2017;15:339–348. doi: 10.1016/j.cgh.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 38.Van Overbeek FM, Uil-Dieterman IG, Mol IW, Köhler-Brands L, Heymans HS, Mulder CJ. The daily gluten intake in relatives of patients with coeliac disease compared with that of the general Dutch population. Eur J Gastroenterol Hepatol. 1997;9:1097–1099. doi: 10.1097/00042737-199711000-00013. [DOI] [PubMed] [Google Scholar]
- 39.Collyer EM, Kaplan BS. Nonceliac gluten sensitivity: an approach to diagnosis and management. Curr Opin Pediatr. 2016;28:638–643. doi: 10.1097/MOP.0000000000000392. [DOI] [PubMed] [Google Scholar]
- 40.Lebwohl B, Cao Y, Zong G, Hu FB, Green PHR, Neugut AI, Rimm EB, Sampson L, Dougherty LW, Giovannucci E, et al. Long term gluten consumption in adults without celiac disease and risk of coronary heart disease: prospective cohort study. BMJ. 2017;357:j1892. doi: 10.1136/bmj.j1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zong G, Lebwohl B, Hu F, Sampson L, Dougherty L, Willett W, Chan A, Sun Q. Abstract 11: Associations of Gluten Intake With Type 2 Diabetes Risk and Weight Gain in Three Large Prospective Cohort Studies of US Men and Women. 2017 doi: 10.1007/s00125-018-4697-9. Available from: https://www.researchgate.net/publication315515450_Associations_of_Gluten_Intake_With_Type_2_Diabetes_Risk_and_Weight_Gain_in_Three_Large_Prospective_Cohort_Studies_of_US_Men_and_Women. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Efficacy of Probiotic ES1 for the Treatment of Non-Celiac Gluten Sensitivity - Full Text View – ClinicalTrials gov. 2017. Available from: https://www.clinicaltrials.gov/show/NCT02810301.
- 43.Salden BN, Monserrat V, Troost FJ, Bruins MJ, Edens L, Bartholomé R, Haenen GR, Winkens B, Koning F, Masclee AA. Randomised clinical study: Aspergillus niger-derived enzyme digests gluten in the stomach of healthy volunteers. Aliment Pharmacol Ther. 2015;42:273–285. doi: 10.1111/apt.13266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Effect of AN-PEP Enzyme on Gluten Digestion in Gluten Sensitive Individuals - Full Text View – ClinicalTrials gov. 2017. Available from: https://www.clinicaltrials.gov/show/NCT02060864.
- 45.Gianfrani C, Camarca A, Mazzarella G, Di Stasio L, Giardullo N, Ferranti P, Picariello G, Rotondi Aufiero V, Picascia S, Troncone R, et al. Extensive in vitro gastrointestinal digestion markedly reduces the immune-toxicity of Triticum monococcum wheat: implication for celiac disease. Mol Nutr Food Res. 2015;59:1844–1854. doi: 10.1002/mnfr.201500126. [DOI] [PubMed] [Google Scholar]
- 46.Zevallos VF, Raker V, Tenzer S, Jimenez-Calvente C, Ashfaq-Khan M, Rüssel N, Pickert G, Schild H, Steinbrink K, Schuppan D. Nutritional Wheat Amylase-Trypsin Inhibitors Promote Intestinal Inflammation via Activation of Myeloid Cells. Gastroenterology. 2017;152:1100–1113.e12. doi: 10.1053/j.gastro.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 47.Mayer EA, Tillisch K. The brain-gut axis in abdominal pain syndromes. Annu Rev Med. 2011;62:381–396. doi: 10.1146/annurev-med-012309-103958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Taché Y, Martinez V, Wang L, Million M. CRF1 receptor signaling pathways are involved in stress-related alterations of colonic function and viscerosensitivity: implications for irritable bowel syndrome. Br J Pharmacol. 2004;141:1321–1330. doi: 10.1038/sj.bjp.0705760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.2017 ICD-10-CM Diagnosis Code K52. 29: Other allergic and dietetic gastroenteritis and colitis. 2017 Available from: http://www.icd10data.com/ICD10CM/Codes/K00-K95/K50-K52/K52-/K52.2. [Google Scholar]
- 50.Branchi F, Ferretti F, Norsa L, Roncoroni L, Conte D, Bardella MT, Elli L. Management of Nonceliac Gluten Sensitivity by Gastroenterology Specialists: Data from an Italian Survey. Biomed Res Int. 2015;2015:530136. doi: 10.1155/2015/530136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Barbaro MR, Cremon C, Caio G, Giorgio RD, Volta U, Stanghellini V, Barbara G. 247 Zonulin Serum Levels Are Increased in Non-Celiac Gluten Sensitivity and Irritable Bowel Syndrome With Diarrhea. Gastroenterology. 2015:148. [Google Scholar]
- 52.Catassi C, Bai JC, Bonaz B, Bouma G, Calabrò A, Carroccio A, Castillejo G, Ciacci C, Cristofori F, Dolinsek J, et al. Non-Celiac Gluten sensitivity: the new frontier of gluten related disorders. Nutrients. 2013;5:3839–3853. doi: 10.3390/nu5103839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hadjivassiliou M, Sanders DS, Grünewald RA, Woodroofe N, Boscolo S, Aeschlimann D. Gluten sensitivity: from gut to brain. Lancet Neurol. 2010;9:318–330. doi: 10.1016/S1474-4422(09)70290-X. [DOI] [PubMed] [Google Scholar]
- 54.Wahnschaffe U, Schulzke JD, Zeitz M, Ullrich R. Predictors of clinical response to gluten-free diet in patients diagnosed with diarrhea-predominant irritable bowel syndrome. Clin Gastroenterol Hepatol. 2007;5:844–850; quiz 769. doi: 10.1016/j.cgh.2007.03.021. [DOI] [PubMed] [Google Scholar]
- 55.Finnie C, Melchior S, Roepstorff P, Svensson B. Proteome analysis of grain filling and seed maturation in barley. Plant Physiol. 2002;129:1308–1319. doi: 10.1104/pp.003681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Elli L, Roncoroni L, Bardella MT. Non-celiac gluten sensitivity: Time for sifting the grain. World J Gastroenterol. 2015;21:8221–8226. doi: 10.3748/wjg.v21.i27.8221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Seyedmirzaee S, Hayatbakhsh MM, Ahmadi B, Baniasadi N, Bagheri Rafsanjani AM, Nikpoor AR, Mohammadi M. Serum immune biomarkers in irritable bowel syndrome. Clin Res Hepatol Gastroenterol. 2016;40:631–637. doi: 10.1016/j.clinre.2015.12.013. [DOI] [PubMed] [Google Scholar]
- 58.Gibson PR, Shepherd SJ. Food choice as a key management strategy for functional gastrointestinal symptoms. Am J Gastroenterol. 2012;107:657–666; quiz 667. doi: 10.1038/ajg.2012.49. [DOI] [PubMed] [Google Scholar]
- 59.Caio G, Volta U, Tovoli F, De Giorgio R. Effect of gluten free diet on immune response to gliadin in patients with non-celiac gluten sensitivity. BMC Gastroenterol. 2014;14:26. doi: 10.1186/1471-230X-14-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thompson T. Gluten contamination of commercial oat products in the United States. N Engl J Med. 2004:351: 2021–2022. doi: 10.1056/NEJM200411043511924. [DOI] [PubMed] [Google Scholar]
- 61.Shaker JL, Brickner RC, Findling JW, Kelly TM, Rapp R, Rizk G, Haddad JG, Schalch DS, Shenker Y. Hypocalcemia and skeletal disease as presenting features of celiac disease. Arch Intern Med. 1997;157:1013–1016. [PubMed] [Google Scholar]
- 62.West J, Logan RF, Smith CJ, Hubbard RB, Card TR. Malignancy and mortality in people with coeliac disease: population based cohort study. BMJ. 2004;329:716–719. doi: 10.1136/bmj.38169.486701.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ventura A, Magazzù G, Greco L. Duration of exposure to gluten and risk for autoimmune disorders in patients with celiac disease. SIGEP Study Group for Autoimmune Disorders in Celiac Disease. Gastroenterology. 1999;117:297–303. doi: 10.1053/gast.1999.0029900297. [DOI] [PubMed] [Google Scholar]
- 64.Pinto-Sánchez MI, Verdú EF. Non-coeliac gluten sensitivity: are we closer to separating the wheat from the chaff? Gut. 2016;65:1921–1922. doi: 10.1136/gutjnl-2016-312471. [DOI] [PubMed] [Google Scholar]
- 65.Frischmeyer-Guerrerio PA, Guerrerio AL, Oswald G, Chichester K, Myers L, Halushka MK, Oliva-Hemker M, Wood RA, Dietz HC. TGFβ receptor mutations impose a strong predisposition for human allergic disease. Sci Transl Med. 2013;5:195ra94. doi: 10.1126/scitranslmed.3006448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ford AC, Moayyedi P, Lacy BE, Lembo AJ, Saito YA, Schiller LR, Soffer EE, Spiegel BM, Quigley EM; Task Force on the Management of Functional Bowel Disorders. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am J Gastroenterol. 2014;109 Suppl 1:S2–26; quiz S27. doi: 10.1038/ajg.2014.187. [DOI] [PubMed] [Google Scholar]
- 67.Soares RL. Irritable bowel syndrome: a clinical review. World J Gastroenterol. 2014;20:12144–12160. doi: 10.3748/wjg.v20.i34.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Picarelli A, Borghini R, Di Tola M, Marino M, Urciuoli C, Isonne C, Puzzono M, Porowska B, Rumi G, Lonardi S, et al. Intestinal, Systemic, and Oral Gluten-related Alterations in Patients With Nonceliac Gluten Sensitivity. J Clin Gastroenterol. 2016;50:849–858. doi: 10.1097/MCG.0000000000000515. [DOI] [PubMed] [Google Scholar]
- 69.Mujagic Z, Tigchelaar EF, Zhernakova A, Ludwig T, Ramiro-Garcia J, Baranska A, Swertz MA, Masclee AA, Wijmenga C, van Schooten FJ, et al. A novel biomarker panel for irritable bowel syndrome and the application in the general population. Sci Rep. 2016;6:26420. doi: 10.1038/srep26420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.El-Salhy M. Irritable bowel syndrome: diagnosis and pathogenesis. World J Gastroenterol. 2012;18:5151–5163. doi: 10.3748/wjg.v18.i37.5151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.El-Salhy M, Hatlebakk JG, Hausken T. Reduction in duodenal endocrine cells in irritable bowel syndrome is associated with stem cell abnormalities. World J Gastroenterol. 2015;21:9577–9587. doi: 10.3748/wjg.v21.i32.9577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Romero-Adrian TB, Leal-Montiel J, Fernandez G. Celiac disease: Participation of Cytokines and Other Factors in the Immune Response. J Gastrointest Disord Liver Func. 2015;1:1–6. [Google Scholar]


