Abstract
There is still debate whether sintethic graft (polytetrafluoroethylene or Dacron) is equivalent to vein as bypass graft material for the above-knee femoropopliteal bypass. Therefore, we performed prospective randomized trial to compare vein with polytetrafluoroethylene/dacron for femoropopliteal bypasses with the distal anastomosis above the knee. Between January 2000 and June 2003, 121 femoropopliteal bypasses were performed. The indications for operation were severe claudication in 96 cases, rest pain in 16 cases, and ulceration in 9 cases. After randomization, 60 reversed saphenous venous bypasses and 61 polytetrafluoroethylene/ dacron bypasses were performed. No perioperative mortality was seen, and 5% of the patients had minor infections of the wound, not resulting in loss of the bypass, the limb, or life. After 5 years, 37% of the patients had died and 7% were lost to follow-up. Only once saphenous vein was necessary for coronary artery bypass grafting. Primary patency rates after 5 years were 76,6% for venous bypass grafts and 59,1% for polytetrafluoroethylene/dacron grafts (p=0,035). Secondary patency rates were 83,3% for vein and 69,2% for polytetrafluoroethylene/dacron bypasses (p = 0,036). In the venous group, 10 bypasses failed, leading to four new bypasses. In the polytetrafluoroethylene group, 22 bypasses failed, leading to 12 reinterventions. After 5 years of follow-up, we conclude that a bypass with saphenous vein has better patency rates at all intervals and needs fewer reoperations. Saphenous vein should be the graft material of choice for above-knee femoropopliteal bypasses and should not be preserved for reinterventions. Polytetrafluoroethylene/dacron is an acceptable alternative if the saphenous vein is not available.
Keywords: femoro-poplitealn bypass, above knee, saphenous vein graft, polytetrafloureth- ylen graft, Dacron graft
INTRODUCTION
It is generally accepted that autologous saphenous vein is the conduit of choice for a femoropoplitial bypass below the knee (1, 2, 3, 4, 5). For the femoropopliteal bypass with the distal anastomosis above the knee, controversy still exists whether prosthetic materials like polytetrafluoroethylene, Dacron, and human umbilical vein are equivalent to autologous saphenous vein. Studies supporting other conduit materials for bypass either are not randomized (6, 7) or do not compare prosthetic material with vein (8). In 2000, this randomized controlled trial was started in our institution to answer the following questions: 1) Are there any difference in cumulative patency rates between saphenous vein and polytetrafluoroethylene/Dacron bypass grafts? 2) What are the consequences of bypass failure? And 3) If polytetrafluoroethylene/Dacron is used, is the autologous vein still available and useful for more distal procedures or for coronary artery bypass grafting?
The conclusions, reported after 2 years of follow-up, were that there was no statistical significant difference in primary and secondary patency rates between vein and polytetrafluoroethylene/Dacron. In the suprageniculate position, polytetrafluoroethylene/Dacron could be an acceptable alternative for femoropopliteal bypass grafting in above-knee procedures, especially in patients with a short life expectancy. There was minimal use of preserved veins for other bypass procedures. However, the follow-up period was only 2 years. Before the start of this study, very few randomized trials comparing vein with polytetrafluoroethylene/Dacron were published. AbuRahma, Robinson, and Holt (10) found no difference in primary patency rates after 6 years. However, Johnson and Lee (11) reported significantly better primary patency rates for vein than for polytetrafluoroethylene after 5 years. This study reports the results of our prospective randomized trial with a 5-year follow-up period.
PATIENTS AND METHODS
Patients who underwent a femoropopliteal bypass operation between January 2000 and June 2003 were eligible for this study. All patients with disabling claudication, rest pain, or tissue-loss who underwent arterial reconstruction were included. Patients with an earlier arterial bypass graft procedure in the same leg or with the greater saphenous vein removed earlier were excluded. History was obtained from interviewing every patient and it included previous operations and risk factors for arterial occlusive disease (diabetes, smoking, cerebrovascular accidents, and cardiac history). In every patient, a hemodynamic profile was obtained, comprising the ankle blood pressures and a velocity profile of the common femoral, popliteal, and distal arteries at the level of the ankle. Also, an arteriogram was obtained with the transbrahcial or transfemoral route with the Seldinger technique. The popliteal and tibial arteries were scored in terms of open or occluded to grade the runoff (12). Patient consent was obtained in all cases. Before the operation, all patients received 1 g of cefasolin intravenously. Patients underwent operation with general or regional anesthesia. The operating surgeon inspected the popliteal artery and the saphenous vein. Above-knee grafting was performed when the above-knee popliteal artery was patent and suitable for anastomosis during the operation. When the quality of the greater saphenous vein was suitable for bypass grafting (e.g. with a diameter of more than 4 mm proximally and 3 mm distally), randomization took place with closed envelope allocation. Either the reversed vein or a stretched thin-walled 6-mm polytetrafluoroethylene or 6 mm Dacron prosthesis was used (depending on availability of the prosthetic material). Before clamping, heparin was given intravenously in a dose of 5000 international units. All anastomoses were made end-to-side with continuous 6-0 prolene sutures, proximal to the common femoral artery and distal to the popliteal artery. During the postoperative hospitalization patients were given Clexan 0,5 mg/kg, once a day. After discharge from the hospital oral 150 mg acetylsalicylic acid was given daily. Follow-up visits were carried out at discharge and thereafter at 6 weeks, 3 months, 6 months, and 1 year and every following year. Examination comprised history, physical examination, and hemodynamic profile. Graft occlusion was determined with a drop in distal blood pressure of more than 20% compared with a previous visit and a velocity profile consistent with collateral flow in the distal popliteal artery. If a polytetrafluoroethylene/ Dacron bypass occluded and the occlusion was detected within 7 days, a thrombectomy was performed. In all other cases, a policy of “wait and see” was followed if the patient had mild claudication developed. In cases of rest pain or necrosis, a redo bypass procedure was performed. The primary endpoint of the study was the patency of the bypass at the end of the fifth year. Patients could be included in the study twice for primary operation on either the left or the right limb. Analysis of the primary endpoint was performed per limb.
Primary patency was considered to be uninterrupted patency with no procedures performed on the bypass or the adjacent native vessel. Secondary patency was the patency after restoration of an occlusion or after a procedure to protect the bypass from occluding. Most of the original bypass and at least one of the anastomosis must have been retained in continuity (12). Randomization took place in 121 bypass graft operations in 109 patients between January 2000 and June 2003. The risk factors and angiographic results were equally divided between those who received a venous bypass graft and those who received a polytetrafluoroethylene/ Dacron bypass graft, except for diabetes mellitus, which was significantly lower in the venous group (Table 1).
TABLE 1.
Patient characteristics from included patients
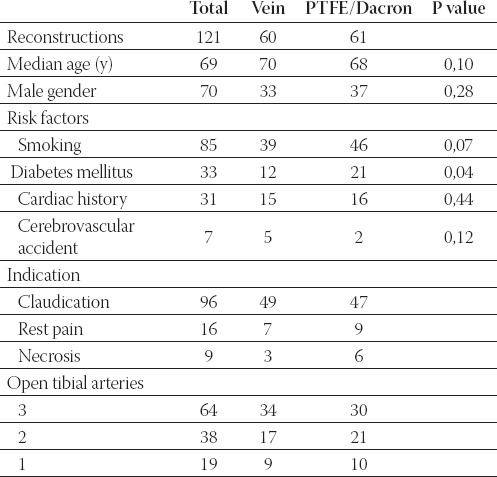
Reversed vein was used in 60 bypass grafts, and 6-mm stretched polytetrafluoroethylene or 6 mm Dacron prostheses were used 61 times. Bilateral reconstruction was done in 12 patients. Five patients received polytetrafluoroethylene/Dacron bypass grafts in both limb, two with bilateral venous bypass grafts, and five patients received polytetrafluoroethylene/Dacron in one limb and vein in the other.
The operating time from skin incision until skin closure was significantly longer in venous bypasses (mean, 125 minutes) than in polytetrafluoroethylene/Dacron grafts (mean, 73 minutes; p = 0,002). A superficial wound infection was seen in seven cases (three times with a polytetrafluoroethylene/Dacron and four times with a venous bypass). None of these infections resulted in reoperation or loss of the bypass. None of the patients died in the hospital or within 30 days after the operation.
RESULTS
After 5 years, 45 patients had died (37%); 34 with an open and 11 with an occluded bypass. Nine patients were lost to follow-up (7%). Primary patency rates after 5 years were 76,6% for venous bypass grafts and 59,1% for polytetrafluoroethylene/Dacron grafts (Tables 2 and 3).
TABLE 2.
Life-table analysis of primary patency rate of autologous saphenous vein
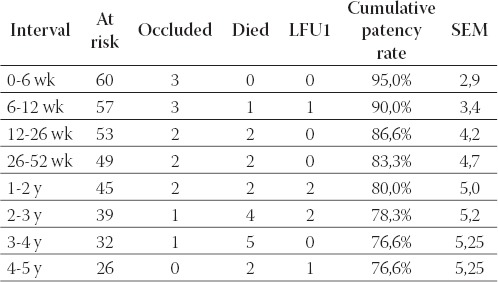
TABLE 3.
Life-table analysis of primary patency rate of polytetrafluo-roethylene/Dacron
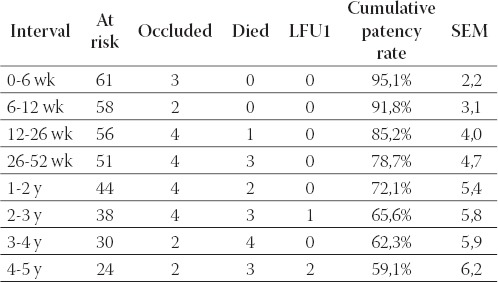
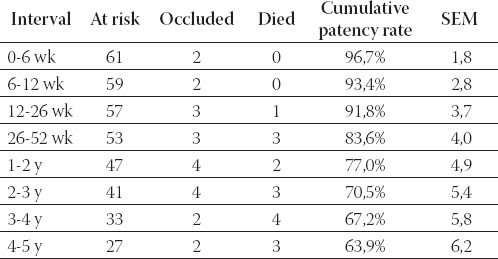
Secondary patency rates were 83,3% for vein and 63,9% for polytetrafluoroethylene/Dacron (Tables 4. and 5.).
TABLE 4.
Life-table analysis of secondary patency rate of autologous saphenous vein
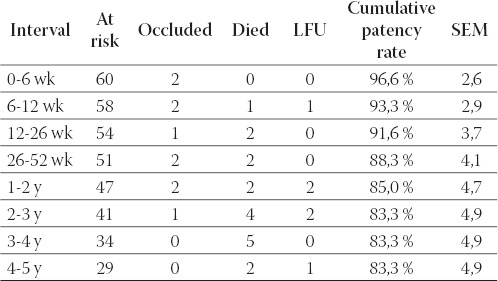
TABLE 5.
Life-table analysis of secondary patency rate of polytetra-fluoroethylene/Dacron
In the venous bypass group, 10 bypasses failed. In six patients, we did not perform a reintervention because the patient only had mild claudication. Four new bypass operations were performed: in three cases, a new polytetrafluoroethylene bypass was made above the knee and in one case, the venous bypass was extended with vein to below the knee for a femoroinfrapopliteal bypass. Failure of two of these redo bypasses led to two polytetrafluoroethylene femorotibial bypasses but finally to an occlusion and an amputation (above-knee). In this group, one coronary bypass operation was performed with the saphenous vein from the contralateral side as the graft material. In the polytetrafluoroethylene group, 22 bypasses failed. Ten times, no reinterventions were planned because the patients only had mild claudication. Because of severe claudication or rest pain, three times a new bypass above the knee was performed, all with polytetrafluoroethylene. Nine bypasses had to be performed below the knee: in seven cases, these were polytetrafluoroethylene bypasses; and in two cases, saphenous vein. One venous femorotibial bypass was constructed. There were significantly more reinterventions because of a failing polytetrafluoroethylene bypass graft compared with failing venous bypasses. Because of failed reinterventions, three patients received a polytetrafluoroethylene femorotibial bypass. Two amputations had to be performed (above-knee). In this group, two coronary bypass reconstructions were performed, but no bypass was constructed of saphenous vein.
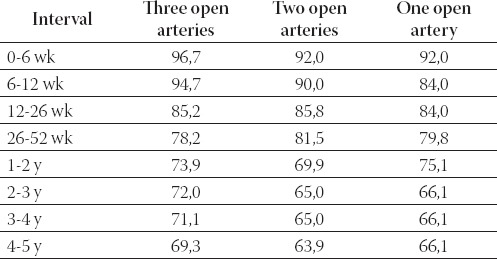
Primary patency rates were related to the outflow. After 5 years, the patency rates were 69,3% in the group with three open crural arteries, 63,9% with two open arteries, and 66,1% with one open artery (Table 6.).
TABLE 6.
Primary patency after 5 years compared with number of patent tibial arteries with preoperative arteriography.
DISCUSSION
The question of the best material for above-knee bypass graft surgery, polytetrafluoroethylene/Dacron or saphenous vein, was once controversial. The problem with many of these randomized trials, including our own, was that patient recruitment proved to be difficult, resulting in deficient power for conclusion. Our conclusion after 2 years of follow-up was that polytetrafluoroethylene/Dacron was a reasonable alternative but that long-term results should be awaited. Another problem is that follow-up is often deficient. With respect to follow-up, we were successful in seeing all but nine of our patients in the outpatient clinic. After 5 years of follow-up, we found a significant difference in primary patency rates of 76,6% for vein and 59,1% for polytetrafluoroethylene/Dacron (p = 0,035). The secondary patency rates were 83,3% and 63,9%, respectively (p = 0,036).
In Table 7., our results are compared with the three other published randomized trials (5, 10, 11).
TABLE 7.
Comparisons of primary patency rates of venous and polytetrafluoroethylene or Dacron bypass grafts from randomized controlled trials
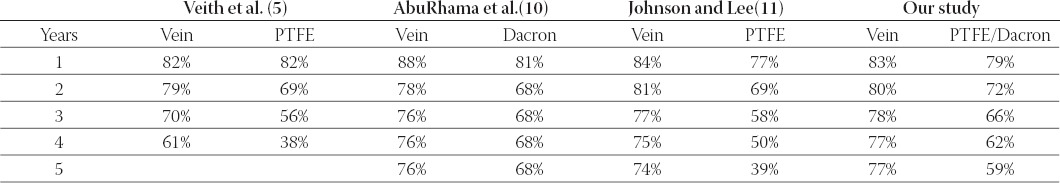
The difference between the four studies is that in the series of Veith et al. (5) and Johnson and Lee (11), 87% and 72%, respectively, of the patients had severe ischemia (rest pain or necrosis). This differs from our series (20%) and the series of AbuRahma, Robinson, and Holt (0%)(10). It can be expected that the outflow in patients with severe ischemia is poor compared with those with claudication. This might explain the less favorable long-term patency rates described by Veith et al and Johnson and Lee (38% and 39%, respectively). Michaels (15) estimated that 160 grafts are required in the two randomized groups to have a 95% chance of showing significance (P < 0,05), assuming that there is a 20% difference in 5-year patency rates. Despite the fact that we did not include that many patients, we found a statistical difference in favor of venous graft material. Johnson and Lee presented the only other trial with a statistically significant difference between vein and polytetrafluoroethylene. They included 226 patients in the venous group and 265 in the polytetrafluoroethylene group. If we compare the patency rates for vein and polytetrafluoroethylene in all four randomized trials, we see at all intervals a better primary patency rate for vein. It was shown in a critical review as well that if saphenous vein is available, a venous bypass should be chosen (15). When the saphenous vein is absent or not suitable for bypass grafting, polytetrafluoroethylene or Dacron is a good alternative for femoropopliteal bypass material above the knee. The only statistically significant risk factor difference between the two groups was the prevalence of diabetes, with significantly more patients in the polytetrafluoroethylene/Dacron group. Evans et al (16) and Prendiville et al (17) found that diabetes has a negative influence on the patency of the bypass, whereas others did not find that effect (6, 18). Because of the small numbers of patients with risk factors, no multivariate analysis could be performed. In 10 failing venous bypasses, four patients had critical ischemia and needed a reoperation. In the polytetrafluoroethylene/Dacron group, 12 reoperations had to be performed for 22 failing bypass grafts. Ten bypasses had to be placed below the knee. Clearly, less reoperation had to be performed in the venous group. The fact that in the polytetrafluoroethylene/ Dacron group during reoperation the distal anastomosis was more often below the knee might strengthen the idea that the polytetrafluoroethylene/Dacron graft promotes progression of distal atherosclerosis (5, 7). One of the arguments for use of polytetrafluoroethylene/Dacron for the above-knee femoropopliteal bypass graft is preservation of the vein for a later distal procedure or a coronary bypass. In the group of 61 polytetrafluoroethylene/Dacron bypasses, thus the group in which the vein was preserved, 22 graft failures occurred, with necessity for a venous bypass in only two cases. Two coronary bypasses were performed with the mammary artery in this patient group during the follow-up period. In other studies, these similar conclusions were made (19, 20). So, it seems unnecessary to save the vein because in case of a failing bypass graft the spared vein was not used often. Moreover, if the vein were used for the above-knee bypass, less reoperations had to be performed below the knee with need for the vein. When an infrapopliteal bypass or a coronary bypass is needed, the saphenous vein of the contralateral side is still available. To save the saphenous vein for coronary bypass grafts can be argued because of the advancement of cardiac revascularisation techniques, for example, percutaneous treatment or the use of the mammary artery.
Finally, four major amputations had to be performed: all upper leg amputations. In three of these cases, the indication for the femoropopliteal bypass was critical ischemia. These results are comparable with the results described by Johnson and Lee, although they performed more bypasses in patients with critical ischemia. AbuRahma, Robinson, and Holt had no amputations at all and performed bypasses in patients with claudication only. Veith et al described limb salvage rates of 77% after 4 years but also had many patients with critical ischemia. No difference was seen between the venous and the polytetrafluoroethylene/Dacron group. Although the use of polytetrafluoroethylene/ Dacron for aboveknee bypass did not result in a significant increase in major limb amputation rates compared with use of vein conduits, the patency rates for polytetrafluoroethylene/Dacron were distinctly inferior to those of vein and significantly more reinterventions were necessary to maintain equivalent limb salvages rates in this series consisting primarily of patients with claudication. An advantage of polytetrafluoroethylene/Dacron is the significantly shorter operation time. One can consider in patients with short life expectancy and high operative risk use of polytetrafluoroethylene/ Dacron as bypass graft material (9). Some authors showed that the runoff (number of patent tibial arteries) did influence the patency of bypass grafts (17). We found no significant differences between good and poor runoff for either venous and polytetrafluoroethylene/Dacron bypass grafts. This could be explained either by the small size of the group or by the relatively proximal site of the distal anastomosis.
CONCLUSION
Our conclusion after 2 years of follow-up was that polytetrafluoroethylene/Dacron could be safely used for above-knee femoropopliteal bypass in patients with compromised conditions and in those with short life expectancy. The current results after 5 years of follow-up show that saphenous vein has better patency rates at all intervals and needs fewer reoperations and that saphenous vein should not be spared for reinterventions. We therefore now prefer the vein as graft material in our institution for all patients needing an above-knee bypass procedure. Polytetrafluoroethylene/Dacron is an acceptable alternative when the saphenous vein is not available.
List of Abbreviations
PTFE -Polytetrafluoroethylene
LFU -Lost to follow-up
SEM -Standard error of mean
REFERENCES
- 1.Bergan JJ, Veith FJ, Bernhard VM, Yao JS, Flinn WR, Gupta SK, et al. Randomization of autogenous vein and polytetrafluo-rethylene grafts in femoral-distal reconstruction. Surgery. 1982;92:921–930. [PubMed] [Google Scholar]
- 2.Londrey GL, Ramsey DE, Hodgson KJ, Barkmeier LD, Sumner DS. Infrapopliteal bypass for severe ischemia: comparison of autogenous vein, composite, and prosthetic grafts. J. Vasc. Surg. 1991;13:631–636. [PubMed] [Google Scholar]
- 3.Sayers RD, Raptis S, Berce M, Miller JH. Long-term results of femorotibial bypass with vein or polytetrafluoroethylene. Br. J. Surg. 1998;85:934–938. doi: 10.1046/j.1365-2168.1998.00765.x. [DOI] [PubMed] [Google Scholar]
- 4.Van de Pavoordt HD, Eikelboom BC, De Geest R, Vermeulen FE. Results of prosthetic grafts in femoro-crural bypass operations as compared to autogenous saphenous vein grafts. Neth. J. Surg. 1986;38:177–179. [PubMed] [Google Scholar]
- 5.Veith FJ, Gupta SK, Ascer E, White-Flores S, Samson RH, Scher LA, et al. Six-year prospective multicenter randomized comparison of autologous saphenous vein and expanded polytetrafluoroethylene grafts in infrainguinal arterial reconstructions. J. Vasc. Surg. 1986;3:104–114. doi: 10.1067/mva.1986.avs0030104. [DOI] [PubMed] [Google Scholar]
- 6.O’Riordain DS, Buckley DJ, O’Donnell JA. Polytetrafluoroethylene in above-knee arterial bypass surgery for critical ischemia. Am. J. Surg. 1992;164:129–131. doi: 10.1016/s0002-9610(05)80370-8. [DOI] [PubMed] [Google Scholar]
- 7.Quinones-Baldrich WJ, Prego AA, Ucelay-Gomez R, Freischlag JA, Ahn SS, Baker JD, et al. Long-term results of infrainguinal revascularization with polytetrafluoroethylene: a ten-year experience. J. Vasc. Surg. 1992;16:209–217. [PubMed] [Google Scholar]
- 8.Abbott WM, Green RM, Matsumoto T, Wheeler JR, Miller N, Veith FJ, et al. Prosthetic above-knee femoropopliteal bypass grafting: results of a multicenter randomized prospective trial. Above-Knee Femoropopliteal Study Group. [see comments] J. Vasc. Surg. 1997;25:19–28. doi: 10.1016/s0741-5214(97)70317-3. [DOI] [PubMed] [Google Scholar]
- 9.AbuRahma AF, Robinson PA, Holt SM. Prospective controlled study of Dacron versus saphenous vein in claudicant patients with bilateral above knee femoropopliteal bypasses. Surgery. 1999;126:594–601. [PubMed] [Google Scholar]
- 10.Johnson WC, Lee KK. A comparative evaluation of polytetrafluoroethylene, umbilical vein, and saphenous vein bypass grafts for femoral-popliteal above-knee revascularization: a prospective randomized Department ofVeterans Affairs cooperative study. J. Vasc. Surg. 2000;32:268–277. doi: 10.1067/mva.2000.106944. [DOI] [PubMed] [Google Scholar]
- 11.Rutherford RB, Baker JD, Ernst C, Johnston KW, Porter JM, Ahn S, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc. Surg. 1997;26:517–538. doi: 10.1016/s0741-5214(97)70045-4. [DOI] [PubMed] [Google Scholar]
- 12.Mills JL. P values may lack power: the choice of conduit for above-knee femoropopliteal bypass graft. J. Vasc. Surg. 2000;32:402–405. doi: 10.1067/mva.2000.106495. [DOI] [PubMed] [Google Scholar]
- 13.Peto R, Pike MC, Armitage P, Breslow NE, Cox DR, Howard SV, et al. Design and analysis of randomized clinical trials requiring prolonged observation of each patient. I. Introduction and design. Br. J. Cancer. 1976;34:585–612. doi: 10.1038/bjc.1976.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Michaels JA. Choice of material for above-knee femoropopliteal bypass graft. Br. J. Surg. 1989;76:7–14. doi: 10.1002/bjs.1800760105. [DOI] [PubMed] [Google Scholar]
- 15.Evans LE, Webster MW, Brooks DH, Bahnson HT. Expanded polytetrafluoroethylene femoropopliteal grafts: forty-eight-month follow-up. Surgery. 1981;89:16–22. [PubMed] [Google Scholar]
- 16.Prendiville EJ, Yeager A, O’Donnell TF, Coleman JC, Jaworek A, Callow AD, et al. Long-term results with the above-knee popliteal expanded polytetrafluoroethylene graft. J Vasc Surg. 1990;11:517–524. [PubMed] [Google Scholar]
- 17.Rutherford RB, Jones DN, Bergentz SE, Bergqvist D, Comerota AJ, Dardik H, et al. Factors affecting the patency of infrainguinal bypass. J. Vasc. Surg. 1988;8:236–246. [PubMed] [Google Scholar]
- 18.Poletti LF, Matsuura JH, Dattilo JB, Posner MP, Lee HM, Scouvart M, et al. Should vein be saved for future operations? A 15-year review of infrainguinal bypasses and the subsequent need for autogenous vein. Ann. Vasc. Surg. 1998;12:143–147. doi: 10.1007/s100169900131. [DOI] [PubMed] [Google Scholar]
- 19.Sterpetti AV, Schultz RD, Feldhaus RJ, Peetz DJ. Seven-year experience with polytetrafluoroethylene as above-knee femoropopliteal bypass graft. Is it worthwhile to preserve the autologous saphenous vein? J. Vasc. Surg. 1985;2:907–912. [PubMed] [Google Scholar]


